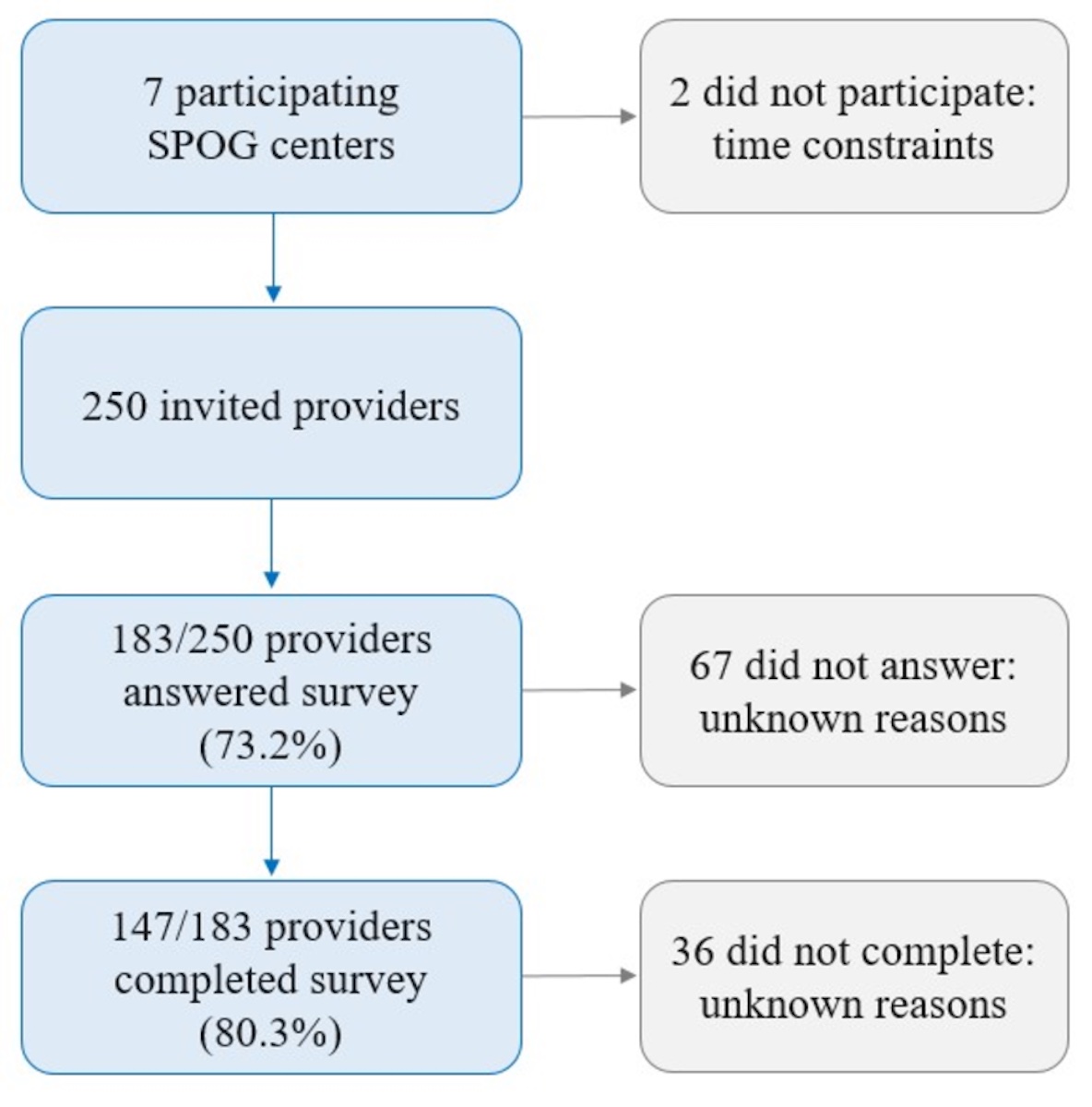
Figure 1 Flow chart of recruitment. SPOG: Swiss Paediatric Oncology Group
DOI: https://doi.org/10.4414/SMW.2022.w30223
In Switzerland, the proportion of permanent residents with foreign nationality reached 26% in 2019 [1]. Although the majority come from the European Union / European Free Trade Association (EU/EFTA) countries (65.9%; e.g., Italy 14.8%, Germany 14.1%), more than one in six come from other continents (17.1%; e.g., Asia and Oceania 8.0%, Africa 6.4%) and non-EU European countries (17.0%; e.g., Kosovo 5.2%, Northern Macedonia 3.1%) [1]. Among permanent residents older than 15 years of age, 37% have a migration background, which covers foreign and naturalised citizens as well as children of foreign citizens [2]. In the group of child and adolescent permanent residents, 27% of children younger than 15 years of age have a foreign nationality, with a significant proportion from the Balkans and a greater proportion from EU countries [3, 4]. Lastly, foreign residents accounted for 11.6% of all childhood cancer cases between 2014 and 2018 [5].
Studies indicate that the population with a migration background in Switzerland exhibits higher rates of health problems [6, 7]. Related to this, severe barriers to healthcare access for migrant children have been described for the Swiss context [8]. Reasons for these health problems are: migration-related factors, such as traumatic experiences; socioeconomic situation, such as a lower level of income and education; poor health literacy, such as limited knowledge of the healthcare system; or the structuring of the healthcare system, such as insufficient consideration of the needs of the migrant population [6]. It is known that paediatric healthcare providers in Swiss settings face difficulties due to language barriers and different cultural backgrounds of families [6, 8]. Acquiring cross-cultural competences is crucial for understanding the patient's cultural context, as well as providing effective and culturally safe healthcare [6, 8—10]. Developing cross-cultural competence means adopting and understanding the features of one’s own culture, developing a positive attitude to other cultural groups, and increasing the ability to understand and interact with the latter [11]. Ultimately, cross-cultural competence facilitates culturally congruent care, a process through which families’ needs and preferences are aligned with providers’ knowledge, attitudes and skills, thereby recognising that care actualises as a result of dynamic interactions between families and providers [12].
For the paediatric setting (including oncology), various studies have evidenced that cultural barriers to decision-making are present [9, 13—16]. For example, different cultural and religious values between healthcare providers and families are seen as major barriers to palliative care provision in paediatric oncology [17, 18]. Similarly, recent Swiss studies in palliative care in paediatric oncology revealed difficulties due to cultural aspects, such as families’ religiously determined understanding of illness and late palliative care initiation [9, 19]. Another study showed that paediatric oncology providers were not aware of their own stereotypes and prejudices or their impact on care [20]. Moreover, it is known that adult cancer patients decline, or delay, care because of a perceived lack of cross-cultural competence on the part of healthcare providers [21]. It is therefore not surprising that European guidelines in paediatric oncology refer to cultural needs of children and families that have to be addressed through culturally competent care, and see cultural barriers as a main reason for shortcomings in the provision of paediatric palliative care [22, 23]. Improving cross-cultural competence is all the more urgent as children from some migrant groups may have distinct health needs, such as psychological problems, and often already face unique challenges of acculturation [7, 24]. The imperative to study barriers to culturally equitable paediatric oncology care in Switzerland is both an ethical and a medical one because access to healthcare is a fundamental human right [25], not to mention that good health of migrant children benefits population health [7]. Finally, many migrant children face different layers of vulnerability (e.g., worse psychological health, parents’ increased risk to be affected by poverty, or precarious working). Health systems should strive to minimise these vulnerabilities [26].
That there are numerous Swiss initiatives, is further testimony to the need and national ambition to adapt to demographic trends and work towards cultural equity in healthcare. Recognising cultural and communication difficulties in Swiss healthcare, the “National Programme on Migration and Health” recommends the integration of cross-cultural competence into training of health professions [6]. Along similar lines, the Swiss initiative “Swiss Hospitals for Equity” is dedicated to the challenge of “ensuring a high level of patient safety and quality of care in view of increasing patient diversity” [27]. Against this backdrop, our study aimed to examine the cross-cultural competence of Swiss paediatric oncology care providers using a validated survey: the Cross-Cultural Competence of Healthcare Professionals (CCCHP) questionnaire [28].
We surveyed paediatric oncology care providers to capture their cross-cultural competence and perceptions so as to facilitate cross-culturally competent care. This exploratory quantitative study was part of a larger project on barriers to culturally equitable paediatric oncology care in Switzerland, which was funded by the Swiss Cancer League (project number: KLS 4822-08-2019). The responsible ethics committee, the Ethikkommission Nordwest- und Zentralschweiz, noted that the study does not fall inside the scope of the Swiss Human Research Act (Art. 2), because we intended to survey health professionals and to collect data anonymously. Moreover, the EKNZ noted that the study fulfils the general ethical and scientific standards for research with humans (Req-2020-01391). Furthermore, the University of Basel’s data protection office approved the online survey tool.
We defined our study population as all Swiss paediatric oncology care providers. Thus, the only inclusion criterion was that providers were caring for paediatric cancer patients. Paediatric oncology care providers included all occupational groups who are in direct contact with patients and are involved in care, for example, nurses, physicians, psycho-oncologists, social workers or physiotherapists.
In Switzerland, there are nine Swiss Paediatric Oncology Group (SPOG) stations, six in the German-speaking, two in the French-speaking and one in the Italian-speaking language region. All SPOG stations provide care for children (0—18 years) along the entire cancer trajectory. Based on existing collaborations with the heads of the SPOG stations, we approached all nine SPOGs, introduced the study by a formal letter, and presented our study during a virtual SPOG research council meeting. Seven SPOG stations agreed to participate in the study. Subsequently, we sent the survey-link, along with a description of the study objectives, to the collaborators (heads of departments or senior physicians) who shared the link with their colleagues (i.e., providers). In addition, we checked with each of the seven collaborators from the respective SPOG stations whether all eligible providers had received the link, which the collaborators confirmed. The data collection period was three weeks (13 January to 3 February 2021). After one week, the collaborators sent a reminder.
Using the German online survey tool “soscisurvey” (soscisurvey.de), we created an online version of the CCCHP (in German, French, and Italian). Additionally, we included sociodemographic (e.g., age) and professional variables (e.g., work experience) as well as open items on barriers to and facilitators of cross-culturally competent care. Besides the overall scale (α = 0.87), the 27 items of the CCCHP capture five subscales of cross-cultural competence: motivation/curiosity (α = 0.84), attitudes (α = 0.78), skills (α = 0.68), knowledge/awareness (α = 0.54) and emotions/empathy (α = 0.69); CCCHP’s internal consistency, as indicated by Cronbach's alpha, is mostly very good, good, and moderate [28]. CCCHP’s underlying conceptual framework was derived from an expert survey, interviews with providers and a broad narrative review on assessment instruments and conceptual models of cultural competence [28]. The CCCHP has been validated in German (i.e., for the biggest language region in Switzerland; six SPOG stations) and Finnish [29, 30], but not in French or Italian (i.e., the other two major Swiss language regions; two SPOG stations in the French-speaking language region and one SPOG station in the Italian-speaking language region). We therefore used the CCCHP for the German-speaking language region and translated it into French and Italian, using translation and retranslation. More precisely, two senior researchers from the first author’s institute translated the CCCHP. Both researchers have extensive research and translation experience in the Swiss oncology setting. Finally, a group of researchers from the first authors' institute (doctoral students and postdocs) re-evaluated both translations and checked them for accuracy and correctness. The study tool was pilot tested by three providers. We made minor language adjustments, which did not change the overall structure.
We analysed the data using statistical software SPSS.26 (SSPS Inc., Chicago, IL). We performed descriptive statistics (mean, median, mode, proportions) to summarise providers’ sociodemographic and professional characteristics, and inferential statistics (multivariate analysis of variance [MANOVA] including post-hoc tests, correlation analysis) to compare occupational groups’ cross-cultural competence. Statistical significance level was set at p<0.05. In addition to quantitative analysis, we used content analysis to qualitatively analyse open items on barriers to and facilitators of cross-culturally competent care and to determine the presence and frequency of certain codes [31]. Content analysis involved several steps, namely, collecting all responses to open items, familiarising with the data, inductive development of a category system, determining presence and frequency of codes.
Seven of nine SPOG stations agreed to participate: four (out of six) from the German-speaking language region, two (out of two) from the French-speaking language region, one (out of one) from the Italian-speaking language region of Switzerland. The remaining two SPOG stations from the German-speaking language region did not participate owing to time constraints. In total, we invited 250 paediatric oncology care providers to complete the survey. The response rate was 73.2% (n = 183/250). The completion rate was 80.3% (147/183), which means that almost one in five providers did not complete the entire survey, resulting in missing values (fig. 1). It has to be noted that missing data can vary across items. We did not account for missing data.
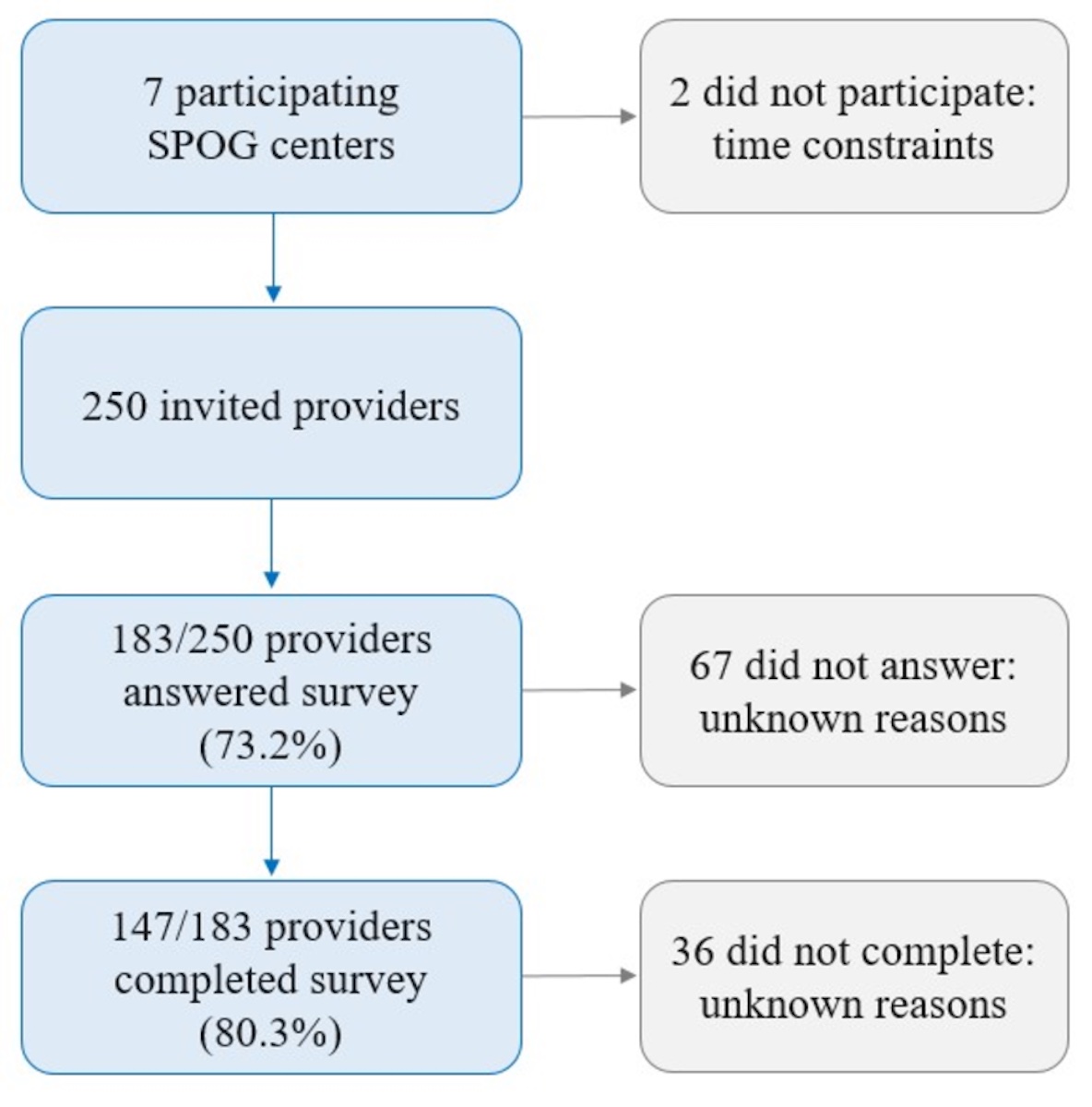
Figure 1 Flow chart of recruitment. SPOG: Swiss Paediatric Oncology Group
Of the participating providers, 84% were women, 67% worked in the German-speaking language region, and 45% were not or little religious. The sample of the participating providers was composed of the following occupational groups (n = 147): nurses (41.5%), physicians (25.9%), occupational therapists and physiotherapists (8.2%), social workers (7.5%), psycho-oncologist (4.8%), and other groups (12.1%; study nurse, educators, music-therapist, dieticians, neuro-psychologists, pastoral workers, animator, medical assistant, pharmacist, administrative staff). Mean work experience was 11.5 years (n = 147, range 0.5–35 years, median 10 years, mode 10 years). Three out of four providers’ country of origin was Switzerland. Further information is presented in table 1.
Table 1Socio-demographic characteristics.
| Age (n = 146) | M = 42.1 (SD = 10.4), Mdn = 42, Mo = 35, Min = 23, Max = 64 |
| Gender (n = 147) | 83.7% women, 16.3% men |
| Language region (n = 147) | 67.3% German, 25.9% French, 6.8% Italian |
| Country of origin (n = 147) | 72.8% Swiss, 21.1% EU, 6.1% non-EU |
| Religiosity1 (N = 147) | 44.9% not/little (1—3), 29.9% moderately (4—7), 25.2% strongly (8—10) |
EU: European Union; M; mean; Mdn: median; Mo mode; Min: minimum; Max maximum; SD: standard deviation. 11-item scale, 10-point Likert item ranging from 1 (not religious) to 10 (religious).
Agreement and disagreement with the 27 single items of the CCCHP (percentages of provider responses on the five-point Likert items) are presented in figure 2. With the exception of one sub-scale (αknowledge/awareness = 0.557), reliability of the overall CCCHP scale and the subscales was mostly good and moderate (αoverall = 0.810, αmotivation/curiosity = 0.728, αattitudes = 0.690, αskills = 0.680, αemotions/empathy = 0.680).
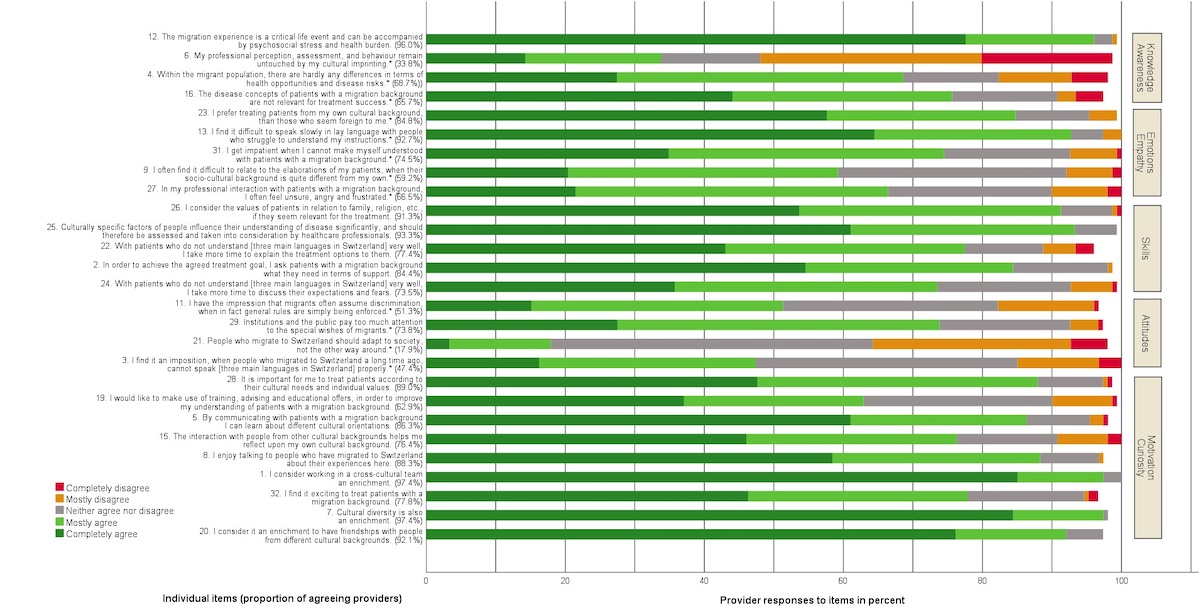
Figure 2 Agreement and disagreement with the 27 items of the Cross-Cultural Competence of Healthcare Professionals (CCCHP) questionnaire.
We conducted multivariate analysis of variance among the four main occupational groups (nurses, physicians, occupational therapists and physiotherapists, social workers) for the overall CCCHP scale and the subscales. We could not include all occupational groups because some were small (e.g. music therapist, dietician). Analysis revealed that there were significant effects of occupational groups on the overall scale - F(3,118) = 7.991, p = 0.000, and the following four subscales: attitudes - F(3,118) = 4.913, p = 0.003; skills - F(3,118) = 9.629, p = 0.000; emotions and empathy - F(3,118) = 4.330, p = 0.006; knowledge and awareness - F(3,118) = 4.366, p = 0.006. Besides, the four occupational groups did not differ significantly regarding their social desirability scores. Post-hoc tests (Bonferroni) were performed to determine which occupational groups differed significantly from one another (fig. 3).
Overall: physicians (p = 0.017) and social workers (p = 0.000) had higher cross-cultural competence scores than nurses; social workers had higher scores than occupational therapists and physiotherapists (p = 0.003). Attitudes: both physicians (p = 0.035) and social workers (p = 0.011) had significantly higher scores than nurses. Skills: occupational therapists and physiotherapists had significantly lower scores than all three other groups, namely nurses (p = 0.001), physicians (p = 0.000), social workers (p = 0.000). Emotions/empathy: social workers had significantly higher scores than all three other groups, namely nurses (p = 0.020), physicians (p = 0.004), occupational therapists and physiotherapists (p = 0.023). Knowledge/awareness: physicians had significantly higher scores than nurses (p = 0.005).
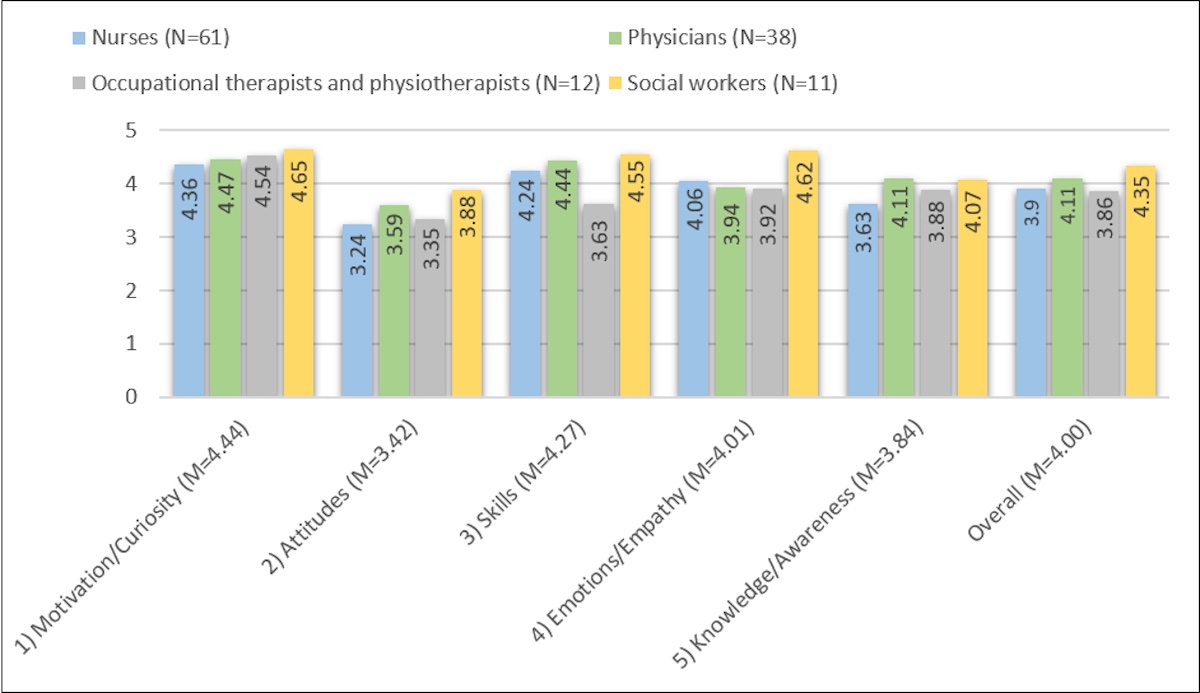
Figure 3 Means for Cross-Cultural Competence of Healthcare Professionals (CCCHP) scales.
In addition, we determined paediatric oncology care providers’ (highest and least) degree of agreement as indicated by the proportion of providers who completely or strongly (dis-)agreed with individual items to provide a more nuanced understanding of their responses that goes beyond aggregated subscale scores (table 2).
Table 2Paediatric oncology care providers’ highest and least agreement with individual items.
| Highest agreement | ||
| Positive items | 97.4% (item 7) | “Cultural diversity is also an enrichment.” |
| 97.4% (item 1) | “I consider working in a cross-cultural team an enrichment.” | |
| 96.0% (item 12) | “The migration experience is a critical life event and can be accompanied by psychosocial stress and health burden.” | |
| Negative items | 92.7% (item 13) | “I find it difficult to speak slowly in lay language with people who struggle to understand my instructions.” |
| 84.8% (item 23) | “I prefer treating patients from my own cultural background, than those who seem foreign to me.” | |
| 75.7%, (item 16) | “The disease concepts of patients with a migration background are not relevant for treatment success.” | |
| Least agreement | ||
| Positive items | 62.9% (item 19) | “I would like to make use of training, advising and educational offers, in order to improve my understanding of patients with a migration background.” |
| 73.5% (item 24) | “With patients who do not understand [three main languages in Switzerland] very well, I take more time to discuss their expectations and fears.” | |
| 76.4% (item 15) | “The interaction with people from other cultural backgrounds helps me reflect upon my own cultural background.” | |
| Negative items | 17.9% (item 21) | “People who migrate to Switzerland should adapt to society, not the other way around.” |
| 33.8% (item 6) | “My professional perception, assessment, and behaviour remain untouched by my cultural imprinting.” | |
| 51.3% (item 11) | “I have the impression that migrants often assume discrimination, when in fact general rules are simply being enforced.” | |
Paediatric oncology care providers described the main barriers to, and facilitators of, cross-culturally competent care using open items (table 3). Among all barriers mentioned (n = 130), language barriers (68.5%), different culture and values (19.2%), and different illness understanding (9.2%) were most frequently mentioned. The most frequently mentioned facilitators (n = 125) were professional translators (47.2%), continuous training (20.8%) and the use of professional cultural mediators (8.8%). Time was rarely a major barrier (2.3%) or facilitator (5.6%).
Table 3Main barriers to and facilitators of cross-culturally competent care.
| Barriers to cross-culturally competent care | |
| 68.5% (n = 89) | Language barriers: "For me, language is the biggest challenge. Often, due to language barriers, only technical/objective keywords can be communicated (on both sides). Emotions and humour are often lost." |
| 19.2% (n = 25) | Different culture and values: "Especially in the diversity of the many intercultural, religious and related biographical contexts, which we as individuals and often also as a team, despite our will and our pediatric motivation, (can) only do justice to a limited extent to." |
| 9.2% (n = 12) | Different understanding of illness: "The understanding of their illness, particularly serious illnesses, and their position in regard to the end of life." |
| 8.5% (n = 11) | Lack of trust and respect: "In individual cases, the counterpart with a migrant background (tends to depend more on the educational level of the parents than on the culture) behaves uncooperatively and hides behind their own culture/tradition, which can lead to a stalemate.»«Less respect/authority towards women as healthcare providers." |
| 3.8% (n = 5) | Translators not available: "Availability of interpreters (not just translators)." |
| 2.3% ( = 3) | Lack of time: "To have enough time." |
| Facilitators of cross-culturally competent care | |
| 47.2% (n = 59) | Professional translators: "Very easy access to translators of the same culture, who must be well trained in "medical" translation, which must also include this cultural and social care." |
| 20.8% (n = 26) | Continuous training in this area: "Regular (e.g., once a year) workshops on transculturality in the hospital context." |
| 8.8% (n = 11) | Cultural mediators: "In the case of unfamiliar cultures and if communication with parents/patient is poor in terms of language, an interdisciplinary roundtable discussion with a cultural mediator would be helpful." |
| 5.6% (n = 7) | More time: "Have more time than allowed to meet challenges." |
We determined whether paediatric oncology care providers’ cross-cultural competence was associated with the following characteristics: age, gender, work experience, language region, country of origin, religiosity [32]. Since we tested the overall hypothesis of a relationship between a demographic variable and cross-cultural competence through multiple correlations (five CCCHP-subscales), we had to control for the increased likelihood of a type I error and thus adjusted the alpha level by applying the Bonferroni-Holm correction [33, 34]. After Bonferroni-Holm correction, no correlation was significant (supplementary table S1 in the appendix).
We aimed to investigate the cross-cultural competence of Swiss paediatric oncology care providers. Our sample represented the distribution of language regions in Switzerland (sample: 67.3% German, 25.9% French, 6.8% Italian; Switzerland: 62.6% German, 22.9% French, 8.2% Italian) [35]. Our response rate (73.2%) surpasses similar studies from Switzerland (41.2%) [36], the US (31.2%) [37] or Finland (44.3%) [30] and can be considered good, especially for the paediatric setting [38]. Overall, social workers’ cross-cultural competence was higher than nurses’ and occupational therapists' and physiotherapists'. Physicians’ cross-cultural competence was higher than nurses’. Our analysis revealed noteworthy differences among the four occupational groups on the five subscales. Physicians and social workers had more positive attitudes than nurses; occupational therapists and physiotherapists had lower skills than the other three groups. Social workers scored higher on the emotions/empathy subscale than the other three groups. Physicians were more knowledgeable and aware than nurses. Since one strength of the CCCHP is its potential to identify starting points for further development of cross-cultural competence [28], these differences provide first points of leverage for training to enhance specific competences for particular occupational groups.
With respect to cross-cultural motivation, occupational groups did not differ significantly from one another. All paediatric oncology care providers exhibited a strong “motivation to provide culturally responsive care”, much “curiosity to engage in cross-cultural encounters,” and a “wish to enrich their understanding in working with culturally different populations” [28, p11]. This is to be welcomed as a literature review pointed out that motivation is a prerequisite for implementing effective cross-cultural competence training [39].
Both physicians and social workers had more positive cross-cultural attitudes than nurses. This subscale captures “tolerance, valuing and respecting differences, and [has] a positive orientation towards other cultures and cultural diversity” [28, p11]. Physicians’ positive attitudes have been described in another Swiss study which found that,despite perceiving communication with migrant patients as less effective and less satisfactory, physicians frequently relied on interpreters and appreciated their dual role as interpreters and cultural mediators, but still lamented their own inability to communicate more directly with patients [40]. Physicians and nurses work closely with patients and family members regarding treatment, whereas social workers work as care managers, for example, helping families with work issues, finances and support systems. This could enable them to observe the difficulties that patients and their families face in their daily lives in the healthcare setting and make them sympathise with the patients and their families, ultimately shaping their positive attitudes.
Occupational therapists and physiotherapists had less cross-cultural skills than the other three occupational groups. Given that this subscale considers providers’ “adaptability in meeting the (cultural) needs of their patients, professionals’ communicative competence and to make time for their patients” [28, p11], this finding should be interpreted cautiously. These aspects may play a less central role in occupational therapists and physiotherapists’ work. Nevertheless, this is not to say that patients and families with a different cultural background could not benefit from improved cross-cultural skills on the part of occupational therapists and physiotherapists. The other three occupational groups (nurses, physicians, social workers) appear to be equally skilled in meeting the cultural needs of patients and their families. With regard to Swiss frontline providers’ skills, a study found that physicians’ self-assessed cross-cultural skillfulness was higher than nurses’ [36]. In light of this finding, the authors expressed surprise, as nurses in Switzerland traditionally have emphasised the need to improve cross-culturally competent care. The difference was attributed to, amongst others, nurses’ reduced access to training as a result of historical inequalities between the two occupational groups [41]. Hence our result, namely no difference between physicians and nurses, could be explained by enhanced access to training on the part of nurses. Nurses’ enhanced access to training has been acknowledged by a paediatric oncology nurse in a Swiss focus group study [9].
Social workers had higher scores on the emotions/empathy subscale than the other three occupational groups. This subscale refers to “feelings and emotional reactions towards diversity, with being comfortable with difficulties arising in cross-cultural encounters and with being multicultural empathic” [28, p11]. This finding is a bit surprising since it has been lamented that social workers are not yet fully prepared to work in an increasingly diverse environment [42]. Again, social workers’ daily work with patients and their families might render them more likely to be familiar with difficulties due to differing cultural backgrounds, to be comfortable with such difficulties and to respond with empathy.
Physicians had a higher level of cross-cultural knowledge/awareness than nurses. This subscale measures “cultural and migration-specific knowledge, an understanding of concepts of illness and health, and awareness of one’s own perceptions and values” [28, p11]. Again, such discrepancies have been seen as a direct consequence of nurses having less access to training resources [36]. However, our finding that nurses’ cross-cultural skills were comparable to physicians’ suggests enhanced access to training on the part of nurses over the past years, which was also shown by a Swiss focus group study [9]. Therefore, the finding that nurses’ cross-cultural knowledge/awareness was still lower than physicians’ may indicate that the training improved nurses’ skills more effectively than their knowledge/awareness. Another explanation could be that nurses’ knowledge/awareness, due to a lack of pre-employment training during their studies, might have been less than physicians’ at the beginning of their respective careers and hence the received training could not entirely make up for this pre-existing deficit on the part of nurses [9]. As such, this finding points toward a possibility to focus on this particular dimension of cross-cultural competence, not only in postgraduate training, but also in nursing curricula.
In our sample, the highest subscale means were motivation/curiosity (4.44) and skills (4.27); the lowest were attitudes (3.42) and knowledge/awareness (3.84). Thus, on the one hand Swiss paediatric oncology care providers appeared to possess high motivation to provide cross-culturally competent care and the skills to meet cultural needs of their patients and families. On the other hand, providers appeared to lack cultural and migration-specific knowledge, as well as awareness of their own preconceptions and, sometimes, to hold negative attitudes towards other cultures and cultural diversity. For example, more than one third of paediatric oncology care providers believed that their “professional perception, assessment, and behaviour remain untouched by [their] cultural imprinting” (item 6, knowledge/awareness) and more than half had the impression “that migrants often assume discrimination, when in fact general rules are simply being enforced” (item 11, attitudes).
Similar results were obtained by a US study in which paediatric oncology nurses’ motivation was highest and knowledge was lowest [43]. Another US study showed that 3 out of 10 paediatric physicians indicated unpreparedness to provide care for patients whose beliefs or practices are at odds with western medicine, or who distrust the health system [16]. Taken together, these findings suggest that providers are often highly motivated to develop cross-cultural competence, but that their knowledge and – to a smaller extent – awareness is often limited. Fortunately, there is empirical evidence of the effectiveness of cross-cultural training in paediatrics, suggesting that knowledge and awareness can be significantly improved [44, 45].
Overall, cross-cultural training was shown to advance cross-cultural competence of paediatric oncology care providers, such as communication skills, delivery of care, interaction with interpreters, or knowledge [44, 46]. A recent scoping review, however, concluded that “effects of interventions beyond practitioner knowledge and attitudes remain unclear” [45, p1]. In fact, our findings mandate a nuanced approach to training that takes into consideration, and purposely targets, the differences among occupational groups of paediatric oncology care providers on the various subscales. A general recommendation to provide the same cross-cultural training for all occupational groups might not do full justice to the pattern of inter-occupational variance. For example, nurses may benefit more from knowledge training than physicians (since the former’s is lower than the latter’s), social workers may benefit less from training that focuses on emotions/empathy than physicians (since the former’s is higher than the latter’s). Specifically tailored training, workshops and interventions should therefore be implemented. Notably, almost 4 out of 10 providers in our sample did not want to make use of training to improve their cross-cultural competence (item 19, motivation/curiosity), highlighting the need to tailor training and interventions to particular occupational groups’, if not to individual providers’ preferences. Apart from training, a cross-cultural mediator accompanying the team on a daily basis can benefit the relationship between families and providers [47].
Besides training, implementing checklists for culturally competent care could be a good way forward. In the Swiss palliative care context, such aids exist for adult patients and their families [48]. Covering the areas of symptoms, decision-making, network organisation, and support for families, they incorporate questions relevant to treatment and care, and supplement existing assessment instruments by adding migration-specific aspects. Furthermore, against the backdrop of interoccupational differences on the various cross-cultural subscales, reciprocal supervision and regular exchange within multidisciplinary teams is crucial. In this way, paediatric oncology care providers can learn from each other, as well as ensuring that existing resources are being used in a cost-effective way.
Language barriers represented the most frequently cited barrier to cross-culturally competent care, which is why paediatric oncology care providers' demands for more professional translators need to be heard. In some cases, cultural mediators could provide additional support in explaining differing cultural concepts of health, illness and care. The Swiss Medical Association has described professional interpreters as “a key to health equality”. Our analysis of subscale differences between the two main occupational groups in our sample (physicians: 25.9%, nurses: 41.5%) demonstrated that physicians exhibited more positive cross-cultural attitudes and more cross-cultural knowledge/awareness. In the face of similar results (i.e., nurses’ lower self-assessed skillfulness), authors of a Swiss study hypothesised that nurses are more self-aware and have higher expectations of themselves than physicians, who are less likely to report limited competency [36]. In fact, higher self-assessed skillfulness ratings on the part of those with less formal training on the respective competences have been observed elsewhere [49]. Also, nurses are often confronted with work overload due to, for example, understaffing, resulting in less time and resources to attend cross-cultural competence training, despite their intention to improve their cross-cultural knowledge [9]. The discrepancy between these two occupational groups merits further careful examination given the centrality of nurses to advancing the health and well-being of patients and their families. Lastly, when asked explicitly, more than half of providers agreed that their professional behaviour is affected by their cultural values (item 6, fig. 2). However, this theme did not come up in providers’ responses to the open item on barriers to cross-culturally competent care. This is possibly indicative of providers’ implicit tendency to attribute barriers to factors outside of themselves. Related to this, it has been shown that providers have more difficulty in thinking of themselves as cultural beings than of their patients [50].
First, social desirability could have biased providers’ responses. Indeed, social desirability was positively associated with three subscales: motivation/curiosity (r = 0.295, p = 0.000), skills (r = 0.373, p = 0.000) and emotions/empathy (r = 0.499, p = 0.000). However, occupational groups did not differ significantly regarding their social desirability scores and hence social desirability influenced providers’ responses equally. Moreover, anonymity of data collection contributed to minimising social desirability bias. Second, paediatric oncology care providers could have overestimated their cross-cultural competence [50]. Nevertheless, if all occupational groups equally overestimated their competences, results can be interpreted accurately. Third, paediatric oncology care providers with an interest in, or a strong opinion on, the topic might be overrepresented. However, this does not invalidate our findings. On the contrary, this means that even among providers who are interested and more competent there is room for improvement. Fourth, due to small population size, sample sizes for some providers, such as psycho-oncologists, music therapists, and dieticians, were small. Finally, the largest SPOG station did not participate in this study, which could represent a bias.
Culturally diverse countries such as Switzerland are confronted with the challenge of, and imperative to, provide cross-culturally competent care. Training and interventions are widely considered a principal strategy to advance providers’ cross-cultural competence, at least for cross-cultural knowledge, attitudes and skills [45]. In light of differently effective interventions for different dimensions of cross-cultural competence, our findings of differences among occupational groups in paediatric oncology lend additional support to the need to adapt training and interventions to the particular occupational group. Furthermore, reciprocal supervision and the promotion of multidisciplinary teams is crucial to enable oncology care providers to learn from each other and this exchange could also help to reduce some of the differences between the various occupational groups. Finally, it is important to elaborate the training with regard to the respective dimension(s) of cross-cultural competence. Doing so increases the likelihood of enhancing cross-cultural competence. Apart from provider training and interventions, additional seconding strategies to improve quality of care have to be followed, not only for culturally diverse populations, for example, further implementation of professional interpreters and cultural mediators, or intra-team supervision and exchange. Ultimately, as the social anthropologist Dagmar Domenig rightly points out: “the transcultural transformation of the health system has not only positive effects on work with migrants, [but also for other] patients who (…) benefit from (...) more adapted treatment that is appropriate for their individual way of life and has regard for their personal and social suffering” [41, p215].
Data are available from the authors upon reasonable request.
The authors greatly appreciate all SPOG healthcare professionals who participated in the questionnaire study.
Author contributions: Michael Rost and Bernice S. Elger contributed to the study conception and design. Milenko Rakic and Michael Rost performed material preparation, data collection and analysis. Milenko Rakic and Michael Rost wrote the first draft of the manuscript. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
The Swiss Cancer League (Grant number KFS-4822-08-2019) funded this study.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
Table S1Exploratory correlation analyses (Pearson, Spearman, point-biserial correlations).
| Age 1 | Gender | Work experience 2 | Language region 3 | Country of origin 4 | Religiosity 5 | ||
| Motivation | Coefficient | 0.001 | 0.085 | 0.077 | 0.072 | 0.006 | 0.016 |
| Unadjusted sig. | 0.989 | 0.308 | 0.356 | 0.385 | 0.472 | 0.851 | |
| n | 146 | 147 | 146 | 147 | 147 | 147 | |
| Attitudes | Coefficient | 0.029 | 0.003 | 0.214* | 0.023 | 0.180* | 0.085 |
| Unadjusted sig. | 0.732 | 0.972 | 0.010 | 0.781 | 0.015 | 0.306 | |
| n | 146 | 147 | 146 | 147 | 147 | 147 | |
| Skills | Coefficient | 0.132 | 0.029 | 0.109 | 0.027 | 0.030 | 0.132 |
| Unadjusted sig. | 0.113 | 0.728 | 0.190 | 0.750 | 0.357 | 0.110 | |
| n | 146 | 147 | 146 | 147 | 147 | 147 | |
| Emotions Empathy | Coefficient | 0.087 | 0.081 | 0.115 | 0.155 | 0.007 | 0.141 |
| unadjusted Sig. | 0.297 | 0.331 | 0.166 | 0.060 | 0.466 | 0.089 | |
| N | 146 | 147 | 146 | 147 | 147 | 147 | |
| Knowledge Awareness | Coefficient | 0.085 | 0.031 | 0.055 | 0.049 | 0.115 | 0.063 |
| Unadjusted sig. | 0.308 | 0.712 | 0.509 | 0.559 | 0.082 | 0.451 | |
| n | 146 | 147 | 146 | 147 | 147 | 147 | |
Sig. = significance (p-value); 1Continous variable; 2continous variable; 3dichotomous variable: German vs Latin (Italian and French); 4dichotomous variable: Swiss vs non-Swiss; 5continous variable ranging from 1 to 10. Except for country of origin two-tailed significance values are reported, for country of origin we hypothesised a directed effect (i.e. Swiss < non-Swiss); We used Pearson correlation when all assumptions were met (all correlations in the age column), Spearman correlation when assumptions were not met (all correlations in the work experience and religiosity columns), and point-biserial correlation in cases of correlation between a continuous and dichotomous variable (all correlations in the gender, language region, and country of origin columns).
1. Swiss Federal Statistical Office . Foreign population. 2020; Available from: https://www.bfs.admin.ch/bfs/en/home/statistics/population/migration-integration/foreign.html
2. Swiss Federal Statistical Office . Die Bevölkerung der Schweiz 2017. 2018.
3. Swiss Federal Statistical Office . Statistischer Bericht zur Integration der Bevölkerung mit Migrationshintergrund. 2017.
4. Swiss Federal Statistical Office . Bevölkerung nach Migrationsstatus 2017. 2018.
5. Swiss Childhood Cancer Registry . Annual Report 2017/2018. 2019.
6. Swiss Federal Office of Public Health . National Programme on Migration and Health - 2008–2013 results and priorities for 2014–2017. 2013.
7. Jaeger FN , Hossain M , Kiss L , Zimmerman C . The health of migrant children in Switzerland. Int J Public Health. 2012 Aug;57(4):659–71. https://doi.org/10.1007/s00038-012-0375-8
8 Gehri M et al. Primary care for the migrant population in Switzerland: a paediatric focus. Paediatrica. 2016;27(Special issue: migrants):9-15.
9. Rost M , et al. Barriers to Palliative Care in Pediatric Oncology in Switzerland: A Focus Group Study. J Pediatr Oncol Nurs. Accepted 2019.
10. Campinha-Bacote J . The Process of Cultural Competence in the Delivery of Healthcare Services: a model of care. J Transcult Nurs. 2002 Jul;13(3):181–4. https://doi.org/10.1177/10459602013003003
11. Stefanenko T , Kupavskaya A . Developing Cross-cultural Competence, in Encyclopedia of the Sciences of Learning, N.M. Seel, Editor. 2012, Springer US: Boston, MA. p. 941-944.
12. Schim SM , Doorenbos AZ . A three-dimensional model of cultural congruence: framework for intervention. J Soc Work End Life Palliat Care. 2010;6(3-4):256–70. https://doi.org/10.1080/15524256.2010.529023
13. Mack JW , Uno H , Twist CJ , Bagatell R , Rosenberg AR , Marachelian A , et al. Racial and Ethnic Differences in Communication and Care for Children With Advanced Cancer. J Pain Symptom Manage. 2020 Oct;60(4):782–9. https://doi.org/10.1016/j.jpainsymman.2020.04.020
14. Mitchison D , Butow P , Sze M , Aldridge L , Hui R , Vardy J , et al. Prognostic communication preferences of migrant patients and their relatives. Psychooncology. 2012 May;21(5):496–504. https://doi.org/10.1002/pon.1923
15. Wiener L , McConnell DG , Latella L , Ludi E . Cultural and religious considerations in pediatric palliative care. Palliat Support Care. 2013 Feb;11(1):47–67. https://doi.org/10.1017/S1478951511001027
16. Weissman JS , Betancourt J , Campbell EG , Park ER , Kim M , Clarridge B , et al. Resident physicians’ preparedness to provide cross-cultural care. JAMA. 2005 Sep;294(9):1058–67. https://doi.org/10.1001/jama.294.9.1058
17. De Clercq E , Rost M , Pacurari N , Elger BS , Wangmo T . Aligning guidelines and medical practice: literature review on pediatric palliative care guidelines. Palliat Support Care. 2017 Aug;15(4):474–89. https://doi.org/10.1017/S1478951516000882
18. Haines ER , Frost AC , Kane HL , Rokoske FS . Barriers to accessing palliative care for pediatric patients with cancer: A review of the literature. Cancer. 2018 Jun;124(11):2278–88. https://doi.org/10.1002/cncr.31265
19. Cheng BT , Rost M , De Clercq E , Arnold L , Elger BS , Wangmo T . Palliative care initiation in pediatric oncology patients: A systematic review. Cancer Med. 2019 Jan;8(1):3–12. https://doi.org/10.1002/cam4.1907
20. Suurmond J , Lieveld A , van de Wetering M , Schouten-van Meeteren AY . Towards culturally competent paediatric oncology care. A qualitative study from the perspective of care providers. Eur J Cancer Care (Engl). 2017 Nov;26(6):e12680. https://doi.org/10.1111/ecc.12680
21. Doorenbos AZ , Morris AM , Haozous EA , Harris H , Flum DR , Doorenbos AZ , et al. Assessing Cultural Competence Among Oncology Surgeons. J Oncol Pract. 2016 Jan;12(1):61–2. https://doi.org/10.1200/JOP.2015.006932
22. Nemeth, C. and E. Pochobradsky . Hospiz- und Palliativversorgung für Kinder, Jugendliche und junge Erwachsene. 2013.
23. EAPC Taskforce for Palliative Care in Children. Palliative Care for Infants, Children and Young People. The Facts. 2009.
24. Lee RM , Titzmann PF , Jugert P . Towards a More Dynamic Perspective on Acculturation Research, in Youth in multicultural societies: New directions for future research and interventions, P.F. Titzmann and P. Jugert, Editors. in press, Psychology Press.
25. United Nations . Universal Declaration of Human Rights. 1948.
26. Luna F . Elucidating the Concept of Vulnerability: Layers Not Labels. Int J Fem Approaches Bioeth. 2009;2(1):121–39. https://doi.org/10.3138/ijfab.2.1.121
27. Federal Office of Public Health (FOPH) . Swiss Hospitals for Equity. 2019; Available from: https://www.bag.admin.ch/bag/en/home/strategie-und-politik/nationale-gesundheitsstrategien/gesundheitliche-chancengleichheit/chancengleichheit-in-der-gesundheitsversorgung/swiss-hospitals-for-equity.html
28. Bernhard G , Knibbe RA , von Wolff A , Dingoyan D , Schulz H , Mösko M . Development and Psychometric Evaluation of an Instrument to Assess Cross-Cultural Competence of Healthcare Professionals (CCCHP). PLoS One. 2015 Dec;10(12):e0144049. https://doi.org/10.1371/journal.pone.0144049
29. Universitätsklinikum Hamburg-Eppendorf (UKE). Fragebogen zur Erhebung Interkultureller Kompetenz in der Gesundheitsversorgung (CCCHP-27).
30. Hietapakka L , Elovainio M , Wesolowska K , Aalto AM , Kaihlanen AM , Sinervo T , et al. Testing the psychometric properties of the Finnish version of the cross-cultural competence instrument of healthcare professionals (CCCHP). BMC Health Serv Res. 2019 May;19(1):294. https://doi.org/10.1186/s12913-019-4105-2
31. Mayring, P. , Qualitative content analysis: theoretical foundation, basic procedures and software solution. 2014.
32. Zentralarchiv für empirische Sozialforschung (ZA) & Zentrum für Umfragen, M.u.A.Z.e.V. Religiosity scale. Zusammenstellung sozialwissenschaftlicher Items und Skalen (ZIS). 2014; Available from: https://zis.gesis.org/skala/ZA-ZUMA-Religiosit%C3%A4tsskala
33. Matsunaga M . Familywise Error in Multiple Comparisons: Disentangling a Knot through a Critique of O’Keefe’s Arguments against Alpha Adjustment. Commun Methods Meas. 2007;1(4):243–65. https://doi.org/10.1080/19312450701641409
34. Rubin M . Do p Values Lose Their Meaning in Exploratory Analyses? It Depends How You Define the Familywise Error Rate. Rev Gen Psychol. 2017;21(3):269–75. https://doi.org/10.1037/gpr0000123
35. Federal statistical Office. Languages - Main languages of the permanent resident population. 2020; Available from: https://www.bfs.admin.ch/bfs/en/home/statistics/population/languages-religions/languages.html
36. Casillas A , Paroz S , Green AR , Wolff H , Weber O , Faucherre F , et al. Cultural competency of health-care providers in a Swiss University Hospital: self-assessed cross-cultural skillfulness in a cross-sectional study. BMC Med Educ. 2014 Jan;14(1):19. https://doi.org/10.1186/1472-6920-14-19
37. Nageswara Rao AA , Warad DM , Weaver AL , Schleck CD , Rodriguez V . Cross-Cultural Medical Care Training and Education: a National Survey of Pediatric Hematology/Oncology Fellows-in-Training and Fellowship Program Directors. J Cancer Educ. 2019 Jun;34(3):478–87. https://doi.org/10.1007/s13187-018-1326-8
38. Cunningham CT , Quan H , Hemmelgarn B , Noseworthy T , Beck CA , Dixon E , et al. Exploring physician specialist response rates to web-based surveys. BMC Med Res Methodol. 2015 Apr;15(1):32. https://doi.org/10.1186/s12874-015-0016-z
39. Watt K , Abbott P , Reath J . Developing cultural competence in general practitioners: an integrative review of the literature. BMC Fam Pract. 2016 Nov;17(1):158. https://doi.org/10.1186/s12875-016-0560-6
40. Hudelson P . Contextualizing cultural competence training of residents: results of a formative research study in Geneva, Switzerland. Med Teach. 2006 Aug;28(5):465–71. https://doi.org/10.1080/01421590600607567
41. Domenig D . Transcultural change: a challenge for the public health system. Appl Nurs Res. 2004 Aug;17(3):213–5. https://doi.org/10.1016/j.apnr.2004.07.001
42. Parrott L . Constructive Marginality: Conflicts and Dilemmas in Cultural Competence and Anti-Oppressive Practice. Soc Work Educ. 2009;28(6):617–30. https://doi.org/10.1080/02615470903027322
43. Eche IJ , Aronowitz T . Evaluating Cultural Competence of Pediatric Oncology Nurses at a Teaching Hospital: A Pilot Study. J Pediatr Oncol Nurs. 2017 Nov/Dec;34(6):422–6. https://doi.org/10.1177/1043454217713452
44. Dabney K , McClarin L , Romano E , Fitzgerald D , Bayne L , Oceanic P , et al. Cultural Competence in Pediatrics: Health Care Provider Knowledge, Awareness, and Skills. Int J Environ Res Public Health. 2015 Dec;13(1):ijerph13010014. https://doi.org/10.3390/ijerph13010014
45. Jongen C , McCalman J , Bainbridge R . Health workforce cultural competency interventions: a systematic scoping review. BMC Health Serv Res. 2018 Apr;18(1):232–232. https://doi.org/10.1186/s12913-018-3001-5
46. Rao, A.N. , D. Warad , and V. Rodriguez , Cross-Cultural Care Training for Pediatric Hematology/Oncology Fellows. 2017. 13.
47. Lachal J , Escaich M , Bouznah S , Rousselle C , De Lonlay P , Canoui P , et al. Transcultural mediation programme in a paediatric hospital in France: qualitative and quantitative study of participants’ experience and impact on hospital costs. BMJ Open. 2019 Nov;9(11):e032498. https://doi.org/10.1136/bmjopen-2019-032498
48. Federal Office of Public Health . Migrationssensitive Palliative Care. 2016; Available from: https://www.bag.admin.ch/bag/de/home/strategie-und-politik/nationale-gesundheitsstrategien/strategie-palliative-care/sensibilisierung-zu-palliative-care/mitgrationssensitive-palliative-care.html
49. Chun MB , Jackson DS , Lin SY , Park ER . A comparison of surgery and family medicine residents’ perceptions of cross-cultural care training. Hawaii Med J. 2010 Dec;69(12):289–93.
50. Moleiro, C. , et al. , Cultural Diversity Competencies in Child and Youth Care Services in Portugal: Development of two measures and a brief training program. 2011. 33: p. 767-773.