“Shaping the new freedom”: A reflexive thematic analysis on patients’ post cure needs after years of living with hepatitis C
DOI: https://doi.org/10.4414/SMW.2022.w30177
Helen
Guggisbergab, Dunja
Niccaac, Anton
Kohlerd, Philip
Bruggmannd, Patrizia
Künzler-Heuleae
aInstitute of Nursing Science, University of Basel, Basel, Switzerland
bDepartment of Surgery, Cantonal Hospital Aarau, Aarau, Switzerland
cDepartment of Global and Public Health, Institute for Epidemiology, Biostatistics and Prevention, University of Zurich, Switzerland
dArud Centre for Addiction Medicine, Zurich, Switzerland
eDepartment of Gastroenterology/Hepatology and Department of Nursing, Cantonal Hospital St. Gallen, St. Gallen, Switzerland
Summary
BACKGROUND: Direct-acting antivirals present a treatment opportunity that provides high rates of sustained viral response even for people who have lived for years with hepatitis C virus (HCV) infection. While it is known that liver-related morbidity and mortality can be decreased and many symptoms reversed, this population's need for post-treatment professional support has not been extensively assessed. Therefore, our study aimed to describe the experiences of patients cured of chronic HCV infection and explore the meaning of these experiences regarding specific follow-up care needs within the context of the Swiss health system.
METHODS: For this qualitative study, we applied a reflexive thematic analysis approach with a social constructivist orientation. Twelve participants shared their experiences of being cured and their needs regarding follow-up care. Subsequently, the data were analysed in an iterative process based on Braun and Clarke's six phases of analysis.
RESULTS: In the overarching theme, participants summarised their new situation with the statement, “being cured feels like being released from a cage”. They experienced striking health improvements with overwhelmingly positive influences on their everyday lives. This experience was characterised for all participants by important changes on three levels. We categorised these in three sub-themes: a) “the ball and chain have been lightened”: this sub-theme illustrates the reduction of social limitations and emotional stress; b) “the gnawing at the liver has let up”: this signifies relief from physical symptoms and strongly improved well-being. And under the third sub-theme, “shaping the new freedom”, the participants described their new situation as a sometimes-stressful challenge because they had to reorient their self-management. They shared their concerns regarding the ongoing stigma of HCV infection, feeling insecure in their own health after being cured, and learning how to use their heightened sense of confidence and openness to enact behavioural changes that would improve their health-related lifestyles.
CONCLUSION: The findings of this study provide insights into treatment experiences of patients cured of chronic HCV infection and the need for follow-up care even after successful virus eradication. The results can sensitise healthcare professionals to patients’ post-cure challenges and guide their care interventions. Some of these challenges, such as dealing with stigma, can be addressed during treatment; other needs, like providing motivation to engage in healthy behaviour, may warrant targeted follow-up.
Introduction
In 2021, the World Health Organization (WHO) reported two important figures regarding the hepatitis C virus (HCV): first, that 58 million people are living with chronic HCV infections; and second, that they expect 1.5 million new infections per year [1] , this since HCV infection had become a leading cause of deaths worldwide by 2013 [2]. In Switzerland, a 2021 study estimated a viral infection prevalence of approximately 32,000 (0.37%) [3]. This is a reduction from 2016, mainly due to improved therapies. However, liver failure and liver cancer remain significant causes of death in Switzerland [4]. Successful treatment of HCV leads to sustained viral response (SVR), i.e., no detectable HCV-RNA 12 to 24 weeks after therapy (SVR12-SVR24). This greatly decreases the risk for liver-related morbidity and mortality [4–6].
Since 2013, well-tolerated and effective direct-acting antivirals have facilitated treatment, increasing SVR rates significantly. Direct-acting antivirals offer a >95% probability of curing HCV infections [7]. Until their full implementation in 2015, the former standard interferon-based treatment commonly failed, at a rate of 50–60% in genotype 1 or 20–30% in genotype 2. As the treatment itself had numerous unpleasant side effects, patients were reluctant to start it and it was sometimes contraindicated because of comorbidities, such as major depression, decompensated cirrhosis [8]. As a result, many people spent years coping with HCV's physical and social consequences. For example, patients reported high symptom prevalence for fatigue [9, 10], nausea, abdominal, joint, and muscle pain, depression and forgetfulness [9, 11]. These led to serious social limitations including difficulty maintaining a full-time job [12]. Adding to these burdens, patients were often stigmatised because of HCV's common association with drug use or high-risk sexual behaviours [13–15].
With the introduction of direct-acting antiviral therapy, research showed tremendous improvements. Quantitative studies showed that, in addition to eliminating any measurable HCV-related PCR, the new therapies positively impacted well-being and quality of life, especially pain reduction, alleviation of depressive symptoms [16–18], and improvements in mobility, functional well-being and fatigue [16, 17, 19]. In qualitative studies, patients reported that they were relieved that they could no longer transmit HCV, expected less stigmatisation, felt healthier, and had regained some sense of well-being. Generally, they envisioned their future more positively and were motivated to stay healthy and prevent reinfection [20–23].
Despite these effects, continued follow-up care is medically recommended for selected patient groups [5]. The current Swiss HCV guidelines [24] suggest three conditions where patients should remain in follow-up: hepatocellular carcinoma (HCC) surveillance is indicated because of either advanced liver fibrosis (Metavir F3) or cirrhosis (Metavir F4); co-factors for the development/progression of liver diseases; or if they are particularly at risk of reinfection.
However, these guidelines currently focus only on medically-defined physical conditions and major risk factors. In contrast, cancer survivor follow-up care guideline include psychosocial and behavioural criteria for referral to counselling services to ease former cancer patients' worries and fears while supporting their health-enhancing behaviours [25]. To date, as few qualitative studies describe HCV patients’ post-cure experiences, little is known about their follow-up care needs or useful support services [21–23]. Aiming at a patient-centred care approach such as recommended by Madden et. al. [20] for people who use drugs, the perspectives of HCV patients who have achieved SVR24 are needed, as they potentially complement the medical criteria of current follow-up guidelines [5, 24].
Therefore, within the context of the Swiss health system, this qualitative study's aim is to describe patients' experiences during and after treatment for chronic HCV infection, and to use these experiences to understand HCV-specific follow-up care needs.
Methods
This qualitative study was conducted using a reflexive thematic analysis approach [26] with a constructivist orientation. The authors treat meaning and experience as socially produced and reproduced within certain contexts and with communalities and differences between individuals [27].
This study was approved by the lead Ethics Committee of St. Gallen, Switzerland and the corresponding local Ethics Committee of Zurich (reference number 2019-01202 EKOS 19/099). It was conducted in accordance with principles enunciated in the current version of the Declaration of Helsinki [27], the principles of Good Clinical Practice issued by the International Council on Harmonisation (ICH), and Swiss legal regulations (Human Research Ordinance, 2013; SR 810. 301). All participants provided written informed consent prior to participation.
Setting and sampling
This study was conducted at two centres providing medical and psychosocial care for patients with HCV infections—one specialising in hepatology, the other in addiction medicine. Health care professionals (HCPs) at both centres invited patients to participate and provided written study information. Patients were eligible to participate if they were at least 18 years old, had lived at least ten years with a chronic HCV infection, had achieved SVR24 with direct-acting antivirals, were able to participate in an interview in German and provided written informed consent.
We used a purposive sampling approach to include a diverse range of participants [28]. Based on pre-defined criteria, we included participants a) of both genders; b) of various ages; and c) for whom the current Swiss guidelines either recommend or do not recommend a need for medical follow-up after SVR24 [24]. Of 15 patients contacted, twelve agreed to participate. The remaining three declined due to lack of time.
Patient and public involvement
For this research, patient and public involvement was crucial at several points. First, the patient representatives were also active members of the Swiss Hepatitis Strategy and were involved in the development of the current study's research question [29]. Second, to add a patient perspective throughout the study, we involved one patient representative [30]. That representative's feedback was vital to the development of our interview guide, data analyses and critical readings of the manuscript.
Data collection
Data were collected via semi-structured interviews, all conducted by the same researcher (HG) who had no prior relationship with participants. She followed an interview guide with open-ended questions based on published evidence and input from the patient representative and clinicians [30]. Questions addressed patients’ experiences before, during and after treatment. All interviews started with the open question, “How do you experience your situation after being cured of hepatitis C?" and continued with questions about self-perceived health status, treatment decisions and interactions both with the healthcare system and with individual professionals. These were followed by questions about the patient's perceptions of follow-up needs, for example, “Why do you attend aftercare appointments and what do you want to discuss?” Additionally, to facilitate comparison of the situation before and after treatment, we explored earlier experiences of daily life with an HCV infection, social support needs and the impact of stigma.
According to the participants’ preferences, seven interviews took place at the medical centre, three at a coffee shop and two at the interviewees’ residences. The interviews were audio-recorded and lasted 34–78 minutes (mean: 54 minutes). Data were transcribed verbatim and pseudonymised. Field notes were taken by the interviewer, allowing thoughts and observations to be transformed into systematically usable data [28]
After their interviews, participants completed a structured questionnaire to give socio-demographic (age, gender, education) and clinical data (years of living with a chronic HCV infection, former treatment experiences, treatment completion date, whether they were in medical follow-up and the reason(s) why/why not).
Data analysis
Data analysis followed the six phases of Braun and Clarke's reflexive thematic analysis approach [26]. It started after the third interview and was then conducted in parallel with ongoing data collection [28]. A group of experienced qualitative researchers and clinicians specialised in infectious diseases supported the data analysis. Further, one patient representative signed a confidentiality agreement and acted as a co-researcher [31].
Reflexive thematic analysis works in six phases allowing an iterative and recursive process (Braun & Clarke 2019). An overview of the six phases is shown in table 1. The process of data analysis was supported by MAXQDA software (MaxQDA Plus 2020) for qualitative data analyses. To systematically review the methodological approach and outcome, we worked with Braun and Clarke's 13-item "Evaluating and Reviewing TA Research" checklist and the COREQ Guidelines [32].
Table 1Phases of reflexive thematic analysis.
|
Phase
|
Description of the process
|
| 1 Familiarisation |
The analysis started with data familiarisation. Two researchers (HG/PKH) carefully read each transcript several times, discussed their initial thoughts and summarised each interview in a visual mind map. |
| 2 Generating codes |
The first author (HG) systematically coded the dataset and regularly met with two senior researchers (DN/PKH). The coded data were examined to understand how different codes might be combinable to identify patterns of broader meaning (e.g., potential themes). |
| 3 Constructing themes |
The process of developing initial themes by using the codes was conducted by the smaller research team (HG/DN/PKH). |
| 4 Revising themes |
All themes were continuously reviewed and further developed regarding a) each individual's data set and b) the overall data set (regarding commonalities and differences within themes). |
| 5 Defining themes |
The entire research group discussed the themes (HG/DN/AK/PB/PKH). The resulting feedback led to the refinement of the themes into a final pattern, thereby answering the corresponding research question. |
| 6 Producing the report |
Finally, three researchers (HG/DN/PKH) wrote the study report, which was critically reviewed by all co-authors. |
Results
Twelve patients shared their experiences of being cured via direct-acting antivirals treatment and their perspective regarding follow-up care needs. At the time of the interview, eleven of the twelve participants had achieved SVR24. For six of the twelve, follow-up was recommended according to the current guidelines. See the characteristics of participants in table 2.
Table 2Characteristics of participants.
|
Characteristics
|
n = 12
|
| Age, median (IQR) |
55.5 (45.5–59) |
| Female gender, n (%) |
7 (58) |
| HCV duration, median (IQR) |
17 (15–24) |
| Experienced with interferon-therapy, n (%) |
1 (8) |
| With indication for follow-up, n (%) |
6 (50) |
| – HCC surveillance because Metavir F3/ F4 |
2 (16.6) |
| – Liver cirrhosis and diagnosed HCC |
2 (16.6) |
| – Behavioural risk of reinfection |
2 (16.6) |
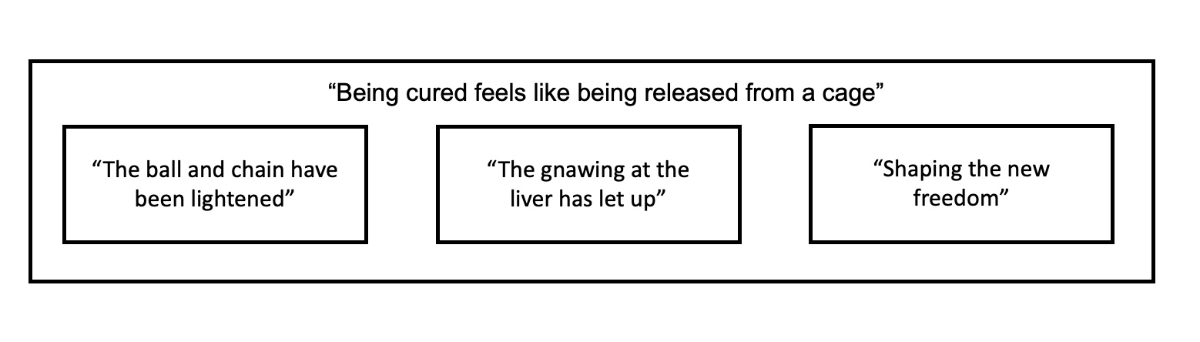
These patients’ shared cure experience is encompassed by the overarching theme, “Being cured feels like being released from a cage.” This experience is further characterised by three sub-themes: “The ball and chain have been lightened” and “the gnawing at the liver has let up“ illustrating the psychosocial and physical changes that patients experienced. “Shaping the new freedom” describes the needed adaptation of self-management and explains many of patients' follow-up care needs (fig. 1).
Figure 1 Overarching theme and sub-themes. The constitutive theme “Being cured feels like being released from a cage” described by recounting experiences of three sub-themes: “the ball and chain have been lightened”; “the gnawing at the liver has let up”; and “shaping the new freedom”.
“Being cured feels like being released from a cage”
The participants described their post-cure experiences as positive and liberating. One man described this evocatively:
It’s probably as though someone was released after he had been kept in a cage for 20 years. (A01)
This cage metaphor was used in several ways and represents how the participants remembered their early impressions of the changes they experienced. Before being cured, life with chronic HCV was restrictive and sometimes stressful. Afterward, the change in their situation seemed like being released from confinement.
Whereas this overarching theme was central to all participants, the two subtheme — “the ball and chain have been lightened” and “the gnawing at the liver has let up” — were more dominant in some individual narratives. Depending on the problems experienced before, participants' stories were more focused either on psychological or physiological changes. However, the third sub-theme factored in all the participants' stories. In “Shaping the new freedom,” participants explained that being cured prompted them to reflect on their lives, goals and behaviours and challenged them to think about further adjustments.
“The ball and chain have been lightened”
The participants experienced their years of hepatitis C infection as a period of great emotional stress. On the one hand, they had feared infecting others with the virus; on the other, they had either feared or concretely experienced stigmatisation because of the disease. One participant described the emotional burden of the hepatitis C infection vividly as “being incumbered” and, using language that is analogous to the cage metaphor, expressed the loss of freedom:
It’s a relief and even new freedom to not have to talk about hepatitis C anymore. It was like being incumbered, and the ball and chain have been lightened. (I09)
A great emotional burden—one which many participants carried for years—was their concern about transmitting the virus to others. Prior to their cure, this concern was omnipresent; the participants had developed strategies to protect others. Caution surrounding blood was especially important to them. For example, if injured they avoided help from other people, and they kept their toothbrushes separate so no mix-ups could occur. Afterward, this burden and fear no longer existed; they felt relieved. One woman experienced this as follows:
I told the children, be careful when mom is bleeding […] It’s really always at the back of your mind, you’re not really free and now it’s been more than a year since I was cured and I can forget about it. (L12)
Whereas the continual worry about infecting others decreased over time for all participants, the fear of future stigmatisation was an emotional burden that appeared to decrease but which they could not leave completely behind. Some of those questioned said that, even after being cured, they did not like to talk about hepatitis C and still feared being stigmatised. For one woman, this fear appeared to become real. After her physician suffered a needle stick injury while treating her, she experienced what she considered stigma:
Then she (the doctor) noticed that I had antibodies and she reacted with panic and asked “Why didn’t you tell me?“ I said, “I don’t have hepatitis C anymore, the antibodies are there for life.” […] I wasn’t required to say anything because I don’t have hepatitis C anymore. […] The prejudice is still there, even though you really only have antibodies.” (I09)
This situation made it clear to her that she would be vulnerable to such situations for the rest of her life. Still, despite this tension, the participant was happy that she could receive support from her treatment team. One other participant was so impressed by the success that he wanted to tell the people about his former HCV infection and cure. Because he was afraid of being reproached for having contracted the disease in the first place, he kept quiet about it. Unlike this patient, many other participants completely lost all desire to talk about hepatitis C.
“The gnawing at the liver has let up”
The hepatitis C infection cause many participants physical discomfort. For example, some reported that they always felt tired and exhausted during their HCV infection and/or their liver had become sensitive and sometimes painful. One participant described these often diffuse complaints vividly as a constant “gnawing at the liver.” Complementing the cage metaphor, this evokes another aspect of life in captivity.
“Yeah, the liver is simply the battery and energy centre […] so I wasn’t really seriously ill […] but the virus had always just gnawed a little.” (B02)
While affected by the virus, many participants had had to cut back in various situations because of exhaustion. One man spoke of a “red light” that warned him to be careful. Others had actively reduced their social activities, such as meeting friends, or their occupational tasks, for example taking on fewer assignments. Even during their direct-acting antiviral therapy, they suddenly felt much more energetic and no longer saw the “red light.” As they gathered new vitality, everyday life improved for many of them. Still, even coping with the regained vitality could be overwhelming. One man reported his initial difficulty with this:
Sometimes I feel too well […] I was always sort of at a slower speed and now it’s more … sometimes I can’t bear it. At the beginning, when I felt too well, I had to consume something [drugs] that pulled me back down. (C03)
Another change for some participants was the relief from food intolerances related to hepatitis C. During their years of chronic infection, for example, some felt liver pains or a kind of “twinge” after consuming alcohol or high-fat foods. These participants reduced their alcohol consumption or avoided rich foods. After the cure, these symptoms abated, as this man described:
It was extreme, when I drank a glass of alcohol, for example, it didn’t agree with me. I simply felt sick and this is not at all the case since the cure. (B02)
“Shaping the new freedom”
Many of the participants felt unprepared for the changes accompanying their cure. They needed time to become accustomed to their new situation and to learn to experience relief. One woman reported:
It’s like a process of letting go. I really always took care that nothing would happen in my environment and that’s sort of stayed the same […] Yeah, it’s like not yet clear, what I no longer have, or because it lasted so many years. (E05)
Our participants also generally needed time to reconsider their previous methods of coping with HCV infection. In this respect, some who no longer needed follow-up described a lack of orientation concerning “liver health” without access to regular medical controls. In addition, they had to face the question of which health-relevant behaviours they should maintain or if they should make new behaviour changes. Returning to the cage metaphor, after a long captivity the entire concept of freedom had to be shaped anew.
Before therapy, all participants were receiving regular medical care. Having experienced several years of direct exchanges with healthcare professionals, they considered themselves well-informed about their health status. For example, they understood that their liver values and sonographic results were related to their physical symptoms. After being cured, some underwent medical follow-up care. In accordance with Swiss guidelines, this included regular controls of liver values and/or sonographs. This subgroup considered ongoing monitoring very important, both because it kept them informed about the health of their liver and because it ensured regular contact with professionals. As one participant said,
I like having this follow-up. Then I can talk a little with experts and know how my liver looks. The virus is gone, but you can still destroy the liver, for example with alcohol. (J10)
Those no longer undergoing follow-up care also expressed a desire to know the condition of their liver. One woman expressed her desire for additional regular controls as follows:
My liver was infected for 20 years. What is going on with it now? […] I don’t know whether my liver will recover so that the necrosis goes away, that’s one thing I don’t know, for example. I don’t know whether blood tests are enough. I miss that a little. (I09)
While the interviewees were living with viremia, many adapted their lifestyles to protect their liver from further damage. In addition to those who had stopped drinking alcohol because of intolerances (“The gnawing at the liver has let up”), some had lessened their drinking for health and well-being and some participants without intolerances even stopped all together. After being cured, these participants asked themselves whether the behaviours they had changed were still relevant. Several who had been concerned about alcohol consumption felt released from earlier limitations and particularly from their ambivalence. Others decided to maintain their adjusted behaviours to be more attentive to their health. Their liver-related worries concerning their decisions to abstain from alcohol or certain medications still remained. As one woman related,
Actually I still look, you know, worry a little about the liver, you know. […] I was the one who thought twice, should I take this medication or not […] that hasn‘t changed. (L12)
In addition to protecting their livers, participants showed increasing overall interest in general health behaviour. Many reported being motivated to make longer-term plans, e.g., quitting smoking, losing weight, or engaging in more exercise. One woman even mentioned that her chronic hepatitis C infection had increased her awareness of health and that this remained in force:
I think my whole awareness of health over the past 20 years has profited me, so that I now can say I had to change because of the diagnosis. […] Nevertheless, in that moment when I knew (hepatitis C) was there, I tried to avoid everything that could cause more damage and the awareness of health like has continued until now. That is, I don’t have the feeling at the moment, “Yippee, everything is ok and I can do everything”: it’s stayed the same. (E05)
Additionally, patients with former or current drug use, felt intense gratitude for the opportunity to undergo such expensive therapy. They described the cure as a chance for a new beginning. For those who were still consuming drugs, their HCV-free status motivated them to take reliable protective measures against reinfection. For example, one interviewee said that he only used his own tubes for intranasal drug consumption.
Knowing the risks of such practices, others considered quitting drug use altogether. However, quitting a long-term drug habit is not a simple task. One man who recognised the challenge it presented said he would have liked more support from health experts.
Discussion
These qualitative findings reflect the experiences of patients in Switzerland who were cured of chronic hepatitis C infection of 10 years or more. The study also explores the follow-up needs of patients. Participants described their HCV-free situation as “like being released from a cage.” This overarching theme describes the powerful emotions HCV patients experience on being cured from a chronic disease that had impeded their well-being and daily activities for many years. Participants reported decreases in physical symptoms (“the gnawing at the liver has let up”) and reductions in their psychosocial burdens (“the ball and chain have been lightened”), particularly due to the relief they felt that they could no longer transmit the virus. Although reduced, the fear of stigma was clearly an ongoing psychosocial burden. With cure as a starting point, participants needed to “shape the new freedom.” For some, this seemed easy, for others challenging.
Participants felt mostly liberated after being cured, reflecting the overarching theme that being cured “feels like being released from a cage.” This attitude is also illustrated in two sub-themes: "the ball and chain have been lightened" and "the gnawing at the liver has let up", which were used to describe patients’ experiences of decreased psychosocial burden and elimination of physical symptoms. This finding supports those of other qualitative studies whose participants experienced cure as a mainly positive and liberating feeling, especially the decreased physical symptoms and increased energy for daily activities [16–19]. Most also highlighted their reduced emotional burden [20–23].
However, in contrast with former research, stigma remained an important topic for some participants. HCV-related stigma is well researched, especially regarding transmission, disclosure, health care settings, interpersonal relationships and work environments [15]. Our study also showed that residual stigma was particularly common regarding disclosure to and in contact with health care providers. Post-cure, one might reasonably expect that some stigmatisation factors, e.g., the risk of transmitting HCV, would no longer be relevant; still, as our data show, some experienced stigma even after being cured.
On the patient level, stigma experiences or fears should be addressed in medical consultations following the direct-acting antiviral treatment phase. Additionally, discussing fears with peers who have had similar experiences can help reduce them [33].
On the health care provider level, those providing treatment should inform both the patients and their general practitioners that, while future antibody tests will always be positive, this is no reason for concern. To prevent healthcare-associated stigma, this advice was also included in the new recommendations for follow-up care in Switzerland [34].
Further, as noted regarding the theme of “Shaping the new freedom,” our results indicate a need for patients’ self-management to be adapted post-cure. The absence of noticeable symptoms and the cessation of regular medical check-ups, which formerly provided them with health-relevant feedback, triggered uncertainty in our participants.
This reaction might be explained by these patients’ long disease duration: for over 10 years, they had learned to live with chronic HCV infection. Their narratives included mentions of specific elements of self-management, a concept widely promoted in chronic illness care [35] and described in a qualitative literature review as a vital topic for people living with chronic HCV [36]. The cure naturally disrupted patients’ self-management behaviours.
They expressed mixed feelings about recovery. Our participants demonstrated similar confusion and needs as presented by cancer survivors who were initially uncertain regarding the reduction of medical controls, leading to new needs, specifically for clear information about their next steps and health promotion activities [37]. Having learned over many years to assess quantitative values (blood values, ultrasound results), they had developed competencies in spotting and interpreting warning signs of advanced liver disease. For those with no indicated need for follow-up, their focus suddenly shifted from receiving regular, precise medical feedback to having no need for such data and to manage their new situation on their own.
To support those patients’ transition to independent self-management, one might consider two steps: firstly, prepare them for this situation during direct-acting antiviral therapy; secondly, to smooth the transition of patients who show higher uncertainty levels by briefly continuing to offer a small number of controls. These would not necessarily have to be carried out by doctors, but could be delegated, for example, to specialised nurses. This approach is also proposed for cancer survivorship models of care [25].
Another aspect of self-management adaptation was to help participants realize their desire to implement a healthier lifestyle. Many spoke of feeling motivated to quit smoking, reduce alcohol consumption, lose weight, or become more active. This suggests a window of opportunity regarding changes in key health behaviours. However, as many have trouble managing such changes alone, post-cure health promotion interventions and coaching should be implemented. Internationally, brief motivational interventions provided by health care workers have proved effective in improving patients health behaviours [38]. Our study patients had already demonstrated one indispensable requirement for behavioural modification: willingness to change [39].
In Switzerland, a “health coaching program” applicable to a range of health behaviours has been developed to support behavioural counselling by general practitioners [40, 41]. Given the importance of health behaviours in chronic disease management and this post-cure window of opportunity in HCV patients, HCPs could use follow-up meetings to coach patients in this direction. Again, interventions for health promotion are not restricted to physicians: they can be delegated to other HCPs or peers with advanced communication skills, e.g., motivational interviewing techniques and expertise in behavioural change interventions.
This study faces certain limitations, especially regarding data sampling. First, the results apply primarily to a patient group who had known about their HCV infection for at least ten years. Second, as our inclusion criteria included SVR24 status, it remains an open question whether similar needs will exist in patients with short-term HCV experience before receiving direct-acting antivirals treatment and third, the small sample size does not allow any generalisation of the results. Nevertheless, through purposive sampling, we achieve a reasonably diverse study group. This enabled us to identify noteworthy differences and similarities in their experiences. One vital strength of this research was the inclusion of a patient representative, who enabled the development of our interview guide and gave important feedback on the preliminary results as a first quality check. Further, to ensure high quality in our methodological approach, we used Braun and Clarke's 13-item TA checklist of [32].
In summary, our findings identify specific additional patient follow-up care needs, especially regarding dealing with stigma, regaining health-related confidence after being cured, and using patients’ openness post-cure as a window for behavioural change to improve their health-related lifestyle.
Conclusion
Being cured of chronic HCV infection is a tremendous experience for participants, however, certain needs do remain and new ones also arise for patients post-cure. The results use the patients’ perspectives to define implications for their follow-up care. Patients would likely benefit from early preparation for their post-cure period, especially addressing their fear of ongoing stigma and concerns about the discontinuation of previously familiar medical controls. Health care providers can explore these needs early and plan ahead. For some patients, access to low-threshold services such as specialised nurses can be beneficial. Post-cure openness to self-management and a healthier lifestyle indicates a window of opportunity. HCPs should integrate patient coaching for health-behavioural change into their follow-up. Well-established evidence-based counselling tools are available to design such coaching sessions. We recommend further research on individually planned follow-up care interventions, for example a personalised plan to promote healthy lifestyle behaviours. Further study is also recommended for exploring the experiences of people who have lived less than 10 years with HCV.
Availability of data and materials
The study protocol was not published. The individual level datasets generated during and/or analysed during the current study are not publicly available as the data are too dense and comprehensive to preserve patient privacy but are available from the corresponding author on reasonable request.
Acknowledgments
We would like to thank all the participants of this study, Joanne Eysell for the translation of results and Chris Shultis for editing the manuscript.
Patrizia Künzler-Heule, PhD, RN
Nursing Science, University of Basel
Medical Faculty, Department Public Health
Bernoullistrasse 28
CH-4056 Basel
patrizia.kuenzler-heule[at]unibas.ch
References
1.
World Health Organization (WHO)
. Hepatitis C 2021 [cited 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/hepatitis-c
2.
Stanaway JD
,
Flaxman AD
,
Naghavi M
,
Fitzmaurice C
,
Vos T
,
Abubakar I
, et al.
The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013. Lancet. 2016 Sep;388(10049):1081–8. https://doi.org/10.1016/S0140-6736(16)30579-7
3.
Bihl F
,
Bruggmann P
,
Castro Batänjer E
,
Dufour J-F
,
Lavanchy D
,
Müllhaupt B
, et al.
HCV disease burden and population segments in Switzerland. Liver International. 2021;n/a(n/a).
4.
Roelens M
,
Bertisch B
,
Moradpour D
,
Cerny A
,
Semmo N
,
Schmid P
, et al.
All-Cause Mortality and Causes of Death in the Swiss Hepatitis C Cohort Study (SCCS). Open Forum Infect Dis. 2020;7(8):ofaa308-ofaa.
5.
Pawlotsky JM
,
Negro F
,
Aghemo A
,
Berenguer M
,
Dalgard O
,
Dusheiko G
, et al.; European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu; Clinical Practice Guidelines Panel: Chair; EASL Governing Board representative; Panel members
. EASL recommendations on treatment of hepatitis C: final update of the series☆
. J Hepatol. 2020 Nov;73(5):1170–218. https://doi.org/10.1016/j.jhep.2020.08.018
6.
Carrat F
,
Fontaine H
,
Dorival C
,
Simony M
,
Diallo A
,
Hezode C
, et al.; French ANRS CO22 Hepather cohort
. Clinical outcomes in patients with chronic hepatitis C after direct-acting antiviral treatment: a prospective cohort study. Lancet. 2019 Apr;393(10179):1453–64. https://doi.org/10.1016/S0140-6736(18)32111-1
7.
Bruggmann P
,
Hepatitis C
. Eine Erfolgsgeschichte. Primary and Hospital Care: Allgemeine Innere Medizin. 2018;16:282–5.
8.
Moradpour D
,
Müllhaupt B
. [Hepatitis C: current therapy]. Rev Med Suisse. 2015 Apr;11(471):902–6.
9.
Conrad S
,
Garrett LE
,
Cooksley WG
,
Dunne MP
,
MacDonald GA
. Living with chronic hepatitis C means ‘you just haven’t got a normal life any more’. Chronic Illn. 2006 Jun;2(2):121–31.
10.
Glacken M
,
Coates V
,
Kernohan G
,
Hegarty J
. The experience of fatigue for people living with hepatitis C. J Clin Nurs. 2003 Mar;12(2):244–52. https://doi.org/10.1046/j.1365-2702.2003.00709.x
11.
Glacken M
,
Kernohan G
,
Coates V
. Diagnosed with Hepatitis C: a descriptive exploratory study. Int J Nurs Stud. 2001 Feb;38(1):107–16. https://doi.org/10.1016/S0020-7489(00)00046-8
12.
Fry M
,
Bates G
. The tasks of self-managing hepatitis C: the significance of disclosure. Psychol Health. 2012;27(4):460–74. https://doi.org/10.1080/08870446.2011.592982
13.
Janke EA
,
McGraw S
,
Garcia-Tsao G
,
Fraenkel L
. Psychosocial issues in hepatitis C: a qualitative analysis. Psychosomatics. 2008 Nov-Dec;49(6):494–501. https://doi.org/10.1176/appi.psy.49.6.494
14.
Butt G
,
Paterson BL
,
McGuinness LK
. Living with the stigma of hepatitis C. West J Nurs Res. 2008 Mar;30(2):204–21. https://doi.org/10.1177/0193945907302771
15.
Moore GA
,
Hawley DA
,
Bradley P
. Hepatitis C: experiencing stigma. Gastroenterol Nurs. 2009 Mar-Apr;32(2):94–104. https://doi.org/10.1097/SGA.0b013e31819de48b
16.
Juanbeltz R
,
Martínez-Baz I
,
San Miguel R
,
Goñi-Esarte S
,
Cabasés JM
,
Castilla J
. Impact of successful treatment with direct-acting antiviral agents on health-related quality of life in chronic hepatitis C patients. PLoS One. 2018 Oct;13(10):e0205277. https://doi.org/10.1371/journal.pone.0205277
17.
Evon DM
,
Sarkar S
,
Amador J
,
Lok AS
,
Sterling RK
,
Stewart PW
, et al.
Patient-reported symptoms during and after direct-acting antiviral therapies for chronic hepatitis C: the PROP UP study. J Hepatol. 2019 Sep;71(3):486–97. https://doi.org/10.1016/j.jhep.2019.04.016
18.
Goutzamanis S
,
Spelman T
,
Harney B
,
Dietze P
,
Stoove M
,
Higgs P
, et al.
Patient-reported outcomes of the Treatment and Prevention Study: A real-world community-based trial of direct-acting antivirals for hepatitis C among people who inject drugs. J Viral Hepat. 2021 Jul;28(7):1068–77. https://doi.org/10.1111/jvh.13516
19.
Fagundes RN
, Ferreira LEVVdC, Pace FHdL. Health-related quality of life and fatigue in patients with chronic hepatitis C with therapy with direct-acting antivirals agents interferon-free. PloS one. 2020;15(8):e0237005-e.
20.
Madden A
,
Hopwood M
,
Neale J
,
Treloar C
. Beyond cure: patient reported outcomes of hepatitis C treatment among people who inject drugs in Australia. Harm Reduct J. 2018 Aug;15(1):42. https://doi.org/10.1186/s12954-018-0248-4
21.
Torrens M
,
Soyemi T
,
Bowman D
,
Schatz E
. Beyond clinical outcomes: the social and healthcare system implications of hepatitis C treatment. BMC Infect Dis. 2020 Sep;20(1):702. https://doi.org/10.1186/s12879-020-05426-4
22.
Pourmarzi D
,
Smirnov A
,
Hall L
,
FitzGerald G
,
Rahman T
. ‘I’m over the moon!’: patient-perceived outcomes of hepatitis C treatment. Aust J Prim Health. 2020 Aug;26(4):319–24. https://doi.org/10.1071/PY20013
23.
Richmond JA
,
Ellard J
,
Wallace J
,
Thorpe R
,
Higgs P
,
Hellard M
, et al.
Achieving a hepatitis C cure: a qualitative exploration of the experiences and meanings of achieving a hepatitis C cure using the direct acting antivirals in Australia. Hepatol Med Policy. 2018 Aug;3(1):8. https://doi.org/10.1186/s41124-018-0036-5
24.
Moradpour D
,
Fehr J
,
Semela D
,
Rauch A
,
Müllhaupt B
. Treatment of Chronic Hepatitis C- January 2021 Update Expert Opinition Statement by SASL, SSG and SSI. Swiss Association for the Liver. 2021.
25.
Jacobs LA
,
Shulman LN
. Follow-up care of cancer survivors: challenges and solutions. Lancet Oncol. 2017 Jan;18(1):e19–29. https://doi.org/10.1016/S1470-2045(16)30386-2
26.
Braun V
,
Clarke V
. Reflecting on reflexive thematic analysis. Qual Res Sport Exerc Health. 2019;11(4):589–97. https://doi.org/10.1080/2159676X.2019.1628806
27.
World Medical Association
. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013 Nov;310(20):2191–4. https://doi.org/10.1001/jama.2013.281053
28.
Creswell JW
,
Poth CN
. Qualitative Inquiry and research design: choosing among five approaches Thousand Oaks. Sage. 2017.
29. Swiss Hepatitis Strategy. Swiss Hepatitis Strategy 2014- 2030. 2019.
30.
INVOLVE
. Briefing notes for researchers: public involvement in NHS, public health and social care research 2012 [Available from: http://www.invo.org.uk/wp-content/uploads/2014/11/9938_INVOLVE_Briefing_Notes_WEB.pdf
31.
Shippee ND
,
Domecq Garces JP
,
Prutsky Lopez GJ
,
Wang Z
,
Elraiyah TA
,
Nabhan M
, et al.
Patient and service user engagement in research: a systematic review and synthesized framework. Health Expect. 2015 Oct;18(5):1151–66. https://doi.org/10.1111/hex.12090
32.
Braun V
,
Clarke V
. Evaluating and reviewing TA research: A checklist for editors and reviewers.2017. Available from: https://cdn.auckland.ac.nz/assets/psych/about/our-research/documents/TA%20website%20update%2010.8.17%20review%20checklist.pdf
33.
Stagg HR
,
Surey J
,
Francis M
,
MacLellan J
,
Foster GR
,
Charlett A
, et al.
Improving engagement with healthcare in hepatitis C: a randomised controlled trial of a peer support intervention. BMC Med. 2019 Apr;17(1):71. https://doi.org/10.1186/s12916-019-1300-2
34.
Bobzin C
,
Bsiger C
,
Bruggmann P
,
Cerny A
,
Christinet M
,
Keiser O
, et al.
Empfehlungen für die Nachsorge von Patientinnen/Patienten mit ausgeheilter Hepatitis C. Swiss Medical Forum ‒ Schweizerisches Medizin-Forum. 2021.
35.
Bodenheimer T
,
Lorig K
,
Holman H
,
Grumbach K
. Patient self-management of chronic disease in primary care. JAMA. 2002 Nov;288(19):2469–75. https://doi.org/10.1001/jama.288.19.2469
36.
Künzler-Heule P
,
Panfil EM
. [Hepatitis C! Experience in diagnosis and medical treatment. A literature review]. Pflege. 2012 Jun;25(3):185–95.
37.
Mayer DK
,
Nasso SF
,
Earp JA
. Defining cancer survivors, their needs, and perspectives on survivorship health care in the USA. Lancet Oncol. 2017 Jan;18(1):e11–8. https://doi.org/10.1016/S1470-2045(16)30573-3
38.
Frost H
,
Campbell P
,
Maxwell M
,
O’Carroll RE
,
Dombrowski SU
,
Williams B
, et al.
Effectiveness of Motivational Interviewing on adult behaviour change in health and social care settings: A systematic review of reviews. PLoS One. 2018 Oct;13(10):e0204890. https://doi.org/10.1371/journal.pone.0204890
39.
Zimmerman GL
,
Olsen CG
,
Bosworth MF
. A ‘stages of change’ approach to helping patients change behavior. Am Fam Physician. 2000 Mar;61(5):1409–16.
40.
Neuner-Jehle Stefan
. Schmid M, Ueli G. The „Health Coaching“ programme: a new patient centred and visually supported approach for thealth behaviour change in primary care. BMC Fam Pract. 2013;14(100):1471–2296.
41.
Grüninger U
,
Hösli R
,
Neuner S
,
Schmid M
. Gesdunheitscoaching- ein Programm für Gesundheitsförderung und Prävention in der Hausarztpraxis vom Kollegium für Hausarztmedizin; (KMH). Schweiz Arzteztg. 2009;90(45):1729–32. https://doi.org/10.4414/saez.2009.14736