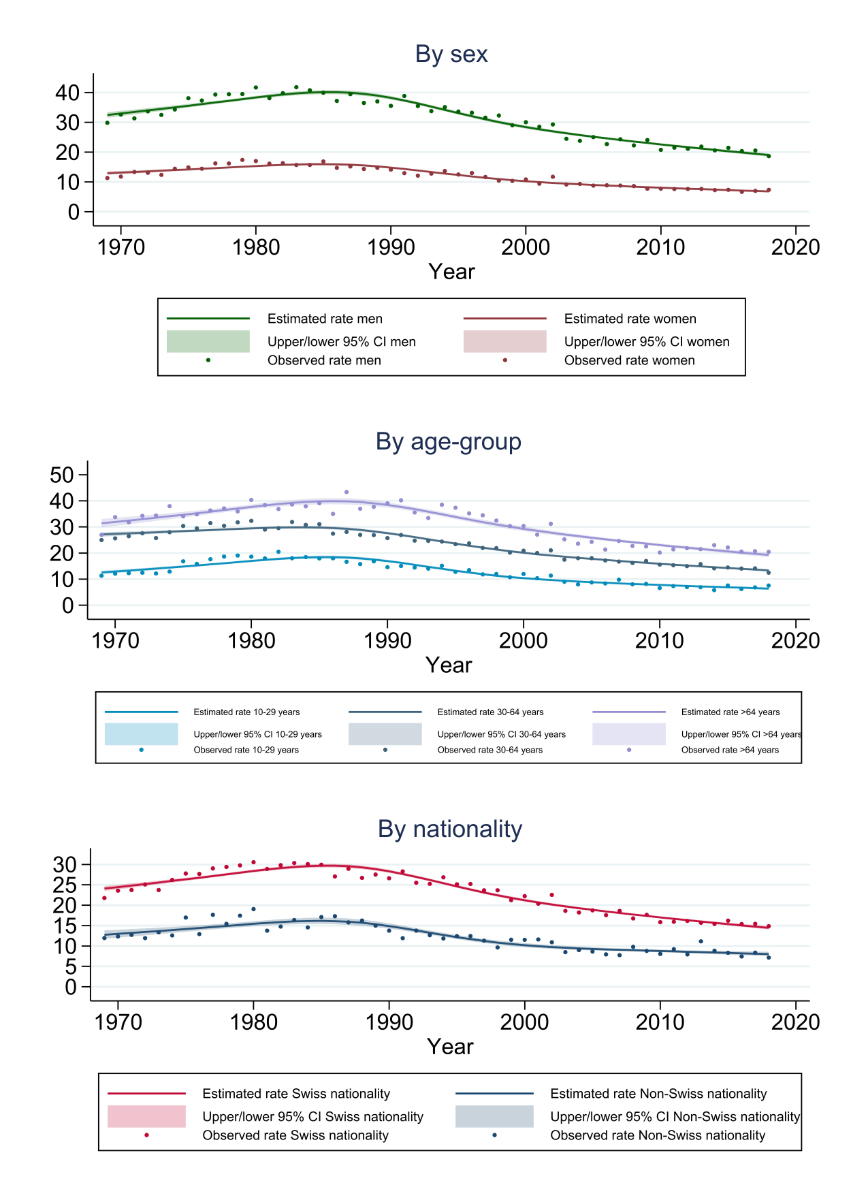
Figure 1 Suicide rates per 100,000 population (person-years). Note: estimated true rates and associated confidence intervals (CI) were derived from Poisson regressions using a restricted cubic-spline model.
DOI: https://doi.org/10.57187/smw.2022.40007
Suicide is a serious societal and public health problem [1]. Worldwide, more than 700,000 people die due to suicide every year, placing suicide among the twenty leading causes of death [1]. Suicide may occur over the whole lifespan and is the most frequent cause of death among 15–24-year-olds globally [2]. According to the diathesis-stress model, suicidal behaviour can be triggered by internal stressors (e.g., mental disorders) or by external stressors (e.g., life-events) if they come across with predisposing biological or psychological characteristics (e.g., heightened perception of emotional distress or greater propensity for emotion to influence decisions) [3, 4]. Due to the economic and human costs of suicidal behaviour to individuals, families, communities and society [5], the World Health Organization (WHO) has prioritised suicide prevention and declared the reduction of suicide mortality by one third until 2030 as a global target [1, 6, 7]. Accordingly, the suicide rate is a health indicator of the United Nations Sustainable Development Goals [1].
In Switzerland, the population-based suicide rate declined after reaching a peak in the 1980s [8]. Nevertheless, there are still approximately 1000 suicides every year [9], which is around five times the number road traffic fatalities [10].
International data showed age-, gender- and region-specific differences in the methods of suicide used [2, 11–13]. Different groups of people may have different access to lethal methods and/or they may be attracted by different means of suicide [14]. As the availability of lethal means was shown to affect the methods of suicide used [15–18], restricting access to lethal methods is an important suicide prevention strategy [3, 6, 19]. Knowledge of the most commonly used methods of suicide [1] and a better understanding of the dynamics over time of the suicide methods used [8] may inform targeted and adequate preventive and control measures [7].
In Switzerland, Hepp et al. [8] found diverging calendar time trends for different methods of suicide between 1969 and 2005. The current study aimed to extend these descriptive analyses by including more recent years (up to 2018), the application of more sophisticated statistical methods (Poisson regression models for rate events in order to estimate the true rates of completed suicides behind the observed numbers), and by in-depth analyses of calendar time trends of specific suicide methods in population subgroups (age, gender and nationality subgroups). Specifically, we aimed at answering the following research questions: (1) Did the population-based rates of specific suicide methods used in Switzerland change over the latest five decades (1969–2018)? (2) Did these calendar time trends in the rates of the suicide methods used differ depending on age, sex and nationality (Swiss vs other citizenship)?
Based on previous findings [8], we expected diverging time trends for specific methods of suicide over the latest five decades. Likewise, we expected that at least some of these time trends differ depending on age, sex and/or nationality. However, subgroup analyses were exploratory and no specific hypotheses were formulated regarding the role of age, gender and nationality.
We performed secondary analyses of the Swiss cause of death statistics [20] for the period 1969–2018. Incidence rates and calendar time trends of specific suicide methods were examined in population subgroups which were stratified according to sex (men vs women), age (10–29, 30–64, >64 years), and nationality (Swiss vs other citizenship).
The Swiss cause of death statistics, courtesy of the Federal Statistical Office (FSO), is a mandatory and comprehensive registration based on data from civil registries and on death certificates issued by physicians [20]. Data have been available in electronic form since 1969 and include the following information for all deceased persons in the permanent resident population of Switzerland: causes of death, age, sex, civil status, occupation (with low data quality), commune of residence (civil domicile) and nationality [20]. There is almost full data coverage on cause of death for all deceased persons (only about 2% missing data) [17]. Causes of death are coded according to the WHO's International Classification of Diseases (ICD) [21, 22]. Registration rules prescribe the highest priority to violent causes of death; therefore, suicides are usually registered as the main cause of death [8]. In Switzerland, suicides are routinely investigated by the police and by legal medicine because they are a violent cause of death; an autopsy is not performed in all cases, however [8]. In 1995, there was a revision of the Swiss cause of death statistics with transition from ICD-8 [22] to ICD-10 [21]. A separate ICD-10 code for assisted suicide (X61.8) was introduced in 1998 and allows for the analysis of assisted suicides since then [8].
Data on the permanent resident population to calculate annual suicide rates were based on the population statistics of the FSO [23] (see appendix, table S1).
Methods of suicide were grouped into nine categories based on ICD-8 and ICD-10 codes, respectively [21, 22]: (1) poisoning by solid or liquid substances (exclusive of assisted suicides) (ICD-8: 950 / ICD-10: X60-X66.9); (2) poisoning by gases (952 / X67-X69.9); (3) hanging, strangulation or suffocation (953 / X70-X70.9); (4) drowning or submersion (954 / X71-X71.9); (5) firearms or explosives (955 / X72-X75.9); (6) cutting by sharp or blunt objects (956 / X78-X79.9), (7) jumping from high places (957 / X80-X80.9), (8) jumping or lying in front of moving object (particularly trains) (958.00 / X81.8); and (9) other means (951, 958 (exclusive of 958.00), 959 / other ICD-10 codes).
For the years 1970 and earlier, the FSO had no annual population data stratified according to age, sex and nationality [23]. We therefore substituted the number of inhabitants in population subgroups (e.g., Swiss men over 64 years) for the years 1969 and 1970 with the respective figures of 1971.
We used Poisson regression models to analyse annual incidence rates and calendar time trends of specific suicide methods used in specific subpopulations in Switzerland between 1969–2018. Poisson regression is the standard approach to analyse incidence rates in prospective studies [24]. In Poisson regression models, the natural log (In) of the incidence rate of events (e.g., the ln of the suicide rate) is modelled as a linear function of the predictor variables (e.g., calendar time or nationality) [24]. The exposure time or the population denominator are included as an offset term in the regression equation for model estimation in statistical software [24], such as STATA version 16 [25] used in this study.
We first estimated smoothed curves for true annual incidence rates of specific suicide methods using a restricted (natural) cubic-spline model with knots set at 10-year intervals (1978, 1988, 1998, and 2008) [26]. Spline functions are piecewise polynomials used in curve fitting to model nonlinear relationships [27] trough the transformation of an independent variable (e.g., calendar time) [28]. Cubic polynomials were found to have good ability to fit sharply curving shapes and they can be made to be smooth at the join points (knots) by forcing the first and second derivatives of the function to agree at the knots [27]. Since cubic spline functions can behave poorly (be unstable) at the tails, constraining the function to be linear before the first and after the last knot has been recommended (therefore called restricted or natural splines) [29]. It was shown that the location of the knots (which has to be specified in advance) is not very crucial in restricted cubic spline models in most situations; the model fit depends much more on the number of knots [30]. For many datasets, k = 4 knots offers an adequate fit of the model and is a good compromise between flexibility and loss of precision caused by overfitting a small sample [27]. Following this recommendation, we used restricted cubic-spline models with k = 4 knots (set at 1978, 1988, 1998, and 2008) to estimate calendar time trends of annual suicide rates in population subgroups which were stratified according to sex and age groups [26].
In addition, we estimated Poisson regression models with the predictors calendar-time period (1969–1978, 1979–1988, etc.) and nationality to examine the impact of these predictors on the (true) rates of specific suicide methods. These analyses were again stratified for sex and age groups, and results were reported in terms of incidence rate ratios (IRRs) between time periods and nationalities, respectively.
We considered two-sided p <0.05 to be statistically significant and we report 95% confidence intervals (CIs) of the modelled rates. Please note that the 95% CIs relate to the uncertainty of the estimated rates behind the observed numbers (and not to the observed rates, which were realised under the assumption of these true rates); that is, the 95% CIs do not represent prediction intervals for the observed rates.
Statistical analyses were performed with STATA version 16 [25] and the program "grc1leg2" (http://digital.cgdev.org/doc/stata/MO/Misc) to customise graphs. A study protocol has not been prepared and registered.
The responsible ethics committee of the canton of Zurich declared that the study does not fall within the scope of the Swiss Human Research Act (HRA). Therefore, the approval of study protocols and the need of informed consent were waived by the ethics committee of the canton of Zurich (BASEC-Nr. Req-2021-01125).
There were 64,996 suicides registered in Switzerland between 1969 and 2018 (table 1).
Table 1Number of suicides in Switzerland (1969–2018).
| Age group | Sex | Nationality | Period | Total | ||||
| 1969-1978 | 1979-1988 | 1989-1998 | 1999-2008 | 2009-2018 | ||||
| 10-29 years | Male | Swiss | 1924 | 2433 | 1826 | 1114 | 820 | 8117 |
| Other | 185 | 238 | 230 | 166 | 174 | 993 | ||
| Female | Swiss | 539 | 701 | 400 | 352 | 262 | 2254 | |
| Other | 92 | 70 | 83 | 61 | 50 | 356 | ||
| 30-64 years | Male | Swiss | 4685 | 5339 | 5088 | 4257 | 3533 | 22902 |
| Other | 517 | 639 | 646 | 639 | 740 | 3181 | ||
| Female | Swiss | 2064 | 2424 | 2'093 | 1693 | 1418 | 9692 | |
| Other | 193 | 236 | 198 | 212 | 253 | 1092 | ||
| >64 years | Male | Swiss | 1704 | 2179 | 2419 | 2034 | 2163 | 10499 |
| Other | 81 | 107 | 124 | 137 | 204 | 653 | ||
| Female | Swiss | 913 | 1216 | 1'200 | 885 | 746 | 4960 | |
| Other | 51 | 63 | 78 | 59 | 46 | 297 | ||
| Total | 12948 | 15645 | 14385 | 11609 | 10409 | 64996 | ||
This figure resulted after excluding two suicides of 9-year-old boys and 8781 assisted suicides. After peaking in the 1980s, the population-based overall suicide rate declined over most recent decades in both sexes, in Swiss and foreign citizens, and in young (10–29 years), middle-aged (30–64 years) and older (>64 years) inhabitants (fig. 1). Across the five decades studied, the overall suicide rate was higher in men than in women (IRR 2.622, 95% CI 2.577–2.666), in Swiss citizens than in residents with foreign nationality (IRR 2.019, 95% CI 1.968–2.071), and in older inhabitants than in middle-aged (IRR 1.348, 95% CI 1.324–1.373) and younger inhabitants (IRR 2.374, 95% CI 2.319–2.431). Hanging accounted for most suicides over the 50-year study period (26.7%), followed by firearms (23.6%), poisoning by solid or liquid substances (12.7%) and jumping form high places (11.1%) (table 2).
Table 2Methods of suicides used in Switzerland (1969–2018).
| Suicide method | ICD-8 code | ICD-10 code | Absolute frequency | Relative frequency | Rate per 100000 person-years | Absolute frequency | Relative frequency | Rate per 100000 person-years | Absolute frequency | Relative frequency | Rate per 100000 person-years |
| Men | Women | All | |||||||||
| Poisoning by solid or liquid substances1 | 950 | X60-X66.9 | 3893 | 8.4% | 2.56 | 4336 | 23.2% | 2.70 | 8229 | 12.7% | 2.63 |
| Poisoning by gases | 952 | X67-X69.9 | 2882 | 6.2% | 1.89 | 570 | 3.1% | 0.36 | 3452 | 5.3% | 1.10 |
| Hanging, strangulation or suffocation | 953 | X70-X70.9 | 13486 | 29.1% | 8.86 | 3849 | 20.6% | 2.40 | 17335 | 26.7% | 5.54 |
| Drowning or submersion | 954 | X71-X71.9 | 2252 | 4.9% | 1.48 | 2926 | 15.7% | 1.82 | 5178 | 8.0% | 1.66 |
| Firearms or explosives | 955 | X72-X75.9 | 14615 | 31.5% | 9.61 | 694 | 3.7% | 0.43 | 15309 | 23.6% | 4.90 |
| Cutting by sharp or blunt objects | 956 | X78-X79.9 | 1020 | 2.2% | 0.67 | 359 | 1.9% | 0.22 | 1379 | 2.1% | 0.44 |
| Jumping from high places | 957 | X80-X80.9 | 3944 | 8.5% | 2.59 | 3291 | 17.6% | 2.05 | 7235 | 11.1% | 2.31 |
| Jumping or lying in front of moving object (particularly railway) | 958.00 | X81.8 | 3145 | 6.8% | 2.07 | 1915 | 10.3% | 1.19 | 5060 | 7.8% | 1.62 |
| Other | 1108 | 2.4% | 0.73 | 711 | 3.8% | 0.44 | 1819 | 2.8% | 0.58 | ||
| All methods | 46345 | 100.0% | 30.46 | 18651 | 100.0% | 11.62 | 64996 | 100.0% | 20.79 | ||
1 Exlusive of assisted suicides.
Subsequently, the most common methods of suicide will be described with particular regard to deviations from these overall trends and patterns as well as regarding their relevance in population subgroups in most recent years.
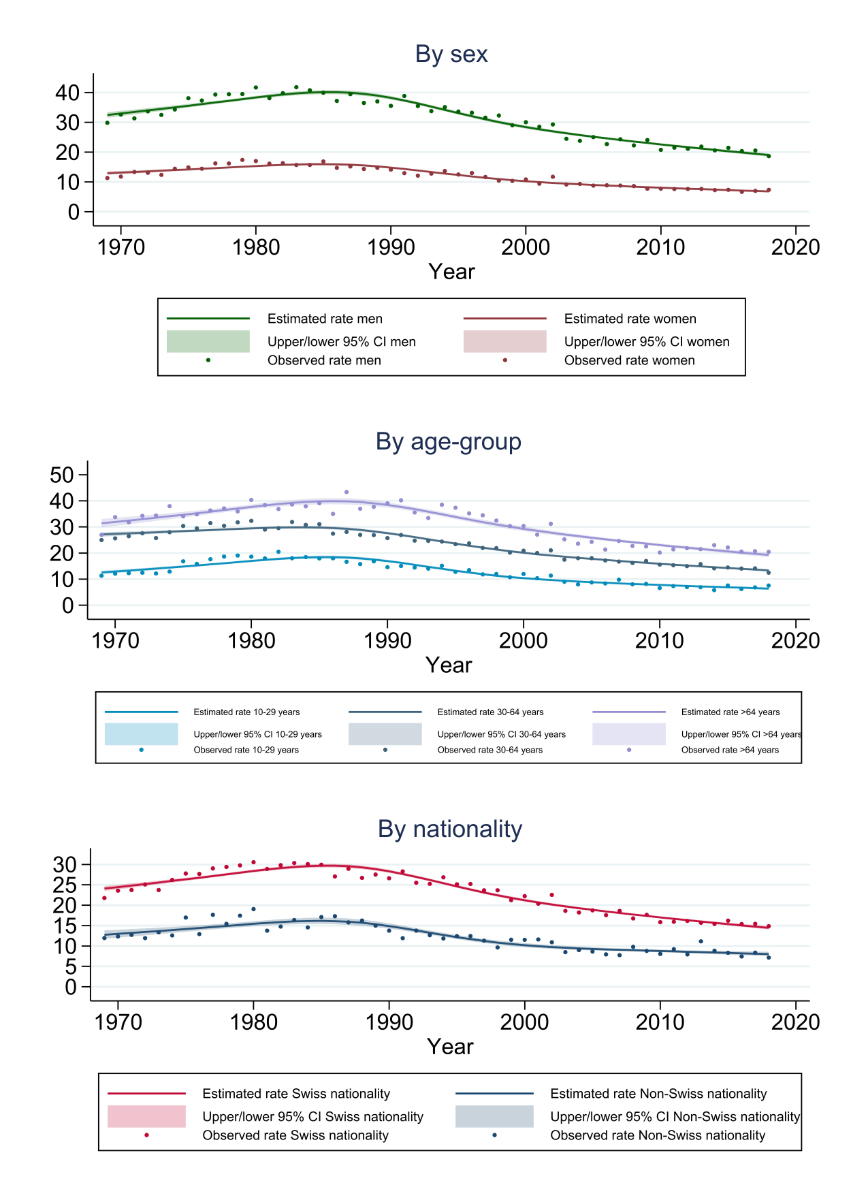
Figure 1 Suicide rates per 100,000 population (person-years). Note: estimated true rates and associated confidence intervals (CI) were derived from Poisson regressions using a restricted cubic-spline model.
Although most suicide methods were more often used by men than by women, the estimated population-based incidence rates for suicides by poisoning with solid or liquid substances developed on a rather similar level for both sexes between 1969 and 2018 (figures 2–4). In addition, the incidence rates were not consistently lower and sometimes even higher among foreigners than among Swiss citizens (tables 3 and 4). There was a downward trend in suicides by poisoning over more recent decades in all population subgroups (appendix, figures S1 and S2). This trend started with some delay in older people (>64 years), however (figures 2–4).
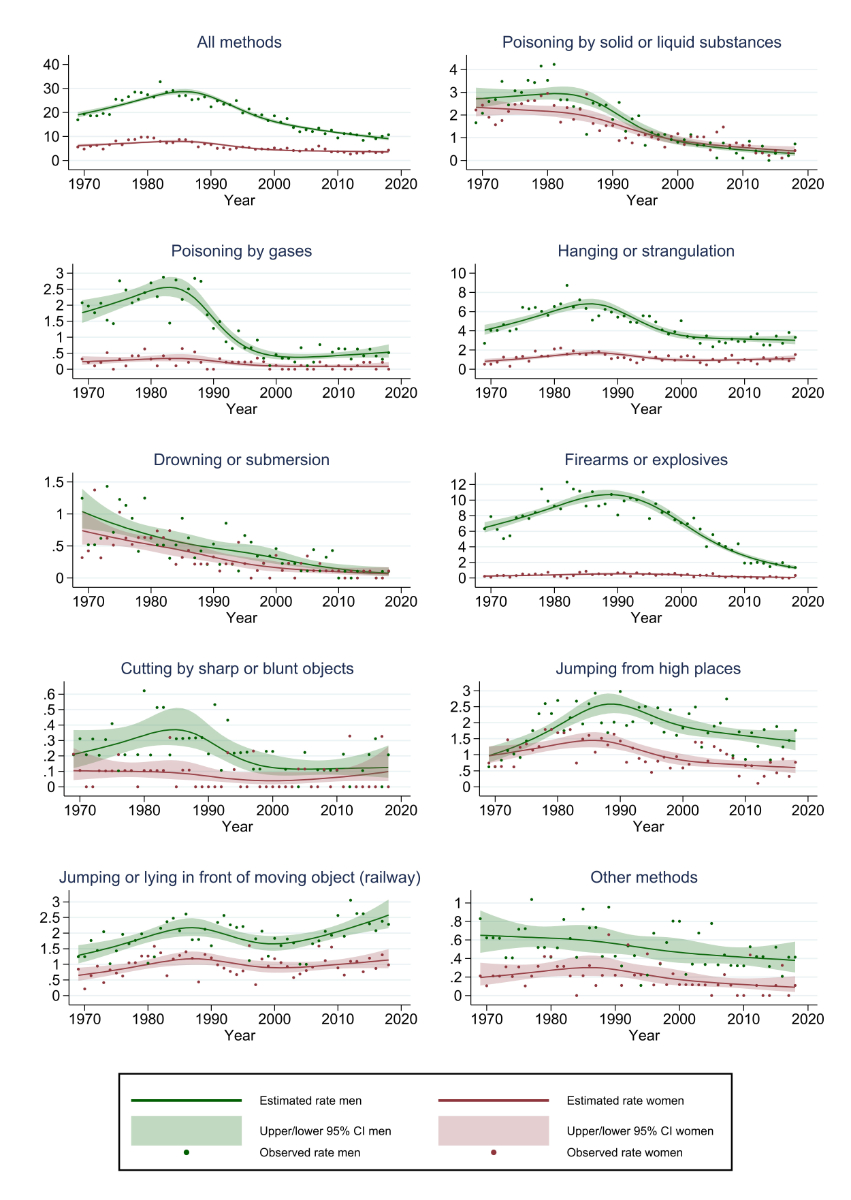
Figure 2 Rates of suicide methods per 100,000 population (person-years) in the age group 10–29 years. Note: estimated true rates and associated confidence intervals (CI) were derived from Poisson regressions using a restricted cubic-spline model.
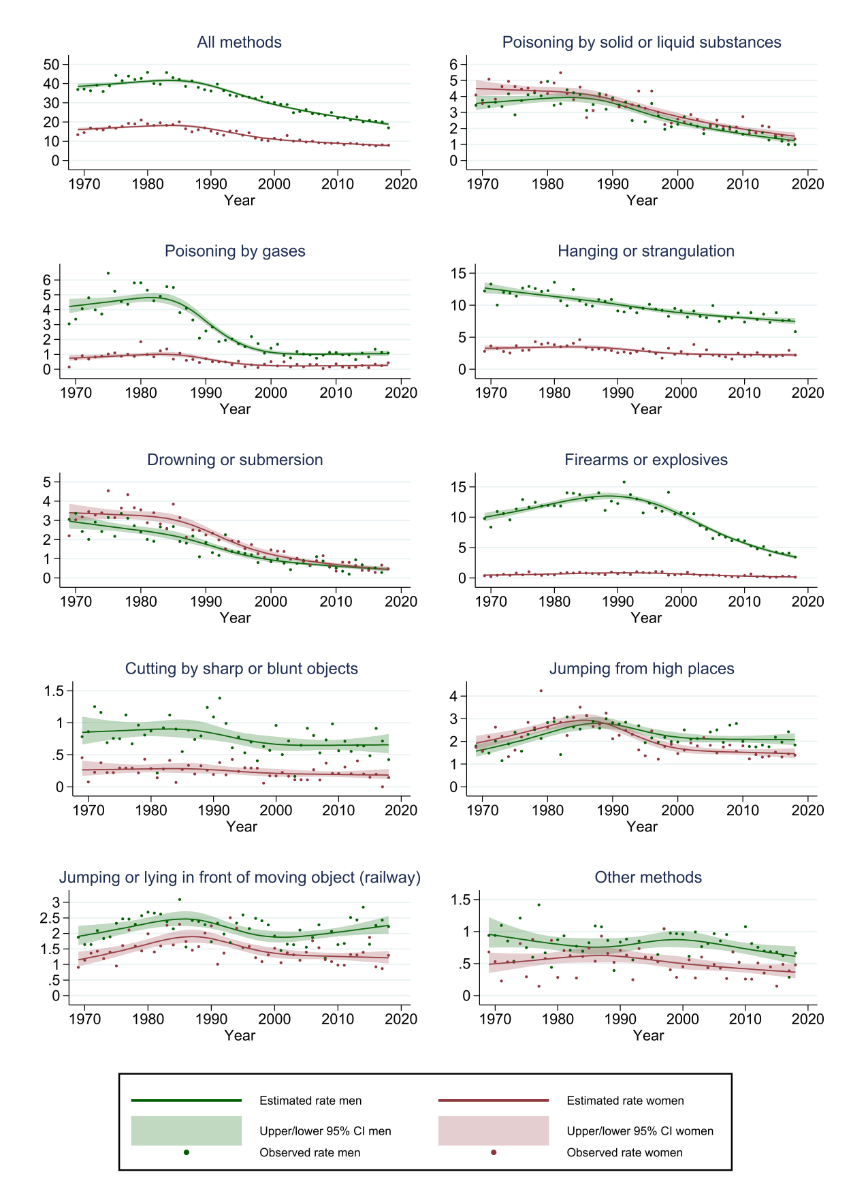
Figure 3 Rates of suicide methods per 100,000 population (person-years) in the age group 30–64 years. Note: estimated true rates and associated confidence intervals (CI) were derived from Poisson regressions using a restricted cubic-spline model.
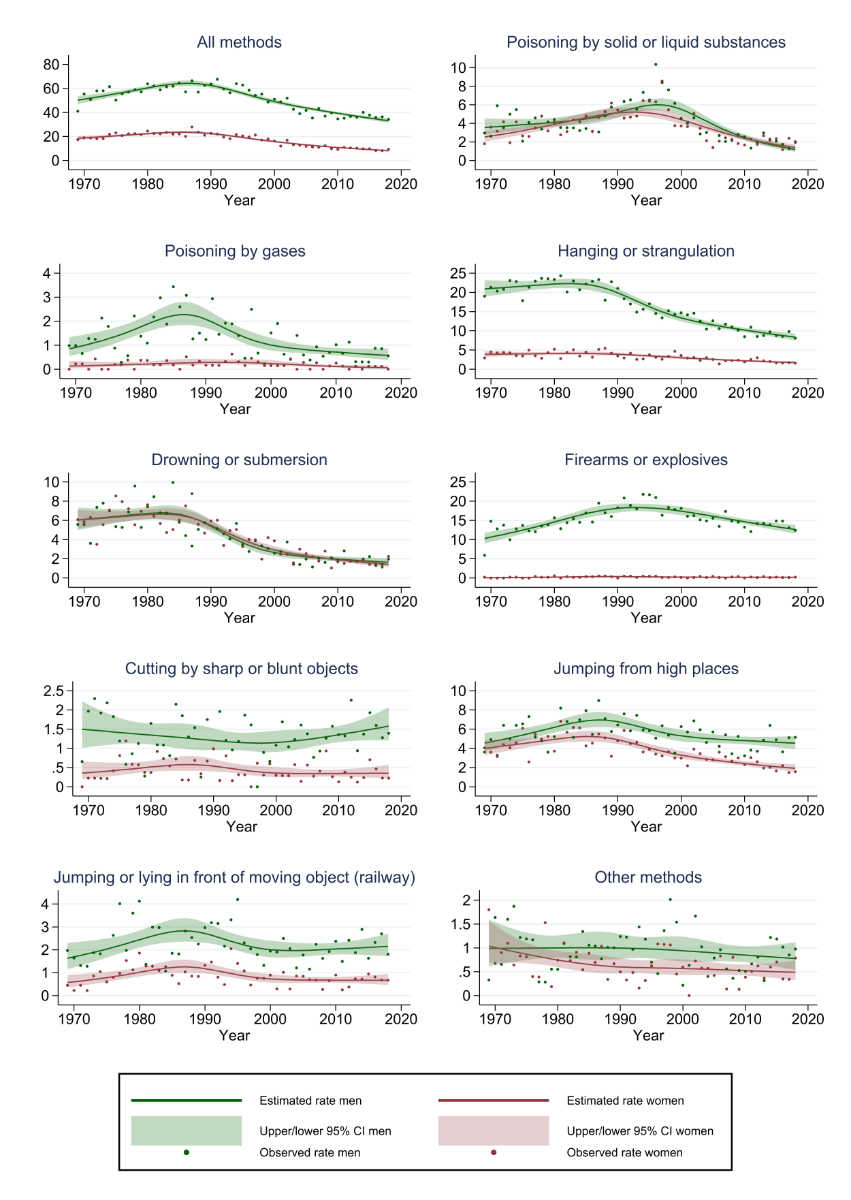
Figure 4 Rates of suicide methods per 100,000 population (person-years) in the age group 65 or more years. Note: estimated true rates and associated confidence intervals (CI) were derived from Poisson regressions using a restricted cubic-spline model.
Suicides by poisoning with gas were rare among women (figures 2-4). In men, suicides by gas peaked in the 1980s and then declined rapidly. Except for older (>64 years) male and female inhabitants, the rates of gas suicides were higher in Swiss citizens than in foreigners (tables 3 and 4).
Table 3Rate ratios of suicides in men.
| Period vs reference period 1969−1978 (95% CI) | Foreigners vs Swiss citizens (95% CI) | |||||||||
| Agegroup | Suicide method | Period 1979−1988 | Period 1989−1998 | Period 1999−2008 | Period 2009−2018 | Period 1969−1978 | Period 1979−1988 | Period 1989−1998 | Period 1999−2008 | Period 2009−2018 |
| 10−29 years | Poisoning | 0.958 (0.800−1.148) | 0.609 (0.492−0.753) | 0.286 (0.215−0.381) | 0.109 (0.071−0.167) | 0.650 (0.445−0.950) | 0.921 (0.656−1.293) | 0.515 (0.314−0.842) | 0.397 (0.181−0.869) | 1.545 (0.769−3.104) |
| Gas | 1.211 (1.003−1.463) | 0.500 (0.390−0.642) | 0.173 (0.118−0.255) | 0.263 (0.192−0.361) | 0.427 (0.321−0.570) | −1 | −1 | −1 | −1 | |
| Hanging | 1.324 (1.175−1.493) | 1.046 (0.920−1.189) | 0.681 (0.589−0.788) | 0.649 (0.561−0.751) | 0.836 (0.746−0.937) | −1 | −1 | −1 | −1 | |
| Drowning | 0.689 (0.493−0.961) | 0.439 (0.297−0.648) | 0.285 (0.179−0.452) | 0.115 (0.060−0.222) | 1.484 (1.084−2.032) | −1 | −1 | −1 | −1 | |
| Firearms | 1.369 (1.243−1.507) | 1.339 (1.213−1.479) | 0.827 (0.739−0.927) | 0.298 (0.254−0.349) | 0.153 (0.126−0.184) | −1 | −1 | −1 | −1 | |
| Cutting | 1.487 (0.876−2.525) | 1.063 (0.596−1.896) | 0.427 (0.197−0.924) | 0.534 (0.265−1.075) | 0.937 (0.562−1.563) | −1 | −1 | −1 | −1 | |
| Falls | 1.719 (1.382−2.138) | 1.729 (1.386−2.156) | 1.445 (1.148−1.820) | 1.125 (0.884−1.432) | 0.743 (0.618−0.893) | −1 | −1 | −1 | −1 | |
| Railway | 1.250 (1.009−1.549) | 1.334 (1.076−1.654) | 1.039 (0.826−1.308) | 1.585 (1.290−1.949) | 0.601 (0.496−0.729) | −1 | −1 | −1 | −1 | |
| Other | 0.941 (0.660−1.343) | 0.714 (0.483−1.055) | 0.788 (0.537−1.156) | 0.609 (0.406−0.915) | 0.799 (0.569−1.123) | −1 | −1 | −1 | −1 | |
| All methods | 1.271 (1.200−1.345) | 1.061 (0.999−1.128) | 0.685 (0.639−0.735) | 0.504 (0.467−0.544) | 0.516 (0.483−0.551) | −1 | −1 | −1 | −1 | |
| 30−64 years | Poisoning | 1.076 (0.953−1.215) | 0.843 (0.744−0.956) | 0.593 (0.519−0.677) | 0.410 (0.354−0.474) | 0.710 (0.637−0.792) | −1 | −1 | −1 | −1 |
| Gas | 1.101 (0.981−1.235) | 0.470 (0.408−0.541) | 0.243 (0.205−0.289) | 0.221 (0.185−0.264) | 0.305 (0.223−0.418) | 0.334 (0.254−0.440) | 0.358 (0.250−0.513) | 0.421 (0.272−0.650) | 0.715 (0.518−0.987) | |
| Hanging | 0.859 (0.797−0.925) | 0.749 (0.695−0.808) | 0.672 (0.623−0.724) | 0.622 (0.576−0.671) | 0.423 (0.359−0.499) | 0.698 (0.609−0.800) | 0.608 (0.530−0.698) | 0.685 (0.602−0.780) | 0.720 (0.641−0.809) | |
| Drowning | 0.814 (0.702−0.945) | 0.495 (0.420−0.585) | 0.306 (0.254−0.370) | 0.187 (0.150−0.233) | 0.600 (0.510−0.705) | −1 | −1 | −1 | −1 | |
| Firearms | 1.171 (1.093−1.254) | 1.188 (1.111−1.271) | 0.803 (0.747−0.862) | 0.469 (0.432−0.509) | 0.189 (0.172−0.209) | −1 | −1 | −1 | −1 | |
| Cutting | 0.868 (0.670−1.124) | 0.929 (0.726−1.189) | 0.739 (0.573−0.953) | 0.770 (0.601−0.986) | 0.544 (0.435−0.681) | −1 | −1 | −1 | −1 | |
| Falls | 1.393 (1.186−1.636) | 1.327 (1.133−1.555) | 1.221 (1.042−1.429) | 1.135 (0.969−1.330) | 0.543 (0.477−0.617) | −1 | −1 | −1 | −1 | |
| Railway | 1.188 (1.014−1.392) | 1.088 (0.929−1.273) | 0.887 (0.755−1.042) | 1.110 (0.954−1.292) | 0.520 (0.454−0.595) | −1 | −1 | −1 | −1 | |
| Other | 0.922 (0.715−1.189) | 0.833 (0.647−1.073) | 0.967 (0.761−1.228) | 0.786 (0.614−1.006) | 0.552 (0.444−0.686) | −1 | −1 | −1 | −1 | |
| All methods | 1.041 (1.001−1.082) | 0.894 (0.859−0.930) | 0.678 (0.651−0.707) | 0.549 (0.526−0.574) | 0.426 (0.389−0.467) | 0.465 (0.428−0.505) | 0.418 (0.385−0.453) | 0.475 (0.437−0.516) | 0.503 (0.464−0.544) | |
| >64 years | Poisoning | 0.941 (0.728−1.217) | 1.890 (1.516−2.356) | 0.888 (0.694−1.137) | 0.564 (0.435−0.731) | 2.900 (1.741−4.829) | 2.563 (1.543−4.259) | 1.410 (0.950−2.095) | 1.185 (0.742−1.892) | 1.128 (0.694−1.832) |
| Gas | 2.062 (1.389−3.061) | 1.486 (0.987−2.236) | 0.796 (0.508−1.248) | 0.631 (0.403−0.986) | 0.767 (0.462−1.274) | −1 | −1 | −1 | −1 | |
| Hanging | 1.036 (0.937−1.146) | 0.796 (0.717−0.883) | 0.601 (0.540−0.670) | 0.441 (0.395−0.493) | 0.635 (0.545−0.739) | −1 | −1 | −1 | −1 | |
| Drowning | 0.977 (0.811−1.177) | 0.689 (0.566−0.840) | 0.335 (0.266−0.423) | 0.297 (0.238−0.372) | 0.910 (0.695−1.193) | −1 | −1 | −1 | −1 | |
| Firearms | 1.274 (1.121−1.447) | 1.587 (1.407−1.789) | 1.354 (1.200−1.528) | 1.186 (1.054−1.335) | 0.368 (0.306−0.443) | −1 | −1 | −1 | −1 | |
| Cutting | 0.832 (0.553−1.252) | 0.855 (0.576−1.269) | 0.807 (0.549−1.187) | 1.039 (0.732−1.474) | 1.015 (0.681−1.511) | −1 | −1 | −1 | −1 | |
| Falls | 1.221 (1.006−1.483) | 1.142 (0.942−1.383) | 0.951 (0.784−1.153) | 0.852 (0.707−1.028) | 1.130 (0.932−1.370) | −1 | −1 | −1 | −1 | |
| Railway | 1.298 (0.943−1.786) | 1.422 (1.046−1.933) | 0.938 (0.679−1.297) | 1.152 (0.855−1.553) | 0.560 (0.374−0.839) | −1 | −1 | −1 | −1 | |
| Other | 0.895 (0.555−1.445) | 1.146 (0.737−1.782) | 0.790 (0.498−1.254) | 0.804 (0.520−1.244) | 1.085 (0.675−1.744) | −1 | −1 | −1 | −1 | |
| All methods | 1.114 (1.046−1.187) | 1.117 (1.050−1.188) | 0.830 (0.779−0.886) | 0.697 (0.654−0.743) | 0.908 (0.727−1.135) | 0.896 (0.738−1.088) | 0.720 (0.601−0.863) | 0.571 (0.480−0.678) | 0.644 (0.558−0.743) | |
Note: Incidence rate ratios were derived from Poisson regression models and adjusted for the interaction of period*nationality, if adding such interaction term statistically significantly improved the fit of the model as compared to the respective model without interaction term (log−likelihood ratio test).
1 Adding the interaction period*nationality did not statistically significantly improve the fit of the model when compared to a model without interaction term (log−likelihood ratio test).
Table 4Rate ratios of suicides in women.
| Period vs. reference period 1969−1978 (95% CI) | Foreigners vs. Swiss citizens (95% CI) | |||||||||
| Age group | Suicide method | Period 1979−1988 | Period 1989−1998 | Period 1999−2008 | Period 2009−2018 | Period 1969−1978 | Period 1979−1988 | Period 1989−1998 | Period 1999−2008 | Period 2009−2018 |
| 10−29 years | Poisoning | 1.109 (0.904−1.361) | 0.505 (0.387−0.659) | 0.527 (0.403−0.689) | 0.198 (0.134−0.291) | 1.085 (0.764−1.541) | 0.424 (0.251−0.717) | 0.764 (0.446−1.308) | 0.384 (0.193−0.766) | 0.931 (0.442−1.961) |
| Gas | 1.336 (0.795−2.247) | 0.794 (0.433−1.455) | 0.230 (0.088−0.601) | 0.352 (0.159−0.780) | 0.442 (0.213−0.914) | −1 | −1 | −1 | −1 | |
| Hanging | 1.728 (1.343−2.223) | 1.159 (0.878−1.531) | 1.058 (0.794−1.409) | 0.995 (0.746−1.327) | 0.826 (0.659−1.036) | −1 | −1 | −1 | −1 | |
| Drowning | 0.749 (0.510−1.101) | 0.357 (0.215−0.591) | 0.277 (0.158−0.488) | 0.106 (0.046−0.245) | 0.679 (0.419−1.100) | −1 | −1 | −1 | −1 | |
| Firearms | 1.372 (0.863−2.183) | 1.561 (0.986−2.473) | 1.072 (0.646−1.779) | 0.318 (0.151−0.668) | 0.479 (0.285−0.804) | −2 | −2 | −2 | −2 | |
| Cutting | 0.913 (0.371−2.246) | 0.548 (0.187−1.603) | 0.342 (0.094−1.242) | 0.761 (0.289−2.002) | 0.559 (0.196−1.591) | −1 | −1 | −1 | −1 | |
| Falls | 1.348 (1.045−1.739) | 0.888 (0.667−1.183) | 0.952 (0.717−1.265) | 0.495 (0.351−0.697) | 0.710 (0.547−0.920) | −1 | −1 | −1 | −1 | |
| Railway | 1.577 (1.168−2.129) | 1.369 (0.999−1.876) | 1.395 (1.016−1.914) | 1.490 (1.094−2.030) | 0.453 (0.333−0.615) | −1 | −1 | −1 | −1 | |
| Other | 1.165 (0.649−2.093) | 1.378 (0.779−2.438) | 0.577 (0.278−1.198) | 0.498 (0.234−1.060) | 1.004 (0.599−1.683) | −1 | −1 | −1 | −1 | |
| All methods | 1.308 (1.169−1.463) | 0.841 (0.739−0.957) | 0.782 (0.684−0.895) | 0.561 (0.484−0.650) | 0.853 (0.684−1.064) | 0.544 (0.426−0.696) | 0.773 (0.610−0.979) | 0.569 (0.434−0.747) | 0.592 (0.438−0.801) | |
| 30−64 years | Poisoning | 0.944 (0.843−1.057) | 0.806 (0.719−0.904) | 0.544 (0.480−0.616) | 0.433 (0.380−0.493) | 0.606 (0.536−0.686) | −1 | −1 | −1 | −1 |
| Gas | 1.232 (0.962−1.578) | 0.500 (0.369−0.679) | 0.369 (0.266−0.513) | 0.305 (0.216−0.431) | 0.392 (0.270−0.569) | −1 | −1 | −1 | −1 | |
| Hanging | 1.106 (0.975−1.254) | 0.828 (0.725−0.944) | 0.756 (0.662−0.862) | 0.729 (0.639−0.832) | 0.553 (0.485−0.632) | −1 | −1 | −1 | −1 | |
| Drowning | 0.886 (0.778−1.010) | 0.556 (0.481−0.642) | 0.329 (0.279−0.389) | 0.171 (0.139−0.211) | 0.501 (0.419−0.598) | −1 | −1 | −1 | −1 | |
| Firearms | 1.321 (0.981−1.777) | 1.571 (1.185−2.083) | 0.961 (0.707−1.305) | 0.542 (0.381−0.770) | 0.284 (0.191−0.422) | −1 | −1 | −1 | −1 | |
| Cutting | 1.025 (0.653−1.607) | 0.994 (0.638−1.548) | 0.700 (0.436−1.123) | 0.805 (0.513−1.264) | 0.443 (0.269−0.730) | −1 | −1 | −1 | −1 | |
| Falls | 1.431 (1.232−1.662) | 0.996 (0.851−1.166) | 0.865 (0.737−1.014) | 0.711 (0.603−0.838) | 0.683 (0.591−0.789) | −1 | −1 | −1 | −1 | |
| Railway | 1.266 (1.047−1.530) | 1.235 (1.025−1.488) | 1.033 (0.854−1.249) | 0.953 (0.786−1.155) | 0.378 (0.306−0.468) | −1 | −1 | −1 | −1 | |
| Other | 1.199 (0.878−1.637) | 1.173 (0.863−1.593) | 0.886 (0.644−1.220) | 0.783 (0.566−1.083) | 0.568 (0.418−0.773) | −1 | −1 | −1 | −1 | |
| All methods | 1.087 (1.028−1.150) | 0.842 (0.795−0.893) | 0.640 (0.602−0.680) | 0.529 (0.497−0.564) | 0.538 (0.505−0.573) | −1 | −1 | −1 | −1 | |
| >64 years | Poisoning | 1.198 (0.965−1.486) | 1.811 (1.488−2.204) | 0.944 (0.760−1.173) | 0.677 (0.540−0.850) | 1.909 (1.103−3.307) | 2.403 (1.560−3.700) | 1.939 (1.369−2.746) | 1.179 (0.718−1.936) | 0.578 (0.295−1.131) |
| Gas | 1.393 (0.577−3.361) | 1.795 (0.786−4.101) | 0.924 (0.371−2.297) | 0.565 (0.212−1.507) | 1.497 (0.597−3.751) | −2 | −2 | −2 | −2 | |
| Hanging | 1.124 (0.928−1.362) | 0.847 (0.695−1.034) | 0.721 (0.590−0.883) | 0.538 (0.436−0.663) | 0.591 (0.423−0.824) | −1 | −1 | −1 | −1 | |
| Drowning | 1.006 (0.864−1.172) | 0.672 (0.571−0.792) | 0.421 (0.351−0.505) | 0.251 (0.205−0.308) | 0.627 (0.465−0.844) | −1 | −1 | −1 | −1 | |
| Firearms | 2.568 (1.020−6.470) | 2.521 (1.012−6.278) | 1.580 (0.607−4.111) | 1.529 (0.598−3.910) | 1.107 (0.445−2.750) | −1 | −1 | −1 | −1 | |
| Cutting | 1.091 (0.624−1.907) | 0.928 (0.528−1.629) | 0.946 (0.548−1.634) | 0.641 (0.361−1.138) | 1.523 (0.840−2.762) | −1 | −1 | −1 | −1 | |
| Falls | 1.230 (1.029−1.469) | 0.940 (0.782−1.129) | 0.708 (0.584−0.857) | 0.500 (0.409−0.610) | 1.034 (0.812−1.318) | −1 | −1 | −1 | −1 | |
| Railway | 1.513 (1.000−2.290) | 1.449 (0.963−2.181) | 0.902 (0.581−1.399) | 0.941 (0.617−1.436) | 0.477 (0.236−0.964) | −1 | −1 | −1 | −1 | |
| Other | 0.798 (0.518−1.227) | 0.703 (0.457−1.082) | 0.562 (0.361−0.875) | 0.524 (0.341−0.807) | 1.542 (0.948−2.506) | −1 | −1 | −1 | −1 | |
| All methods | 1.136 (1.042−1.238) | 0.996 (0.914−1.085) | 0.672 (0.613−0.737) | 0.491 (0.446−0.541) | 1.074 (0.810−1.424) | 1.072 (0.832−1.380) | 1.213 (0.965−1.526) | 0.888 (0.682−1.155) | 0.630 (0.467−0.848) | |
Note: Incidence rate ratios were derived from Poisson regression models and adjusted for the interaction of period*nationality, if adding such interaction term statistically significantly improved the fit of the model as compared to the respective model without interaction term (log−likelihood ratio test).
1 Adding the interaction period*nationality did not statistically significantly improve the fit of the model when compared to a model without interaction term (log−likelihood ratio test).
2 Model with interaction period*nationality could not be estimated (non−convergence) due to very low suicide rates.
Hanging ranked second of all suicide methods in men (after firearms) and in women (after poisonings by solid or liquid substance) during the 50-year study period (table 2). Incidence rates typically declined since the 1980s, with flattening trends in more recent decades (figures 2–4). Between 2009-2018, hanging was the most common suicide method among men, except for older (>64 years) Swiss citizens who most often committed suicide by firearms (appendix, fig. S1). In women, hanging was also the most common suicide means up to 64 years, when jumping from heights became most frequent (appendix, fig. S2).
The incidence rate of suicides by drowning developed on a similar level in men and in women over the last 50 years (figures 2–4). Suicides by drowning were relatively common in earlier decades, particularly among older people, and declined in all age groups and in both sexes over recent decades. Interestingly, the rate of drownings was permanently higher in foreign than in Swiss young men (IRR 1.484, 95% CI 1.084–2.032) throughout the study period (table 3).
Rarely used by women, firearms accounted for most suicides among men between 1969–2018 (table 2). In young (10–29 years) and middle-aged (30–64 years) men, firearm suicides had the highest incidence rate of all methods until the early 2000s, when hanging became most frequent after a steep decline in firearms suicides (figures 2 and 3). In older Swiss men (>64 years), however, the rate of firearm suicides declined to a lesser extent and guns replaced hanging as the most common suicide method since the 1990s (fig. 4 and appendix fig. S1). The IRR for suicides by firearms between foreign and Swiss men was the lowest of all suicide methods in each of the age groups (table 3).
Suicide by cutting with sharp or blunt objects accounted for only 2.1% of all suicides (table 2) and was rarely used in all subpopulations (appendix, figures S1 and S2).
The rate of suicides by falls declined since the late 1980s in all population subgroups (figures 2–4 and appendix, figures S1 and S2). However, in women, jumping from high places was among the most common suicide methods, and middle-aged women had similar incidence rates as their male contemporaries.
Suicides by jumping or lying in front of moving objects (almost exclusively trains) followed an increasing trend in men (all age groups) and in young women (10–29 years) during the latest decade (figures 2–4). In consequence, railway suicides most recently became one of the most common suicide means in young people (fig. 2 and appendix, figures S1 and S2).
Other suicide methods such as intentional self-harm by crashing a motor vehicle or by unspecified means were rare throughout our study period (figures 2–4).
We examined trends in Swiss suicide rates between 1969 and 2018 with a particular focus on different methods of suicide used in various subgroups of the resident population. This meets with the WHO recommendation to "conduct a situation analysis (for instance, rates of suicide and self-harm, specific populations at risk, common methods of suicide, […]) to inform the planning of suicide prevention activities" [7]. Following this line of reasoning, our results may contribute to the Swiss national action plan on prevention of suicide, which was introduced in 2017 and which aims to reduce the rate of suicides by about 25% by 2030 as compared with 2013 [31].
Hepp et al. [8] had previously demonstrated that the overall suicide rate in Switzerland peaked in the 1980s and then declined up to 2005 in both sexes. We found that these declining trends also occurred in different age groups and in Swiss as well as in foreign citizens. Furthermore, the declining trends in Swiss suicide rates went on up to 2018, even though they tended to attenuate in most recent years.
The decline in the overall Swiss suicide rate corresponds with declining trends in Europe and globally [32]. When compared with the European Union (EU), the decline in Switzerland was even more pronounced: after having been much higher in 1980 (24.9 vs 14.0 suicides per 100,000 population), most recently (2017), the age-standardised overall suicide rate in Switzerland (10.4) approached the EU rate (9.0) [33]. This sharp decline in Switzerland had occurred despite the lack of a national suicide prevention strategy until 2017 [31]. However, public and private stakeholders had implemented a range of prevention measures already earlier. The stable economic situation and improvements in mental health care are further possible explanations for declining suicide rates in Switzerland [31].
Interestingly, even the 2007 financial crisis did not halt the declining trend of suicides in Switzerland, although the Swiss economy was hit hard by the crisis. This contrasts with increasing suicide rates in other European countries which were more severely struck by the crisis (e.g., Greece, the Netherlands or UK) [34]. Unemployment was shown to be associated with increased suicide rates across nations [35]. The relatively low unemployment rate in Switzerland despite the financial crisis and the aforementioned overall political and socioeconomic stability as well as a well-functioning healthcare system might help to explain the declining trend in Swiss suicide rates.
Up to 90% of people who commit suicide suffer from a mental disorder, most often affective disorders [36]. Adequate mental health care is therefore crucial to prevent suicides. Access to psychiatric and psychotherapeutic care was facilitated in Switzerland with the 1996 introduction of mandatory health insurance for all residents. Together with efforts to destigmatise mental disorders, this resulted in a steadily increasing proportion of the Swiss population who used psychiatric services [37]. Further measures to improve mental health care in Switzerland (and elsewhere) involved education of non-psychiatric health professionals (e.g., primary care physicians) for better recognition and treatment of depression [38–41], greater awareness of the high suicide risk after discharge from psychiatric hospitals [3, 42, 43], and increased prescription of antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), which are easier to handle by general practitioners than other antidepressants [44–48]. These improvements in mental health care most probably contributed to declining suicide rates in Switzerland.
However, in other countries such as the USA, the suicide rate did not decline and was even increasing since the millennium [49], despite preventive developments such as increased prescription of antidepressants [50]. Although most suicide decedents suffer from mental disorders [36], most people with mental disorders do not commit suicide [51]. This suggests the importance of factors other than mental health which may place people at risk for suicide [2, 5]. Among these precipitating factors are stressful life events such as interpersonal conflicts [1, 52] or the availability of lethal means [3, 53], which seem to be particularly important for impulsive suicidal acts. The in-depth study of the use of different suicide methods in different population subgroups may help to better understand risk factors for suicide and inform targeted preventive measures.
As the overall suicide rate, suicides by specific methods typically declined since the 1980s in both sexes, in all age groups, and in Swiss as well as in foreign citizens. Also consistent with suicides in general, the specific suicide methods were typically more often used by men, by older people and by Swiss citizens. However, the use of some specific suicide means diverged from this general pattern, at least in some subpopulations. Together with the most frequently used methods in recent years, this requires particular attention with respect to targeted suicide prevention measures.
Suicides by poisoning with solid or liquid substances had declined in Switzerland over most recent decades. This corresponds with more cautious dispersion of potentially lethal drugs such as reduction of paracetamol package sizes to non-lethal doses [54, 55] or replacement of tricyclic antidepressants with less toxic SSRIs [8]. The decline in suicides by poisoning occurred with some delay and not until the late 1990s in older people (>64 years). However, this could be due to erroneous reporting of assisted suicides, which were not documented with an extra ICD-10 code until 1998. Assisted suicides most likely occur in older and physically ill people [56], and they were particularly prone to be miss-classified as "conventional" suicides by poisoning in the 1990s, when this phenomenon was new in Switzerland. Yet another explanation for the delayed decline among the elderly could be the higher availability of potentially lethal drugs in their households. Due to relatively high incidence rates, prevention of suicides by poisoning with solid or liquid substances deserves particular attention in women and in foreigners, especially when taking into account the steadily increasing proportion of migrants in Switzerland [57].
Suicides by poisoning with gas had already declined in Switzerland in the 1950s and 1960s when the domestic gas was detoxified [58]. During the 50 years studied here (1969–2018), suicides by gas were rare in women. In men, gasification remained a relatively common suicide means until the mid-1980s, when new legislation prescribed catalytic converters for new motor vehicles. As a result, the exhaust of new cars was no longer available as a lethal means [8] and gas suicides began to decline rapidly in all male age groups and across nationalities. The association between the introduction of catalytic converters and declining rates of gas suicides was observed in various countries, with no or only moderate shifts to suicides by other means [18, 59–61]. In Switzerland, some method substitution might have occurred among older men (>64 years), among whom suicides by poisonings with solid or liquid substances and firearm suicides had increased in the late 1980s and early 1990s. However, the overall suicide rate had decreased even in this age group. Our findings therefore underpin the potential of restricting access to lethal means as an evidence-based strategy for suicide prevention [19, 53], even though emission laws were introduced for environmental and not for suicide prevention purposes. Suicides by charcoal burning had most recently attained increasing popularity in some Asian countries [53] after extensive media reporting of a few cases [62]. So far, our data suggest no increase of poisonings with gases in Switzerland.
Hanging accounted for most suicides in Switzerland between 1969–2018. Incidence rates had typically declined since the 1980s but trends then tended to level out more recently. In consequence, hanging had become the most common suicide means in younger and middle-aged people (<64 years). Maybe, other methods to which access was restricted (e.g., firearms or toxic substances) had been partially substituted with hanging, which is an easily available and highly lethal method [63]. Restricting access to ties and ligature points is difficult, especially in public places [64]. Some preventive evidence is available for infrastructural measures (e.g., "anti-suicide" shower heads) in controlled environments such as psychiatric hospitals or prisons [63, 65].
Drowning used to be a common suicide method with similar incidence rates in men and women, but rates declined in all subpopulations over more recent decades. This might be explained by efforts to teach swimming at Swiss schools since the 1960s, when public and private swimming pools became popular in Switzerland [8]. Although swimming lessons were intended to prevent accidental drowning, they apparently also had an impact on suicides. The delayed decline among older people and consistently higher rates in young foreign men (as compared with young Swiss men) might be due to the lower penetration of swimming lessons in older people and migrants.
Firearms are a highly lethal suicide method [66], which is often used in impulsive suicidal acts [67]. The availability of guns in households was shown to be associated with firearms suicides [68, 69], whereas restricting access to firearms seems to reduce firearm suicides, with only modest method substitution [3, 19]. If suicides by firearms ranked second (after hanging) in Switzerland over the last 50 years, this corresponds with the quite liberal firearms legislation and the high availability of firearms in Swiss households [68, 69]. Further underpinning the relevance of availability, firearm suicides were particularly common in Swiss men, who usually have easy access to firearms. In Switzerland, all male citizens are obliged to serve in the militia army. Army weapons are usually stored at home between army trainings and they often go to private ownership after termination of military services for a small fee [70, 71]. In 2003, the personnel of the Swiss army was approximately halved and since 2007 ammunition is no longer stored at home by the militia soldiers [71]. These reforms reduced the availability of firearms and provide an explanation for the decline in firearm suicides. This decline was particularly pronounced in younger Swiss men. A previous study showed that this decline in young men was indeed due to reduced suicides by military firearms, whereas suicides with other guns did not decrease [70]. Further findings from Switzerland suggest only modest method substitution following the army reform [71], even though some shift to railway suicides might have occurred in younger men. Among older Swiss men, the decline in firearm suicides was less pronounced and firearms had even become the most common suicide means in most recent decades. However, these older generations had served in the army before the reforms and they often still stored weapons and ammunition at home. Assuming that the choice of suicide means not only depends on their availability but also on their cultural and societal acceptance [72], reduced public acceptance of private firearms possession could provide yet another explanation for decreasing firearms suicides in Switzerland.
Suicides by cutting are hard to prevent by restricting access to widely available sharp or blunt objects. However, suicides by cutting are relatively rare in Switzerland (2.1% of all suicides) and we could not identify a subpopulation in which this method is of major relevance. Nevertheless, it should be kept in mind that cutting is a frequently used means for non-lethal self-injurious behaviour.
Suicides by falls had decreased less than other common methods of suicide (e.g., hanging or firearms in men or poisoning in women) over the last 50 years. Most recently, jumping from heights had even become one of the most common suicide means in women and in older foreign men. Previous findings suggested that leap suicides often occur among people with severe mental illness (e.g., psychosis) [8, 67] and among inpatients who lack access to other means while being at hospital [73]. Therefore, safeguarding jumping sites at hospitals seems to be an important prevention strategy [74], as is the safeguarding of so-called "hotspots" in general. Leap suicides tend to accumulate at hotspots such as iconic bridges, towers or other high-rise buildings [73]. This suggests the role of imitation effects in leap suicides, which may be additionally inspired by media reports [75]. Restricting access by erecting barriers (e.g., fences or safety nets) at hotspots and installing signage offering help at popular jumping sites were shown to reduce leap suicides, with little evidence for major method substitution in Switzerland [76–78] and elsewhere [19, 79]. However, moving to another nearby jumping location may still occur [80] and securing hotspots by barriers can be hindered by high costs or aesthetic objections. This might explain the modest decline in leap suicides in Switzerland. Yet another explanation could be that other methods with declining trends (e.g., firearm suicides) were partially substituted with leap suicides.
Railway suicides were increasing in the current millennium, particularly in younger and in male subpopulations. Among younger people, railway suicides had even become the most common means in recent years aside from hanging [81]. Maybe reduced suicides by other methods (e.g., firearms) were partially substituted with railway suicides. Switzerland has a dense railway network, making trains readily available as a highly lethal means of suicide [14]. Correspondingly, railway suicides are more common in Switzerland than in other countries [82]. In 2013, the Swiss Federal Railways company started an action plan to prevent suicides [82]. However, measures such as training of staff, surveillance of hotspots and more cautious communication of railway suicides probably need some more time to unfold their full preventive effects. As railway suicides are highly prone to imitation, media guidelines for responsible reporting are yet another preventive strategy to limit the awareness of this easily available and highly lethal suicide method [83–85]. While physically securing all railways is impossible, barriers at hotspots (e.g., fences at railways near psychiatric hospitals) represent other promising strategies for railway suicide prevention [82, 86, 87].
Suicides by other methods such as crashing a motor vehicle and suicides by other unspecified means were rare in Switzerland throughout the five decades. Thus, they are of minor relevance with regard to method-specific suicide prevention measures.
Our study has some limitations. First, we discussed and interpreted changes in suicide rates in relation to changes in potentially explaining factors (e.g., availability of firearms) but we did not quantitatively correlate changes in suicide rates with changes in risk or protective factors. Our explanations were discussed among experts from various disciplines, but they should be considered rather speculative, as the data and methods used in this study did not allow testing of the stated hypotheses. Second, there might be erroneous reporting of causes of death in the mortality statistics (e.g., misattribution of suicide to accidental deaths or, less likely, vice versa). However, it is unlikely that registration patterns had systematically changed during the study period. Effects of misreporting on time trends in suicide rates should therefore be tolerable. Last but not least, our analyses were restricted to completed suicides and did not take into account attempted suicides and suicidal ideation, which are much more prevalent than completed suicides [2, 6, 19], particularly in women [88].
Suicides in total and suicides by specific methods generally declined in Switzerland over the latest three decades across sexes, ages and nationalities. Some methods (e.g., drowning or poisoning by gases) had become relatively rare, whereas other methods also declined but go on accounting for many suicides in Switzerland every year, at least in some subgroups of the resident population (e.g., firearms in older Swiss men or railway suicides in young residents). In summary, our results both corroborate previous findings that suicides are preventable [3, 19, 88] but they also refer to the need for further and targeted preventive efforts, if a 25% reduction of the Swiss suicide rate is to be achieved by 2030 as intended by the national action plan [31].
The decline in specific suicide methods such as firearms, drownings or poisonings was associated with changes in the availability of these lethal means in Switzerland. Suicide attempters usually have a preferred method [16, 89] and they often act impulsively [52, 90, 91]. If immediate access to the preferred means is restricted, brief suicidal crises with strong ambivalence may pass by [3]. And even if people switch to other means, restricting access to highly lethal methods increase chances that a less lethal method is chosen [8]. In this line of reasoning, our data also suggest no major method substitution after access to specific means was restricted. Aside from method restriction, further explanations for decreasing suicide rates in Switzerland are the development of media guidelines for more responsible reporting of suicide events (e.g., avoidance of explicit descriptions and speculation about reasons) [31] and improvements in health care, including easier access to health services (following the introduction of mandatory health insurance), measures to improve early identification and management of mental disorders [41] and changes in drug prescription (more SSRIs, less toxic drugs) [8].
Further efforts to reduce suicides in Switzerland and elsewhere require coordination and collaboration among multiple sectors of the society (e.g., health, education, justice, law, politics, media sector) [2, 19, 88]. Suicidal behaviour is a complex issue with many factors beyond mental disorders being involved [7]. A public health approach to prevention should therefore include combinations of evidence-based universal (e.g., means restriction), selective (e.g., early detection of mental disorders) and indicated (e.g., follow-up care after attempted suicide) strategies on both an individual and a population level [6, 19]. Our analyses underpinned that different suicide methods are chosen by different people or subgroups of the population. Targeted prevention measures should take these findings into account and aim at differentiated prevention strategies for individuals or groups at high risk in order to further reduce suicides.
We thank Dr Vladeta Ajdacic-Gross, PhD, for providing us detailed information on how the methods of suicide were categorised based on ICD-8 and ICD-10 codes in the Swiss cause of death statistics for the preceding study of Hepp et al. (2010).
There was no funding for this study.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. World Health Organization. Suicide. Geneva: World Health Organization; 2022. Available from: https://www.who.int/news-room/fact-sheets/detail/suicide
2. Fazel S, Runeson B. Suicide. N Engl J Med. 2020 Jan;382(3):266–74. https://doi.org/10.1056/NEJMra1902944
3. Mann JJ, Michel CA, Auerbach RP. Improving Suicide Prevention Through Evidence-Based Strategies: A Systematic Review. Am J Psychiatry. 2021 Jul;178(7):611–24. https://doi.org/10.1176/appi.ajp.2020.20060864
4. Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. 2003 Oct;4(10):819–28. https://doi.org/10.1038/nrn1220
5. National Center for Injury Prevention and Control. Suicide prevention: A public health issue. Atlanta: Centers for Disease Control and Prevention; 2021; Available from: https://www.cdc.gov/violenceprevention/pdf/asap_suicide_issue2-a.pdf
6. World Health Organization. Preventing suicide: A global imperative. Geneva: World Health Organization; 2014.
7. World Health Organization. Comprehensive mental health action plan 2013-2030. Geneva: World Health Organization; 2021.
8. Hepp U, Ring M, Frei A, Rössler W, Schnyder U, Ajdacic-Gross V. Suicide trends diverge by method: swiss suicide rates 1969-2005. Eur Psychiatry. 2010 Apr;25(3):129–35. https://doi.org/10.1016/j.eurpsy.2009.05.005
9. Federal Statistical Office. Specific causes of death. Neuchatel: Federal Statistical Office; 2021. Available from: https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitszustand/sterblichkeit-todesursachen/spezifische.html
10. Federal Statistical Office. Transport accidents. Neuchatel: Federal Statistical Office; 2021. Available from: https://www.bfs.admin.ch/bfs/en/home/statistics/mobility-transport/accidents-environmental-impact/transport-accidents.html
11. Ajdacic-Gross V, Weiss MG, Ring M, Hepp U, Bopp M, Gutzwiller F, et al. Methods of suicide: international suicide patterns derived from the WHO mortality database. Bull World Health Organ. 2008 Sep;86(9):726–32. https://doi.org/10.2471/BLT.07.043489
12. Värnik A, Kõlves K, Allik J, Arensman E, Aromaa E, van Audenhove C, et al. Gender issues in suicide rates, trends and methods among youths aged 15-24 in 15 European countries. J Affect Disord. 2009 Mar;113(3):216–26. https://doi.org/10.1016/j.jad.2008.06.004
13. Värnik A, Kõlves K, van der Feltz-Cornelis CM, Marusic A, Oskarsson H, Palmer A, et al. Suicide methods in Europe: a gender-specific analysis of countries participating in the “European Alliance Against Depression”. J Epidemiol Community Health. 2008 Jun;62(6):545–51. https://doi.org/10.1136/jech.2007.065391
14. Hepp U, Stulz N, Unger-Köppel J, Ajdacic-Gross V. Methods of suicide used by children and adolescents. Eur Child Adolesc Psychiatry. 2012 Feb;21(2):67–73. https://doi.org/10.1007/s00787-011-0232-y
15. Dahlberg LL, Ikeda RM, Kresnow MJ. Guns in the home and risk of a violent death in the home: findings from a national study. Am J Epidemiol. 2004 Nov;160(10):929–36. https://doi.org/10.1093/aje/kwh309
16. Daigle MS. Suicide prevention through means restriction: assessing the risk of substitution. A critical review and synthesis. Accid Anal Prev. 2005 Jul;37(4):625–32. https://doi.org/10.1016/j.aap.2005.03.004
17. Gunnell D, Middleton N, Frankel S. Method availability and the prevention of suicide—a re-analysis of secular trends in England and Wales 1950-1975. Soc Psychiatry Psychiatr Epidemiol. 2000 Oct;35(10):437–43. https://doi.org/10.1007/s001270050261
18. McClure GM. Changes in suicide in England and Wales, 1960-1997. Br J Psychiatry. 2000 Jan;176(1):64–7. https://doi.org/10.1192/bjp.176.1.64
19. Zalsman G, Hawton K, Wasserman D, van Heeringen K, Arensman E, Sarchiapone M, et al. Suicide prevention strategies revisited: 10-year systematic review. Lancet Psychiatry. 2016 Jul;3(7):646–59. https://doi.org/10.1016/S2215-0366(16)30030-X
20. Federal Statistical Office. Cause of death and stillbirth statistics (CoD). Neuchatel: Federal Statistical Office; 2016. Available from: https://www.bfs.admin.ch/bfs/en/home/statistics/health/surveys/ecod.assetdetail.7037.html
21. World Health Organization. International statistical classification of diseases and related health problems. Tenth revision. Geneva: World Health Organization; 2004.
22. World Health Organization. International statistical classification of diseases and related health problems. Eighth revision. Geneva: World Health Organization; 1965.
23. Federal Statistical Office. Demographic balance by age. Neuchatel: Federal Statistical Office; 2021; Available from: https://www.pxweb.bfs.admin.ch/pxweb/en/px-x-0102020000_103/-/px-x-0102020000_103.px/
24. Kirkwood BR, Sterne AC. Essential medical statistics. Malden, MA: Blackwell; 2005. Chapter 24: Poisson regression; p. 249-262.
25. StataCorp. Stata Statistical Software: Release 16. College Station (TX): StataCorp LLC; 2019.
26. StataCorp. mkspline – linear and restricted cubic spline construction. In: StataCorp, editor. Stata 17 Base Reference Manual. College Station, TX: Stata Pres; 2019. p. 1551-7.
27. Harrell FE. Regression Modeling Strategies. Cham: Springer; 2015. https://doi.org/10.1007/978-3-319-19425-7
28. Croxford R. Restricted cubic spline regression: a brief introduction. Paper 5621-2016. Cary (NC): SAS Institute Inc; 2016.
29. Stone CJ, Koo CY. Additive splines in statistics. In: American Statistical Association, editor. Proceedings of the Statistical Computing Section. Washington, DC: American Statistical Association; 1985. p. 45-8.
30. Stone CJ. Generalized additive models. Stat Sci. 1986;1(3):312–4. https://doi.org/10.1214/ss/1177013607
31. Federal Office of Public Health. Suicide prevention in Switzerland. Bern: Swiss Confederation; 2018.
32. World Health Organization. Suicide in the world. Global health estimates. Geneva: World Health Organization; 2019.
33. World Health Organization. Suicide and intentional self-harm, per 100 000 population. Copenhagen: World Health Organization; 2022. Available from: https://gateway.euro.who.int/en/indicators/hfamdb_771-sdr-suicide-and-intentional-self-harm-per-100-000/
34. Alicandro G, Malvezzi M, Gallus S, La Vecchia C, Negri E, Bertuccio P. Worldwide trends in suicide mortality from 1990 to 2015 with a focus on the global recession time frame. Int J Public Health. 2019 Jun;64(5):785–95. https://doi.org/10.1007/s00038-019-01219-y
35. Nordt C, Warnke I, Seifritz E, Kawohl W. Modelling suicide and unemployment: a longitudinal analysis covering 63 countries, 2000-11. Lancet Psychiatry. 2015 Mar;2(3):239–45. https://doi.org/10.1016/S2215-0366(14)00118-7
36. Arsenault-Lapierre G, Kim C, Turecki G. Psychiatric diagnoses in 3275 suicides: a meta-analysis. BMC Psychiatry. 2004 Nov;4(1):37. https://doi.org/10.1186/1471-244X-4-37
37. Schuler D, Tuch A, Peter C. Psychische Gesundheit in der Schweiz. Monitoring 2020. (Obsan Bericht 15/2020). Neuchâtel: Schweizerisches Gesundheitsobservatorium; 2020.
38. Rutz W. Preventing suicide and premature death by education and treatment. J Affect Disord. 2001 Jan;62(1-2):123–9. https://doi.org/10.1016/S0165-0327(00)00356-6
39. Szanto K, Kalmar S, Hendin H, Rihmer Z, Mann JJ. A suicide prevention program in a region with a very high suicide rate. Arch Gen Psychiatry. 2007 Aug;64(8):914–20. https://doi.org/10.1001/archpsyc.64.8.914
40. Hegerl U, Maxwell M, Harris F, Koburger N, Mergl R, Székely A, et al.; OSPI-Europe Consortium. Prevention of suicidal behaviour: results of a controlled community-based intervention study in four European countries. PLoS One. 2019 Nov;14(11):e0224602. https://doi.org/10.1371/journal.pone.0224602
41. Michel K, Valach L. Suicide prevention: spreading the gospel to general practitioners. Br J Psychiatry. 1992 Jun;160(6):757–60. https://doi.org/10.1192/bjp.160.6.757
42. Chung D, Hadzi-Pavlovic D, Wang M, Swaraj S, Olfson M, Large M. Meta-analysis of suicide rates in the first week and the first month after psychiatric hospitalisation. BMJ Open. 2019 Mar;9(3):e023883. https://doi.org/10.1136/bmjopen-2018-023883
43. Chung DT, Ryan CJ, Hadzi-Pavlovic D, Singh SP, Stanton C, Large MM. Suicide Rates After Discharge From Psychiatric Facilities: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2017 Jul;74(7):694–702. https://doi.org/10.1001/jamapsychiatry.2017.1044
44. Gibbons RD, Brown CH, Hur K, Marcus SM, Bhaumik DK, Mann JJ. Relationship between antidepressants and suicide attempts: an analysis of the Veterans Health Administration data sets. Am J Psychiatry. 2007 Jul;164(7):1044–9. https://doi.org/10.1176/ajp.2007.164.7.1044
45. Simon GE, Savarino J, Operskalski B, Wang PS. Suicide risk during antidepressant treatment. Am J Psychiatry. 2006 Jan;163(1):41–7. https://doi.org/10.1176/appi.ajp.163.1.41
46. Ludwig J, Marcotte DE. Anti-depressants, suicide, and drug regulation. J Policy Anal Manage. 2005 Mar;24(2):249–72. https://doi.org/10.1002/pam.20089
47. Ludwig J, Marcotte DE, Norberg K. Anti-depressants and suicide. J Health Econ. 2009 May;28(3):659–76. https://doi.org/10.1016/j.jhealeco.2009.02.002
48. Rihmer Z. Can better recognition and treatment of depression reduce suicide rates? A brief review. Eur Psychiatry. 2001 Nov;16(7):406–9. https://doi.org/10.1016/S0924-9338(01)00598-3
49. Pettrone K, Curtin SC. Urban-rural differences in suicide rates, by sex and three leading methods: united States, 2000-2018. NCHS Data Brief. 2020 Aug;(373):1–8.
50. Pratt LA, Brody DJ, Gu Q. Antidepressant Use Among Persons Aged 12 and Over:United States,2011-2014. NCHS Data Brief. 2017 Aug;(283):1–8.
51. Ajdacic-Gross V, Hepp U, Seifritz E, Bopp M. Rethinking suicides as mental accidents: towards a new paradigm. J Affect Disord. 2019 Jun;252:141–51. https://doi.org/10.1016/j.jad.2019.04.022
52. Stulz N, Hepp U, Gosoniu DG, Grize L, Muheim F, Weiss MG, et al. Patient-identified priorities leading to attempted suicide. Crisis. 2018 Jan;39(1):37–46. https://doi.org/10.1027/0227-5910/a000473
53. Yip PS, Caine E, Yousuf S, Chang SS, Wu KC, Chen YY. Means restriction for suicide prevention. Lancet. 2012 Jun;379(9834):2393–9. https://doi.org/10.1016/S0140-6736(12)60521-2
54. Turvill JL, Burroughs AK, Moore KP. Change in occurrence of paracetamol overdose in UK after introduction of blister packs. Lancet. 2000;355(9220):2048–9. https://doi.org/10.1016/S0140-6736(00)02355-2
55. Hawton K, Bergen H, Simkin S, Dodd S, Pocock P, Bernal W, et al. Long term effect of reduced pack sizes of paracetamol on poisoning deaths and liver transplant activity in England and Wales: interrupted time series analyses. BMJ. 2013 Feb;346 feb07 1:f403. https://doi.org/10.1136/bmj.f403
56. Steck N, Egger M, Zwahlen M; Swiss National Cohort. Assisted and unassisted suicide in men and women: longitudinal study of the Swiss population. Br J Psychiatry. 2016 May;208(5):484–90. https://doi.org/10.1192/bjp.bp.114.160416
57. Federal Statistical Office. Anteil der ständigen ausländischen Wohnbevölkerung. Neuchatel: Federal Statistical Office; 2021. Available from: https://www.bfs.admin.ch/bfs/en/home/statistics/population/migration-integration/foreign.assetdetail.18264545.html
58. Lester D. The effect of the detoxification of domestic gas in Switzerland on the suicide rate. Acta Psychiatr Scand. 1990 Nov;82(5):383–4. https://doi.org/10.1111/j.1600-0447.1990.tb01406.x
59. Amos T, Appleby L, Kiernan K. Changes in rates of suicide by car exhaust asphyxiation in England and Wales. Psychol Med. 2001 Jul;31(5):935–9. https://doi.org/10.1017/S0033291701003920
60. Nordentoft M, Qin P, Helweg-Larsen K, Juel K. Restrictions in means for suicide: an effective tool in preventing suicide: the Danish experience. Suicide Life Threat Behav. 2007 Dec;37(6):688–97. https://doi.org/10.1521/suli.2007.37.6.688
61. Studdert DM, Gurrin LC, Jatkar U, Pirkis J. Relationship between vehicle emissions laws and incidence of suicide by motor vehicle exhaust gas in Australia, 2001-06: an ecological analysis. PLoS Med. 2010 Jan;7(1):e1000210. https://doi.org/10.1371/journal.pmed.1000210
62. Thomas K, Chang SS, Gunnell D. Suicide epidemics: the impact of newly emerging methods on overall suicide rates - a time trends study. BMC Public Health. 2011 May;11(1):314. https://doi.org/10.1186/1471-2458-11-314
63. Gunnell D, Bennewith O, Hawton K, Simkin S, Kapur N. The epidemiology and prevention of suicide by hanging: a systematic review. Int J Epidemiol. 2005 Apr;34(2):433–42. https://doi.org/10.1093/ije/dyh398
64. Large M, Nielssen O. The need to prevent suicide by hanging in Australia. Aust N Z J Psychiatry. 2021 May;55(5):519–20. https://doi.org/10.1177/0004867420951249
65. Kapur N, Hunt IM, Windfuhr K, Rodway C, Webb R, Rahman MS, et al. Psychiatric in-patient care and suicide in England, 1997 to 2008: a longitudinal study. Psychol Med. 2013 Jan;43(1):61–71. https://doi.org/10.1017/S0033291712000864
66. Shenassa ED, Catlin SN, Buka SL. Lethality of firearms relative to other suicide methods: a population based study. J Epidemiol Community Health. 2003 Feb;57(2):120–4. https://doi.org/10.1136/jech.57.2.120
67. de Moore GM, Robertson AR. Suicide attempts by firearms and by leaping from heights: a comparative study of survivors. Am J Psychiatry. 1999 Sep;156(9):1425–31. https://doi.org/10.1176/ajp.156.9.1425
68. Ajdacic-Gross V, Killias M, Hepp U, Gadola E, Bopp M, Lauber C, et al. Changing times: a longitudinal analysis of international firearm suicide data. Am J Public Health. 2006 Oct;96(10):1752–5. https://doi.org/10.2105/AJPH.2005.075812
69. Ajdacic-Gross V, Killias M, Hepp U, Haymoz S, Bopp M, Gutzwiller F, et al. Firearm suicides and availability of firearms: the Swiss experience. Eur Psychiatry. 2010 Nov;25(7):432–4. https://doi.org/10.1016/j.eurpsy.2010.04.006
70. Thoeni N, Reisch T, Hemmer A, Bartsch C. Suicide by firearm in Switzerland: who uses the army weapon? Results from the national survey between 2000 and 2010. Swiss Med Wkly. 2018 Sep;148:w14646. https://doi.org/10.4414/smw.2018.14646
71. Reisch T, Steffen T, Habenstein A, Tschacher W. Change in suicide rates in Switzerland before and after firearm restriction resulting from the 2003 “Army XXI” reform. Am J Psychiatry. 2013 Sep;170(9):977–84. https://doi.org/10.1176/appi.ajp.2013.12091256
72. Farmer R, Rohde J. Effect of availability and acceptability of lethal instruments on suicide mortality. An analysis of some international data. Acta Psychiatr Scand. 1980 Nov;62(5):436–46. https://doi.org/10.1111/j.1600-0447.1980.tb00632.x
73. Gunnell D, Nowers M. Suicide by jumping. Acta Psychiatr Scand. 1997 Jul;96(1):1–6. https://doi.org/10.1111/j.1600-0447.1997.tb09897.x
74. Mohl A, Stulz N, Martin A, Eigenmann F, Hepp U, Hüsler J, et al. The “Suicide Guard Rail”: a minimal structural intervention in hospitals reduces suicide jumps. BMC Res Notes. 2012 Aug;5(1):408. https://doi.org/10.1186/1756-0500-5-408
75. Beautrais A. Suicide by Jumping. Crisis. 2007 Jan;28(S1 Suppl 1):58–63. https://doi.org/10.1027/0227-5910.28.S1.58
76. Reisch T, Michel K. Securing a suicide hot spot: effects of a safety net at the Bern Muenster Terrace. Suicide Life Threat Behav. 2005 Aug;35(4):460–7. https://doi.org/10.1521/suli.2005.35.4.460
77. Reisch T, Schuster U, Michel K. Suicide by jumping and accessibility of bridges: results from a national survey in Switzerland. Suicide Life Threat Behav. 2007 Dec;37(6):681–7. https://doi.org/10.1521/suli.2007.37.6.681
78. Hemmer A, Meier P, Reisch T. Comparing Different Suicide Prevention Measures at Bridges and Buildings: Lessons We Have Learned from a National Survey in Switzerland. PLoS One. 2017 Jan;12(1):e0169625. https://doi.org/10.1371/journal.pone.0169625
79. Pirkis J, Spittal MJ, Cox G, Robinson J, Cheung YT, Studdert D. The effectiveness of structural interventions at suicide hotspots: a meta-analysis. Int J Epidemiol. 2013 Apr;42(2):541–8. https://doi.org/10.1093/ije/dyt021
80. Sinyor M, Levitt AJ. Effect of a barrier at Bloor Street Viaduct on suicide rates in Toronto: natural experiment. BMJ. 2010 Jul;341 jul06 1:c2884. https://doi.org/10.1136/bmj.c2884
81. Steck N, Egger M, Schimmelmann BG, Kupferschmid S; Swiss National Cohort. Suicide in adolescents: findings from the Swiss National cohort. Eur Child Adolesc Psychiatry. 2018 Jan;27(1):47–56. https://doi.org/10.1007/s00787-017-1019-6
82. Wyss Schneider T, Teotino G, Hepp U. Schienensuizide auf dem Netz der SBB. Dossier zu Präventionsmassnahmen, Handlungsbedarf und Empfehlungen. 2018. Available from https://news.sbb.ch/_file/10354/schienensuizide-auf-dem-netz-der-sbb.pdf
83. Niederkrotenthaler T, Sonneck G. Assessing the impact of media guidelines for reporting on suicides in Austria: interrupted time series analysis. Aust N Z J Psychiatry. 2007 May;41(5):419–28. https://doi.org/10.1080/00048670701266680
84. Barker E, Kolves K, De Leo D. Rail-suicide prevention: systematic literature review of evidence-based activities. Asia-Pac Psychiatry. 2017 Sep;9(3):e12246. https://doi.org/10.1111/appy.12246
85. Sinyor M, Schaffer A, Nishikawa Y, Redelmeier DA, Niederkrotenthaler T, Sareen J, et al. The association between suicide deaths and putatively harmful and protective factors in media reports. CMAJ. 2018 Jul;190(30):E900–7. https://doi.org/10.1503/cmaj.170698
86. Cox GR, Owens C, Robinson J, Nicholas A, Lockley A, Williamson M, et al. Interventions to reduce suicides at suicide hotspots: a systematic review. BMC Public Health. 2013 Mar;13(1):214. https://doi.org/10.1186/1471-2458-13-214
87. Law CK, Yip PS, Chan WS, Fu KW, Wong PW, Law YW. Evaluating the effectiveness of barrier installation for preventing railway suicides in Hong Kong. J Affect Disord. 2009 Apr;114(1-3):254–62. https://doi.org/10.1016/j.jad.2008.07.021
88. Turecki G, Brent DA. Suicide and suicidal behaviour. Lancet. 2016 Mar;387(10024):1227–39. https://doi.org/10.1016/S0140-6736(15)00234-2
89. Runeson B, Tidemalm D, Dahlin M, Lichtenstein P, Långström N. Method of attempted suicide as predictor of subsequent successful suicide: national long term cohort study. BMJ. 2010 Jul;341 jul13 1:c3222. https://doi.org/10.1136/bmj.c3222
90. Miller M, Hemenway D. Guns and suicide in the United States. N Engl J Med. 2008 Sep;359(10):989–91. https://doi.org/10.1056/NEJMp0805923
91. Simon OR, Swann AC, Powell KE, Potter LB, Kresnow MJ, O’Carroll PW. Characteristics of impulsive suicide attempts and attempters. Suicide Life Threat Behav. 2001;32(1 Suppl):49–59.
The appendix is available in the pdf version of the article.