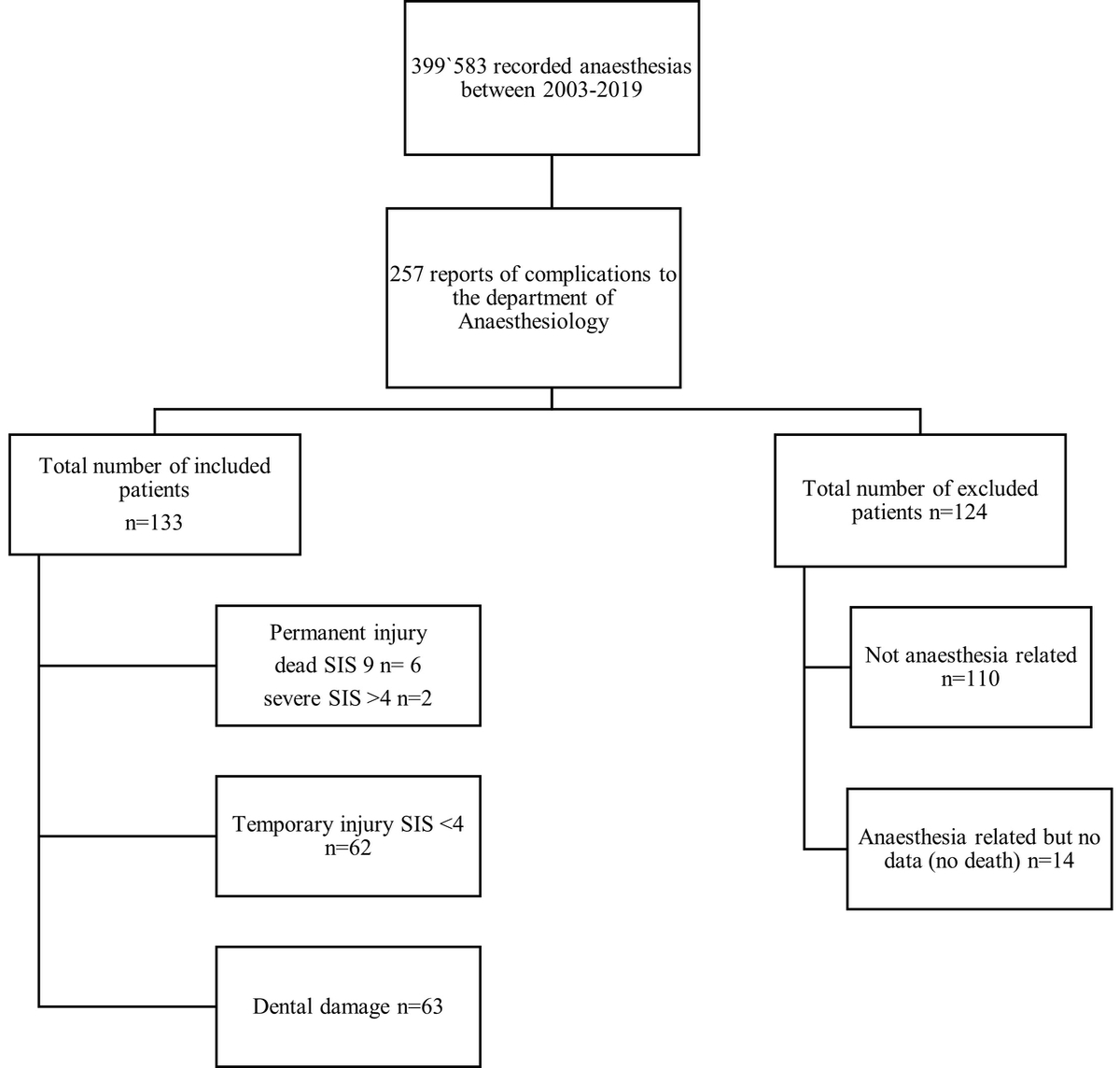
Figure 1 Included and excluded reports. SIS: severe injury scale
DOI: https://doi.org/10.4414/SMW.2022.w30169
Anaesthesiology has a wide area of expertise and intersects with many other medical specialities. An important aim for anaesthesiologists is to improve patient safety. Many studies have reported on anaesthesia-related complications [1–4]. One of the earliest studies that dealt with anaesthesia-related mortality and patient safety was a large multicentre study by Beecher and Todd in 1954. The mortality rate from 1948 to 1952 ranged between 53 and 69 per 100,000 anaesthetics. the main cause of severe complications were pharmacological and technical errors [5]. Over time, there has been technical improvement with the implementation of pulse oximetry and capnography as well as an increasing awareness of anaesthesia-related complications and death. In the 1980s, closed claims regarding anaesthesia-related complications were analysed to improve patient safety and to reduce the complication rate. Shortly afterwards, in 1987, the first anaesthetic teams were trained in crew resource management, as it became clear that in anaesthesia teamwork most of all and not individual skill was important for the success or failure of patient management [6]. In the 1990s, the critical incident reporting system (CIRS), which had been developed by Cooper et al. in 1978, was implemented nationwide in Switzerland [6, 7]. Due to this immense effort to improve anaesthesia safety, the anaesthesia-related mortality rate was drastically decreased [6]. In 2014, Schiff et al. found in a German retrospective study that the number of major complications was about 3 per 100,000 in elective surgery for healthy patients of American Society of Anesthesiologists (ASA) physical status class I and II [1].
Although there are many studies on this subject, there are none reporting on anaesthesia complications during a period of 17 years in one hospital. We compared our findings with those published in journals from other countries, corroborating the changes we observed at the Luzerner Kantonsspital (LUKS).
In our single centre retrospective cohort study, we analysed anaesthesia-related complications over 17 years at the Luzerner Kantonsspital (LUKS), Switzerland. Our main aims were to assess the temporal trends of anaesthesia-related complications, their distribution among hospital departments and their relation to emergency versus non-emergency surgery. We extracted the data from incident reports which had been reported to the department of anaesthesiology. The complications were classified into categories and the temporal changes, the distribution of these complications to hospital departments as well as the impact of emergency surgery were analysed. Our null hypothesis was that complications occur at the same rate in non-emergency anaesthesia as in emergency anaesthesia.
During this study period, a critical incident reporting system was successfully implemented in 2006, and the head of department of anaesthesiology changed in 2007.
We conducted a single centre retrospective cohort data analysis at the LUKS. The LUKS is a large tertiary hospital in central Switzerland, serving 700,000 citizens [8].
Ethical approval was given by the responsible ethics commission (Ethikkommission Nordwest- und Zentralschweiz, Hebelstrasse 53, Basel, Switzerland, President Prof. C Beglinger, Req-2019-00879) on 11 September 2019. The study is reported in accordance with the ‘Strengthening the Reporting of Observational Studies in Epidemiology’ (Strobe) Statement.
This study was based on data of anaesthesia protocols, when complications occurred, case notes from memory of those who were involved, file notes, as well as information on all anaesthetic procedures collected during the period from 1 January 2003 until 31 December 2019. All data were anonymised before inclusion.
Inclusion criteria for complication files were a completed anaesthesia chart, anaesthesia-related complications (e.g., dental damage, nerve injury, wrong medication administered, vocal cord injury, dislocation of jaw, lip injuries, "cannot ventilate, cannot intubate"), a completed standardised form for reported complications and notes of councils (e.g., neurologist, dentist). If one of the before mentioned criteria were missing, the complication file was excluded. Figure 1 summarises included and excluded reports.
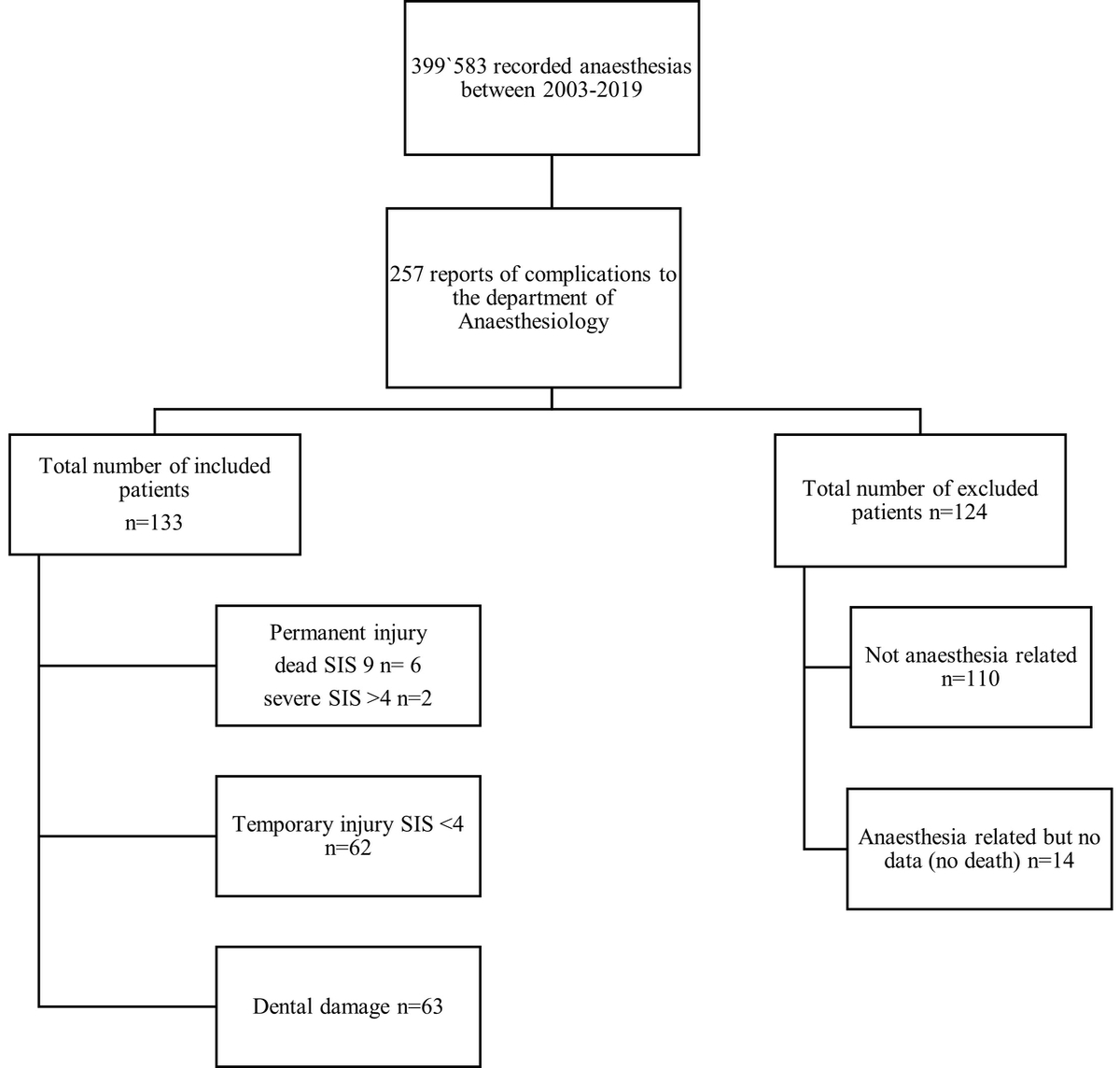
Figure 1 Included and excluded reports. SIS: severe injury scale
Out of the total of 257 cases that were reported to the department of anaesthesia at the LUKS, 110 were excluded as they were not anaesthesia related and 14 because of incomplete reporting forms.
The primary endpoint was occurrence of an anaesthesia-related complication and its relation to hospital departments. Secondary endpoints were temporal trends, emergency status of the intervention and mortality rate.
All anaesthetic procedures were documented by year, hospital department, emergency status of the intervention and the nature of the anaesthetic procedure.
Subsequently, the complication data was then organised by category, age, sex, ASA physical status, and the main surgical diagnosis that led to the intervention. The list of the 26 most common diagnoses is included in table 1. For a better overview, only surgical diagnoses that had been mentioned at least twice were included.
Table 1The most common surgical diagnosis of the patients who received anaesthesia and for whom an anaesthesia-related complication occurred between 2003 and 2019, n = 98. The rest of the patients are not included in this table as their diagnosis occurred only once.
| Surgical diagnosis | Frequency |
| Hip endoprothesis surgery | 10 |
| Laparotomy ovarian, pancreas, kidney tumour | 7 |
| Aorto-coronary bypass, aortic valve replacement | 6 |
| Hand surgery, e.g., radius osteosynthesis, carpal tunnel syndrome | 5 |
| Septorhinoplasty | 5 |
| Hysterectomy non-tumour (uterus myomatosus, metrorrhagia ) | 5 |
| Thyreoidectomy | 5 |
| Vaccuum-assisted closure | 4 |
| Shoulder surgery, e.g., shoulder endoprothesis, rotator cuff | 4 |
| Birth | 4 |
| Caesarean section | 3 |
| Mammary surgery non-tumour, e.g. breast reduction surgery | 3 |
| Mammary tumour resection surgery | 3 |
| Laparoscopic surgery, e.g., cholecystectomy, appendectomy | 3 |
| Laparoscopic sleeve surgery | 3 |
| Microlaryngoscopy | 3 |
| Pigtail procedure | 3 |
| Knee arthroscopy, e.g., anterior cruciate ligament, meniscectomy | 3 |
| Osteosynthesis ankle joint | 3 |
| Lymph node excision cervical | 3 |
| Implantable cardioverter defibrillator / pacemaker implantation | 3 |
| Cataract surgery | 2 |
| Olecranon surgery | 2 |
| Achilles tendon | 2 |
| Knee endoprothesis surgery | 2 |
| Thoracotomy tumour surgery | 2 |
| Total | 98 |
We added perioperatively dental status, location of dental damage, mouth opening, Mallampati score, nature of intubation technique and difficulty of intubation. For nerve injuries we added location of nerve injury, regression of symptoms, nature of nerve injury, symptom of nerve injury (e.g., paraesthesia, motor and sensation deficits), and use of ultrasound.
Complications were categorised by the severity of injury scoring system (SIS), except dental injuries, which were based on data from Sowaka [9]. The scoring systems range from zero to nine on the severity scale, zero meaning no obvious injury, one emotional injury only, two to four temporary injuries (two = insignificant, three = minor, four = major). From score five onwards, the severity scales include only permanent injuries (five = minor, six = significant, seven = major, eight = grave), ending with a score of nine for death.
We included 133 anaesthesia-related complications. Table 2 shows all types of reported complications and the specific description of each complication.
Table 2Summary and description of complications leading to a report classified by the severity injury scale (n = 133). Dental damage cannot be classified by SIS and is therefore labelled as N/A. SIS ≤4: temporary; SIS >4; permanent; SIS = 9: death
| Complication leading to a report | Total (%) | SIS ≤4 (%) | SIS >4 (%) | SIS = 9 (%) | Description of complications |
| Local anaesthesia intoxication | 3 (2.3) | 3 (2.3) | 0 | 0 | Patient had a seizure during peripheral nerve block |
| Cardiovascular event | 4 (3.0) | 2 (1.5) | 0 | 2 (1.5) | Cardiovascular mismanagement such as alarm suppression or drug overdose in spinal anaesthesia that led to a cardiovascular complication such as cardiovascular arrest |
| Vascular catheterisation event | 4 (3.0) | 2 (1.5) | 0 | 2 (1.5) | Mis-insertion of a central or peripheral venous catheter into arterial system |
| Catheter event | 5 (3.8) | 4 (3.0) | 0 | 1 (0.8) | Mis-insertion of a peridural, peripheral or gastric catheter or accidentally cutting it through so that parts of the catheter remained in the body |
| Positioning event | 8 (6.0) | 8 (6.0) | 0 | 0 | Neurological deficits reported after surgery that were clearly due to mal-positioning |
| Respiratory/airway event | 8 (6.0) | 7 (5.2) | 0 | 1 (0.8) | A "cannot ventilate cannot oxygenate" situation, or aspiration, or accidental one-sided intubation that led to pulmonary oedema |
| Other* | 10 (7.5) | 10 (7.5) | 0 | 0 | Complications that occurred only one to three times were summarised as "other" |
| Drug error | 11 (8.3) | 10 (7.5) | 1 (0.8) | 0 | Wrong drug unintentionally administered |
| Nerve injury | 17 (12.8) | 16 (12.0) | 1 (0.8) | 0 | Neurological impairment after neuraxial or peripheral nerve block |
| Teeth injury | 63 (47.3) | NA | NA | NA | Avulsion, crown fracture, enamel fracture, filling loss, subluxation of a tooth after insertion of airway device |
| Total | 133 (100) | 62 (46.5) | 2 (1.6) | 6 (4.6) |
* Includes ophthalmology, pain clinic and internal medicine
The complications that only occurred one to three times per category were summarised as "other" and are listed in table 3. Many of these complications, such as lip or vocal cord injuries, occur more often during anaesthestic procedures than reflected in this study.
Table 3Complications that only occurred one to three times and summarised as "others".
| Other complications | n |
| Eye injury | 1 |
| Post-spinal headache | 1 |
| Total spinal anaesthesia | 1 |
| Vocal cord injury | 1 |
| Dislocation of jaw | 1 |
| Incorrect breathing circuit | 1 |
| Incorrect technique without consent | 1 |
| Lip injuries | 3 |
| Total | 10 |
At the LUKS all patient data are uniformly recorded and documented in a hospital database. All patients undergoing surgery automatically get a standardised anaesthesia form, which includes patient demographic information, diagnosis, medication, ASA physical status, information on dental status, mouth opening ability and cervical spine movement, as well as notes on any cardiac and pulmonary health conditions. Mortality data were collected from the hospital database. Outcomes of anaesthesia-related complications were also documented in the hospital database.
The statistical evaluation included descriptive statistic (means, relative frequency) and calculation of incidence. We did not do a logistic regression. Statistical analysis was performed with R x64, version 3.6.1. Pearson's chi-square test was used on a 2 x 2 contingency table to test for differences in complications between emergency and non-emergency anaesthetic procedures. A p-value of less than 0.05 was considered statistically significant. The power of the study at this sample size has an 87% probability to detect emergency complications occurring twice as often as complications in non-emergency procedures for a 5% significance level. Calculations were carried out using methods laid out by Cohen in 1988 in statistical power analysis for the behavioural sciences [10]. Because of a p-value = 0.53 we cannot reject the null hypothesis that complications occur at a different rate in non-emergency anaesthesia compared to emergency anaesthesia.
We refer to annual anaesthetic reports dating back to 2003; between 2003 and 2019 there were 399,583 recorded anaesthetic procedures. Of these, 56,721 were emergency procedures. Five partially and one solely anaesthesia-related events ("cannot ventilate, cannot intubate situation") led to death. For calculation of the frequency of anaesthesia -related fatal complications all six cases were included. The partially anaesthesia death-related complications were all combined surgical and anaesthesiological complications.
Two patients suffered from permanent damage (SIS >4), 62 patients had temporary symptoms (SIS <4) and in 63 patients dental damage occurred.
A total of 257 complications were reported between 2003 and 2019. Of these, 124 complications were either not anaesthesia related or had incomplete data and were therefore excluded. There were no reported deaths or severe complications among the excluded files. Of the remaining 133 complications, 58% involved female patients. The age distribution showed a mean age of 55, ranging from a minimum age of 6 to a maximum age of 98 years. The majority of patients had an ASA physical status score of I or II (68%), 29% were ASA III or IV, and for 3% the score was undocumented. Table 4 gives an overview of the patients’ characteristics and shows the summary of complication incidences by hospital department. Most complications occurred in orthopaedic surgery with a frequency of 22.5%, followed by general surgery with 21.1% and 15% in otorhinolaryngological, obstetrics and gynaecological surgery.
In the majority of complications, the corresponding anaesthetic procedure was a general anaesthesia in 76.7% and a combined peripheral and general anaesthesia in 12%. 11.3% of all complications occurred in a regional anaesthesia, as seen in table 4.
Table 4Summary of complication incidences and patient descriptive statistics by hospital department with total anaesthesia numbers between 2003-2019.
| Variable | Cardiothoracic | Ear, nose and throat | General | Gynaecologyand obstetrics | Hand & plastic surgery | Neurosurgery | Oral and maxillofacial | Orthopaedics | Others* | Urology | Vascular | Total | ||
| Total patients | 8891 | 29,247 | 75`506 | 51,633 | 23,997 | 9557 | 7501 | 21,016 | 88,856 | 18`619 | 12`918 | 399`583 | ||
| Anaesthetic procedures, n (%) | ||||||||||||||
| General | 6626 (74.5) | 27,980 (95.7) | 48`981 (64.9) | 27,511 (53.3) | 7589 (31.6) | 9123 (95.5) | 7359 (98.1) | 11,063 (52.6) | 19,312 (21.7) | 11`182 (60.1) | 6`739 (52.2) | 183`465 | ||
| Regional | 114 (1.3) | 38 (0.1) | 11`602 (15.4) | 20,659 (40.0) | 12,243 (51.0) | 40 (0.4) | 5 (0.1) | 6044 (28.8) | 24,169 (27.2) | 3`697 (19.8) | 3`322 (25.7) | 81`933 | ||
| Combined | 1105 (12.4) | 65 (0.2) | 10`679 (14.1) | 810 (1.6) | 442 (1.9) | 8 (0.1) | 14 (0.2) | 3868 (18.4) | 150 (0.2) | 775 (4.2) | 549 (4.2) | 18`465 | ||
| MAC | 1046 (11.8) | 1164 (4.0) | 4`244 (5.6) | 2653 (5.1) | 3723 (15.5) | 386 (4.0) | 123 (1.6) | 41 (0.2) | 45,225 (50.9) | 2`965 (15.9) | 2`308 (17.9) | 63`878 | ||
| Complications | ||||||||||||||
| Patients, n (%) | 13 (9.8) | 20 (15.0) | 28 (21.1) | 20 (15.0) | 2 (1.5) | 4 (3.0) | 3 (2.3) | 30 (22.5) | 6 (4.5) | 4 (3.0) | 3 (2.3) | 133 (100) | ||
| Per 100000 | 146 | 68 | 37 | 39 | 8 | 42 | 40 | 143 | 7 | 21 | 23 | 33 | ||
| Age (years), mean ± SD | 66.7 ± 8.7 | 49.8 ± 21.8 | 53.5 ± 15.8 | 47 ± 17.2 | 51 ± 11.3 | 61.3 ± 16.5 | 51 ± 16.6 | 55.1 ± 25 | 59.5 ± 17.2 | 69.8 ± 16.1 | 69.7 ± 5.8 | 54.9 ± 19.4 | ||
| Sex, % | Male | 69.2 | 50.0 | 50.0 | 0.0 | 100.0 | 50.0 | 100.0 | 40.0 | 16.7 | 50.0 | 33.3 | 42.1 | |
| Female | 30.8 | 50.0 | 50.0 | 100.0 | 0.0 | 50.0 | 0.0 | 60.0 | 83.3 | 50.0 | 67.7 | 57.9 | ||
| ASA score, % | 1–2 | 23.1 | 80.0 | 71.4 | 88.9 | 50.0 | 75.0 | 66.7 | 75.9 | 66.7 | 66.7 | 33.3 | 69.8 | |
| 3–4 | 76.9 | 20.0 | 28.6 | 11.1 | 50.0 | 25.0 | 33.3 | 24.1 | 33.3 | 33.3 | 66.7 | 30.2 | ||
| BMI, % | <18.5 kg/m2 | 0.0 | 5.6 | 0.0 | 6.7 | 0.0 | 0.0 | 0.0 | 4.3 | 50.0 | 50.0 | 0.0 | 4.8 | |
| 18.5–24.9 kg/m2 | 18.2 | 27.8 | 30.4 | 46.7 | 50.0 | 0.0 | 33.3 | 30.4 | 0.0 | 0.0 | 0.0 | 28.6 | ||
| 25.0–29.9 kg/m2 | 27.3 | 44.4 | 47.8 | 20.0 | 0.0 | 50.0 | 66.7 | 30.4 | 0.0 | 50.0 | 50.0 | 36.2 | ||
| >30 kg/m2 | 54.5 | 22.2 | 21.7 | 26.7 | 50.0 | 50.0 | 0.0 | 34.8 | 50.0 | 0.0 | 50.0 | 30.5 | ||
| Anaesthesia, % | General | 100.0 | 100.0 | 71.4 | 75.0 | 50.0 | 100.0 | 100.0 | 56.7 | 66.7 | 75.0 | 33.3 | 76.7 | |
| Regional or combined | 0.00.0 | 0.0 0.0 | 10.717.9 | 25.00.0 | 0.050.0 | 0.00.0 | 0.00.0 | 13.330.0 | 33.30.0 | 0.025.0 | 66.70.0 | 11.312.0 | ||
| Emergency, % | No | 92.3 | 95.0 | 78.6 | 80.0 | 100.0 | 75.0 | 66.7 | 76.7 | 100.0 | 75.0 | 100.0 | 83.5 | |
| Yes | 7.7 | 5.0 | 21.4 | 20.0 | 0.0 | 25.0 | 33.3 | 23.3 | 0.0 | 25.0 | 0.0 | 16.5 | ||
| Died, % | No | 84.6 | 100.0 | 96.4 | 100.0 | 100.0 | 100.0 | 100.0 | 93.3 | 100.0 | 100.0 | 66.7 | 84.6 | |
| Yes | 15.4 | 0.0 | 3.6 | 0.0 | 0.0 | 0.0 | 0.0 | 6.7 | 0.0 | 0.0 | 33.3 | 15.4 | ||
* Others includes ophthalmology, pain clinic and internal medicine. Combined: combined regional with general anaesthesia; MAC: monitored anaesthesia care; SD: standard deviation
Table 2 outlines the incidence of all complications and the SIS score. Most frequent were dental injuries (47.3%), followed by nerve injuries (12.8%). Respiratory and airway events were 6% and included five cases of "cannot ventilate cannot intubate" situations. Permanent injuries (SIS >4) occurred in two cases (1.6%) and death (SIS = 9) in six cases (4.6%). 62 complications (46.5%) were temporary (SIS ≤4). Temporary complications and dental injuries accounted for 93.8% of all complications.
Figure 2 shows the number of events, ranging from 2 to 17, by year.
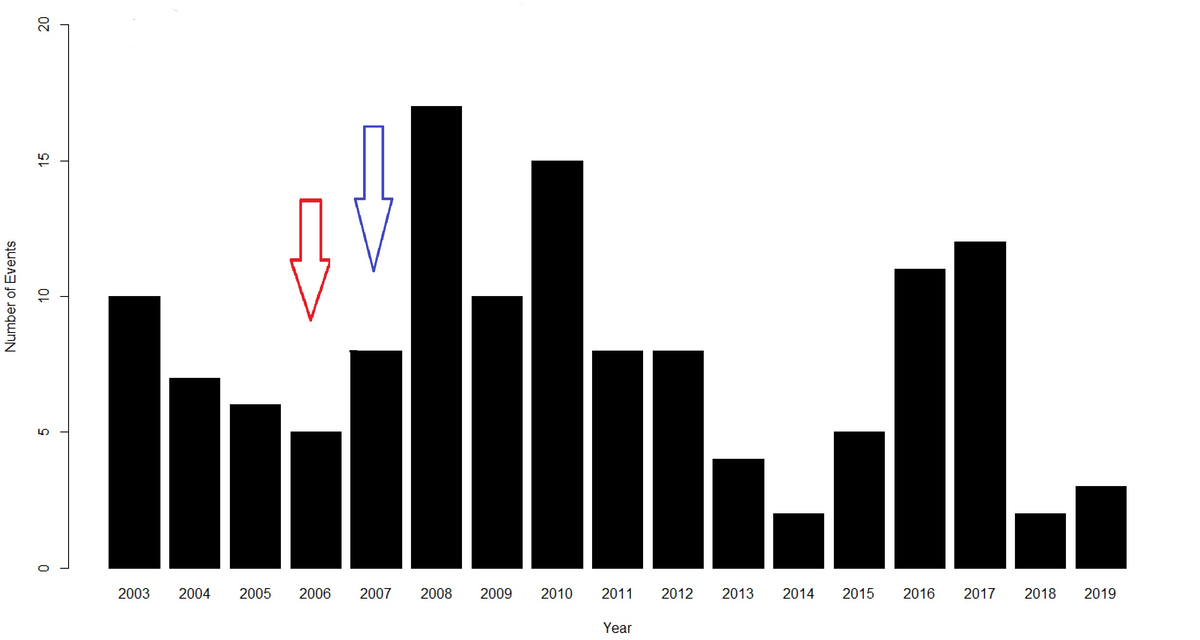
Figure 2 Number of events by year n = 133. The red arrow indicates implementation of the critical incident reporting system (CIRS) at the LUKS in 2006. The blue arrow represents arrival of a new head of the Department of Anaesthesiology in 2007.
The red arrow represents the implementation of a critical incident reporting system (CIRS) in 2006 and the blue arrow the arrival of a new head of department of anaesthesiology in 2007, involving relevant changes detailed in the discussion below. The temporal trends of the complications are shown in fig. 3.
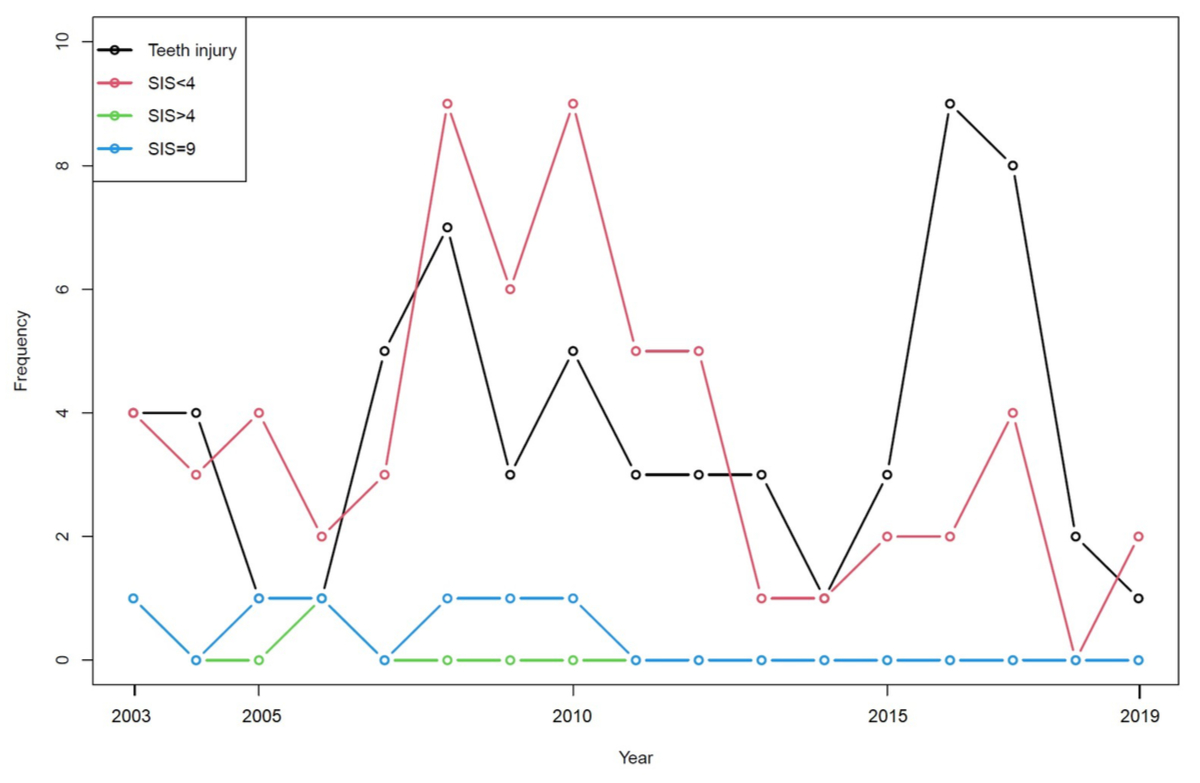
Figure 3 Temporal trends of anaesthesia-related complications SIS <4 (red dotted line), SIS >4 (green dotted line), SIS = 9 (blue dotted line) and tooth injuries (black dotted line) from 2003 to 2019. Number of events by year (n = 133). Each dot represents one year.
There was a sharp decrease of SIS >4, and in particular of deaths. After 2010, no death due to a partially anaesthesia-related complication occurred. Although major complications declined, there was an increase of SIS <4 and dental damage between 2008 and 2010, followed by a second peak in 2016/2017. The first increase of complications related to incidents with SIS <4, whereas in 2016/2017 the majority of complications were dental damage.
The anaesthesia-related death rate was approximately 1.5 per 100,000. There were five cases of a "cannot ventilate, cannot intubate" situation during this period, leading to a frequency of 1.25 cases per 100,000 anaesthetics. The estimated frequency for nerve injury (11 neuraxial, 6 peripheral) during the same period was 4 nerve injuries per 100,000 anaesthetics. The frequencies for neuraxial and peripheral nerve injuries were 3 and 1.5 per 100,000 anaesthetics, respectively.
The approximate incidence for dental injuries between 2003 and 2019 was 0.02% with a frequency of 16 cases per 100,000 anaesthetics.
The overall frequency of complications was 133 events from 2003 to 2019, resulting in 33 complications per 100,000 anaesthetics. Minor complications (including dental damage) occurred in approximately 31 per 100,000 anaesthetics.
In 87.5% the complication occurred during elective day surgery. However, there was no significant difference in the incidence of complications between elective day surgery and emergency surgery (p = 0.45).
The two most frequent complications, nerve and dental injuries, are considered in more detail in the following sections.
Nerve injuries were the second most frequent complications and were reported most frequently in the orthopaedic department (35.3%).
Nerve injuries were mostly caused by neuraxial nerve blocks (64.7%, 11 of 17). The most common nerve injuries were a combined partial motor deficit (35.3%, 6 of 17), followed by partial motor and sensory deficits (29.4%, 5 of 17). Only a minority of patients suffered from paraesthesia (11.8%, 2 of 17); both had received a neuraxial nerve block. One patient developed a total motor deficit after a thoracic epidural.
Of the neuraxial nerve injuries, 41.2% (7 of 11) were due to epidural anaesthesia and 17.4% (3 of 11) due to spinal anaesthesia. Among the epidural anaesthetics, three were thoracic epidurals and four lumbar epidurals. One thoracic and one lumbar epidural anaesthetic led to permanent damage due to an epidural haematoma.
In our study, femoral and interscalene nerve blocks led to most of the peripheral nerve block injuries (25%, 4 of 6), followed by axillary and supraclavicular nerve blocks (6.25%, 1 of 6). Most peripheral nerve injuries occurred in the orthopaedic surgery department(83.3%, 5 of 6).
Dental injuries were the most frequent complications and occurred mostly in the general and otorhinolaryngology departments.
In 71% (45 of 63) of events, dental damage resulted from using a conventional laryngoscope. Airway assist tools such as c-Mac® videolaryngoscopes were purchased first in 2009 and device numbers increased over time, especially in 2016. In total, 14% (9 of 63) of dental injuries occurred with videolaryngoscopy.
In 30% (19 of 63) a difficult airway situation led to dental damage. During emergency intubation only upper teeth were damaged.
In most cases dental injuries were caused by poor intubation technique (38%, 24 of 63), by using excessive force and/or touching fragile teeth during intubation.
We found that the upper maxillary incisors "11" and "21" (numbered according to the two-digit World Dental Federation notation system) were most prone to be injured during intubation, with an incidence of 24% and 23%, respectively. Prior to their operation, 37% (23 of 63) of patients with dental damage had a good dental status, whereas the dental status was impaired in 30% (19 of 63). In 17% (11 of 63), the patients suffered from periodontal disease. In 76% (48 of 63) dental status was described as strong without prior dental examination. Most reported dental injuries were avulsion (25%, 16 of 63) and enamel fracture (24%, 15 of 63).
In general, and in our study, severe anaesthesia-related incidents and deaths have decreased over time and are rare events [1, 11]. Permanent damage and death as an anaesthesia-related complication is reported in literature at less than 1 per 100,000 anaesthetics [2, 12–15]. Minor anaesthesia-related incidents are much more frequent, however. The overall incidence of minor anaesthesia-related perioperative events is reported to be between 18% and 22% [15, 16]. In our study, we had an anaesthesia-related mortality rate of approximately 1.5 per 100,000, and minor complications (SIS <4) occurred in approximately 31 per 100,000 anaesthetics.
During the study period, 399,583 anaesthetics took place with 254 complications being reported to the department of anaesthesiology. Because of incomplete forms or incidents not being anaesthetic complications, 124 were excluded. The excluded complications did not include any cases of SIS >4. We therefore estimated the impact of reporting bias from the excluded files to be minimal.
Of the 133 anaesthesia-related complications in our study, 47.3% were related to dental damage and 12.8% to nerve injuries. There were five "cannot ventilate, cannot intubate" situations, resulting in a relative frequency of 1.25 per 100,000 general anaesthetics. The incidence of "cannot ventilate, cannot oxygenate" in the literature varies according to clinical setting and study. Incidence rates of between 3 and 100 per 100,000 in trauma patients [17] or 4.5 per 100,000 general anaesthetics [18] are reported .
Of the six deaths that occurred, four were due to emergency operations. This suggests that in emergency cases, the potential risk for mistakes can be higher. Several studies showed that emergency situations are an important contributory factor for mistakes [19, 20].
Although not statistically significant (p = 0.45), the majority of complications occurred during elective day surgery rather than emergency surgery because more interventions were elective. In Denmark, Pedersen et al. studied the impact of emergency surgery on anaesthesia-related complication and found that in emergency procedures complications attributed to anaesthesia were less common than in elective surgery. Yet Pedersen et al. stated that the probability of a severe complication in an emergency procedure was much higher than with an elective procedure [21].
At the LUKS hospital, a critical incident reporting system (CIRS) was implemented in 2006. It was improved in 2008 with easy electronic accessibility, minimal paperwork and regular feedback rounds, so that this reporting system has been well established over time with increasing incident reports. This trend is shown in figure 2 [8].
There was a change of head of department in 2007, who encouraged the reporting of incidents or injuries in special anaesthesia report files. Because of new standards as well as a reorganisation of the reporting system, more incidents were reported, as can be seen in figures 2 and 3.
Although the reported incidents increased after implementation of CIRS and the departmental changes, the number of reported complications decreased. Most of all, SIS >4 and death did not occur after 2010. This could suggest that, owing to new techniques and safety standards, the probability of a severe complication or death decreased. On the other hand, minor complications and dental damage increased. Although other studies have shown the same decreasing tendency in severe anaesthesia complications, the incidence of minor complications has not changed much over time [15, 16]. This could suggest that new techniques and safety standards are not enough to prevent complications, but have to be combined with improvement of education, crew resource management training and unwavering vigilance [22].
It is generally believed that nerve injuries due to neuraxial anaesthesia are rare. However, there is evidence in literature that these incidents are more frequent than expected. The incidence of complications differs widely in different studies. The third national audit project of the Royal College of Anaesthetists estimated the incidence of permanent injury after central neuraxial block to be 4.2 per 100,000 pessimistically and 2.0 per 100,000 optimistically [23]. In our study, we calculated a relative frequency for neuraxial nerve injuries of about 3 per 100,000 anaesthetics.
Haematoma was the most common cause of neuraxial injuries and the majority (72%) were associated with either intrinsic or iatrogenic coagulopathy [24]. Cheney et al. reported in his closed claims report that 22% of spinal cord injuries were due to epidural haematoma [25]. The two cases of paraplegia in our study were both due to epidural haematoma without iatrogenic coagulopathy.
Peripheral nerve injuries due to regional anaesthesia are rare. In Saba et al., it is 0.3% for permanent nerve injuries [26]. In our study we had a relative frequency for all peripheral nerve injuries of 0.002%.
In our study, most anaesthesia complications were dental damage. We calculated an approximate frequency of 0.02%. A retrospective study on dental injuries by Christensen et al. showed similar results, with an incidence of approximately 0.02% [27]. Other studies showed a much higher frequency of anaesthesia-related events, as in the case-control study by Newland et al. with 0.048% [28]. In other retrospective studies incidences ranged from 0.02% to 0.11% [27, 29, 30] and up to 38.6% in prospective studies [31, 32]. An explanation for these large differences in incidence in prospective studies could be that dental examination was performed before and after surgery in these prospective studies [27].
There was a major peak of reported dental injuries in 2016 and 2017. During these two years there was a major acquisition of c-Mac® videolaryngoscopes. Of the 17 reported dental injuries in these two years, 10 were with conventional and 7 with c-Mac® videolaryngoscopes. After the two years of increasing dental injuries with c-Mac® videolaryngoscopes in 2016 and 2017, numbers decreased. This could suggest a learning curve and that initial wrong handling can enhance the risk of dental injury. Ham et al. identified the use of videolaryngoscopy as a statistically significant predictor of dental injuries due to the user's focus being more on the screen and less on the patient's teeth [33]. Other studies showed, however, that videolaryngoscopy offers better visualisation of the glottis and vocal cords and can lead to less dental damage when used by skilled practitioners [34, 35].
In our study, teeth numbers "11" and 21" were the most at risk for dental trauma. Other studies also showed a greater risk for injury of upper maxillary incisors during intubation, most of all when the view of the glottis was unsatisfactory or impossible to obtain. To improve the view, the patients’ maxillary anterior teeth are sometimes used as a fulcrum for the laryngoscope blade [28, 36–38]. Additionally, increased force exerted during laryngoscopy is a potential risk for dental trauma, as well as inadequate intubation technique [38].
Most dental injuries in our study were avulsions, followed by enamel fractures. A previous review by Ham et al. reported subluxation or loosened teeth as the most common form of injury [33] while a study by Mourão found enamel fracture to be the most common lesion [31].
The majority of dental damage was related to a pre-existing good (37%) and impaired dental status (30%). During preoperative evaluation of dental status, 76% were recorded as strong, though there was no physical inspection of individual teeth. Most of the dental councils at the LUKS stated postoperatively that tooth avulsion or subluxation were due to periodontitis and preoperatively loosened teeth. This can also explain why we had a large number of cases of dental damage in supposedly good dental status in our study, which leads to the suggestion that, if in doubt, a physical preoperative evaluation of periodontal disease could be sensible. According to several authors, the preoperative visit is important for the evaluation of dental injury predictors, mainly regarding possible difficult intubation and conspicuous dental status [38, 39]. Furthermore, there is a five-fold higher risk for dental injury with pre-existing pathology and even a twenty-fold higher risk for patients with previously reported intubation difficulties [28].
The strength of this study is that it included different types of anaesthetic complications over 17 years and the impact of new techniques and departmental changes on the occurrence of complications. An important limitation of this study is the reporting bias. Research has shown that only a small percentage of doctors report incidents. Possible factors are unfamiliarity with the reporting process, and fear of discrimination at the workplace or of legal ramifications [40–44]. Additionally, cultural factors, such as the belief that only "bad doctors" make mistakes, as well as a lack of understanding of how a reported incident can improve system processes, may influence the reporting process [43–45]. Furthermore, many medical workers do not even consider reporting a "near miss", although these incidents are an important source of learning and improvement [44, 45].
Further limitations of this study are that it was only observational and from one single hospital unit over a period of 17 years.
However, this study gives an interesting overview of anaesthesia-related complications and it certainly had an impact on the day-to-day processes at the department of anaesthesiology at the LUKS.
The present study supports the view that anaesthesia-related complications are rare events, occurring most often during elective procedures. The majority of complications were only temporary. The mortality rate, and the incidence of dental and nerve injuries reported in this study were comparable to international studies. During the study period, the temporal trend of complications showed a clear decline in severe incidents and deaths, whereas minor complications and dental injuries predominated after 2010. This trend is also represented in international studies. Although complications at the LUKS decreased with implementation of new techniques, safety standards and reporting systems, the occurrence of minor complications could not be reduced. It suggests this does not depend solely on structural and safety changes, but rather that more effort needs to be put into education, crew resource management and vigilance. It is therefore necessary to evaluate further strategies and assess possible risk factors to decrease the risk of complications.
The authors received no specific funding for this article.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Schiff JH , Welker A , Fohr B , Henn-Beilharz A , Bothner U , Van Aken H , et al. Major incidents and complications in otherwise healthy patients undergoing elective procedures: results based on 1.37 million anaesthetic procedures. Br J Anaesth. 2014 Jul;113(1):109–21. https://doi.org/10.1093/bja/aeu094
2. Mellin-Olsen J , Staender S , Whitaker DK , Smith AF . The Helsinki Declaration on Patient Safety in Anaesthesiology. Eur J Anaesthesiol. 2010 Jul;27(7):592–7. https://doi.org/10.1097/EJA.0b013e32833b1adf
3. Staender S , Schaer H , Clergue F , Gerber H , Pasch T , Skarvan K , et al. A Swiss anaesthesiology closed claims analysis: report of events in the years 1987-2008. Eur J Anaesthesiol. 2011 Feb;28(2):85–91. https://doi.org/10.1097/EJA.0b013e3283414fea
4. Reason J . Safety in the operating theatre – Part 2: human error and organisational failure. Curr Anaesth Crit Care. 1995;6(2):121–6. https://doi.org/10.1016/S0953-7112(05)80010-9
5. Beecher HK , Todd DP . A study of the deaths associated with anesthesia and surgery: based on a study of 599, 548 anesthesias in ten institutions 1948-1952, inclusive. Ann Surg. 1954 Jul;140(1):2–35. https://doi.org/10.1097/00000658-195407000-00001
6. Staender S . Patientensicherheit, Morbidität, Letalität in der Anästhesiologie. In Roissant R, Werner C, Zwissler B, editors. Die Anästhesiologie. Vol 1., 4th ed. Berlin: Springer; 2019. pp. 1101-1112.
7. Cooper JB , Newbower RS , Long CD , McPeek B . Preventable anesthesia mishaps: a study of human factors. Anesthesiology. 1978 Dec;49(6):399–406. https://doi.org/10.1097/00000542-197812000-00004
8. Luzerner Kantonsspital Annual Report 2019. May 2020. https://www.luks.ch/sites/default/files/2020-06/QBericht_1152-2019_de.pdf [Accessed 02 September 2020].
9. Sowaka MP . Medical malpractice closed claims : final compilation. In : Sowka M, ed. Brookefield, WI, USA : National Association of Insurance Commissioners; 1980
10. Cohen J . Statistical power analysis for the behavioural sciences. 2nd ed. USA: Lawrence Erlbaum associates, publishers; 1988.
11. Gibbs NM . National anaesthesia mortality reporting in Australia from 1985-2008. Anaesth Intensive Care. 2013 May;41(3):294–301. https://doi.org/10.1177/0310057X1304100304
12. Arbous MS , Grobbee DE , van Kleef JW , de Lange JJ , Spoormans HH , Touw P , et al. Mortality associated with anaesthesia: a qualitative analysis to identify risk factors. Anaesthesia. 2001 Dec;56(12):1141–53. https://doi.org/10.1111/j.1365-2044.2001.02051.x https://doi.org/10.1046/j.1365-2044.2001.02051.x
13. Lienhart A , Auroy Y , Péquignot F , Benhamou D , Warszawski J , Bovet M , et al. Survey of anesthesia-related mortality in France. Anesthesiology. 2006 Dec;105(6):1087–97. https://doi.org/10.1097/00000542-200612000-00008
14. Li G , Warner M , Lang BH , Huang L , Sun LS . Epidemiology of anesthesia-related mortality in the United States, 1999-2005. Anesthesiology. 2009 Apr;110(4):759–65. https://doi.org/10.1097/ALN.0b013e31819b5bdc
15. Bothner U , Georgieff M , Schwilk B . Building a large-scale perioperative anaesthesia outcome-tracking database: methodology, implementation, and experiences from one provider within the German quality project. Br J Anaesth. 2000 Aug;85(2):271–80. https://doi.org/10.1093/bja/85.2.271
16. Fasting S , Gisvold SE . Statistical process control methods allow the analysis and improvement of anesthesia care. Can J Anaesth. 2003 Oct;50(8):767–74. https://doi.org/10.1007/BF03019371
17. Tachibana N , Niiyama Y , Yamakage M . Incidence of cannot intubate-cannot ventilate (CICV): results of a 3-year retrospective multicenter clinical study in a network of university hospitals. J Anesth. 2015 Jun;29(3):326–30. https://doi.org/10.1007/s00540-014-1847-1
18. Frerk C , Mitchell VS , McNarry AF , Mendonca C , Bhagrath R , Patel A , et al.; Difficult Airway Society intubation guidelines working group . Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015 Dec;115(6):827–48. https://doi.org/10.1093/bja/aev371
19. Donchin Y , Gopher D , Olin M , Badihi Y , Biesky M , Sprung CL , et al. A look into the nature and causes of human errors in the intensive care unit. Crit Care Med. 1995 Feb;23(2):294–300. https://doi.org/10.1097/00003246-199502000-00015
20. Reason J . Safety in the operating theatre – Part 2: human error and organisational failure. Curr Anaesth Crit Care. 1995;6(2):121–6. https://doi.org/10.1016/S0953-7112(05)80010-9
21. Pedersen T . Complications and death following anaesthesia. A prospective study with special reference to the influence of patient-, anaesthesia-, and surgery-related risk factors. Dan Med Bull. 1994 Jun;41(3):319–31.
22. Aitkenhead AR . Injuries associated with anaesthesia. A global perspective. Br J Anaesth. 2005 Jul;95(1):95–109. https://doi.org/10.1093/bja/aei132
23. Cook TM , Counsell D , Wildsmith JA ; Royal College of Anaesthetists Third National Audit Project . Major complications of central neuraxial block: report on the Third National Audit Project of the Royal College of Anaesthetists. Br J Anaesth. 2009 Feb;102(2):179–90. https://doi.org/10.1093/bja/aen360
24. Lee LA , Posner KL , Domino KB , Caplan RA , Cheney FW . Injuries associated with regional anesthesia in the 1980s and 1990s: a closed claims analysis. Anesthesiology. 2004 Jul;101(1):143–52. https://doi.org/10.1097/00000542-200407000-00023
25. Cheney FW , Domino KB , Caplan RA , Posner KL . Nerve injury associated with anesthesia: a closed claims analysis. Anesthesiology. 1999 Apr;90(4):1062–9. https://doi.org/10.1097/00000542-199904000-00020
26. Saba R , Brovman EY , Kang D , Greenberg P , Kaye AD , Urman RD . A Contemporary Medicolegal Analysis of Injury Related to Peripheral Nerve Blocks. Pain Physician. 2019 Jul;22(4):389–400.
27. Christensen RE , Baekgaard JS , Rasmussen LS . Dental injuries in relation to general anaesthesia-A retrospective study. Acta Anaesthesiol Scand. 2019 Sep;63(8):993–1000. https://doi.org/10.1111/aas.13378
28. Newland MC , Ellis SJ , Peters KR , Simonson JA , Durham TM , Ullrich FA , et al. Dental injury associated with anesthesia: a report of 161,687 anesthetics given over 14 years. J Clin Anesth. 2007 Aug;19(5):339–45. https://doi.org/10.1016/j.jclinane.2007.02.007
29. Vogel J , Stübinger S , Kaufmann M , Krastl G , Filippi A . Dental injuries resulting from tracheal intubation—a retrospective study. Dent Traumatol. 2009 Feb;25(1):73–7. https://doi.org/10.1111/j.1600-9657.2008.00670.x
30. Warner ME , Benenfeld SM , Warner MA , Schroeder DR , Maxson PM . Perianesthetic dental injuries: frequency, outcomes, and risk factors. Anesthesiology. 1999 May;90(5):1302–5. https://doi.org/10.1097/00000542-199905000-00013
31. Mourão J , Neto J , Luís C , Moreno C , Barbosa J , Carvalho J , et al. Dental injury after conventional direct laryngoscopy: a prospective observational study. Anaesthesia. 2013 Oct;68(10):1059–65. https://doi.org/10.1111/anae.12342
32. Mourão J , Neto J , Viana JS , Carvalho J , Azevedo L , Tavares J . A prospective non-randomised study to compare oral trauma from laryngoscope versus laryngeal mask insertion. Dent Traumatol. 2011 Apr;27(2):127–30. https://doi.org/10.1111/j.1600-9657.2010.00947.x
33. Ham SY , Kim J , Oh YJ , Lee B , Shin YS , Na S . Risk factors for peri-anaesthetic dental injury. Anaesthesia. 2016 Sep;71(9):1070–6. https://doi.org/10.1111/anae.13560
34. Cooper RM . Complications associated with the use of the GlideScope videolaryngoscope. Can J Anaesth. 2007 Jan;54(1):54–7. https://doi.org/10.1007/BF03021900
35. Chemsian R , Bhananker S , Ramaiah R . Videolaryngoscopy. Int J Crit Illn Inj Sci. 2014 Jan;4(1):35–41. https://doi.org/10.4103/2229-5151.128011
36. Yasny JS . Perioperative dental considerations for the anesthesiologist. Anesth Analg. 2009 May;108(5):1564–73. https://doi.org/10.1213/ane.0b013e31819d1db5
37. Givol N , Gershtansky Y , Halamish-Shani T , Taicher S , Perel A , Segal E . Perianesthetic dental injuries: analysis of incident reports. J Clin Anesth. 2004 May;16(3):173–6. https://doi.org/10.1016/j.jclinane.2003.06.004
38. de Sousa JM , Mourão JI . Tooth injury in anaesthesiology. Braz J Anesthesiol. 2015 Nov-Dec;65(6):511–8. https://doi.org/10.1016/j.bjane.2013.04.011
39. Owen H , Waddell-Smith I . Dental trauma associated with anaesthesia. Anaesth Intensive Care. 2000 Apr;28(2):133–45. https://doi.org/10.1177/0310057X0002800202
40. Vincent C , Stanhope N , Crowley-Murphy M . Reasons for not reporting adverse incidents: an empirical study. J Eval Clin Pract. 1999 Feb;5(1):13–21. https://doi.org/10.1046/j.1365-2753.1999.00147.x
41. Eland IA , Belton KJ , van Grootheest AC , Meiners AP , Rawlins MD , Stricker BH . Attitudinal survey of voluntary reporting of adverse drug reactions. Br J Clin Pharmacol. 1999 Oct;48(4):623–7. https://doi.org/10.1046/j.1365-2125.1999.00060.x
42. Firth-Cozens J . Barriers to incident reporting. Qual Saf Health Care. 2002 Mar;11(1):7–7. https://doi.org/10.1136/qhc.11.1.7
43. Mahajan RP . Critical incident reporting and learning. Br J Anaesth. 2010 Jul;105(1):69–75. https://doi.org/10.1093/bja/aeq133
44. Polisena J , Gagliardi A , Urbach D , Clifford T , Fiander M . Factors that influence the recognition, reporting and resolution of incidents related to medical devices and other healthcare technologies: a systematic review. Syst Rev. 2015 Mar;4(1):37. https://doi.org/10.1186/s13643-015-0028-0
45. Evans SM , Berry JG , Smith BJ , Esterman A , Selim P , O’Shaughnessy J , et al. Attitudes and barriers to incident reporting: a collaborative hospital study. Qual Saf Health Care. 2006 Feb;15(1):39–43. https://doi.org/10.1136/qshc.2004.012559