Point prevalence of burnout in Switzerland: a systematic review and meta-analysis
DOI: https://doi.org/10.4414/SMW.2022.w30229
Muaamar
Al-Gobaria, Yara
Shomana, Solenne
Blanca, Irina
Guseva Canua
aCentre for Primary Care and Public Health (Unisanté), Department for Health, Work and Environment (DSTE), University of Lausanne, Epalinges, Switzerland
Summary
AIMS OF THE STUDY: To estimate the prevalence of occupational burnout among the Swiss working population.
METHODS: We interrogated three international databases (Medline (PubMed), EMBASE, and PsycINFO) and the databases of 15 Swiss universities to identify studies reporting the prevalence of occupational burnout in Swiss workers over the last 10 years, before the COVID-19 pandemic. Data were summarised descriptively and quantitatively using random-effects meta-analysis. We investigated between-study heterogeneity by stratifying results according to the type of burnout measurement tool, by occupation and by cut-off values. Three outcomes were considered: clinical/severe burnout, overall burnout and emotional exhaustion.
RESULTS: We identified 23 studies about workers in Switzerland and estimated the prevalence of clinical or severe burnout at 4% (95% confidence interval [CI] 2–6%). The average prevalence estimates for overall burnout and emotional exhaustion were similar at 18% (95% CI 12–25%) and 18% (95% CI 15–22%), respectively. When stratified by occupation, the clinical or severe burnout rates were higher among the healthcare workers than the general working population.
CONCLUSIONS: These estimates of prepandemic (baseline) prevalence of occupational burnout are comparable with those available in the other countries where it is recognised and treated as a disease. They may prove useful in planning and assessing the effectiveness of interventions for prevention of occupational burnout and in minimising its negative consequences on individuals and on societies during and after the pandemic.
Background
Occupational burnout has become one of the most discussed mental health problems in recent years [1]. However, it is unclear whether this is due to its widespread use in the media and public discourse, a misunderstanding of the term or a genuine increase in the incidence of burnout in the general working population. Currently, there are no data on the incidence of occupational burnout. The reason for this is that the estimation of incidence rates entails following a population for some time and identifying new cases of the health condition (burnout) that occur during that period [2]. In practice, it is not possible to estimate the incidence because burnout has neither a disease status nor clear and recognised diagnosis criteria. This is one of the major research gaps in the current literature and practice. The definition of occupational burnout has been harmonised only recently [3] and the lack of an official diagnosis by the World Health Organization (WHO) – albeit its appearance in the list of the International Classification of Diseases (ICD 11) [4] – may explain why only few European countries recognise burnout as an occupational or occupation-related disease [5]. In scientific papers, occupational burnout has been linked to job dissatisfaction, lower productivity and absenteeism, intentions to leave the job, increased turnover and healthcare costs, as well as other socioeconomic consequences [6–8].
Moreover, a great heterogeneity in the definition and measurement of occupational burnout [9] used in the published literature made a single-point prevalence estimate infeasible, despite an increasing number of studies reporting burnout scores and their changes over time in various occupational groups [8]. For instance, during the COVID-19 pandemic, occupational burnout has frequently been reported among frontline healthcare workers considered as particularly vulnerable to it [10, 11]. Yet other workers from the general active population can burn out as well to a similar extent [12].
Fortunately, several researchers and clinicians have been able to overcome the absence of diagnostic standards for occupational burnout and to dichotomise continuous burnout scores from some measurement tools using either statistical or clinically validated cut-off values [13–16]. Their guidance and the legitimated use of burnout score dichotomisation made it possible to estimate the prevalence of occupational burnout (and sometimes, incidence) from the reported percentage of burned-out people in different study samples. These epidemiological indicators are paramount for understanding the nature of the burnout phenomenon, estimating its magnitude and burden, deciding whether it constitutes a public health and research priority, and, if so, initiating efficient and effective interventions. Unlike Switzerland, some countries such as the Netherlands, Sweden or Belgium consider occupational burnout an established medical diagnosis related to work, which would eventually have contributed to better health policies and data availability. In general, any advocacy for national policies and efforts that aim to detect, prevent or treat clinical burnout would warrant the establishment of up-to-date data on the incidence and prevalence of this mental health outcome among the working population.
Therefore, the present study aimed at estimating the prevalence of occupational burnout in the Swiss working population based on the available data over the last 10 years. These estimates could further inform the need and the nature of interventions aimed to prevent occupational burnout in Switzerland.
Methods
We conducted a systematic review and adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [17]. The study protocol was previously registered on the international prospective register of systematic reviews (PROSPERO RecordID = 266633) [18].
Literature searches
We designed a systematic search strategy and interrogated the following databases: Medline (PubMed), EMBASE, PsycINFO, and Swiss university databases: ArODES (HES-SO), SERVAL, RERO DOC, BORIS, edoc, LORY, Université St. Gall, ZHAW digital collection, ZORA and SUPSI (see abbreviations in fig. 1). In PubMed, for instance, the search strategy comprised Medical Subject Heading Terms (MeSH) (e.g., "burnout, professional" [Mesh]), free text words (e.g., "emotional exhaust" [tiab]), Boolean terms (e.g., AND, OR) and truncations (e.g., work*) where necessary. In EMBASE, we used EMTREE terms, free text words, Boolean terms, proximity operators (e.g., near/n), and truncations where necessary (see appendix). Besides electronic searches, we manually searched references lists of identified studies, and used the google search engine as well as the Google scholar platform to identify additional eligible studies. We focused our search strategy on the period 2010–2021 in order to consider the most recent, but sufficiently numerous and methodologically robust, studies for providing useful and relevant estimates of the current prevalence of occupational burnout. As the first estimates related to occupational burnout (namely emotional exhaustion) in the general Swiss population have been reported only since 2012 [19], we interrogated the databases from January 2010 to 6 July 2021.
Eligibility of studies
Studies were included if they measured the prevalence of occupational burnout in Swiss workers of any occupation. In our study, we defined the prevalence as the proportion of persons identified as burned-out among the study population. We only included studies that reported such a proportion or provided data enabling its calculation. We excluded studies that failed to report cut-off scores to estimate occupational burnout prevalence in patient-reported outcome measures. Additionally, we excluded systematic reviews after screening their reference lists to identify any additional primary studies. We applied no limitation with respect to study design or publication language, considering three languages officially used in Switzerland (German, French, and Italian) as well as English.
Data abstraction and synthesis
Three reviewers (MA, SB and IGC) were involved in the inclusion of studies and the extraction of the data in a standardised form such that one verified the work of the other intrinsically. One author (IGC) solved any discrepancies in the process of study inclusion. We extracted key characteristics from the studies included, such as study design, type of population, occupational group, sample size, age, gender, work experience (in years) and burnout measuring tools/instruments along with their cut-off scores.
Definitions of the outcomes
Given the high heterogeneity in the measurement of occupational burnout, we attempted to reduce it by grouping the studies using the same measurement methods and cut-off values. For this, we reviewed the construct definition, the measurement method and the cut-off values of burnout severity in each of the included studies and classified them according to the commonality of the outcome measured. This strategy enabled us to consider all homogeneously defined outcomes individually and estimate their respective prevalence.
Quality appraisal (risk of bias)
One author assessed the risk of bias of the included studies while a co-author randomly double-checked the quality appraisal of at least 20%, with any discrepancies being resolved via discussion, and the involvement of a third reviewer when necessary. We assessed the risk of bias using the Methodological Evaluation of Observational Research (MORE) for incidence and prevalence studies [20]. This tool allows appraisal of the quality and reporting of prevalence studies by rating three domains: general (e.g., funding and conflict of interest), external validity, and internal validity. Each item in each domain was rated as low, unclear or high. Finally, each study was rated as having either low, unclear or high risk of bias, based on the overall judgment of the three aforementioned domains. More specifically, we decided to rate the overall quality of included studies as unclear if at least one domain was rated unclear and the other domains were rated low or unclear. If a study had a high risk of bias for any of the three domains, the overall quality was finally judged as high risk of bias. In comparison, studies with low rating on the three domains, the overall quality was finally judged as low risk of bias.
Statistical analysis
We meta-analysed the prevalence data and assessed the statistical between-study heterogeneity using the chi-square test and I-square statistic, using a random-effects model. In our random-effects model, we used the method of DerSimonian and Laird, with the estimate of heterogeneity being taken from the inverse-variance fixed-effect model [21]. To understand the sources of heterogeneity and reduce it, we further produced the prevalence estimates of each outcome stratified by occupational groups. We considered a p-value of ≤0.10 (instead of the conventional 0.05) to indicate statistically significant heterogeneity as recommended by the Cochrane handbook [22]. We analysed data with STATA version 16.1 (StataCorp LP, Texas).
Missing data
We did not impute missing outcomes when they were missing in the retrieved papers. Instead, we contacted their respective corresponding authors during our study to obtain the missing data. In the case of non-response, we did not consider those studies for further analyses and excluded them from our systematic review.
Results
Study selection
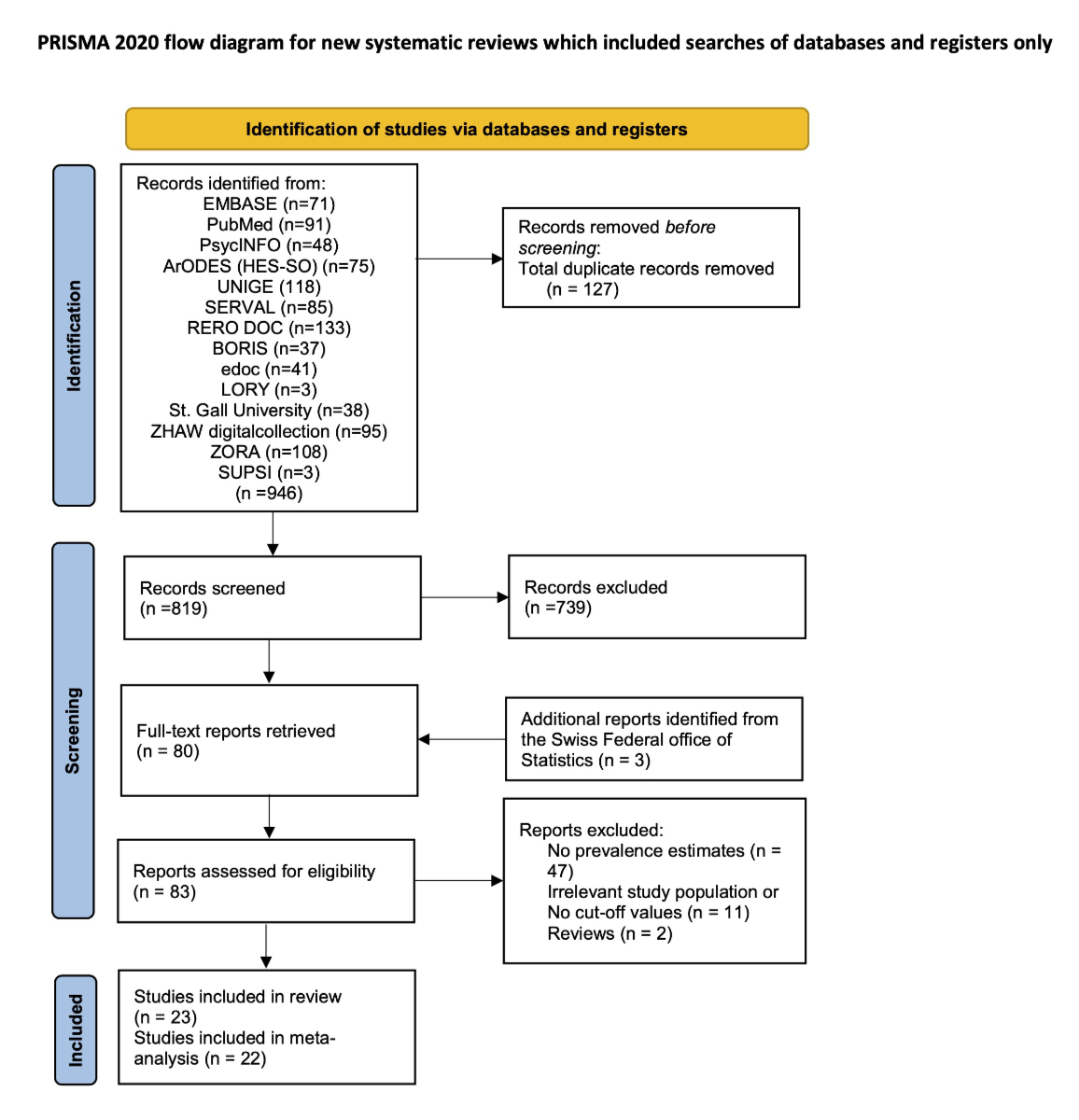
From electronic searches of databases, we identified and screened 819 potentially relevant unique records after the removal of duplicates. Of those, 80 records were assessed at a full-text level against inclusion criteria of which 60 were excluded for various reasons (e.g., no prevalence estimates or irrelevant study population, or no cut-off values) (fig. 1).
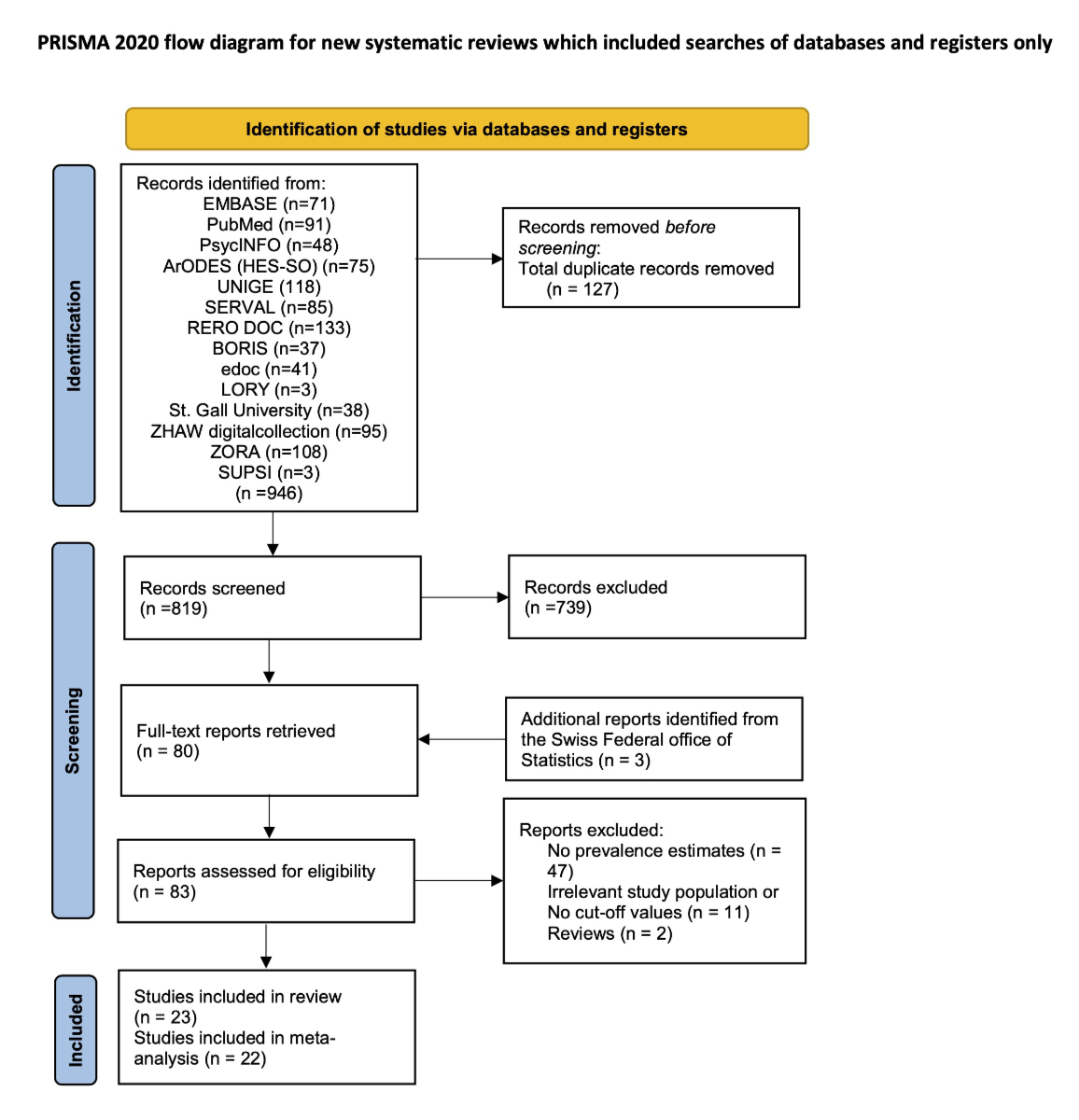
Figure 1 Flowchart of included studies.
ArODES (HES-SO): Archive ouverte des HES de Suisse occidentale; SERVAL: Serveur académique lausannois; RERO DOC: Dépôt institutionnel des institutions membres de RERO; BORIS: Bern Open Repository and Information System; edoc: Institutional Repository University of Basel; LORY: Lucerne Open Repository; Université St. Gall: Plateforme de recherche Alexandria; ZORA: Zurich Open Repository and Archive; SUPSI: La Scuola universitaria professionale della Svizzera italiana
Thereafter, we identified a further three studies by hand searching and from the screening of the reference list of the eligible articles. Eventually, we included 23 studies [19, 23–44] of which 22 [19, 23, 25–44] were in a meta-analysis.
Characteristics of included studies
As shown in table 1, all studies but one [40] used a cross-sectional design where the prevalence of occupational burnout was measured at least once at a specific time.
Table 1Main characteristics of included studies.
|
Study ID
|
Region/Canton
|
Study design
|
Sample size (n); population
|
Mean age (years)
|
Women (%)
|
Baseline prevalence rates (%)
|
Mean work experience (years)
|
Risk of bias assessment
|
| Arigoni 2010 |
French-speaking; German- and Italian-speaking |
Cross-sectional |
In 2002: 1755; in 2004: 365; in 2007: 615; cancer physicians, paediatricians, internal medicine specialists, GPs |
NR |
29.9 |
Severe: in 2002: 3.5; in 2004: 6.3; in 2007: 3.7 |
11 (65% in the year 2004) |
Unclear |
| Businger 2010 |
German-speaking |
Cross-sectional |
405; surgical residents and surgeons |
Surgical residents, median 31; surgeons, median 46 |
23.7 |
EE: 12.6, DP: 29.9; PA: 21.7; Severe: 3.7 |
~7 |
High |
| Divaris 2012 |
German-speaking |
Cross-sectional |
36, dental residents |
30 |
51 |
EE: 17; DP: 8; PA: 36 |
~4 |
Unclear |
| Favrod 2018 |
NR |
Cross-sectional |
213; midwives and (neonatal intensive care) nurses |
18 – >40 (range) |
~93.7 |
EE: 21.4; DP: 6.0; PA: 3.6; severeb, nurses: 4.8, Mmdwives: 0.00 |
≤10 (54.9% for nurses; 39.3% for midwives) |
Low |
| FSO 2019 |
French-speaking; German- and Italian-speaking |
Cross-sectional |
11,318; Swiss workers |
15–64 (range) |
49.6 |
20 |
NR |
Unclear |
| FSO 2014 |
French-speaking; German- and Italian-speaking |
Cross-sectional |
11,157; Swiss workers |
15–64 (range) |
48.4 |
Male: 18; female: 20 |
NR |
Unclear |
| Gerber 2019 |
German-speaking |
Cross-sectional |
309; Swiss workers |
42.66 (SD 14.18) |
48 |
EE: 1.8; physical exhaustion: 2.72; cognitive weariness: 2.43; overall: 2.42 |
21.64 |
High |
| Hämmig 2018 |
German-speaking |
Cross-sectional |
1840; hospital employees, physicians, nurses |
<45 (58%) |
88 |
8.2 |
NR |
Unclear |
| Hämmig 2014 |
German-speaking |
Cross-sectional |
2014; industrial workers |
16–69 (range) |
18 |
Men: 6; women: 10 |
NR |
Low |
| Hämmig 2012 |
German-speaking |
Cross-sectional |
456; hospital employees |
NR |
77.8 |
16.9 |
NR |
Unclear |
| Heeb 2014 |
Western Switzerland |
Cross-sectional |
449, nursing (57.23%) and medical mangers (42.76%) |
46.7 |
58 |
Nursing managers: EE: 10.9; DP: 16.7; PA: 28.4; Severeb: 2.3 |
16 (63.8)% |
Low |
| Medical managers: EE: 12.5; DP: 19.3; PA: 38.0; Severeb: 3.1 |
| Kind 2020 |
German-speaking |
Longitudinal |
159 ; professional caregivers in youth residential care |
35.85 (SD 9.68) |
57.9 |
36.7 |
8.3 |
High |
| Lindemann 2019 |
German-speaking (91.5%) |
Cross-sectional |
523; medical students, residents, GPs |
33.6 (SD 5.7) |
75.1 |
14.9 |
NR |
Unclear |
| Merlani 2011* |
French-,German- andItalian-speaking |
Cross-sectional |
2987; nurse assistants, nurses, physicians |
<40 (70%) |
76 |
EE: 2.93; severe: 29 |
Median: 7.5 |
Low |
| Nguyen Huynh 2021 |
French-speaking |
Cross-sectional |
Mean: 558.6**; patients |
NR |
NR |
3.02**
|
NR |
Unclear |
| Nicolin 2018 |
French-speaking |
Cross-sectional |
90; specialised teachers |
41.5 (range 24–61) |
81 |
EE 15.6; DP 3.3; PA 31.1 |
12 |
Low |
| Reissig 2019 |
French-,German-, and Italian-speaking |
Cross-sectional |
1321; farmers |
49 |
23.9 |
12 |
NR |
Low |
| SECO 2017 |
French-,German-, and Italian-speaking |
Cross-sectional |
871; Swiss workers |
15–65 |
49.8 |
35.2 |
NR |
Unclear |
| Squillaci 2020 |
French-speaking |
Cross-sectional |
345; special education teachers |
31–40 (range) |
>80 |
EE 7.2; DP 1.2; PA 23.6 |
NR |
Unclear |
| Steinlin 2017 |
German-speaking |
Cross-sectional |
319; social education workers or trainees |
36.6 (SD 10.0) |
61 |
18 |
10 (SD 8.2) |
Low |
| Studer 2017 |
French-speaking |
Cross-sectional |
5519; teachers |
31–60 (85.4%) |
76.2 |
Personal burnout; work-related burnout; client-related burnout: 42.4; 22.5; 26 |
≥6 (87.4%) |
Unclear |
| Welp 2019 |
German-speaking |
Cross-sectional |
1496; nurses, physicians |
39.6 (SD 9.4) |
69.6 |
EE 37.8; DP 35.8; PA 27.2; overall severeb: 11.8 |
12.6 (SD 8.9) |
Low |
| Zumbrunn 2020 |
German-speaking |
Cross-sectional |
450; general internal medicine residents |
Median 30 |
61 |
EE 60; DP 47; EE + DP 32 |
|
Low |
The sample size of included studies ranged from 36 to 11318 Swiss workers with a median of 523. The female workers ranged from 18% to 93.7%. Eight different measures were used to assess burnout prevalence among the participants in the primary studies: nine used Maslach Burnout Inventory (MBI), five used Copenhagen Burnout Inventory (CBI), three used Emotional exhaustion (EE), two used the Burnout Screening Scale (BOSS), one each used the medical diagnosis, Shirom-Melamed Burnout Measure (SMBM), Physician Well-Being Index (PWBI), and a single-item scale. Ten studies reported on physicians, residents, dentists, medical students, nurses, midwives, medical managers and hospital employees while the remaining studies were conducted on other subpopulations such as education and social workers (4 studies), industrial workers, farmers, or the general population.
Burnout outcomes
As shown in table 2, three outcomes, namely clinical/severe burnout, overall burnout, and emotional exhaustion, were considered in our analysis.
Table 2Burnout outcome definitions: measures and cutoffs.
|
Outcomes
|
Frequency
|
References
|
| I. Clinical/severe burnout |
Clinical burnout diagnosed by physicians |
1 |
Nguyen Huynh 2021 |
| High/severe burnout measured by MBI-HSS |
Statistical cutoffs based on American normative sample |
EE ≥27 (10 items) AND DP ≥10 (5 items) AND PA ≤33 (7 items) |
1 |
Arigoni 2010 |
| EE ≥27 (9 items) AND DP ≥10 (5 items) AND PA ≤33 (8 items) |
2 |
Businger 2010; Heeb 2014 |
| EE ≥27 (9 items) AND DP ≥13 (5 items) AND PA ≤33 (8 items) |
2 |
Divaris 2012; Welp 2019 |
| Statistical cutoffs based on French normative sample |
EE ≥30 (9 items) AND DP ≥12 (5 items) AND PA ≤33 (8 items) |
3 |
Favrod 2018; Nicolin 2018; Squillaci 2020 |
| Clinical/severe burnout according to SMBM |
|
|
| Physical fatigue (6 items) AND emotional exhaustion (5 items) AND cognitive weariness (5 items); ≥4.4 |
1 |
Gerber 2019 |
| II. Overall burnout |
Overall burnout according to CBI |
Personal burnout ≥50 (3 items) OR ork-related burnout ≥50 (3 items) OR client-related burnout ≥50 (3 items) |
1 |
Hämmig 2012 |
| Personal burnout ≥16 (6 items) |
2 |
Hämmig 2014; Hämmig 2018 |
| Personal burnout (often Or always to ≥4 questions, 6 items) |
1 |
Reissig 2019 |
| Personal burnout ≥50 (6 items) OR work-related burnout ≥50 (7 items) OR client-related burnout ≥50 (6 items) |
1 |
Studer 2017 |
| Overall burnout according to BOSS |
Work-related burnout ≥60 (10 items) |
2 |
Kind 2020; Steinlin 2017 |
| Overall Burnout according to PWBI |
|
|
| Work-related burnout (yes/no, 1 item) AND emotional hardening (yes/no, 1 item ) |
1 |
Zumbrunn 2020 |
| III. Emotional Exhaustion (EE)
|
FSO (rather yes OR yes, 1 item) |
2 |
FSO 2019; FSO 2014 |
| SECO ( often OR always, 1 item) |
1 |
SECO 2017 |
| Single-item scale ≥3 |
1 |
Lindemann 2019 |
| MBI-HSS |
EE ≥27 (10 items); American normative sample |
1 |
Arigoni 2010 |
| MBI-HSS |
EE ≥27 (9 items) |
4 |
Businger 2010; Divaris 2012; Heeb 2014; Welp 2019 |
| MBI-HSS |
EE ≥30 (9 items)); French normative sample |
3 |
Favrod 2018; Nicolin 2018; Squillaci 2020 |
| Emotional hardening (PWBI) ( yes/no, 1 item) |
1 |
Zumbrunn 2020 |
A burnout was considered as clinical or severe when the cut-off values of the three dimensions (emotional exhaustion, depersonalisation and low personal accomplishment) of the Maslach Burnout Inventory (MBI) were met. The diagnosis of burnout cases by physicians was also considered clinical. A burnout was classified as “overall burnout” if the clinical stage or severity of the syndrome were not specified or if the measurement tool used had not allowed its clinical stage or severity to be determined.
Finally, emotional exhaustion was a third possible outcome. emotional exhaustion was measured and reported either as a separate outcome based on the question of how often the person feels emotionally exhausted at work or as a dimension of a more complex measure, most often the MBI. In our study, we considered both options and analysed them as one outcome.
In summary, three types of outcomes were considered: clinical/severe burnout, overall burnout, and emotional exhaustion.
Only one study [45] reported clinical burnout prevalence assessed by physicians. Among the eight studies that used the MBI, five reported the burnout level as high or severe where authors used a combination of high emotional exhaustion, high depersonalisation, and low personal accomplishment. The remaining three studies analysed the three dimensions of the MBI separately. Five studies used the statistical cut-offs based on the American normative sample and three studies used the statistical cut-offs based on the French normative sample (table 2).
Regarding the use of the CBI, the studies either used selected items related to personal burnout, work-related burnout and client-related burnout, or used exclusively one subscale (e.g., personal burnout).
For those that measured the emotional exhaustion, four studies used a one-item Likert-type scale, nine used a dimension of the MBI and one used a single item (yes/no) scale.
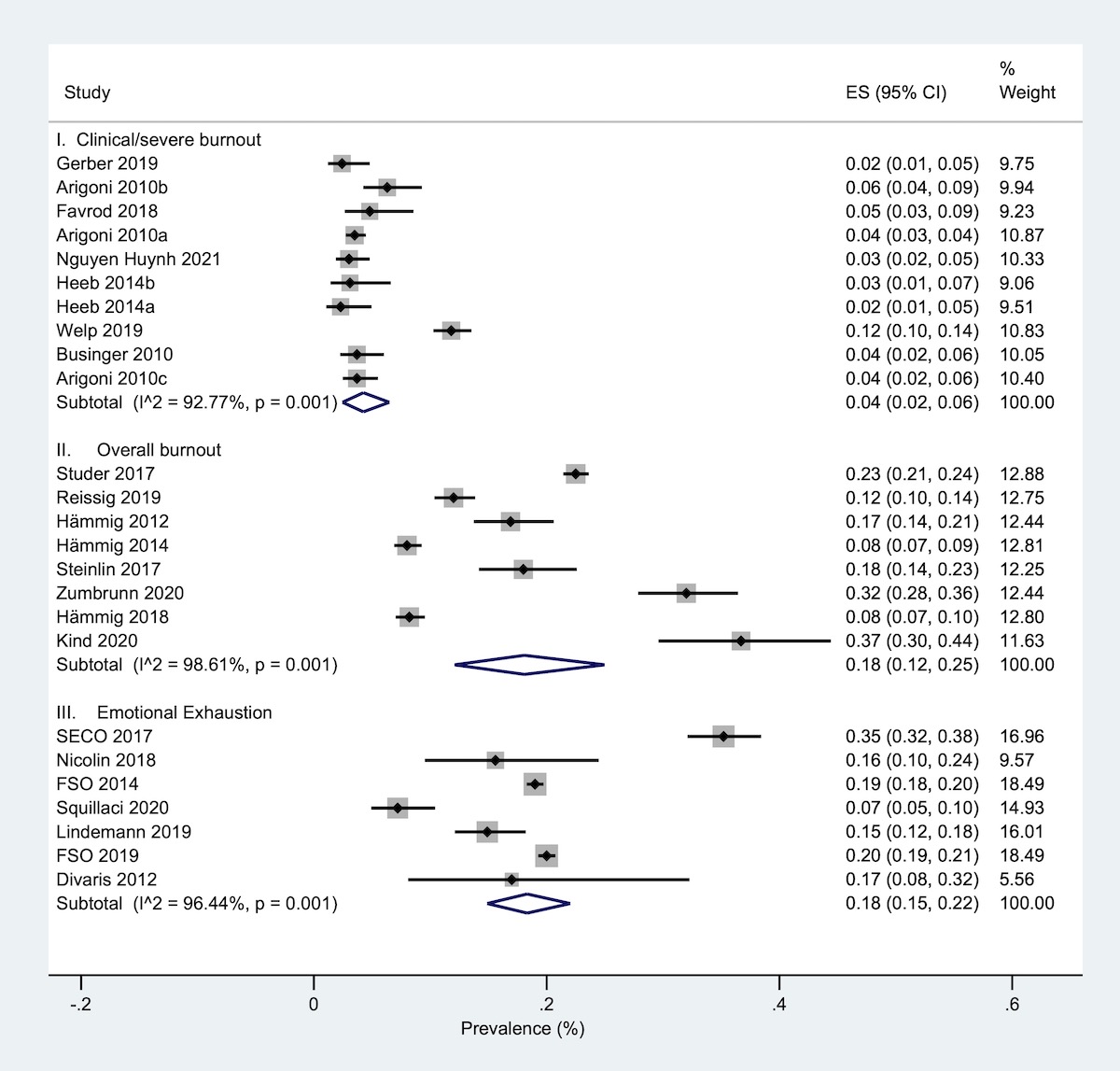
Prevalence of burnout among Swiss workers
Overall, we included 22 studies in our quantitative synthesis. One study [24] was not included in the meta-analysis because of unclear cut-off values. Prevalence of burnout among included studies varied from one population to another and by occupation or work setting. Regardless of the occupation, clinical/severe burnout was estimated at 4% (95% confidence interval [95 CI] 2–6%) and overall burnout or emotional exhaustion were relatively similar at 18% (95% CI 12–25%) and 18% (95% CI 15–22%), respectively (fig. 2).
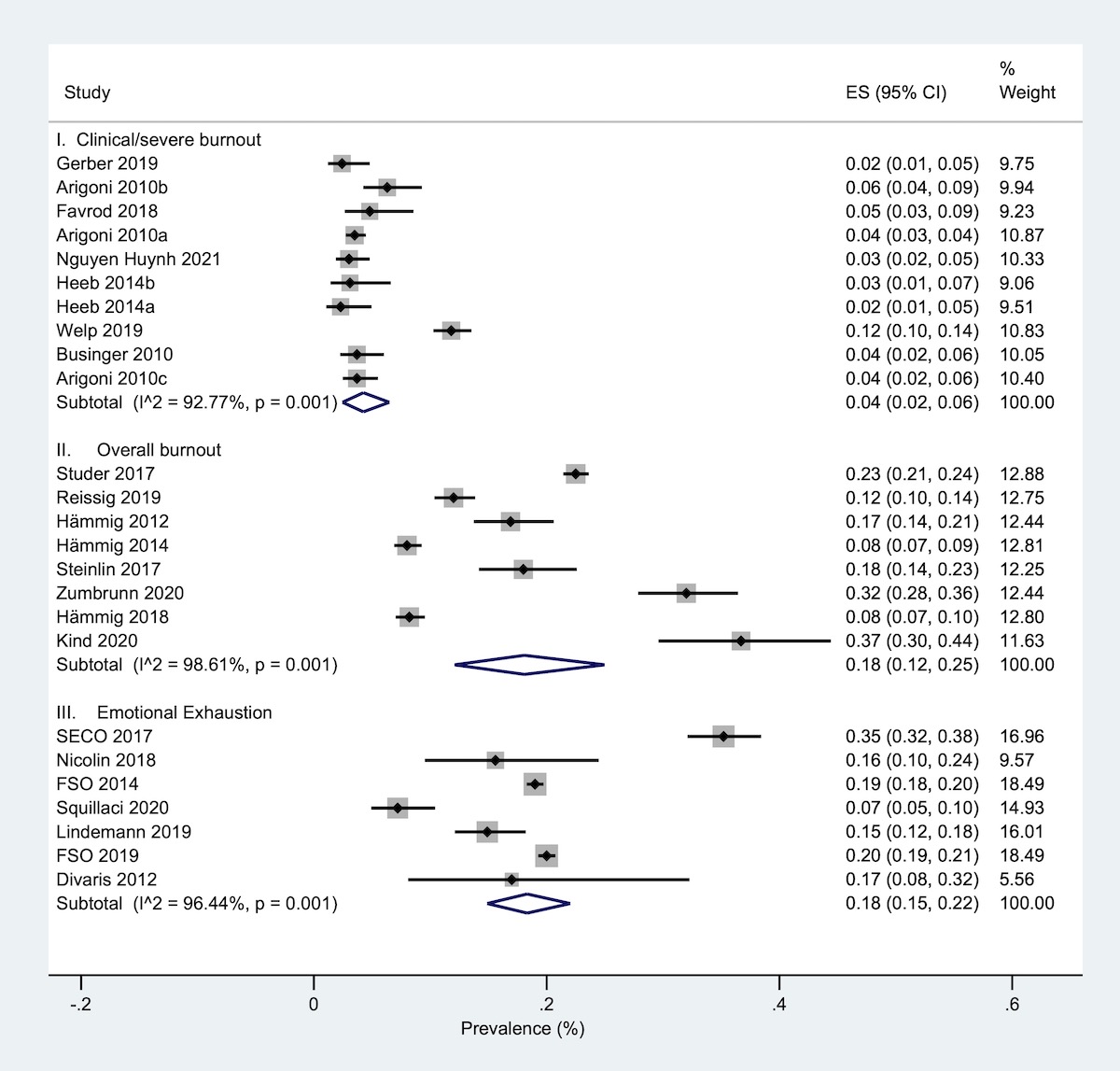
Figure 2 Prevalence of burnout stratified by burnout ouctomes in any occupation.
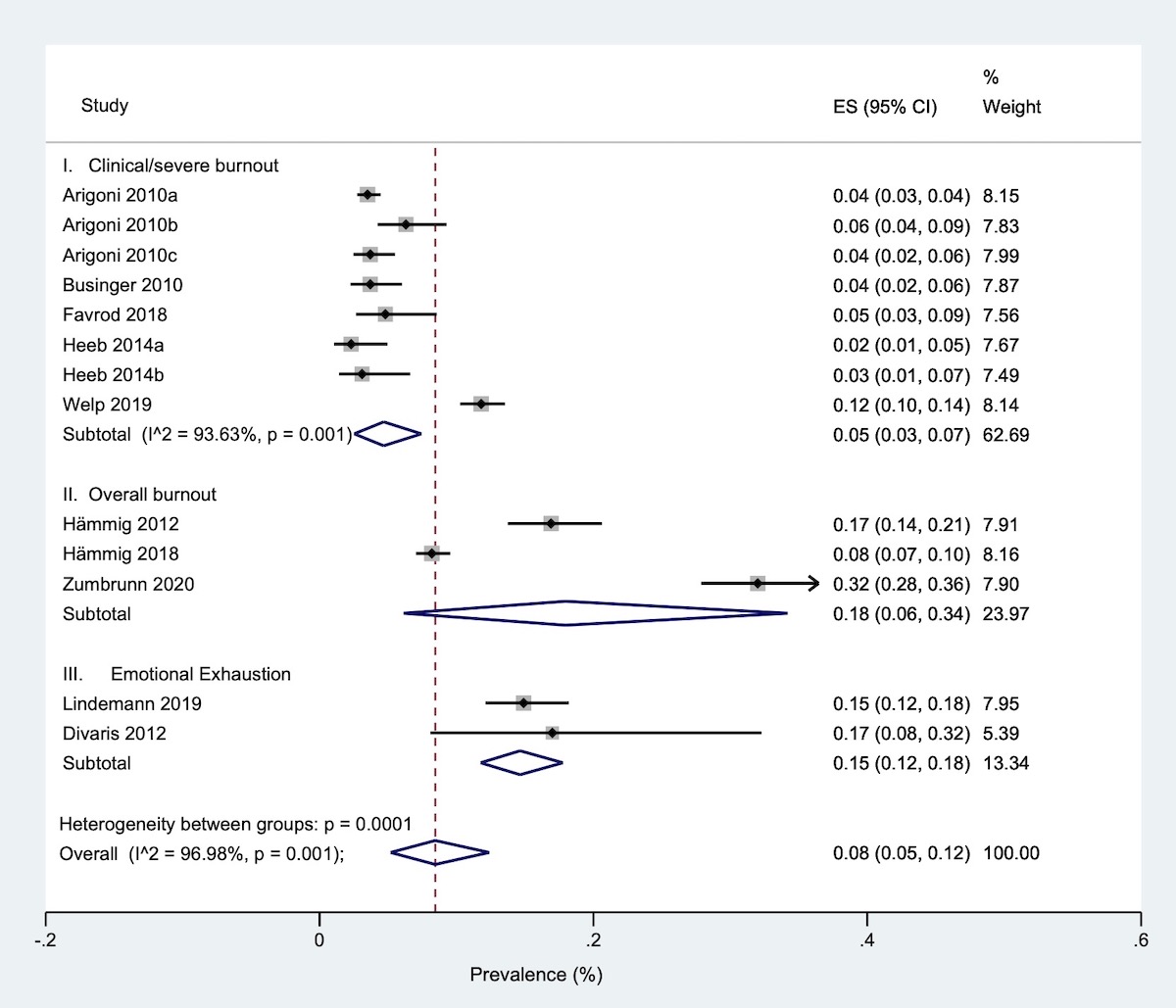
When stratified by occupation, healthcare workers (e.g., physicians, general practitioners, residents, dentists or hospital managers) had rates of severe burnout, overall burnout or emotional exhaustion estimated at 5% (95% CI 3–7%), 18% (95% CI 6–34%) and 15% (95% CI 12–18%), respectively (fig. 3).
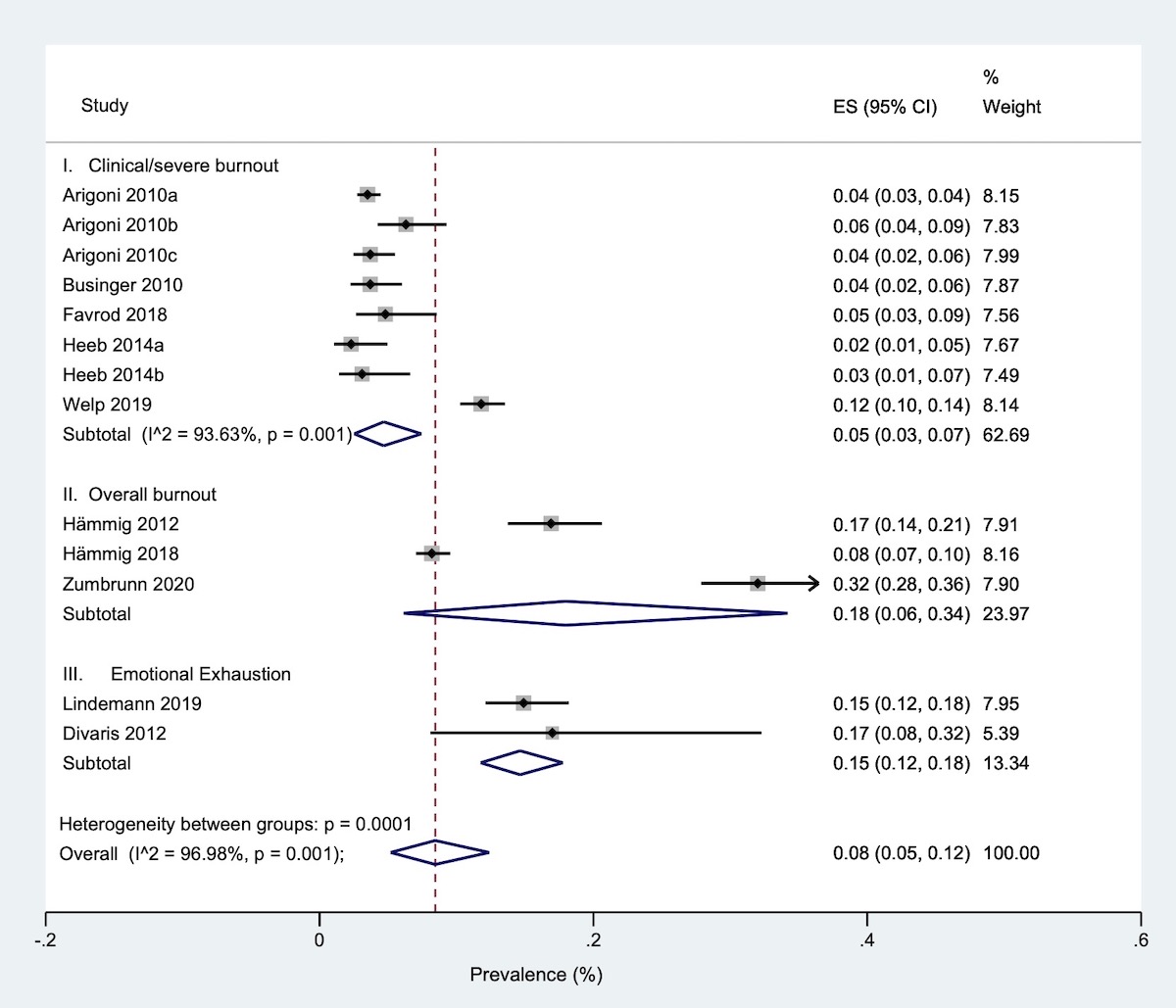
Figure 3 Prevalence of burnout in healthcare workers.
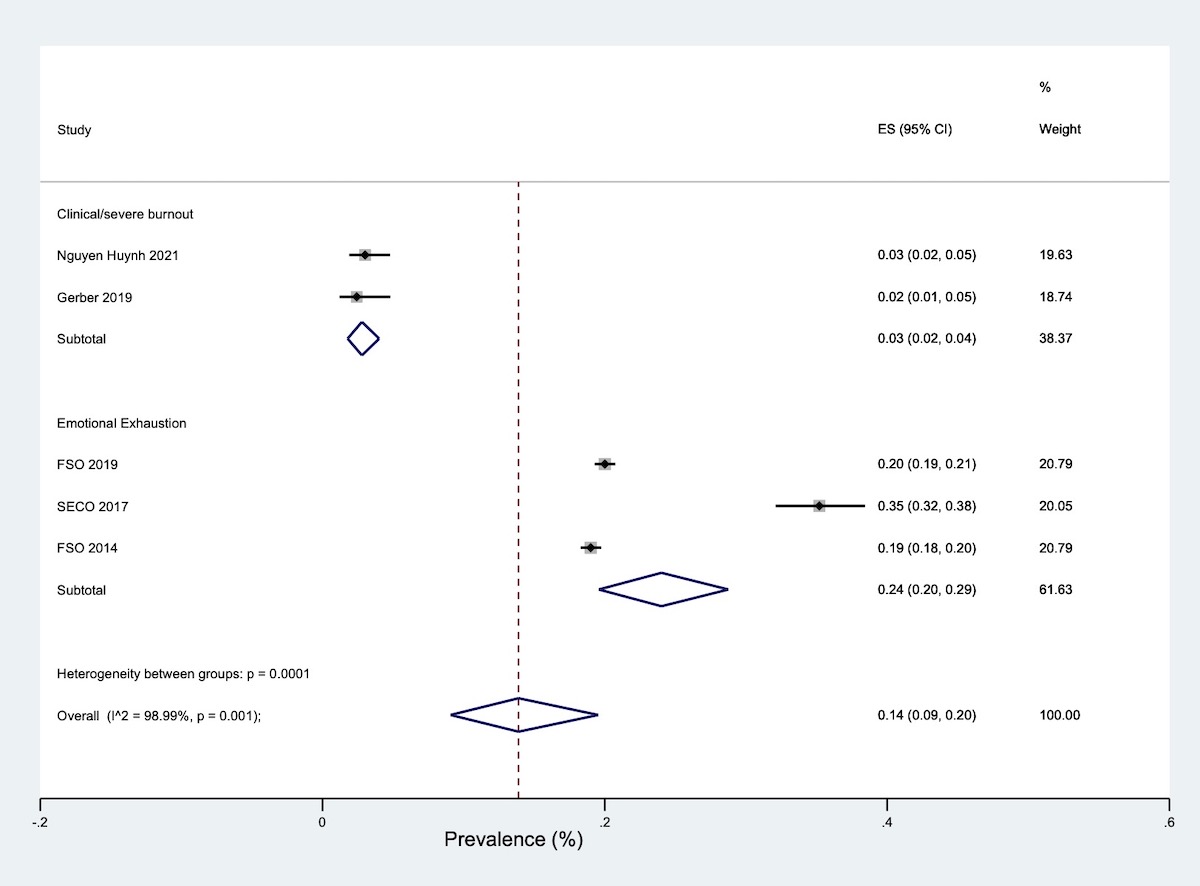
In the general working population, clinical or severe burnout and emotional exhaustion rates were estimated at 3% (95% CI 2–4%) and 24% (95% CI 20–29%), respectively (fig. 4).
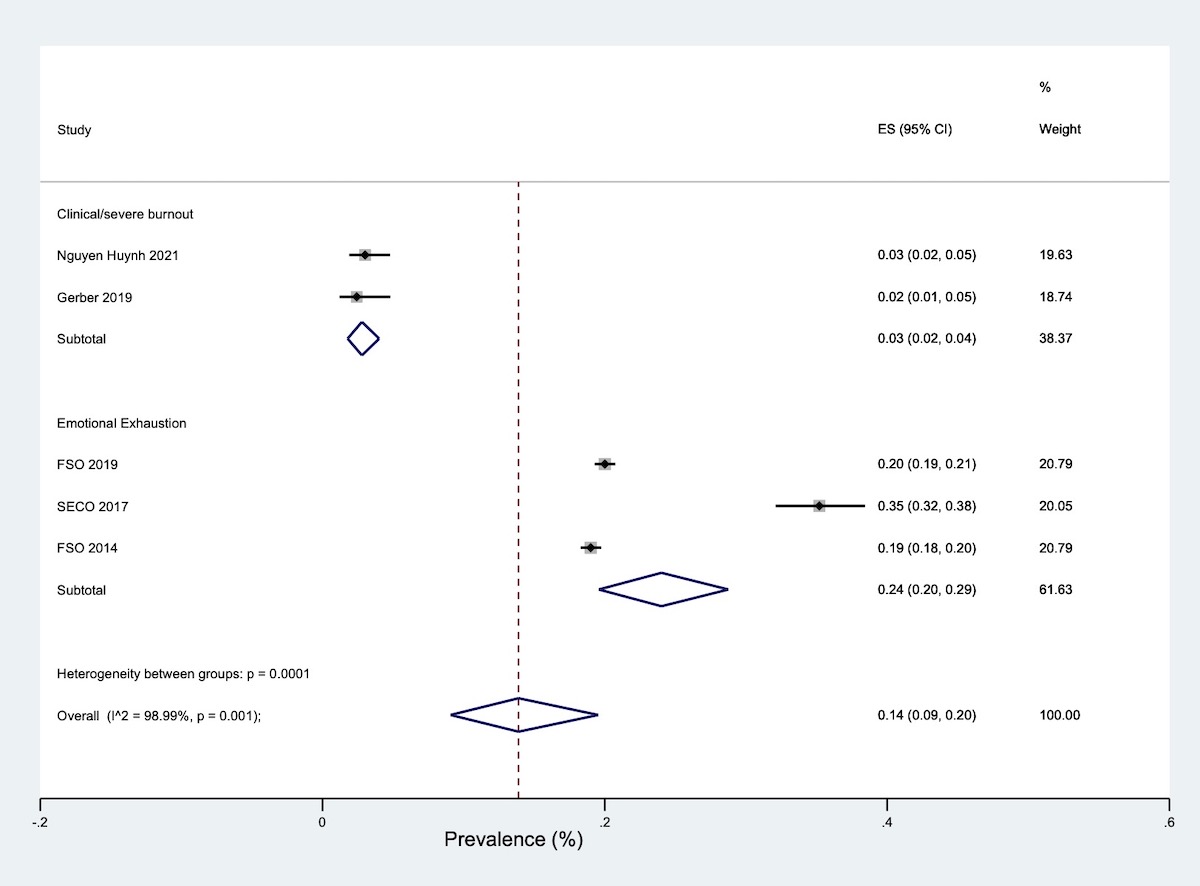
Figure 4 Prevalence of burnout in the general working population.
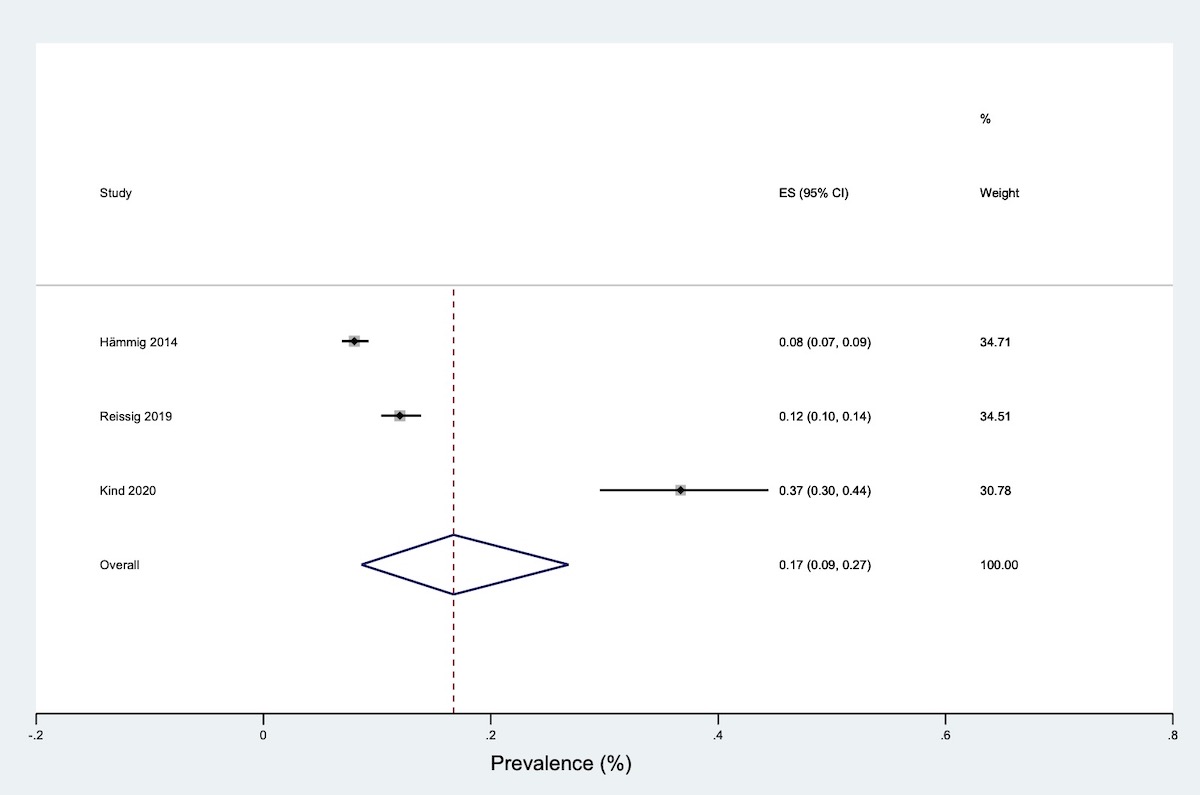
In education workers, overall burnout and emotional exhaustion were estimated at 22% (95% CI 21–23%) and 9% (95% CI 6–11%), respectively (fig. 5).Overall burnout was estimated at 17% (95% CI 9–27%) in other workers (industrial workers, farmers and residential youth caregivers) (fig. 6).
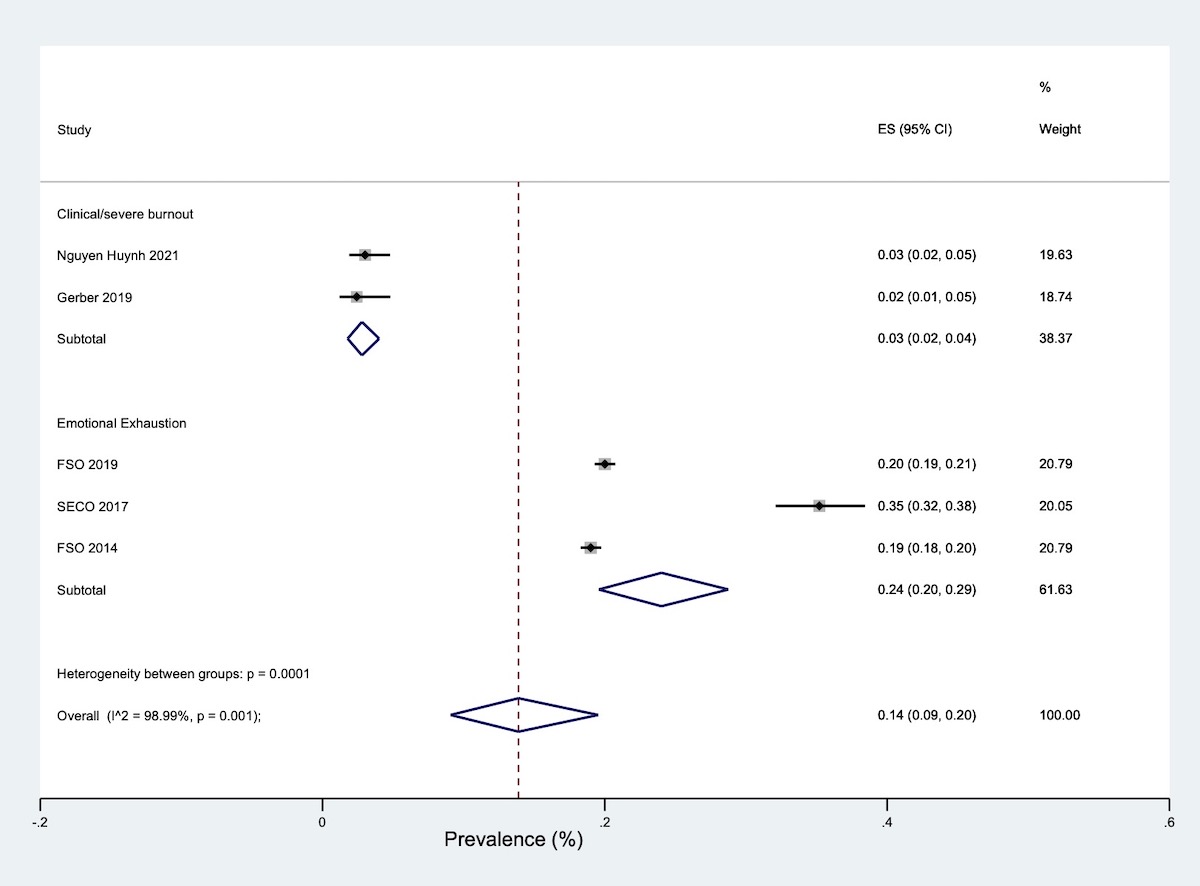
Figure 5 Prevalence of burnout among workers in the education sector.
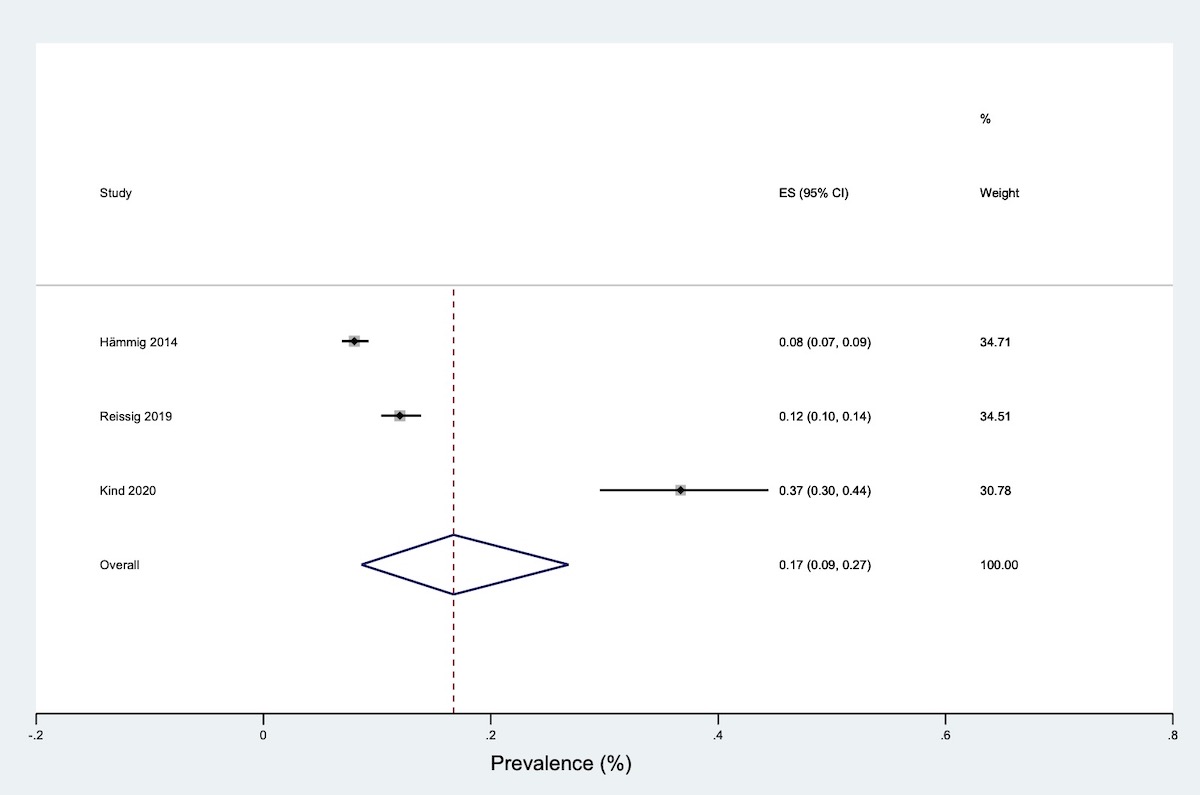
Figure 6 Prevalence of burnout among other workers.
We also provided the burnout prevalence rates per scale or measurement tool (figure S1 in the appendix).
Between-study heterogeneity was considerable (I-square >90%, p <0.001) for all outcomes and across the studied populations (e.g., healthcare workers or the general working population). In subgroup analyses, heterogeneity was not estimated in the analysis – owing to power issues – except for severe or clinical burnout in healthcare workers (I-square = 92.63, p <0.001).
Risk of bias assessment
Based on MORE risk-of-bias assessment [20], all studies had low risk of bias in general reporting and most of the studies had low risk of bias in external validity. Eleven studies had unclear risk of bias in internal validity mainly due to the reliability of the estimates and the validation of outcome measurement tools. Overall, 9 studies [24, 27, 28, 31–33, 36, 42, 44] were at low risk of bias, 10 studies [23, 25, 26, 29, 35, 37, 38, 41, 43, 45] had unclear risk of bias and four [23, 30, 34, 40] were at high risk of bias (table 1 and table S1 in the appendix). Based on a visual assessment of the funnel plot, we considered that the likelihood for publication bias was low (figure S2 in the appendix).
Discussion
This study aimed to estimate the prevalence of occupational burnout in the Swiss population and searched for primary studies that were published in 2010 and later. We identified 23 studies that assessed the prevalence of burnout among workers in Switzerland. Regardless of occupation, our meta-analysis estimated a prevalence of clinical/severe burnout of 4% and overall burnout or emotional exhaustion prevalences were of 18%. Interestingly, the prevalence of emotional exhaustion was assessed at 20% between 2012 and 2017 in a large representative study of Swiss workers [19]. Although emotional exhaustion is a core dimension of burnout, our results suggest that this dimension is not sufficient to constitute burnout. This is consistent with the harmonised definition of occupational burnout [3]. Therefore, the estimates of emotional exhaustion overestimate the prevalence of clinical burnout. Indeed, clinical/severe burnout estimation of 4% seems robust enough and equates to the proportion of burnout cases that were diagnosed in clinical practice in the cantonal polyclinics in Western Switzerland [45].
In the international literature, a systematic review aimed to evaluate burnout prevalence reported a range of 0 to 80.5% among physicians in 45 countries [8].
In our study, the prevalence of clinical/severe burnout was 5% in healthcare workers compared with 3%–4% in the general working population. Such a high estimate may be explained by the fact that working in a particularly stressful and emotionally demanding setting (e.g., clinics, hospitals) constitutes an independent risk factor for occupational burnout [46, 47]. In addition, our estimate of clinical or severe burnout prevalence is also congruent with findings in several European countries. For example, in Denmark, a 7-year follow-up study reported an incidence rate for moderate or severe burnout of 13.2% and a prevalence rate of 5.3% among general practitioners [48, 49]. In the Netherlands, the prevalence estimate of clinical or severe burnout based on the Dutch clinically valid cut-off values ranged between 4% and 7% of the working population. In some occupations, a 10% prevalence was reported, but the representativeness of the data was not ensured [50]. Kant et al. reported a prevalence estimate of 13.7% in a relatively large Dutch cohort [51]. The burnout definition was based on the MBI for General Services with high scores of exhaustion and either high scores of cynicism or low scores of professional efficacy. This may have overestimated clinical or severe burnout and should instead be considered as an overall burnout, with a prevalence estimate similar to ours. In Germany, 4.2% (women 5.2%, men 3.3%) of the general working population self-reported a lifetime prevalence of a diagnosed burnout by a physician or psychotherapist and many of them had a current mental disorder [52]. In Belgium, 7.14% of long-term disabled persons, who were unable to work or return to work, suffered from burnout and 17% suffered from depression with an increase of 32.53% for burnout cases between 2016 and 2020 [53].
In addition to depression, occupational burnout has been linked to other mental health problems and symptoms such as anxiety, anger, feelings of helplessness [54], cognitive functions or impaired sleep [55]. Moreover, a modelling study suggested that depression might be an outcome of occupational burnout rather than a precursor [56]. However, a recent systematic review that investigated the relationship between depression, anxiety and burnout concluded that there is no evidence of overlap and that they seem to have robust constructs [57]. Other authors disagree, believing that "depressive and burnout symptoms often co-occur and develop in tandem," and include depressive mood as a secondary dimension of burnout [58].
In terms of health economics, the costs related to work-related stress (e.g., healthcare utilisation, work interruption, early retirement, sickness leave or early mortality) are estimated at several billion euros in Switzerland, Germany, the Netherlands, France or the United Kingdom according to the statistics from the European Agency for Safety and Health at Work [59]. More precisely, according to a report about costs of stress in Switzerland, the related prescribed medical costs may exceed 2 billion Swiss francs, which represents approximately 7% of the costs of the Swiss health system for medical costs prescribed by health professionals [60]. Given such negative and costly consequences, addressing occupational burnout and its predictors [61] would have social, economic and mental health benefits.
It is noteworthy to clarify that “point” prevalence refers to the prevalence measured at a particular point in time compared to “period” prevalence where the measures are taken over an interval of time. All studies included in our systematic review estimated point prevalence. Given these results, we did not find it useful to consider this issue in a subgroup analysis or a meta-regression. We did not identify other study characteristic that would have explained the observed heterogeneity by a meta-regression. Moreover, it is important to state that although the between-study heterogeneity in our study was considerable, I2 or I-square can be imprecise and biased in small meta-analyses [62].
Strengths and limitations
By applying a rigorous assessment of the methods of occupational burnout measurement, our systematic review/meta-analysis is the first to provide the prevalence estimate for occupational burnout in the Swiss working population. This study enabled us to distinguish between clinical or severe burnout, overall (unspecified) burnout, and its proxy and core dimension, emotional exhaustion, as three distinct outcomes. The estimated prevalence of clinical/severe burnout is consistent with prevalence estimates reported in the European countries where occupational burnout is recognised as a disease. The study findings are rather alarming and shed light on the importance of addressing such a prevalent mental disorder in the workplace.
Our literature search was conducted up to July 2021, when only a few studies had assessed and published burnout prevalence estimates during the COVID-19 pandemic period. None of these studies was conducted in Switzerland. Therefore, our estimates reflect the prepandemic, baseline, prevalence of burnout. They should enable comparisons with the estimates from studies conducted during the pandemic period and the assessment of the pandemic’s impact on mental health, which we believe is very important [63, 64]. Our estimates could be also helpful in assessing the effectiveness of interventions for mental health promotion during the pandemic and postpandemic periods [65].
In our search of the literature, we were able to identify only one study in which physicians reported the number of burned-out patients in their consultations [45]. This was one of the most recent studies included in our review, and in contrast to all other included studies, it was conducted after the release of the harmonised definition of burnout [3], presented by the study's authors to the participating physicians before data collection. Having more studies based on standardised criteria of clinical burnout assessment would increase the quality of the meta-estimates and facilitate straightforward comparisons of prevalence rates between countries where occupational burnout is recognised and treated as a disease.
In this meta-analysis, we observed a considerable heterogeneity of our combined estimates of occupational burnout. This was due to known disagreements in the definition of burnout [3, 13], validity concerns of patient-reported burnout measures [9], and a variety of clinical and non-clinical work settings and occupation types besides regional and linguistic or cross-cultural issues. Having this in mind, we used a random-effects model to run the meta-analysis and judged that the existing heterogeneity is expected given the aforementioned factors and the fact that a high value of I2 – used here to measure heterogeneity – could be interpreted as substantial but also as a trivial level of heterogeneity or being clinically unimportant [22].
Our overall study sample size was large enough and representative of the Swiss working population although limited by the heterogeneity of burnout measures used and the absence of Swiss clinically valid cut-off values. This latter issue should be addressed in future studies. Finally, there were a few included studies in specific occupations that resulted in rough prevalence estimates and should be interpreted with caution.
Implications and conclusions
Clinicians and researchers will need to continue identifying patients with occupational burnout. Newly developed screening and diagnostic tools, once validated, will be helpful in the further screening and diagnosis of patients with this mental disorder as soon as possible. In conclusion, our systematic review and meta-analysis showed that the prepandemic prevalence of occupational burnout in the Swiss working population is comparable to that in other countries where prevalence estimates for occupational burnout are available. As our estimates correspond to the baseline prevalence of occupational burnout, they should be helpful in the assessment of the effectiveness of interventions for mental health promotion during the pandemic and postpandemic periods. As the COVID-19 pandemic had a disastrous impact on all mental health outcomes, including burnout, more efforts to detect it earlier are necessary to reduce its negative consequences on an individual and societal level.
Data sharing statement
All data are available in the manuscript and its supported files. Any more information can be requested from the corresponding author.
Acknowledgements
The authors would like to acknowledge the contribution of Mr. Thomas Brauchli (Librarian, Unisanté) and Mr. Olivier Talpain in the search and selection of studies and other related tasks during the early stages of this systematic review. In addition, we thank Ms. Julia Banerjee for proofreading a previous version of the manuscript.
Author contributions: YS, SB, IGC conceived and designed the study. MA drafted the protocol and conducted the statistical analyses. MA and IGC drafted the manuscript. All authors critically revised the manuscript and agreed on the final version.
Muaamar Al-Gobari, PharmD, PhD
Centre of primary care and Public Health (Unisanté)
Rte de la Corniche 2
CH-1066 Epalinges
muaamar.al-gobari[at]unisante.ch /muaamar.algobari[at]gmail.com
References
1.
Heinemann LV
,
Heinemann T
. Burnout Research:Emergence and Scientific Investigation of a Contested Diagnosis. SAGE Open. 2017;7(1):2158244017697154. https://doi.org/10.1177/2158244017697154
2.
Bouter LM
,
Zielhuis GA
,
Zeegers MP
. Textbook of epidemiology: Bohn, Stafleu van Loghum.; 2018.
3.
Guseva Canu I
,
Marca SC
,
Dell'Oro F
,
Balázs Á
,
Bergamaschi E
,
Besse C
, et al.
Harmonized definition of occupational burnout: A systematic review, semantic analysis, and Delphi consensus in 29 countries. Scandinavian journal of work, environment & health. 2021;47(2):95-107. Epub 2020/12/02. doi: https://doi.org/10.5271/sjweh.3935. PubMed PMID: 33258478; PubMed Central PMCID: PMCPMC8114565.
4.
WHO
. World Health Organization. International classification of diseases for mortality and morbidity statistics (11th Revision). Retrieved from https://icd.who.int/browse11/l-m/en. 2018.
5.
Guseva Canu I
,
Mesot O
,
Györkös C
,
Mediouni Z
,
Mehlum IS
,
Bugge MD
. Burnout syndrome in Europe: towards a harmonized approach in occupational health practice and research. Industrial health. 2019;57(6):745-52. Epub 2019/03/01. doi: https://doi.org/10.2486/indhealth.2018-0159. PubMed PMID: 30814391; PubMed Central PMCID: PMCPMC6885602.
6.
Maslach C
,
Leiter MP
. Understanding the burnout experience: recent research and its implications for psychiatry. World psychiatry : official journal of the World Psychiatric Association (WPA). 2016;15(2):103-11. Epub 2016/06/07. doi: https://doi.org/10.1002/wps.20311. PubMed PMID: 27265691; PubMed Central PMCID: PMCPMC4911781.
7.
Rodrigues H
,
Cobucci R
,
Oliveira A
,
Cabral JV
,
Medeiros L
,
Gurgel K
, et al.
Burnout syndrome among medical residents: A systematic review and meta-analysis. PloS one. 2018;13(11):e0206840. Epub 2018/11/13. doi: https://doi.org/10.1371/journal.pone.0206840. PubMed PMID: 30418984; PubMed Central PMCID: PMCPMC6231624.
8.
Rotenstein LS
,
Torre M
,
Ramos MA
,
Rosales RC
,
Guille C
,
Sen S
, et al.
Prevalence of Burnout Among Physicians: A Systematic Review. Jama. 2018;320(11):1131-50. Epub 2018/10/17. doi: https://doi.org/10.1001/jama.2018.12777. PubMed PMID: 30326495; PubMed Central PMCID: PMCPMC6233645 Form for Disclosure of Potential Conflicts of Interest and none were reported.
9.
Shoman Y
,
Marca SC
,
Bianchi R
,
Godderis L
,
van der Molen HF
,
Guseva Canu I
. Psychometric properties of burnout measures: a systematic review. Epidemiology and psychiatric sciences. 2021;30:e8. Epub 2021/01/14. doi: https://doi.org/10.1017/s2045796020001134. PubMed PMID: 33436137; PubMed Central PMCID: PMCPMC8057391. https://doi.org/10.1017/S2045796020001134
10.
Bellanti F
,
Lo Buglio A
,
Capuano E
,
Dobrakowski M
,
Kasperczyk A
,
Kasperczyk S
, et al.
Factors Related to Nurses’ Burnout during the First Wave of Coronavirus Disease-19 in a University Hospital in Italy. International Journal of Environmental Research and Public Health. 2021;18(10):5051. PubMed PMID: doi:https://doi.org/10.3390/ijerph18105051.
11.
Mion G
,
Hamann P
,
Saleten M
,
Plaud B
,
Baillard C
. Psychological impact of the COVID-19 pandemic and burnout severity in French residents: A national study. Eur J Psychiatry. 2021;35(3):173–80. https://doi.org/10.1016/j.ejpsy.2021.03.005
12.
Schaufeli WB
,
Greenglass ER
. Introduction to special issue on burnout and health. Psychol Health. 2001 Sep;16(5):501–10. https://doi.org/10.1080/08870440108405523
13.
Schaufeli W.
The burnout enigma solved? Scandinavian journal of work, environment & health. 2021;47(3):169-70. Epub 2021/02/20. doi: https://doi.org/10.5271/sjweh.3950. PubMed PMID: 33604675; PubMed Central PMCID: PMCPMC8126437.
14.
Leclercq C
,
Braeckman L
,
Firket P
,
Babic A
,
Hansez I
. Interest of a Joint Use of Two Diagnostic Tools of Burnout: Comparison between the Oldenburg Burnout Inventory and the Early Detection Tool of Burnout Completed by Physicians. Int J Environ Res Public Health. 2021 Oct;18(19):10544. https://doi.org/10.3390/ijerph181910544
15.
Brenninkmeijer V
,
VanYperen N
. How to conduct research on burnout: advantages and disadvantages of a unidimensional approach in burnout research. Occupational and environmental medicine. 2003;60 Suppl 1(Suppl 1):i16-20. Epub 2003/06/05. doi: https://doi.org/10.1136/oem.60.suppl_1.i16. PubMed PMID: 12782742; PubMed Central PMCID: PMCPMC1765718.
16.
Schaufeli WB
,
Bakker AB
,
Hoogduin K
,
Schaap C
,
Kladler A
. on the clinical validity of the maslach burnout inventory and the burnout measure. Psychol Health. 2001 Sep;16(5):565–82. https://doi.org/10.1080/08870440108405527
17.
Page MJ
,
McKenzie JE
,
Bossuyt PM
,
Boutron I
,
Hoffmann TC
,
Mulrow CD
, et al.
The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. Epub 2021/03/31. doi: https://doi.org/10.1136/bmj.n71. PubMed PMID: 33782057; PubMed Central PMCID: PMCPMC8005924 at http://www.icmje.org/conflicts-of-interest/
18.
Al-Gobari M
,
Shoman Y
,
Blanc C
,
Guseva Canu I
. Prevalence of occupational burnout in Swiss Adult population: a systematic review available at https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=266633 (accessed on 15.02.2022). 2021.
19.
Federal Statistical Office (FSO)
. Enquête suisse sur la santé (ESS): Conditions de travail et état de santé, 2012–2017. OFS, 2019.
20.
Shamliyan T
,
Ansari MT
,
Raman G
,
Berkman N
,
Grant M
,
Janes G
, et al.
Development and Implementation of the Standards for Evaluating and Reporting Epidemiologic Studies on Chronic Disease Incidence or Prevalence. Am J Public Health Res. 2013;1(7):183–90. https://doi.org/10.12691/ajphr-1-7-7
21.
DerSimonian R
,
Laird N
. Meta-analysis in clinical trials. Control Clin Trials. 1986 Sep;7(3):177–88. https://doi.org/10.1016/0197-2456(86)90046-2
22.
Higgins JP
,
Green S
, editors
. Identifying and measuring heterogeneity. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. 2011.
23.
State Secretariat for Economic Affaires (SECO)
. Sixième Enquête européenne sur les conditions de travail en 2015 2017 [18.02.2022]. Available from: https://www.seco.admin.ch/seco/fr/home/Publikationen_Dienstleistungen/Publikationen_und_Formulare/Arbeit/Arbeitsbedingungen/Studien_und_Berichte/6_europaeische_erhebung_arbeitsbedingungen_2015.html#:~:text=Working%20Conditions%20Survey%2C%20EWCS)%20est,et%20de%20travail%20(EUROFOUND).
24.
Merlani P
,
Verdon M
,
Businger A
,
Domenighetti G
,
Pargger H
,
Ricou B
; STRESI+ Group
. Burnout in ICU caregivers: a multicenter study of factors associated to centers. Am J Respir Crit Care Med. 2011 Nov;184(10):1140–6. https://doi.org/10.1164/rccm.201101-0068OC
25.
Arigoni F
,
Bovier PA
,
Sappino AP
. Trend of burnout among Swiss doctors. Swiss Med Wkly. 2010 Aug;140(AUGUST):w13070. https://doi.org/10.4414/smw.2010.13070
26.
Hämmig O
,
Brauchli R
,
Bauer GF
. Effort-reward and work-life imbalance, general stress and burnout among employees of a large public hospital in Switzerland. Swiss Med Wkly. 2012 May;142(MAY):w13577. https://doi.org/10.4414/smw.2012.13577
27.
Zumbrunn B
,
Stalder O
,
Limacher A
,
Ballmer PE
,
Bassetti S
,
Battegay E
, et al.
The well-being of Swiss general internal medicine residents. Swiss Med Wkly. 2020 Jun;150(23-24):w20255. https://doi.org/10.4414/smw.2020.20255
28.
Steinlin C
,
Dolitzsch C
,
Kind N
,
Fischer S
,
Schmeck K
,
Fegert JM
, et al.
The influence of sense of coherence, self-care and work satisfaction on secondary traumatic stress and burnout among child and youth residential care workers in Switzerland. Child & Youth Services. 2017;38(2):159-75. doi: https://doi.org/10.1080/0145935x.2017.1297225. PubMed PMID: WOS:000403475800006. https://doi.org/10.1080/0145935X.2017.1297225
29.
Studer R
,
Quarrez S
. Enquête sur la santé des enseignants romands Lasuanne, Switzerland: Institut universitaire romand de Santé au Travail, 2017 2017. Report No.
30.
Businger A
,
Stefenelli U
,
Guller U
. Prevalence of burnout among surgical residents and surgeons in Switzerland. Archives of surgery (Chicago, Ill : 1960). 2010;145(10):1013-6. Epub 2010/10/20. doi: https://doi.org/10.1001/archsurg.2010.188. PubMed PMID: 20956772.
31.
Favrod C
,
Jan du Chene L
,
Martin Soelch C
,
Garthus-Niegel S
,
Tolsa JF
,
Legault F
, et al.
Mental Health Symptoms and Work-Related Stressors in Hospital Midwives and NICU Nurses: A Mixed Methods Study. Frontiers in psychiatry. 2018;9:364. Epub 2018/09/05. doi: https://doi.org/10.3389/fpsyt.2018.00364. PubMed PMID: 30177890; PubMed Central PMCID: PMCPMC6109791.
32.
Reissig L
,
Crameri A
,
von Wyl A
. Prevalence and predictors of burnout in Swiss farmers – Burnout in the context of interrelation of work and household. Ment Health Prev. 2019;14:200157. https://doi.org/10.1016/j.mph.2019.200157
33.
Hämmig O
,
Bauer GF
. Work, work-life conflict and health in an industrial work environment. Occup Med (Lond). 2014 Jan;64(1):34–8. https://doi.org/10.1093/occmed/kqt127
34.
Gerber M
,
Schilling R
,
Colledge F
,
Ludyga S
,
Pühse U
,
Brand S
. More than a simple pastime? The potential of physical activity to moderate the relationship between occupational stress and burnout symptoms. Int J Stress Manag. 2020;27(1):53–64. https://doi.org/10.1037/str0000129
35.
Divaris K
,
Lai CS
,
Polychronopoulou A
,
Eliades T
,
Katsaros C
. Stress and burnout among Swiss dental residents. Schweizer Monatsschrift fur Zahnmedizin = Revue mensuelle suisse d'odonto-stomatologie = Rivista mensile svizzera di odontologia e stomatologia. 2012;122(7-8):610-5. Epub 2012/08/24. PubMed PMID: 22914975.
36.
Welp A
,
Rothen HU
,
Massarotto P
,
Manser T
. Teamwork and clinician burnout in Swiss intensive care: the predictive role of workload, and demographic and unit characteristics. Swiss Med Wkly. 2019 Mar;149(11-12):w20033. https://doi.org/10.4414/smw.2019.20033
37.
Lindemann F
,
Rozsnyai Z
,
Zumbrunn B
,
Laukenmann J
,
Kronenberg R
,
Streit S
. Assessing the mental wellbeing of next generation general practitioners: a cross-sectional survey. BJGP open. 2019;3(4). Epub 2019/10/17. doi: https://doi.org/10.3399/bjgpopen19X101671. PubMed PMID: 31615787; PubMed Central PMCID: PMCPMC6995859.
38.
Hammig O.
Explaining burnout and the intention to leave the profession among health professionals - a cross-sectional study in a hospital setting in Switzerland. BMC health services research. 2018;18(1):785. Epub 2018/10/21. doi: https://doi.org/10.1186/s12913-018-3556-1. PubMed PMID: 30340485; PubMed Central PMCID: PMCPMC6194554.
39.
Nguyen Huynh A
,
Béguelin A
,
Krief P
,
Marion-Veyron R
,
Mediouni Z
,
Regamey F
, et al.
[Detection and treatment of burnout by physicians of Unisanté]. Rev Med Suisse. 2021 Jan;17(723):221–4. https://doi.org/10.53738/REVMED.2021.17.723.0221
40.
Kind N
,
Burgin D
,
Fegert JM
,
Schmid M
. What Protects Youth Residential Caregivers from Burning Out? A Longitudinal Analysis of Individual Resilience. Int J Environ Res Public Health. 2020;17(7). Epub 2020/03/29. doi: https://doi.org/10.3390/ijerph17072212. PubMed PMID: 32218385; PubMed Central PMCID: PMCPMC7178075.
41.
Federal Statistical Office (FSO)
. Travail et santé: Résultats de l’enquête suisse sur la santé 2012. 2014.
42.
Nicolin E.
Enseignant· e· s spécialisé· e· s face au stress professionnel: état des lieux, ressources et stratégies d'ajustement: Université de Lausanne, Faculté des sciences sociales et politiques; 2018.
43.
Squillaci M.
Analysis of the burnout levels of special education teachers in Switzerland in link with a reform implementation. European Journal of Special Needs Education. 2020. doi: https://doi.org/10.1080/08856257.2020.1809802. PubMed PMID: WOS:000564308500001.
44.
Heeb JL
,
Haberey-Knuessi V
. Health Professionals Facing Burnout: What Do We Know about Nursing Managers? Nursing research and practice. 2014;2014:681814. Epub 2014/05/08. doi: https://doi.org/10.1155/2014/681814. PubMed PMID: 24804090; PubMed Central PMCID: PMCPMC3997154.
45.
Nguyen Huynh A
,
Béguelin A
,
Krief P
,
Marion-Veyron R
,
Mediouni Z
,
Regamey F
, et al.
[Detection and treatment of burnout by physicians of Unisanté]. Rev Med Suisse. 2021 Jan;17(723):221–4. https://doi.org/10.53738/REVMED.2021.17.723.0221
46.
Thomas M
,
Kohli V
,
Choi J
. Correlates of job burnout among human services workers: implications for workforce retention. J Sociol Soc Welf. 2014;41:69.
47.
Shanafelt TD
,
Sloan JA
,
Habermann TM
. The well-being of physicians. Am J Med. 2003 Apr;114(6):513–9. https://doi.org/10.1016/s0002-9343(03)00117-7 https://doi.org/10.1016/S0002-9343(03)00117-7
48.
Pedersen AF
,
Andersen CM
,
Olesen F
,
Vedsted P
. Risk of Burnout in Danish GPs and Exploration of Factors Associated with Development of Burnout: A Two-Wave Panel Study. Int J Family Med. 2013;2013:603713. https://doi.org/10.1155/2013/603713
49.
Pedersen AF
,
Andersen CM
,
Olesen F
,
Vedsted P
. [Stress and burnout increase among general practitioners in Denmark]. Ugeskr Laeger. 2014 Jan;176(2):135–8.
50.
Schaufeli W
. Past performance and future perspectives of burnout research. SA J Ind Psychol. 2003;29(4):1–15. https://doi.org/10.4102/sajip.v29i4.127
51.
Kant IJ
,
Bültmann U
,
Schröer KA
,
Beurskens AJ
,
Van Amelsvoort LG
,
Swaen GM
. An epidemiological approach to study fatigue in the working population: the Maastricht Cohort Study. Occupational and environmental medicine. 2003;60 Suppl 1(Suppl 1):i32-9. Epub 2003/06/05. doi: https://doi.org/10.1136/oem.60.suppl_1.i32. PubMed PMID: 12782745; PubMed Central PMCID: PMCPMC1765733.
52.
Maske UE
,
Riedel-Heller SG
,
Seiffert I
,
Jacobi F
,
Hapke U
. [Prevalence and Comorbidity of Self-Reported Diagnosis of Burnout Syndrome in the General Population - Results of the German Health Interview and Examination Survey for Adults (DEGS1)]. Psychiatr Prax. 2016 Jan;43(1):e1. https://doi.org/10.1055/s-0035-1552702
53.
INAMI
. Institut national d'assurance maladie-invalidité. Incapacité de Travail de Longue Durée: Combien de Burnouts et de Dépressions de Longue Durée? Quel Coût Pour L’assurance Indemnités? Available online: https://www.inami.fgov.be/fr/statistiques/indemnites/Pages/incapacite-travail-longue-duree-combien-burn-outs-depressions.aspx (accessed on 15.02.2022)
54.
Kahill S
. Symptoms of professional burnout: A review of the empirical evidence. Can Psychol. 1988;29(3):284–97. https://doi.org/10.1037/h0079772
55.
Rudman A
,
Arborelius L
,
Dahlgren A
,
Finnes A
,
Gustavsson P
. Consequences of early career nurse burnout: A prospective long-term follow-up on cognitive functions, depressive symptoms, and insomnia. EClinicalMedicine. 2020;27:100565. Epub 2020/11/06. doi: https://doi.org/10.1016/j.eclinm.2020.100565. PubMed PMID: 33150328; PubMed Central PMCID: PMCPMC7599295.
56.
Glass DC
,
McKnight JD
,
Valdimarsdottir H
. Depression, burnout, and perceptions of control in hospital nurses. J Consult Clin Psychol. 1993 Feb;61(1):147–55. https://doi.org/10.1037//0022-006x.61.1.147 https://doi.org/10.1037/0022-006X.61.1.147
57.
Koutsimani P
,
Montgomery A
,
Georganta K.
The Relationship Between Burnout, Depression, and Anxiety: A Systematic Review and Meta-Analysis. Frontiers in psychology. 2019;10:284. Epub 2019/03/29. doi: https://doi.org/10.3389/fpsyg.2019.00284. PubMed PMID: 30918490; PubMed Central PMCID: PMCPMC6424886.
58.
Schaufeli WB
,
Desart S
,
De Witte H
. Burnout Assessment Tool (BAT)-Development, Validity, and Reliability. Int J Environ Res Public Health. 2020;17(24). Epub 2020/12/24. doi: https://doi.org/10.3390/ijerph17249495. PubMed PMID: 33352940; PubMed Central PMCID: PMCPMC7766078.
59. Calculating the cost of work-related stress and psychosocial risks European Risk Observatory Literature Review: European Agency for Safety and Health at Work (EU-OSHA); 2014 [cited 11.02.2022]. Available from: https://osha.europa.eu/en/publications/calculating-cost-work-related-stress-and-psychosocial-risks
60.
Ramaciotti D
,
Perriard J
. Les coûts du stress en Suisse: State Secretariat for Economic Affaires (SECO); 2003 [cited 2022 12.07.2022]. Available from: https://www.seco.admin.ch/seco/fr/home/Publikationen_Dienstleistungen/Publikationen_und_Formulare/Arbeit/Arbeitsbedingungen/Studien_und_Berichte/6_europaeische_erhebung_arbeitsbedingungen_2015.html#:~:text=Working%20Conditions%20Survey%2C%20EWCS)%20est,et%20de%20travail%20(EUROFOUND).
61.
Shoman Y
,
El May E
,
Marca SC
,
Wild P
,
Bianchi R
,
Bugge MD
, et al.
Predictors of Occupational Burnout: A Systematic Review. International Journal of Environmental Research and Public Health. 2021;18(17):9188. PubMed PMID: doi:https://doi.org/10.3390/ijerph18179188.
62.
von Hippel PT
. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med Res Methodol. 2015 Apr;15(1):35. https://doi.org/10.1186/s12874-015-0024-z
63.
Eyles E
,
Moran P
,
Okolie C
,
Dekel D
,
Macleod-Hall C
,
Webb RT
, et al.
Systematic review of the impact of the COVID-19 pandemic on suicidal behaviour amongst health and social care workers across the world. Journal of affective disorders reports. 2021;6:100271. Epub 2021/11/30. doi: https://doi.org/10.1016/j.jadr.2021.100271. PubMed PMID: 34841385; PubMed Central PMCID: PMCPMC8607051.
64.
De Kock JH
,
Latham HA
,
Leslie SJ
,
Grindle M
,
Munoz SA
,
Ellis L
, et al.
A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. BMC Public Health. 2021;21(1):104. Epub 2021/01/11. doi: https://doi.org/10.1186/s12889-020-10070-3. PubMed PMID: 33422039; PubMed Central PMCID: PMCPMC7794640.
65.
Peters SE
,
Dennerlein JT
,
Wagner GR
,
Sorensen G
. Work and worker health in the post-pandemic world: a public health perspective. The Lancet Public health. 2022;7(2):e188-e94. Epub 2022/02/06. doi: https://doi.org/10.1016/s2468-2667(21)00259-0. PubMed PMID: 35122760; PubMed Central PMCID: PMCPMC8809900. https://doi.org/10.1016/S2468-2667(21)00259-0
Appendix: Supplementary data
The appendix is available in the PDF version of the manuscript.