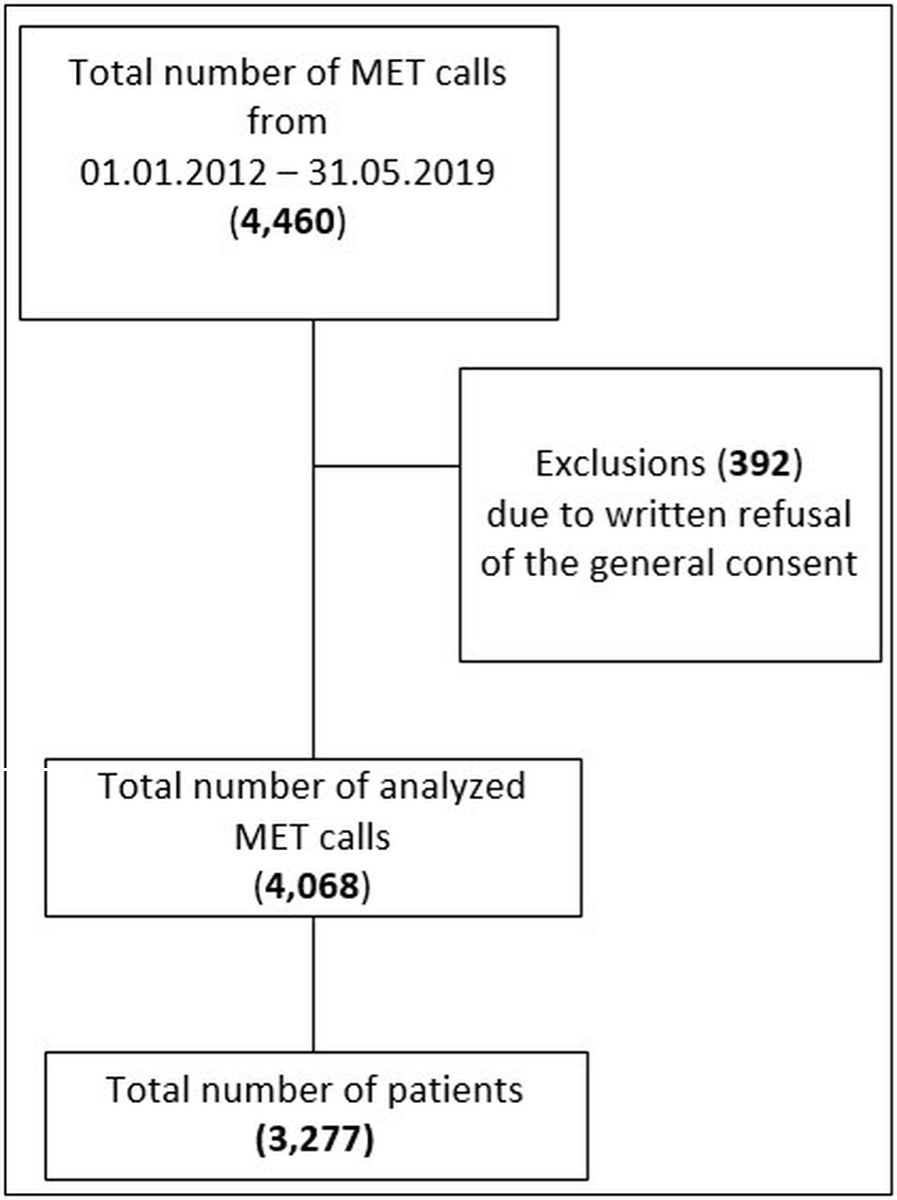
Figure 1 STROBE flowchart.
DOI: https://doi.org/10.57187/smw.2022.40006
In October 2009, the University Hospital Bern, Inselspital, was the first tertiary care centre in Switzerland to introduce a medical emergency team (MET), aiming to deliver critical care expertise at the bedside of deteriorating patients [1, 2]. The concept of the MET dates back to the nineties, when Lee and colleagues introduced a MET complementary to the cardiac arrest team in order to prevent irreversible metabolic and organ failure [3, 4]. Since then, MET or rapid response systems have been widely accepted and established in modern hospitals as a way to improve patients’ safety and outcome [5]. Many centres with rapid response systems use dedicated trigger scores to improve the detection of deteriorating patients, so-called early warning scores [6–8]. Such scoring systems increase the number of MET calls and decrease numbers of cardiac arrests and in-hospital mortality [9]. Some authors even suggest automated electronic notification systems to minimize afferent limb failure (failure to promptly recognise patient deterioration or activate the MET in response to it) [10]. However, such an approach might increase the number of inappropriate MET calls, imposing a significant burden on the MET itself. Our MET system allows for every staff member involved in patient care to call the MET and uses the vital sign score, a set of validated physiological parameters, as guidance to seek assistance of the MET in case of an impending deterioration [1, 11]. There are several studies describing the epidemiology of METs in other health care systems [2, 12–14], as well as the circadian distribution of MET activation [15, 16], however in Switzerland MET activation and the epidemiology of patients receiving MET calls is largely unknown. In addition, in the last decade, intensive care unit (ICU) and hospital admissions in our institution have increased, as has the proportion of multimorbid patients treated in the ICU in Europe [17]. Therefore, the aim of this retrospective observational study was to describe the reasons for MET calls over time, to analyse outcomes, and to describe the circadian distribution of MET calls and ICU admissions.
In this study, we analysed data collected on all MET calls between first of January 2012 until the 31st of May 2019. Some data have previously been published in an analysis by our institution, which reviewed process parameter to establish the prognostic significance of antecedents of MET calls on patient outcomes in the context of MET calls and was performed between 2009 and 2013 [1]. The study was approved by the Ethical Committee on human research of the Canton of Bern (EC approval no.: 2019-01260) and adheres to the tenets of the Declaration of Helsinki. Patient consent was waived by the Ethical Committee, however we excluded all patients with documented written refusal of the general consent. Study reporting complies with the “STrengthening the Reporting of OBservational studies in Epidemiology (STROBE)” guidelines [18].
The primary objective of this study was to describe the reasons for MET calls and outcomes over time. Secondary objectives were to describe the circadian distribution of MET calls and ICU admissions, the reasons for MET calls in the overall population, distribution of referring wards over time and the diagnosis category leading to the MET call.
All data on date and time of MET event, baseline characteristics of the patient, vital sings at the beginning and end of each MET call, outcome of the MET event (death or alive), disposition (ICU, intermediate care [IMC], emergency department, operation theatre or ward), and diagnosis are routinely collected at the time of the event by the responsible attending physician, and entered prospectively into a MET database by research staff. Reasons for the MET call are documented by choosing one of the MET calling criteria described below [11]. Each MET event is attributed to a diagnosis group by the respective MET physician. In the interest of study purposes additional data on mortality, length of hospital and ICU stay were extracted from the hospital patient administration system and merged with the MET database before analysis.
The University Hospital of Bern, Switzerland, is a 900-bed tertiary academic centre with a mixed 36 bed ICU, and 26 IMC beds. We have a large general internal department with several wards, as well as wards for all internal and surgical subspecialties (e.g. nephrology, oncology, orthopaedics, visceral surgery, etc.). We tagged patients from all non-surgical specialties as “medical”, and surgical subspecialties as “surgical”.
Our MET is staffed by a board certified intensivist and an accredited intensive care nurse and is available 24/7 everywhere in the hospital, except in the emergency department, on paediatric wards and inside operating theaters [1]. The vital sign score criteria consist of threatened airway, respiratory rate <6/min or >35/min, peripheral oxygen saturation (SpO2) <90% despite supplemental oxygen, systolic blood pressure <90 mm Hg, heart rate <40/min or >140/min, Glasgow coma scale score (GCS) <13/15 or a drop by ≥2 points, and repeated or prolonged (>5 minutes) seizure. In addition, our MET calling criteria include a “concern” criterion as a fall-back position for hospital staff if their concern about a patient’s well-being does not meet the physiological criteria [19]. The MET dose is defined as number of MET calls per 1000 hospital admissions [20].
Nursing shifts were defined as: day shift 7:00 to 15:59, evening shift 16:00 to 22:59 and night shift 23:00 to 6:59. Doctors’ day shifts on duty were defined as 8:00 to 16:59; accordingly out of hours was 17:00 to 7:59.
Normal distribution of continuous variables were tested with the Shapiro-Wilk test. Normally distributed variables are presented as mean ± standard deviation. Skewed or interval and ordinal variables are presented as medians with interquartile ranges (IQRs). All MET calls were allocated to the hourly intervals over the 24-hour cycle of the day based on the time of activation. Comparisons of categorical variables were be performed using Pearson’s chi-square test or Fisher’s exact test for two groups, and the Kruskal-Wallis rank sum test for the comparison of three groups [4]. Statistical analyses were performed with R (R Studio, PBC, Version 1.4.1106).
The study was approved by the Ethics Committee on human research of the Canton of Bern (EC no.: 2019-01260) and adheres to the tenets of the Declaration of Helsinki, and individual informed consent was waived by the ethics committee.
From 1 January 2012 to 31 May 2019, a total number of 4459 MET calls were documented, involving 3627 patients. After excluding patients with documented written refusal, a total of 4068 calls involving 3277 patients remained in the final analysis set (see fig. 1), of whom 37% were female (n = 1210). The mean age was 65.9 (±15.7 years. Mean age increased over time (see fig. 4). About one in ten patients requiring a MET call was initially hospitalised in the ICU (n = 366 patients, 9.1%), whereof 180 were re-admitted to the ICU via MET. A total of 581 patients (17.7%) had more than one MET call (range 2–7) and in 24 patients, the MET calls occurred during the same hospitalisation. Median time between those MET calls was 119.4 hours (IQR 48.5–360.5). Only 0.2% of all calls (9/4068) were repeat MET calls in patients left on the ward who were then admitted to the ICU.
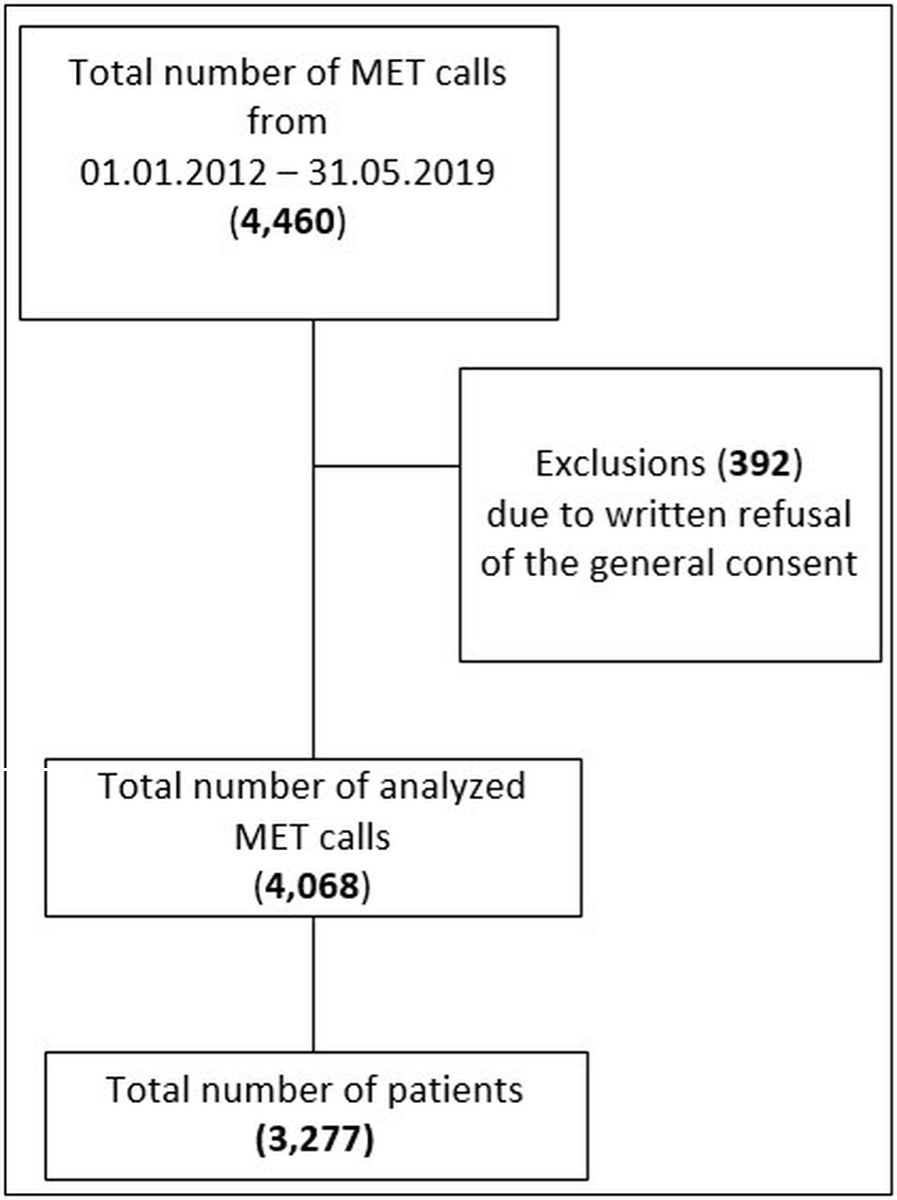
Figure 1 STROBE flowchart.
Table 1Baselines and outcomes according to nursing shifts.
| N* | Overall (n = 4068) 1 | Shift | p-value2 | |||
| Day (n = 1494) 1 | Evening (n = 1336) 1 | Night (n = 1238) 1 | ||||
| Age | 3277┼ | 65.9 (15.7) | 65.0 (15.8) | 65.4 (15.8) | 67.5 (15.5) | <0.001 |
| Sex (female) | 3277** | 1210 (37%) | 457 (39%) | 380 (35%) | 373 (37%) | 0.2 |
| BMI | 2679** | 25.5 (22.3, 29.2) | 25.3 (21.9, 29.2) | 25.6 (22.5, 29.3) | 25.7 (22.3, 29.2) | 0.3 |
| LOS (days) | 4068 | 16 (9, 30) | 17 (9, 31) | 16 (8, 29) | 17 (9, 30) | 0.077 |
| MET response time (min)┼┼┼ | 4068 | 5 (0–374) | 5 (0–374) | 5 (0–150) | 5 (0–185) | 0.004 |
| MET duration (min) | 4068 | 25 (15, 30) | 25 (16, 33) | 23 (15, 30) | 23 (15, 30) | <0.001 |
| Ward | 4068 | 0.045 | ||||
| – Medical | 2514 (62%) | 932 (62%) | 851 (64%) | 731 (59%) | ||
| – Surgical | 1554 (38%) | 562 (38%) | 485 (36%) | 507 (41%) | ||
| Disposition | 4,059 | |||||
| – Remained on ward | 1993 (49%) | 652 (45%) | 685 (52%) | 656 (53%) | <0.001 | |
| – Intensive care | 1871 (46%) | 735 (50%) | 586 (44%) | 550 (44%) | 0.007 | |
| – Intermediate care | 163 (4.0%) | 73 (5.0%) | 58 (4.4%) | 32 (2.6%) | 0.007 | |
| – Other (emergency department, operating room) | 32 (0.8%) | 28 (1.9%) | 4 (0.3%) | 0 (0%) | - | |
| Outcome | ||||||
| – 24-hour mortality | 3277** | 225 (5.5%) | 87 (5.8%) | 52 (3.9%) | 86 (6.9%) | 0.003 |
| - In hospital mortality | 3277** | 880 (22%) | 332 (22%) | 281 (21%) | 267 (22%) | 0.7 |
1 Mean (standard deviation); n (%); median (IQR), ┼┼┼ (range)
2 Kruskal-Wallis rank sum test; Pearson's chi-square test; Fisher's exact test
* Total of 4068
** Total of 3277 patients
BMI: body mass index; LOS: length of hospital stay; MET: medical emergency team
The mean number of MET calls per month was 49.2 (±11.7), and increased from 35.8 calls per month in 2012 to 58.8 calls per month in 2019. The total number of hospital admissions increased from 55,029 in 2012 to 86,905 in 2018. The MET dose remained relatively stable over the years, with a median of 8.0 calls/1000 hospitalisations (IQR 7.0–10.0). A total of 2526 calls (62%) occurred out of hours (between 5 pm and 8 am). Peak MET activation hours were noted during the evening shift: 1375 calls (33.8%) were documented during the 7-hour evening shift (mean 196.4 calls/hours), 1238 calls (30.4%) during the 8-hour night shift (mean 154.8 calls/hour), 1455 calls (35.8%) during the 9-hour day shift (mean 161.7 calls/hour) (fig. 2).

Figure 2 MET calls by hour of the day.
Dark grey line: All MET calls; light grey line: MET calls on medical wards; dotted line: MET calls on surgical wards. Blue shades: half hour before and after nursing shift changes, red arrows indicate beginning and end of doctors’ day shifts (8 am to 5 pm), blue horizontal line: average of calls.
The reason for MET activation was reported for 3473 patients (85.4%). The most common reason was “staff concern” for any reason, in 1192 calls (34%). In 64.8% (n = 760) of those cases, the patient could be managed on the ward, 30.7% were transferred to the ICU, and 52 calls (4.4%) were transferred to IMC. The second most common cause for a MET call was low SpO2 refractory to oxygen therapy, in 776 calls (22%) whereof in 61.6% calls (n = 478) the patients had to be admitted to intensive care. The respiratory rate was reason for 44 (1.3%) of calls. Half of the patients with an abnormal respiratory rate had a rate above 35/min (n = 24, 54.6%), one had a rate <6/min, and the majority had a rate above 22/min (n = 38, 86.4%). The reasons for MET calls remained similar over the years, apart from the respiratory rate, which was first documented in 2017 and was the reason in 6.8% of calls in 2019 (fig. 3).
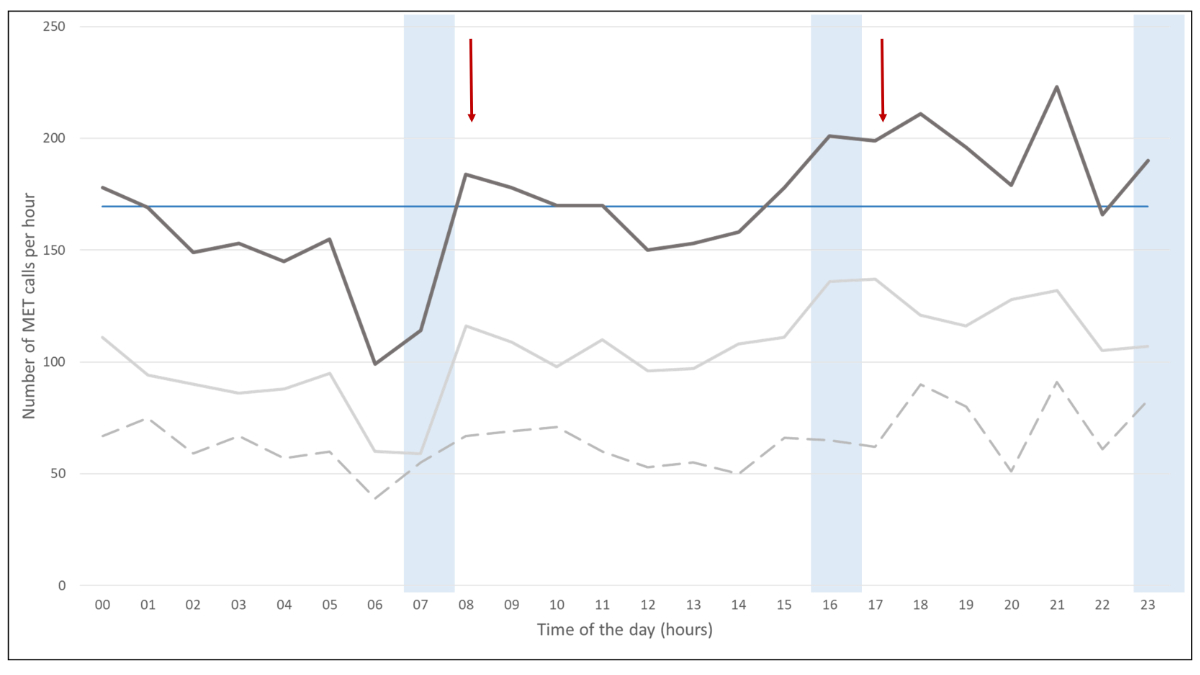
Figure 3 Reason for medical emergency team calls over time.
Oxygen saturation: <90% despite supplemental oxygen; systolic blood pressure: <90 mm Hg; Glasgow coma scale (GCS): <13/15 or a drop by ≥2 points; heart rate: <40/min or >140/min; seizure: repeated or prolonged (>5min); respiratory rate: <6/min or >35/min.
In 997 (24.5%) cases, the main cause for deterioration was respiratory (e.g. pneumonia, respiratory distress, aspiration). Sepsis and septic shock was the main cause in 743 cases (18.2%) and in 728 cases (17.9%) the event was categorised as cardiovascular.
The majority of MET calls (2514, 61.7%) were for patients on medical wards, whereas 1554 (38.2%) calls were documented in surgical wards. Most of the MET calls were for patients admitted to a general internal ward (n = 831 calls, 20%), visceral surgery and gastroenterology (n = 545 calls, 13%), oncology (396 calls, 9.7%), orthopaedics (n = 391 calls, 9.6%) and cardiovascular surgery (n = 291 calls, 7.2%).
After the evaluation by the MET, in 1993 (49%) cases the patients remained on the ward, in 1871 (46%) cases the patients required ICU admission and in 163 (4%) cases the patients were admitted to IMC. In 32 calls, patients were referred to another department (e.g. emergency department for further assessment, operation theatre) and in 9 cases the data were missing. The rate of patients admitted to ICU was significantly higher during the day shift (n = 735, 49%), compared with the evening (n = 586, 44%) or night shift (n = 550, 44%; p = 0.007).
The 24-hour mortality after a MET call was 5.7% and in-hospital mortality was 22%. Twenty-four-hour mortality increased over time (see fig. 4) and was significantly higher during night shifts (7.1%) than during evening (3.8%) or day shifts (6.3%; p = 0.03). In our cohort, in only 559 (14 %) cases there was a “do not resuscitate” (DNR) order in place.
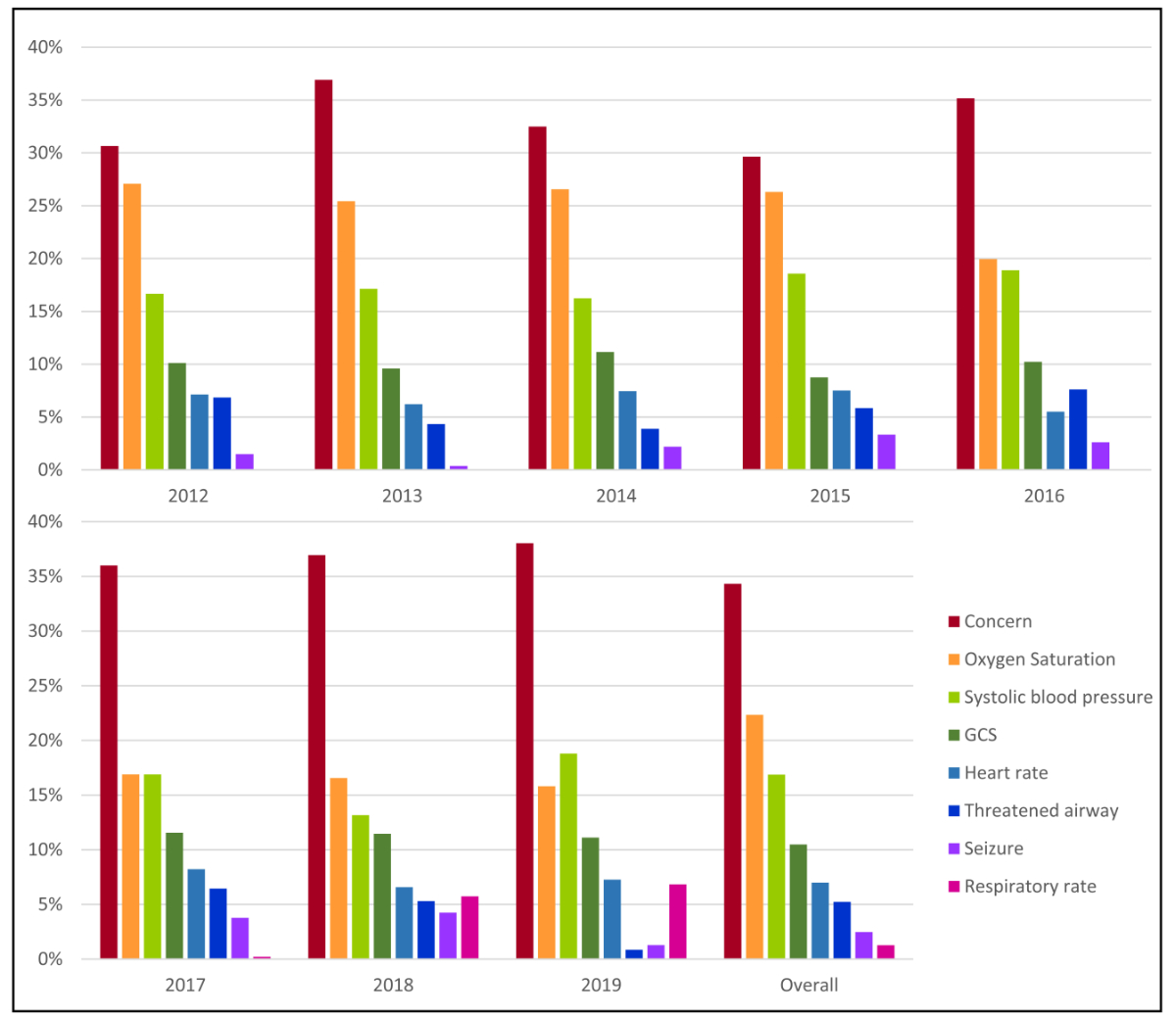
Figure 4 Mortality and age of patients triggering ing MET calls over time.
Over a period of 7 years, the number of MET calls in our institution increased from 35.8 calls per month in 2012 to 58.8 calls per month in 2019, but the “MET dose” remained relatively constant at 8.0 calls/1000 hospitalisations. The most frequent reasons for a MET call were staff concern, low SpO2, and decrease in GCS. MET calls occurred predominantly on general medical wards. Although one in five patients died in hospital after a MET call, 24-hour mortality was low (5%), and increased during night shifts. The higher mortality during the night-shifts is unclear. However, patients who receive MET calls at night are older, and it may be that they have limitation of care in place. In addition, older patients tend to be underestimated regarding the acuity of their conditions which may influence the disposition decision [45]. In-hospital mortality was 22% and is comparable to other studies on rapid response systems and our previous study [1, 14, 21]. However, we noticed a decrease in mortality in 2018. The reason for this observation remains unclear (due to the observational nature of our analysis).
Previous data show a vast variation of MET dose, ranging from 3 to 149/1000 hospitalisations depending on healthcare systems and regions [8, 22–27]. One reason for the variation in numbers might be the definition and role of the MET; in some hospitals, MET and resuscitation teams are the same team, and in other centres, such as ours, the MET is different from the resuscitation team, and therefore the MET dos not attend cardiac arrests. Another reason might be that our calling criteria might be less stringent than in other healthcare systems, where a change in scores rather than an individual vital sign triggers an escalation to the MET (e.g. the National Early Warning Score – NEWS – in the UK [28, 29]). Our data seem in line with those reported from Japan and Sweden, with MET doses of 6.6/1000 hospitalisations, and 11/1000 hospitalisations, respectively [27, 30].
Most MET calls were activated on medical wards (62%), and only a third were attributed to surgical wards. This seems in line with the literature, where studies report a two thirds / one third ratio in MET referrals from medical and surgical units [31]. Therefore, when planning to introduce a MET system, these may be the units were it could be worthwhile to establish the MET system with priority.
We noted a considerable increase in MET calls in the morning after nursing handover. This could theoretically be due to reduced routine observations performed during the night time, but exact reasons remain speculative. Approximately 60% of our MET calls were activated between out-of-hours (5 pm to 8 am), when fewer senior doctors are present [4, 32], which was also observed in a study by Bellomo et al. [9]. However, a majority of patients seen out-of-hours remained on wards, whereas more patients were admitted to the ICU during daytime. This might support the theory that more calls are made when wards are covered by junior doctors. As seen in figure 2, in the evening, the number of MET calls are above mean hourly rate. This has important implications for resource allocation to the MET service during the evening shifts.
The majority of MET calls were due to staff’s concern regarding patient well-being. This is well in line with a previous data analysis from the same hospital, where most calls were due to concern [1]. This criterion subsumes not only the subjective concern about a potential deterioration, but also signs and symptoms that don’t fit into any category of the vital sign score, such as agitation, delirium, uncontrollable pain or acute chest pain. All of these symptoms might have a potential life-threatening underlying cause and, therefore, it seems important not to limit MET activation only to patients fitting into a vital sign score, such as NEWS or MEWS [8, 29, 33–35]. Accordingly, the criterion “staff concern” has been reported to be the most frequent reason for MET calls in other studies [36, 37]. However, sociocultural reasons may prevent worried staff from calling the MET when indicated. One study on incidence and factors behind failure to activate the rapid response team revealed that the majority of the bedside staff on the ward was aware of the deterioration and concerned about the patient. One of the main barriers for calling the MET was a feeling that they should be able to manage patients by themselves on the ward [38]. Therefore, including the criterion “staff concern” is one step to break down this barrier.
The low rate of MET calls due to abnormal respiratory rate suggests that this is still under-recorded on hospital wards [30]. Studies have shown that the introduction of a MET system was associated with improvement in the rate of documentation of vital signs [40]. Interestingly, we observed increasing rates of MET calls due to an abnormal respiratory rate after 2017 (fig. 3), the year after the publication of the third international consensus definition for sepsis and septic shock (Sepsis-3) in 2016 [41], which promoted the use of the quick sequential organ failure assessment (qSOFA). This abbreviated score contains altered mental state and systolic blood pressure in addition to respiratory rate as diagnostic criteria. It is conceivable that the qSOFA score led to an increased awareness of abnormal respiratory rate as a key predictor of adverse events [42, 43]. This is also reflected by the fact that the majority of patients with a MET call due to abnormal respiratory rate had a rate of above 22/min, and not according to our calling criteria (>35/min).
Importantly, our MET and ICU has 24/7 board-certified intensivist staffing, which on one hand could positively influence the outcome. On the other hand, as a large tertiary academic hospital, we treat a high volume of highly complex patients with greater illness severity and thus higher risk of detrimental outcome. In our population, only a minority of patients had treatment limitations prior to the MET call. This might simply reflect a selection bias, as we might get less involved in patients with advanced directives and clear treatment limitations. However, a previous study has revealed that a third of the limitation of medical therapy (LOMT) or do-not-resuscitate (DNR) decisions are taken in close conjunction to a MET review. Moreover, treatment limitations do not preclude repeated MET reviews [44]. This suggests that MET teams appear to be often involved in LOMT decisions and may indicate a need to support wards in charge of patients at the end of life.
To our knowledge, this is the largest analysis of MET calls in Switzerland. We report detailed, large-scale information on prospectively recorded MET calls and our results provide important information on the most frequent trigger criteria, key reasons for clinical deterioration and patient outcomes. Such data seem important for resource allocation and staffing models for hospitals with similar services.
However, the present retrospective observational study has limitations, as it is purely descriptive (by nature of the study design). In addition, it is a single centre study, and therefore lacks generalisability. Further, although the patient’s DNR status was available, we could not obtain information on advanced directives concerning intensive care admission. In addition, our MET calls are recorded on a written report form filled out by the physician who attends the call, which could lead to data transmission errors, as well as missed documentation of MET calls. However, according to our documentation, the MET dose stayed relatively constant over the years, suggesting stable adherence to reporting.
In our cohort, patients reviewed by the MET had an in-hospital mortality of 22%. While the most common reasons for a MET call over the years were staff concern and low oxygen saturation, abnormal respiratory rate was the least frequent among the calling criteria and only gained recognition after the introduction of the qSOFA in 2016. Most MET service activation were observed during evening shifts, highlighting the importance of proper resource allocation in respective shifts. Most MET calls occurred in patients admitted to medical wards.
The data are available upon reasonable non-commercial request from the author.
ASM, LC, JCS designed the work; ASM, LC, RL, and CAP performed the data collection, ASM and AE did the data cleaning and performed the data analysis, and ASM, LC and JCS interpreted the data. ASM, LC, and EC drafted the manuscript, and CAP, RL, and JCS revised it for important intellectual content.
No external funding was received for this project.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. ASM, CAP and JCSreport grants from Orion Pharma, Abbott Nutrition International, B. Braun Medical AG, CSEM AG, Edwards Lifesciences Services GmbH, Kenta Biotech Ltd, Maquet Critical Care AB, Omnicare Clinical Research AG, Nestle, Pierre Fabre Pharma AG, Pfizer, Bard Medica S.A., Abbott AG, Anandic Medical Systems, Pan Gas AG Healthcare, Bracco, Hamilton Medical AG, Fresenius Kabi, Getinge Group Maquet AG, Dräger AG, Teleflex Medical GmbH, Glaxo Smith Kline, Merck Sharp and Dohme AG, Eli Lilly and Company, Baxter, Astellas, Astra Zeneca, CSL Behring, Novartis, Covidien, Phagenesis, Cytel, and Nycomed outside the submitted work. The money was paid into departmental funds; no personal financial gain applied. All other authors have nothing to disclose.
1. Etter R, Takala J, Merz TM. Intensive care without walls - introduction of a Medical Emergency Team system in a Swiss tertiary care centre. Swiss Med Wkly. 2014 Oct;144:w14027. https://doi.org/10.4414/smw.2014.14027
2. Andersen LW, Kim WY, Chase M, Berg KM, Mortensen SJ, Moskowitz A, et al.; American Heart Association’s Get With the Guidelines(®) – Resuscitation Investigators. The prevalence and significance of abnormal vital signs prior to in-hospital cardiac arrest. Resuscitation. 2016 Jan;98:112–7. https://doi.org/10.1016/j.resuscitation.2015.08.016
3. Daly FF, Sidney KL, Fatovich DM. The Medical Emergency Team (MET): a model for the district general hospital. Aust N Z J Med. 1998 Dec;28(6):795–8. https://doi.org/10.1111/j.1445-5994.1998.tb01556.x
4. Lee A, Bishop G, Hillman KM, Daffurn K. The Medical Emergency Team. Anaesth Intensive Care. 1995 Apr;23(2):183–6. https://doi.org/10.1177/0310057X9502300210
5. Herod R, Frost SA, Parr M, Hillman K, Aneman A. Long term trends in medical emergency team activations and outcomes. Resuscitation. 2014 Aug;85(8):1083–7. https://doi.org/10.1016/j.resuscitation.2014.04.010
6. Buist M, Bernard S, Nguyen TV, Moore G, Anderson J. Association between clinically abnormal observations and subsequent in-hospital mortality: a prospective study. Resuscitation. 2004 Aug;62(2):137–41. https://doi.org/10.1016/j.resuscitation.2004.03.005
7. Cretikos M, Parr M, Hillman K, Bishop G, Brown D, Daffurn K, et al. Guidelines for the uniform reporting of data for Medical Emergency Teams. Resuscitation. 2006 Jan;68(1):11–25. https://doi.org/10.1016/j.resuscitation.2005.06.009
8. Ahn JH, Jung YK, Lee JR, Oh YN, Oh DK, Huh JW, et al. Predictive powers of the Modified Early Warning Score and the National Early Warning Score in general ward patients who activated the medical emergency team. PLoS One. 2020 May;15(5):e0233078. https://doi.org/10.1371/journal.pone.0233078
9. Bellomo R, Goldsmith D, Uchino S, Buckmaster J, Hart G, Opdam H, et al. Prospective controlled trial of effect of medical emergency team on postoperative morbidity and mortality rates. Crit Care Med. 2004 Apr;32(4):916–21. https://doi.org/10.1097/01.CCM.0000119428.02968.9E
10. Subbe CP, Duller B, Bellomo R. Effect of an automated notification system for deteriorating ward patients on clinical outcomes. Crit Care. 2017 Mar;21(1):52. https://doi.org/10.1186/s13054-017-1635-z
11. Etter R, Ludwig R, Lersch F, Takala J, Merz TM. Early prognostic value of the medical emergency team calling criteria in patients admitted to intensive care from the emergency department. Crit Care Med. 2008 Mar;36(3):775–81. https://doi.org/10.1097/CCM.0B013E3181643C15
12. Jones D. The epidemiology of adult Rapid Response Team patients in Australia. Anaesth Intensive Care. 2014 Mar;42(2):213–9. https://doi.org/10.1177/0310057X1404200208
13. Opio MO, Nansubuga G, Kellett J. In-hospital mortality of acutely ill medical patients admitted to a resource poor hospital in sub-Saharan Africa and to a Canadian regional hospital compared using the abbreviated VitalPAC Early Warning Score. Eur J Intern Med. 2014 Feb;25(2):142–6. https://doi.org/10.1016/j.ejim.2013.09.013
14. Psirides AJ, Hill J, Jones D. Rapid Response Team activation in New Zealand hospitals-a multicentre prospective observational study. Anaesth Intensive Care. 2016 May;44(3):391–7. https://doi.org/10.1177/0310057X1604400314
15. Jones D, Bates S, Warrillow S, Opdam H, Goldsmith D, Gutteridge G, et al. Circadian pattern of activation of the medical emergency team in a teaching hospital. Crit Care. 2005 Aug;9(4):R303–6. https://doi.org/10.1186/cc3537
16. Conway SR, Tegtmeyer K, Wheeler DS, Loechtenfeldt A, Stalets EL, Brady PW. Diurnal Variation in Medical Emergency Team Calls at a Tertiary Care Children’s Hospital. Pediatr Qual Saf. 2020 Sep;5(5):e341. https://doi.org/10.1097/pq9.0000000000000341
17. Flaatten H, De Lange DW, Morandi A, Andersen FH, Artigas A, Bertolini G, et al.; VIP1 study group. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med. 2017 Dec;43(12):1820–8. https://doi.org/10.1007/s00134-017-4940-8
18. Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al.; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology. 2007 Nov;18(6):805–35. https://doi.org/10.1097/EDE.0b013e3181577511
19. Etter R, Ludwig R, Lersch F, Takala J, Merz TM. Early prognostic value of the medical emergency team calling criteria in patients admitted to intensive care from the emergency department. Crit Care Med. 2008 Mar;36(3):775–81. https://doi.org/10.1097/CCM.0B013E3181643C15
20. Jones D, Bellomo R, DeVita MA. Effectiveness of the Medical Emergency Team: the importance of dose. Crit Care. 2009;13(5):313–313. https://doi.org/10.1186/cc7996
21. ANZICS-CORE MET dose investigators. Mortality of rapid response team patients in Australia: a multicentre study. Crit Care Resusc. 2013 Dec;15(4):273–8.24289508
22. Jeon SB, Lee HB, Koo YS, Lee H, Lee JH, Park B, et al. Neurological Emergencies in Patients Hospitalized With Nonneurological Illness. J Patient Saf. 2021 Dec;17(8):e1332–40. https://doi.org/10.1097/PTS.0000000000000682
23. Parmar A, Meeberg G, Bigam D, Richardson H, Gibney RT, Bagshaw SM. Peri-operative medical emergency team activation in liver transplantation. BMJ Qual Saf. 2011 Mar;20(3):243–50. https://doi.org/10.1136/bmjqs.2010.041541
24. Boniatti MM, Azzolini N, da Fonseca DL, Ribeiro BS, de Oliveira VM, Castilho RK, et al. Prognostic value of the calling criteria in patients receiving a medical emergency team review. Resuscitation. 2010 Jun;81(6):667–70. https://doi.org/10.1016/j.resuscitation.2010.01.025
25. Tirkkonen J, Tamminen T, Skrifvars MB. Outcome of adult patients attended by rapid response teams: A systematic review of the literature. Resuscitation. 2017 Mar;112:43–52. https://doi.org/10.1016/j.resuscitation.2016.12.023
26. Devita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006 Sep;34(9):2463–78. https://doi.org/10.1097/01.CCM.0000235743.38172.6E
27. Jäderling G, Calzavacca P, Bell M, Martling CR, Jones D, Bellomo R, et al. The deteriorating ward patient: a Swedish-Australian comparison. Intensive Care Med. 2011 Jun;37(6):1000–5. https://doi.org/10.1007/s00134-011-2156-x
28. Whebell SF, Prower EJ, Zhang J, Pontin M, Grant D, Jones AT, et al. Increased time from physiological derangement to critical care admission associates with mortality. Crit Care. 2021 Jun;25(1):226. https://doi.org/10.1186/s13054-021-03650-1
29. Physicians RC. National Early Warning Score (NEWS): Standardising the assessment of acute illness severity in the NHS. Report of a working party. London: RCP; 2012.
30. Kurita T, Nakada TA, Kawaguchi R, Fujitani S, Atagi K, Naito T, et al.; IHER-J collaborators. Impact of increased calls to rapid response systems on unplanned ICU admission. Am J Emerg Med. 2020 Jul;38(7):1327–31. https://doi.org/10.1016/j.ajem.2019.10.028
31. Mullins CF, Psirides A. Activities of a Medical Emergency Team: a prospective observational study of 795 calls. Anaesth Intensive Care. 2016 Jan;44(1):34–43. https://doi.org/10.1177/0310057X1604400107
32. Sundararajan K, Flabouris A, Thompson C. Diurnal variation in the performance of rapid response systems: the role of critical care services-a review article. J Intensive Care. 2016 Feb;4(1):15. https://doi.org/10.1186/s40560-016-0136-5
33. Tirkkonen J, Olkkola KT, Huhtala H, Tenhunen J, Hoppu S. Medical emergency team activation: performance of conventional dichotomised criteria versus national early warning score. Acta Anaesthesiol Scand. 2014 Apr;58(4):411–9. https://doi.org/10.1111/aas.12277
34. Smith GB, Prytherch DR, Jarvis S, Kovacs C, Meredith P, Schmidt PE, et al. A Comparison of the Ability of the Physiologic Components of Medical Emergency Team Criteria and the U.K. National Early Warning Score to Discriminate Patients at Risk of a Range of Adverse Clinical Outcomes. Crit Care Med. 2016 Dec;44(12):2171–81. https://doi.org/10.1097/CCM.0000000000002000
35. Subbe CP, Gao H, Harrison DA. Reproducibility of physiological track-and-trigger warning systems for identifying at-risk patients on the ward. Intensive Care Med. 2007 Apr;33(4):619–24. https://doi.org/10.1007/s00134-006-0516-8
36. Santiano N, Young L, Hillman K, Parr M, Jayasinghe S, Baramy LS, et al. Analysis of medical emergency team calls comparing subjective to “objective” call criteria. Resuscitation. 2009 Jan;80(1):44–9. https://doi.org/10.1016/j.resuscitation.2008.08.010
37. Chen J, Bellomo R, Hillman K, Flabouris A, Finfer S; MERIT Study Investigators for the Simpson Centre and the ANZICS Clinical Trials Group. Triggers for emergency team activation: a multicenter assessment. J Crit Care. 2010 Jun;25(2):359.e1–7. https://doi.org/10.1016/j.jcrc.2009.12.011
38. Shearer B, Marshall S, Buist MD, Finnigan M, Kitto S, Hore T, et al. What stops hospital clinical staff from following protocols? An analysis of the incidence and factors behind the failure of bedside clinical staff to activate the rapid response system in a multi-campus Australian metropolitan healthcare service. BMJ Qual Saf. 2012 Jul;21(7):569–75. https://doi.org/10.1136/bmjqs-2011-000692
39. Cretikos MA, Bellomo R, Hillman K, Chen J, Finfer S, Flabouris A. Respiratory rate: the neglected vital sign. Med J Aust. 2008 Jun;188(11):657–9. https://doi.org/10.5694/j.1326-5377.2008.tb01825.x
40. Chen J, Hillman K, Bellomo R, Flabouris A, Finfer S, Cretikos M; MERIT Study Investigators for the Simpson Centre; ANZICS Clinical Trials Group. The impact of introducing medical emergency team system on the documentations of vital signs. Resuscitation. 2009 Jan;80(1):35–43. https://doi.org/10.1016/j.resuscitation.2008.10.009
41. Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al.; The Third International Consensus Definitions for Sepsis and Septic Shock. Sepsis-3. JAMA. 2016 Feb;315(8):801–10. https://doi.org/10.1001/jama.2016.0287
42. Subbe CP, Davies RG, Williams E, Rutherford P, Gemmell L. Effect of introducing the Modified Early Warning score on clinical outcomes, cardio-pulmonary arrests and intensive care utilisation in acute medical admissions. Anaesthesia. 2003 Aug;58(8):797–802. https://doi.org/10.1046/j.1365-2044.2003.03258.x
43. Cretikos M, Chen J, Hillman K, Bellomo R, Finfer S, Flabouris A; MERIT study investigators. The objective medical emergency team activation criteria: a case-control study. Resuscitation. 2007 Apr;73(1):62–72. https://doi.org/10.1016/j.resuscitation.2006.08.020
44. Jäderling G, Bell M, Martling CR, Ekbom A, Konrad D. Limitations of medical treatment among patients attended by the rapid response team. Acta Anaesthesiol Scand. 2013 Nov;57(10):1268–74. https://doi.org/10.1111/aas.12202
45. Misch F, Messmer AS, Nickel CH, Gujan M, Graber A, Blume K, et al. Impact of observation on disposition of elderly patients presenting to emergency departments with non-specific complaints. PLoS One. 2014 May;9(5):e98097. https://doi.org/10.1371/journal.pone.0098097