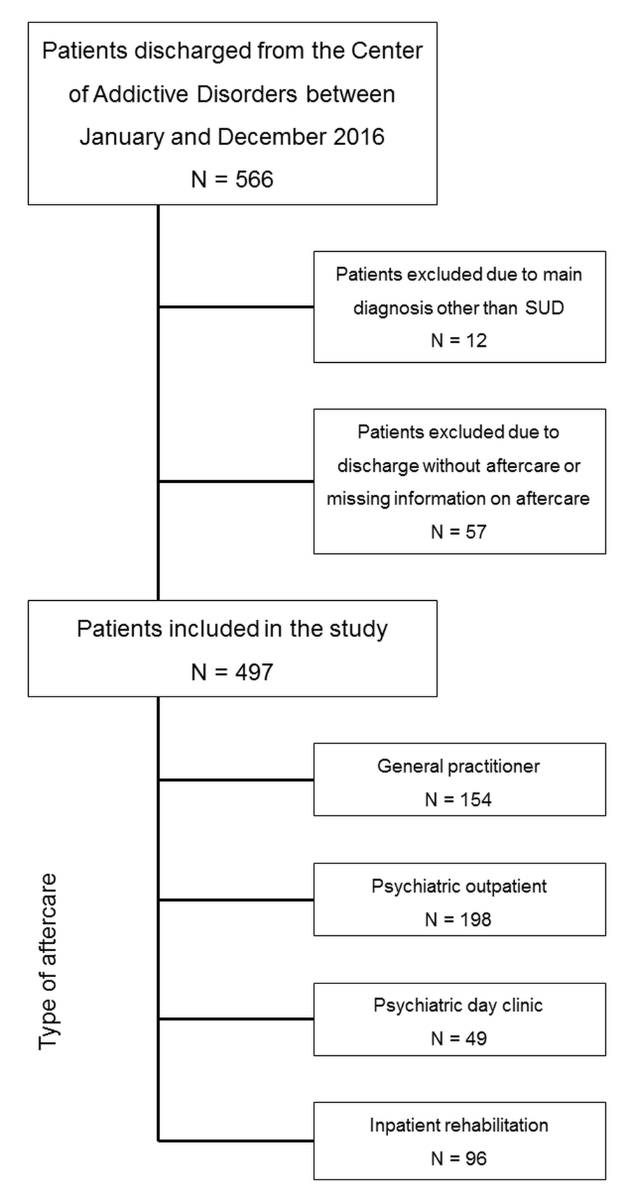
Figure 1 Patient selection flow chart.
DOI: https://doi.org/10.4414/SMW.2022.w30213
Substance use disorders are chronic diseases that typically go along with periods of recovery, relapse and subsequent readmissions before a stable state of abstinence can be achieved [1]. The complexity of substance use disorders can be explained by the fact that their severity is related not only to the pharmacological effects of the respective substances, but also to other areas such as medical needs, underlying psychosocial distress, legal problems, unemployment, and problems in relationships or with housing [2]. The majority of substance use disorder patients do not require medically supervised withdrawal treatment in a hospital and are adequately managed in the outpatient healthcare system. For patients with greater substance use disorder severity, a higher risk for a complicated clinical course and/or with comorbid mental disorders, a beneficial long-term outcome appears to be more likely if the initial treatment phase involves inpatient withdrawal treatment and is combined with a second phase in which some form of at least lower intensity aftercare is established (for a review, see [3]). Previous studies showed that aftercare successfully prevents future readmissions to inpatient treatment, although it remains unclear whether the index hospitalisations were superior to outpatient treatment [4]. Accordingly, the guidelines of the German Association for Psychiatry, Psychotherapy and Psychosomatics recommend a seamless treatment continuation following acute withdrawal treatment [5]. This aftercare can be provided in different settings, which all proved to be effective in maintaining abstinence or reducing substance use and negative consequences of substance use disorders, i.e., outpatient care [6], day clinic [7], and alcohol or drug rehabilitation facilities providing inpatient rehabilitation programmes for periods of up to 12 months [8]. However, there is no clear evidence for the superiority of any one of these settings in the aftercare of substance use disorders.
All of these approaches may be considered valuable, but there are huge differences in costs, availability and funding of treatment places. In general, outpatient aftercare provided by a general practitioner can be considered to be the best available and least costly option. Psychiatric outpatient treatment is more disorder-specific, but less accessible. In Switzerland, the costs of psychiatric outpatient treatment are similar to the treatment in the primary healthcare setting (for comprehensive information on the Swiss tariff system, see [9]). Psychiatric day clinics combine more intensive psychiatric care with occupational and vocational therapy, and meanwhile the patients maintain their activities of daily living. Day clinics are more cost-intensive than outpatient care as they provide treatment throughout the whole week. In inpatient rehabilitation, a similar level of psychiatric care as in a day clinic is provided and the therapy is free from distractions of home life. However, this setting usually goes with the highest costs of all of these options [10].
In order to prevent over- or underutilisation of treatment resources, it would therefore be reasonable to match treatment intensity to specific patient characteristics. In recent years, allocation guidelines for the treatment of substance-related disorders based on the patients’ specific needs have been implemented in several countries, for example, the Patient Placement Criteria of the American Society of Addiction Medicine (ASAM) [11]. According to the ASAM criteria assessment, the patients’ needs are rated during a standardised interview following six dimensions: acute intoxication and/or withdrawal potential; biomedical conditions and complications; emotional, behavioural, or cognitive conditions and complications; readiness to change; relapse, continued use, or continued problem potential; and recovery/living environment. Depending on the severity ratings, patients can be allocated to one of the following levels of care (LOC): outpatient; intensive outpatient; residential; and inpatient services. Nine evaluation studies of the ASAM criteria confirmed that their use in clinical practice was associated with lower morbidity, better psychosocial functioning and more effective service utilisation [11]. The usefulness of these criteria has also been confirmed outside the United States, for example, in Norway [12].
A European equivalent called Measurement in the Addictions for Triage and Evaluation (MATE) was developed in the Netherlands in the context of a reform project of substance use disorder treatment services [13]. The assessment comprises 10 modules: substance use; substance dependence and abuse; craving; depression, anxiety, and stress; indicators for psychiatric and physical treatment; personality disorders; physical complaints and symptoms; personal and social functioning; environmental factors influencing recovery; and substance abuse treatment history. Depending on the ratings, MATE allows an allocation to different LOC: outpatient advice; outpatient treatment; day/residential treatment; and intensive in- or outpatient care. It has been evaluated in the Netherlands [14] as well as in Germany [13]. A recent study in a German sample of patients with alcohol use disorder reported that treating patients according to the MATE score and the respective LOC reduced days of heavy drinking and costs of treatment compared with the control groups [15]. Both tools (ASAM criteria and MATE) have in common that they rely on patient characteristics, such as addiction severity, psychiatric impairment, psychosocial functioning and treatment history, in order to allocate the appropriate LOC.
In Switzerland, there are only recommendations for the identification of the appropriate LOC, but no explicit criteria or official guidelines. For example, the Swiss national network of addiction recommends inpatient rehabilitation for patients who suffer from severe comorbid somatic or mental disorders, have no social support, are not integrated into the labour market, live in unstable housing situations and/or show problems with maintaining abstinence in the current treatment setting [17]. These recommendations correspond well to the mandatory preconditions that are required by the German pension fund as the main sponsor of alcohol and drug rehabilitation in Germany [18]. In Switzerland, however, the decision as to which setting a patient is referred mainly depends on the individual recommendations of the therapist, the preference of the patient and the acceptance by the treatment providers. The findings from a recent Swiss survey [19] showing that up to 82.5% of the patients do not have any form of aftercare at all following inpatient alcohol withdrawal treatment imply that the current practice of referral to subsequent aftercare in substance use disorders would benefit from clearly defined and consistent guidelines. However, for the interpretation of this finding it is important to bear in mind that more than 90% of acute inpatient treatments for substance use disorders are carried out in general hospitals and only 6% in psychiatric and 3% in addiction-specific healthcare services [20].
In Switzerland, aftercare for substance use disorders following psychiatric inpatient treatment is usually provided in one of the following settings: outpatient treatment by a general practitioner, outpatient treatment by a psychiatrist, treatment in a psychiatric day clinic or inpatient treatment in a specialised rehabilitation facility. Hence, this spectrum includes treatment options ranging from rather low-threshold aftercare by the general practitioner to very high treatment intensity provided in the inpatient rehabilitation programmes. Rüesch et al. [21] showed that substance use disorders are responsible for 23% of psychiatric inpatient treatments in Switzerland (without differentiating between substance use disorder inpatients in acute and in rehabilitative treatment), whereas they represent only 5% in the psychiatric outpatient sector. Studies from Germany suggest that 80% of alcohol-dependent patients consult a general practitioner within one year [22] and that treatment by the general practitioner contributes to successful aftercare [23]. However, detailed epidemiological data about the use of different types of aftercare for substance use disorders in Switzerland is lacking. Moreover, a recently published national report on the Swiss healthcare system criticised the lack of data about quality and efficacy of treatment in the mental healthcare sector [24]. It is therefore unknown whether patients in need of a higher level of aftercare finally receive the appropriate treatment, and whether patients treated in rather high-threshold rehabilitation programmes would likewise benefit from less intense aftercare. In addition, it is unclear from the perspective of the healthcare system whether the respective resources are used in the most appropriate way.
The present study therefore aimed to contribute to a better understanding of the current practice of referral to substance use disorder aftercare. In particular, we aimed to assess (1) the rate of substance use disorder patients being referred to different settings of aftercare following inpatient withdrawal treatment focusing on the four levels of aftercare, (2) the clinical and sociodemographic characteristics of the patients of these four groups, (3) the factors that affect the likelihood of being referred to one of these settings of aftercare, and (4) the rate of readmission to inpatient treatment within one year after discharge.
In this retrospective chart review, we included all patients of the Centre for Addictive Disorders of the Psychiatric Services Aargau (PDAG) who were discharged within the period from January 2016 to December 2016. The PDAG provide inpatient psychiatric treatment for the approximately 680,000 inhabitants of the canton of Aargau, Switzerland, and are the only provider of acute inpatient treatment for patients with substance use disorders. Patients with a substance use disorder according to the International Classification of Diseases, 10th edition (ICD-10) diagnostic criteria (F10–F19) were included to this analysis. Patients with missing information about subsequent aftercare or patients who did not wish any aftercare at all were not considered. Apart from the aforementioned criteria, there were no further inclusion or exclusion criteria. We analysed sociodemographic and clinical variables of the index episode and the readmission rate within a 1-year period following discharge.
We extracted the sociodemographic and clinical variables of interest from the medical database (ORBIS Medical, Dedalus HealthCare GmbH, Bonn, Germany). The data sets were anonymised and transferred to a statistical software program on an independent computer for further analysis. The sociodemographic variables included the patients’ age, sex, marital status, living situation, occupational qualification and employment status. Moreover, detailed information on the different substances, the number of substance use disorders, the presence of a dual diagnosis and the severity of the substance use disorder as assessed by the Health of the Nation Outcome Scale (HoNOS) total score [25] were used. We further included information on the clinical course (number of previous admissions, length of inpatient stay, type of admission and type of discharge). The treatment setting following discharge (general practitioner, psychiatric outpatient facility, psychiatric day clinic and inpatient rehabilitation programme) and the readmission rate within one year after discharge were defined as primary outcome measures.
In order to estimate the impact of baseline patient characteristics on the likelihood of being referred to a particular type of aftercare, we performed multinomial logistic regression analyses. Of the four categories of the response variable "type of aftercare" we used referral to a "general practitioner" as the reference category, as we considered the treatment by a general practitioner to be the lowest level of aftercare in terms of intensity and specificity. As independent variables, we considered all sociodemographic and clinical characteristics specified in table 1. To identify important covariates associated with the type of aftercare, we fitted regression models with one covariate at a time (bivariate analyses). The likelihood ratio test was used to check the significance of the coefficient. In table 2, all independent variables that proved to be statistically significant are listed. Table 2 gives the parameter estimates of these variables, odds ratios (ORs), 95% confidence intervals (95% CIs) and the p-values based on the Wald χ2 statistics. The chi-square test was applied in order to determine whether the four aftercare groups differ in the proportion of readmissions within the 1-year follow-up. Differences in the length of inpatient stay were analysed by means of the Kruskal-Wallis test. Statistical significance level was fixed at α = 0.05. All analyses were performed with IBM SPSS Statistics for Windows, Version 25.0 (Armonk, NY: IBM Corp.).
This study and its study protocol were approved by the responsible regional ethics committee (Ethikkommission Nordwest- und Zentralschweiz, EKNZ, BASEC ID: 2017-01533) and included to the Registry of all Projects in Switzerland of the Swiss Ethics Committees (raps.swissethics.ch). There were no protocol deviations throughout the overall study procedures. According to the Swiss Human Research Act, the retrospective design of the study does not require explicit informed consent by the patients included in the study. The corresponding author has full access to and is able to provide any anonymised study data.
Between January and December 2016, 566 patients were discharged from the Centre for Addictive Disorders. Of these, 69 patients were excluded for this study because in 12 patients substance use disorder was not the main diagnosis, and 57 patients were discharged without any aftercare or missing information on aftercare (fig. 1). The sociodemographic and clinical characteristics of the remaining 497 patients (study sample), separately for the whole sample and the different settings of aftercare, are given in table 1.
Table 1Sociodemographic and clinical characteristics of the study sample.
| Total | General practitioner | Psychiatric outpatient | Psychiatric day clinic | Inpatient rehabilitation | ||
| 497 (100%) | 154 (31.0%) | 198 (39.8%) | 49 (9.9%) | 96 (19.3%) | ||
| Demographic characteristics | ||||||
| Age, mean (SD) | 40.96 (12.35) | 41.73 (12.97) | 40.38 (11.74) | 39.76 (11.86) | 41.54 (12.86) | |
| Male sex, n (%) | 343 (69.0) | 112 (72.7) | 125 (63.1) | 33 (67.3) | 73 (76.0) | |
| Maritial status, n (%) | Married | 79 (15.9) | 29 (18.8) | 25 (12.6) | 8 (16.3) | 17 (17.7) |
| Unmarried, seperated, widowed | 418 (84.1) | 125 (81.2) | 173 (87.4) | 41 (83.7) | 79 (82.3) | |
| Occupational qualification, n (%) | Apprenticeship or university education | 63 (12.7) | 14 (9.1) | 27 (13.6) | 6 (12.2) | 16 (16.7) |
| Compulsory schooling, unknown | 434 (87.3) | 140 (90.9) | 171(86.4) | 43 (87.8) | 80 (83.3) | |
| Substances of use, n (%) | ||||||
| Alcohol | 334 (67.2) | 111 (72.1) | 112 (56.6) | 33 (67.3) | 78 (81.3) | |
| Opioids | 123 (24.7) | 40 (26.0) | 51 (25.8) | 13 (26.5) | 19 (19.8) | |
| Cannabis | 87 (17.5) | 26 (16.9) | 36 (18.2) | 13 (26.5) | 12 (20.9) | |
| Benzodiazepines | 79 (15.9) | 23 (14.9) | 41 (20.7) | 4 (8.2) | 11 (11.5) | |
| Cocaine/amphetamins | 83 (16.7) | 26 (16.9) | 27 (13.6) | 10 (20.4) | 20 (20.8) | |
| Social integration, n (%) | ||||||
| Employment | Employed | 124 (24.9) | 36 (23.4) | 46 (23.2) | 10 (20.4) | 32 (33.3) |
| Unemployed | 373 (75.1) | 118 (76.6) | 152 (76.8) | 39 (79.6) | 64 (66.7) | |
| Living situation | At home | 399 (80.3) | 127 (82.5) | 168 (84.8) | 43 (87.8) | 83 (86.5) |
| Others | 98 (19.7) | 27 (17.5) | 30 (15.2) | 6 (12.2) | 13 (13.5) | |
| Substance use disorder severity | ||||||
| ≥2 substance use disorder diagnoses, n (%) | 190 (38.2) | 60 (39.0) | 76 (38.4) | 19 (38.8) | 35 (36.5) | |
| Dual diagnosis, n (%) | 365 (73.4) | 94 (61.0) | 166 (83.8) | 38 (77.6) | 67 (69.8) | |
| Psychosis/mania | 45 (9.1) | 12 (7.8) | 26 (13.1) | 4 (8.2) | 3 (3.1) | |
| Depression | 172 (34.6) | 41 (26.6) | 67 (33.8) | 19 (38.8) | 45 (46.9) | |
| Anxiety | 80 (16.1) | 20 (13.0) | 37 (18.7) | 12 (24.5) | 11 (11.5) | |
| Personality disorder | 106 (21.3) | 31 (20.1) | 52 (26.3) | 9 (18.4) | 14 (14.6) | |
| ADHD | 40 (8.0) | 10 (6.5) | 13 (6.6) | 7 (14.3) | 10 (10.4) | |
| HoNOS at discharge, n (%) ≤12 | 340 (68.4) | 89 (57.8) | 130 (65.7) | 42 (85.7) | 79 (82.3) | |
| Missing n (%) | 71 (14.3) | 31 (20.1) | 36 (18.2) | 2 (4.1) | 2 (2.1) | |
| Clinical course of substance use disorder treatment | ||||||
| Number of previous admissions | 1–2 admissions | 315 (63.4) | 104 (67.5) | 110 (55.6) | 32 (65.3) | 69 (71.9) |
| >2 admissions | 182 (36.6) | 50 (32.5) | 88 (44.4) | 17 (34.7) | 27 (28.1) | |
| Compulsory admission, n (%) | 95 (19.1) | 28 (18.2) | 57 (28.8) | 5 (10.2) | 5 (5.2) | |
| Type of discharge, n (%) | Mutual consent | 355 (71.4) | 83 (53.9) | 141 (71.2) | 42 (85.7) | 89 (92.7) |
| Treatment discontinuation | 142 (28.6) | 71 (46.1) | 57 (28.8) | 7 (14.3) | 7 (7.3) | |
HoNOS: Health of the Nation Outcome Scale; ADHD: attention deficit hyperactivity disorder; SD: standard deviation
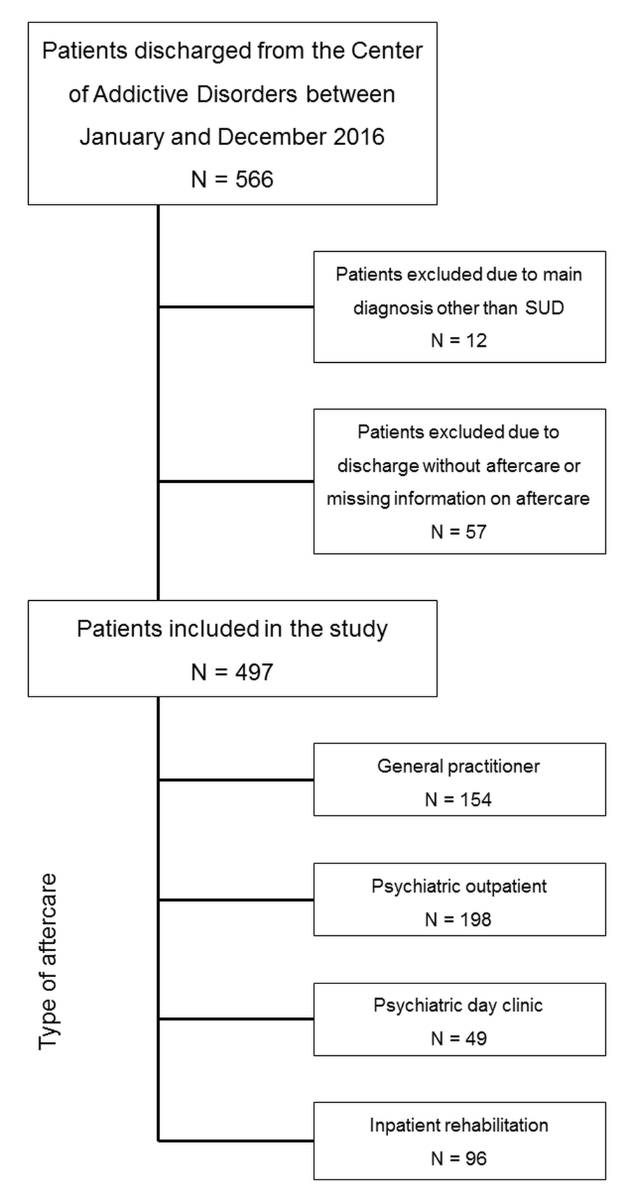
Figure 1 Patient selection flow chart.
The mean age ± standard deviation among all patients was 40.96 ± 12.35 years. We found male patients to prevail in all groups. Moreover, most patients were unmarried, separated or widowed. Regarding educational qualification, the vast majority of patients attended only compulsory school (up to the age of 16).
In all groups, alcohol use disorder was by far the most frequent substance use disorder. Of the patients referred to an inpatient rehabilitation clinic, more than 80% were treated because of an alcohol use disorder, whereas this percentage was considerably lower in the other groups. On the other hand, opioid use was less frequent in the inpatient rehabilitation group. The percentage of cannabis use disorders was highest in those referred to day clinics (26.5%), and most patients with a problematic use of benzodiazepines were referred to the psychiatric outpatient setting. Cocaine and amphetamine use was more frequent in the day clinic and inpatient rehabilitation setting, compared with the other types of aftercare.
Patients with more than two substance use disorder diagnoses were least likely to be referred to inpatient rehabilitation, and patients with a dual diagnosis were more often referred to the psychiatric outpatient setting than to any other type of aftercare. Patients with psychosis or mania were rather rare in inpatient rehabilitation or day clinic programmes; most of them were referred to psychiatric outpatient treatment. Depression was the most frequent comorbid mental disorder across all types of aftercare; it outweighed the other groups in the inpatient rehabilitation setting. We found the highest number of patients with a HoNOS total score at discharge below 12 points, what is suggestive of no or only minor problems, in psychiatric day clinics and inpatient rehabilitation programmes and the lowest number in the general practitioner group.
The proportion of patients with more than two previous admissions was lowest in the inpatient rehabilitation programmes and highest in the psychiatric outpatient setting. Patients with compulsory admission were very rarely referred to inpatient rehabilitation and, in the case of treatment discontinuation, aftercare was most often provided by the general practitioner.
Table 2 presents the variables that showed a significant effect on the likelihood of referral to a particular type of aftercare following inpatient withdrawal treatment (relative to the reference group "general practitioner"). Regarding the demographic patient characteristics, we did not find any significant effects. As to the type of substances, we found a significantly lower relative risk to be referred to psychiatric outpatient care for alcohol-related disorders.
Patients with a dual diagnosis (of any kind) were more likely to be referred to psychiatric outpatient care as well as to psychiatric day clinics. However, patients suffering from depression and substance use disorders were more likely to be referred to inpatient rehabilitation. Low symptom severity at discharge, i.e., HoNOS total score <12, was associated with a higher likelihood to be referred to a psychiatric day clinic or to an inpatient rehabilitation programme. Patients who discontinued inpatient treatment against medical advice were more often referred to the general practitioner than to any other setting.
The analysis showed that more than two previous admissions, as well as compulsory admissions, were significantly linked to a referral to psychiatric outpatient care. None of the indicators of the patients’ social integration (employment, living situation) assessed in this study showed a significant association with the level of aftercare.
Table 2Predictors of referral to a particular type of aftercare following inpatient withdrawal treatment.
| Psychiatric outpatient treatment | Psychiatric day clinic | Inpatient rehabilitation | ||||||||||
| vs General practitioner | vs General practitioner | vs General practitioner | ||||||||||
| B | Odds ratio | 95 % CI | p-value | B | Odds ratio | 95 % CI | p-value | B | Odds ratio | 95 % CI | p | |
| Substance: Alcohol (ref other) | –0.68 | 0.50 | 0.32–0.79 | 0.003 | –0.22 | 0.80 | 0.40–1.60 | 0.53 | 0.52 | 1.68 | 0.90–3.13 | 0.10 |
| Dual diagnosis (ref no dual diagnosis) | 1.20 | 3.31 | 2.01–5.45 | <0.001 | 0.79 | 2.20 | 1.05–4.64 | 0.04 | 0.39 | 1.47 | 0.86–2.54 | 0.16 |
| Substance use disorder & depression (ref no DD depression) | 0.34 | 1.41 | 0.89–2.24 | 0.15 | 0.56 | 1.75 | 0.89–3.43 | 0.11 | 0.89 | 2.43 | 1.42–4.16 | 0.001 |
| HoNOS at discharge ≤12 | 0.44 | 1.55 | 0.89–2.70 | 0.12 | 1.17 | 3.21 | 1.17–8.79 | 0.02 | 0.70 | 2.01 | 1.02–3.97 | 0.04 |
| Number of admissions >2 | 0.51 | 1.66 | 1.07–2.58 | 0.02 | 0.10 | 1.10 | 0.56–2.18 | 0.77 | –0.21 | 0.81 | 0.47–1.42 | 0.47 |
| Compulsory admission (ref voluntary) | 0.60 | 1.82 | 1.09–3.04 | 0.02 | –0.67 | 0.51 | 0.19–1.41 | 0.19 | –1.40 | 0.25 | 0.09–0.66 | 0.006 |
| Treatment discontinuation (ref mutual consent) | –0.75 | 0.47 | 0.30–0.74 | 0.001 | –1.64 | 0.19 | 0.08–0.46 | <0.001 | –2.39 | 0.09 | 0.04–0.21 | <0.001 |
HoNOS: Health of the Nation Outcome Scale; CI: confidence interval
General practitioner n = 154; Psychiatric outpatient treatment n = 198; psychiatric day clinic n = 49; Inpatient rehabilitation n = 96
Table 3 gives the length of stay in the initial inpatient withdrawal treatment and the readmission rate within one year for the four settings of aftercare. We found a significant difference in the length of inpatient stay for the different aftercare treatments (Kruskal Wallis H = 55.3, df(3); p <0.001). Patients referred to day clinics or inpatient rehabilitation had the longest length of stay, compared with the patients referred to the general practitioner or to psychiatric outpatient care. The readmission rate within the first year after discharge was very similar in the four groups (range between 40.4% and 42.9%; chi2 = 0.282, df(3); p = 0.963).
Table 3Length of stay in inpatient withdrawal treatment and readmissions within 12 months according to the four settings of aftercare.
| General practitioner | Psychiatric outpatient treatment | Psychiatric day clinic | Inpatient rehabilitation | ||
| N | 154 | 198 | 49 | 96 | |
| Length of stay (days) | M (SD) | 25.03 (18.85) | 27.93 (22.11) | 39.57 (20.06) | 41.36 (20.29) |
| Perc 25 /Median/ Perc75 | 9.0 / 20.5 / 38.0 | 12.0 / 23.5 / 39.0 | 26.5 / 40.0 / 50.0 | 25.5 / 39.0 / 54.7 | |
| Readmission within 12 months, N (%) | 66 (42.9) | 80 (40.4) | 21 (42.9) | 39 (40.6) | |
This study aimed to contribute to a better understanding of the current practice of referral to substance use disorder aftercare in Switzerland. The very high number of patients who leave inpatient withdrawal treatment without aftercare, as reported in a previous study [19], was not seen in this sample of psychiatric inpatients. In our study, a maximum of 10% of the patients had no aftercare at all. The gap between previous findings [19] and our study might be explained by the higher awareness of aftercare in psychiatric departments specialised in substance use disorders compared with general hospitals without this specialisation.
Of the 497 patients included in this study, 343 (69%) were assigned to a treatment setting that included specialised psychiatric care. The vast majority of these cases (40%) were referred to the psychiatric outpatient setting, 19% to an inpatient rehabilitation programme and 10% to psychiatric day clinics. In 31% of the cases, aftercare was provided by a general practitioner.
Data on the current practice of referral to substance use disorder aftercare for German speaking countries is scarce and, to our knowledge, completely lacking for Switzerland. A recent German study on the placement of patients with alcohol-related disorders following inpatient withdrawal treatment using the MATE criteria demonstrated that 16.5% of the patients received only the lowest level of care in terms of a psychosocial counseling service [15]. According to this German study, 28.5% of the patients were referred to psychiatric outpatient aftercare, 29.1% to day clinic treatment and 19.0% to more intensive inpatient or outpatient psychiatric care, including substance use disorder rehabilitation programmes. The higher rate of patients in psychiatric outpatient aftercare in our study might be explained by the higher per capita rate of psychiatrists in Switzerland, which is more than twice that in Germany (45.1 per 100,000 vs. 20.9 per 100,000) [26]. This assumption is supported by a German survey reporting that only 23% of the persons receiving psychosocial counseling for substance use disorders had additional psychiatric support in the previous 6 months [19]. On the other hand, the lower utilisation of psychiatric day clinics in our study, compared with the German data, suggests that in Switzerland the concept of day clinics for treatment of substance use disorders is still not as established as itapparently is in Germany.
In our sample, 19% of the patients were referred to an inpatient rehabilitation programme following qualified withdrawal treatment. In Switzerland, inpatient rehabilitation is primarily funded by the obligatory health insurance. In Germany, the costs of these programmes are mainly covered by the obligatory pension insurance fund following approval of the respective application. In 2014, 75% of these applications were approved and 41,000 patients completed their aftercare in an inpatient rehabilitation setting [27]. However, in relation to the estimated 3.2 million people suffering from substance use disorders in Germany [28] this corresponds to only 1.2% of the number of potential patients. In this context, the 96 patients from our sample would correspond to only 0.5% of the estimated substance use disorder patients of the catchment area of this study. However, a direct comparison remains difficult, given the different healthcare systems of the two countries.
For another 31% of the patients, referral to a general practitioner was organised. This high proportion underlines the importance of the general practitioner in substance use disorder aftercare. When interpreting this finding, it has to be considered that the majority of these patients had already consulted the general practitioner prior to the inpatient withdrawal treatment because of their substance use disorder and accompanying somatic problems. Therefore, the general practitioner not only plays a key role in substance use disorder aftercare, but also in substance use disorder screening, motivation for change and harm reduction [29]. However, the level of expertise in the treatment of substance use disorder patients among general practitioners is not clear and might be rather low, as demonstrated, for example, by low rates of prescription of anti-craving medications in Germany [30].
Stepped care approaches allow allocation of the patients to more specific and intensive treatment settings according to their needs and resources when previous treatment steps failed to achieve sufficient stability. In the present study, the main substance seems to be most important for the type of subsequent aftercare. We found that patients with alcohol use disorder were more likely to be referred to a general practitioner, rather than to a psychiatric outpatient setting. Apart from tobacco, alcohol is by far the most frequently used substance in Switzerland, and alcohol-related disorders often go along with physical symptoms. Therefore, the general practitioner is usually the first person to address these problems. The fact that patients with alcohol-related disorders were commonly (re-)referred to the general practitioner appears to be inconsistent with a stepped care approach, in which the treatment strategy should be escalated stepwise. Considering this stepped care approach, we might have expected that more patients, particularly those with higher substance use disorder severity or a complicated clinical course, would have been referred to more intensive aftercare settings, regardless of the substance.
On the other hand, it is worth noting that the percentage of alcohol-related disorders (81.3 %) is also quite high in the inpatient rehabilitation programmes. This finding might be explained by the fact that, especially for alcohol-related disorders, the inpatient rehabilitation setting has a long tradition in Switzerland. Although this setting seems to be well established and effective, one has to keep in mind that it is much more cost-intensive than the outpatient alternatives [31]. Interestingly, the psychiatric outpatient and day clinic setting which are more specialised on substance use disorder treatment compared with the general practitioner, but less cost-intensive than inpatient rehabilitation, played only a minor role in substance use disorder aftercare, particularly for alcohol-related disorders, which is inconsistent with the strategy of the stepped care approach.
Moreover, we expected that social integration would have a strong influence on the type of subsequent aftercare, according to the Swiss national recommendations. However, we did not find any significant effect of employment status or living situation on aftercare setting. Most surprisingly, the proportion of employed patients was highest in the inpatient rehabilitation group, although unemployment should be one of the main criteria for inpatient rehabilitation, according to the national recommendations. Instead, unemployed patients were more likely to be treated by the general practitioner. In this context, it is worth noting that an increase in the number of sick leaves as well as a long duration of sick leave is associated with a higher risk of future unemployment [32]. The type of aftercare for employed substance use disorder patients should therefore be evaluated very carefully and allow an early return to work in order to prevent future unemployment. This is even more important as a recent study showed that employment has a protective effect against readmission to inpatient psychiatric treatment [33].
Substance use disorder severity is considered to be an indicator for stepping up the treatment intensity. Dual diagnoses, for example, are considered to markedly increase substance use disorder severity. They go along with the so-called revolving door phenomenon and worsen the prognosis of substance use disorders. If comorbid psychiatric disorders contribute to the overall pathology, a more specific psychiatric treatment approach is warranted. It is therefore not surprising to see that in our study patients with dual diagnoses were more likely to be referred to psychiatric outpatient care than to the general practitioner. Apart from that, patients suffering from substance use disorders and depression were more likely to be referred to inpatient rehabilitation. There is some evidence that the comorbidity of substance use disorders and depression is associated with greater substance use disorder severity and worse prognosis for both diseases [34]. It would be helpful to better understand why depression can be found more often in the inpatient rehabilitation setting than in the other psychiatric settings. An integrated treatment of substance use disorders and depression in the psychiatric outpatient setting has been reported to effectively contribute to lower depression scores and fewer admissions to inpatient care [35]. On the other hand, the relatively low number of patients with comorbid psychosis in the psychiatric day clinic and inpatient rehabilitation setting is striking. The prevalence of this comorbidity is relatively high [36] and treatment of patients with substance use disorders and psychotic disorders is a considerable challenge [37]. However, previous studies showed that the detrimental effects of substance use disorders on the prognosis of psychotic disorders can be improved if the substance use disorder can be successfully treated in time [38]. It should therefore be expected that more patients with substance use disorders and comorbid psychosis would significantly benefit from a more specialised and intensive aftercare, as provided by psychiatric day clinics and inpatient rehabilitation programmes.
A previous study by Andreas et al. [25] has shown that the HoNOS is a reliable instrument to assess the severity of mental and social problems in patients with substance-related disorders. Based on the concept of stepped care, we expected to find the highest symptom load in the most intensive level of aftercare and vice versa. However, we rather found the opposite distribution. Patients with a rather low symptom load, as displayed by a total score of less than 12 points on the HoNOS at discharge, were primarily referred to the more specialised and cost-intensive psychiatric day clinics or even to inpatient rehabilitation. This finding challenges the efficient resource management in substance use disorder treatment as recommended by the stepped care approach.
Similarly, the number of previous admissions, compulsory admission and treatment discontinuation were associated with a higher likelihood to be referred to less intensive aftercare settings, although they are known as robust indicators of greater substance use disorder severity and worse outcome [39]. In detail, patients with more than two previous admissions were more often referred to the psychiatric outpatient setting, rather than to a psychiatric day clinic or inpatient rehabilitation. Given that the number of previous admissions is one of the strongest predictors of future readmission [33], it is contradictory that this well-known risk factor at the patient level did not lead to a more intensive psychiatric aftercare setting. Likewise, the highest proportion of patients with compulsory admission were referred to psychiatric outpatient care and the findings suggest that in these patients, referral to the general practitioner was more likely than referral to an inpatient rehabilitation programme. Moreover, substance use disorder patients who have discontinued their treatment against medical advice were much more likely to end up in non-psychiatric than in psychiatric aftercare.
Taken together, the findings from this analysis suggest that those factors that are considered to be robust indicators for a favourable prognosis, such as being in employment, were not associated with lower levels of aftercare, whereas established indicators for inpatient rehabilitation, such as dual diagnosis or previous admissions, did not steer allocation towards more intensive level of care. It appears that the higher the level of care is, the lower is the likelihood to find rather unmotivated patients or patients at high risk of endangerment to self and/or others. The findings of this study suggest that the current practice of referral to substance use disorder aftercare, at least in our sample, does not correspond to a stepped care approach, in which more impaired and demanding patients would clearly benefit from more intensive treatment settings. It might be speculated whether the access to more intensive level of care, such as psychiatric day clinics or inpatient rehabilitation, rather depends on the patients’ motivation than on factors that are associated with the severity of the substance use disorder or a more complex clinical course of the disease.
The length of prior inpatient withdrawal treatment differed significantly between the different aftercare settings. Patients referred to psychiatric day clinics or to inpatient rehabilitation showed a much longer length of stay than patients referred to outpatient psychiatric treatment or to the general practitioner. Since the factors discussed above do not substantiate or explain the need for a longer treatment in these groups, we assume that this finding was mainly related to the waiting time for these specialised aftercare settings.
Repeated readmissions of patients with substance use disorders are a major challenge for the public healthcare system and contribute to the so-called revolving door phenomenon [40]. They not only increase the burden and stigmatisation of substance use disorder patients [41], but are also associated with high treatment costs [42]. The number of previous admissions and a higher symptom load at discharge could be identified as strong predictors of psychiatric readmission in patients with substance use disorders [33]. The readmission rates of patients with alcohol use disorder of between 30% within 6 months [43] and 51% within 1 year [44] are comparable to the readmission rates detected in our study. However, there were no significant differences in the readmission rates between the four different types of aftercare (range 40.4 to 42.9%). This finding is even more remarkable as those patients with rather mild impairments were referred to an even higher level of aftercare, i.e., psychiatric day clinic and inpatient rehabilitation, compared with those patients with a high symptom load but low level of aftercare in the outpatient setting.
These results do not necessarily support the hypothesis that higher levels of aftercare increase their chances of treatment success. It remains speculative whether those patients with a putative favourable prognosis actually benefit from a more intensive treatment setting or whether they would have benefitted more from a lower level of aftercare where they could have remained in their social and occupational environment. On the other hand, the lower rate of patients with greater substance use disorder severity and worse prognosis referred to a higher level of aftercare may not only reflect a procedure which, at first glance, seems to be contrary to a stepped care approach; it might also be assumed that general practitioners and outpatient psychiatric services were more likely to be trusted to manage the most severe cases.
Several limitations of our study have to be taken into account for the interpretation of the results. In our study, we assessed only to which settings the patients were referred following inpatient qualified withdrawal treatment, but we had no further information on their actual use. Therefore, our data only provide information on the process level of referral to aftercare, but not on the effectiveness of the different types of aftercare. In order to answer the latter question, further prospective studies with randomised referral to the different aftercare settings would be required. Moreover, during the 1-year follow-up it is not clear whether some patients were readmitted to inpatient withdrawal treatment in a general hospital or in another psychiatric hospital outside the canton of Aargau which might have confounded our results regarding the readmission rates. However, we estimate the number of these patients to be rather small, as the PDAG is the only provider of acute inpatient substance use disorder treatment within the catchment area. And finally, we cannot exclude that our findings might have reflected a specific allocation pattern in this region of Switzerland, which might not be representative of other institutions treating substance use disorders. Further research is needed for a more comprehensive analysis, for example, based on a larger sample a multivariate assessment of patient and treatment characteristics (taking interdependence of variables into account) would be worthwhile.
To our knowledge, this study was the first to provide information on the current practice of referral to substance use disorder aftercare in Switzerland. Our results indicate that most patients were referred to aftercare following inpatient withdrawal treatment. This can be considered as a positive sign in general, but the study findings also address some critical aspects. In particular, patients with alcohol-related disorders were considerably underrepresented in the psychiatric outpatient setting and comparatively overrepresented in inpatient rehabilitation programmes. For severely impaired substance use disorder patients, referral to psychiatric day clinics or inpatient rehabilitation was less likely than for patients with mild impairment, with the consequence that patients who would have an additional benefit from a more intensive treatment setting might be under-treated, and that patients who have a favourable prognosis even without this more intensive treatment setting might be over-treated. In the light of comparable readmission rates and an even longer length of stay in the less impaired patients, we would strongly recommend considering a more efficient resource management by promoting stepped care approaches in substance use disorder treatment.
There was no funding for this study.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Dennis M , Scott CK . Managing addiction as a chronic condition. Addict Sci Clin Pract. 2007 Dec;4(1):45–55. https://doi.org/10.1151/ascp074145
2. McLellan AT , Luborsky L , Woody GE , O’Brien CP . An improved diagnostic evaluation instrument for substance abuse patients. The Addiction Severity Index. J Nerv Ment Dis. 1980 Jan;168(1):26–33. https://doi.org/10.1097/00005053-198001000-00006
3. Proctor SL , Herschman PL . The continuing care model of substance use treatment: what works, and when is “enough,” “enough?”. Psychiatry J. 2014;2014:692423. https://doi.org/10.1155/2014/692423
4. Reif S , Acevedo A , Garnick DW , Fullerton CA . Reducing behavioral inpatient readmissions for people with substance use disorders: do follow-up services matter? Psychiatr Serv. 2017 Aug;68(8):810–8. https://doi.org/10.1176/appi.ps.201600339
5. Deutsche Gesellschaft für Psychiatrie und Psychotherapie . Psychosomatik und Nervenheilkunde. S3-Leitlinie Screening, Diagnose und Behandlung alkoholbezogener Störungen; 2020 [Internet]. Available from: https://www.awmf.org/leitlinien/detail/ll/076-001.html
6. McCarty D , Braude L , Lyman DR , Dougherty RH , Daniels AS , Ghose SS , et al. Substance abuse intensive outpatient programs: assessing the evidence. Psychiatr Serv. 2014 Jun;65(6):718–26. https://doi.org/10.1176/appi.ps.201300249
7. Lotz-Rambaldi W , Buhk H , Busche W , Fischer J , Bloemeke U , Koch U . [Outpatient rehabilitation of alcohol dependent patients in a day clinic: initial results of a comparative follow-up study of day clinic and inpatient treatment]. Rehabilitation (Stuttg). 2002 Apr-Jun;41(2-3):192–200. https://doi.org/10.1055/s-2002-28451
8. Reif S , George P , Braude L , Dougherty RH , Daniels AS , Ghose SS , et al. Residential treatment for individuals with substance use disorders: assessing the evidence. Psychiatr Serv. 2014 Mar;65(3):301–12. https://doi.org/10.1176/appi.ps.201300242
9. TARPSY . tarifsuisse [Internet]. c2020. Available from: https://www.tarifsuisse.ch/tarifstrukturen/stationaere-tarifstrukturen/tarpsy/
10. Heekeren K , Antoniadis S , Habermeyer B , Obermann C , Kirschner M , Seifritz E , et al. Psychiatric acute day hospital as an alternative to inpatient treatment. Front Psychiatry. 2020 May;11:471. https://doi.org/10.3389/fpsyt.2020.00471
11. American Society of Addiction Medicine . ASAM PPC-2R Patient Placement Criteria for the Treatment of Substance-Related Disorders. 2nd ed. Chevy Chase (MD): American Society of Addiction Medicine; 2007.
12. Stallvik M , Gastfriend DR , Nordahl HM . Matching patients with substance use disorder to optimal level of care with the ASAM Criteria software. J Subst Use. 2015;20(6):389–98. https://doi.org/10.3109/14659891.2014.934305
13. Schippers GM , Broekman TG , Buchholz A , Rutten R . Introducing a new assessment instrument: The Measurements in the Addictions for Triage and Evalution (MATE). Sucht. 2009 Aug;55(4):209–18. https://doi.org/10.1024/2009.04.03
14. Schippers GM , Broekman TG , Buchholz A , Koeter MW , van den Brink W . Measurements in the Addictions for Triage and Evaluation (MATE): an instrument based on the World Health Organization family of international classifications. Addiction. 2010 May;105(5):862–71. https://doi.org/10.1111/j.1360-0443.2009.02889.x
15. Buchholz A , Dams J , Rosahl A , Hempleman J , König HH , Konnopka A , et al. Patient-centered placement matching of alcohol-dependent patients based on a standardized intake assessment: primary outcomes of an exploratory randomized controlled trial. Eur Addict Res. 2020;26(3):109–21. https://doi.org/10.1159/000505913
16. Röhrig J , Buchholz A , Wahl S , Berner M . Placement matching for patients with alcohol use disorders using standardized assessment: A pilot study. J Subst Use. 2015;20(2):97–105. https://doi.org/10.3109/14659891.2013.866175
17. Praxis Suchtmedizin . Entwöhnung/Langzeittherapie [Internet]. c2020. Available from: https://praxis-suchtmedizin.ch/praxis-suchtmedizin/index.php/de/alkohol/entwoehnung
18. Deutsche Rentenversicherung Bund . Vereinbarungen im Suchtbereich [Internet]. c2013. Available from: https://www.deutsche-rentenversicherung.de/SharedDocs/Downloads/DE/Experten/infos_reha_einrichtungen/konzepte_systemfragen/konzepte/vereinbarungen_im_suchtbereich.html
19. Haug S . Wirksamkeit ambulanter Beratung bei Alkoholproblemen. Zürich: Schweizerisches Institut für Sucht- und Gesundheitsforschung; 2015.
20. John U . Prävalenz und Sekundärprävention von Alkoholmissbrauch und -abhängigkeit in der medizinischen Versorgung. Nomos; 1996.
21. Rüesch P , Bänziger A , Juvalta S . Regionale psychiatrische Inanspruchnahme und Versorgungsbedarf in der Schweiz. Datengrundlagen, statistische Modelle, ausgewählte Ergebnisse – eine explorative Studie. Neuchâtel: Schweizerisches Gesundheitsobservatorium; 2013.
22. Hill A , Rumpf HJ , Hapke U , Driessen M , John U . Prevalence of alcohol dependence and abuse in general practice. Alcohol Clin Exp Res. 1998 Jun;22(4):935–40. https://doi.org/10.1111/j.1530-0277.1998.tb03892.x
23. Köhler J , Grünbeck P , Soyka M . [Applicability, duration, and sociomedical course of rehabilitation of alcohol dependency. Current results and perspectives from the insurers’ point of view]. Nervenarzt. 2007 May;78(5):536–46.
24. Vincent C , Staines A . Enhancing the Quality and Safety of Swiss Healthcare. Bern: Federal Office of Public Health; 2019.
25. Andreas S , Harries-Hedder K , Schwenk W , Hausberg M , Koch U , Schulz H . Is the Health of the Nation Outcome Scales appropriate for the assessment of symptom severity in patients with substance-related disorders? J Subst Abuse Treat. 2010 Jul;39(1):32–40. https://doi.org/10.1016/j.jsat.2010.03.011
26. OECD . Psychiatrists and mental health nurses [Internet]. OECD Publishing. Available from: http://dx.doi.org/https://doi.org/10.1787/health_glance-2013-en.
27. Deutsche Rentenversicherung Bund . Reha-Bericht: Update 2014 [Internet]. Available from: https://www.deutsche-rentenversicherung.de/SharedDocs/Downloads/DE/Statistiken-und-Berichte/Berichte/reha_bericht_update_2014.html
28. Deutsche Hauptstelle für Suchtfragen . DHS Jahrbuch Sucht 2020 [Internet]. Available from: https://www.dhs.de/informationsmaterial/jahrbuch-sucht.html
29. Delargy I , Crowley D , Van Hout MC . Twenty years of the methadone treatment protocol in Ireland: reflections on the role of general practice. Harm Reduct J. 2019 Jan;16(1):5. https://doi.org/10.1186/s12954-018-0272-4
30. Scherbaum N , Holzbach R , Stammen G , Kirchof U , Bonnet U . Very low frequency of drug therapy of alcohol dependence in Germany - Analysis of data of a statutory health insurance. Pharmacopsychiatry. 2020 Jan;53(1):37–9. https://doi.org/10.1055/a-0896-2757
31. de Andrade D , Elphinston RA , Quinn C , Allan J , Hides L . The effectiveness of residential treatment services for individuals with substance use disorders: A systematic review. Drug Alcohol Depend. 2019 Aug;201:227–35. https://doi.org/10.1016/j.drugalcdep.2019.03.031
32. Hesselius P . Does sickness absence increase the risk of unemployment? J Socio-Economics. 2007;36(2):288–310. https://doi.org/10.1016/j.socec.2005.11.037
33. Böckmann V , Lay B , Seifritz E , Kawohl W , Roser P , Habermeyer B . Patient-level predictors of psychiatric readmission in substance use disorders. Front Psychiatry. 2019 Nov;10:828. https://doi.org/10.3389/fpsyt.2019.00828
34. Hasin D , Liu X , Nunes E , McCloud S , Samet S , Endicott J . Effects of major depression on remission and relapse of substance dependence. Arch Gen Psychiatry. 2002 Apr;59(4):375–80. https://doi.org/10.1001/archpsyc.59.4.375
35. Worley MJ , Trim RS , Tate SR , Hall JE , Brown SA . Service utilization during and after outpatient treatment for comorbid substance use disorder and depression. J Subst Abuse Treat. 2010 Sep;39(2):124–31. https://doi.org/10.1016/j.jsat.2010.05.009
36. Hunt GE , Large MM , Cleary M , Lai HM , Saunders JB . Prevalence of comorbid substance use in schizophrenia spectrum disorders in community and clinical settings, 1990-2017: systematic review and meta-analysis. Drug Alcohol Depend. 2018 Oct;191:234–58. https://doi.org/10.1016/j.drugalcdep.2018.07.011
37. Lambert M , Conus P , Lubman DI , Wade D , Yuen H , Moritz S , et al. The impact of substance use disorders on clinical outcome in 643 patients with first-episode psychosis. Acta Psychiatr Scand. 2005 Aug;112(2):141–8. https://doi.org/10.1111/j.1600-0447.2005.00554.x
38. Weibell MA , Hegelstad WT , Auestad B , Bramness J , Evensen J , Haahr U , et al. The effect of substance use on 10-year outcome in first-episode psychosis. Schizophr Bull. 2017 Jul;43(4):843–51. https://doi.org/10.1093/schbul/sbw179
39. Habermeyer B , Wyder L , Roser P , Vogel M . Coercion in substance use disorders: clinical course of compulsory admissions in a Swiss psychiatric hospital. Swiss Med Wkly. 2018 Sep;148:w14644. https://doi.org/10.4414/smw.2018.14644
40. Mark TL , Vandivort-Warren R , Montejano LB . Factors affecting detoxification readmission: analysis of public sector data from three states. J Subst Abuse Treat. 2006 Dec;31(4):439–45. https://doi.org/10.1016/j.jsat.2006.05.019
41. Verhaeghe M , Bracke P , Christiaens W . Part-time hospitalisation and stigma experiences: a study in contemporary psychiatric hospitals. BMC Health Serv Res. 2008 Jun;8(1):125. https://doi.org/10.1186/1472-6963-8-125
42. Jencks SF , Williams MV , Coleman EA . Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009 Apr;360(14):1418–28. https://doi.org/10.1056/NEJMsa0803563
43. Slater EJ , Linn MW . Predictors of rehospitalization in a male alcoholic population. Am J Drug Alcohol Abuse. 1982-1983-1983;9(2):211–20. https://doi.org/10.3109/00952998209002623
44. Van den Berg JF , Van den Brink W , Kist N , Hermes JS , Kok RM . Social factors and readmission after inpatient detoxification in older alcohol-dependent patients. Am J Addict. 2015 Oct;24(7):661–6. https://doi.org/10.1111/ajad.12287