
Figure 1 Detailed technical skills organised in a colour-coded circular design.
DOI: https://doi.org/10.4414/SMW.2022.w30225
Competency in airway management is an essential skill for many medical specialists, including anaesthesiologists, intensive care or emergency physicians, pulmonologists and otorhinolaryngologists. Airway management is a routine procedure in most situations. However it can sometimes be unexpectedly challenging, complex, stressful and even life-threatening for patients.
Despite continuous improvements in equipment, clinical understanding, education and training, airway management complications remain a leading cause of anaesthesia-related morbidity and mortality. Retrospective analyses of legal claims or large national prospective audits have identified areas requiring improvement in several technical skills [1–6]. Additionally, human factors and insufficient non-technical skills can either be responsible for or severely contribute to airway complications. Known contributing factors are a lack of airway assessment and planning, weak situational awareness, inadequate decision-making, and poor communication and teamwork [1–6]. Several national and international societies have published comprehensive and regularly-updated guidelines to standardize the management of difficult airways and improve patient outcomes [7–17]. However, although more than 700,000 general anaesthesias are performed in Switzerland yearly [18], the country has no official national guidelines.
The Fondation Latine des Voies Aériennes (FLAVA) is a Swiss non-profit foundation established in 2010 to promote safe airway management (www.flava.ch). Its primary mission is to improve patient outcomes by supporting education, research, and technological innovations in airway management. Since its creation, FLAVA has organised a yearly, comprehensive, two-day airway management course certified and endorsed by the UK’s Difficult Airway Society (www.das.uk.com) and the European Airway Management Society (www.eamshq.net). The Swiss Society for Anesthaesiology and Perioperative Medicine recognises FLAVA as Switzerland’s airway expert group.
This article presents the newly developed 2022 FLAVA Airway Guidelines (FLAGs) and their scientific basis.
In 2013, FLAVA developed its first algorithm for managing unexpected difficult tracheal intubation (supplementary material in appendix 1). Its development was inspired by several international guidelines, notably the Difficult Airways Society’s algorithm [19], which was the first to emphasise use of a simple linear sequence of successive plans and techniques. To highlight the notion of urgency and elapsing time in cases of management failure, FLAVA’s algorithm was the first to introduce colour coding (green to red) to visually represent its various airway management plans. This simple, streamlined, innovative design received immediate positive feedback and was quickly adopted by a majority of hospitals and private clinics in Switzerland’s French- and Italian-speaking regions. FLAVA was the first expert group to link its algorithm to a dedicated airway cart, with four colour-coded drawers containing the required equipment for each the management plans.
Clinical realities often demonstrate that difficult airway management can be complex and dynamic, and then a linear algorithm provides limited help, especially regarding cognitive aids. In addition, unexpected difficult airway management requires significant non-technical skills [20]. In 2016, Chrimes published his vortex approach concept, a conical-spiral-shaped visual aid for emergency airway management that included a cognitive approach [21]. This representation is now firmly established as an essential aid during airway crises as it allows physicians to focus on key aspects of management while minimising the risks of delay, task fixation or cognitive overload [22].
Like other contemporary algorithms, the main limitations of FLAVA’s 2013 algorithm were its linearity, its focus on one situation (unexpected difficult intubation), and the lack of integration of human factors and non-technical skills. To address these, the 2022 FLAGs were developed to combine technical and non-technical skills. They were designed to guide and assist clinicians in managing the wide array of airway situations that can be encountered in all types of institutions, in daily routine management, and when there are anticipated or unanticipated airway difficulties.
The 2022 FLAGs consist of a colour-coded circular cognitive aid (fig. 1) that includes the most up to date technical skills. It is combined with a blue circular cognitive aid (fig. 4) that emphasises the fundamental non-technical skills and human factors. Both aids are complemented by key mnemonics (fig. 3) and ergonomic tools such as the colour-coded airway cart (fig. 5).

Figure 1 Detailed technical skills organised in a colour-coded circular design.
Four distinct coloured plans are organised circularly (fig. 1), representing the different possible steps in an airway management strategy. The clinically relevant combination and sequence of the different possible plans (as opposed to the classic linear sequence from green to red) enables the selection of the safest strategy for anticipated or unanticipated airway difficulties. This cognitive aid’s circular shape reflects the need for flexibility, allowing a change from one plan to another in consideration of the clinical problem encountered, the situation, and the team’s expertise.
The first acronym — O2PTIM (Oxygenation, Position, Type and size, Introducers / stylets and guides, Muscle relaxants / cricothyroid Membrane identified) — in the centre of the figure, reflects the fundamentals of airway management: maintaining perioperative oxygenation and optimising the chosen technique to maximise the chances of success and patient safety. A second acronym — SOS (Stop, Options, Share) — reminds us of the importance of human factors.
In the event of the most frequent relevant clinical emergency, i.e., unexpected difficult intubation, the FLAG’s circular cognitive aid transforms easily into a linear algorithm (fig. 2).
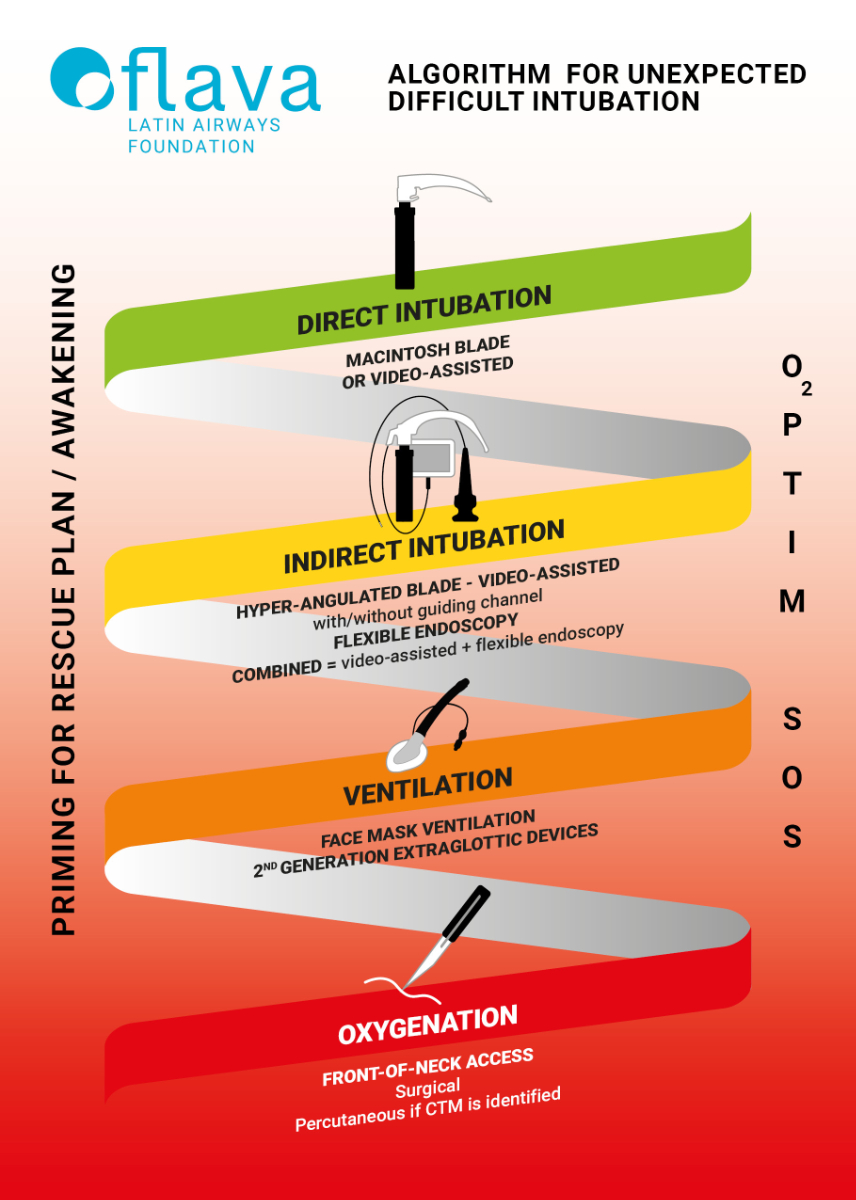
Figure 2 2022 FLAGs’ algorithm for unexpected difficult intubation.
Since it was introduced in 1913 [23, 24], with subsequent blade modifications in the 1940s by Miller [25] and Macintosh [26], direct laryngoscopy has become a conventional tracheal intubation technique and is the accepted gold standard worldwide. A rigid laryngoscope consisting of a handle, a blade and a light source in its distal portion is used to expose the larynx and facilitate the introduction of a tracheal tube beyond the vocal cords. The tip of the blade is designed to lift the epiglottis either directly or indirectly. Many laryngoscope blades exist, but the curved (Macintosh) and the straight (Miller) blade designs still dominate. Unlike Miller’s blade, which allows the epiglottis to be lifted directly, Macintosh’s blade does so indirectly. Anatomical factors (e.g., limited mouth opening, short thyromental distance, a modified Mallampati scale class III or IV, prominent or protruding maxillary incisors, limited neck extension, obesity) have been described as predictors of difficult intubation and may reduce a direct line of vision and render intubation challenging. The incidence of difficult tracheal intubation using this technique ranges from 4% to 8%, and failed tracheal intubation ranges from 0.05% to 0.35% [27]. In the event of difficult direct laryngoscopy, correctly positioning the patient’s head [28] and external laryngeal manipulation (the BURP manoeuvre: Backward, Upward, and Rightward laryngeal Pressure [29]) may improve the alignment of the oral, pharyngeal, and laryngeal axes and thus the clinician’s line of vision.
In the 2022 FLAGs, direct laryngoscopy intubation using a Macintosh blade, with or without video assistance, is the green plan. This technique remains the first choice in most institutions. Furthermore, direct laryngoscopy is still considered the most effective tool for assisting tracheal intubation in specific clinical situations, such as the necessity of a double-lumen tracheal tube or the presence of significant upper airway secretions or bleeding [30, 31].
Thirty years ago, anaesthesiologists had to rely solely on direct laryngoscopy to perform tracheal intubation, but several alternative tools are now available, including a variety of extraglottic devices, tracheal introducers, flexible endoscopes and videolaryngoscopes.
Since their first use in clinical practice in 2003 [32], videolaryngoscopes have rapidly gained popularity as rescue or primary devices, mainly because of improved glottis visualisation through a video camera positioned on their blade, a steep learning curve and the possibility to share airway visualisation with the patient’s care management team. Videolaryngoscopes are now included in most airway guidelines [7–11, 13, 33].
Several different types of videolaryngoscopes are currently available, with differences in blade shape, camera field of view and presence or not of a tube guiding channel. Videolaryngoscopes can be separated in Macintosh-type or hyperangulated blades.
Even though Macintosh-type videolaryngoscopes seem likely to require skills resembling those needed for traditional direct laryngoscopy, studies suggest that handling devices equipped with a tube guiding channel is easily mastered by both experienced and novice laryngoscopists [34].
Although videolaryngoscopes are included in most difficult airway algorithms, they have specific limitations, such as difficulty in directing the tube toward the glottis despite having a clear view of it, difficult visualisation in the presence of blood or excessive secretions, or the potential for injury related to the camera’s position and the oropharyngeal blind spot during endotracheal tube insertion [35]. Nevertheless, videolaryngoscopes can be used in sedated and spontaneously breathing patients [36].
Flexible endoscopes (often still called fibrescopes) have been used routinely since their introduction into clinical practice in the early 1970s [37]; they quickly became part of all difficult airway algorithms. Consisting of an insertion tube, available in different diameters, a flexible tip mounted with a camera and a light source, they enable indirect visualisation either via an eyepiece or on a screen. In special clinical situations oral or nasal fiberopticintubation may also be performed in awake patients [38].
Further enhancements in clinical understanding and technology have now led to the combined use of videolaryngoscopes and fibrescopes, and this can be particularly helpful in difficult cases. The tracheal tube is mounted on a flexible endoscope that serves as an intubation guide, while visualization of the intubation process is assured by the associated videolaryngoscope [39].
Since 1850 face masks have been successfully used to assist or provide ventilation and deliver oxygen or inhaled anaesthesia to the lungs. In cases involving failed intubation, an unsuccessful extraglottic airway device insertion, or both, a face mask still represents an adequate rescue option providing oxygenation and the valuable time to re-establish the strategy. Ineffective or failed attempts at face-mask ventilation must be recognised and should promptly trigger an appropriate response [40]. Two-handed technique, chin lift, proper head position, oropharyngeal airway, and nasopharyngeal airway are useful ways of optimising face-mask ventilation.
Extraglottic airway devices are airway devices positioned out of the glottis and designed to establish and maintain a clear airway for oxygenation and ventilation [40]. Insertion does not require neuromuscular blockade, and incidences of dysphagia and dysphonia associated with tracheal intubation decrease significantly. Their relative ease of use, low complication rate and ventilation efficiency have revolutionised airway management. The original, classic laryngeal mask airway was designed in 1981 and has been widely used in clinical practice since 1988.
The two major drawbacks of first-generation extraglottic airway devices were their incomplete protection against gastric regurgitation (oesophageal seal) and their limitations in providing closed-loop ventilation due to air leaks during positive pressure ventilation (airway seal). Today’s second-generation devices are specifically designed to mitigate both these problems, increasing the devices’ safety and efficacy. Improved cuff designs (inflatable or anatomically pre-shaped) provide a better airway seal enabling controlled ventilation at higher pressure (higher leak pressure). The addition of an accessory channel allows the insertion of a gastric tube, reducing the the risk of aspiration (pneumonia) while safely venting off regurgitated fluids.
Second-generation extraglottic airway devices are probably the most versatile airway management devices. They are mainly used in routine elective practices but play a crucial role in difficult airway management. They can be used as rescue devices after the failure of either face-mask ventilation, tracheal intubation, or both, while additionally providing, in most of them, a conduit to assist flexible endoscopy intubation. When choosing an extraglottic airway device as a first-choice instrument for airway management in a predicted difficult airway, clinicians should be aware of the risks of dislodgement or a complete loss of airway (laryngospasm, major leak, broncho-aspiration); a fiberoptic intubation through an extraglottic airway device before surgery may be a lower-risk alternative.
Understanding the limitations of the extraglottic airway device chosen is critical to its proper use. Ease of insertion, appropriate airway seal pressure, protection against gastric insufflation and pulmonary aspiration, and the ability to intubate through the device are not common to all devices [41].
In the FLAGs guidelines, ensuring ventilation is represented by the Orange Plan. Face-mask ventillation and second-generation extraglottic airway devices are the recommended techniques.
The “can’t intubate, can’t oxygenate” (CICO) scenario is rare but potentially devastating. A CICO event arises when attempts to oxygenate the patient by tracheal intubation or placement of an extraglottic airway device or face-mask ventilation have all failed. Hypoxic brain damage, cardiac arrest and patient death will result unless there is a rapid resolution [7]. The only rescue option unanimously proposed by all the international guidelines is emergency front-of-neck access (eFONA) to the trachea through the cricothyroid membrane. The reported incidence of CICO scenarios requiring eFONA during airway management is 0.002% to 0.07% (1 in 50,000 to 1 in 1400 cases) [5, 42, 43], with the highest incidence described among otorhinolaryngology patients. The cricothyroid membrane is a dense fibroelastic ligament connecting the thyroid and cricoid cartilages. It is the most superficial tracheal access to the neck. Accurate identification of the cricothyroid membrane using digital palpation may be challenging in women [44] and obese patients [45]. Localising the cricothyroid membrane using ultrasound is more precise and reliable but takes longer and should be done before the induction of anaesthesia [46]. Most airway societies recommend a surgical (scalpel-finger-bougie-tube) approach for cricothyroidotomy: a vertical incision of the skin and the subcutaneous tissue to avoid anterior jugular vein damage, digital blunt dissection of tissues, a transverse incision of the cricothyroid membrane, bougie introduction into the trachea, and the railroading of a lubricated tracheal tube [7, 8, 47]. In real-life conditions, this technique seems to be the fastest and has the highest success rate. Experienced operators may occasionally consider a percutaneous, cannula-based technique [10]. Cannula cricothyroidotomy involves puncturing the cricothyroid membrane to allow passage of either a narrow or wide bore cannula to facilitate oxygenation. Analyses of adverse outcomes in CICO situations have demonstrated that difficulties related to inexperience with such rare events are aggravated by inadequate non-technical skills and human factors [48, 49]. Task fixation (a clinician’s reluctance to diagnose a CICO situation), poor team communication and cognitive overload can all delay the transition to an eFONA plan and cause avoidable harm to the patient [47]. Cognitive tools can help to improve situational awareness and teamwork in such crises. The vortex approach and its visual cognitive aid have demonstrated the time savings and the options available if the selected airway management technique fails [21]. It is therefore essential to anticipate the potential need for neck rescue by preparing the team and its equipment (“priming” the CICO rescue) in parallel with additional attempts to secure the airways using less invasive techniques.
In the FLAGs, oxygenation using eFONA is represented by the red plan. This colour emphasises the urgency and dangers of a CICO situation. A surgical cricothyroidotomy using the scalpel–bougie–tube technique is the first-choice method. In cases where the cricothyroid membrane can be precisely localised using palpation (e.g., a skinny neck) or ultrasound, a percutaneous cricothyroidotomy may be an alternative for an experienced operator trained in this technique. The red circle (fig. 1) surrounding the four plans on our cognitive aid becomes progressively more intense in colour as it approaches the red plan, highlighting the importance of early priming for eFONA as difficulties intubating and oxygenating the patient increase.
The O2PTIM acronym (fig. 3) is a mnemonic aid to remind clinicians of the importance of optimising each technique to maximise the chances of success.
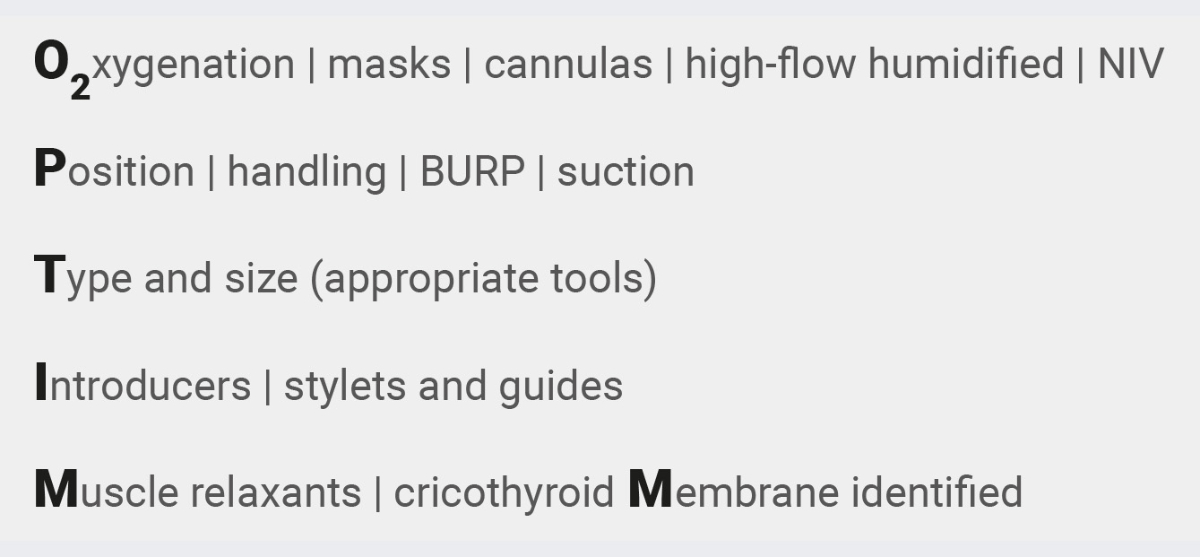
Figure 3 The O2PTIM acronym highlights the importance of adjuncts to optimise technical skills.
BURP: backward, upward, and rightward laryngeal pressure; NIV: noninvasive ventilation
Periprocedural oxygenation prolongs apnoeic time and provides precious additional time in which to solve the problems that may arise during airway management. Situational awareness will help clinicians know which techniques should be considered to enable oxygenation, such as masks, cannulas, noninvasive ventilation, or transnasal oxygenation. Although low-flow transnasal periprocedural oxygenation already significantly extends safe apnoeic time, the current availability of devices delivering high-flow humidified oxygen (up to 70 l/min O2 flow) has further improved this approach [50].
Proper patient positioning and external airway handling (BURP manoeuvre [29]) to improve the alignment of the oral, pharyngeal and laryngeal axes, complemented with suction, may improve the view of the tracheal inlet.
Choosing the right size of the right type of tool can be a game-changer. This is particularly true with extraglottic airway devices. The choice of tool is context-sensitive and should be suitably adapted to the anatomical problem encountered.
If the patient’s anatomy cannot be bent, the clinician may consider using and bending an introducer/stylet or different guides to pre-shape the tube and give themselves the possibility of turning it 360° [51].
The use of neuromuscular blocking drugs is the standard of care to improve conditions of tracheal intubation and reduce upper airway injury [52]. A neuromuscular blockade has be proven to significantly improve face-mask ventilation [53] and therefore a “can’t ventilate” situation should not be declared before attempting muscle relaxation. Nowadays, if necessary, the paralysing effect of rocuronium may be rapidly antagonized by the administration of suggamadex to facilitate the recovery of spontaneous breathing.
Localisation of the cricothyroid membrane using cervical ultrasound has been described as more precise and reliable than palpation, but it takes longer to perform. It should therefore be done before induction of anaesthesia. We encourage practitioners to routinely use ultrasound to localise the cricothyroid membrane for the purpose of improved practice.
Major complications during airway management are often caused by or linked to human, teamwork, communication, psychological or cognitive failures [5]. Poor preparation and planning, failure to change routine plans despite evidence of a potential difficulty, or losing sight of the big picture (fixation error) are all commonly identified problems [1, 4, 5, 54–57]. Experts have therefore called for a “paradigm shift in airway management”, stating that an appreciation of non-technical skills and human factors could be the most radical change in this field since the introduction of the laryngoscope and the laryngeal mask airway [20]. This new paradigm’s motto should be “humans before tools, strategy before instruments, and targets before devices” [20]. Safe airway management is rendered possible thanks to a combination of robust technical and non-technical skills, including planning and preparation, teamwork and assertive communication.
The 2022 FLAGs strive to highlight and integrate both types of skills. Technical skills are embodied in the colour-coded circular cognitive aid (fig. 1), whereas non-technical skills are captured in the FLAGs’ blue circular cognitive aid (fig. 4). Both circles are tightly bounded to facilitate a shared understanding and to reflect the use of common critical language across airway management.
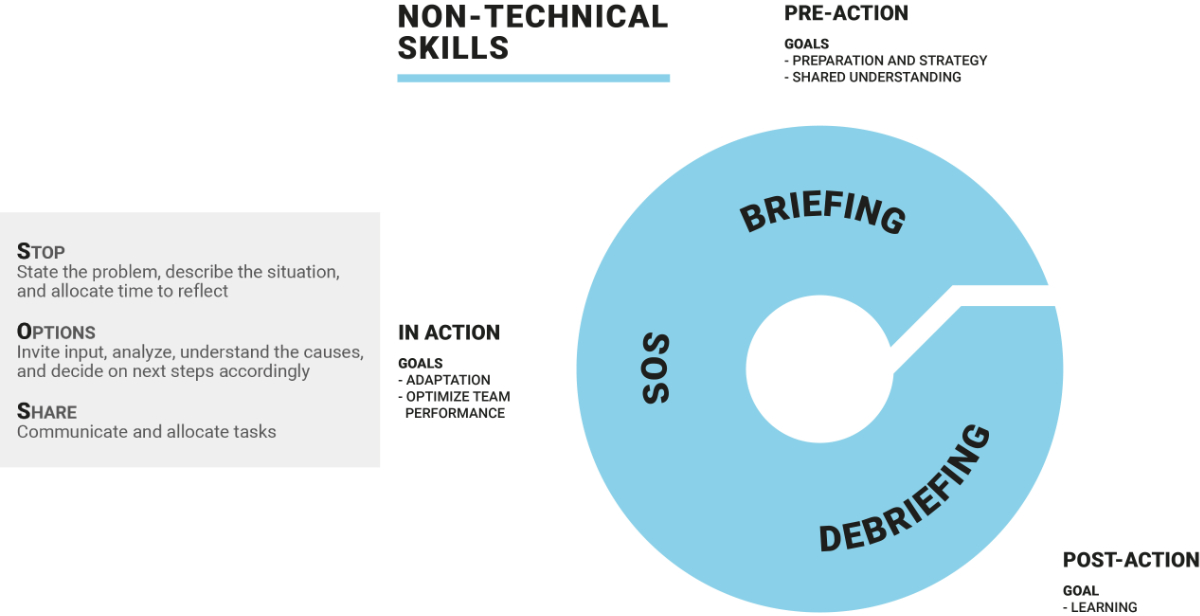
Figure 4 SOS acronym and non-technical skills in airway management.
The FLAGs’ blue circular cognitive aid features the three keywords of “briefing”, “SOS” and “debriefing”. Each represents a different time-point during airway management — “pre-action”, “in action” and “post-action” — and each embodies essential non-technical skills aimed at reinforcing teamwork and team reflexivity. Team reflexivity refers to a team’s ability to reflect collectively on goals, strategies, processes, and the outcomes of past, current and future performance to process key information and adapt accordingly [58].
The briefing is the first step in any airway management situation and the starting point for cognitive aid. The aim is to promote team situational awareness and develop a shared mental model of the coming events, resources and plans of action.
The focus is on creating an explicit team mindset (“we” instead of “me”), climate (psychological safety), structure (role allocation), and organisation (task allocation) together with the necessary resources (do we have what we need?). The airway management strategy should be clearly defined (which plan or technique in which sequence) and understood by every team member (shared mental model) around a common goal (oxygenation).
The briefing establishes the safe space that is crucial for smooth communication and coordinated action [59]. A poor team atmosphere may result in low feelings of psychological safety, a lack of assertiveness, poor communication, and an absence of mutual support and cross-monitoring, all of which affect teamwork and, potentially, patient outcomes.
The SOS mnemonic (Stop, Options, Share) underlies the importance of maintaining the team’s situational awareness and adapting its actions during airway management. SOS is a handbrake (stop) to slow down automatic thinking in favour of thinking more analytically and avoiding cognitive biases (analyse options) [20]. This prompts teams to regularly reassess their actions and communicate (share). A typical SOS trigger could be the occurrence of complications (regurgitation, unexpected difficulties) that require a shift in focus and priorities; another could be when coordination gets out of hand and calling for clarification gets everybody back on track [58, 60, 61].
During high-stakes airway management, the tendency to act on first impressions is high but could prove catastrophic. Although it may seem paradoxical, slowing down interventions with short sequences of shared reflection might prove very useful to help teams avoid going too far down the wrong treatment pathway and minimise the occurrence of fixation errors [58]. Although team leaders would most likely initiate in-action team reflexivity, all team members should feel empowered to trigger an SOS.
Deliberate team reflexivity about past airway management helps teams minimise future mistakes and explicitly identify and reinforce positive behaviours [61]. A post-action analysis of how the team adapted and reacted during a difficult intubation facilitates an understanding of how its adaptation mechanisms can replicate good performance or perform better next time. Debriefings must be done respectfully, and they are intended to help teams learn constructively from their unavoidable errors or regular successes in order to form a collective memory of optimal airway management [62, 63]. To maximise the potential for learning, a debriefing should take place immediately after the action, with all the team members present, and any member of the team can trigger it.
A standardised, colour-coded FLAVA airway cart concept was developed in 2013. Previously, our institutions’ difficult airway carts were heterogeneous, with multiple storage units filled with different devices chosen according to each physician’s preferences and habits. We were convinced that strategies that decreased the potential for team cognitive overload were crucial during an airway crisis. Essential airway cart features, such as limited content, a structured layout, integrated cognitive aids, and standardisation across specialties, can significantly enhance team performance and facilitate decision-making [64]. The FLAVA airway cart is organised to reflect the FLAGs’ dedicated coloured plans. Each drawer is colour-coded and contains a limited range of strategically chosen tools — those necessary to achieve the corresponding plan. It is the intrinsic characteristics of each tool that are essential, not the brand (left to institutional preference). The FLAGs’ algorithm must be easily accessible and clearly visible on the airway cart.
Purchasing a specially customised cart with each front drawer coloured according to the FLAGs is the best option; however, an easily affordable solution consists of using colored stickers with stylised representations of the relevant technical skills for each plan (printable sticker templates can be downloaded for free from our website www.flava.ch). Figure 5 presents two cart designs and their stickers.
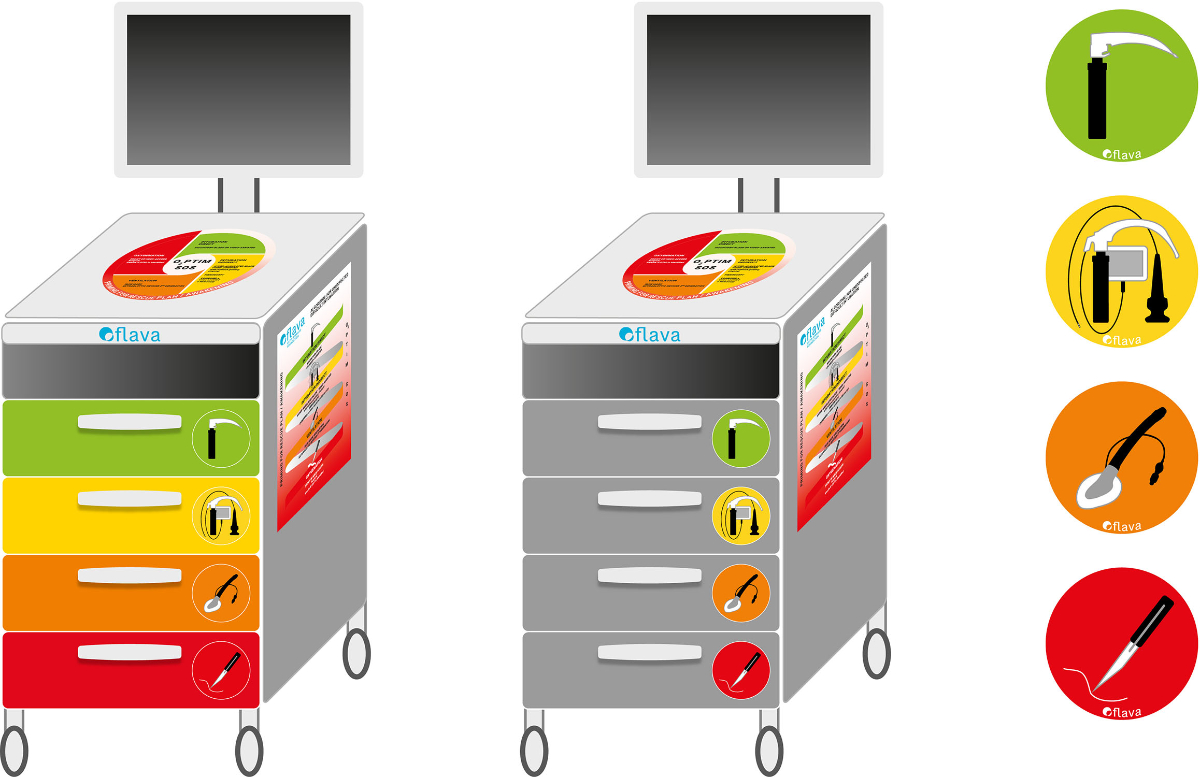
Figure 5 Colour-coded FLAVA airway cart (coloured drawers or sticker-labelled drawers).
Although they were initially only found in the institutions that founded FLAVA, the use of colour-coded airway trolleys has spread rapidly throughout French- and Italian-speaking Switzerland and into some German-speaking regions [65].
Although the focus has traditionally been on the problem of difficult intubation, it is now recognised that extubation may also involve potentially life-threatening complications. Up to one in five patients in intensive care unit settings will require reintubation within 72 hours of their extubation, exposing them to significant increases in associated morbidity and from 23–50% higher rates of in-hospital mortality [66]. In 2012, the UK’s Difficult Airway Society released a set of guidelines for managing tracheal extubation, mainly based on expert opinions [67]. It aimed to provide clinicians with practical guidelines that were easily applicable in daily practice and highlight specific situations that might lead to risk of difficult extubation, such as a history of difficult intubations or extubations, obesity and sleep apnoea syndrome, head or neck pathologies, or the length of surgery. To minimise the potential for peri-extubation complications, a structured, team approach, combining clinical understanding and dedicated equipment allowing a staged extubation strategy is essential [68].
Translating the FLAGs into clinical practice and institutional policy requires each hospital or healthcare establishment to design and implement a strategy. It is beyond the scope of this article to describe such a process, and its complexity will vary depending on the institution’s size, context (private vs public), and mission (teaching vs non-teaching). Nevertheless, we believe that the following key aspects should always be considered. Institutions should regularly train their personnel (physicians, nurses) on airway management using the FLAGs with an airway cart adapted to their setting. Healthcare personnel handling airways should acquire the necessary technical skills related to the devices that their institutions have chosen for each plan in the FLAGs. This should be complemented by regular team training focusing on non-technical skills. Maintaining or updating competencies and knowledge requires regular practice, and the use of active, hands-on learning methods, especially different types of simulation, is strongly recommended [69, 70].
Indeed, we strongly believe that these educational strategies should be part of broader, institutional, quality improvement programmes that also include regular audits of guideline adherence, occurrence of complications, and regular morbidity–mortality conferences. The UK’s Difficult Airway Society recommends that every anaesthesia department appoint a departmental Airway Lead to coordinate such efforts [48].
Safe airway management, in every situation and setting, remains a daily challenge for healthcare providers. The 2022 FLAVA Airway Guidelines are intended to help physicians with daily, routine airway management and with anticipated and unanticipated airway difficulties. The key to successful, safe airway management is combining the use of technical skills and non-technical skills, as summarised in figure 6.
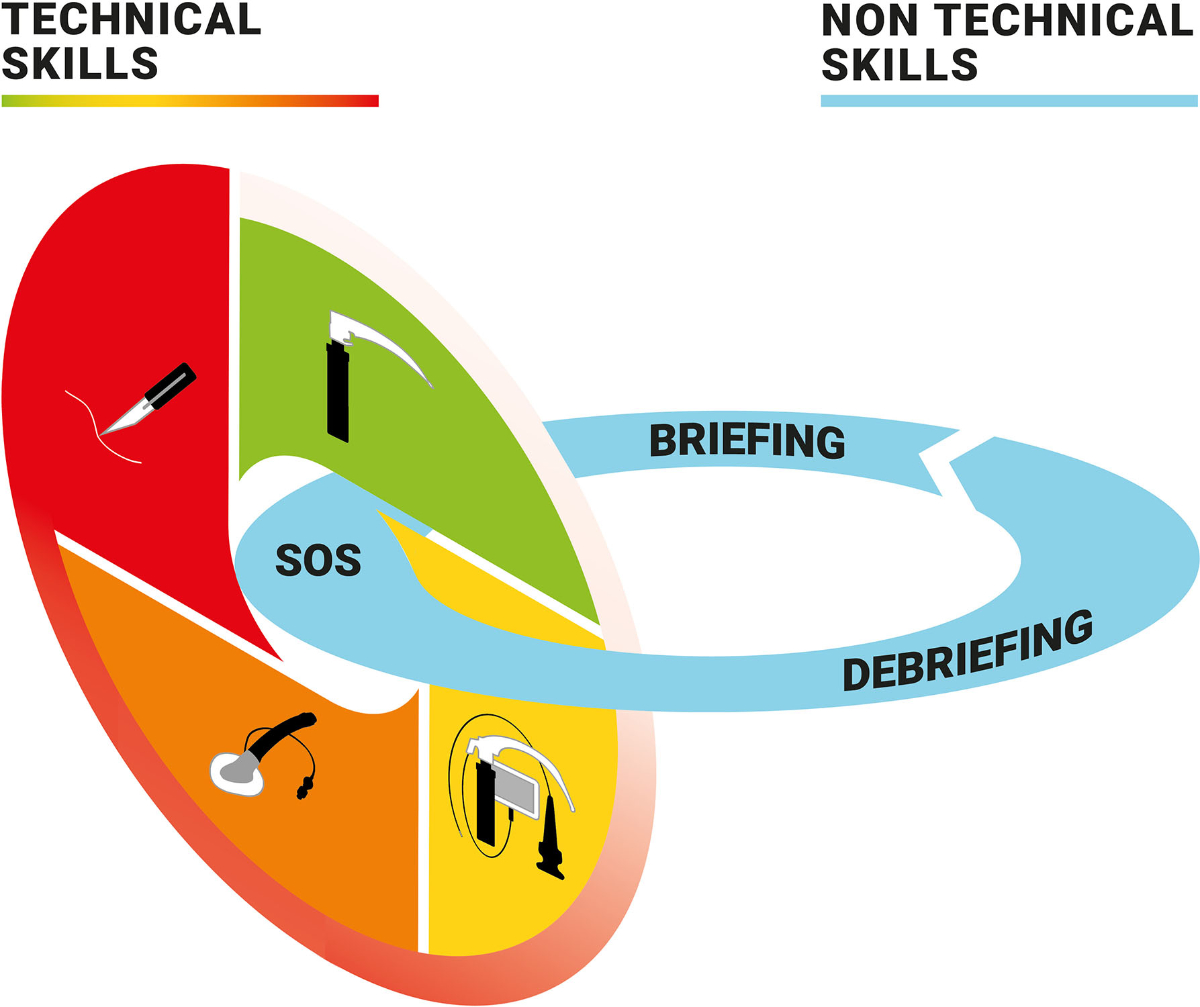
Figure 6 Graphic representation of the 2022 FLAGs with combined technical and non-technical skills.
We wish to thank the Espace Saint-François (www.esf.ch) for its support in graphical communication and the Center for Medical Simulation (www.harvardmedsim.org) for their insightful advice.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Joffe AM , Aziz MF , Posner KL , Duggan LV , Mincer SL , Domino KB . Management of Difficult Tracheal Intubation: A Closed Claims Analysis. Anesthesiology. 2019 Oct;131(4):818–29. https://doi.org/10.1097/ALN.0000000000002815
2. Fornebo I , Simonsen KA , Bukholm IR , Kongsgaard UE . Claims for compensation after injuries related to airway management: a nationwide study covering 15 years. Acta Anaesthesiol Scand. 2017 Aug;61(7):781–9. https://doi.org/10.1111/aas.12914
3. Cook TM , Scott S , Mihai R . Litigation related to airway and respiratory complications of anaesthesia: an analysis of claims against the NHS in England 1995-2007. Anaesthesia. 2010 Jun;65(6):556–63. https://doi.org/10.1111/j.1365-2044.2010.06331.x
4. Crosby ET , Duggan LV , Finestone PJ , Liu R , De Gorter R , Calder LA . Anesthesiology airway-related medicolegal cases from the Canadian Medical Protection Association. Can J Anaesth. 2021 Feb;68(2):183–95. https://doi.org/10.1007/s12630-020-01846-7
5. Cook TM , Woodall N , Frerk C ; Fourth National Audit Project . Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth. 2011 May;106(5):617–31. https://doi.org/10.1093/bja/aer058
6. Cook TM , Woodall N , Harper J , Benger J ; Fourth National Audit Project . Major complications of airway management in the UK: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: intensive care and emergency departments. Br J Anaesth. 2011 May;106(5):632–42. https://doi.org/10.1093/bja/aer059
7. Frerk C , Mitchell VS , McNarry AF , Mendonca C , Bhagrath R , Patel A , et al.; Difficult Airway Society intubation guidelines working group . Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015 Dec;115(6):827–48. https://doi.org/10.1093/bja/aev371
8. Law JA , Duggan LV , Asselin M , Baker P , Crosby E , Downey A , et al.; Canadian Airway Focus Group . Canadian Airway Focus Group updated consensus-based recommendations for management of the difficult airway: part 1. Difficult airway management encountered in an unconscious patient. Can J Anaesth. 2021 Sep;68(9):1373–404. https://doi.org/10.1007/s12630-021-02007-0
9. Law JA , Duggan LV , Asselin M , Baker P , Crosby E , Downey A , et al.; Canadian Airway Focus Group . Canadian Airway Focus Group updated consensus-based recommendations for management of the difficult airway: part 2. Planning and implementing safe management of the patient with an anticipated difficult airway. Can J Anaesth. 2021 Sep;68(9):1405–36. https://doi.org/10.1007/s12630-021-02008-z
10. Apfelbaum JL , Hagberg CA , Connis RT , Abdelmalak BB , Agarkar M , Dutton RP , et al. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022 Jan;136(1):31–81. https://doi.org/10.1097/ALN.0000000000004002
11. Langeron O , Bourgain JL , Francon D , Amour J , Baillard C , Bouroche G , et al. Difficult intubation and extubation in adult anaesthesia. Anaesth Crit Care Pain Med. 2018 Dec;37(6):639–51. https://doi.org/10.1016/j.accpm.2018.03.013
12. Piepho T , Cavus E , Noppens R , Byhahn C , Dörges V , Zwissler B , et al.; German Society of Anesthesiology and Intensive Care Medicine . [S1 guidelines on airway management]. Anaesthesist. 2015 Nov;64(11):859–73. https://doi.org/10.1007/s00101-015-0087-6
13. Higgs A , McGrath BA , Goddard C , Rangasami J , Suntharalingam G , Gale R , et al.; Difficult Airway Society; Intensive Care Society; Faculty of Intensive Care Medicine; Royal College of Anaesthetists . Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth. 2018 Feb;120(2):323–52. https://doi.org/10.1016/j.bja.2017.10.021
14. Cook TM , El-Boghdadly K , McGuire B , McNarry AF , Patel A , Higgs A . Consensus guidelines for managing the airway in patients with COVID-19: Guidelines from the Difficult Airway Society, the Association of Anaesthetists the Intensive Care Society, the Faculty of Intensive Care Medicine and the Royal College of Anaesthetists. Anaesthesia. 2020 Jun;75(6):785–99. https://doi.org/10.1111/anae.15054
15. Quintard H , l’Her E , Pottecher J , Adnet F , Constantin JM , De Jong A , et al. Experts’ guidelines of intubation and extubation of the ICU patient of French Society of Anaesthesia and Intensive Care Medicine (SFAR) and French-speaking Intensive Care Society (SRLF) : In collaboration with the pediatric Association of French-speaking Anaesthetists and Intensivists (ADARPEF), French-speaking Group of Intensive Care and Paediatric emergencies (GFRUP) and Intensive Care physiotherapy society (SKR). Ann Intensive Care. 2019 Jan;9(1):13. https://doi.org/10.1186/s13613-019-0483-1
16. Chrimes N , Higgs A , Law JA , Baker PA , Cooper RM , Greif R , et al. Project for Universal Management of Airways - part 1: concept and methods. Anaesthesia. 2020 Dec;75(12):1671–82. https://doi.org/10.1111/anae.15269
17. Frova G , Sorbello M . Algorithms for difficult airway management: a review. Minerva Anestesiol. 2009 Apr;75(4):201–9.
18. Hofer CK , Wendel Garcia PD , Heim C , Ganter MT . Analysis of anaesthesia services to calculate national need and supply of anaesthetics in Switzerland during the COVID-19 pandemic. PLoS One. 2021 Mar;16(3):e0248997. https://doi.org/10.1371/journal.pone.0248997
19. Henderson JJ , Popat MT , Latto IP , Pearce AC , Difficult Airway S ; Difficult Airway Society . Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia. 2004 Jul;59(7):675–94. https://doi.org/10.1111/j.1365-2044.2004.03831.x
20. Sorbello M , Afshari A , De Hert S . Device or target? A paradigm shift in airway management: implications for guidelines, clinical practice and teaching. Eur J Anaesthesiol. 2018 Nov;35(11):811–4. https://doi.org/10.1097/EJA.0000000000000893
21. Chrimes N . The Vortex: a universal ‘high-acuity implementation tool’ for emergency airway management. Br J Anaesth. 2016 Sep;117 Suppl 1:i20–7. https://doi.org/10.1093/bja/aew175
22. Cook TM . Strategies for the prevention of airway complications - a narrative review. Anaesthesia. 2018 Jan;73(1):93–111. https://doi.org/10.1111/anae.14123
23. Jackson C . The technique of insertion of intratracheal insufflation tubes. Surg Gynecol Obstet. 1913;17:507–9.
24. Janeway H . Intra-tracheal anaesthesia from the standpoint of the nose, throat and oral surgeon with a description of a new instrument for catheterizing the trachea. Laryngoscope. 1913;23(11):1082–90. https://doi.org/10.1288/00005537-191311000-00009
25. Miller Robert A . A NEW LARYNGOSCOPE. Anesthesiology. 1941;2(3):317–20. https://doi.org/10.1097/00000542-194105000-00008
26. Macintosh RR . A NEW LARYNGOSCOPE. Lancet. 1943;241(6233):205. https://doi.org/10.1016/S0140-6736(00)89390-3
27. Levitan RM , Heitz JW , Sweeney M , Cooper RM . The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann Emerg Med. 2011 Mar;57(3):240–7. https://doi.org/10.1016/j.annemergmed.2010.05.035
28. Greenland KB , Eley V , Edwards MJ , Allen P , Irwin MG . The origins of the sniffing position and the Three Axes Alignment Theory for direct laryngoscopy. Anaesth Intensive Care. 2008 Jul;36(1_suppl Suppl 1):23–7. https://doi.org/10.1177/0310057X0803601s05
29. Knill RL . Difficult laryngoscopy made easy with a “BURP”. Can J Anaesth. 1993 Mar;40(3):279–82. https://doi.org/10.1007/BF03037041
30. Kim YS , Song J , Lim BG , Lee IO , Won YJ . Different classes of videoscopes and direct laryngoscopes for double-lumen tube intubation in thoracic surgery: A systematic review and network meta-analysis. PLoS One. 2020 Aug;15(8):e0238060. https://doi.org/10.1371/journal.pone.0238060
31. Kristensen MS , McGuire B . Managing and securing the bleeding upper airway: a narrative review. Can J Anaesth. 2020 Jan;67(1):128–40. https://doi.org/10.1007/s12630-019-01479-5
32. Cooper RM . Use of a new videolaryngoscope (GlideScope) in the management of a difficult airway. Canadian journal of anaesthesia = Journal canadien d'anesthesie. 2003;50(6):611-3.
33. Lewis SR , Butler AR , Parker J , Cook TM , Schofield-Robinson OJ , Smith AF . Videolaryngoscopy versus direct laryngoscopy for adult patients requiring tracheal intubation: a Cochrane Systematic Review. Br J Anaesth. 2017 Sep;119(3):369–83. https://doi.org/10.1093/bja/aex228
34. Zhu H , Liu J , Suo L , Zhou C , Sun Y , Jiang H . A randomized controlled comparison of non-channeled king vision, McGrath MAC video laryngoscope and Macintosh direct laryngoscope for nasotracheal intubation in patients with predicted difficult intubations. BMC Anesthesiol. 2019 Aug;19(1):166. https://doi.org/10.1186/s12871-019-0838-z
35. Cooper RM , Pacey JA , Bishop MJ , McCluskey SA . Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005 Feb;52(2):191–8. https://doi.org/10.1007/BF03027728
36. Desai N , Ratnayake G , Onwochei DN , El-Boghdadly K , Ahmad I . Airway devices for awake tracheal intubation in adults: a systematic review and network meta-analysis. Br J Anaesth. 2021 Oct;127(4):636–47. https://doi.org/10.1016/j.bja.2021.05.025
37. Taylor PA , Towey RM . The broncho-fiberscope as an aid to endotracheal intubation. Br J Anaesth. 1972 Jun;44(6):611–2. https://doi.org/10.1093/bja/44.6.611
38. Cabrini L , Baiardo Redaelli M , Ball L , Filippini M , Fominskiy E , Pintaudi M , et al. Awake Fiberoptic Intubation Protocols in the Operating Room for Anticipated Difficult Airway: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Anesth Analg. 2019 May;128(5):971–80. https://doi.org/10.1213/ANE.0000000000004087
39. Schoettker P , Bathory I , Broome M . Use of the nasotracheal Airtraq to assist difficult nasal fibreoptic intubation. Can J Anaesth. 2008 Dec;55(12):884. https://doi.org/10.1007/BF03034066
40. Core Topics in Airway Management . In: Kristensen MS, Cook T, editors. Core Topics in Airway Management. 3 ed. Cambridge: Cambridge University Press; 2020. p. i-ii.
41. Ramaiah R , Das D , Bhananker SM , Joffe AM . Extraglottic airway devices: A review. Int J Crit Illn Inj Sci. 2014 Jan;4(1):77–87. https://doi.org/10.4103/2229-5151.128019
42. Rosenstock CV , Nørskov AK , Wetterslev J , Lundstrøm LH ; Danish Anaesthesia Database . Emergency surgical airway management in Denmark: a cohort study of 452 461 patients registered in the Danish Anaesthesia Database. Br J Anaesth. 2016 Sep;117 Suppl 1:i75–82. https://doi.org/10.1093/bja/aew190
43. Ahmad I , El-Boghdadly K , Bhagrath R , Hodzovic I , McNarry AF , Mir F , et al. Difficult Airway Society guidelines for awake tracheal intubation (ATI) in adults. Anaesthesia. 2020 Apr;75(4):509–28. https://doi.org/10.1111/anae.14904
44. Campbell M , Shanahan H , Ash S , Royds J , Husarova V , McCaul C . The accuracy of locating the cricothyroid membrane by palpation - an intergender study. BMC Anesthesiol. 2014 Nov;14(1):108. https://doi.org/10.1186/1471-2253-14-108
45. You-Ten KE , Desai D , Postonogova T , Siddiqui N . Accuracy of conventional digital palpation and ultrasound of the cricothyroid membrane in obese women in labour. Anaesthesia. 2015 Nov;70(11):1230–4. https://doi.org/10.1111/anae.13167
46. Kristensen MS , Teoh WH , Rudolph SS . Ultrasonographic identification of the cricothyroid membrane: best evidence, techniques, and clinical impact. Br J Anaesth. 2016 Sep;117 Suppl 1:i39–48. https://doi.org/10.1093/bja/aew176
47. Price TM , McCoy EP . Emergency front of neck access in airway management. BJA Educ. 2019 Aug;19(8):246–53. https://doi.org/10.1016/j.bjae.2019.04.002
48. Cook T , Woodall N , Frerk C . 4th National audit Project of the Royal College of Anaesthetists and the difficult airway society. Major complications of airway management in the United Kingdom London: The Royal College of Anaesthetists. 2011.
49. Onrubia X , Frova G , Sorbello M . Front of neck access to the airway: A narrative review. Trends in Anaesthesia and Critical Care. 2018;22:45–55. https://doi.org/10.1016/j.tacc.2018.06.001
50. Patel A , Nouraei SA . Transnasal Humidified Rapid-Insufflation Ventilatory Exchange (THRIVE): a physiological method of increasing apnoea time in patients with difficult airways. Anaesthesia. 2015 Mar;70(3):323–9. https://doi.org/10.1111/anae.12923
51. Schoettker P . The orotracheal tube dance. Eur J Anaesthesiol. 2015 Jun;32(6):443–4. https://doi.org/10.1097/EJA.0000000000000134
52. Lundstrøm LH , Duez CH , Nørskov AK , Rosenstock CV , Thomsen JL , Møller AM , et al. Effects of avoidance or use of neuromuscular blocking agents on outcomes in tracheal intubation: a Cochrane systematic review. Br J Anaesth. 2018 Jun;120(6):1381–93. https://doi.org/10.1016/j.bja.2017.11.106
53. Warters RD , Szabo TA , Spinale FG , DeSantis SM , Reves JG . The effect of neuromuscular blockade on mask ventilation. Anaesthesia. 2011 Mar;66(3):163–7. https://doi.org/10.1111/j.1365-2044.2010.06601.x
54. Schnittker R , Marshall S , Horberry T , Young KL . Human factors enablers and barriers for successful airway management - an in-depth interview study. Anaesthesia. 2018 Aug;73(8):980–9. https://doi.org/10.1111/anae.14302
55. Schulz CM , Krautheim V , Hackemann A , Kreuzer M , Kochs EF , Wagner KJ . Situation awareness errors in anesthesia and critical care in 200 cases of a critical incident reporting system. BMC Anesthesiol. 2016 Jan;16(1):4. https://doi.org/10.1186/s12871-016-0172-7
56. Bromiley M . The husband’s story: from tragedy to learning and action. BMJ Qual Saf. 2015 Jul;24(7):425–7. https://doi.org/10.1136/bmjqs-2015-004129
57. Fioratou E , Flin R , Glavin R . No simple fix for fixation errors: cognitive processes and their clinical applications. Anaesthesia. 2010 Jan;65(1):61–9. https://doi.org/10.1111/j.1365-2044.2009.05994.x
58. Schmutz JB , Eppich WJ . Promoting Learning and Patient Care Through Shared Reflection: A Conceptual Framework for Team Reflexivity in Health Care. Acad Med. 2017 Nov;92(11):1555–63. https://doi.org/10.1097/ACM.0000000000001688
59. Rudolph JW , Raemer DB , Simon R . Establishing a safe container for learning in simulation: the role of the presimulation briefing. Simul Healthc. 2014 Dec;9(6):339–49. https://doi.org/10.1097/SIH.0000000000000047
60. Konradt U , Otte KP , Schippers MC , Steenfatt C . Reflexivity in Teams: A Review and New Perspectives. J Psychol. 2016;150(2):153–74. https://doi.org/10.1080/00223980.2015.1050977
61. Schmutz JB , Eppich WJ . When I say … team reflexivity. Med Educ. 2019 Jun;53(6):545–6. https://doi.org/10.1111/medu.13768
62. Eppich W , Cheng A . Promoting Excellence and Reflective Learning in Simulation (PEARLS): development and rationale for a blended approach to health care simulation debriefing. Simul Healthc. 2015 Apr;10(2):106–15. https://doi.org/10.1097/SIH.0000000000000072
63. Rudolph JW , Simon R , Rivard P , Dufresne RL , Raemer DB . Debriefing with good judgment: combining rigorous feedback with genuine inquiry. Anesthesiol Clin. 2007 Jun;25(2):361–76. https://doi.org/10.1016/j.anclin.2007.03.007
64. Chrimes N , Bradley WP , Gatward JJ , Weatherall AD . Human factors and the ‘next generation’ airway trolley. Anaesthesia. 2019 Apr;74(4):427–33.
65. Fuchs A , Haller M , Riva T , Nabecker S , Greif R , Berger-Estilita J . Translation and application of guidelines into clinical practice: A colour-coded difficult airway trolley. Trends in Anaesthesia and Critical Care. 2021;40:46–54. https://doi.org/10.1016/j.tacc.2021.06.007
66. Sturgess DJ , Greenland KB , Senthuran S , Ajvadi FA , van Zundert A , Irwin MG . Tracheal extubation of the adult intensive care patient with a predicted difficult airway - a narrative review. Anaesthesia. 2017 Feb;72(2):248–61. https://doi.org/10.1111/anae.13668
67. Popat M , Mitchell V , Dravid R , Patel A , Swampillai C , Higgs A ; Difficult Airway Society Extubation Guidelines Group . Difficult Airway Society Guidelines for the management of tracheal extubation. Anaesthesia. 2012 Mar;67(3):318–40. https://doi.org/10.1111/j.1365-2044.2012.07075.x
68. Corso RM , Sorbello M , Mecugni D , Seligardi M , Piraccini E , Agnoletti V , et al. Safety and efficacy of Staged Extubation Set in patients with difficult airway: a prospective multicenter study. Minerva Anestesiol. 2020 Aug;86(8):827–34. https://doi.org/10.23736/S0375-9393.20.14105-1
69. Casso G , Schoettker P , Savoldelli GL , Azzola A , Cassina T . Development and Initial Evaluation of a Novel, Ultraportable, Virtual Reality Bronchoscopy Simulator: The Computer Airway Simulation System. Anesth Analg. 2019 Nov;129(5):1258–64. https://doi.org/10.1213/ANE.0000000000003316
70. Zoric L , Savoldelli GL . Evidence base in airway management training. Trends in Anaesthesia and Critical Care. 2015;5(1):36–41. https://doi.org/10.1016/j.tacc.2014.12.002
We wish to thank the Espace Saint-François (www.esf.ch) for its support in graphical communication and the Center for Medical Simulation (www.harvardmedsim.org) for their insightful advice.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
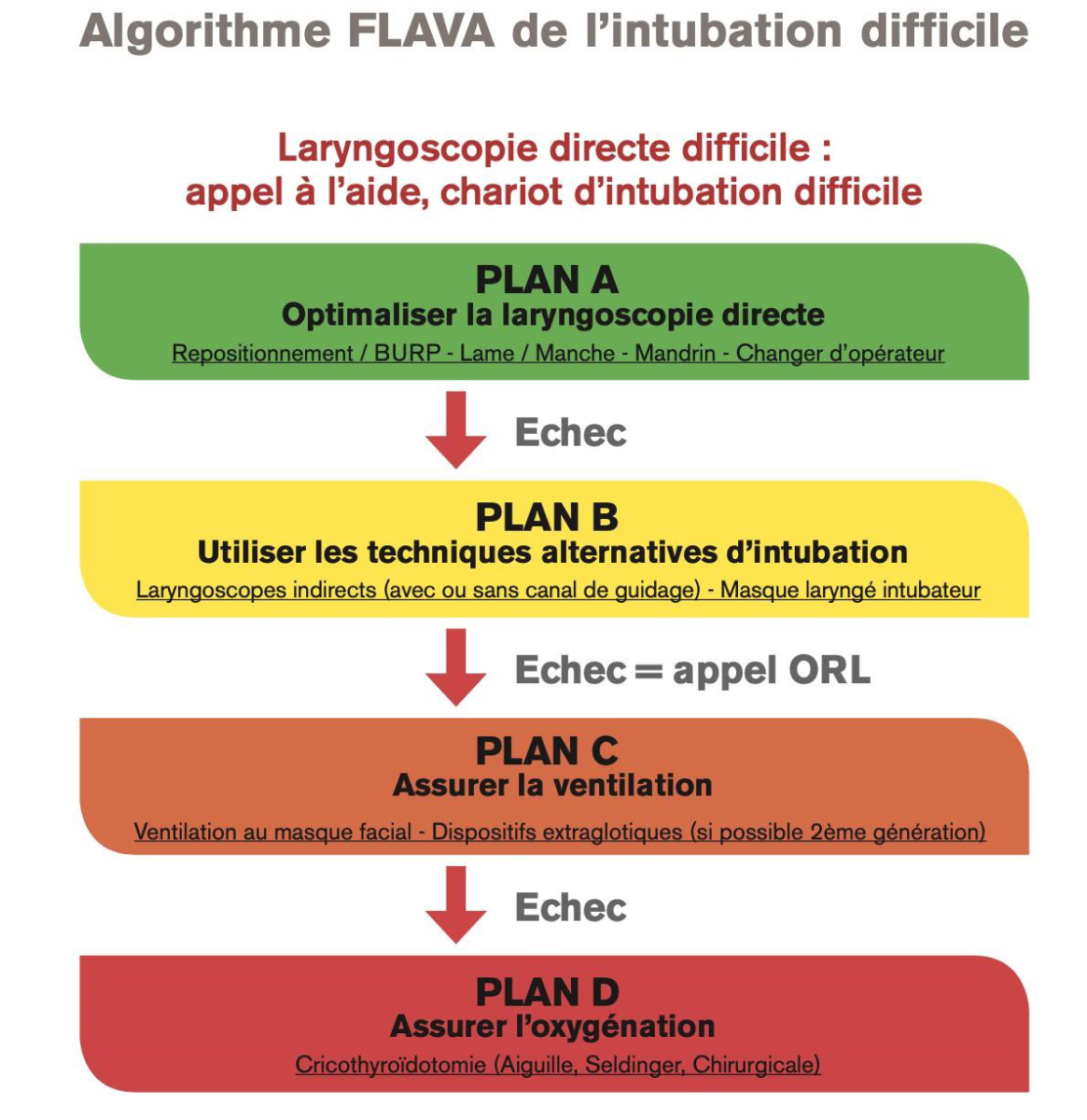
Figure S1 The 2013 FLAVA algorithm for unexpected difficult tracheal intubation (French version).
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.