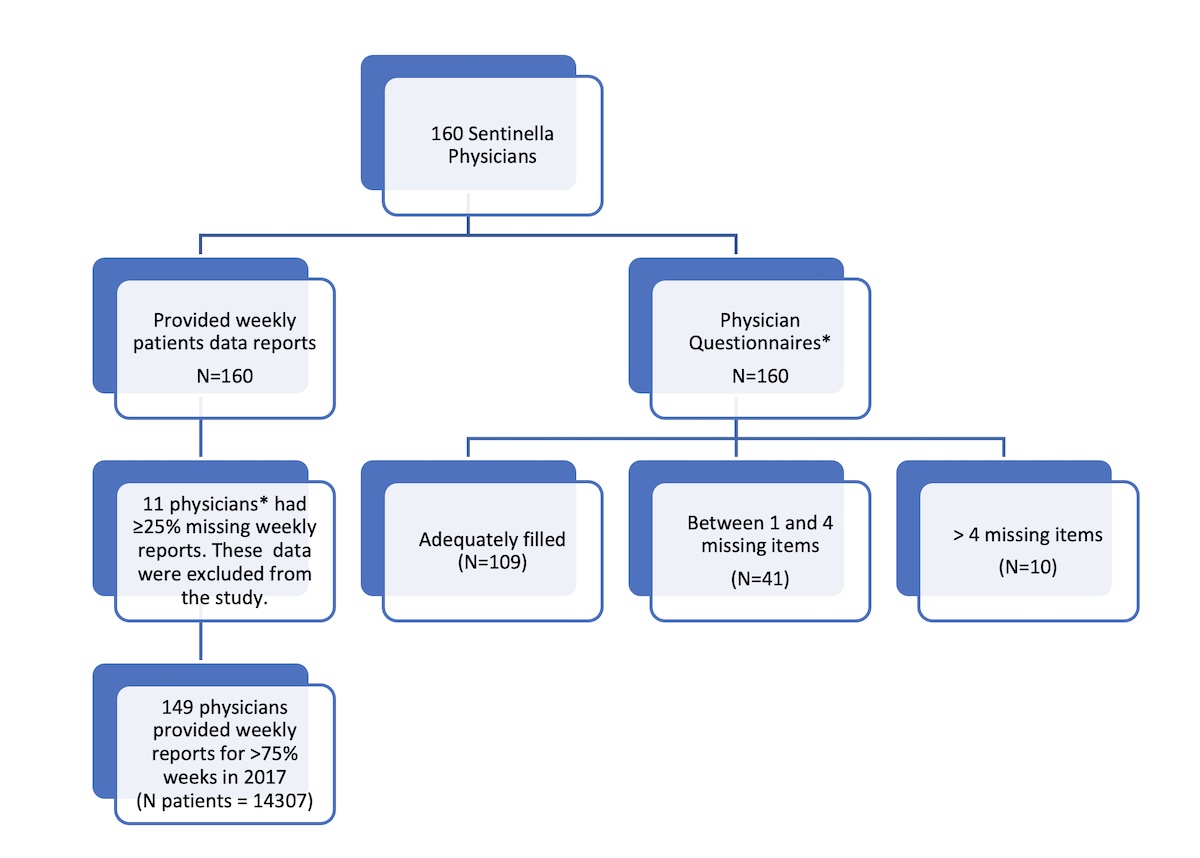
Figure 1 Summary of the data collection.
* Characteristics of physicians with missing weekly reports were included in the analysis of the physician questionnaires.
DOI: https://doi.org/10.4414/SMW.2022.w30226
Injuries are amongst the most frequent causes of morbidity and mortality in the general population worldwide [1]. This is also true in Switzerland where, according to the Global Burden of Disease study, falls are the second overall cause of years lost to disability [1].
In high income countries, injured patients increasingly seek care from emergency services directly, without referral from a primary care physician, even for minor injuries [2]. In the Australian BEACH (Bettering the Evaluation of Care and Health) study, injuries and musculoskeletal problems (including non-traumatic musculoskeletal reasons) represented approximately 11.5% of reasons for encounter in general practice [3]. A recent Swiss study showed that general practitioners (GPs) were involved in the management of 70% of all injuries in a sample of a predominantly male, working age population. GPs were the primary provider in more than half of all injury cases in this population [4]. Initial evaluation of injuries and aftercare by GPs are more cost-effective [2, 5, 6]. A small randomised trial comparing GP and emergency service department follow-up care for minor ankle injuries in Switzerland showed that the two options were similar in relation to patients’ satisfaction with care and with outcomes [2]. Very little data were found on injury as a reason for encounter in primary care. As a result, we know little about the extent to which management of injuries remains significant in primary care, in Switzerland and internationally.
In Switzerland, physicians seeking the title of specialist in general internal medicine (FMH) are required to master the evaluation, treatment and potential referral of injured patients as part of their postgraduate training. Yet placements in surgery and orthopaedics are no longer compulsory for future GPs. Similarly, postgraduate training in paediatrics does not include management of injuries beyond acute emergency care.
To this day, there are no available data on the workload represented by injury-related consultations in the primary care physicians’ (GPs or paediatricians) daily practice. There is also little information about Swiss primary care physicians’ postgraduate rotations or their equipment, allowing no conclusion on their level of training and its potential association with the amount of injury care they provide.
A more precise knowledge of the frequency and type of injury care provided in primary care would be useful to contribute to an optimally focused postgraduate training. It could also indicate the extent to which primary care physicians in Switzerland may be prepared to provide more frequent injury management to relieve the increasing overcrowding of emergency services, particularly in urban areas, whilst providing more cost-effective care. The extent to which Swiss primary care physicians manage injuries may vary according to practice type and location and also according to practitioners’ training and personal characteristics.
The aim of this study was to describe the frequency and type of injury management in a representative sample of primary care physicians’ practices throughout Switzerland. Secondary objectives were to describe the characteristics of injury management in Swiss primary care and to assess the extent to which variations in injury management in Swiss primary care practices are associated with physician and/or practice characteristics.
This cross-sectional study took place over the year 2017 within the Swiss Sentinella network. The Swiss Sentinella network is an epidemiological surveillance system which covers infectious disease outbreak surveillance (e.g. influenza, COVID 19) but also contributes to primary care research. The network is composed of a representative sample of primary care practices (general internist and paediatric) throughout Switzerland. Using a web interface managed by the Swiss Federal Office of Public Health (FOPH), the physicians provide weekly anonymous patient data in relation to specific research or epidemiological surveillance themes.
All patients whose motive for consulting one of the Sentinella network physicians included an injury (see definition below), regardless of their age, were included. Patients could be included at their first consultation for this motive but also subsequently. In the context of this study only physical injury was considered and not psychological injury (also described as “trauma” in the literature). An injury is a damage or harm resulting exclusively from an exterior agent [1]. A tick bite, for example can be considered as an injury. On the other hand, a blocked back after lifting a heavy weight is not an injury according to Swiss insurance law, although it can be considered as such in various countries. In this study, only damage or harm resulting from an exterior agent was considered as an injury.
Patients who had suffered an injury but attended the practice for a reason that was unrelated to this injury were excluded from this study.
From 01 January to 31 December 2017, the 160 Sentinella physicians were asked to provide data about each patient they saw who presented with an injury-related motive for the encounter, within their usual weekly report.
Data included information about the patient’s age and gender, up to three types of injury (diagnoses), and up to two localisations. Only the main localisation and the main diagnosis were analysed. The primary care physicians also provided information about whether the patient was consulting for primary care (directly following the injury), follow-up (subsequent consultations following primary care management), or after-care (following treatment initiated in another context, such as in an emergency department); if the consultation was for primary care, whether the primary care physician proposed (1) evaluation and management within the practice, (2) evaluation in another centre and management within the practice, or (3) referral for evaluation and management in another centre. Patient data provided by physicians who failed to regularly transmit weekly reports were excluded from the study (see fig. 1).
At the beginning of the study, Sentinella physicians were asked to complete an anonymous questionnaire about their characteristics (age, gender, location of practice, material equipment, specialist title) and their training and experience in relation to injuries, including postgraduate rotations preparing them for the management of injuries.
In practices involving several physicians, only the main Sentinella reporting physician completed a questionnaire. Data missing from the questionnaires were excluded from the analysis. For some aspects of surgical training, however, if the physician had answered the other questions on this topic, a lack of response was considered to be a lack of surgical training in the relevant area. Figure 1 shows the data collection process.
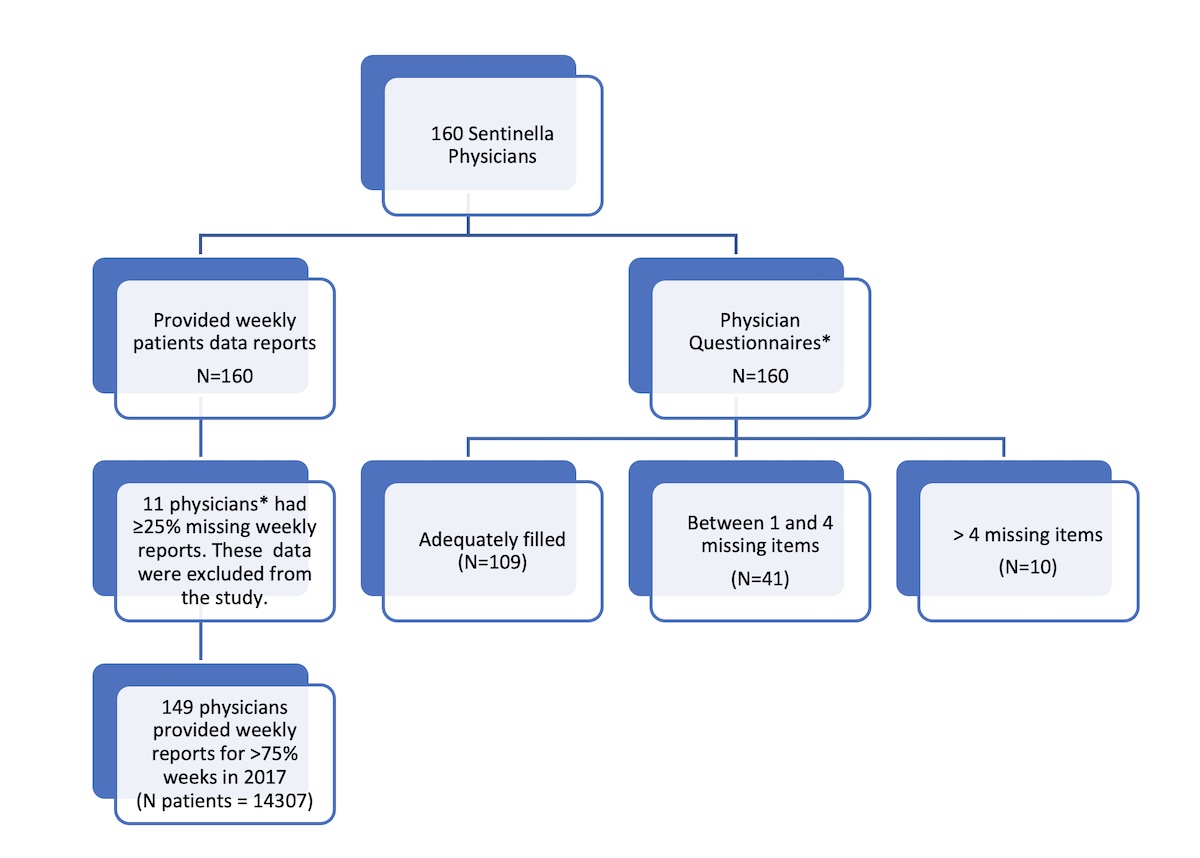
Figure 1 Summary of the data collection.
* Characteristics of physicians with missing weekly reports were included in the analysis of the physician questionnaires.
The anonymous data were sent directly to the FOPH (Federal Office of Public Health) in accordance to the Sentinella protocol, and this data set was transmitted in an anonymous form to the research team at the Geneva Faculty of Medicine for analysis.
There is some evidence in the literature suggesting that the Sentinella Collective is representative of the Swiss population of primary care physicians. A recent study on multimorbidity in primary care in Switzerland within the Sentinella network [7], compared the Sentinella physicians collective in 2015 [8] with that of the Swiss Medical Association (FMH) and found the two distributions (age, gender and speciality) were similar. We compared the distribution of our injury diagnoses to that of the accident claims of the SUVA, the largest accident insurance for people of working age in Switzerland, from year 2013 to 2017 [9], and found both distributions of the main diagnoses (sprains/dislocations, contusions, cutaneous injuries and fractures) to be similar. Therefore, we consider our results to be representative of the distribution of injuries in Switzerland.
As data were anonymous, each consultation was considered as an independent event, not considering whether the patient had already been seen in the practice for this injury before. However, first consultations for a given injury were identified to allow a stratified analysis.
The primary outcome of interest was the prevalence of consultations for injury among Sentinella network physicians. Secondary outcomes included: the prevalence of consultations for injury as compared with the total number of consultations, type and localisation of the injuries and the type of care provided. The total number of consultations was estimated by calculating the total number of patient contacts for two weeks extrapolated to the entire year, in compliance with the usual Sentinella procedure. The proportion represented by injury-related consultations was obtained by dividing the number of consultations for injury by the total number of consultations per year for each physician.
Categorical data were summarised using frequencies and proportions. Means and standard deviations (SDs) were used to summarise continuous variables. Negative binomial regression models for count data were used to investigate the association between different physician characteristics and two of the outcomes (injury-related consultation and injury management within the practice). With these models, the associations are expressed as a ratio of prevalence. A robust sandwich estimator of the variance was used to prevent an issue in the calculation of p-values and confidence intervals (CIs) due to a potential heteroscedasticity. A potential misspecification of the models was investigated with a link test and deviance residuals were visually inspected to identify potential outliers. Sensitivity analyses were conducted, excluding potential outliers.
Physicians with fewer than 10 initial consultations for trauma were excluded from the analysis in table 5, because these low counts threatened the stability of the models and they represented a small part of the overall number of initial consultations.
If one item was missing, the entire patient-related record was excluded from this analysis. A two-sided p-value of 0.05 significance was used. The data were analysed using Stata Corp V15 software and Stata Corp V17 software (for the multivariable analyses).
Since the study involved the analysis of completely anonymous data, the Human Research Ethics Committee confirmed that it did not require formal ethical approval under the Swiss research law. The research team had no access to identifiable individual physician or patient data. Thus, no patient consent procedure was required. Physicians in the Sentinella surveillance network received written information about the objectives of the study and the good use of the weekly questionnaire to report relevant data.
In 2017, the Sentinella network comprised 160 physicians. A total of 149 Sentinella physicians adequately provided data about patients they saw presenting with an injury-related motive for the encounter within their usual weekly report and 160 returned the personal questionnaire.
Table 1 summarises the physicians’ characteristics.
Table 1Characteristics of the physician population of the study (Total n = 160).
| Characteristics | Overall n = 160* | Missing data (%) |
| Sociodemographics | ||
| Male gender | 121 (75.6%) | 0 (0.0%) |
| German language | 105 (65.6%) | 0 (0.0%) |
| Urban / suburban Setting | 135 (86.5%) | 4 (2.5%) |
| Work rate ≥80% | 101 (68.7%) | 13 (8.8%) |
| Proportion of injury related consultations in % | ||
| Amongst general practitioners, median (IQR) | 2.1 (0.7–3.9) | 8 (6.0%) |
| Amongst paediatricians, median (IQR) | 1.2 (0.6–2.7) | 3 (11.5%) |
| FMH title | ||
| General medicine (before 2011) | 58 (36.3%) | 0 (0.0%) |
| Internal medicine or general internal medicine | 63 (39.4%) | |
| Internal medicine and other specialty | 4 (2.5%) | |
| None | 9 (5.6%) | |
| Paediatrics | 26 (16.3%) | |
| Level of postgraduate surgical training (overall) | ||
| Duration of surgical training in years, median (IQR) | 1.0 (0.0–1.5) | 1 (0.6%) |
| Duration of surgical training in years among those who reported having such training, median (IQR) | 1.0 (1.0–2.0) | 1 (0.9%) |
| Duration of training in orthopaedics in years, median (IQR) | 0.0 (0.0–0.0) | 8 (5%) |
| Duration of orthopaedic training in years among those who reported having such training, median (IQR) | 1.0 (0.5–1.0) | 8 (19.5%) |
| Experience in private practice in years, mean (SD) | 17.8 (10.7) | 0 (0.0%) |
| Level of postgraduate surgical training (amongst general practitioners) | ||
| General surgery only | 63 (47.7%) | 2 (1.5%) |
| Orthopaedics only | 1 (0.7%) | |
| Both | 31 (23.5%) | |
| Level of postgraduate surgical training (amongst paediatricians) | ||
| General surgery only | 9 (36.0%) | 1 (4.0%) |
| Orthopaedics only | 2 (8.0%) | |
| Both | 4 (16.0%) | |
| Participation in a regional emergency system | ||
| Emergency service | 125 (83.8%) | 11 (6.9%) |
| Rescue service (ambulance or helicopter) | 23 (15.9%) | 15 (9.4%) |
| Attitude | ||
| Agrees to receive patients at the practice in an emergency | 141 (94.6%) | 11 (6.9%) |
| Agrees to travel at the patient’s location in an emergency | 107 (71.3%) | 10 (6.2%) |
| Equipment / skills at the practice | ||
| Conventional radiology | 102 (68%) | 10 (6.2%) |
| Splints | 110 (73.3%) | 10 (6.2%) |
| Casts | 51 (34.5%) | 12 (7.5%) |
| Suturing | 119 (79.3%) | 10 (6.2%) |
| Wound care | 145 (96.7%) | 10 (6.2%) |
IQR: interquartile range
* Numbers are frequencies and (%) unless stated otherwise
Most were males and their average number of years of experience was 18 ± 11 (SD). Although the majority of them practiced in cities or in a suburban environment, 13.5% worked in rural areas. In terms of postgraduate training, 29.9% had not completed any surgical rotation. However, the majority (68.2%) had completed training in general surgery with a median duration of 1.0 year. Among those who had had training in orthopaedics, the median duration of this training was also 1.0 year; 22.2% had completed dual training in general and orthopaedic surgery. Only 1.9% were trained exclusively in orthopaedics.
The majority of primary care physicians (76.4%) had undergone postgraduate training in an emergency department, and 83.8% contributed to an emergency service in their region. Only a minority participated in a rescue system (e.g., helicopter). There were 125 general practitioners (GPs) with a Swiss Federal Specialist Title (FMH) in internal and/or general medicine, 9 practitioners without FMH title and 26 FMH paediatricians who accounted for 5.6% and 16.3% of the study population, respectively.
Over the year 2017, the physicians reported a total of 14,307 injury-related consultations. Fifty-nine percent of the reported consultations involved men, mostly aged between 18 and 65 years, consulting in an urban or suburban setting (86.5%). In contrast, 57.8% of consultations for patients over 65 involved women (table 2).
Table 2Characteristics of injury-related consultations.*
| Characteristics of the consultations | n | % | |
| Gender and Age (n = 14301) | Male | 8422 | 58.9% |
| Age <18 years | 3000 | 21.0% | |
| Age ≥18 and <65 years | 9116 | 63.7% | |
| Age ≥65 years | 2189 | 15.3% | |
| Geographic setting (n = 13899) | Urban | 7106 | 51.1% |
| Suburban | 3873 | 27.9% | |
| Rural | 2920 | 21.0% | |
| Injured body parts (n = 14213) | Skull / Back | 2408 | 16.9% |
| Thorax | 712 | 5.0% | |
| Abdomen | 131 | 1.0% | |
| Superior Limb | 4980 | 35.0% | |
| Inferior Limb | 5982 | 42.1% | |
| Type of injury (n = 14266) | Fracture | 2676 | 18.8% |
| Sprain / Dislocation | 4449 | 31.2% | |
| Contusion | 2865 | 20.1% | |
| Traumatic Brain Injury | 466 | 3.3% | |
| Intoxication | 21 | 0.0% | |
| Cutaneous Trauma | 3279 | 23.0% | |
| Other | 510 | 3.6% | |
* n varies between 13,899 and 14,301 due to missing data
First-line consultation at the primary care practice represented 70.7% (n = 10,117) of the total number of injury-related consultations in 2017. The rest were follow-ups or secondary care referrals.
Table 3 shows the association between the proportion of consultations for injury and different physician’s characteristics in a multivariable analysis.
Table 3Multivariable negative binomial regression analysis of the association between different primary care physician characteristics at the practice and prevalence of injury related consultations.
| Characteristic (n) | No. of primary care physicians (n = 126) | No. total consultations | No. injury-related consultations (n = 11,438) | % injury-related consultations* | Unadjusted PR (95% CI) ** | p-value | Adjusted PR (95% CI) ** | p-value | |
| Gender | Female | 30 | 82,971 | 2124 | 2.6 | 1 (reference) | 1 (reference) | ||
| Male | 89 | 358,321 | 12,021 | 3.4 | 1.69 (1.16–2.46) | 0.006 | 1.26 (0.87–1.84) | 0.222 | |
| Paediatrician | No | 101 | 352,225 | 9881 | 2.8 | 1 (reference) | 1 (reference) | ||
| Yes | 18 | 89,067 | 1557 | 1.7 | 0.59 (0.37–0.94) | 0.028 | 0.49 (0.31–0.78) | 0.003 | |
| Activity rate | ≤60 % | 17 | 37,268 | 960 | 2.6 | 1 (reference) | 0.079 | 1 (reference) | 0.234 |
| >60% and ≤80% | 20 | 67,837 | 1274 | 1.9 | 0.58 (0.33–0.99) | 0.048 | 0.67 (0.40–1.12) | 0.129 | |
| >80% | 82 | 336,187 | 9204 | 2.7 | 0.97 (0.64–1.48) | 0.900 | 0.72 (0.46–1.14) | 0.159 | |
| Years of experience | ≤5 | 25 | 68,512 | 2248 | 3.3 | 1 (reference) | 0.142 | 1 (reference) | 0.017 |
| >5 and ≤15 | 25 | 96,185 | 2130 | 2.2 | 0.65 (0.37–1.16) | 0.149 | 0.73 (0.41–1.27) | 0.263 | |
| >15 and ≤25 | 44 | 185,496 | 5276 | 2.8 | 0.76 (0.46–1.24) | 0.267 | 0.82 (0.50–1.36) | 0.452 | |
| >25 | 25 | 91,099 | 1784 | 2.0 | 0.49 (0.26–0.91) | 0.025 | 0.41 (0.23–0.75) | 0.004 | |
| Urban setting | No | 49 | 204,796 | 5799 | 2.8 | 1 (reference) | 1 (reference) | ||
| Yes | 70 | 236,496 | 5639 | 2.4 | 0.97 (0.68–1.39) | 0.884 | 0.97 (0.69–1.35) | 0.837 | |
| Postgraduate training in surgery /orthopaedics | None | 37 | 114,149 | 3163 | 2.8 | 1 (reference) | 0.650 | 1 (reference) | 0.120 |
| Surgery only | 58 | 228,819 | 5347 | 2.3 | 0.88 (0.56–1.37) | 0.561 | 0.66 (0.42–1.03) | 0.070 | |
| Surgery+ortho | 24 | 98,324 | 2928 | 3.0 | 1.06 (0.71–1.60) | 0.763 | 0.91 (0.55–1.50) | 0.705 | |
| Postgraduate training in emergency department | No | 27 | 88,456 | 2009 | 2.3 | 1 (reference) | 1 (reference) | ||
| Yes | 92 | 352,836 | 9429 | 2.7 | 1.38 (0.87–2.18) | 0.177 | 0.97 (0.64–1.47) | 0.880 | |
| Radiological equipment | No | 37 | 121,049 | 2169 | 1.8 | 1 (reference) | 1 (reference) | ||
| Yes | 82 | 320,243 | 9269 | 2.9 | 1.64 (1.08–2.51) | 0.021 | 1.18 (0.80–1.74) | 0.414 | |
| Splints/casts | No | 31 | 89,752 | 1369 | 1.5 | 1 (reference) | 0.016 | 1 (reference) | 0.004 |
| Splints | 49 | 183,835 | 4680 | 2.5 | 1.57 (0.94–2.62) | 0.087 | 1.70 (1.09–2.66) | 0.020 | |
| Splints+casts | 39 | 167,705 | 5389 | 3.2 | 2.20 (1.27–3.78) | 0.005 | 2.38 (1.43–3.97) | 0.001 | |
| Wound care | No | 3 | 10,962 | 11 | 0.1 | 1 (reference) | <0.001 | 1 (reference) | <0.001 |
| Wound care without suture | 23 | 65,002 | 854 | 1.3 | 11.75 (3.85–35.86) | <0.001 | 5.97 (2.17–16.39) | 0.001 | |
| Wound care with suture | 93 | 365,328 | 10573 | 2.9 | 26.71 (9.63–74.06) | <0.001 | 9.36 (3.42–25.61) | <0.001 | |
* We report here the proportion of injury-related consultations so that readers can have an idea of the difference in proportion according to different characteristics of the primary care physician.
** Prevalence ratios (PRs) unadjusted and adjusted for all other variables using negative binomial regression models. CI: confidence interval
Being paediatrician alone was associated with seeing proportionally fewer injured patients at the practice. Indeed, the median proportion of consultations for injury across all GPs (not including paediatricians) was 2.1 % and that of paediatricians only was 1.2% (p = 0.03). Furthermore, 37.1% (n = 1114) of the total 3000 consultations involving patients of paediatric age occurred at a GP’s practice (p <0.001).
Physicians with more than 25 years of experience had a lower prevalence of injury-related consultations, whereas the ability to perform wound care and to place splints and casts were associated with a greater prevalence ratio of injury-related consultations at the practice.
Descriptive information about injury-related consultations is presented in table 2. Most injuries involved the inferior limbs and the superior limbs (42.1% and 35.0% respectively) and the skull or the back (16.9%). Out of all reported cases, sprains and dislocations were the most frequent diagnoses (31.2%), followed by cutaneous injuries (23.0%), contusions (20.1%) and fractures (18.8%). However, cutaneous injuries and fractures were the main diagnoses in people over 65.
Table 4 presents the evaluation and management by type of injury following a first consultation (i.e., not a follow-up) in primary care.
Table 4Evaluation and management characteristics by type of injury following a first consultation for injury in primary care.
| Type of evaluation and management | Most frequent main diagnoses (%) | |||||||
| Fracture n= 1454 | Sprain/dislocation n = 3444 | Contusion n = 2284 | Traumatic brain Injury n = 295 | Intoxication n = 19 | Cutaneous trauma n = 2261 | Other n = 335 | Total n = 10,092* | |
| Evaluation and treatment at the practice, no referral | 987 (67.9) | 3048 (88.5) | 2119 (92.8) | 244 (82.7) | 14 (73.7) | 2115 (93.5) | 253 (75.5) | 8780 (87.0) |
| External evaluation followed by treatment at the primary care physician | 146 (10.0) | 186 (5.4) | 78 (3.4) | 16 (5.4) | 1 (5.3) | 47 (2.1) | 16 (4.8) | 490 (4.9) |
| Immediate referral for external evaluation and treatment | 268 (18.4) | 174 (5.1) | 77 (3.4) | 25 (8.5) | 2 (10.5) | 86 (3.8) | 58 (17.3) | 690 (6.8) |
| Other | 53 (3.7) | 36 (1.0) | 10 (0.4) | 10 (3.4) | 2 (10.5) | 13 (0.6) | 8 (2.4) | 132 (1.3) |
* actual n <10117 due to missing data
Eighty-seven percent (87.0%) of them were managed in primary care without further referral. Analysis of cases evaluated and treated externally revealed that fractures were the most common diagnosis motivating a referral, followed by sprains and dislocations, cutaneous injuries and contusions.
The association between practice characteristics and injury management at first consultation is presented in table 5.
Table 5Multivariable negative binomial regression analysis of the association between different practice characteristics and prevalence of independent management of patients at the primary care physician’s practice without secondary referral, at first consultation.
| Characteristic (n) | No. of primary care physicians (n = 87) * | No. injury-related initial consultations (n = 7649) * | No. treatment in primary care | % of treatment in primary care (descriptive)** | Unadjusted PR (95% CI) † | p-value | Adjusted PR (95% CI) † | value | |
| Gender | Female | 15 | 924 | 794 | 85.9 | 1 (reference) | 1 (reference) | ||
| Male | 72 | 6725 | 5893 | 87.6 | 1.02 (0.94–1.10) | 0.619 | 1.06 (0.98–1.14) | 0.140 | |
| Peadiatrician | No | 73 | 6425 | 5603 | 87.2 | 1 (reference) | 1 (reference) | ||
| Yes | 14 | 1224 | 1084 | 88.6 | 1.02 (0.94–1.09) | 0.681 | 1.02 (0.97–1.07) | 0.365 | |
| Activity rate | ≤ 60 % | 11 | 568 | 516 | 90.8 | 1 (reference) | 0.373 | 1 (reference) | 0.380 |
| > 60% and ≤ 80% | 13 | 727 | 633 | 87.1 | 0.96 (0.90–1.03) | 0.229 | 0.98 (0.91–1.07) | 0.688 | |
| > 80% | 63 | 6354 | 5538 | 87.2 | 0.96 (0.90–1.02) | 0.177 | 0.96 (0.90–1.02) | 0.181 | |
| Years of experience | ≤ 5 | 18 | 1549 | 1420 | 91.7 | 1 (reference) | 0.191 | 1 (reference) | 0.140 |
| > 5 and ≤ 15 | 20 | 1550 | 1371 | 88.5 | 0.96 (0.90–1.03) | 0.294 | 0.97 (0.91–1.02) | 0.247 | |
| > 15 and ≤ 25 | 35 | 3405 | 2934 | 86.2 | 0.94 (0.88–1.00) | 0.066 | 0.95 (0.90–1.00) | 0.038 | |
| > 25 | 14 | 1145 | 962 | 84.0 | 0.92 (0.83–1.01) | 0.084 | 0.91 (0.83–1.01) | 0.063 | |
| Urban setting | No | 41 | 4189 | 3652 | 87.2 | 1 (reference) | 1 (reference) | ||
| Yes | 46 | 3460 | 3035 | 87.7 | 1.01 (0.96–1.06) | 0.802 | 1.01 (0.96–1.05) | 0.809 | |
| Postgraduate training in surgery/orthopaedics | None | 23 | 2163 | 1918 | 88.7 | 1 (reference) | 0.489 | 1 (reference) | 0.656 |
| Surgery only | 42 | 3648 | 3211 | 88.0 | 0.99 (0.94–1.05) | 0.791 | 1.00 (0.95–1.04) | 0.882 | |
| Surgery+ortho | 22 | 1838 | 1558 | 84.8 | 0.96 (0.88–1.03) | 0.257 | 0.97 (0.92–1.04) | 0.406 | |
| Postgraduate training in emergency department | No | 14 | 1385 | 1199 | 86.6 | 1 (reference) | 1 (reference) | ||
| Yes | 73 | 6264 | 5488 | 87.6 | 1.01 (0.95–1.08) | 0.714 | 1.03 (0.97–1.09) | 0.332 | |
| Radiological equipment | No | 22 | 1300 | 1064 | 81.8 | 1 (reference) | 1 (reference) | ||
| Yes | 65 | 6349 | 5623 | 88.6 | 1.08 (1.01–1.16) | 0.025 | 1.08 (1.00–1.16) | 0.038 | |
| Splints/casts | No | 14 | 638 | 536 | 84.0 | 1 (reference) | 0.603 | 1 (reference) | 0.476 |
| Splints | 39 | 3104 | 2706 | 87.2 | 1.04 (0.93–1.15) | 0.496 | 1.05 (0.94–1.17) | 0.378 | |
| Splints+casts | 34 | 3907 | 3445 | 88.2 | 1.05 (0.95–1.16) | 0.336 | 1.06 (0.96–1.17) | 0.245 | |
| Wound care | No | 0 | / | / | / | / | / | ||
| Wound care without suture | 10 | 375 | 321 | 85.6 | 1 (reference) | 1 (reference) | |||
| Wound care with suture | 77 | 7274 | 6366 | 87.5 | 1.02 (0.95–1.10) | 0.555 | 0.99 (0.89–1.09) | 0.794 | |
* After excluding 33 primary care physicians with <10 initial consultations for injury and missing data, total number of first consults = 10117
** We report here the proportion of injury-related consultations so that readers can have an idea of the difference in proportion according to different characteristics of the primary care physician .
† Prevalence ratios (PR) unadjusted and adjusted for all other variables using negative binomial regression models. CI: confidence interval
The ability to perform conventional radiology was associated with a higher relative prevalence of independent management of injured patients (without further referral), whereas experience between 15 and 25 years was associated with a lower relative prevalence of independent management of these patients.
Over the year 2017, 149 primary care physicians of the Swiss Sentinella network reported more than 14,000 injury-related consultations, representing a median 2.1% of the total number of consultations in their practices. The distribution of the proportion of injury-related consultations is very heterogeneous ranging from 0.0 to 19.8% of a primary care physician’s total activity.
Most injuries that presented to primary care (87.0%) were entirely managed in the practice without further referral. The ability to perform conventional radiology was associated with a higher probability of independent management, without further referral.
Most of this representative sample of primary care physicians worked full time and had a mean of 17 years professional experience. Although this is no longer required for their title as a primary care specialist, 68.1% had completed postgraduate surgical training and 24.2% had trained in orthopaedics. There was no statistical difference between the proportion of patients with injury seen by primary care physicians who had completed a surgical and/or orthopaedic training and those who had not.
Paediatricians saw proportionally fewer injured patients than their GP colleagues. These data correlate with a 2016 Australian study estimating that only 35% of the parents of a child with a minor injury consulting in an emergency department (ED) tried to make an appointment with their family doctor before travelling to the ED [10]. The majority of these parents reported having more confidence in an emergency department than their family physician for these situations.
It could indicate that parents perform a pre-triage and decide whether to go to the paediatrician, to the GP or to the ED based on their perceived level of severity of a particular injury. Another possibility would be that paediatricians are less exposed to injuries (beyond acute emergency care) in their postgraduate training and tend to refer these patients elsewhere (to specialists or ED) directly. Supporting this hypothesis, only 16.0% of the paediatricians in our sample reported completing dual training in general and orthopaedic surgery and 40.0% had not completed any surgical postgraduate training, compared with 28.0% for general practitioners (see table 1). However, this difference was not statistically significant (p = 0.07), probably due to the small number of paediatricians in the study.
Most consultations involved male patients (58.9%) in an urban or suburban setting. Sprains/dislocations, skin injuries, contusions and fractures accounted for the four main diagnoses encountered in the primary care setting of this study, independently of any age, sex or geographical setting.
The important role of the primary care physician in the management of injuries is underlined by a recent Swiss study that analysed accident claims data from the largest accident insurance fund in Switzerland between 2008 and 2016. It showed that GPs are involved in the management of 70% of accidents and figured as the initial care provider in 56%. However, these data comprised only a population of working age (i.e., not under 18 or above 65) and women employees only accounted for 20% of the sample [4].
Our data also differ slightly from a Spanish study analysing more than 300,000 patient contacts in primary care in Madrid in 2011, in which wounds and contusions (such as bruises) were the most prevalent diagnoses. Burns were also significant, representing 6% of injuries in women. The majority (54%) of patients were women [11]. It could be partially explained by cultural differences in attitudes to seeking help in primary care, with women possibly consulting primary care physicians more often than men.
However, the distribution of injuries by age was similar in both studies.
Overall, 87.0% of all primary care consultations for an injury were managed entirely by the primary care physician without any assistance or referral, indicating a good preparedness. Fracture was the main diagnosis motivating referral, although 67.9% of fractures were managed entirely by the primary care physician.
Still, sprains/dislocations and skin injuries accounted for a significant part of referrals and could potentially be avoided if primary care physicians were optimally equipped and/or trained.
The ability to provide wound care, sutures, splints and casts were all linked to a higher prevalence of injury-related consultations in the practice. Management entirely within the practice was more common if physicians had radiological equipment.
Therefore, we consider the ability to perform wound care and conventional radiology as “must have” competences for injury management at the practice.
Although the prevalence of injury-related consultations seemed higher in practices in which primary care physicians had undergone orthopaedic training, this difference was no longer statistically significant in the adjusted analysis. Thus, our findings provide little guidance about the place of surgery and orthopaedics in the postgraduate training of primary care physicians in relation to injury management.
Interestingly, the proportion of injury-related consultations and independent management within primary care were lower with increasing experience. Our hypothesis is that over the course of their professional career, a primary care physician will tend to accumulate more patients with chronic illnesses, leaving less time for patients with acute consultation motives (including injuries). A reduction in working hours or less continuing medical education while experience increases could also partially explain these findings.
The main strength of this study lies in its extensive coverage of the Swiss territory and its representativeness of the primary care physician population in the country. It also includes a large group of consultations for injuries from people of all ages, representative of the population of patients in Switzerland.
Yet the Sentinella network contains fewer paediatricians than GPs which limits further analysis of this subgroup characteristic. Women primary care physicians might also be underrepresented as they account for 24.4% of the collective only.
Although we do not know the proportion of patients with an injury consulting the ED or a primary care physician, our study gives an idea of the workload represented by injury related consultations in the daily activity of a primary care physician.
Missing data accounted overall for less than 20%. Nevertheless, it could have had an impact on the results especially on the multivariable analysis.
As the data collection were entirely anonymous, we could not define the characteristics of primary care physicians seeing a large number of injured patients more closely, nor could we further investigate the detailed follow-up of these patients. We do not know to which extent variations of the proportion of injury-related consultations of the primary care physicians could be due to a difference in the incidence of injuries between regions (e.g., mountains, sport-related tourism vs plains), to a difference between age groups or to a difficult access either to primary or secondary care (e.g., some regions where paediatric injuries could be more abundant in practices due to the absence of a children’s hospital nearby).
As data were collected through questionnaires, the possibility of a recollection bias subsists. However, Sentinella physicians are accustomed to answering these standardised questionnaires every year.
As the management of patients unnecessarily sent to specialised hospitals has substantial costs [12], knowing to which extent primary care physicians are prepared to provide injury management could contribute to relieving overcrowding in the EDs and limit healthcare costs. It could also help focus postgraduate training, considering essential skills and materials, such as a postgraduate training in trauma management and the ability to perform wound care.
Qualitative studies are needed to further define patient satisfaction, outcome and specific characteristics of primary care physicians seeing many patients presenting with an injury. Other studies could also explore factors (such as geographical proximity and opening hours of the practice, patient’s level of trust) involved in the decision of patients whether to consult their primary care physician or the ED for a particular injury, especially in paediatrics.
The proportion represented by injured patients in a primary care physician’s total activity is heterogeneous. The great majority of injuries presenting to primary care were managed entirely at the practice, confirming that most patients with mild to moderate injuries can be managed within primary care without referral to secondary care. The ability to perform wound care and orthopaedic care such as splints and casts were associated with a higher proportion of injured patients at the primary care physician, highlighting the importance of acquiring these skills during postgraduate training and maintaining them through continuous medical education.
Our study provides key findings to inform health service and for the training of primary care physicians in our country and other similar contexts.
The data underlying this article can be shared pending reasonable request to the corresponding author.
The authors thank the Sentinella commission for their support and scientific input and all the members of the Sentinella network who participated in our study. We also wish to thank Mr Amir Moussa for his help in preparing the database.
The Sentinella Network is supported by the Federal Office of Public Health. This study was conducted as part of the master of medicine thesis of RB & CK, with institutional support from the University of Geneva.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Vos T , Barber RM , Bell B , Bertozzi-Villa A , Biryukov S , Bolliger I , et al. Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015 Aug;386(9995):743–800. https://doi.org/10.1016/S0140-6736(15)60692-4
2. Schwab PR , Benneker LM , Eggli S , Zimmermann H , Exadaktylos AK . Outcome and patients’ satisfaction after functional treatment of acute lateral ankle injuries at emergency departments versus family doctor offices. BMC Fam Pract. 2008 Dec;9(1):69. https://doi.org/10.1186/1471-2296-9-69
3. Britt H . Britt. General practice activity in Australia 1998?1999. N S W Public Health Bull. 1999;10(12):167. https://doi.org/10.1071/NB99073
4. Höglinger M , Knöfler F , Schaumann-von Stosch R , Scholz-Odermatt SM , Eichler K . Recent trends and variations in general practitioners’ involvement in accident care in Switzerland: an analysis of claims data. BMC Fam Pract. 2020 Jun;21(1):99. https://doi.org/10.1186/s12875-020-01170-5
5. Hugentobler W . Kostenvergleich der ambulanten Notfallversorgung in der hausärztlichen Praxis mit den Notfallstationen der Spitäler. Prim Hosp Care. 2006 Aug;6(32):586–9.
6. Eichler K , Hess S , Chmiel C , Bögli K , Sidler P , Senn O , et al. Sustained health-economic effects after reorganisation of a Swiss hospital emergency centre: a cost comparison study. Emerg Med J. 2014 Oct;31(10):818–23. https://doi.org/10.1136/emermed-2013-202760
7. Gnädinger M , Herzig L , Ceschi A , Conen D , Staehelin A , Zoller M , et al. Chronic conditions and multimorbidity in a primary care population: a study in the Swiss Sentinel Surveillance Network (Sentinella). Int J Public Health. 2018 Dec;63(9):1017–26. https://doi.org/10.1007/s00038-018-1114-6
8. Gnädinger M , Conen D , Herzig L , Puhan MA , Staehelin A , Zoller M , et al. Medication incidents in primary care medicine: a prospective study in the Swiss Sentinel Surveillance Network (Sentinella). BMJ Open. 2017 Jul;7(7):e013658. https://doi.org/10.1136/bmjopen-2016-013658
9. Statistique des accidents [Internet]. [cited 2021 Aug 28]. Available from: https://www.suva.ch/fr-ch/la-suva/autoportrait/statistique-des-accidents
10. Gafforini S , Turbitt E , Freed GL . Lower urgency paediatric injuries: parent preferences for emergency department or general practitioner care. Emerg Med Australas. 2016 Oct;28(5):564–8. https://doi.org/10.1111/1742-6723.12651
11. Zoni AC , Domínguez-Berjón MF , Esteban-Vasallo MD , Regidor E . [Injuries treated in primary care in the Community of Madrid: analyses of electronic medical records]. Gac Sanit. 2014 Jan-Feb;28(1):55–60. https://doi.org/10.1016/j.gaceta.2013.06.005
12. Faul M , Wald MM , Sullivent EE , Sasser SM , Kapil V , Lerner EB , et al. Large cost savings realized from the 2006 Field Triage Guideline: reduction in overtriage in U.S. trauma centers. Prehosp Emerg Care. 2012 Apr-Jun;16(2):222–9. https://doi.org/10.3109/10903127.2011.615013