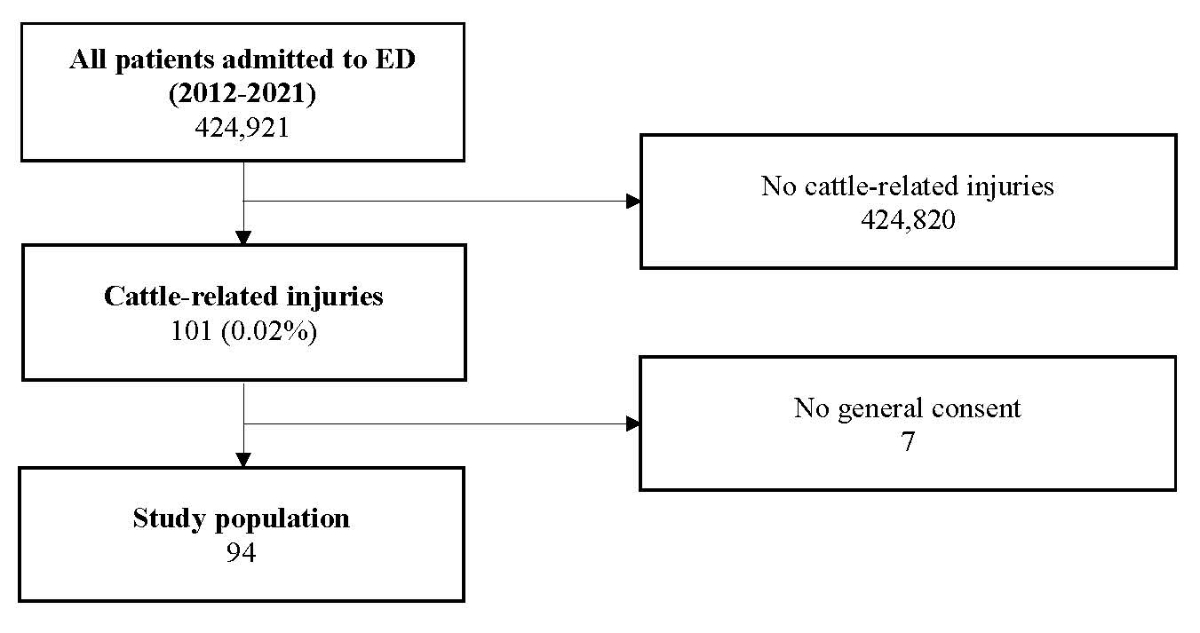
Figure 1 Patient flowchart. ED: emergency department.
DOI: https://doi.org/10.4414/SMW.2022.w30201
Cattle are large, strong animals and unpredictable in their behaviour [1, 2]. Handling cattle is a dangerous activity and injuries associated with cattle pose a serious risk to rural communities [3, 4]. It is well described that farmers in particular are at risk for cattle related injuries in their daily farming activities. The farmers may be trapped, trampled, bitten, or impaled with the horns [1, 5, 6]. In the United Kingdom, there are 4–5 cattle-related deaths per year [7]. In the United States, agriculture is among the industries with the highest number of fatal and non-fatal occupational injuries [3]; of these, 7% were reported in connection with cattle [8, 9]. A recently published systematic review claimed cattle related trauma responsible for more fatal work accidents than any other animal [8].
Most cattle-related injuries occur in farmworkers [10], especially in men under 50 years of age [1, 4, 5]. However, contact with cattle is not limited to farmers: other members of the public may also be at risk if they use public footpaths through farms and walk across pastures with cows and calves [7]. Thus, cattle-related injuries are a public risk and their prevention is in the interest of public health.
Switzerland is traditionally an agricultural country with around 8 million inhabitants. In 2020, there were approximately 50,000 farms and more than 1.5 million cattle registered in Switzerland, i.e., there was one cow per six inhabitants [11]. To our knowledge, there are no studies evaluating cattle-related injuries in Switzerland. Consequently, the aim of this 10-year retrospective cohort study was to close the gap in the literature and give an overview on cattle-related injuries of patients admitted to a tertiary emergency department in Switzerland. In addition, the results may be useful in developing data-driven prevention measures for cattle-related injuries.
The present study was conducted at the Department of Emergency Medicine for Adults of the Inselspital, Bern University Hospital, Switzerland – a tertiary trauma centre. This 10-year retrospective analysis included patients with emergency consultations for cattle-related trauma between 1 July 2012 and 30 June 2021. Our emergency department is located in the Swiss capital with a population of 143,043 (as of 30 June 2020) and a catchment area of about 1 million inhabitants for severe trauma; the capital is surrounded by a rural area with meadows and cows.
All trauma patients admitted to our department are treated according to the principles of Advanced Trauma Life Support (ATLS®).
All medical records of adult patients (≥16 years) admitted to our emergency department within the given time period were screened using the following keywords “cattle, cow, bull, horn” coupled with the Boolean operator “OR”. The medical emergency department report of every hit in our computerised database (Ecare, Turnhout, Belgium) was then manually screened to ensure that a cattle-related trauma was present. We included all patients who were admitted after a cattle-related injury.
Exclusion criteria were patients <16 years, as they are not routinely treated in our emergency department for adults. Patients who refused to give general consent for the use of their anonymised data or subsequently withdrew it were excluded from the study.
For all patients following cattle-related trauma the following data were extracted:
demographic data such as age, gender, occupation of the injured patient (e.g., farmer, veterinary, other), data on the animal that caused the injury (cow, bull, calf), data on mechanism of injury extracted by the clinical notes and classified into the following groups (head-butt, kick, body contact, trample, others), data on anatomic location and severity of the injury by calculating the abbreviated injury scale (AIS) [12] for each body region and the injury severity score (ISS) [13, 14] for each patient. Severe injury was defined as AIS ≥3, and data on treatment procedures were extracted from discharge notes and operation room reports. The procedures were stratified into the following groups: neurosurgical procedure related to brain (craniectomy, craniotomy, intracranial pressure monitoring), fracture reposition including open reduction internal fixation (ORIF), chest procedures including thoracotomy and chest tube insertion, laparotomy, spinal decompression, vascular procedures, wound closure under local or general anaesthesia. Conservative treatment was considered to be present when no procedure was performed. Data on disposition after emergency department consultation for each patient, and data on outcome parameters including the total hospital length of stay and in-hospital mortality were also collected. In addition, the total costs per case calculated by the coding office were extracted for each patient.
Trauma scoring systems provide a method for quantitative and comparative analysis of injury severity [4]. The injury severity score (ISS) was one of the first trauma scoring systems [13] and is by far the most widely used worldwide [6]. The ISS is calculated based on the abbreviated injury scale (AIS) for clinical classification of anatomical location and severity of injury, and combines this information into a single score that correlates predictively with outcome (i.e., mortality) [4]. A threshold ISS ≥16 is commonly used to define major trauma [15].
The statistical analysis was performed using SPSS for windows version 25.0 (SPSS Inc, Chicago, IL). For descriptive analysis, the distribution of continuous variables were described as median and interquartile range (IQR) as they were not normally distributed. The distribution of categorical data was reported as numbers and percentages. Mann-Whitney U-test was used to compare medians for continuous variables. Categorical variables were compared using chi-Square test or Fisher’s exact test. Fisher's exact test was used when more than 20% of cells had expected frequencies <5 [16]. Univariate analysis was used to identify differences in baseline and outcome variables between patients who were admitted to the hospital vs patients who were treated as outpatients. Variables with ap-value <0.05 were considered significant.
This study has been accepted and approved by the local ethics committee, and informed consent was waived (BE-2021-01949).
A total of 424,921 trauma patients were admitted to Bern University Hospital between 1 July 2012 and 30 June 2021, of which 101 (0.02%) were cattle-related. After exclusion of 7 patients, who refused general consent, 94 patients with cattle-related trauma remained for final analysis. (fig. 1).
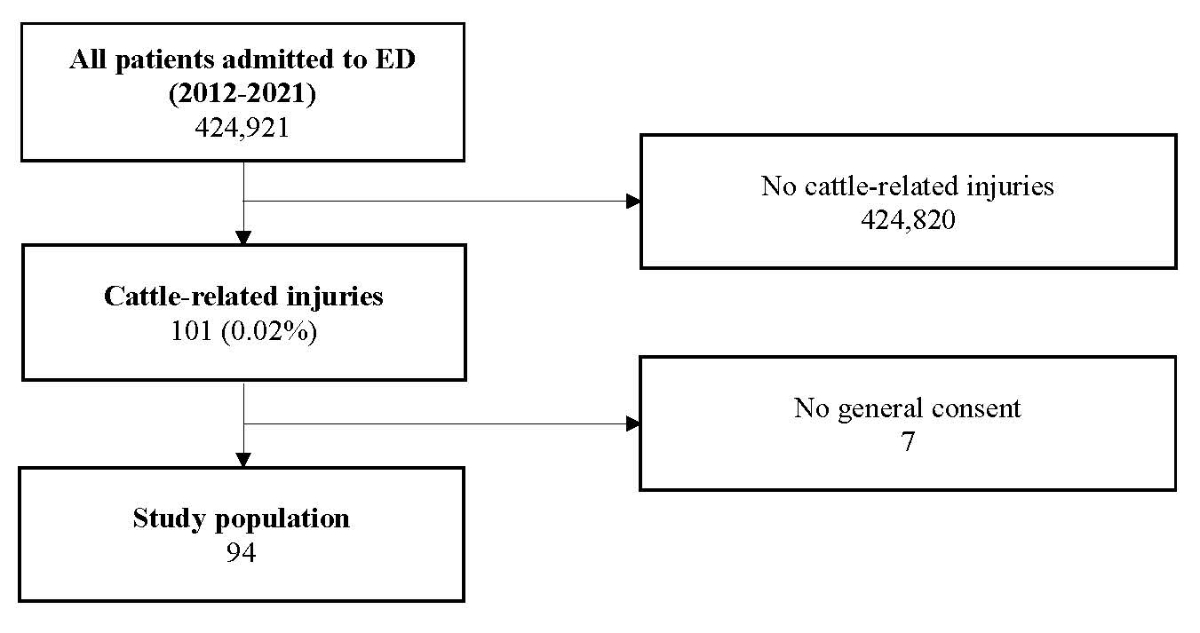
Figure 1 Patient flowchart. ED: emergency department.
Overall, the median age was 52 years (IQR 37–63) and 75% (n = 70) were male. Cattle-related injuries were most common among farmers (73%, n = 69) and most often caused by cows (86%, n = 81), followed by bulls (10%, n = 10) and calves (2%, n = 2). Blunt trauma (89%, n = 84) was the leading mechanism of injury, including headbutt (36%, n = 30), kick (35%, n = 29), physical contact (20%, n = 17) and trample injury (12%, n = 10). Penetrating injury occurred in 11% (n = 10), all caused by headbutt. The majority of patients were transported to the hospital by ground ambulance (57%, n = 54), followed by self-admission (21%, n = 20) and helicopter (21%, n = 20). Overall, 43 patients (46%) were transferred in from outside hospitals (42 patients by ground ambulance and 1 patient by helicopter) (table 1).
Table 1Baseline characteristics of patients admitted after cattle-related trauma. Values are numbers (percentages) unless indicated otherwise.
| All patients (n = 94) | ||
| Demographics | Age, median IQR | 52 (37–63) |
| – Age >65 years | 18 (19%) | |
| Gender, male | 70 (75%) | |
| Occupation of patients | Farmer | 69 (73%) |
| Veterinary | 3 (3%) | |
| Other | 19 (20%) | |
| Unknown | 3 (3%) | |
| Injured by animal | Cow | 81 (86%) |
| Bull | 10 (11%) | |
| Calf | 2 (2%) | |
| Unknown | 1 (1%) | |
| Mechanism of injury | Blunt | 84 (89%) |
| – Headbutt* | 30 (36%) | |
| – Kick* | 29 (35%) | |
| – Body contact* | 17 (20%) | |
| – Trample* | 10 (12%) | |
| – Others* | 3 (4%) | |
| Penetrating | 10 (11%) | |
| – Headbutt | 10 (100%) | |
| Mode of arrival | Ambulance | 54 (57%) |
| Helicopter | 20 (21%) | |
| Self-admission | 20 (21%) | |
| Tranferred in from outside hospital | 43 (46%)** | |
* Percentages exceed 100% due to multiple mechanisms of injury in 5 patients
** † One patient was transferred in by helicopter, the remainder by ambulance
IQR: interquartile range.
Contusions (82%, n = 87) and lacerations (31% superficial, n = 29; 15% deep, n = 14) were the most common injuries after cattle-related accidents, followed by face fractures (28%, n = 26), closed head trauma (19%, n = 18) and chest injuries (17%, n = 16). Following penetrating trauma (n = 10), deep lacerations occurred in 8 cases (80%) and superficial lacerations in 2 cases (20%). The remaining lacerations resulted secondary to blunt trauma (table 2).
Table 2Injury distribution in patients admitted after cattle-related trauma. Percentages exceed 100% due to multiple injuries per patient. Values are numbers (percentages).
| All patients (n = 94) | |
| Closed head injury | 18 (19%) |
| Face fracture | 26 (28%) |
| Chest injury | 16 (17%) |
| Abdominal injury | 4 (4%) |
| Spine injury | 4 (4%) |
| Pelvic injury | 3 (3%) |
| Upper extremity fracture | 7 (7%) |
| Lower extremity fracture | 4 (4%) |
| Contusion | 77 (82%) |
| Laceration superficial | 29 (31%) |
| Laceration deep* | 14 (15%) |
* More than 1 cm deep.
All face fractures were associated with a face AIS <3. Eleven patients (12%) had a head AIS of ≥3; eight patients (9%) had a chest AIS of ≥3, whereas only three patients (3%) had a severe abdominal injury (abdominal AIS ≥3). All four patients with lower extremity fracture had an AIS of 3. All patients with upper extremity fracture had an AIS <3. All spine injuries were classified as spine AIS <3. One pelvic fracture was classified as severe (AIS = 3), two pelvic fractures were associated with a pelvic AIS <3.
A combined severe head (head AIS ≥3) and chest trauma (chest AIS ≥3) was present in two patients. One patient had a combined severe chest and extremity trauma (both AIS = 3). All three patients who sustained severe abdominal injuries (abdomen AIS ≥3) did not have associated severe injuries (AIS ≥3 other than abdomen).
Following the injury distribution, the majority of all patients (63%, n = 59) were minorly injured with an ISS of ≤5; 12% (n = 11) had an ISS of ≥16.
In 37% (n = 35), treatment was conservative. Of all procedures, wound closure was initiated most frequently (40%, n = 38), followed by ORIF (28%, n = 26), neurosurgical procedures (6%, n = 6), insertion of a chest tube (3%, n = 3) and laparotomy (2%, n = 2). One patient (1%) required vascular intervention due to a penetrating injury to the superficial femoral artery. No thoracotomy was performed. Sixteen patients had ORIF for maxillofacial fractures, six for upper extremity fractures, four for lower extremity fractures. Of the total of six neurosurgical procedures, two patients required a craniotomy to remove intracranial haematoma, one patient underwent reduction of a depressed skull fracture, and three patients required monitoring of the intracranial pressure. The majority of patients (51%) were admitted as inpatients, with a median length of hospital stay of 4.5 days (IQR 3–8). Three patients died, corresponding to an in-hospital mortality of 3%. Two of those were injured by a bull. All three patients were 65 years or older (65 years, 70 years and 75 years) and two of the patients who died had a combined severe head and chest trauma; one patient an isolated severe head trauma. The median cost per case was CHF 3,939 (IQR 860–11,369) (table 3).
Table 3Procedures performed, outcomes and case costs of patients admitted after cattle-related trauma.
| All patients (n = 94) | ||
| Conservative treatment | 35 (37%) | |
| Wound closure | 38 (40%) | |
| Neurosurgical procedure | 6 (6%) | |
| Reposition of fracture / ORIF | 26 (28%) | |
| Chest tube | 3 (3%) | |
| Laparotomy | 2 (2%) | |
| Vascular procedures | 1 (1%) | |
| Disposition after ED | Home | 42 (45%) |
| Hospital admission | 48 (51%) | |
| Transfer | 4 (4%) | |
| Hospital length of stay*, median (IQR) | 4.5 (3-8) | |
| In hospital mortality | 3 (3%) | |
| Case costs, median (IQR) (Swiss francs) | 3939 (860–11,369) | |
* Of 48 patients who were admitted to hospital, reported in days
ED: emergency department; ORIF: open reduction, internal fixation.
Of the patients injured by a bull, inpatient treatment was required in in 90% (9 of 10 patients) compared with 49% (38 of 77 patients) injured by a cow, p = 0.029. Patients who sustained penetrating injuries were more often admitted as inpatients (19% inpatients vs 2% outpatients, p = 0.017). Overall, 48 patients were admitted to hospital compared with 42 patients treated as outpatients. Four patients were transferred from our emergency department to outside hospitals and were not included in the outcome analysis. The mean ISS in patients admitted to hospital was 7 (IQR 5–11) compared with 4 (IQR 1–5) in patients treated as outpatients (p <0.001). Conservative treatment was initiated in 26 of 42 outpatients (62%) and in 8 of 48 patients (17%) admitted to the hospital (p <0.001). Cost per case was significantly higher in patients admitted to hospital (CHF 11,241, IQR 5,890–22,974) vs CHF 828, IQR 410–1,384; p <0.001). The in-hospital mortality rate was 6% (n = 3) in patients admitted to the hospital (table 4).
Table 4Comparison of patients treated as outpatient and patients admitted to hospital. Four patients were transferred from our emergency department to outside hospitals and were not considered for this analysis. Pearson chi-square test unless indicated otherwise;.
* Fisher’s exact test ** Mann–Whitney test; *** all penetrating injury due to headbutt. Values are numbers (percentages) unless indicated otherwise.
IQR: interquartile range; ISS: injury severity score.
In this 10-year retrospective study, 101 of 424,921 trauma patients (0.02%) were admitted for cattle-related injuries. However, the prevalence of cattle-related injuries is likely to be underestimated [4]. In Ireland, for example, it was found that the majority of patients with minor agricultural injuries (80 %) are treated by the general practitioner [17]. For severe cattle-related injuries, patients are treated in hospital, but often in regional hospitals [4]. Therefore, not all patients with cattle-related trauma are admitted to a tertiary hospital.
In line with the literature, most patients were male farmers in the middle age (median age of 52 years, IQR 37–63, in the present study) [4, 7, 18]. Other studies also described a younger average age: a study from New Zealand found a mean age of 34 years and a Turkish study of 29 years [1, 5]. In the present study, 19% of all patients were over 65 years old. Two other studies found similar data, with 20% and 25% of patients over 65 years of age, respectively [4, 18]. One explanation for this high proportion of injured elderly is that farms are frequently family businesses and farmers often work beyond the average retirement age [19]. An Australian study found that among those over 55 years of age working in agriculture, animal-related deaths were the fourth leading cause of death [20]. Farmers over 75 years of age were even more likely to die on the job and older male farmers with blunt head and chest injuries were identified as the most vulnerable group for livestock-related deaths [19]. In the present study, three fatal accidents related to cattle were recorded. In line with the findings above, all three accidents occurred in patients aged 65 years and older. All of them had a severe traumatic brain injury; two of them also sustained an associated severe chest trauma.
Our study showed that cows were responsible for 86% of all accidents, 11% of the patients were injured by a bull and 2% by calves. A prospective study from New Zealand reported that 90% of farmer injuries were caused by dairy cows and only 3% by beef cattle [1]. Reasons for this are that dairy cows are more likely to be in contact with people, for example during milking, and they are also more possessive of their herd [19]. Based on our data, it was not possible to distinguish between dairy cows and beef cattle. It is known that accidents involving bulls occur less frequently, but are associated with more severe injuries, indicated by greater injury severity, and are more likely to result in death [3, 4, 7]. Our data confirm these findings, as patients injured by a bull had a significantly higher ISS than patients injured by cows. Furthermore, 9 out of 10 patients inured by a bull required hospitalisation and two of the three deaths were caused by bull-related trauma.
Cattle-related injuries can be caused by a variety of mechanisms and vary widely in type and severity [8]. Overall, they result in the most severe injuries caused by animals [1, 4, 5, 18] and can lead to injuries of similar severity as high-velocity trauma caused by motor vehicles [8, 21]. Injuries sustained at higher speeds are commonly associated with head and facial fractures, followed by fractures of the lower limbs, particularly the femur [4, 8]. In this study, the majority of patients suffered blunt trauma: head butts (36%) and kicks (35%) were the most common causes. Trampling was noted in 12%. Penetrating trauma from head butts occurred in 11%. It is important to emphasise that in Switzerland an estimated 73% of dairy cows are dehorned for safety reasons. In Europe, dehorning is practised in 61% of cattle herds [22]. We consider the widespread of cattle dehorning to be an important reason why penetrating injuries do not occur more frequently despite the high number of head butts. A review article cites kicking as the most common cause of injury, followed by pushing and head butting [8]. In the present study, two thirds of patients suffered minor trauma (ISS ≤5) and 12% had severe trauma (ISS ≥16). Apart from contusions and lacerations, which frequently occurred as concomitant injuries, fractures (44%) were the most common injuries, followed by closed head injury (19%) and chest injury (17%). Sheehan and Deasy examined 54 patients admitted with farm animal-related major traumas at the largest university teaching hospital in Ireland. Similar to our findings, limb trauma, blunt chest trauma and head injuries were the most common injuries [18]. A study from the UK including 44 emergency department patients after cattle-related trauma also reported that fractures were the most common primary injury, followed by blunt chest trauma and soft-tissue injury [7]. Similar injury patterns are described in other parts of the world, e.g., New Zealand and Sweden [1, 6]. Distal and extremity injuries are associated with high patient morbidity, whereas torso and head injuries are responsible for high patient mortality [8].
Half of the patients (51%) evaluated in our emergency department after a cattle-related accident were followed up as inpatients with a median length of stay of 4.5 days (ranging from 3 to 8 days). Thirty-seven percent were treated conservatively, 28% required reduction of a fracture, 3% required an insertion of a chest tube and only 2% needed a laparotomy. A previous retrospective study conducted over a 5-year period at an adult major trauma centre in England, which included only patients directly injured by cattle, found slightly higher rates of admission (70%) and surgery (50%), which may be due to the fact that half of these patients were severely injured with an ISS >16 [7].
In summary, over 70% of all cattle-related injuries treated in our emergency department involved farmers. As a consequence, preventive measures to reduce cattle-related morbidity and mortality should be implemented primarily among farmers. It is important to take preventive measures that target the working environment, on-the-job training and personal protective equipment for farmers [3, 8]. In addition, training and understanding of animal behaviour are critical.
To our knowledge, this is the first study evaluating cattle-related injuries not only in Switzerland but in all German speaking countries. One strength is the inclusion of all consecutive admissions after cattle-related injuries in a large tertiary trauma centre over a 10-year period. However, this was a retrospective study and was associated with all the inherent limitations of this study design. Consultations with primary care physicians and at smaller rural emergency departments after minor trauma were not included in the analyses. This underestimates the prevalence of cattle-related injuries. As Bern University hospital is a tertiary trauma centre almost 50% of the patients were transferred in from outside hospitals, which may lead to an additional selection bias. Furthermore, in more than 50% of the cases, no precise description of the circumstances of the accident could be determined from the data. An analysis in this respect could therefore not be performed. Finally, patients who died before hospital admission due to cattle-related trauma could not be considered for this analysis.
In Switzerland, cattle-related injuries mainly affect male farmers and are associated with considerable morbidity and mortality. Kicking and head butts are the two most common mechanisms leading to trauma. Facial fractures, head injuries and chest injuries are common after cattle-related trauma, and the latter two in particular can be severe. Patients presenting to the emergency department following injuries from cattle, particularly those injured by bulls, should be treated as high velocity trauma. Unlike other professions, there are no standards for safety training in cattle-handling for farmers. The results of the present study can help to formulate data-driven preventive measures for the safe handling of cattle in Switzerland.
Author Contributions: SE, JK, DAJ designed the study. SE, FB, DAJ did the literature search, FB, JK, DAJ carried out data acquisition, FB, DAJ analysed data, SE, DAJ wrote the first draft of the manuscript. All authors contributed to the interpretation of the data and writing of the manuscript and approved the final version of the manuscript.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
1. Watts M , Meisel EM . Cattle associated trauma—a one year prospective study of all injuries. Injury. 2011 Oct;42(10):1084–7. https://doi.org/10.1016/j.injury.2011.02.019
2. Drudi D . Are animals’ occupational hazards. Compensation and Working Conditions. 2000:15-22.
3. Hakan K , Demirci S . Livestock-Handling Related Injuries and Deaths. Livestock Production2012.
4. Murphy CG , McGuire CM , O’Malley N , Harrington P . Cow-related trauma: a 10-year review of injuries admitted to a single institution. Injury. 2010 May;41(5):548–50. https://doi.org/10.1016/j.injury.2009.08.006
5. Caglayan K , Celik A , Ozkan OF , Celik AS , Koksal N , Altinli E . Large animal-related injuries in a rural population in northeastern Turkey. Indian J Surg. 2013 Jun;75(3):200–3. https://doi.org/10.1007/s12262-012-0485-9
6. Björnstig U , Eriksson A , Ornehult L . Injuries caused by animals. Injury. 1991 Jul;22(4):295–8. https://doi.org/10.1016/0020-1383(91)90009-4
7. Rhind JH , Quinn D , Cosbey L , Mobley D , Britton I , Lim J . Cattle-related trauma: A 5-year retrospective review in a adult major trauma center. J Emerg Trauma Shock. 2021 Apr-Jun;14(2):86–91. https://doi.org/10.4103/JETS.JETS_92_20
8. Wheeler JA . Cattle related trauma: are we underestimating its severity? Australas Med J. 2019;12(4).
9. Casey GM , Grant AM , Roerig DS , Boyd J , Hill M , London M , et al. Farm worker injuries associated with cows. New York State 1991-1996. AAOHN J. 1997 Sep;45(9):446–50. https://doi.org/10.1177/216507999704500905
10. Lindsay S , Selvaraj S , Macdonald JW , Godden DJ . Injuries to Scottish farmers while tagging and clipping cattle: a cross-sectional survey. Occup Med (Lond). 2004 Mar;54(2):86–91. https://doi.org/10.1093/occmed/kqh032
11. Bundesamt für Statistik. Landwirtschaft und Ernährung: Taschenstatistik 2021. 2021. [Available from: https://www.bfs.admin.ch/bfs/de/home/statistiken/land-forstwirtschaft/landwirtschaft.html
12. Association for the Advancement of Automotive Medicine . The Abbreviated Injury Scale 2015 revision. Des Plaines: AAAM; 2015. [Available from: https://www.aaam.org/abbreviated-injury-scale-ais/
13. Baker SP , O’Neill B , Haddon W Jr , Long WB . The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974 Mar;14(3):187–96. https://doi.org/10.1097/00005373-197403000-00001
14. Baker SP , O’Neill B . The injury severity score: an update. J Trauma. 1976 Nov;16(11):882–5. https://doi.org/10.1097/00005373-197611000-00006
15. Van Ditshuizen JC , Sewalt CA , Palmer CS , Van Lieshout EM , Verhofstad MH , Den Hartog D ; Dutch Trauma Registry Southwest . The definition of major trauma using different revisions of the abbreviated injury scale. Scand J Trauma Resusc Emerg Med. 2021 May;29(1):71. https://doi.org/10.1186/s13049-021-00873-7
16. Kim HY . Statistical notes for clinical researchers: chi-squared test and Fisher’s exact test. Restor Dent Endod. 2017 May;42(2):152–5. https://doi.org/10.5395/rde.2017.42.2.152
17. Doyle Y , Conroy R . The spectrum of farming accidents seen in Irish general practice: a one-year survey. Fam Pract. 1989 Mar;6(1):38–41. https://doi.org/10.1093/fampra/6.1.38
18. Sheehan M , Deasy C . A Descriptive Study Of The Burden Of Animal-Related Trauma At Cork University Hospital. Ir Med J. 2018 Jan;111(1):673.
19. Centers for Disease Control and Prevention (CDC) . Fatalities caused by cattle—four States, 2003-2008. MMWR Morb Mortal Wkly Rep. 2009 Jul;58(29):800–4.
20. Bury D , Langlois N , Byard RW . Animal-related fatalities—part I: characteristic autopsy findings and variable causes of death associated with blunt and sharp trauma. J Forensic Sci. 2012 Mar;57(2):370–4. https://doi.org/10.1111/j.1556-4029.2011.01921.x
21. Nogalski A , Jankiewicz L , Cwik G , Karski J , Matuszewski Ł . Animal related injuries treated at the Department of Trauma and Emergency Medicine, Medical University of Lublin. Ann Agric Environ Med. 2007;14(1):57–61.
22. Agroscope. Horn-Status bei Rindern [Available from: https://www.agroscope.admin.ch/agroscope/de/home/themen/nutztiere/wiederkaeuer/horn-status-bei-rindern.html