DOI: https://doi.org/10.4414/smw.2012.13726
Colonoscopies are informative diagnostic procedures, especially for the detection of colorectal cancer and several other gastrointestinal diseases [1]. Because clinical symptoms are often signs of cancer that is already advanced, the threshold used to screen asymptomatic people should be kept low [2]. However, negotiating the endoscope along the colon can be an uncomfortable, painful and very unpleasant experience for some patients [3]. Performing a colonoscopy is thus a complex procedure, the success of which depends just as much on the patient’s cooperation as on the sensitivity and judgment of the endoscopy team regarding the patient’s level of pain and discomfort [4, 5]. When analgesic and sedative drugs are given, the patient’s levels of consciousness and reaction are altered. Under these conditions, constant supervision and, if judged necessary, supplemental drug administration are required to ensure that the procedure is being well tolerated [6]. For colonoscopy and other endoscopic procedures, sedation protocols that are essentially based on the continuous clinical assessment of the patient by the endoscopy team have become a widely accepted standard [7–10]. However, even if the endoscopy team pays great attention to the patient, the patient’s perception of the procedure is often different from that of the medical and nursing staff [11]. Little is known regarding the accuracy of the correlation between the patient’s own assessment of his or her level of comfort/discomfort during a colonoscopy and the assessments provided by medical staff.
We prospectively evaluated how well the assessments of discomfort made by endoscopists and endoscopy nurses correlated with the patients’ own evaluations of their procedures.
In this prospective cohort study, we investigated consecutive colonoscopic procedures performed on routinely scheduled patients. The study was conducted over a three-month period in the Gastroenterology Department at the University Hospital of Basel, Switzerland. The study protocol was approved by the local ethics committee. Inclusion criteria were sufficient knowledge of the German language, mental competence and the ability to place a vertical mark on a 100-mm visual analog scale (VAS) labeled only with descriptors at each end (0: none; 100: severe) [12]. The distance from the mark to the left end point was used to quantify the variable.
Prior to endoscopy, the patients were asked to estimate their level of anxiety (0: none; 100: extreme) and to name the primary reason for any fear. After the endoscopy, patients were asked “How bearable was the procedure for you?” (0: no problem; 100: unbearable). The attending endoscopy nurse and endoscopist were then asked “How bearable do you feel the procedure was for the patient?” (0: no problem; 100: unbearable). The nurse and endoscopist were also asked to evaluate the technical difficulty of the procedure (0: easy; 100: very difficult). All questions were posed in a blinded manner by someone not involved in the endoscopic procedure. For the statistical analysis, the assessments were categorized into two groups: values ≤50 were considered good, and those >50 were considered bad. The cut-off point of 50 was chosen arbitrarily as a qualitative interpretation of the VAS scale.
Demographic data, namely the age and gender of the patients, were recorded, as were the types and amounts of administered drugs and the duration of the procedure. The endoscopies were performed by 9 experienced gastroenterologists and 12 experienced endoscopy nurses in different combinations.
A Spearman correlation coefficient was calculated to evaluate the relationship between the assessments of the patients, nurses, and endoscopists. Categorical outcomes were analysed with the χ2 test or Fisher’s exact test where appropriate. P values <0.05 were considered significant. SPSS software (IBM SPSS, Version 20.0, IBM Corporation, Armonk, NY) was used for all statistical calculations.
Over a period of 12 weeks, 222 patients (108 females, 114 males; mean age, 62 years [SD 14.1]) were included in the study. A total of 215 patients (97%) received an opioid, either pethidine or alfentanil, as an analgesic; 48 patients (22%) were sedated with midazolam and 167 (75%) with propofol; and 7 patients (3%) had no sedation or analgesia. The mean duration of the procedure was 28 minutes (range: 9–107). A total of 156 (70%) patients indicated that their fear was primarily centred on the procedure itself (fig. 1). Overall, the patients judged the procedure as tolerable, with a mean value of 19 mm [SD 21] on the 100-mm VAS scale. However, 12% (27/222) of the patients (13 females, 14 males; mean age, 61 years [SD 13]) rated the examination as less tolerable (VAS >50 mm). Of the patients who rated the examination as less tolerable, 66% (18/27) were sedated with propofol (11% of the propofol group), 30% (8/27) were sedated with midazolam (17% of the midazolam group), and 1 patient was not sedated. The mean duration of the procedure in this group was 44 minutes (range: 10–92). The patients’ judgments of the tolerability were not related to either initial anxiety (r = 0.15) or differences in baseline characteristics (table 2).
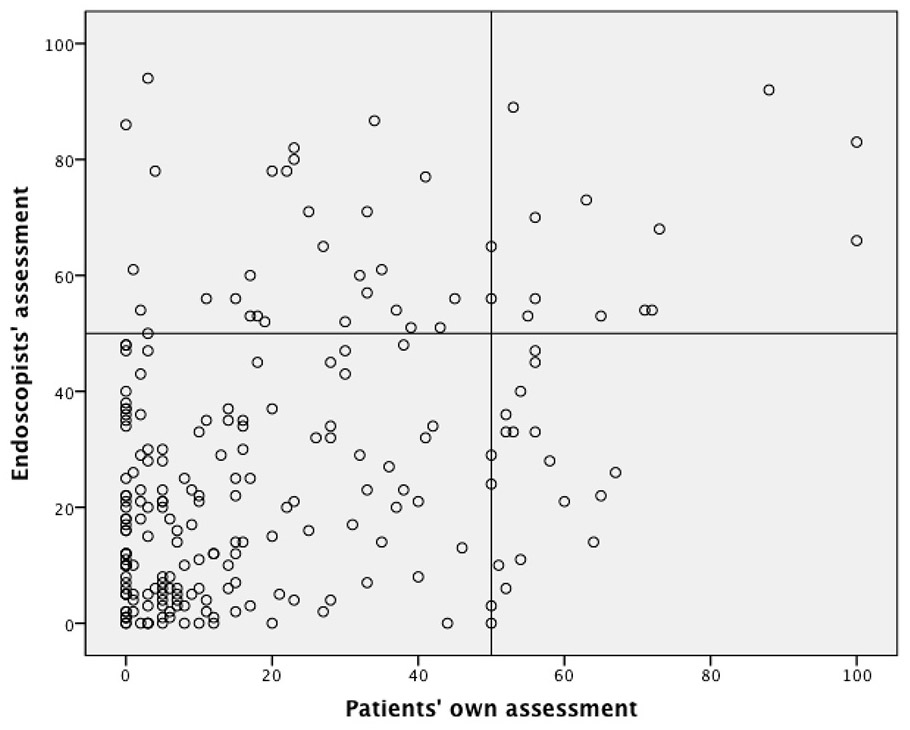
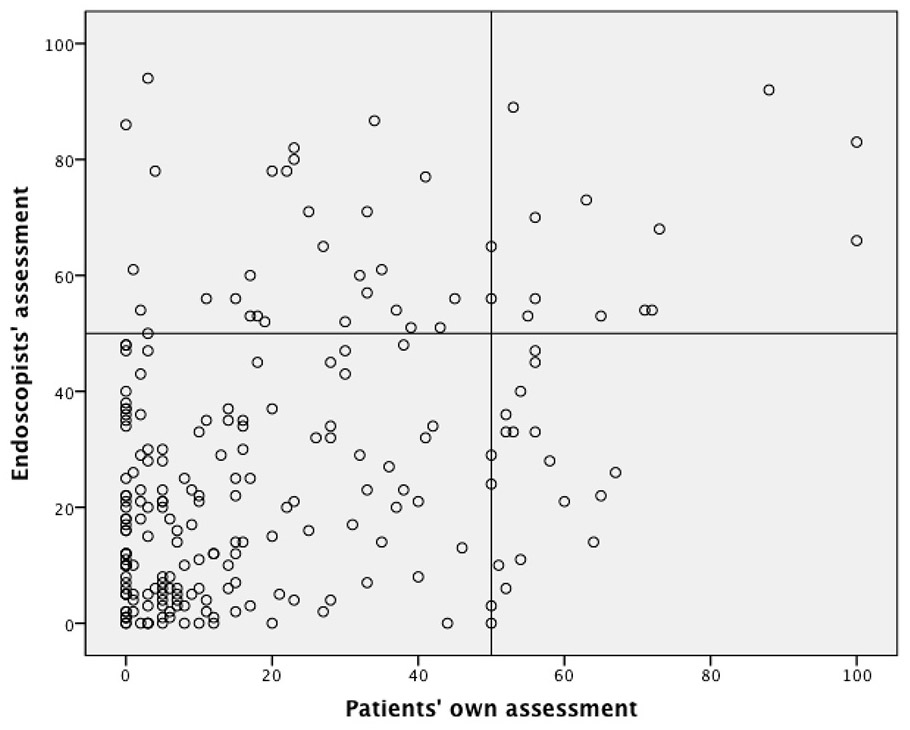
Figures 1A/B
Scatterplots showing the results of patients’ own assessments compared with the assessments of the endoscopists (1A) and nurses (1B).
The questions asked were “How bearable was the procedure for you?” (patients’ own assessment) and “How bearable do you feel the procedure was for the patient?” (endoscopists’ and nurses’ assessment). Above the 50-mm line, the procedure was categorized as unpleasant. VAS scale: 0, no problem; 100, unbearable.
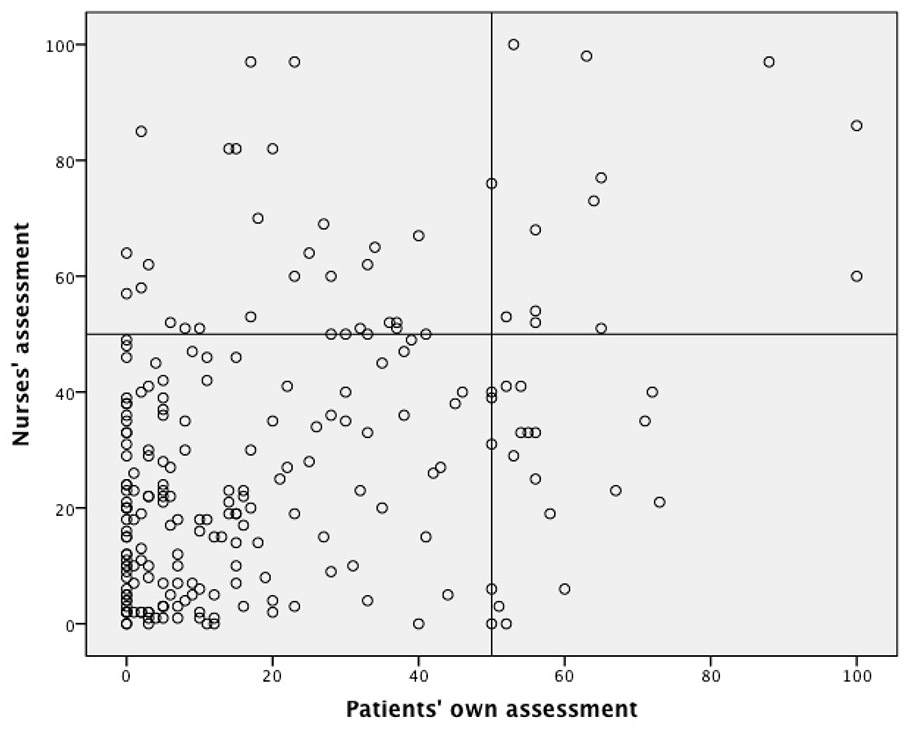
Endoscopists’ and nurses’ estimates of the procedure’s technical difficulty were highly correlated (r = 0.62). When evaluating patient discomfort, the scores of the endoscopists and nurses correlated better with each other (r = 0.58) than with the patients’ self-assessed scores (r = 0.37 and 0.35, respectively). Both endoscopists and nurses tended to overestimate the patients’ discomfort levels, with mean values of 27 mm [SD 2] and 28 mm [SD 2], respectively, on the 100-mm VAS scale. Scatterplots illustrate the lack of correlation between the patients’ own assessments and those of nurses and endoscopists (figures 1A and 1B). According to the arbitrary classification of a good experience corresponding to ≤50 mm and a bad experience corresponding to >50 mm, the endoscopists’ and nurses’ assessments corresponded to the patients’ statements in 79 and 81% of cases, respectively. In general, both endoscopists and nurses tended to overestimate patient discomfort, with a significant overestimation by at least one of them (the endoscopist or the nurse) in 19% (43) of patients. In 14 cases, both the endoscopist and nurse overestimated the level of discomfort for the same patient. Nevertheless, both professional groups underestimated patients’ perceived discomfort in 7% of cases (table 3). Among the 27 (12%) patients who rated their endoscopy experience as bad, only 8 (4%) were correctly identified by both members of the endoscopy team, a further 8 (4%) were correctly identified by at least one member of the team, but 11 (5%) were mis-classified by both (fig. 2).
| Table 1: Primary reasons that patients gave for being anxious before the colonoscopy (N = 156). | |
| Reason | N (%) |
| Procedure | 54 |
| Result | 22 |
| Both | 18 |
| Don’t know | 6 |
| Table 2: Comparison of the baseline characteristics of patients with good and bad assessments. | ||||
| Patient’s assessment: good (≤50 mm) N = 195 | Patient’s assessment: bad (>50 mm) N = 27 | |||
| Previous endoscopy n (%) | 100 | (51) | 15 | (56) |
| Preprocedural fear VAS mm (SD) | 33 | (± 30) | 37 | (± 30) |
| ASA I n (%) | 33 | (17) | 3 | (11) |
| ASA II n (%) | 71 | (36) | 11 | (40) |
| ASA III n (%) | 67 | (34) | 9 | (33) |
| Table 3:Concordance of patients’, endoscopists’ and endoscopy nurses’ assessments of the patients’ tolerability of the colonoscopy. | |||||
| Endoscopists’ assessment N (%) | Nurses’ assessment N (%) | ||||
| ≤50 mm good | >50 mm bad | ≤50 mm good | >50 mm bad | ||
| Patients’ assessment N (%) | ≤50 mm good | 165 (74) (correct) | 30 (13) (overestim.) | 168 (76) (correct) | 27 (12) (overestim.) |
| >50 mm bad | 15 (7) (underestim.) | 12 (5) (correct) | 15 (7) (underestim.) | 12 (5) (correct) | |
Although the endoscopists’ and nurses’ assessments of the technical difficulty of their joint work agreed to a high level, the endoscopists and nurses were much less able to correctly assess the discomfort of their patients.
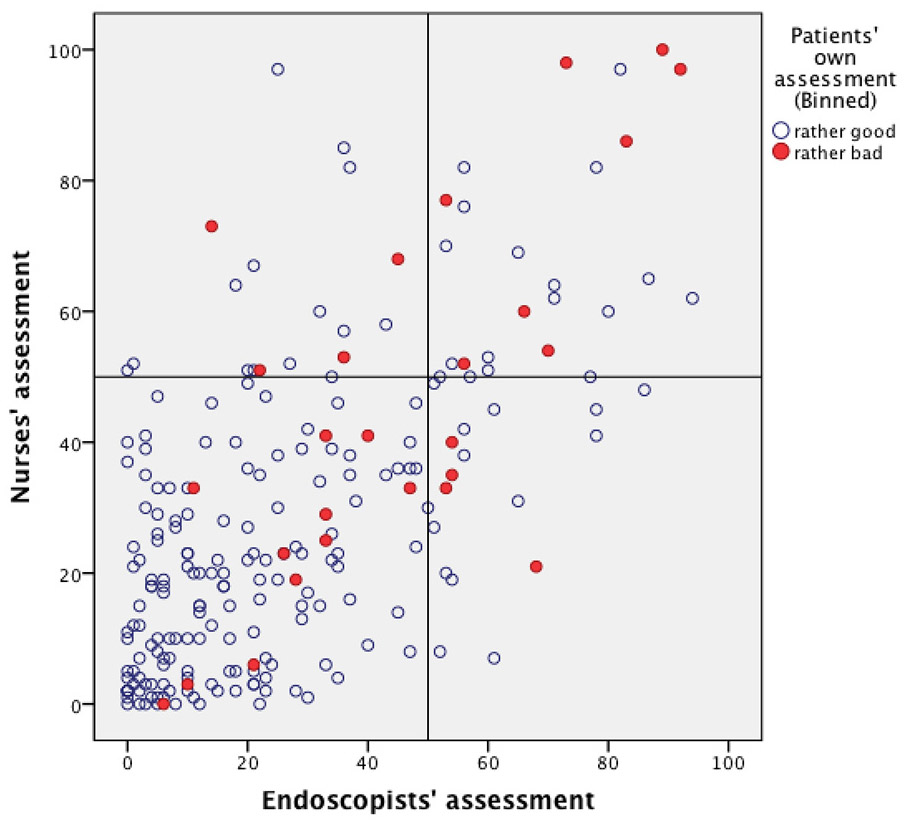
Figure 2
Scatterplots showing the results of endoscopists’ and nurses’ assessments.
Above the 50-mm line, the procedure was categorized as unpleasant. The shape of each dot indicates a patient’s own assessment: red dots represent a bad experience (VAS >50 mm), and open circles represent a good experience (VAS ≤50 mm). Questions and VAS scale: see Figures 1A and 1B.
Not surprisingly, the correct assessment of somebody else’s discomfort level is not easy. Although sedation and analgesia during colonoscopies have become routine, endoscopy teams are often confronted with a wide variety of individual patient behaviors and coping styles for pain and anxiety, which makes the adequate and immediate assessment of a patient’s discomfort difficult [13]. In our study, in two out of ten patients, the endoscopy teams did not correctly assess whether a colonoscopy was regarded by the patient as being nearly painless or highly uncomfortable. Although both physicians and nurses typically tended to overestimate the patients’ discomfort, the more problematic scenario of underestimation was found in 7% of cases. Of the 27 patients in our study who reported that the colonoscopy was a bad experience, 19 were not correctly identified by at least one member of the endoscopy team and may not have received adequate treatment during the procedure.
The overestimation of intolerability by one or both members of the endoscopy team in 19% of all cases may be explained by the (often desired) amnesic effect of sedative drugs. Nevertheless, the level of discomfort reported by 19 patients (9%) was underestimated by one of the team members, and in 11 patients (5%), the level of pain was not recognized by either the physician or the nurse. Among these patients, 7 were sedated with propofol, 3 were sedated with midazolam, and one patient was not sedated. There was no clustering of inappropriate assessments around any particular physician or nurse.
It is remarkable that among the cases in which the level of discomfort was not correctly judged by the medical staff, the sedative drug proportions exhibited the same distribution as that in the whole population, and one patient was even unsedated. In our view, this fact indicates that the misinterpretation of patient comfort levels may be due to different patient behaviors rather than due to an effect of the sedative drugs. Although it would be desirable to spare patients from unpleasant experiences (e.g., by deeper sedation and eliciting more amnesia), this study shows that in certain cases, the interpretation of individual behavior is not predictable based on baseline characteristics. It is noteworthy that these incorrect assessments cannot be prevented by the choice of a specific drug, e.g., propofol. The accuracy of the assessment of the level of comfort or discomfort of a sedated patient is different from that for unsedated patients; however, the aim of this study was to determine the level of concordance between the patients’ assessments and the team’s assessments rather than the concordance between groups exposed to different types of sedation.
Even though sedated endoscopy has become an accepted practice worldwide, there has been little interest in specific aspects of the patient-endoscopist-nurse interactions during the examination. Although many studies have investigated patient or endoscopist satisfaction, we are not aware of any previous studies that investigated the assessment of patient discomfort by the endoscopy team [14]. This lack of data is surprising considering that all of the sedation protocols involving midazolam or propofol, except for patient controlled sedation (PCS), are guided by the personal assessments of the endoscopist and the assisting nurse. Endoscopic procedures differ from other interventions carried out under sedation because the pain is not constant and directly depends on the procedure dynamics and the pressure applied to the instrument by the endoscopist.
This small study has several limitations that should be avoided in further studies on this topic. First, this study was restricted to one endoscopy centre and may therefore, to some extent, reflect a “local culture”. Furthermore, only a small number of patient-related variables, and no team-related variables, were collected before the procedure; therefore, several confounding variables may have been missed.
Nevertheless, this study highlights the fact that endoscopy teams may be professionally constrained by and accustomed to daily routine procedures and may not be critically observing each individual patient [15, 16]. Mutual unspoken confirmation may lead to a high accordance between team members and could result in the neglect of dissimulating patients or patients with uncommon complaints, such as retching, bloating and hiccups. As sedation-facilitated procedures become more common, it is important for medical teams to be aware that their estimation of a patient’s perception of discomfort may be incorrect in a considerable number of cases. Furthermore, the assessments of doctors and nurses may be closer to each other than they sometimes admit. Despite the recent advances made in endoscopy and sedation, there is no single correct measure of the level of comfort during endoscopic procedures; therefore, the patient’s personal feelings will remain the gold standard for assessing comfort levels. Therefore, the endoscopy team should make themselves aware of the patient’s feelings by being communicative and observant, with the goal of making the procedure a pleasant experience for all patients.
Acknowledgments: The authors thank C. Tapparelli and T. Hirt for their help in collecting the data and Prof. Burkhardt Seifert, University of Zurich, Division of Biostatistics, for statistical advice.
1 Rex DK. Colonoscopy: a review of its yield for cancers and adenomas by indication. Am J Gastroenterol. 1995;90(3):353–65.
2 Schoepfer A, Marbet UA. Colonoscopic findings of symptomatic patients aged 50 to 80 years suggest that work-up of tumour suspicious symptoms hardly reduces cancer-induced mortality. Swiss Med Wkly. 2005;135(45-46):679–83.
3 Parker D. Human responses to colonoscopy. Gastroenterol Nurs. 1992;15(3):107–9.
4 Mahajan RJ, Johnson JC, Marshall JB. Predictors of patient cooperation during gastrointestinal endoscopy. J Clin Gastroenterol. 1997;24(4):220–3.
5 Jones MP, Ebert CC, Sloan T, Spanier J, Bansal A, Howden CW, et al. Patient anxiety and elective gastrointestinal endoscopy. J Clin Gastroenterol. 2004;38(1):35–40.
6 Ward B, Shah S, Kirwan P, Mayberry JF. Issues of consent in colonoscopy: if a patient says “stop” should we continue? J R Soc Med. 1999;92(3):132–3.
7 Grendelmeier P, Kurer G, Pflimlin E, Tamm M, Stolz D. Feasibility and safety of propofol sedation in flexible bronchoscopy. Swiss Med Wkly. 2011;141: p. w13248.
8 Rex DK, Heuss LT, Walker JA, Qi R. Trained registered nurses/endoscopy teams can administer propofol safely for endoscopy. Gastroenterology. 2005;129(5):1384–91.
9 Heuss LT, Froehlich F, Beglinger C. Nonanesthesiologist-administered propofol sedation: from the exception to standard practice. Sedation and monitoring trends over 20 years. Endoscopy. 2012;44(5):504–11.
10 Heuss LT, Schnieper P, Drewe J, Pflimlin E, Beglinger C. Risk stratification and safe administration of propofol by registered nurses supervised by the gastroenterologist: a prospective observational study of more than 2000 cases. Gastrointest Endosc. 2003;57(6):664–71.
11 Watson JP, Goss C, Phelps G. Audit of sedated versus unsedated gastroscopy: do patients notice a difference? J Qual Clin Pract. 2001;21(1–2):26–9.
12 Revill SI, Robinson JO, Rosen M, Hogg MI. The reliability of a linear analogue for evaluating pain. Anaesthesia. 1976;31(9):1191–8.
13 Morgan J, Roufeil L, Kaushik S, Bassett M. Influence of coping style and precolonoscopy information on pain and anxiety of colonoscopy. Gastrointest Endosc. 1998;48(2):119–27.
14 Vargo J, Howard K, Petrillo J, Scott J, Revicki DA. Development and validation of the patient and clinician sedation satisfaction index for colonoscopy and upper endoscopy. Clin Gastroenterol Hepatol. 2009;7(2):156–62.
15 Dobkin PL, De Civita M, Abrahamowicz M, Bernatsky S, Schulz J, Sewitch M. Patient-physician discordance in fibromyalgia. J Rheumatol. 2003;30(6):1326–34.
16 Sewitch MJ, Abrahamowicz M, Dobkin PL, Tamblyn R. Measuring differences between patients’ and physicians’ health perceptions: the patient-physician discordance scale. J Behav Med. 2003;26(3):245–64.
Funding / competing conflicts of interest: No financial support and no other potential conflict of interest relevant to this article was reported.