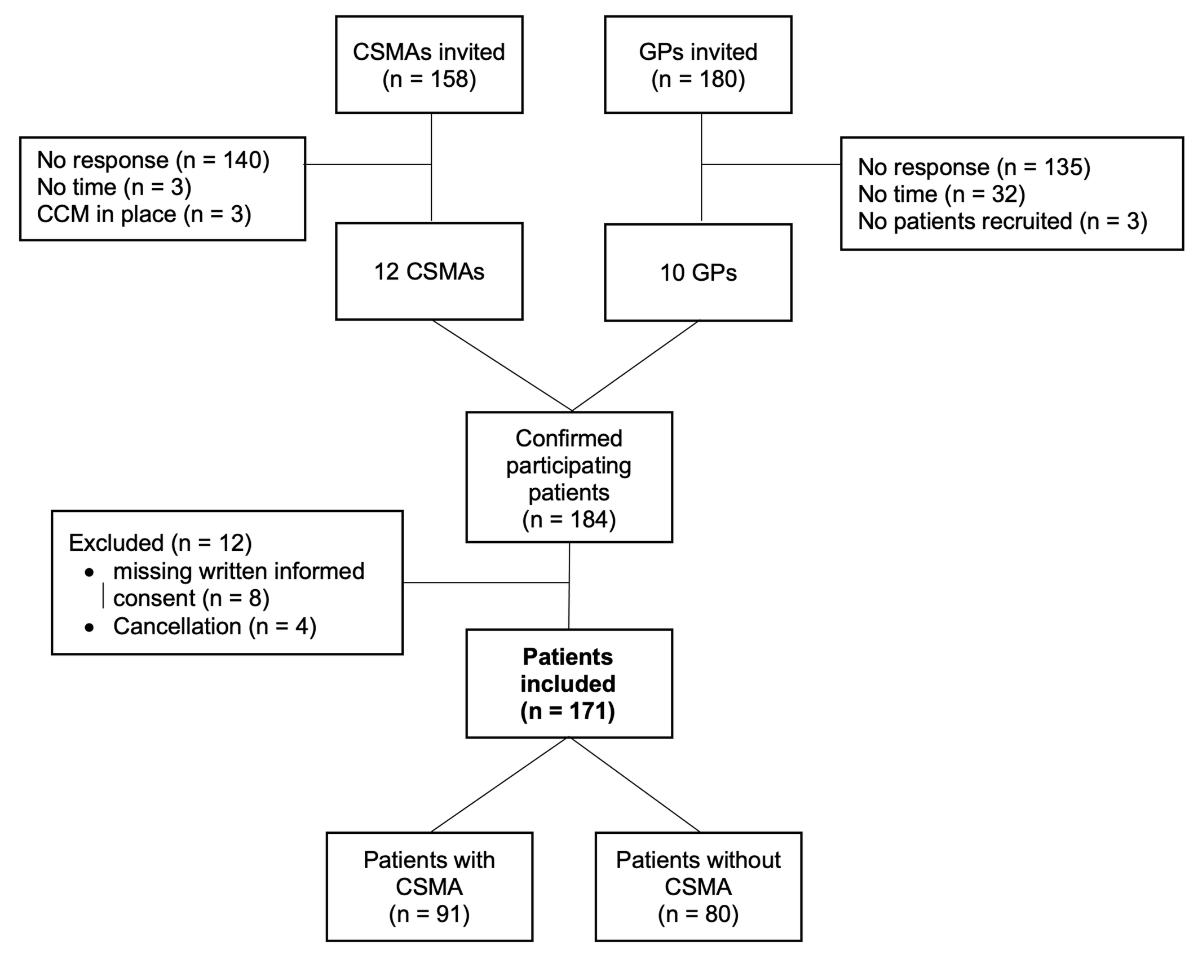
Figure 1 Study flow chart.
DOI: https://doi.org/10.4414/SMW.2022.w30180
Interprofessional collaboration in health care aims, among other goals, at improving the treatment of patients with chronic diseases [1]. There have been national and international calls to promote interprofessional collaboration in recent years [2, 3], with new roles defined [4, 5], but implementation is still lagging behind in Switzerland. The reasons for this are linked to both organizational and financial difficulties as well as problems related to transferring responsibility from general practitioners (GPs) to practice staff [6].
Currently, the care for patients with type 2 diabetes mellitus is an essential field for improvement [6–10]. Type 2 diabetes is a significant cause of cardiovascular diseases and death worldwide [11]. In Switzerland, treatment costs for cardiovascular diseases and diabetes mellitus account for over 10 billion Swiss francs or 15.6% of total health costs per year [12]. Good disease control means better quality of life for patients [13, 14] and fewer disease-specific complications, especially cardiovascular diseases and hospitalizations [15].
A shortage exists of GPs, particularly in rural regions in Switzerland [16]. The care deficit will intensify in the future for demographic reasons; 15% of GPs are over 65 years old [17]. At least another 10–15 years are needed before the deficit can be made up by young GPs [18]. At the same time, the number of patients with chronic diseases is rising, resulting in a gap in the care of the chronically ill. One promising model to overcome this imminent shortage is chronic care management (CCM) [19], in which health care professionals, e.g., medical practice assistants (in German “Medizinische PraxisassistentInnen”, MPA), medical practice coordinators (in German “Medizinische PraxiskoordinatorInnen”, MPK; in English specialized medical assistant, SMA) and advanced practice nurses (APNs) instead of GPs take over consultations.
Unlike an APN, who graduates from a university, an SMA is a trained MPA who has undergone additional work-based training to treat and coach chronically ill people and has received further training in management functions in medical practice. They must have at least three years of practical experience before taking the federal examination. The training is modular and can be completed individually during 2–5 years alongside their work. Through more than 300 classroom hours and an additional approximately 200 hours of self-study, aspiring SMAs acquire advanced competencies for the medical office that can relieve GPs’ workload and contribute to patient care. In addition to the elective modules on chronic care and quality management, further modules, depending on the SMA’s specialty (practice management role), can be chosen, e.g., counseling of long-term patients, dose-intensive x-ray, and accounting [20]. Clinical specialized medical assistants (CSMAs, in German “Medizinische Praxiskoordinatorin klinischer Richtung”) care for patients with a set of chronic conditions such as diabetes mellitus, cardiovascular diseases, rheumatoid arthritis, and pulmonary diseases. Lead specialized medical assistants (LSMAs) concentrate on medical practice management.
Previous studies [21, 22] have already shown a positive effect of integrated care in family care practices on cardiovascular risk factors and other clinical outcomes in diabetic patients, e.g. HbA1c value and length of hospital stay, and therefore cost containments [23, 24]. Diabetes management needs to be improved in screening, diagnosing, achieving reference values (HbA1c, LDL, blood pressure), and the adherence to annual follow-up eye and foot examinations [25, 26]. Patient education is one way to improve this but is a very time-consuming task for GPs. As a key element of CCM, good self-management influences disease management and clinical outcomes, directly contributing to reducing health care costs [27, 13]. CSMAs with clinical direction appear to be suited to support CCM. A total of 830 CSMAs have been trained in Switzerland since 2015 [28], most of them in practice-leading directions. Estimates from the Swiss Association of Medical Practice Professionals (Schweizerischer Verband Medizinischer Praxis-Fachpersonen, SVA) indicate that approximately 200 CSMAs with clinical direction are currently active in GP practices. However, the performance of CSMAs has not been studied yet.
We aimed to compare the quality of care for patients with type 2 diabetes in practices with and without CSMAs. Further, we aimed to investigate whether CSMA care models allow task shifting and the provision of interprofessional care while maintaining a high quality of care and we aimed to assess patient experiences with diabetes care in both care models.
This cross-sectional study collected retrospective data from the year before patients were included in the study. To validate the design, support recruitment, and promote the dissemination of the study, we formed a project group with members from all stakeholders involved: a patient with type 2 diabetes, the patient organization “Diabetesschweiz”, CSMAs, GPs with their professional associations, service providers and researchers. The Swiss Association of Medical Practice Professionals (Schweizerischer Verband Medizinischer Praxis-Fachpersonen, SVA) contributed significantly to the recruitment process of CSMAs. The patient representative and “Diabetesschweiz” helped to develop the questionnaire. INFRAS, as an independent research institute, supported us mainly in the analysis of the qualitative data and the preparations for the dissemination of the study results.
The study took place in primary care settings in the Swiss-German part of Switzerland.
The Ethics Committee of the Canton of Bern issued a permit (Req-2020-01255) for this study. No financial compensation or incentives were given to participants. Study participation was voluntary and in compliance with the Swiss Data Protection Act. Participants were informed about the conditions in advance and gave their written consent to participate before participating in the study.
CSMAs were recruited using an online survey (SurveyMonkey, Palo Alto, CA, USA) sent to all CSMAs in Switzerland who were members of the Swiss Association of Medical Practice Professionals (Schweizerischer Verband Medizinischer Praxis-Fachpersonen, SVA) in the spring of 2020 (n = 158). Eighteen CSMAs were identified, of whom 3 had to be excluded because of special certifications for diabetes care, e.g. EQUAM (EQUAM Stiftung, quality seal), and 3 others withdrew from the study due to a high workload. Finally, 12 CSMAs working in different practices were included (figure 1). For each practice with CSMA(s), we searched for a similar practice without CSMAs. In the best cases, practices were from the same region or belonged to the same network (in German “Ärztenetzwerk”). The reason practices were recruited from the same network was that networks often provide their practices with the same guidelines on treating patients with type 2 diabetes, and practices in the same network usually have similar work processes. Of around 180 invited GPs, 13 agreed to participate. However, 3 GPs did not recruit any patients for the study due to a lack of eligible patients or a work overload, since the recruitment phase coincided with the second wave of the COVID-19 pandemic in Switzerland. Therefore, 10 GPs remained who actively participated. Practices were excluded if they had other structured diabetes treatment plans, e.g., EQUAM for diabetes.
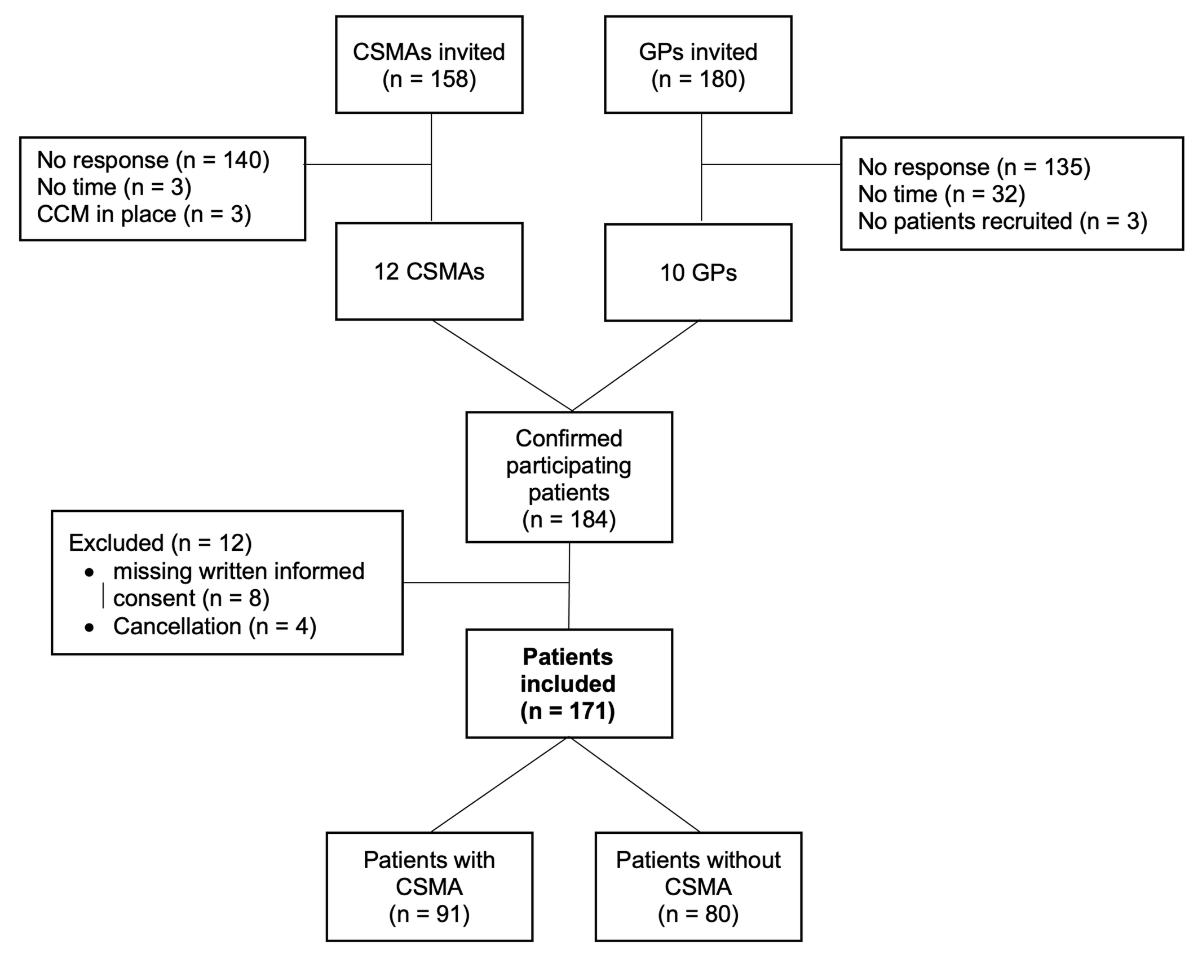
Figure 1 Study flow chart.
Patients had to have been diagnosed with type 2 diabetes mellitus for at least 2 years, be over 18 years of age, and have been under the care of their GP or CSMA for at least one year. Only patients able to give their written informed consent were included. The participating CSMAs had to have had their diploma for at least one year.
Each participating CSMA and GP was asked to recruit 8–10 patients. To avoid selection bias as much as possible, we asked the participating CSMAs and GPs to select patients consecutively. Any patient with type 2 diabetes who came to their consultation and met the inclusion criteria was to be asked whether they would like to participate.
For practical reasons, we distributed the patient questionnaires and informed consent forms to the CSMAs and GPs directly and invited them to inform potential patients about the study and seek informed consent.
As a primary outcome, we chose satisfaction with the ongoing diabetes therapy and occurrence of hypo- and hyperglycemia as measured by the Diabetes Treatment Satisfaction Questionnaire (DTSQ) [29, 30], a patient-reported outcome measure (PROM). This questionnaire encompasses six groups of questions. Each group is based on a 7-point Likert scale from 0 to 6 (0 means very dissatisfied and 6 very satisfied). Two other questions are analyzed separately and involve perceived frequencies of hypo- and hyperglycemia (6 means most of the time and 0 never). A total score (0–36) is calculated from the question groups. The higher the score, the higher the patient satisfaction. The DTSQ has been validated in German for Switzerland [31] and was provided to us on request [32].
As secondary outcomes, data were collected for the SGED score and Treatment Burden Questionnaire (TBQ) score. The SGED score represents the “criteria for good disease management of diabetes in primary care” defined in 2017 by the Swiss Society of Endocrinology and Diabetes (SGED/SSED) [25]. It comprises eight criteria for rating the most important aspects of diabetes treatment: number of GP consultations (max.10 points), lifestyle measures (max. 10 points), HbA1c (max. 25 points), average blood pressure (max. 15 points), LDL cholesterol in patients under 75 years of age (max. 10 points), nephropathy screening (max. 10 points), eye examination (max. 10 points) and foot examination (max. 10 points). The total score (max. 100 points) was calculated, and >70 points were used as a threshold of good quality, as specified by the panel of the SGED.
Data collection for the SGED score was done by the GPs or practice staff based on clinical information recorded in their patient records. We used the official SGED table as a template for the paper-based questionnaire on the SGED criteria [25]. All practices entered the required laboratory parameters, vital signs, and lifestyle information. From the SGED, we received an Excel file to which we transferred the data to calculate the score at the practice level. The table was adapted with the help of a computer scientist so that we could also compare the scores at the patient level. The score was calculated by the researchers. In the questions about the patients’ lifestyle, the answer options Yes and No were expanded with an additional answer option (No but offered). If the answer option “No but offered” was ticked, we evaluated this answer option as a Yes.
The Treatment Burden Questionnaire (TBQ) measures the perceived treatment burden of patients with chronic conditions [33]. It consists of 15 questions rated on a Likert scale from 0 (no problem) to 10 (big problem). It was developed in France using literature research and qualitative semi-structured patient interviews. Items assessed include the burden associated with medication use, self-monitoring, laboratory tests, physician visits, and organizational and administrative tasks. The burden of following advice on diet and physical activity and the social impact of the disease is also recorded. The total score is between 0 and 150, with a score above 59 points indicating that the patient is overwhelmed [34]. Since the TBQ had not been validated in German, we approached Inter-Translations SA [35] to translate and back translate. We evaluated the TBQ with 10 patients. The validation process can be obtained from the providers [33].
Finally, patients and health professionals (CSMAs and GPs) were asked an open-ended question about whether they thought anything needed to be done to improve diabetes care.
We assessed the patient characteristics of age, gender, years since diagnosis, and occupation with the paper-based questionnaire.
For sample size calculations, we used the results from a study with a comparable population, in which almost 6,000 patients with type 2 diabetes from several countries were included [14]. The participants had an average self-reported Diabetes Treatment Satisfaction Questionnaire (DTSQ) of 29.8 (standard deviation [SD] 6.2) in that study. We assumed that a difference of 3 points in the DTSQ is relevant because this corresponds to half the SD in the study mentioned [36]. Further, this is in line with a pilot trial of diabetes self-management, which also found a difference of 3 between the study groups [37]. We used the following assumption to power the study for the primary outcome: 1) difference in the DTSQ between the study groups: 3, 2) common standard deviation: 6.15, 3) alpha: 0.05, and 4) power: 80%. Using a t-test, we calculated a required mean sample size of 134 (67 per group). To allow for 10–20% missing data and dropouts, we fixed the final sample size at 160 (80 per group). From our experience interviewing GPs and patients, we expected around 15% missing variables. This corresponded to 10 practices per group with 8 patients each.
We used the open-source software EpiData Manager and EntryClient v4.6.0.6 (EPI Data Association, 1999, Denmark) to transfer and code data from paper questionnaires into electronic form. The data and analytical code are not available for open access, in accordance with our ethics approval. However, the anonymized dataset used and analyzed during the current study and the analytical code are available from the corresponding author upon reasonable request. STATA® Version 15 (StataCorp LLC, College Station, Texas, US) merged data from patients, CSMAs, and GPs using unique identifiers. Once linked, all data were anonymized.
Quantitative data: Data analysis was performed using STATA® Version 15 (StataCorp LLC, College Station, Texas, USA). Characteristics of patients, CSMAs, and GPs were analyzed with descriptive statistics. Diabetes Treatment Satisfaction Questionnaire (DTSQ), SGED, and Treatment Burden Questionnaire (TBQ) scores were compared between the two groups using t-tests. No evidence was found for intra-cluster correlation.
We performed a text analysis. Free-text responses for suggested improvements in diabetes therapy were grouped into predefined categories. This categorization was done independently by two researchers. In discussion, eventual disagreement was discussed, and a consensus was reached. Responses were listed by frequency of occurrence and summarized textually under the summary of open-ended questions category. We handled missing data by comparing characteristics of responders and non-responders.
A total of 12 CSMAs and 10 GPs agreed to participate in the study (figure 1). The locations of the participating CSMAs and GPs are shown in figure 2. Table 1 describes the essential characteristics of the health professionals; 12 CSMAs with 11 associated GPs and 8 GPs without CSMA provided information. CSMAs were on average 38 years old (mean 37.7, SD 9.7), GPs with CSMAs in their practice were on average 54 years old (mean 54.3, SD 7.7), and GPs without CSMAs were on average 43 years old (mean 43.5, SD 8.2). Regarding gender distribution and workload, GPs with and without CSMAs in their practice were comparable. The CSMAs all worked part-time and were female.

Figure 2 Map Switzerland with participating practices. Red: practices with CSMA; blue: practices without CSMA.
Table 1Characteristics of CSMAs and GPs.
| Characteristics | CSMAs, n = 12 | General practitioners with CSMAs, n = 11 | General practitioners without CSMAs, n = 8 | |
| Age, years (SD) | 37.7 (9.7) | 54.3 (7.7) | 43.5 (8.2) | |
| Female, n (%) | 11 (92%) | 3 (27%) | 3 (38%) | |
| Workload, % (SD) | 43 (32) | 80 (15) | 73 (23) | |
| Experience, years (SD) | 4.4 (1.3) | 18.6 (8.2) | 7.8 (6.5) | |
| Verification of diabetes therapy, n (%) | HbA1c measurements | 10 (83%) | 8 (73%) | 7 (88%) |
| SGED criteria | 7 (58%) | 5 (45%) | 3 (38%) | |
| Patient surveys | 1 (8%) | 4 (36%) | 3 (38%) | |
| Others | 2 (17%) | 1 (9%) | – | |
CSMAs = clinical specialized medical assistants; SD = standard deviation
Table 2 compares the characteristics of 171 participating patients in both models. Regarding age (group with CSMA: mean 69.2, SD 9.0 vs. group without CSMA: mean 68.7, SD 10.2) and gender (40% female patients in the group with CSMA vs. 26% in the group without CSMA), the groups did not differ significantly. Regarding lab and vital indicators, patients did not differ significantly between both groups.
Table 2Characteristics of patients.
| Characteristics | Patients from the CSMA model, n = 91 | Patients from the GP model, n = 80 | P-value* |
| Age, years (SD)a | 68.7 (10.2) | 69.2 (9.0) | 0.75 |
| Female, n (%)b | 40 (44) | 26 (33) | 0.13 |
| Employed, n (%)c | 28 (31) | 17 (22) | 0.22 |
| Years since diagnosis of diabetes, mean (SD)d | 11.7 (7.9) | 13.0 (9.3) | 0.34 |
| BMI (kg/m2), mean (SD)e | 29.7 (5.2) | 28.6 (5.6) | 0.18 |
| Current smoker, n (%) | 12 (13.8) | 9 (11.8) | 0.71 |
| HbA1c (%), mean (SD)f | 7.0 (0.7) | 7.1 (0.8) | 0.78 |
| Systolic blood pressure (mmHg), mean (SD)g | 136 (13) | 138 (13) | 0.30 |
| Diastolic blood pressure (mmHg), mean (SD) | 80 (8) | 81 (7) | 0.66 |
| LDL (mmol/L), mean (SD)h | 2.4 (0.8) | 2.4 (0.9) | 0.81 |
SD = standard deviation.
* For comparison between participants from both groups, we performed a t-test.
Patient variables: a 10 missing, 5.9%; b 0 missing; c 4 missing, 2.3%; d 7 missing, 4.1%; e 8 missing, 4.7%; f 6 missing, 2.9%; g 5 missing, 2.9%; h 14 missing, 0.2%.
Table 3 shows a high treatment satisfaction scale score in both groups, with no statistically significant difference (p = 0.70) in patients with CSMA (32.1 points, SD 3.6) and without CSMA (32.4 points, SD 3.8). Participants in both groups had few high blood glucose episodes (group with CSMA: mean 1.6, SD 1.6 vs. group without CSMA: mean 1.6, SD 1.7, p = 0.97) and very few episodes of hypoglycemia (group with CSMA: mean 0.7, SD 1.2 vs. group without CSMA: mean 0.7, SD 1.3, p = 0.99). In addition, patients with CSMA (mean 80.2, SD 8.5) and patients without CSMA (mean 75.9, SD 4.8, p = 0.18) achieved an SGED score in the target range between 70 and 100 points. Scores of 70 points or higher were achieved by 83% from CSMA and 90% from conventional practices, with no significant difference. Patients with CSMA (mean 19.2, SD 15.6) and patients without CSMA (18.2 SD, 21.4, p = 0.89) had similarly low Treatment Burden Questionnaire (TBQ) values.
Table 3Outcomes in practices with and without CSMAs on Diabetes Treatment Satisfaction Questionnaire (DTSQ), SGED score, and Treatment Burden Questionnaire (TBQ).
| Practices and patients from the CSMA model, (patients: n = 91, practices: n = 12) | Practices and patients from the GP model, (patients: n = 80, practices: n = 10) | P-value | |
| Variables measured at patient level | |||
| Treatment Satisfaction Scale Totala, mean (SD) | 32.1 (3.6) | 32.4 (3.8) | 0.70c |
| Perceived frequency of hyperglycemiab, mean (SD) | 1.6 (1.6) | 1.6 (1.7) | 0.97c |
| Perceived frequency of hypoglycemiab, mean (SD) | 0.7 (1.2) | 0.7 (1.3) | 0.99c |
| Treatment Burden Total Scoree, mean (SD) | 19.2 (15.6) | 18.8 (21.4) | 0.89 |
| Variables measured at practice level | |||
| SGED Scored, mean (SD) | 80.2 (8.5) | 75.9 (4.8) | 0.18 |
| SGED Score, 70 points and higher, n (%) | 10 (83%) | 9 (90%) | 0.65 |
CSMAs = clinical specialized medical assistants; SD = standard deviation.
a Satisfaction scores from 0 to 36 points, with a higher score meaning greater satisfaction.
b Frequencies were reported from 0 (never) to 6 (most of the time).
c Hypothesis testing using unadjusted regression models.
d Criteria for “good” disease management from the Swiss Society of Endocrinology and Diabetes calculated by care model from 0 to 100 points (higher = better quality). Experts reached a consensus that 70 is a minimal standard to achieve for “good clinical practice”.
e Total score is the sum of all 15 items, each scoring 0–10, thus in total 0 (no burden at all) to 150 (maximal burden).
We asked clinical specialized medical assistants, how often and for how long they saw their patients with type 2 diabetes, how often they were seen in total in the practice (GP and CSMA), and whether a CSMA consultation possibly replaced a GP consultation. We learned that CSMAs saw patients every 3–6 months or 3–4 times a year for 30 minutes. In nearly 3 out of 4 cases, task shifting from primary care physicians to CSMAs can be suggested: 78% of CSMAs reported that patients with type 2 diabetes under their care had overall equal or even fewer consultations than patients in a practice without CSMA (figure 3).
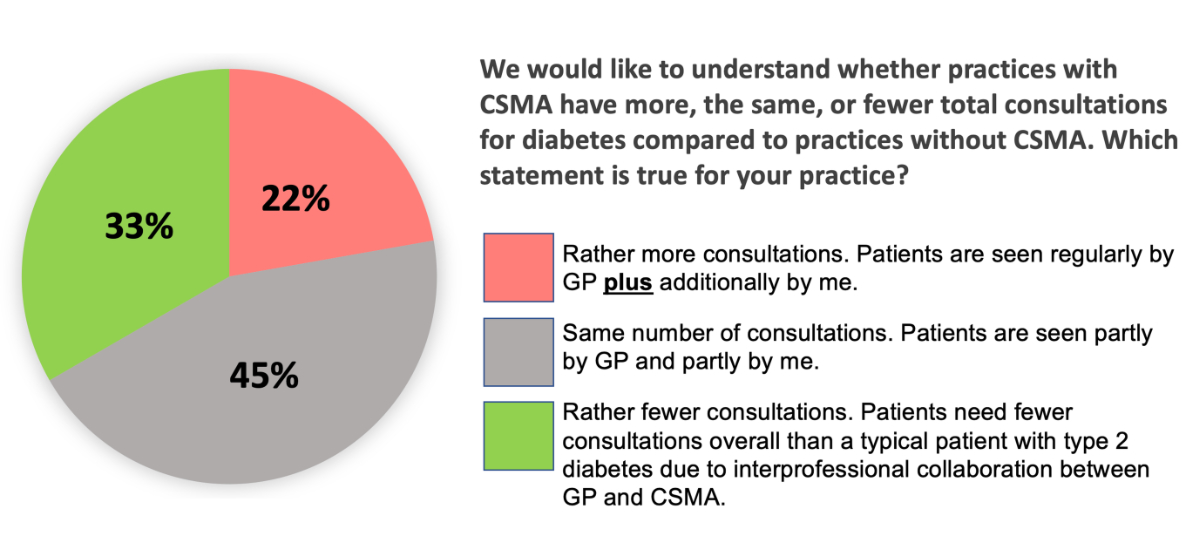
Figure 3 Consultations.
Both CSMAs and GPs had suggestions for improvement in outpatient diabetes care. The responses are listed by frequency of occurrence (in parentheses).
All 12 CSMAs and 11 of the associated GPs provided information on their perceived benefits of interprofessional collaboration (e.g., more time for motivational interviewing and patient education, reduced workload for GPs). 8 GPs without CSMAs provided information on their expectations of CSMA models. 88% of health professionals provided positive feedback. 11 health professionals mentioned the following categories as additional benefits:
Accordingly, a common comment was that the Tarmed billing catalog does not have a billing line item for CSMA services. There have also been calls for CSMA duties to be well-defined; otherwise, it seems to be difficult for CSMAs to protect their daily scope of work. Some practices attempt to resolve this conflict by using written, usually internal, instructions for CSMA activities. CSMAs saw the benefits of their work primarily in having a different approach to patients and thus a special relationship of trust. They indicated that patients were more likely to open up to them and talk about their needs and “weaknesses”. This creates a new opportunity to improve patient satisfaction and compliance and thus the quality of therapy. Regarding other requests from CSMAs for future training, more intensive training in diabetic pharmacotherapy was mentioned. Few patients commented on suggestions to improve. However, two patients commented that they would like fewer consultations and more information about diabetes in general and diabetes in the elderly.
In this one-time survey in the German-speaking part of Switzerland, we assessed satisfaction with ongoing diabetes care in patients with type 2 diabetes and the quality of outpatient diabetes care in over 170 patients in more than 20 primary care practices with and without CSMAs. This demonstrated that participating GP practices in the German-speaking part of Switzerland were already achieving high quality of care with a low treatment burden for patients with diabetes and that practices with a CSMA involved in diabetes care were not inferior to those without a CSMA. It appears that even when tasks were distributed from GP to CSMA, a high level of treatment was maintained, so we suspect that GPs can transfer tasks to CSMAs. Patients, CSMAs, and GPs reported high satisfaction with interprofessional collaboration but also cited several areas for improvement. From the point of view of GPs and CSMAs, interprofessional partnerships could be strengthened by having adequate billing positions for the services of CSMAs.
Our study has the typical limitations of a cross-sectional study. For example, the Diabetes Treatment Satisfaction Questionnaire (DTSQ) and Treatment Burden Questionnaire (TBQ) as PROMs (Patient-Reported Outcome Measures) might be subject to recall bias. However, the SGED score as an objective parameter is not and returned similar results. We chose consecutive sampling to limit selection bias. To confirm that the consecutive sampling strategy was followed, a sample of 30% of participants was reviewed by the research team, and no violations were found. However, we cannot completely rule out a residual positive selection. Notably, patients in both groups had comparable baseline characteristics. Further, with a mean HbA1c value of 7% and an SGED score above 70 points, all patients’ values were in the target range, which suggests the selection of patients with already good diabetes-related care and indicators. This may indicate that predominantly practices participated that already performed better than practices that did not find time to participate or were not from the same network [39]. However, the observed diabetes-related indicators, such as HbA1c, are comparable to the values found in other studies. Consequently, while we cannot rule out differential recruitment of patients, the level of diabetes care seems to be relatively high in Swiss primary care practices [39]. Additionally, in both groups, the characteristics of patients and health care professionals (CSMAs, GPs) were similar. We consider this a strength that outweighs the study's weaknesses and tends to argue against positive selection. The study’s greatest strength is the lived interprofessionalism with which the project group worked together. Patient representatives were actively involved in designing the questionnaires so that we could focus on their needs. For example, the topic of the “financial burden” of diabetes patients was brought in. This was explored in more detail with the help of the Treatment Burden Questionnaire (TBQ). As another strength, we exceeded the number of participants required by the calculated sample size.
The demand for interprofessional collaboration in health care is steadily increasing in Switzerland due to the shortage of GPs [40, 41]. The Swiss Academy of Medical Sciences (SAMW) has been one of Switzerland’s most prominent research funding institutions since 1943 and is supported by the confederation with annual subsidies. From 2016 to 2021, the SAMW focused firmly on interprofessional collaboration in health care [3]. Since then, principles, definitions, and recommendations have been published, and 69 research projects focusing on interprofessional collaboration have been funded and rewarded [42]. The federal government has also established funding programs to promote interprofessional collaboration [43]. This reflects the enormous importance of the topic.
In a cluster-randomized Swiss study from 2010 [22], practices with a medical practice assistant (MPA) trained in the diabetes module for CSMAs were compared to conventional practice models (GP plus MPA without special training). GPs of conventional practice models also received special training. Patient characteristics were similar to those of our participants, namely age (mean 67.1 years, SD 10.6), duration of diabetes (mean 9.9 years, SD 7.6), BMI (mean 30.6 kg/m2, SD 5.6), and gender (57.4% men). After the intervention, significant improvements in cardiovascular risk factors (blood pressure and LDL cholesterol) and patient satisfaction as measured by the Patient Assessment of Chronic Illness Care (PACIC) were observed 1 year later. At the same time, HbA1c values decreased in both groups. This effect on blood pressure and physical activation was again demonstrated in a study by the health insurance company Sanacare [21]. It might be possible that trained MPAs could devote more time to patient education (diet, exercise, medication adherence). This effect of CCM on cardiovascular risk factors, more specifically on blood pressure and LDL cholesterol, was also shown in a US intervention study with a similar population [44] and was described in a 2018 literature review [7]. We could not demonstrate this effect in our comparison, possibly because the participating GPs were already committed and high-performing. This is shown by the fact that they recruited and motivated patients to participate in the survey despite the pandemic with all its difficulties and without compensation. The time required for the survey was not insignificant at approximately 45 minutes per patient.
We assume a ceiling effect on SGED criteria under CCM in the long term. This assumption is supported by another study that examined the effect of newly implemented disease management programs for people with diabetes (DMP-DM). A Swiss health insurer (SWICA) conducted a prospective controlled observational study of practices with DMP-DM from 2017 to 2019 [23]. DMP-DM resulted in significant improvement in guideline compliance as measured by 4 Simple Performance Measures (4SPM). Patients who received care at a DMP-DM centre performed significantly better compared with the control group in terms of both the mean 4SPM level (2018 vs. 2017: difference-in-difference analysis = 0.17 [0.025,0.31]; 2019 vs. 2017: difference-in-difference analysis = 0.18 [0.033,0.33]) and the highest 4SPM level (2018 vs. 2017: +6%-points [2%-points,10%-points]; 2019 vs. 2017: +8%-points [4%-points,12%-points]). The quality of treatment in general, measured by SGED, fluctuated but remained unchanged over the 3 years. This underscores our findings from the SGED analysis, namely that high-quality diabetes care in practices with CSMA was not inferior to practices without CSMA. The ceiling effect assumed here is undoubtedly also due to the high medical standard in Switzerland.
Further, we assume that overall health care costs will decline under CCM in the long term. Our study supports this conjecture by showing that CSMAs are likely to be able to perform GP tasks but at significantly lower wages. In the above-mentioned study, the authors observed a cost reduction trend of 10% per patient, but the results were not statistically significant. The authors assumed that the study period was too short to detect a significant effect. In a similar Swiss population [45], a significant cost reduction of 10% under CCM was noted.
The study is generalizable with caveats. We had a group of high-performing GPs and patients with reasonable diabetes control in our sample, so how transferable our results are outside this group remains unclear.
Politically, the study results are currently relevant for Swiss primary care. For several years, Swiss physicians and other health care professionals have been arguing about the renewal of the outpatient billing catalog (Tarmed [46]). CSMAs are trying to maintain their position in the new catalog (Tardoc) to bill their services appropriately independently from the primary care physician and the medical practice assistant (MPA). We cannot provide a cost analysis due to the lack of a billing position for CSMAs. To date, no evidence exists of the cost-benefit of using CSMAs and CCM in the treatment and care of the chronically ill. Since we did not collect data on this, we do not know which model was more cost-effective in our study. However, it is assumed that the most cost-effective model for diabetes is the one that provides good quality of care because poor-quality care costs more in the long term. Transparent billing arrangements would make further cost comparison studies much more accessible.
All parties involved in the care of chronically ill people can benefit from closer cooperation between various professional groups. For GPs, for example, a way will be paved to ease the burden of daily operations. This is essential for both consistent quality of care and reducing the workload of GPs, who are particularly at risk for burnout [47, 48]. Medical practice professionals also benefit primarily through professional exchange and learning effects [7] and the feeling of bringing real value to patients [49]. It also increases the attractiveness of this new profession by giving SMAs more responsibilities. Promotion and advancement opportunities allow for salary enhancement, which promotes the next generations. Health insurance companies can look forward to more sustainable cost efficiency. Last but not least, patients themselves benefit: they receive more information about the disease. This leads to a better understanding of the disease, supports patients in their self-management, and ultimately leads to less negative impact of the disease on quality of life and fewer complications and hospitalizations [27, 50, 51, 52].
Due to data protection regulations, sharing the original study data is not possible. For further projects, aggregated data can be shared on request if the research group members consent.
We would like to thank all CSMAs, GPs, and patients who participated in this study. Furthermore, we would like to thank our partner organizations for funding and support: Swiss Diabetes Foundation SDS, BEKAG, KPT, Visana, FMH, and Diabetesschweiz, as well as our project partners at the Swiss Association of Medical Practice Professionals (Schweizerischer Verband Medizinischer Praxis-Fachpersonen, SVA) and INFRAS for their support in the conduct of this study and its dissemination. For proofreading the manuscript, we thank Professor Clare Bradley, the developer of the DTSQ.
The initiative for a study on the usability of CSMAs in the care of the chronically ill came from the Aerztegesellschaft des Kantons Bern (Medical Society of the Canton of Bern, BEKAG). Together with the health insurance companies KPT and Visana, they approached the Berner Institut für Hausarztmedizin (Institute of Primary Health Care Bern) and INFRAS (research and consulting company in Zürich) to launch a research project. Finally, the study was funded by various donors: Schweizerische Diabetes Stiftung (Swiss Diabetes Foundation, SDS), BEKAG, Swiss Medical Association (FMH), and the health insurance companies KPT and VISANA. The academic lead of the study was with the team at the Institute of Primary Health Care (BIHAM) at the University of Bern.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Wagner EH . Academia, chronic care, and the future of primary care. J Gen Intern Med. 2010 Sep;25(S4 Suppl 4):S636–8. https://doi.org/10.1007/s11606-010-1442-6
2. World Health Organization (WHO) . Framework for Action on Inter-professional Education and Collaborative Practice. Genf. 2010.
3. Schweiz. Akademie der Med. Wissenschaften. Interprofessionelle Zusammenarbeit in der Gesundheitsversorgung: erfolgskritische Dimensionen und Fördermassnahmen. Differenzierung, Praxis und Implementierung. Swiss Academies Communications. 2020, 15 (2).
4. de Bont A , van Exel J , Coretti S , Ökem ZG , Janssen M , Hope KL , et al.; MUNROS Team . Reconfiguring health workforce: a case-based comparative study explaining the increasingly diverse professional roles in Europe. BMC Health Serv Res. 2016 Nov;16(1):637. https://doi.org/10.1186/s12913-016-1898-0
5. Busca E , Savatteri A , Calafato TL , Mazzoleni B , Barisone M , Dal Molin A . Barriers and facilitators to the implementation of nurse’s role in primary care settings: an integrative review. BMC Nurs. 2021 Sep;20(1):171. https://doi.org/10.1186/s12912-021-00696-y
6. Chmiel C , Giewer I , Frei A , Rosemann T . Four-year long-term follow-up of diabetes patients after implementation of the Chronic Care Model in primary care: a cross-sectional study. Swiss Med Wkly. 2017 Oct;147(4344):w14522. https://doi.org/10.4414/smw.2017.14522
7. Yeoh EK , Wong MC , Wong EL , Yam C , Poon CM , Chung RY , et al. Benefits and limitations of implementing Chronic Care Model (CCM) in primary care programs: A systematic review. Int J Cardiol. 2018 May;258:279–88. https://doi.org/10.1016/j.ijcard.2017.11.057
8. Frei A , Senn O , Huber F , Vecellio M , Steurer J , Woitzek K , et al. Congruency of diabetes care with the Chronic Care Model in different Swiss health care organisations from the patients’ perspective: a cross sectional study. Swiss Med Wkly. 2014 Sep;144:w13992. https://doi.org/10.4414/smw.2014.13992
9. Peytremann-Bridevaux I , Bordet J , Burnand B . Diabetes care in Switzerland: good, but perfectible: a population-based cross-sectional survey. BMC Health Serv Res. 2013 Jun;13(1):232. https://doi.org/10.1186/1472-6963-13-232
10. Ammann L , Fäh D . Potential für Früherkennung von Diabetes mellitus Typ 2. Schweiz Arzteztg. 2019;100(8):264–6. https://doi.org/10.4414/saez.2019.06895
11. Einarson TR , Acs A , Ludwig C , Panton UH . Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol. 2018 Jun;17(1):83. https://doi.org/10.1186/s12933-018-0728-6
12. Huber CA , Wieser S . Die Schweiz zahlt hohen Preis für nichtübertragbare Krankheiten. Schweiz Arzteztg. 2018;99(33):1054–6. https://doi.org/10.4414/saez.2018.06916
13. Polonsky WH , Fisher L , Hessler D . The impact of non-severe hypoglycemia on quality of life in patients with type 2 diabetes. J Diabetes Complications. 2018 Apr;32(4):373–8. https://doi.org/10.1016/j.jdiacomp.2018.01.014
14. Bradley C , Eschwège E , de Pablos-Velasco P , Parhofer KG , Simon D , Vandenberghe H , et al. Predictors of Quality of Life and Other Patient-Reported Outcomes in the PANORAMA Multinational Study of People With Type 2 Diabetes. Diabetes Care. 2018 Feb;41(2):267–76. https://doi.org/10.2337/dc16-2655
15. Kaewput W , Thongprayoon C , Varothai N , Sirirungreung A , Rangsin R , Bathini T , et al. Prevalence and associated factors of hospitalization for dysglycemia among elderly type 2 diabetes patients: A nationwide study. World J Diabetes. 2019 Mar;10(3):212–23. https://doi.org/10.4239/wjd.v10.i3.212
16. Bundesamt für Statistik. Statistischer Atlas der Schweiz - Ärztedichte im ambulanten Sektor. [Online] 2020. [Cited: 12 14, 2021.] https://www.atlas.bfs.admin.ch/maps/13/de/16437_5141_4422_7264/25649.html
17. Zeller A . Resultate der 4. Workforce Studie. Primary and Hospital Care – Allgemeine. Inn Med. 2020;20(11):325–8.
18. Diallo, B. Wer strebt am Ende des Medizinstudiums eine Hausärztekarriere an? Umfrage unter Schweizer Studierenden. Praxis (Bern 1994). 2019 Sep., 108 (12)., pp. 779-786. DOI: https://doi.org/10.1024/1661-8157/a003300.
19. Wagner EH . Chronic disease management: what will it take to improve care for chronic illness? Eff Clin Pract. 1998 Aug-Sep;1(1):2–4.
20. odamed, OdA Berufsbildung Medizinische Praxisassistentin. odamed. http://www.odamed.ch/home.html. [Online] [Cited: 12 14, 2021.]
21. Sahli R . Chronic Care Management in der Hausarztpraxis. . Primary and Hospital Care Allge Inn Med. 2017;17(3):46–50.
22. Frei, A. The Chronic CARe for diAbeTes study (CARAT): a cluster randomized controlled trial. Cardiovasc Diabetol. 2010 Jun, 15; 9:23. DOI: https://doi.org/10.1186/1475-2840-9-23.
23. Carlander, M. Wissenschaftliche Begleitevaluation: SWICA Disease Management Programm Diabetes Mellitus. Winterthur: ZHAW Zürcher Hochschule für Angewandte Wissenschaften. 2010 Mar, zhaw-21956. DOI: https://doi.org/10.21256/zhaw-21956.
24. Steurer-Stey, C. Evidenz und Kosteneffizienz des Chronic Care Models. Institut für Hausarztmedizin, Universität Zürich .
25. QualiCCare , SGED. Anwendungshilfe zu den Kriterien für „gutes“ Disease Management Diabetes in der Grundversorgung. [Online] 2017 Nov. [Cited: 12 14, 2021.]
26. Chmiel C , Birnbaum B , Gensichen J , Rosemann T , Frei A . Das Diabetes-Ampelschema - Entwicklung eines Instruments für das hausärztliche Case Management bei Patienten mit Diabetes mellitus. Praxis (Bern). 2011 Nov;100(24):1457–73. https://doi.org/10.1024/1661-8157/a000751
27. Lorig KR , Sobel DS , Stewart AL , Brown BW Jr , Bandura A , Ritter P , et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999 Jan;37(1):5–14. https://doi.org/10.3399/bjgpopen19X101671 https://doi.org/10.1097/00005650-199901000-00003
28. SVA . Schweiz. Verband Med. Praxis-Fachpersonen. SVA. https://www.sva.ch. [Online] [Cited: 11 22, 2021.]
29. Bradley C . The Diabetes Treatment Satisfaction Questionnaire: DTSQ. Handbook of Psychology and Diabetes: a guide to psychological measurement in diabetes research and practice. Chur, Switzerland: Harwood Academic Publishers. 1994, pp. 111-132. URL: https://www.healthpsychologyresearch.com (Status as of 22.11.21).
30. Bradley C , Lewis KS . Measures of psychological well-being and treatment satisfaction developed from the responses of people with tablet-treated diabetes. Diabet Med. 1990 Jun;7(5):445–51. https://doi.org/10.1111/j.1464-5491.1990.tb01421.x
31. Kubiak, T. Erfassung der diabetesbezogenen Therapiezufriedenheit mit der deutschsprachigen Fassung des Diabetes Treatment Satisfaction Questionnaire (DTSQ) – psychometrische Eigenschaften und Validierung. Diabetes und Stoffwechsel. 12 (1), 56.
32. Health Psychology Research. Health Psychology Research. [Online] https://www.healthpsychologyresearch.com
33. Tran VT , et al. Development and description of measurement properties of an instrument to assess treatment burden among patients with multiple chronic conditions. BMC Med. 2012, 10:68. URL: https://eprovide.mapi-trust.org/, pp. DOI: https://doi.org/10.1186/1741-7015-10-68
34. Tran VT , Montori VM , Ravaud P . Is My Patient Overwhelmed?: Determining Thresholds for Acceptable Burden of Treatment Using Data From the ComPaRe e-Cohort. Mayo Clin Proc. 2020 Mar;95(3):504–12. https://doi.org/10.1016/j.mayocp.2019.09.004
35. ITSA | Inter-Translations SA, Bern, Switzerland. www.itsa.ch. [Online] [Cited: 12 01, 2021.]
36. Norman GR , Sloan JA , Wyrwich KW . Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003 May;41(5):582–92. https://doi.org/10.1097/01.MLR.0000062554.74615.4C
37. Korytkowski MT , Koerbel GL , Kotagal L , Donihi A , DiNardo MM . Pilot trial of diabetes self-management education in the hospital setting. Prim Care Diabetes. 2014 Oct;8(3):187–94. https://doi.org/10.1016/j.pcd.2013.11.008
38. Riesen WF . ESC/EAS-Dyslipidämie-Guidelines. Swiss Med Forum. 2020 Feb, 20 (9-10): 140-148, pp. 140-148.
39. Meier R , Valeri F , Senn O , Rosemann T , Chmiel C . Quality performance and associated factors in Swiss diabetes care - A cross-sectional study. PLoS One. 2020 May;15(5):e0232686. https://doi.org/10.1371/journal.pone.0232686
40. Competence Network Health Workforce . Competence Network Health Workforce. [Online] https://www.cnhw.ch
41. Plattform Interprofessionalität . Plattform Interprofessionalität. https://www.interprofessionalitaet.ch. [Online] [Cited: 12 13, 2021.]
42. SAMW . SAMW Award «Interprofessionalität». https://www.samw.ch/de/Projekte/Uebersicht-der-Projekte/Interprofessionalitaet/Award.html. [Online] [Cited: 12 13, 2021.]
43. Interprofessionalität BA . im Rahmen des Förderprogramms «Interprofessionalität im Gesundheitswesen» 2017-2020. https://www.bag.admin.ch/bag/de/home/das-bag/publikationen/forschungsberichte/forschungsberichte-interprofessionalitaet-im-gesundheits. [Online] [Cited: 12 14, 2021.]
44. Vargas RB , Mangione CM , Asch S , Keesey J , Rosen M , Schonlau M , et al. Can a chronic care model collaborative reduce heart disease risk in patients with diabetes? J Gen Intern Med. 2007 Feb;22(2):215–22. https://doi.org/10.1007/s11606-006-0072-5
45. Huber CA , Reich O , Früh M , Rosemann T . Effects of Integrated Care on Disease-Related Hospitalisation and Healthcare Costs in Patients with Diabetes, Cardiovascular Diseases and Respiratory Illnesses: A Propensity-Matched Cohort Study in Switzerland. Int J Integr Care. 2016 Apr;16(1):11. https://doi.org/10.5334/ijic.2455
46. Arzttarif Schweiz - Tarif Médical Suisse . https://ats-tms.ch. [Online]
47. Hostettler S , et al. Grundlagenpapier der DDQ. Ärztliches Wohlbefinden beeinflusst die Behandlungsqualität. Schweiz Ärzteztg. 2012;93(18):18. https://doi.org/10.4414/saez.2012.00481
48. Lindemann, F. Assessing the mental wellbeing of next generation general practitioners: a cross-sectional survey. BJGP Open. 2019 Oct, 15; 3 (4). DOI: https://doi.org/10.3399/bjgpopen19X101671.
49. Hanak MA , McDevitt C , Dunham DP . Perceptions of Ambulatory Workflow Changes in an Academic Primary Care Setting. Health Care Manag (Frederick). 2017 Jul/Sep;36(3):261–6. https://doi.org/10.1097/HCM.0000000000000174
50. Chatterjee S , Davies MJ , Heller S , Speight J , Snoek FJ , Khunti K . Diabetes structured self-management education programmes: a narrative review and current innovations. Lancet Diabetes Endocrinol. 2018 Feb;6(2):130–42. https://doi.org/10.1016/S2213-8587(17)30239-5
51. Powers MA , Bardsley J , Cypress M , Duker P , Funnell MM , Hess Fischl A , et al. Diabetes Self-management Education and Support in Type 2 Diabetes: A Joint Position Statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. Diabetes Care. 2015 Jul;38(7):1372–82. https://doi.org/10.2337/dc15-0730
52. Lambrinou E , Hansen TB , Beulens JW . Lifestyle factors, self-management and patient empowerment in diabetes care. Eur J Prev Cardiol. 2019 Dec;26(2_suppl 2S):55–63. https://doi.org/10.1177/2047487319885455
53. STATA . https://www.stata.com. [Online] [Cited: 02 28, 2022.] https://www.stata.com/support/updates/stata15.html
54. EpiData . https://www.epidata.dk. [Online] [Cited: 02 28, 2022.] https://www.epidata.dk/download.php
55. Ravaud P . https://eprovide.mapi-trust.org. [Online] [Cited: 03 02, 2022.] https://eprovide.mapi-trust.org/instruments/burden-of-treatment-questionnaire