Hospital incidence and mortality of patients treated for abdominal aortic aneurysms in Switzerland – a secondary analysis of Swiss DRG statistics data
DOI: https://doi.org/10.4414/SMW.2022.w30191
Lorenz
Meulia, Anna-Leonie
Mengesa, Klaus
Steigmillerb, Andreas
Kuehnlc, Benedikt
Reutersberga, Ulrike
Heldb, Alexander
Zimmermanna
aDepartment for Vascular Surgery, University Hospital Zurich, Switzerland
bDepartment of Biostatistics and Epidemiology, Biostatistics and Prevention Institute, University of Zurich, Switzerland
cDepartment for Vascular and Endovascular Surgery, Klinikum rechts der Isar, Technical University of Munich, Germany
*Contributed equally to this study.
Summary
AIM OF THE STUDY: To analyse hospital incidence and in-hospital mortality of patients treated for abdominal aortic aneurysms in Switzerland.
METHODS: Secondary data analysis of case-related hospital discharge data of the Swiss Federal Statistical Office for the years 2009–2018. Patients who were hospitalised and surgically treated for nonruptured abdominal aortic aneurysms or hospitalised and treated for ruptured abdominal aortic aneurysms were included in the analysis. Standardised annual incidences rates were calculated using the European standard population 2013. In-hospital all-cause mortality rates were calculated as raw values and standardised for age, sex, and the van Walraven comorbidity score.
RESULTS: A total of 10,728 cases were included in this study, of which 87.1% were male. Overall, 22.7% of the patients presented with a ruptured abdominal aortic aneurysm; 46% of these cases were surgically treated whereas 54% received conservative therapy. The age-standardised cumulative hospital incidences for treatment of nonruptured abdominal aortic aneurysms were 2.6 (95% confidence interval 2.5–2.8) and 19.7 (19.2–20.1) per 100,000 for women and men, respectively; for ruptured aneurysms it was 0.4 (0.3–2.4) per 100,000 in women, and 2.7 (2.6–2.9) in men. The annual incidence rates were stable in the decade observed. The adjusted mortality rates for treatment of nonruptured aneurysms decreased from 5.5% (2.6–11.2%) in 2009 to 1.4% (0.5–3.6%) in 2018 in women, and from 2.4% (1.3–4.5%) in 2009 to 0.6% (0.2–1.5%) in 2018 in men. The adjusted mortality rates for treatment of ruptured abdominal aortic aneurysms remained high without relevant improvements for either sex over time: for women 32.4% (24.1–42.1%), for men 19.7% (16.8–22.8%).
CONCLUSIONS: The hospital incidence rates for nonruptured and ruptured abdominal aortic aneurysms remained unchanged in the decade observed. Compared with Germany, there was no evidence for a decrease in the annual incidence rates for ruptured abdominal aortic aneurysms in Switzerland. Mortality rates in the elective setting were low and decreased in the last decade but remained high in patients treated for ruptured aneurysms. Efforts to reduce the incidence of ruptured abdominal aortic aneurysms are needed to reduce aneurysm-related mortality in Switzerland.
Introduction
Several countries have published epidemiological data and treatment results for patients with abdominal aortic aneurysms [1–5]. In recent years, endovascular aortic repair (EVAR) has become the recommended standard treatment option for patients with abdominal aortic aneurysms (AAA) in both elective and emergency settings [6]. Thus, EVAR is nowadays used in up to 80% of elective cases and in up to 60% of ruptured cases in several European countries [7]. A recently published analysis of data from Switzerland's national registry for vascular interventions (Swissvasc) showed a different picture for Switzerland, especially for the treatment of ruptured abdominal aortic aneurysms (rAAA). Open aneurysm repair (OAR) was performed in more than 60% of the patients presenting with rAAA [8]. However, data were only presented for the years 2018–2020, not all hospitals enter data in Swissvasc, and the registry has not been validated yet [8]. Thus, robust long-term nationwide epidemiological data on AAA for Switzerland are lacking.
A secondary data analysis of diagnosis-related group (DRG) data on the epidemiology of aortic pathologies in Germany revealed relevant information that might help to further improve the treatment quality [5, 9, 10]. The aim of this study was to analyse hospital incidence, treatment modality and in-hospital mortality after treatment of AAA in Switzerland between 2009 and 2018 using case-related hospital discharge data of the Swiss Federal Statistical Office (SFSO) to gain a better understanding of the healthcare setting in Switzerland.
Materials and methods
This was a secondary data analysis of case-related hospital discharge data of the SFSO. Every hospital, birthing centre and medical specialty institution in Switzerland is bound to report all hospitalisations to the SFSO annually. The SFSO collects sociodemographic variables such as age, sex, up to 50 ICD-10 diagnosis codes, up to 100 procedure codes, type of admission, length of stay and discharge information including in-hospital mortality for each case. Information on hospital admission includes location before admission and type of admission. Information on the hospital stay includes diagnoses, treatment, insurance class, time to treatment, total length of stay, length of stay on the intensive care unit (ICU), and duration of ventilation.
Diagnoses are recorded using the 10th revision of the International Classification of Diseases (ICD-10), procedures are recorded using the Swiss classification of surgical interventions (CHOP). Because of personal data protection regulations, information on patients' residences is unavailable and the exact institution description is encoded. Thus, the data do not allow the identification of patients with reinterventions during new hospital admissions. The institution codes for the treating hospitals were not available for data protection reasons. However, hospitals were categorised into five levels of care, with levels one and two denoting university hospitals and other tertiary referral centres ("major hospitals"), and levels three to five denoted smaller secondary hospitals ("regional hospitals") [11]. Information on hospital discharge includes the destination after discharge. The analysis of this anonymised dataset did not require ethical approval (waived by the local ethics board: BASEC-Nr. Req–2021–01010). The original data can be requested from the SFSO. This study is reported in accordance with the STROBE statement [12]. The research protocol of this study has not been published.
Inclusion and exclusion criteria
All cases in which either nonrupturedAAA (nrAAA, ICD-10: I71.4) or ruptured AAA (rAAA, ICD-10: I71.3) were coded as the primary or secondary diagnosis during the reporting years 2009–2018 were included. Cases for which nrAAA or rAAA were coded as a secondary diagnosis but no surgical treatment for the aneurysm was coded were excluded. Cases with nrAAA a primary diagnosis but without coding of surgical treatment were excluded likewise. Rare cases with hybrid treatments were also excluded, i.e., treated with both open aneurysm and endovascular aortic repair. To avoid duplicates, all cases that had been transferred to another hospital without surgical treatment (open or endovascular repair) and all patients with double entries in the dataset were excluded as well.
Statistical analysis
For descriptive analyses, mean and standard deviation (SD) were reported for approximately normally distributed continuous variables. For variables with skewed distribution, median and interquartile range (IQR) were calculated. For categorical variables, frequency and percentage were given. Distributional assumptions were investigated by inspection of density, violin and QQ plots.
Raw cumulative hospital incidences were calculated with logit-Wald 95% confidence intervals (95% CIs). Additionally, directly age-standardized cumulative incidences were calculated using the European standard population from 2013 and for the Swiss population using SFSO data [12–14]. Since the age-specific distribution of the Swiss population was missing for the year 2009, the age distribution of 2010 of the total Swiss population for the year 2009 was used. Logit-Wald 95% CIs for the directly age-standardised estimates were adjusted as suggested by Altman et al. but on the logit-scale [15]. Although the data for this study contain all cases in Switzerland from 2009 to 2018 and therefore inferential statistics using CIs would not be needed, we decided to additionally report CIs to provide a better impression of the uncertainty to be expected in future observations. Pearson’s chi-square statistics were used to test for differences in incidence rates.
In-hospital mortality rates were calculated raw and standardised for age and a sum score of weighted Elixhauser ICD-10 diagnosis groups according to van Walraven [16]. For adjustment, a generalized linear model with binomial error distribution and logit as link function and with age (continuous), year (factor), sex (factor), van Walraven comorbidity score (continuous) as independent variable and death (factor) as dependent variable was built. Simultaneous CIs were calculated using the R package multcomp (version 1.4.17). The Van Walraven score was calculated from all available ICD-10 codes using the comorbidity R package (version 0.5.3). A complete list of all used R packages with version details is available in the appendix (supplementary table S1). No statistical methods to handle missing data were needed since no missing values were present in all variables of the primary analyses. All analyses were performed using R version 4.1.1 on Windows 10 [17]. All p-values were two-sided with an α-level of 5%.
Results
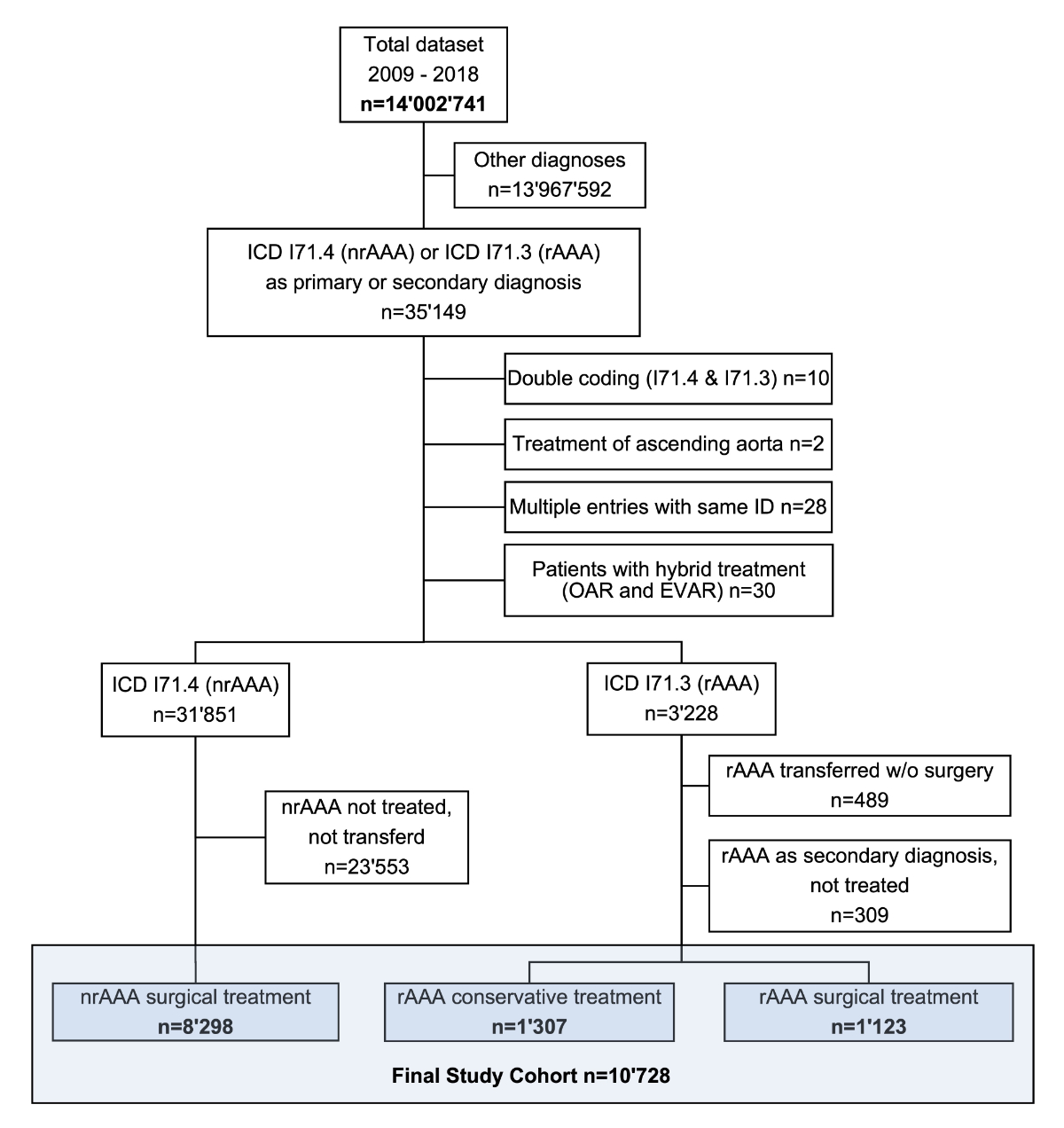
From 01 January 2009 to 31 December 2018, 35,149 cases were hospitalised with either nrAAA or rAAA as a primary or secondary diagnosis. Cases with nrAAA as a primary diagnosis, or as a secondary diagnosis but without surgical treatment during the hospitalisation were excluded (n = 23,553). Cases with a rAAA that were transferred without treatment (n = 489) and other potential duplicates (n = 38) were excluded (fig. 1). A total of 10,728 cases were included in this study, of which 87.1% were male (table 1). In total, 77.3% were treated for nrAAA and 22.7% for rAAA. Data were complete for the published variables.
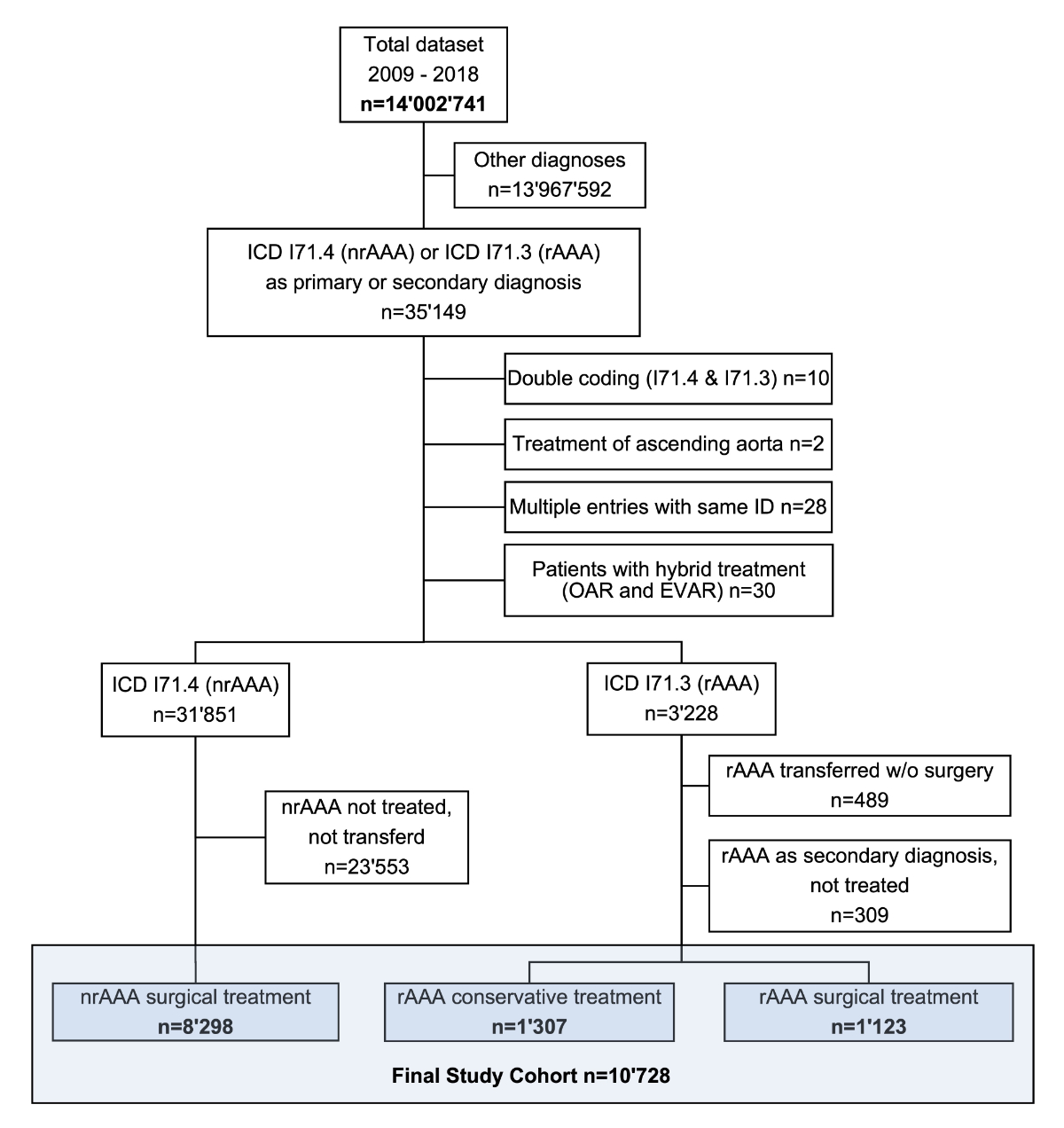
Figure 1 Patient flow. The total dataset contained all hospitalisations in the Swiss population in the years from 2009 to 2018. ICD: International Classification of Diseases (version 10); rAAA: ruptured abdominal aortic aneurysm; nrAAA: non-ruptured abdominal aortic aneurysm.
Table 1Baseline characteristics.
|
Nonruptured AAA
|
Ruptured AAA
|
|
EVAR, n = 4849
|
OAR, n = 3449
|
EVAR, n = 390
|
OAR, n = 733
|
Conservative, n = 1307
|
| Female sex, (%) |
506 (10.4) |
466 (13.5) |
55 (14.1) |
85 (11.6) |
274 (21.0) |
| Age, median (IQR) |
74 (68 to 79) |
70 (64 to 76) |
75 (68 to 81) |
73 (66 to 80) |
80 (72 to 86) |
| Location before admission |
Home or care home, n (%) |
4617 (95.2) |
3228 (93.6) |
230 (59.0) |
452 (61.7) |
862 (66.0) |
| Hospital, n (%) |
172 (3.5) |
173 (5.0) |
151 (38.7) |
269 (36.7) |
417 (31.9) |
| Other, n (%) |
60 (1.2) |
48 (1.4) |
9 (2.3) |
12 (1.6) |
28 (2.1) |
| Type of hospital |
Level 1 university, n (%) |
1605 (33.1) |
1140 (33.1) |
211 (54.1) |
298 (40.7) |
220 (16.8) |
| Level 2 major, n (%) |
2692 (55.5) |
1978 (57.3) |
166 (42.6) |
418 (57.0) |
661 (50.6) |
| Level 3 regional, n (%) |
299 (6.2) |
159 (4.6) |
9 (2.3) |
13 (1.8) |
134 (10.3) |
| Level 4 regional, n (%) |
199 (4.1) |
147 (4.3) |
3 (0.8) |
3 (0.4) |
65 (5.0) |
| Level 5 regional, n (%) |
19 (0.4) |
13 (0.4) |
1 (0.3) |
1 (0.1) |
17 (1.3) |
| Specialty clinics, n (%) |
35 (0.7) |
12 (0.3) |
0 (0.0) |
0 (0.0) |
210 (16.1) |
| van Walraven, median (IQR) |
2 (2 to 3) |
3 (2 to 4) |
3 (2 to 4) |
3 (2 to 5) |
2 (1 to 3) |
Hospital incidence of abdominal aortic aneurysm
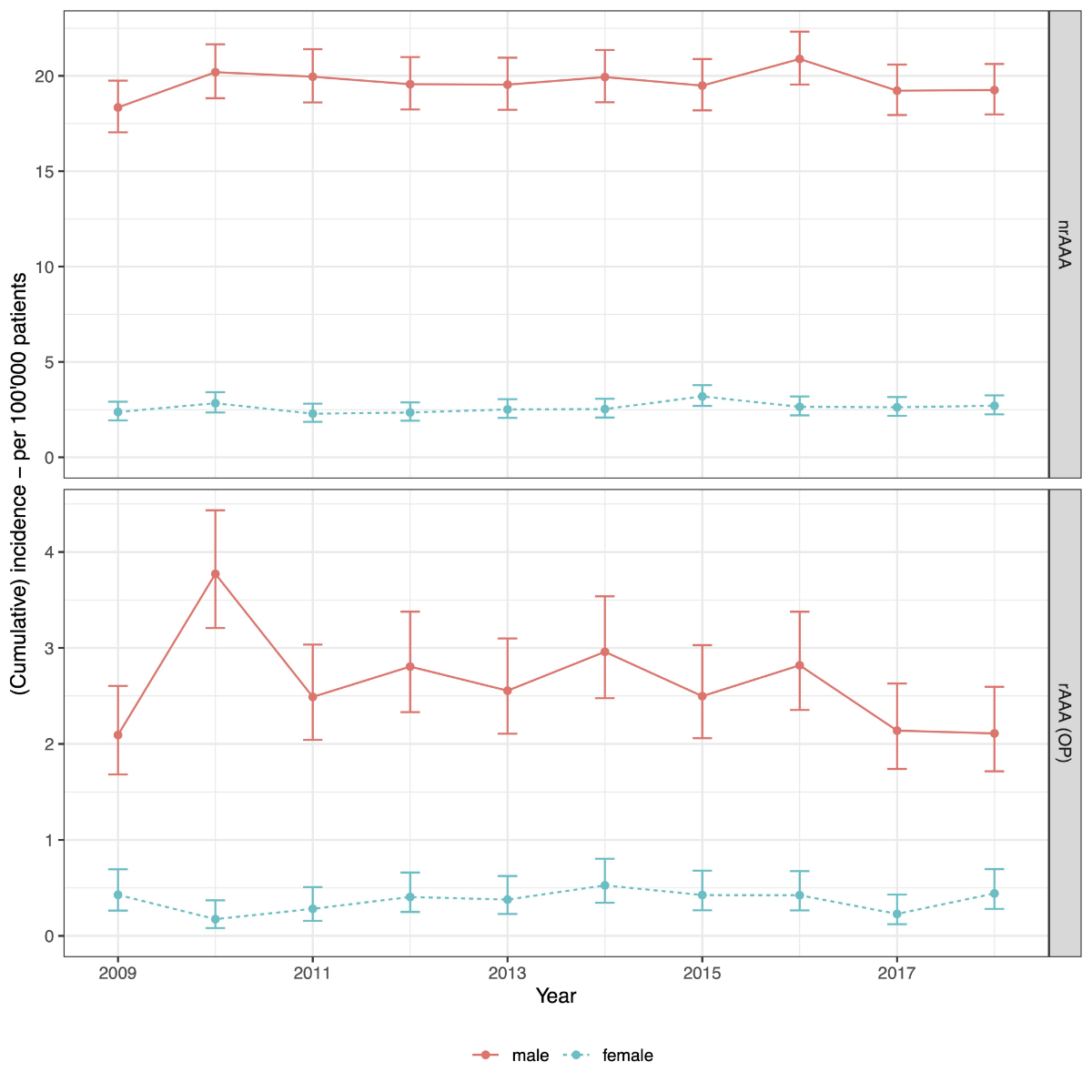
The overall age standardised hospital incidence rates for treatment of nrAAA was 19.6 (95% CI 19.2–20.1) in 100,000 men and 2.6 (95% CI 2.5–2.8) in 100,000 women. For treatment of rAAA the overall age standardised hospital incidence rate was 2.6 (95% CI 2.5–2.8) in 100,000 men and 0.4 (95% CI 0.3–0.4) in 100,000 women. The overall age standardised hospital incidence rate for conservative management of rAAA was 2.7 (95% CI 2.6–2.9) in 100,000 men and 0.7 (95% CI 0.6–0.8) in 100,000 women. The incidence rates were stable in the observed decade (fig. 2). All incidence rates were significantly higher in men than in women, p <0.0001 for each comparison (chi-square statistics).
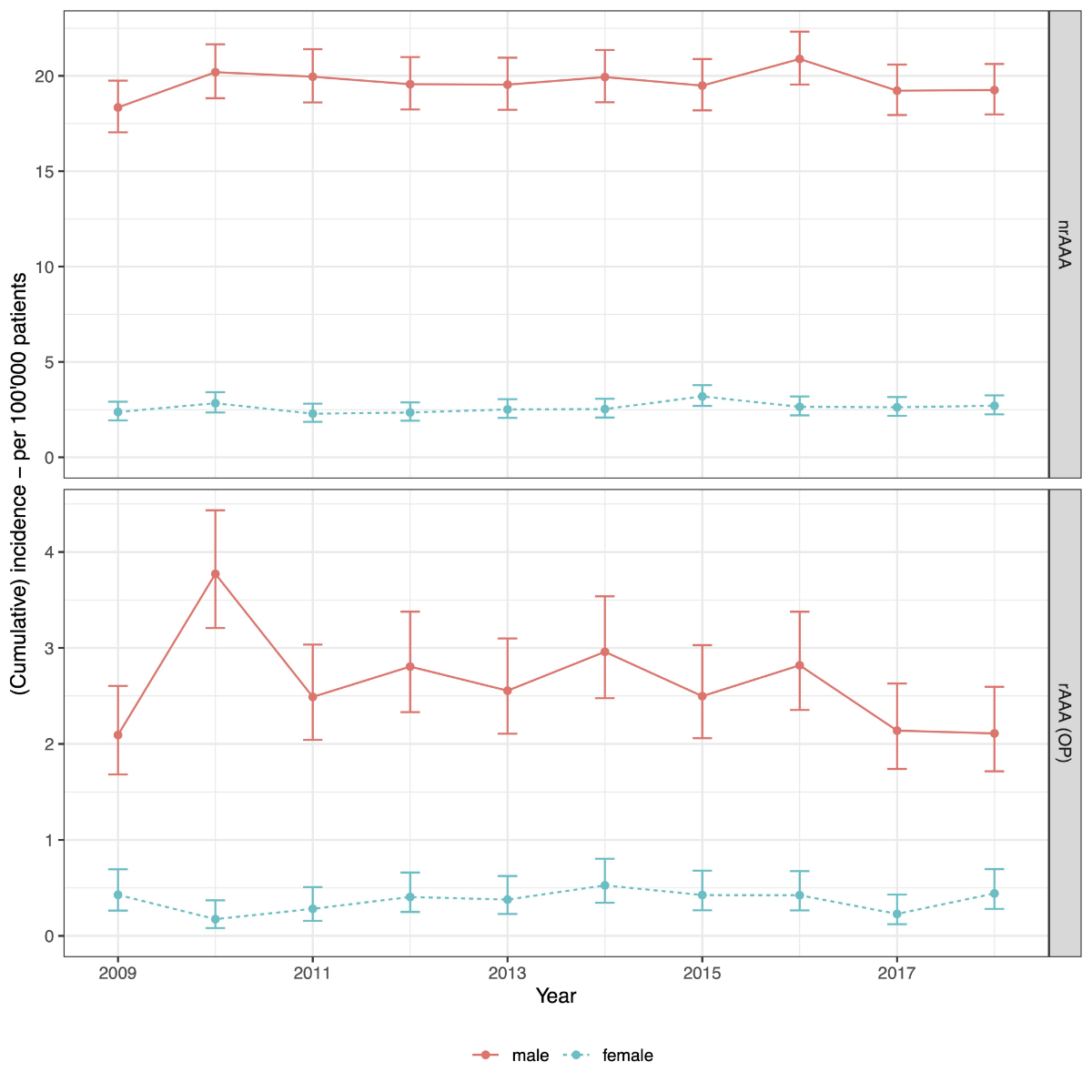
Figure 2 Incidence of abdominal aortic aneurysm (AAA). Standardised incidence rates are presented with 95% confidence intervals for each year and stratified by sex and diagnosis (nonruptured [nrAAA] versus ruptured [rAAA] aneurysms). To increase readability, the y-axis was different for nrAAA and rAAA incidences.
Mode of treatment
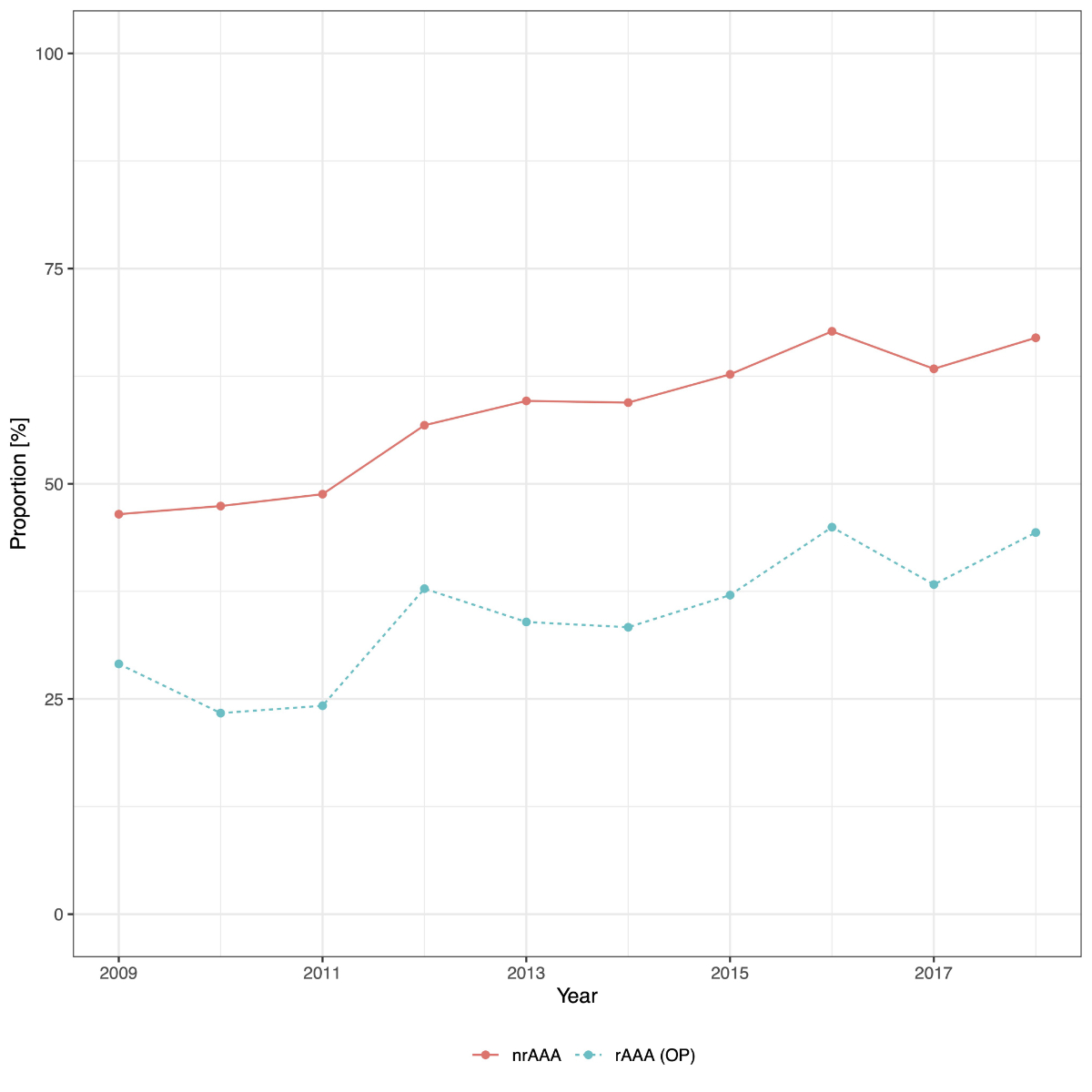
The proportion of cases of nrAAAtreated with EVAR steadily increased from 46.5% in 2009 to 67.0% in 2018. In the same period the proportion of cases of rAAA treated with EVAR increased from 29.1% to 44.3% (fig. 3). Of the 2430 cases presenting with rAAA, 46.2% underwent surgery (open or endovascular repair), the remaining cases received conservative treatment.
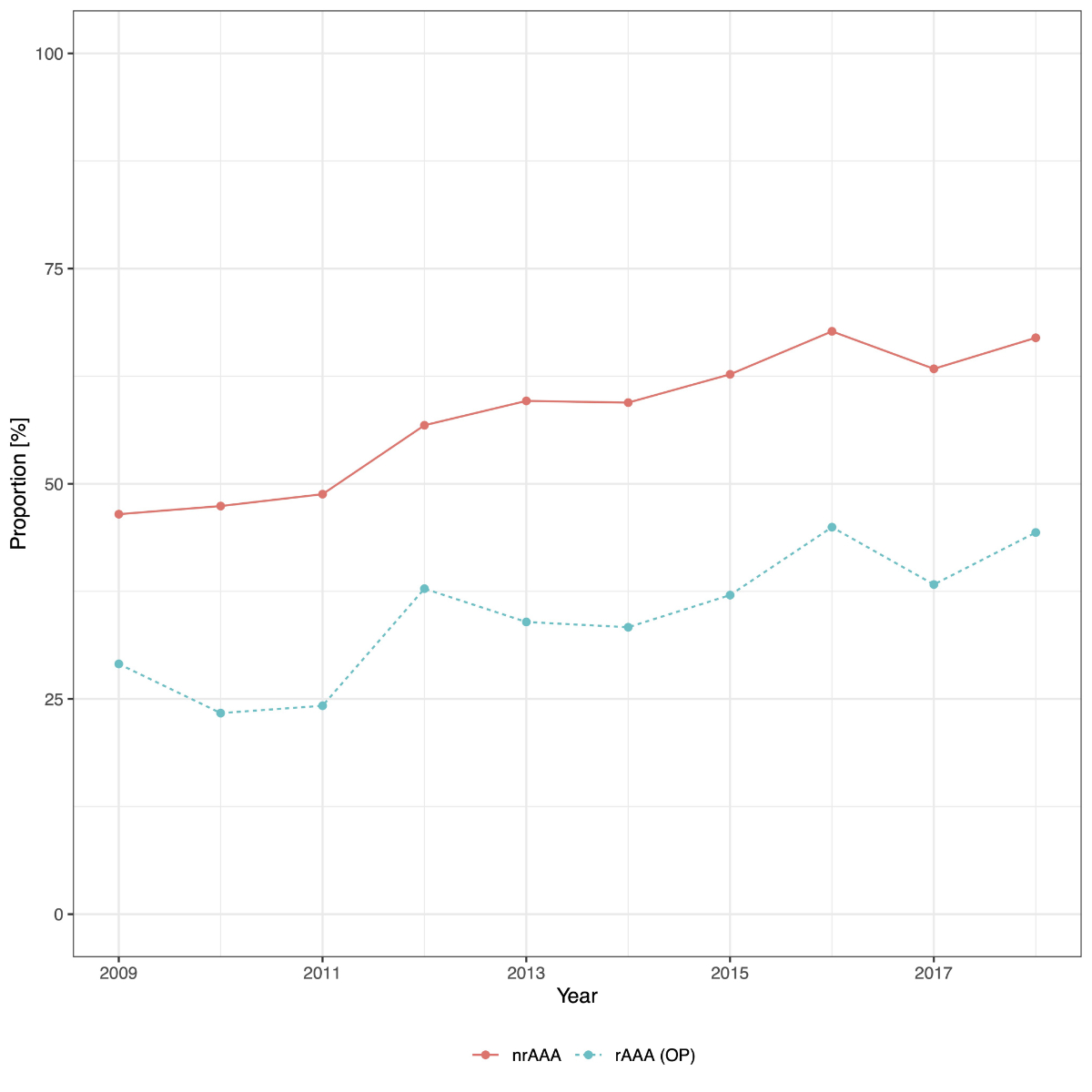
Figure 3 Proportion of patients with endovascular aortic repair (EVAR). The proportion of patients treated with EVAR for each year stratified by diagnosis (nonruptured [nrAAA] versus ruptured [rAAA] abdominal aortic aneurysm).
The majority of the 8298 cases with a nrAAA were treated at major hospitals (33.1% at university hospitals, level 1, and 56.3% at other major hospitals, level 2). The remaining 883 cases (10.6%) were treated in small hospitals (regional hospitals, level 3 to 5). The vast majority of rAAA treatments, 1093 of 1123 (97.3%), were performed at major hospitals (level 1 or 2). A total of 423 (37.4%) were referred from regional hospitals (level 3 to 5) to major hospitals (level 1 and 2) (see table 1).
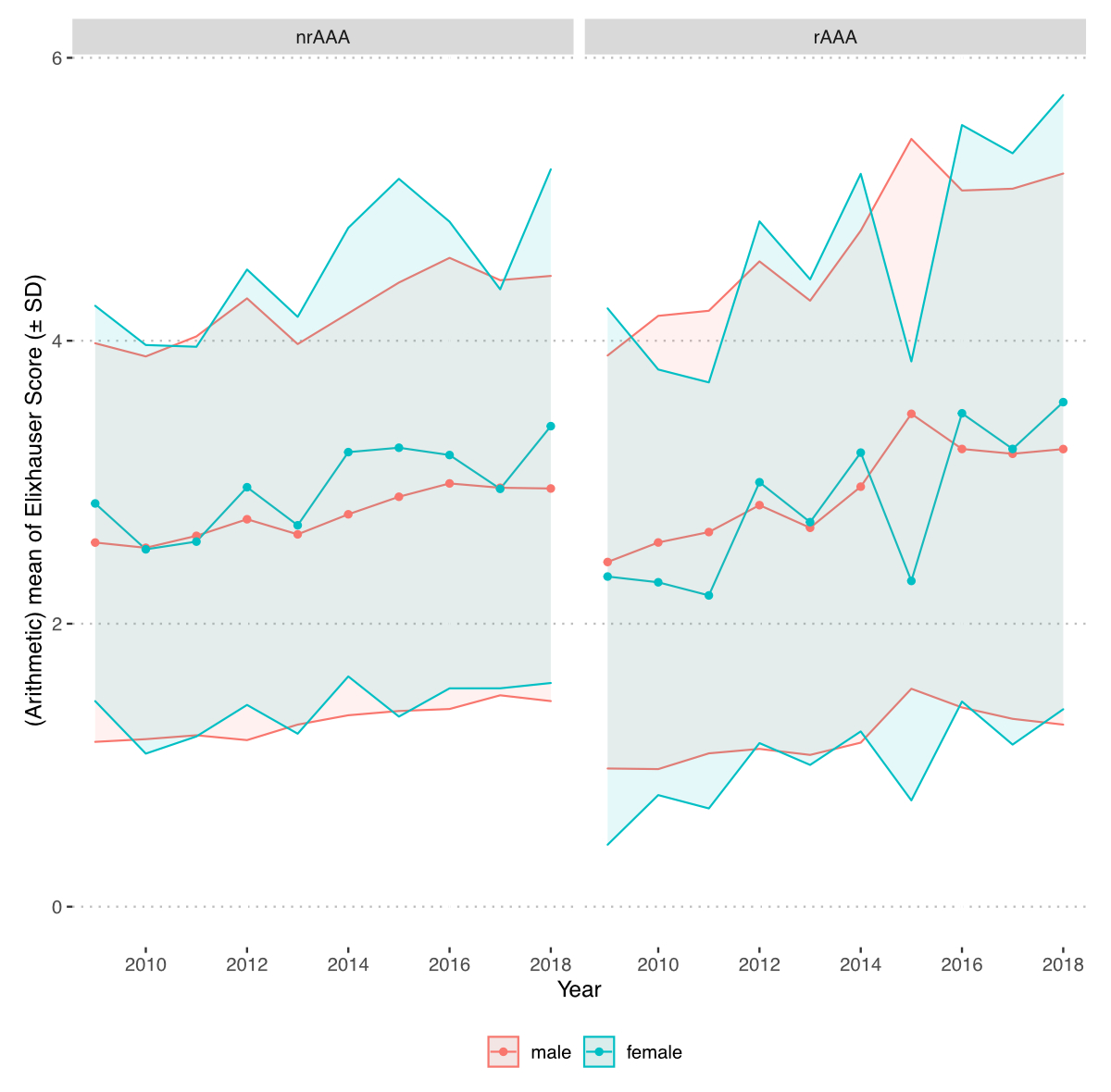
Comorbidities were summarised as the van Walraven score. The mean van Walraven score steadily increased from 2009 to 2018 in both men and women and for both nrAAA and rAAA (supplementary fig. S1 in the appendix).
Treatment outcomes
The overall raw mortality rate was 2.2% (95% CI 1.9–2.5%) in cases treated for nrAAA and 23.1% (95% CI 20.7–25.6%) in cases treated nonconservatively for rAAA. The mortality rates were stratified by sex and type of treatment (endovascular versus open aortic repair). Mortality rates were lower in men than in women for both nrAAA and rAAA, and lower in cases treated by EVAR compared with OAR for nrAAA, but not for rAAA.
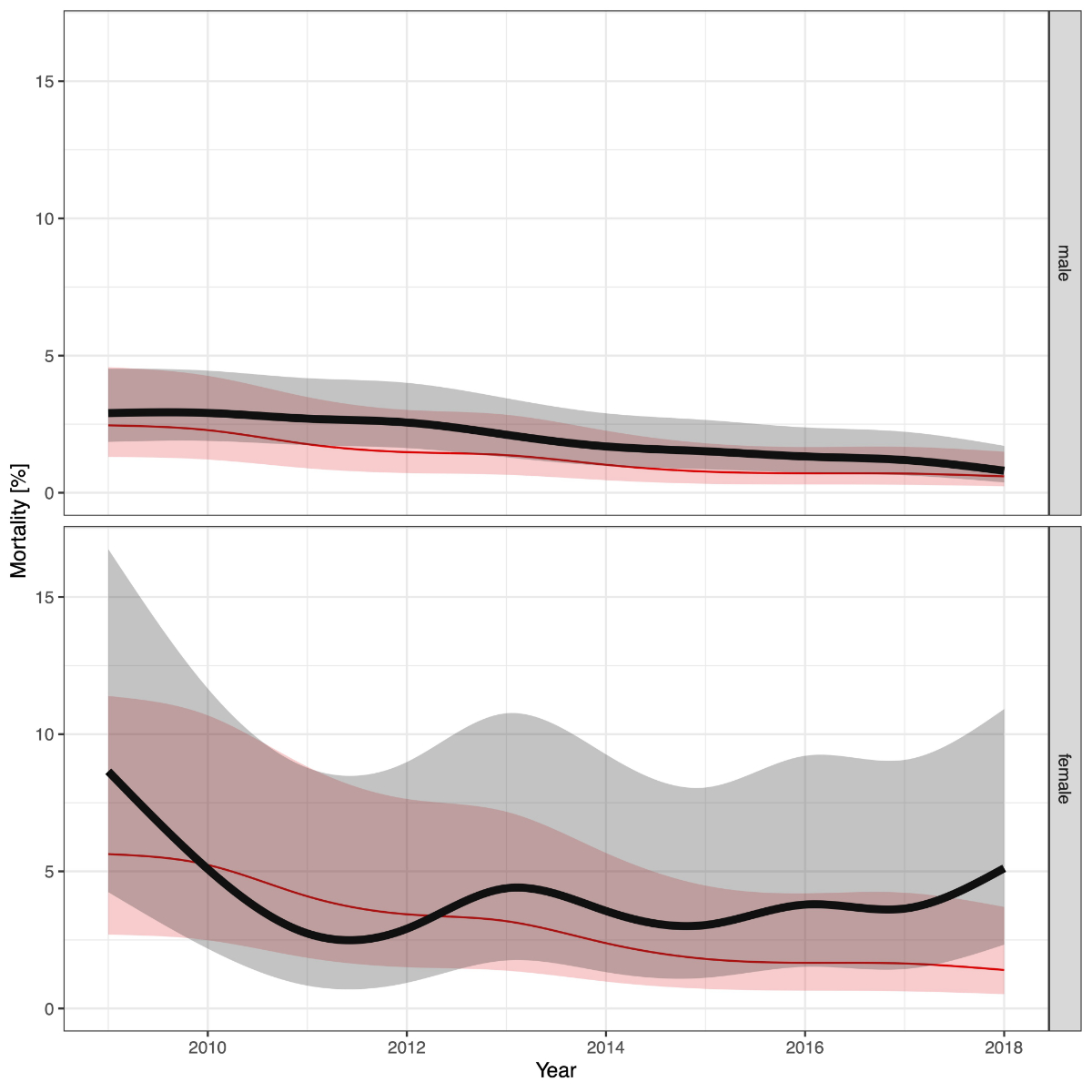
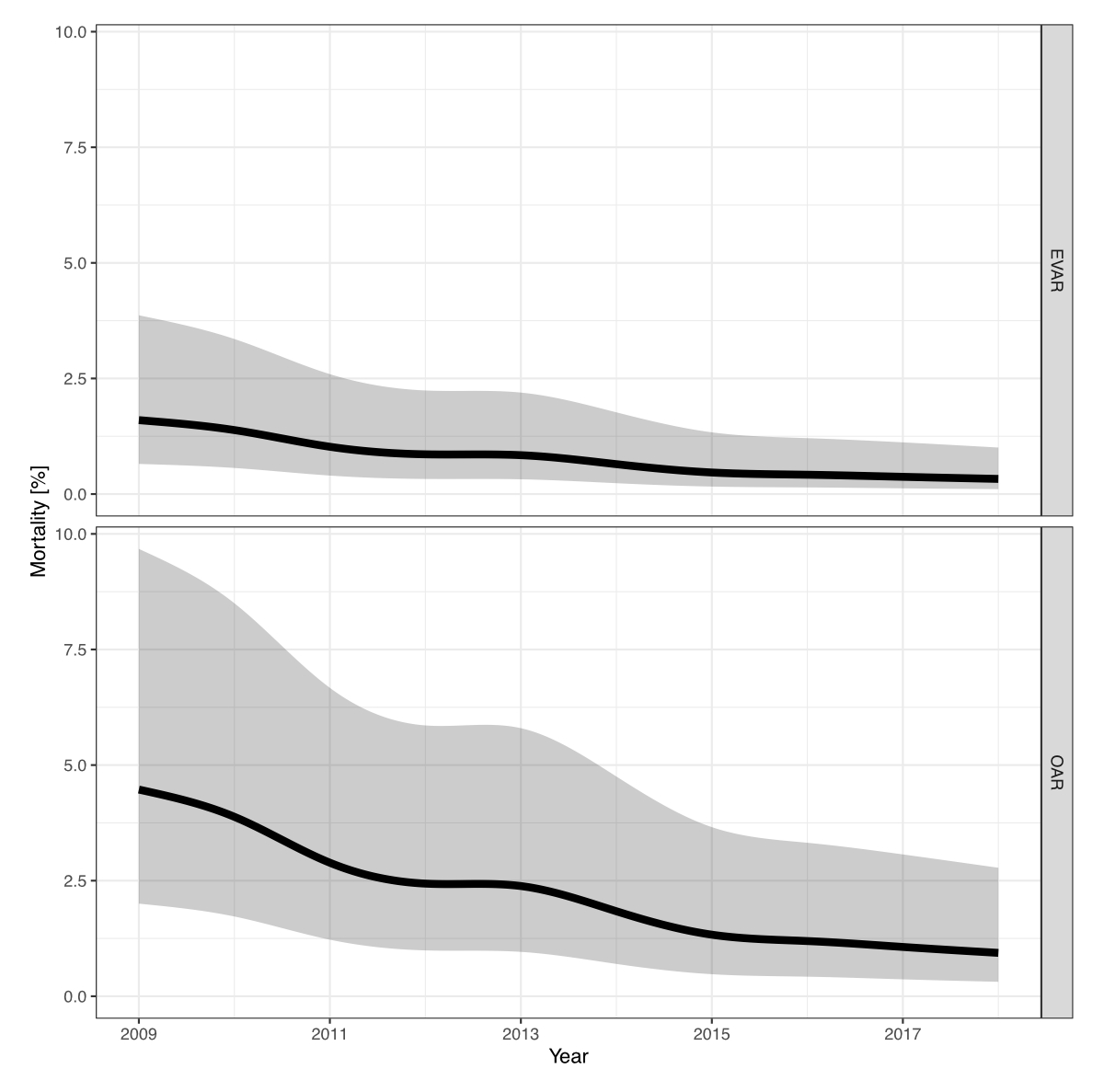
The adjusted mortality rates for treatment of nrAAA decreased from 2.4% (95% CI 1.3–4.5%) in 2009 to 0.6% (95% CI 0.2–1.5%) in 2018 in men, and from 5.5% (95% CI 2.6–11.2%) to 1.4% (95% CI 0.5–3.6%) in women (fig. 4 and table 2).
The adjusted mortality rates for treatment of nrAAA decreased from 1.6% (95% CI 0.6–3.8%) in 2009 to 0.3% (95% CI 0.1–1.0%) in 2018 in cases treated by EVAR, and from 4.4% (95% CI 2.0–9.6%) to 0.9% (95% CI 0.3–2.8%) in cases treated by OAR (supplementary fig. S2).
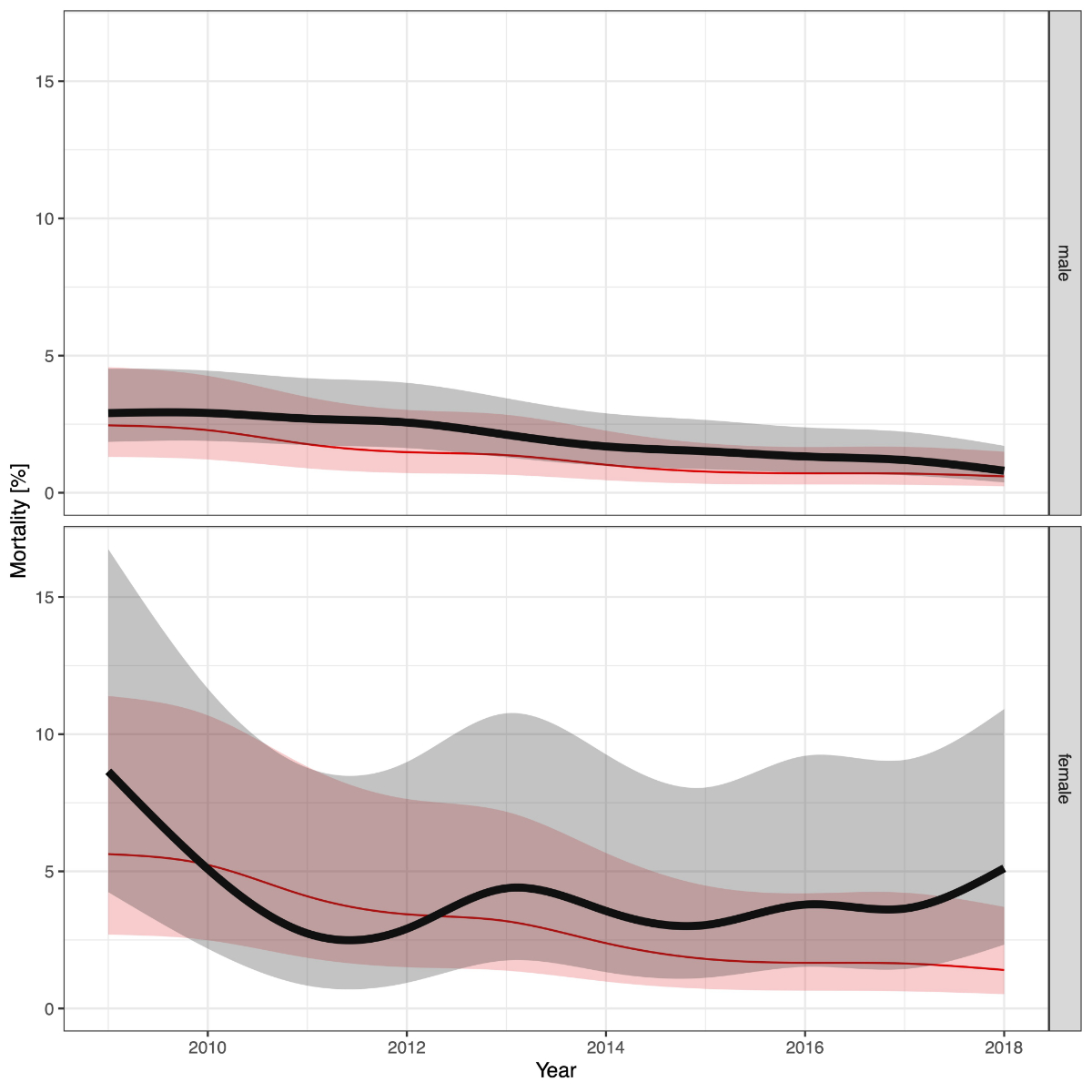
Figure 4 Hospital mortality of patients treated for nonruptured abdominal aortic aneurysm. Smoothed hospital mortality rates of patients treated for nonruptured abdominal aortic aneurysms stratified by sex. The solid black line shows the raw mortality rate, the grey area shows the corresponding 95% confidence interval. The red line shows the mortality rate adjusted for age, sex, year of treatment, van Walraven score.
Table 2 Treatment outcomes.
|
Nonruptured AAA
|
Ruptured AAA
|
|
EVAR, n = 4849 |
OAR, n = 3449 |
EVAR, n = 390 |
OAR, n = 733 |
Conservative, n = 1307 |
| In-hospital mortality, n (%) |
52 (1.1) |
130 (3.8) |
84 (21.5) |
175 (23.9) |
769 (58.8) |
| Type of discharge |
Home,n (%) |
4'383 (90.4) |
2'530 (73.4) |
150 (38.5) |
223 (30.4) |
397 (30.4) |
| Care home, n (%) |
55 (1.1) |
30 (0.9) |
10 (2.6) |
14 (1.9) |
41 (3.1) |
| Rehabilitation, n (%) |
233 (4.8) |
576 (16.7) |
75 (19.2) |
233 (31.8) |
78 (6.0) |
| Acute care hospital, n (%) |
104 (2.1) |
153 (4.4) |
61 (15.6) |
85 (11.6) |
1 (0.1) |
| Other, n (%) |
22 (0.5) |
30 (0.9) |
10 (2.6) |
3 (0.4) |
21 (1.6) |
| Length of stay OECD, median (IQR) |
6 (4 to 9) |
12 (9 to 16) |
11 (6 to 20) |
15 (9 to 24) |
4 (1 to 15) |
| Length of stay DRG, median (IQR) |
5 (4 to 8) |
11 (9 to 15) |
11 (5 to 20) |
14 (9 to 23) |
3 (1 to 15) |
| Length of stay ICU, median (IQR) |
0 (0 to 20) |
23 (0 to 54) |
28 (0 to 91) |
50 (16 to 189) |
0 (0 to 0) |
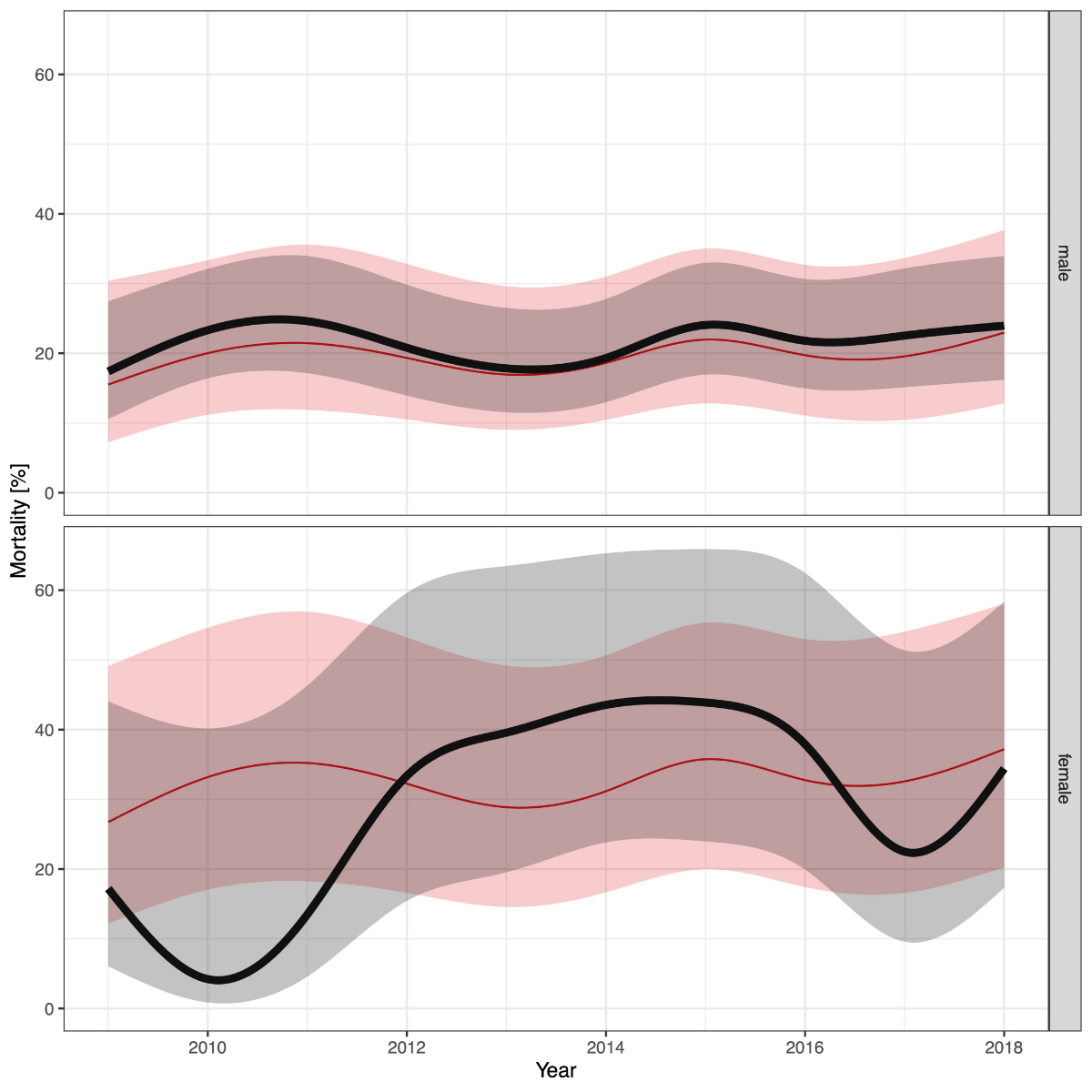
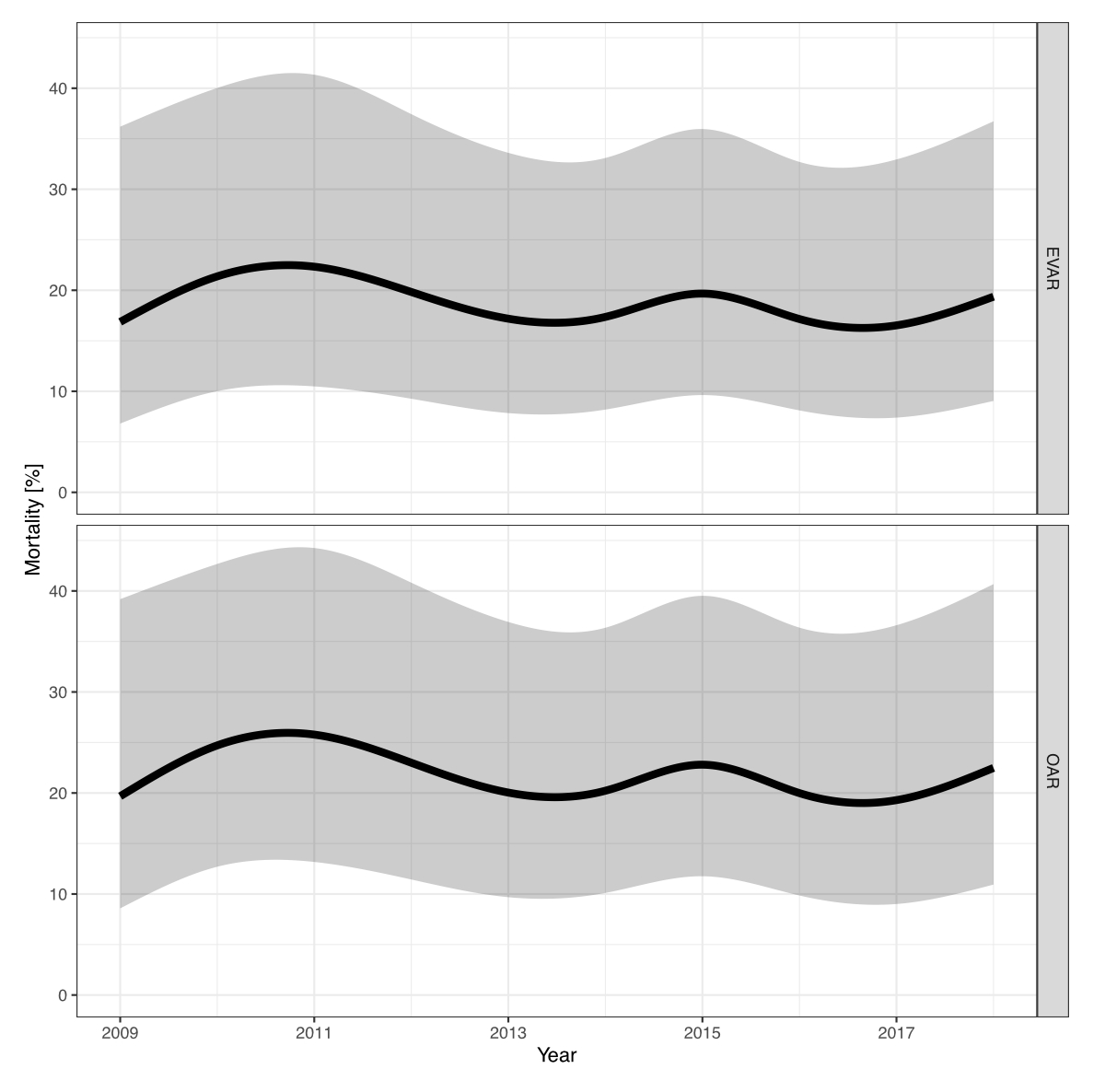
The adjusted mortality rates for treatment of rAAA remained high without relevant improvements for either sex (fig. 5. The overall adjusted mortality rate was 32.4% (95% CI 24.1–42.1%) in women and 19.7% (95% C: 16.8–22.8%) in men.
The overall adjusted mortality rate was 18.5% (95% CI 12.9–25.8%) for EVAR and 22.0% (95% CI 16.3–28.9%) for OAR.
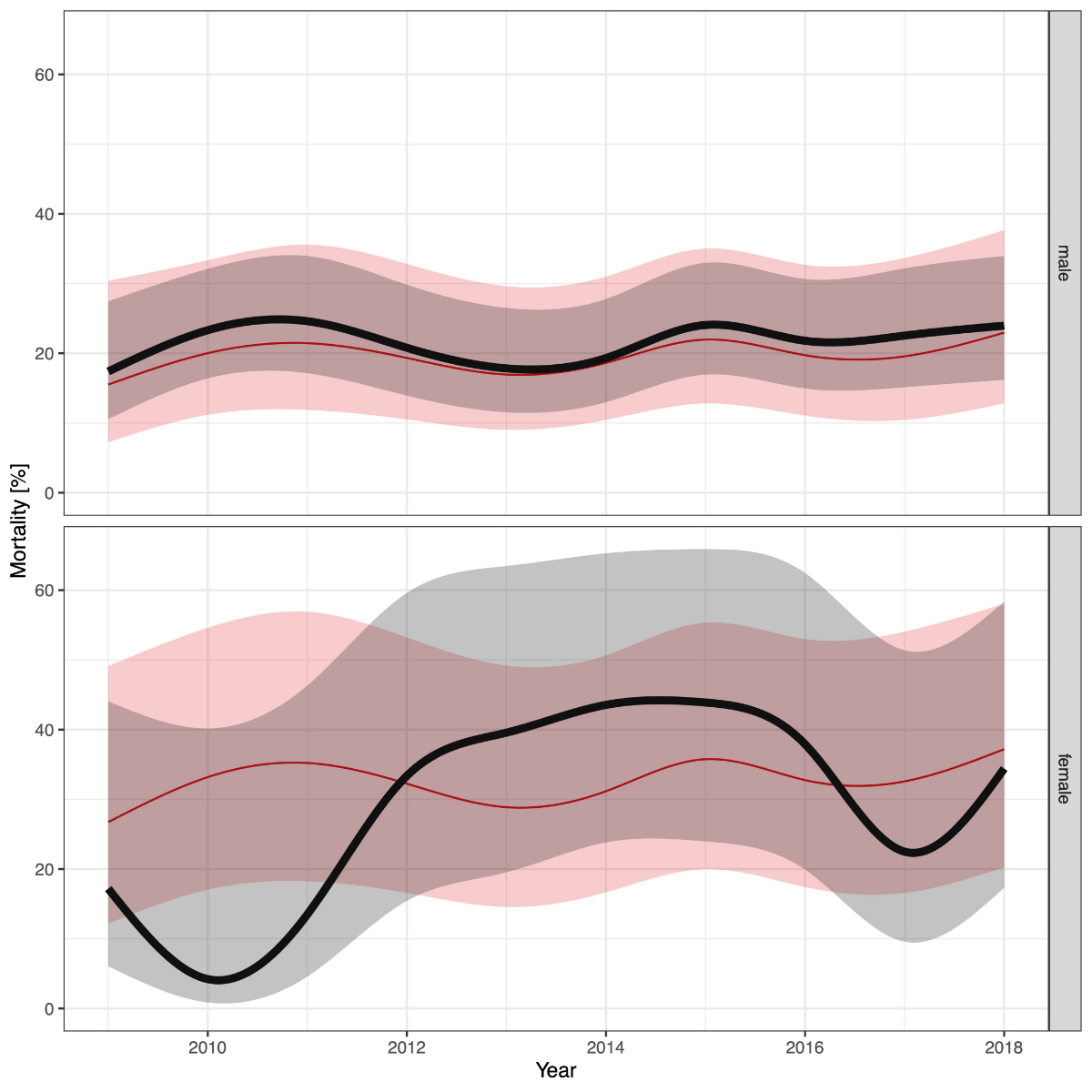
Figure 5 Hospital mortality of patients treated for ruptured abdominal aortic aneurysm. Smoothed hospital mortality rates of patients treated for ruptured abdominal aortic aneurysms stratified by sex. The solid black line shows the raw mortality rate, the grey area shows the corresponding 95% confidence interval. The red line shows the mortality rate adjusted for age, sex, year of treatment, van Walraven score.
Discussion
This is the first study to show the nationwide hospital incidence of AAA treatment in Switzerland. This case-related hospital discharge data can be used within its limitations to estimate the actual incidence and treatment outcomes of patients treated for AAA.
In the analysed period, the hospital incidence for patients treated with EVAR or OAR for nrAAA was roughly constant for both sexes. In line with previously published studies, the overall age standardised cumulative hospital incidence rates for treatment of rAAA and nrAAA were significantly higher in men than in women [1, 5, 18, 19]. The incidence rates are comparable to epidemiological data from other European countries and the USA [1, 5, 18, 19].
A previously described but not fully understood gender gap in survival rates was also detected in Switzerland [19]. The adjusted in-hospital mortality rates for patients treated for nrAAA decreased in the last decade substantially: for men from 2.4% in 2009 to 0.6% in 2018; for women in the same period from 5.5% to 1.4%. Epidemiological data from the 2011 VASCUNET report including patients treated from 2005 to 2009 in eight European countries and Australia showed a pooled mortality rate of 2.6% (95% CI 2.4–2.8%) in men and 4.0% (95% CI 3.4–4.6%) in women [1]. More recent German data for men treated from 2005 to 2014 reported a mortality rate of 3.3% [5]. For women, the mortality rate was higher in 2009 but was comparable to international data thereafter. Though, due to the relatively low number of women treated for AAA, the 95% CI for the observed mortality rates are wide and hinder reliable comparisons.
These advances in survival rates might be explained not only by the broad use of EVAR, which is known to lower in-hospital mortality, but also by the development of specialised vascular surgery clinics in Switzerland in the last decade. Our data were in line with previous publications and confirmed lower mortality rates in patients treated for nrAAA by means of endovascular as compared with open aortic repair [5]. Due to a high risk of confounding and the inability to address this with the available data, OAR and EVAR were not formally compared.
The adjusted mortality rates for the treatment rAAA of 19.7% in men and 32.4% in women were substantially lower in Switzerland than historical international data reporting overall mortality rates of about 35–45% [5, 20, 21]. In line with international data, mortality was substantially higher in women than men [5, 20]. In contrast to the elective setting, no improvement in survival in patients treated for rAAA was observed in the last decade for either sex. Interpretation and direct comparison of results from patients operated on for rAAA is hindered by the lack of standardised reporting of turndown rates for patients presenting with a rAAA. Of note, survival rates were similar in patients treated with EVAR or OAR.
Proportion of ruptures
In contrast to epidemiological data from Germany, the USA, Sweden, England, Wales, and Scotland, we could neither show an increasing incidence of treatment in the elective setting (nonruptured aneurysms) nor a decreasing incidence for ruptures in Switzerland [1–3, 5]. The proportion of patients treated for rAAA (12.0%) was constant in the observed period and is in line with current international epidemiological data [22]. However, we observed a relatively high proportion of patients presenting with rAAA that were conservatively treated (54%). Kuehnl et al. reported a rate of only 43% in conservatively treated patients with rAAA [5]. This study included patients with ruptured aneurysms as a secondary diagnosis who did not receive surgical treatment, a cohort that was not included in our study. Therefore, a comparable rate for conservatively treated patients in Germany would be even lower than the 43%. The substantial difference in the rate of conservatively treated patients with rAAA could be explained either by a higher turndown rate or by a larger proportion of patients transferred to regional hospitals after successful treatment of the aneurysm. These data do not allow for a distinction between these two cohorts. Further, within Switzerland, the proportion of conservatively managed patients with rAAA was substantially higher in level 2 hospitals than in level 1 hospitals. To some extent, this could be explained by the fact that a proportion of patients are transferred to level 2 hospitals after successful treatment of ruptured aneurysms in level 1 hospitals. Detailed information on the burden of comorbidities or the haemodynamic situation on admission is not available. Still, these remarkable differences need further exploration in future research.
The persistently high rate of rAAA in Switzerland might be explained to some extent by the fact that no nationwide screening programme exists. Several screening programmes have resulted in a significant reduction of aneurysm-related mortality in different countries and cost effectiveness has been demonstrated [23, 24]. These findings resulted in a clear recommendation in the current clinical practice guidelines of the ESVS to screen all men at age 65 years for an AAA with a single ultrasound scan (class 1, level A) [25]. This study demonstrated that approximately 75% of all patients presenting with rAAA were in the proposed target group for screening (male, age ≥65). The feasibility of screening in Switzerland has been demonstrated in a pilot study by Engelberger et al. in the Canton Ticino [26]. Nevertheless, no nationwide screening programme has been implemented yet.
The endovascular era in Switzerland
In 2009, 46.5% of patients with nrAAA were treated with EVAR. Today, 67% of all patients with nrAAA are treated with EVAR. This trend is even more pronounced in Germany, where in 2014 already 75% of all men and 68% of all women with nrAAA were treated with endovascular repair [21]. In the emergency setting, the proportion of patients treated for rAAA increased from 29.1% in 2009 to 44.3% in 2018. In contrast, German data showed a lower percentage of endovascular therapy in the emergency setting (16% in 2009 to 36% in 2014, more recent data up to 2018 are not available) [21]. These findings might be explained by the more advanced centralisation for treatment of rAAA to specialised centres in Switzerland.
Centralisation of abdominal aortic aneurysm treatment
Approximately 10% (841 of 8321) of all patients with nrAAA were treated in smaller hospitals. It has been demonstrated that lower hospital volume is associated with increased mortality [22, 28, 29]. Therefore, current treatment guidelines recommend that AAA repair should not be performed in hospitals with an annual caseload <20 [30]. The dataset did not allow exploratory analysis on annual caseload per hospital and treatment outcomes since hospital identifiers were not available. However, a recent Swissvasc report demonstrated that the participating smaller hospitals do not achieve this recommended minimum annual caseload [8].
On the other hand, most patients presenting with ruptured aneurysms are treated at specialised centres (97.4% at university hospitals or tertiary referral centres). Almost all patients presenting in smaller hospitals with rAAAs (n = 423) were referred. It has been demonstrated that a limited time delay in the surgical treatment of patients with ruptured aneurysms for centralisation is justified and might increase the overall survival probability [20, 21, 31]. In Switzerland, 24/7 helicopter emergency medical services enable the transfer of most of the patients with a rAAA from smaller hospitals to centres within one hour [32]. Thereby, the excellent rescue chain allows the centralisation of aortic interventions without deprivation of rural areas.
Limitations
There are several limitations to this analysis. First, the data are not clinical but administrative, using ICD and CHOP codes. This brings the main advantage compared with registry data that a nearly complete coverage of the Swiss population is achieved. Thereby, selection bias and the risk for information bias for hard outcomes such as mortality is presumably low. However, individual clinical data were not available and residual selection bias due to coding errors cannot be ruled out. In addition, the data allow non-independent observations of patients treated twice for the same ICD code, which leads to double counting and distorts the incidence rates. The proportion of such patients remains unknown but is likely to be negligible.
Second, comparison of mortality rates with international data is limited since adjustments were only possible for age, sex, and the van Walraven comorbidity index, which reflects neither the cardiovascular risk profile nor the functional capacity of the treated individuals.
Third, we excluded patients with a secondary diagnosis of rAAA who did not receive surgical treatment to exclude patients with a previously successfully treated ruptured aneurysm. Thereby, an unknown proportion of patients with a rAAA occurring at the time of the index hospitalisation might have been excluded, leading to an underestimation of the turndown rate for patients presenting with a ruptured aneurysm. On the other hand, patients who were transferred after successful surgical treatment of a rAAA and admitted to other hospitals with rAAA as their primary diagnosis fall into the same category, which obscures the actual turndown rate.
Fourth, we only included inpatient treatments. Outpatient interventions were not included in this analysis; however, the proportion of highly selected patients treated with EVAR in an outpatient setting is presumably negligible.
Implications for research and practice
The fact that mortality rates are still significantly higher in females than males for the treatment of nrAAA asks for further research leading to an improvement of perioperative patient care. Further, the persistently high proportion of patients presenting with rAAA and the remarkably high turndown rate for patients presenting with ruptured aneurysms in Switzerland raises questions on the efficacy of a nationwide target population screening program.
Conclusion
The standardised hospital incidence rates for nonruptured and ruptured abdominal aortic aneurysms remained unchanged in the observed decade. The incidence of rAAA is substantially higher than in Germany and a good half of these patients are not treated surgically. No decrease in the proportion of patients treated for ruptures was observed. Given the low mortality rates in the elective setting, but the persistently high mortality rate in an emergency, efforts to identify and treat more AAA before they rupture is needed.
Author contributions
UH: conception and design, statistical analysis, revision of the manuscript, agreed to the publication of this manuscript and to be named as an author. AK: study conception and design, interpretation of the analysis, revision of the manuscript, agreed to the publication of this manuscript and to be named as an author. ALM: study conception and design, interpretation of the analysis, writing of the manuscript, agreed to the publication of this manuscript and to be named as an author. LM: study conception and design, interpretation of the analysis, writing of the manuscript, agreed to the publication of this manuscript and to be named as an author. BR: study conception and design, interpretation of the analysis, revision of the manuscript, agreed to the publication of this manuscript and to be named as an author. KS: study conception and design, statistical analysis, revision of the manuscript, agreed to the publication of this manuscript and to be named as an author. AZ: Study conception and design, interpretation of the analysis, revision of the manuscript, agreed to the publication of this manuscript and to be named as an author.
Lorenz Meuli, MD MSc
Department for Vascular Surgery
University Hospital Zurich
CH-8091 Zurich
lorenz.meuli[at]usz.ch
References
1.
Mani K
,
Lees T
,
Beiles B
,
Jensen LP
,
Venermo M
,
Simo G
, et al.
Treatment of abdominal aortic aneurysm in nine countries 2005-2009: a vascunet report. Eur J Vasc Endovasc Surg. 2011 Nov;42(5):598–607. https://doi.org/10.1016/j.ejvs.2011.06.043
2.
Anjum A
,
Powell JT
. Is the incidence of abdominal aortic aneurysm declining in the 21st century? Mortality and hospital admissions for England & Wales and Scotland. Eur J Vasc Endovasc Surg. 2012 Feb;43(2):161–6. https://doi.org/10.1016/j.ejvs.2011.11.014
3.
Mani K
,
Björck M
,
Wanhainen A
. Changes in the management of infrarenal abdominal aortic aneurysm disease in Sweden. Br J Surg. 2013 Apr;100(5):638–44. https://doi.org/10.1002/bjs.9046
4.
Schermerhorn ML
,
Bensley RP
,
Giles KA
,
Hurks R
,
Oʼmalley AJ
,
Cotterill P
, et al.
Changes in abdominal aortic aneurysm rupture and short-term mortality, 1995-2008: a retrospective observational study. Ann Surg. 2012 Oct;256(4):651–8. https://doi.org/10.1097/SLA.0b013e31826b4f91
5.
Kühnl A
,
Erk A
,
Trenner M
,
Salvermoser M
,
Schmid V
,
Eckstein H-H
. Incidence, Treatment and Mortality in Patients with Abdominal Aortic Aneurysms. Deutsches Aerzteblatt Online. 2017 Jun 5;
6.
Wanhainen A
,
Verzini F
,
Van Herzeele I
,
Allaire E
,
Bown M
,
Cohnert T
, et al.; Esvs Guidelines Committee
. Editor’s Choice - European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur J Vasc Endovasc Surg. 2019 Jan;57(1):8–93. https://doi.org/10.1016/j.ejvs.2018.09.020
7.
Thomas DM
,
Hulten EA
,
Ellis ST
,
Anderson DM
,
Anderson N
,
McRae F
, et al.
Open versus Endovascular Repair of Abdominal Aortic Aneurysm in the Elective and Emergent Setting in a Pooled Population of 37,781 Patients: A Systematic Review and Meta-Analysis. ISRN Cardiol. 2014 Apr;2014:149243. https://doi.org/10.1155/2014/149243
8.
Meuli L
,
Lattmann T
. Versorgungsrealität von Aortenerkrankungen in der Schweiz. Gefasschirurgie. 2021 Jun;26(4):261–9. https://doi.org/10.1007/s00772-021-00782-0
9.
Trenner M
,
Kuehnl A
,
Reutersberg B
,
Salvermoser M
,
Eckstein HH
. Nationwide analysis of risk factors for in-hospital mortality in patients undergoing abdominal aortic aneurysm repair. Br J Surg. 2018 Mar;105(4):379–87. https://doi.org/10.1002/bjs.10714
10.
Trenner M
,
Salvermoser M
,
Busch A
,
Schmid V
,
Eckstein H-H
,
Kühnl A
. The effects of minimum caseload requirements on management and outcome in abdominal aortic aneurysm repair. Deutsches Aerzteblatt Online. 2020 Nov 27;
11. Statistik der stationären Betriebe des Gesundheitswesens. Krankenhaustypologie [Internet]. Statistik der stationären Betriebe des Gesundheitswesens. Krankenhaustypologie. 2013. 9 p. (2006). Available from: https://www.bfs.admin.ch/hub/api/dam/assets/169879/master
12.
https://www.pxweb.bfs.admin.ch/pxweb/de/px-x-0102010000_101/-/px-x-0102010000_101.px. Federal Statistical Office - Permanent and non-permanent resident population by institutional units, citizenship (category), sex and age. 2020.
13.
https://www.bfs.admin.ch/bfs/en/home/statistics/population.assetdetail.14367975.html. Federal Statistical Office - Population Data. 2020.
14.
https://www.gbe-bund.de/gbe/pkg_isgbe5.prc_menu_olap?p_uid=gast&p_aid=3767823&p_sprache=D&p_help=0&p_indnr=1000&p_indsp=&p_ityp=H&p_fid=. Gesund¬heits-bericht¬erstat¬tung des Bundes. 2020.
15.
Altman D
,
Machin D
,
Bryant T
,
Gardner M
. Statistics with Confidence: Confidence Intervals and Statistical Guidelines, 2nd Edition [Internet]. 2000 [cited 2021 Dec 5]. Available from: https://eprints.soton.ac.uk/393017/
16.
van Walraven C
,
Austin PC
,
Jennings A
,
Quan H
,
Forster AJ
. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009 Jun;47(6):626–33. https://doi.org/10.1097/MLR.0b013e31819432e5
17.
R Core Team
. (2013). R: A language and environment for statistical computing. URL http://www.R-project.org/. n.d. Vienna, Austria: R Foundation for Statistical Computing; 2013.
18.
Svensjö S
,
Björck M
,
Gürtelschmid M
,
Djavani Gidlund K
,
Hellberg A
,
Wanhainen A
. Low prevalence of abdominal aortic aneurysm among 65-year-old Swedish men indicates a change in the epidemiology of the disease. Circulation. 2011 Sep;124(10):1118–23. https://doi.org/10.1161/CIRCULATIONAHA.111.030379
19.
Stoberock K
,
Kölbel T
,
Atlihan G
,
Debus ES
,
Tsilimparis N
,
Larena-Avellaneda A
, et al.
Gender differences in abdominal aortic aneurysm therapy - a systematic review. Vasa. 2018 Jun;47(4):267–71. https://doi.org/10.1024/0301-1526/a000703
20.
Powell JT
,
Hinchliffe RJ
,
Thompson MM
,
Sweeting MJ
,
Ashleigh R
,
Bell R
, et al.; IMPROVE trial investigators
. Observations from the IMPROVE trial concerning the clinical care of patients with ruptured abdominal aortic aneurysm. Br J Surg. 2014 Feb;101(3):216–24. https://doi.org/10.1002/bjs.9410
21.
Mandawat A
,
Mandawat A
,
Sosa JA
,
Muhs BE
,
Indes JE
. Endovascular repair is associated with superior clinical outcomes in patients transferred for treatment of ruptured abdominal aortic aneurysms. J Endovasc Ther. 2012 Feb;19(1):88–95. https://doi.org/10.1583/11-3651.1
22.
Scali ST
,
Beck A
,
Sedrakyan A
,
Mao J
,
Behrendt CA
,
Boyle JR
, et al.
Editor’s Choice - Optimal Threshold for the Volume-Outcome Relationship After Open AAA Repair in the Endovascular Era: Analysis of the International Consortium of Vascular Registries. Eur J Vasc Endovasc Surg. 2021 May;61(5):747–55. https://doi.org/10.1016/j.ejvs.2021.02.018
23.
Søgaard R
,
Lindholt JS
. Cost-effectiveness of population-based vascular disease screening and intervention in men from the Viborg Vascular (VIVA) trial. Br J Surg. 2018 Sep;105(10):1283–93. https://doi.org/10.1002/bjs.10872
24.
Thompson SG
,
Ashton HA
,
Gao L
,
Scott RAP
. Screening men for abdominal aortic aneurysm: 10 year mortality and cost effectiveness results from the randomised Multicentre Aneurysm Screening Study. BMJ. 2009 Jun 24;338(jun24 2):b2307–b2307.
25.
Wanhainen A
,
Verzini F
,
Van Herzeele I
,
Allaire E
,
Bown M
,
Cohnert T
, et al.; Esvs Guidelines Committee
. Editor’s Choice - European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur J Vasc Endovasc Surg. 2019 Jan;57(1):8–93. https://doi.org/10.1016/j.ejvs.2018.09.020
26.
Engelberger S
,
Rosso R
,
Sarti M
,
Del Grande F
,
Canevascini R
,
van den Berg JC
, et al.
Ultrasound screening for abdominal aortic aneurysms. Swiss Med Wkly. 2017 Mar;147(0910):w14412.
28.
Landon BE
,
O’Malley AJ
,
Giles K
,
Cotterill P
,
Schermerhorn ML
. Volume-outcome relationships and abdominal aortic aneurysm repair. Circulation. 2010 Sep;122(13):1290–7. https://doi.org/10.1161/CIRCULATIONAHA.110.949172
29.
Cho JS
,
Kim JY
,
Rhee RY
,
Gupta N
,
Marone LK
,
Dillavou ED
, et al.
Contemporary results of open repair of ruptured abdominal aortoiliac aneurysms: effect of surgeon volume on mortality. J Vasc Surg. 2008 Jul;48(1):10–7. https://doi.org/10.1016/j.jvs.2008.02.067
30.
Wanhainen A
,
Verzini F
,
Van Herzeele I
,
Allaire E
,
Bown M
,
Cohnert T
, et al.; Esvs Guidelines Committee
. Editor’s Choice - European Society for Vascular Surgery (ESVS) 2019 Clinical Practice Guidelines on the Management of Abdominal Aorto-iliac Artery Aneurysms. Eur J Vasc Endovasc Surg. 2019 Jan;57(1):8–93. https://doi.org/10.1016/j.ejvs.2018.09.020
31.
Hinchliffe RJ
,
Ribbons T
,
Ulug P
,
Powell JT
. Transfer of patients with ruptured abdominal aortic aneurysm from general hospitals to specialist vascular centres: results of a Delphi consensus study. Emerg Med J. 2013 Jun;30(6):483–6. https://doi.org/10.1136/emermed-2012-201239
32.
Meuli L
,
Zimmermann A
,
Menges AL
,
Tissi M
,
Becker S
,
Albrecht R
, et al.
Helicopter emergency medical service for time critical interfacility transfers of patients with cardiovascular emergencies. Scand J Trauma Resusc Emerg Med. 2021 Dec;29(1):168. https://doi.org/10.1186/s13049-021-00981-4
Appendix
|
Package
|
Version
|
| ggpubr |
0.4.0 |
| DescTools |
0.99.44 |
| tableone |
0.13.0 |
| comorbidity |
0.5.3 |
| gridExtra |
2.3 |
| readxl |
1.3.1 |
| forcats |
0.5.1 |
| stringr |
1.4.0 |
| dplyr |
1.0.8 |
| purrr |
0.3.4 |
| readr |
2.1.1 |
| tidyr |
1.1.4 |
| tibble |
3.1.6 |
| ggplot2 |
3.3.5 |
| tidyverse |
1.3.1 |
| reporttools |
1.1.3 |
| xtable |
1.8-4 |
| kableExtra |
1.3.4 |
| knitr |
1.37 |
| multcomp |
1.4.17 |
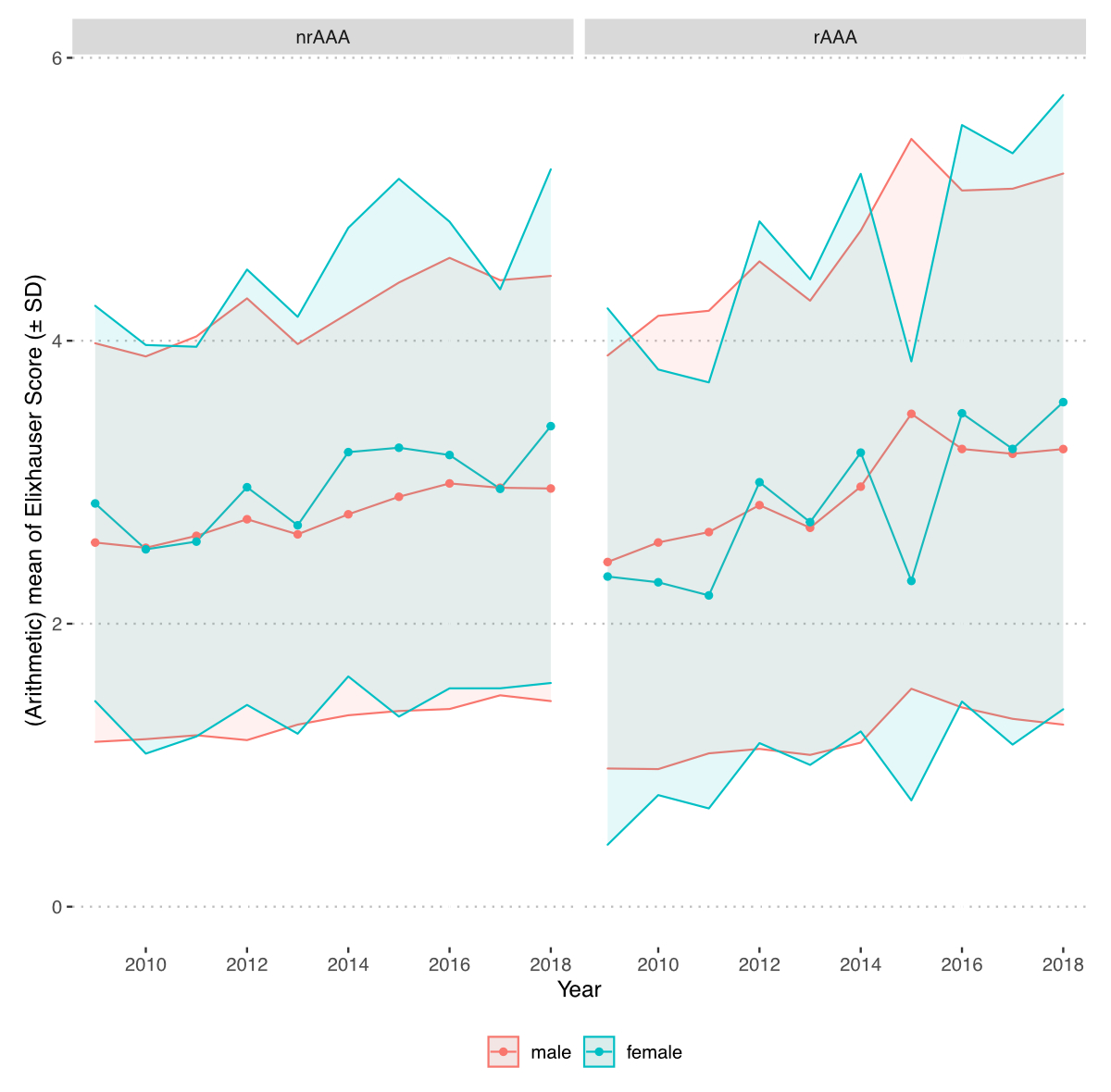
Figure S1 Comorbidities of patients treated for abdominal aortic aneurysm (AAA). Comorbidities were summarised using a sum score of weighted Elixhauser ICD-10 diagnosis groups according to van Walraven.18 The score is calculated from grouped ICD-10 diagnosis per patient and weighted based on the association of each category and mortality. The figure shows the mean score per year stratified by sex and diagnosis (nonruptured AAA [nrAAA] versus ruptured AAA [rAAA]). SD = standard deviation.
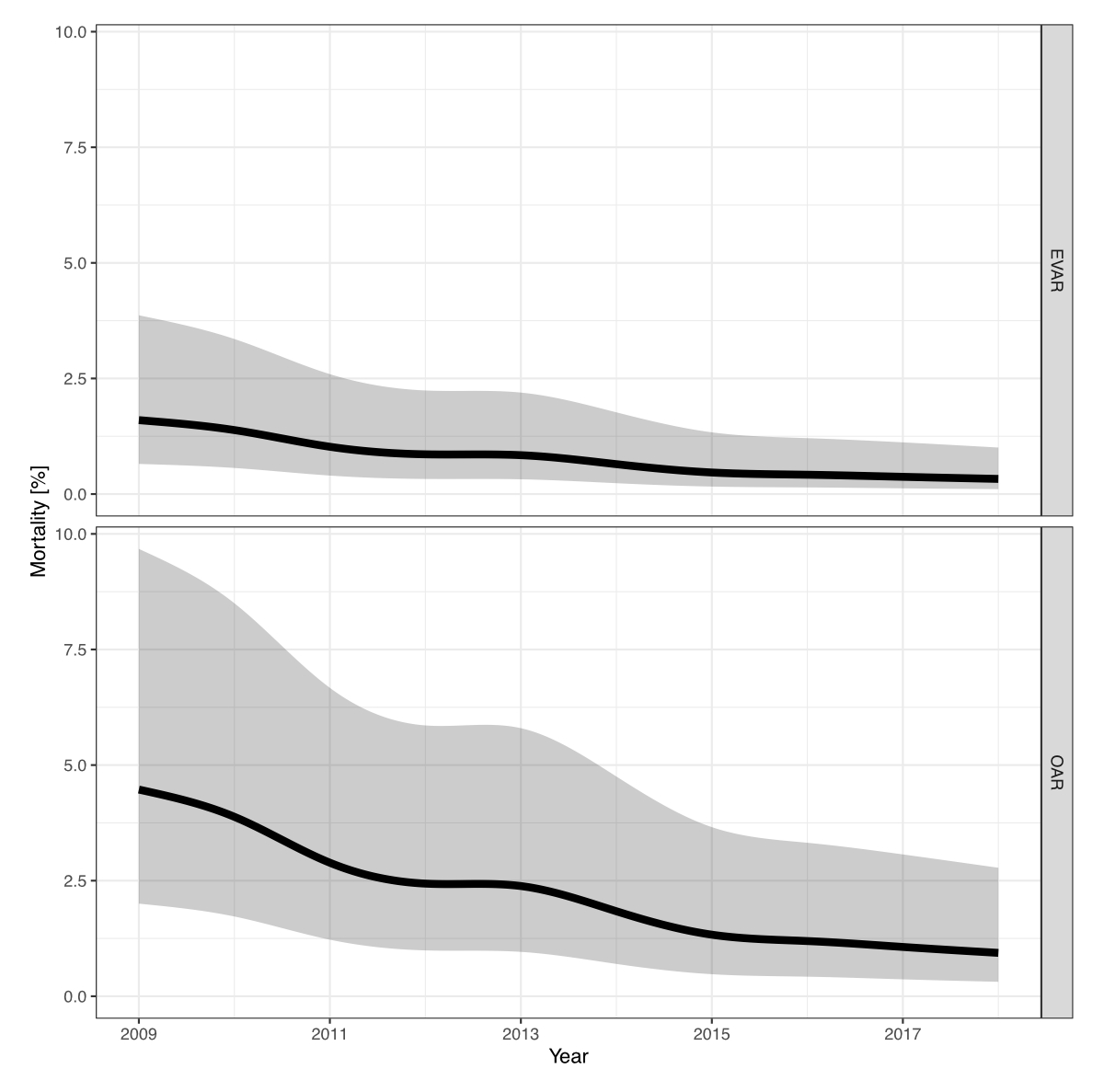
Figure S2 Mortality of patients treated for nonruptured abdominal aortic aneurysms (nrAAA) stratified by treatment. Smoothed adjusted in-hospital mortality rates with 95% confidence interval of patients treated for nrAAA stratified by treatment. Adjustments were made for age, sex, year of treatment and Elixhauser score. EVAR: endovascular aortic repair; OAR: open aneurysm repair.
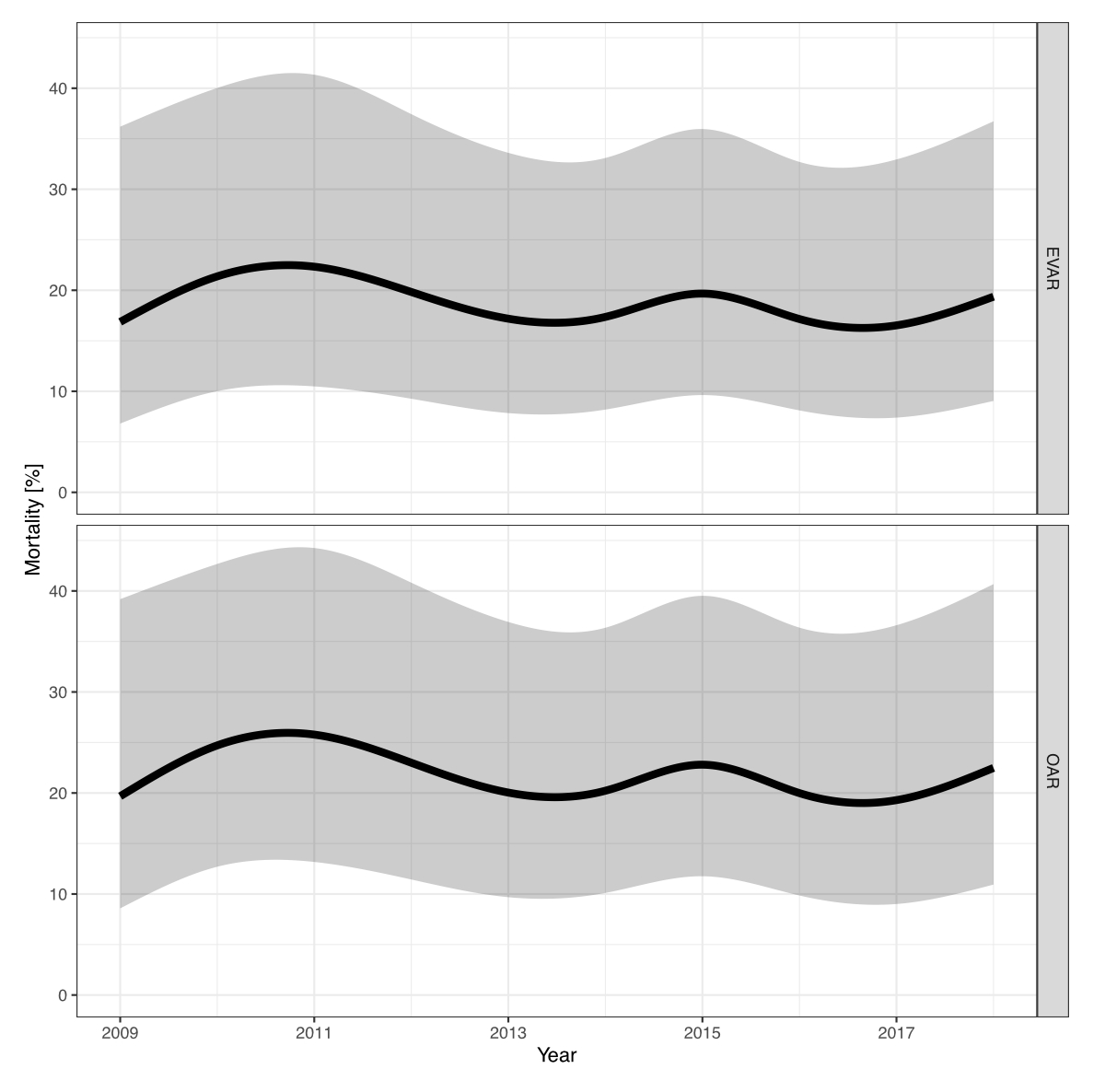
Figure S3 Hospital mortality of patients treated for ruptured abdominal aortic aneurysm (rAAA) stratified by treatment. Smoothed adjusted hospital mortality rates with 95% confidence interval of patients treated for rAAA stratified by treatment. Adjustments were made for age, sex, year of treatment and Elixhauser score. EVAR: endovascular aortic repair. OAR: open aneurysm repair.