SARS-CoV-2 aerosol transmission in schools: the effectiveness of different interventions
DOI: https://doi.org/10.4414/SMW.2022.w30178
Jennifer
Villersa*, Andre
Henriquesb*, Serafina
Calarcoc, Markus
Rognliend, Nicolas
Mounetb, James
Devineb, Gabriella
Azzopardib, Philip
Elsonb, Marco
Andreinib, Nicola
Taroccob, Claudia
Vassellae, Olivia
Keiserf
aGlobal Studies Institute, University of Geneva, Switzerland
bEuropean Organization for Nuclear Research (CERN), Geneva, Switzerland
cFoundation for Innovative New Diagnostics (FIND), Geneva, Switzerland
dNorwegian University of Science and Technology (NTNU), Trondheim, Norway
eFederal Office of Public Health, Consumer Protection Directorate, Indoor Pollutants Unit, Berne, Switzerland
fInstitute of Global Health, University of Geneva, Switzerland
*These authors contributed equally
Summary
BACKGROUND: Indoor aerosol transmission of SARS-CoV-2 has been widely recognised, especially in schools where children remain in closed indoor spaces and largely unvaccinated. Measures such as strategic natural ventilation and high efficiency particulate air (HEPA) filtration remain poorly implemented and mask mandates are often progressively lifted as vaccination rollout is enhanced.
METHODS: We adapted a previously developed aerosol transmission model to study the effect of interventions (natural ventilation, face masks, HEPA filtration and their combinations) on the concentration of virus particles in a classroom of 160 m3 containing one infectious individual. The cumulative dose of viruses absorbed by exposed occupants was calculated.
RESULTS: In the absence of interventions, the cumulative dose absorbed was 1.5 times higher in winter than in spring/summer, increasing chances of indoor airborne transmission in winter. However, natural ventilation was more effective in winter, leading to up to a 20-fold decrease in cumulative dose when six windows were fully open at all times. In winter, partly opening two windows all day or fully opening six windows at the end of each class was effective as well (2.7- to 3-fold decrease). In summer, good ventilation levels could be achieved through the opening of windows all day long (2- to 7-fold decrease depending on the number of windows open). Opening windows only during yard and lunch breaks had minimal effect (≤1.5-fold decrease). One HEPA filter was as effective as two windows partly open all day in winter (3-fold decrease) whereas two filters were more effective (5-fold decrease). Surgical face masks were very effective independently of the season (8-fold decrease). Combined interventions (i.e., natural ventilation, masks, and HEPA filtration) were the most effective (≥25-fold decrease) and remained highly effective in the presence of a super-spreader.
INTERPRETATION: Natural ventilation, face masks, and HEPA filtration are effective interventions to reduce SARS-CoV-2 aerosol transmission. These measures should be combined and complemented by additional interventions (e.g., physical distancing, hygiene, testing, contact tracing and vaccination) to maximise benefit.
Introduction
Although children of all ages can be infected by and transmit SARS-CoV-2 [1], it was initially thought that children did not play a major role in the transmission of the virus because they generally developed less severe symptoms and were more often asymptomatic than adults [2]. However, many studies have described outbreaks in school settings [3–7], demonstrating that schools can contribute to the community spread of COVID-19. This has become more evident with the delta and omicron variants, which spread the fastest among children and young adults (<25 years old), partly due to low vaccination rates and to the lack of mitigation measures in educational establishments [8–10].
A major issue is the high risk of transmission of SARS-CoV-2 by airborne particles. This refers to the dispersion of the virus in small, invisible droplet nuclei that are generated when an infectious person exhales, talks, shouts, coughs, sneezes or sings [11]. These airborne particles have the highest viral concentration in close proximity to an infected person although they can accumulate over time in poorly ventilated indoor spaces, floating in the air for minutes to hours. If another person inhales them, the virus can deposit on the surfaces of the respiratory tract and initiate infection of that person [12], making indoor spaces especially dangerous as infection can occur indirectly and over long distances.
Schools appear to be favourable places for SARS-CoV-2 transmission since children spend most of the day in a crowded and poorly ventilated space [13]. Therefore, it is necessary to implement measures that can reduce the risk of long-range airborne transmission. Such measures include reducing crowding and time spent indoors, natural ventilation, the use of face masks and the use of portable high-efficiency particulate air (HEPA) filtration systems [11, 14, 15]. This type of air filter can remove at least 99.97% of dust, pollen, mould, bacteria, viruses and any airborne particles with a size of, approximately, 0.3 microns (µm).
Physical distancing and disinfection have been recommended since the beginning of the pandemic, but recommendations specifically aimed at decreasing the concentration of viral particles in the air were released by the World Health Organization (WHO) only on 1 March 2021 [16]. It took many more months for governments and health authorities to produce guidelines on how to keep indoor spaces safe and these guidelines varied widely from one country to another. As an example, the US Centers for Disease Prevention and Control (CDC) currently recommends that all children and school personnel wear a face mask [17], whereas the UK have recently lifted mask mandates for pupils and teachers alike [18]. In Switzerland, it is the responsibility of the cantons to decide what measures to introduce in compulsory schools [19].
The objective of this paper was to assess the effectiveness of different interventions aimed at improving ventilation and reducing the risk of SARS-CoV-2 airborne transmission in a typical classroom setting using the COVID Airborne Risk Assessment (CARA) tool developed at the European Organization for Nuclear Research (CERN) by Henriques et al. [20] and to provide recommendations for decision makers that can improve schools’ safety.
Methods
We used the COVID Airborne Risk Assessment (CARA) tool [20] to assess the impact of different interventions on the concentration of virus particles (i.e., virions) in a classroom of 160 m3 containing one infectious occupant with COVID-19. CARA uses a physical model developed to simulate the concentration of virus particles in an enclosed indoor volume. Based on this, the cumulative dose of virions absorbed by exposed occupants is calculated, which could be used to predict the probability of on-site transmission. The interventions modelled include different levels of natural ventilation, the universal use of surgical face masks, high efficiency particulate air (HEPA) filtration, as well as different combinations of these (see table 1). Each intervention was compared with a baseline scenario in which all windows are closed, no one is wearing a mask and no filters have been installed.
This study focused on the "long-range" airborne transmission route that assumes a well-mixed box model with a homogeneous viral concentration in the room. The model follows a probabilistic approach to deal with uncertainties of variables such as viral load of infected occupant(s) or breathing rate [20]. For each intervention, 200,000 Monte Carlo simulations were performed. For each simulation, the viral load, breathing rate, and emission concentration were randomly sampled from distributions (see supplementary fig. S1 in the appendix).
CARA has four main modules outlined below and described in detail elsewhere [20]:
- The emission rate of viruses from the infected person’s mouth or nose (virions h
- The dynamic concentration of viral particles in the air over the exposure time (virions m
- The cumulative absorbed dose of virus particles inhaled by an exposed host (virions). The dose was calculated by integrating the concentration profile over the total exposure time (in a stepwise function) and the effect of other parameters such as the physical activity of the occupants, the efficiency of masks of the exposed persons and an aerosol deposition factor in the respiratory tract.
- The probability of on-site transmission, i.e., the probability that one susceptible exposed person gets infected, based on the absorbed dose. At the time of writing, the dose-response relationship for persons exposed to aerosolised SARS-CoV-2 viruses was not known to the authors. A few studies with other coronaviruses suggest an exponential response [25], meaning that a slight reduction in the inhaled dose would relate to an exponential reduction in the probability of contracting the disease, independently of the infective dose for SARS-COV-2. Preliminary experimental studies on SARS-CoV-2 suggest an infection dose between 10 and 1000 infectious virions [26]. However, owing to the high variability in infectious dose between SARS-CoV-2 variants, we only compared the effectiveness of different indoor preventive measures on the cumulative dose absorbed.
For natural ventilation, we considered the single-sided opening of one, two or six windows (of 0.96 m2 each) all day long, during lunch and yard breaks, or for ten minutes at the end of each class (in addition to breaks). Six windows correspond to an openable window area of 5.76 m2 (the average measured in Switzerland [27]). The opening width of the windows was set to 60 cm (fully open) or 20 cm (slightly open). School days were divided into eight periods of 45 minutes with a 60-minute lunch break in the middle of the day and two 30-minute yard breaks (one in the morning and one in the afternoon). The occupants of the classroom were assumed to remain the same throughout the day and to leave the class during lunch and yard breaks. Since natural ventilation is influenced by the difference between indoor and outdoor temperatures, we simulated two different seasons: spring/summer — with an outdoor temperature of 18°C — and winter — with an outdoor temperature of 5°C. In both scenarios, the indoor temperature was set constant at 22°C. Since the decay rate of aerosolised viral particles is influenced by relative humidity, we set relative humidity to 50% in spring/summer and to 30% in winter (table S1).
For air filtration, we considered the use of one or two HEPA filtration devices, each delivering a flow rate up to 400 m3h-1 of clean air, also known as CADR (calculated based on a particle removal objective of at least 80% in 20 minutes that would yield an exchange rate of 2.5 air changes per hour, ACH). We assumed that the devices were strategically positioned in the room to ensure a homogeneous filtering of the entire volume at occupant height (i.e., 1 to 1.8 m from the floor). In a typical square-like classroom, this would correspond to the center of the room.
For each intervention presented in table 1, we plotted the mean viral concentration and mean cumulative dose (figs 1–3) as well as the full range of cumulative doses (fig. S2). The values for the mean cumulative doses as well as 5th and 95th percentiles are presented in table 1. We also generated heatmaps comparing the effectiveness of different interventions based on the cumulative dose (figs 1a-b and 2a-b).
Ethical approval
This research did not involve human or animal subjects, and ethical approval was therefore not required.
Results
When looking at the full range of simulations for the cumulative dose absorbed by a susceptible person (supplementary fig. S2 in the appendix), we observed that it spanned several orders of magnitude (e.g., from 0.0005 to over 2,500 virions in the spring/summer baseline scenario). This outcome was not surprising considering the wide distribution of viral loads in the infected host population (ranging from 100 to 10 billion virions ml-1, fig. S1b). For a given viral load, breathing rate and expiratory activity of the infectious individual, we can expect the cumulative dose of virions absorbed by an exposed individual to be influenced only by the mitigation measures put in place. Therefore, to compare the effectiveness of different interventions, we decided to look at the mean cumulative dose of virions and at their relative difference, which was conserved throughout the simulations (fig. S2 and table 1).
Table 1List of interventions.
|
Type of intervention
|
Natural ventilation
|
HEPA filters
|
Surgical masks
|
Mean cumulative dose
(5th; 95th percentiles)
|
|
In summer
|
| Baseline |
No |
No |
No |
167 (0.002; 869) |
| Natural ventilation |
1 window fully open during breaks |
No |
No |
146 (0.0018; 760) |
| 1 window fully open at all times |
No |
No |
83 (0.0010; 435) |
| 2 windows fully open during breaks |
No |
No |
140 (0.0017; 731) |
| 2 windows fully open at all times |
No |
No |
55 (0.0007; 287) |
| 6 windows fully open during breaks |
No |
No |
138 (0.0017; 722) |
| 6 windows fully open at all times |
No |
No |
23 (0.0003; 123) |
| 6 windows fully open after every class |
No |
No |
91 (0.0011; 477) |
| HEPA filters |
No |
2.5 ACH/400 m3h-1 CADR |
No |
68 (0.0008; 354) |
| No |
5 ACH/800 m3h-1 CADR |
No |
43 (0.0005; 226) |
| Face masks |
No |
No |
Yes |
21 (0.0003; 110) |
| Combined interventions |
No |
2.5 ACH/400 m3h-1 CADR |
Yes |
9 (0.00011; 49) |
| No |
5 ACH/800 m3h-1 CADR |
Yes |
6 (0.00007; 31) |
|
In winter
|
| Baseline |
No |
No |
No |
245 (0.003; 1293) |
|
1 window fully open during breaks |
No |
No |
173 (0.002; 913) |
| 1 window partly open at all times |
No |
No |
121 (0.0015; 638) |
| 1 window fully open at all times |
No |
No |
58 (0.0007; 305) |
| 2 windows fully open during breaks |
No |
No |
166 (0.002; 877) |
| 2 windows partly open at all times |
No |
No |
78 (0.001; 410) |
| 2 windows fully open at all times |
No |
No |
33 (0.0004; 173) |
| 6 windows fully open during breaks |
No |
No |
166 (0.002; 873) |
| 6 windows partly open at all times |
No |
No |
33 (0.0004; 173) |
| 6 windows fully open at all times |
No |
No |
12 (0.00015; 63) |
| 6 windows fully open after every class |
No |
No |
90 (0.0011; 474) |
| HEPA filters |
No |
2.5 ACH/400 m3h-1 CADR |
No |
76 (0.0009; 399) |
| No |
5 ACH/800 m3h-1 CADR |
No |
46 (0.0006; 244) |
| Face masks |
No |
No |
Yes |
31 (0.0004; 165) |
| Combined interventions |
No |
2.5 ACH/400 m3h-1 CADR |
Yes |
10 (0.00013; 54) |
| No |
5 ACH/800 m3h-1 CADR |
Yes |
6 (0.00008; 32) |
| 2 windows partly open at all times |
No |
Yes |
10 (0.00012; 52) |
| 2 windows partly open at all times |
2.5 ACH/400 m3h-1 CADR |
Yes |
6 (0.00007; 32) |
| 2 windows partly open at all times |
5 ACH/800 m3h-1 CADR |
Yes |
4 (0.00005; 23) |
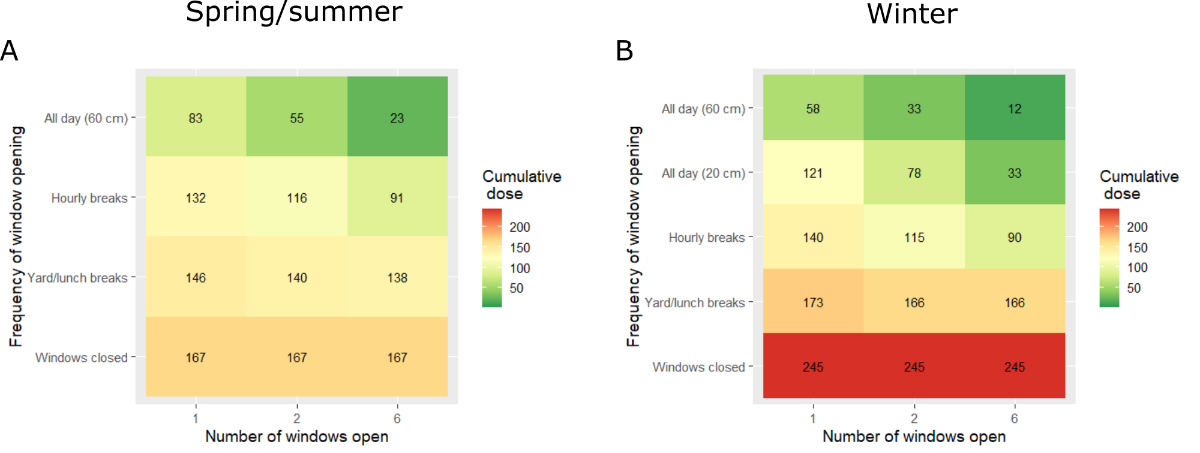
We observed a large difference (1.5-fold) in cumulative dose absorbed between the two baseline scenarios, with a mean cumulative dose of 245 virions in winter and of 167 virions in summer. The effectiveness of natural ventilation was dependent on the number of windows open, the duration and frequency of these openings, and the difference between indoor and outdoor temperature (fig. 1).
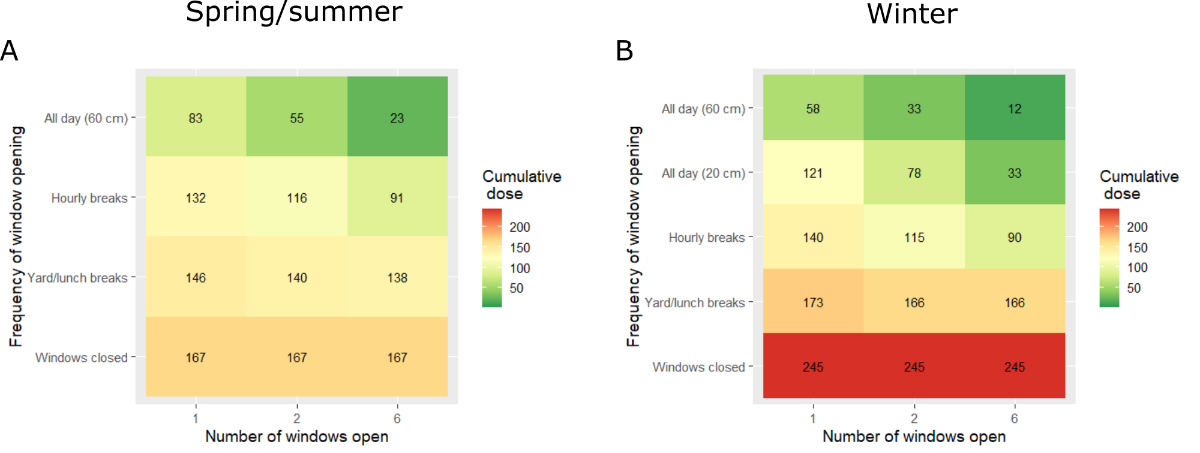
Figure 1 a, b Natural ventilation. (a, b) Heatmaps of the relative effectiveness of natural ventilation strategies. Cumulative doses absorbed are displayed as colours ranging from red to green as shown in the key. (a) Spring/summer simulations. (b) Winter simulations.

Figure 1 c-j (c–j) Estimated mean viral concentration profiles over the exposure time (solid lines, left y-axis) and consequent estimated mean cumulative dose of virions absorbed by the exposed hosts (dotted lines, right y-axis). The red lines show the results for the baseline scenario, the blue and green lines show the results for different natural ventilation scenarios. (c–h) Light blue: windows are fully open during yard and lunch breaks only. Green: windows are fully open (60 cm) all day. Dark blue: windows are partly open (20 cm) all day. (c, d) Results with one window. (c) Spring/summer simulations. (d) Winter simulations. (e, f) Results with two windows. (e) Spring/summer simulations. (f) Winter simulations. (g, h) Results with six windows. (g) Spring/summer simulations. (h) Winter simulations. (i, j) Results with six windows opened for 10 minutes at the end of each class in addition to yard and lunch breaks. (i) Spring/summer simulations. (j) Winter simulations.
Opening windows during yard and lunch breaks had only a minimal effect on the cumulative dose of virions absorbed, with decreases in cumulative dose ranging from 1.1-fold to 1.5-fold depending on the season and number of windows open. Importantly, although the effect was stronger in winter (1.5-fold), it only decreased the cumulative dose to values that are similar to the baseline values in spring/summer (166 virions). In contrast, opening one, two or six windows all day long during spring/summer decreased the cumulative dose absorbed 2-fold, 3-fold and 7-fold, respectively, compared with the baseline scenario (leading to mean cumulative doses of 83, 55 and 23 virions, respectively). Keeping windows open all day was most effective in winter, with a 4-fold decrease in the cumulative dose absorbed when one window was fully open (58 virions), a 7.5-fold decrease when two windows were fully open (33 virions) and a 20-fold decrease when six windows were fully open (12 virions). Since leaving windows wide open during the heating season is unacceptable (waste of heating energy and thermal discomfort), we tested a 20-cm opening all day long, leading to a 2-fold decrease in the cumulative dose when one window was open (121 virions), a 3-fold decrease when two windows were open (78 virions) and a 7.5-fold decrease when six windows were open (33 virions). We also tested the opening of six windows at the end of each class (referred to as “hourly breaks”), leading to 1.8-fold (spring/summer) and 2.7-fold (winter) decreases in cumulative dose (down to around 90 virions in both cases).
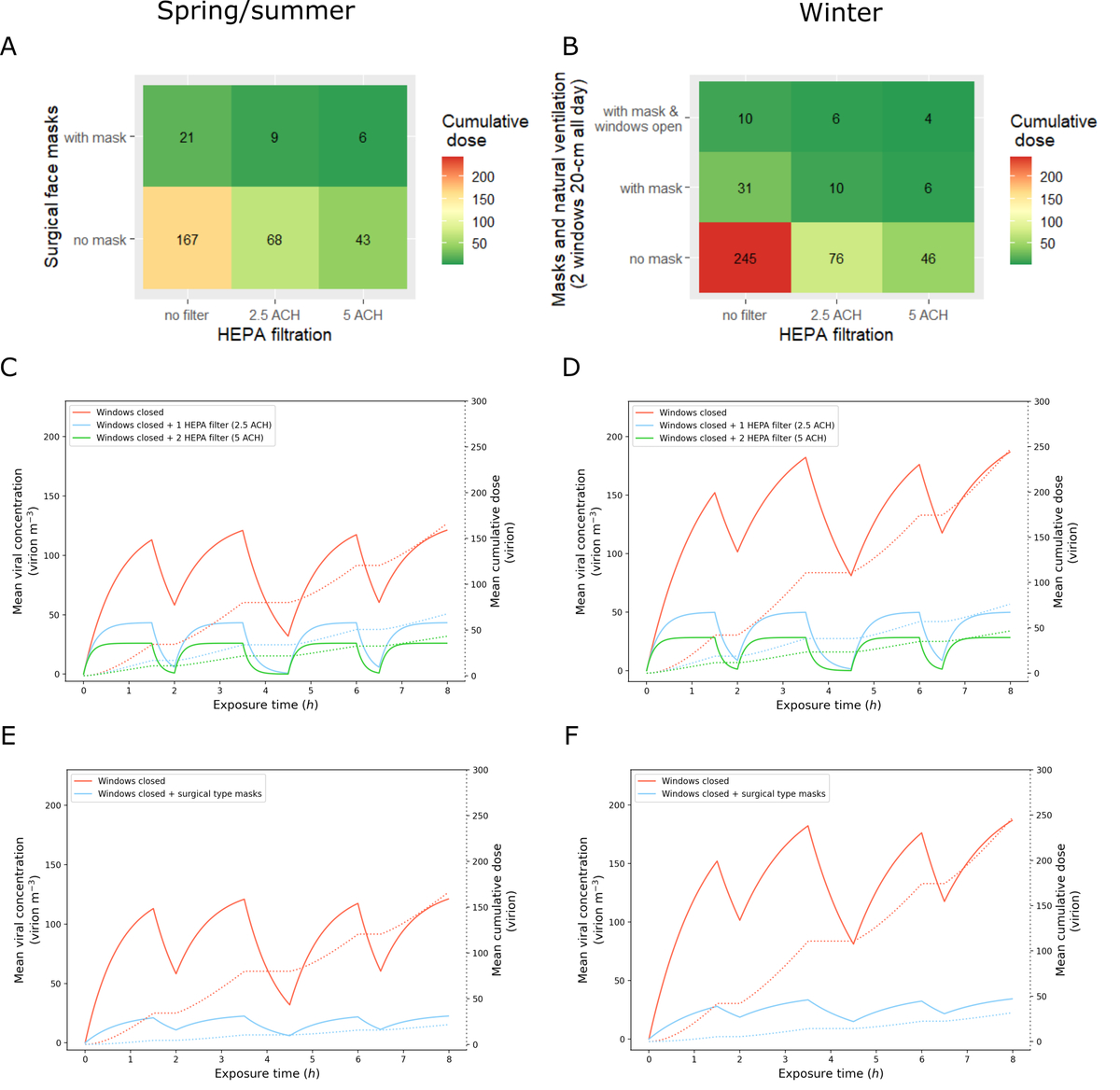
The second intervention simulated was the use of HEPA filtration devices. We tested the recommended 5 air changes per hour (ACH) [28], where two filters per classroom are needed (HEPA device each delivering a CADR up to 400 m3h-1; 800 m3h-1 in total), and an intermediate 2.5 ACH (CADR 400 m3h-1) corresponding to one filter (fig. 2a-d). The 2.5 ACH option (400 m3h-1 CADR) decreased the cumulative dose 2.5-fold in spring/summer (68 virions) and 3-fold in winter (76 virions), making it as effective as two windows 20 cm open all day long during winter (78 virions). The 5 ACH option (800 m3h-1 CADR) was even more effective with a 4-fold decrease in spring/summer and a 5-fold decrease in winter. The universal use of face masks led to an 8-fold decrease in the cumulative dose absorbed in both seasons (fig. 2e-f).
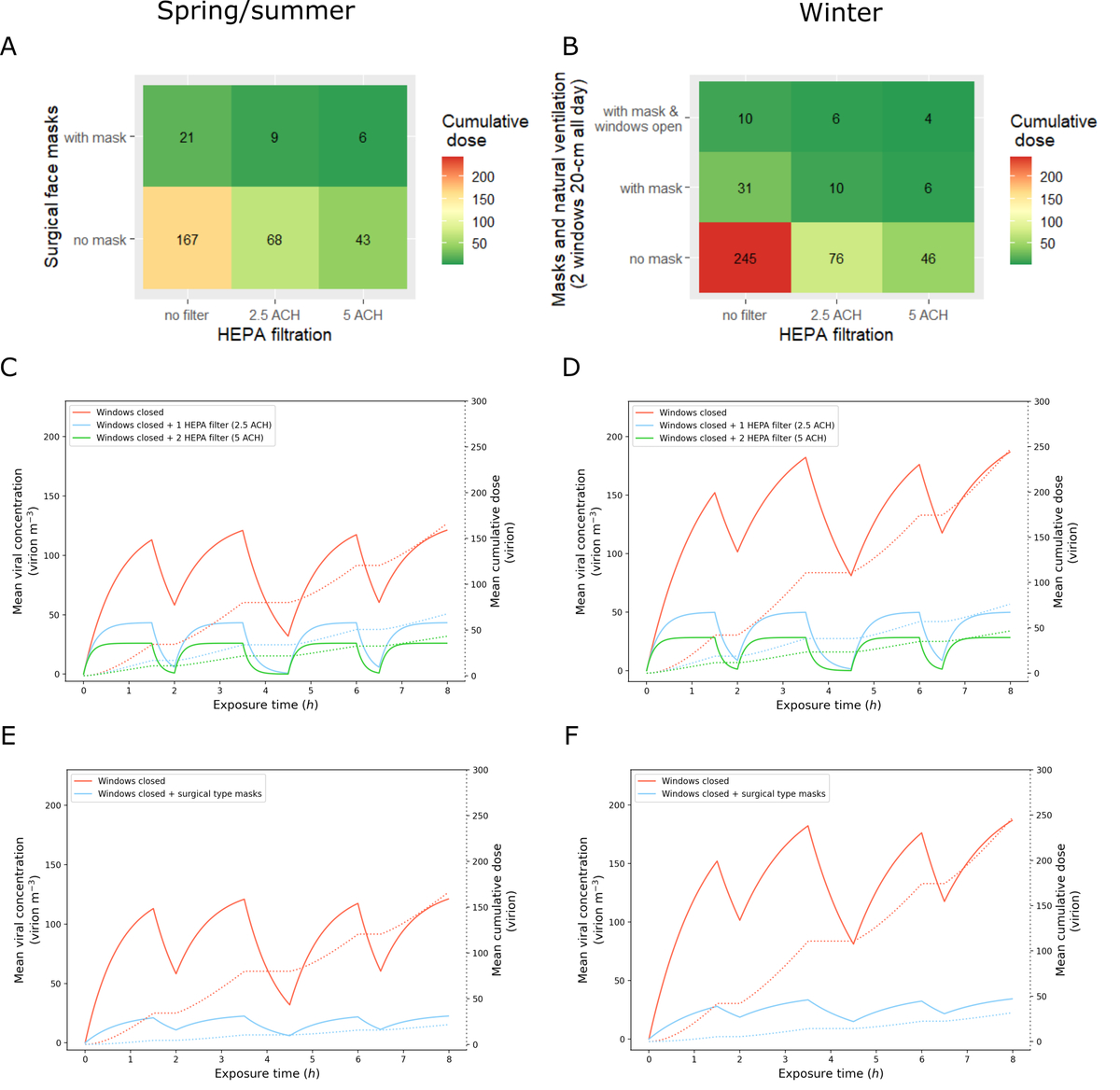
Figure 2 High efficiency particulate air (HEPA) filtration and surgical face masks.
(a, b) Heatmaps of the relative effectiveness of HEPA filtration and surgical face masks. Cumulative doses absorbed are displayed as colours ranging from red to green as shown in the key. (a) Spring/summer simulations. (b) Winter simulations. (c–f) Estimated mean viral concentration profiles over the exposure time (solid lines, left y-axis) and consequent estimated mean cumulative dose of virions absorbed by the exposed hosts (dotted lines, right y-axis). The red lines show the results for the baseline scenario with closed windows, no filters, and no masks. (c, d) The blue and green lines show the results for HEPA filtration scenarios with 2.5 air changes per hour (ACH)/400 m3h-1 and 5 ACH/800 m3h-1, respectively. (c) Spring/summer simulations. (d) Winter simulations. (e, f) The blue lines show the results for a scenario without natural ventilation nor HEPA filters where both the infectious and exposed individuals wear surgical face masks. (e) Spring/summer simulations. (f) Winter simulations.
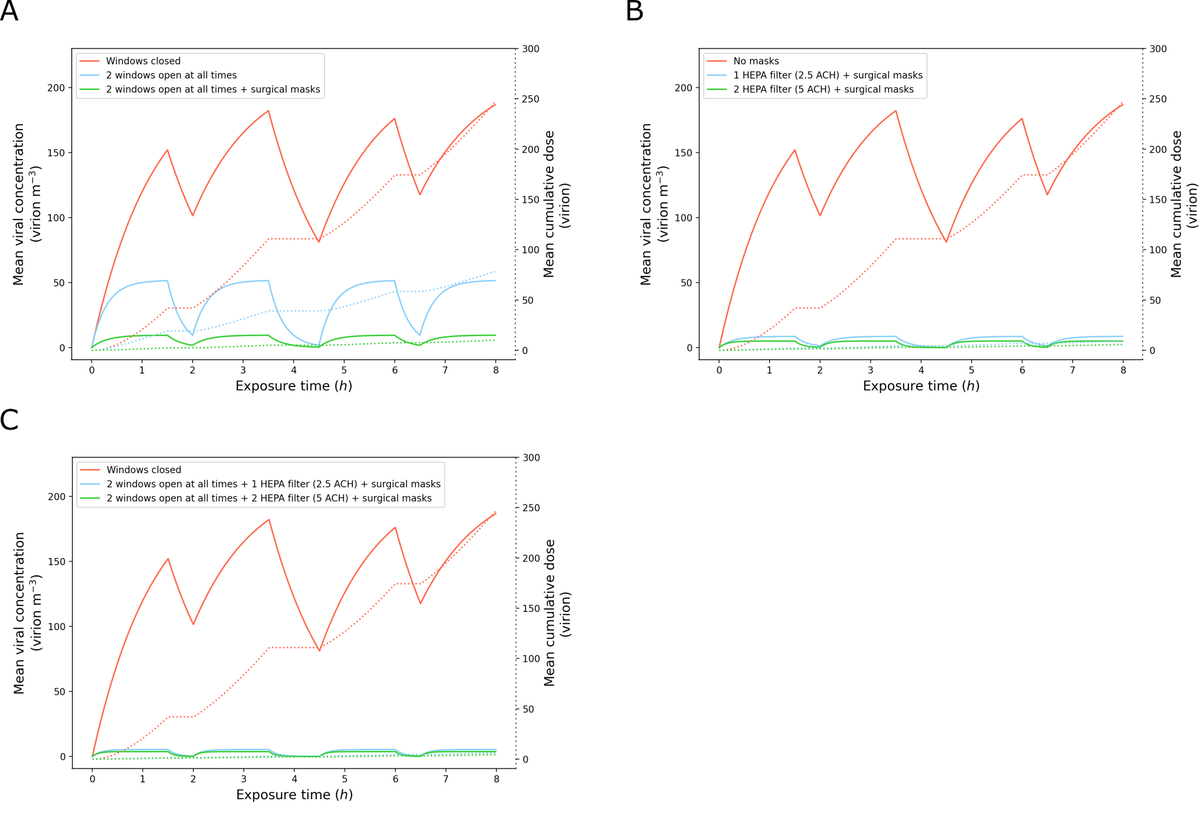
Combined interventions were generally the most effective. For instance, adding surgical face masks to natural ventilation decreased the cumulative dose absorbed 8-fold compared with natural ventilation alone. In winter for instance, adding face masks to a 20-cm opening of 2 windows all day would reduce the total cumulative dose 25-fold compared to the baseline scenario (10 virions, fig. 3a). Similarly, combining surgical face masks and HEPA filtration (2.5 ACH/400 m3h-1 CADR) led to an 18-fold decrease in spring/summer and to a 25-fold decrease in winter (around 10 virions in both cases, fig. 2a-b and 3b). In winter, combining natural ventilation (20-cm opening of two windows all day), surgical face masks and HEPA filtration reduced the cumulative dose 40-fold for 2.5 ACH (400 m3h-1 CADR) and 50-fold for 5 ACH (800 m3h-1 CADR) compared with the baseline scenario (fig. 3c).
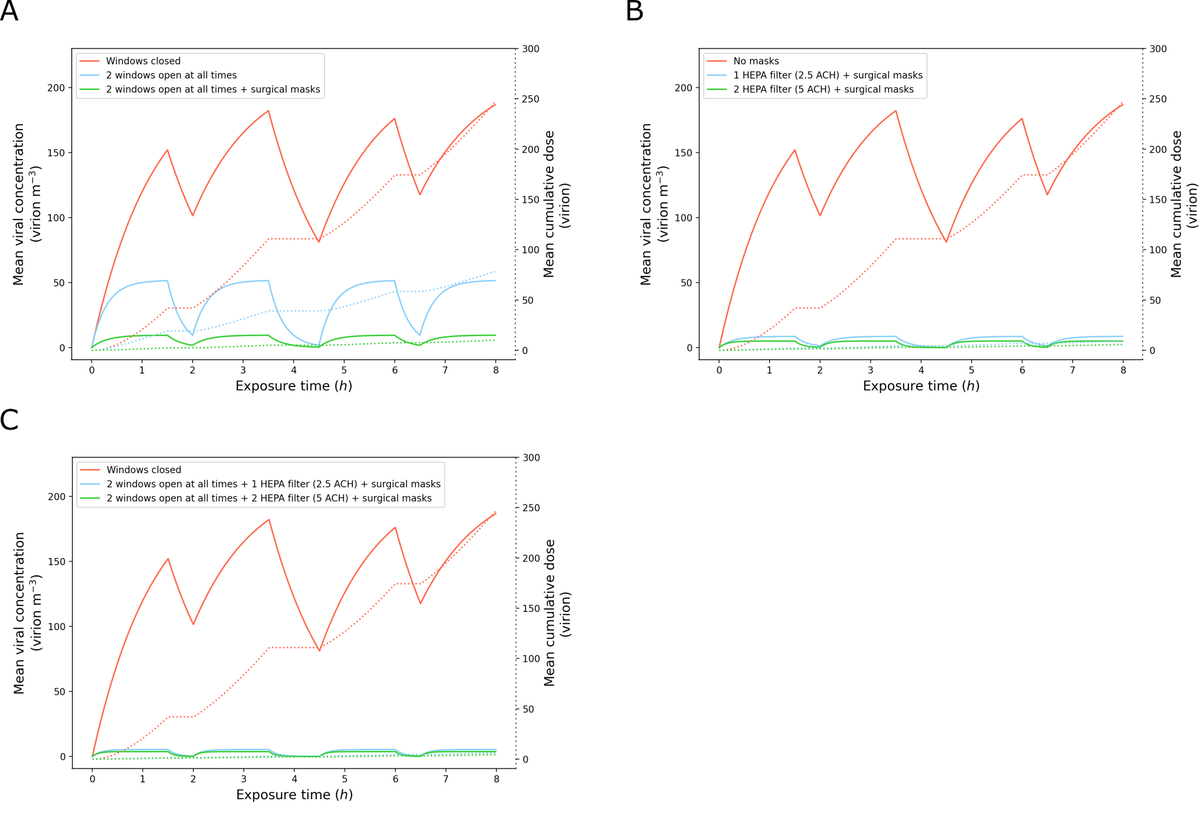
Figure 3 Combinations of interventions in winter.
Estimated mean viral concentration profiles over the exposure time (solid lines, left y-axis) and consequent estimated mean cumulative dose of virions absorbed by the exposed hosts (dotted lines, right y-axis), for different scenarios. The red lines show the results for the baseline scenario with closed windows, no high efficiency particulate air (HEPA) filtration, and no face masks. The blue and green lines show the results for different combinations of interventions. (a) Results with natural ventilation (two windows 20 cm open all day long during winter) without surgical face masks (blue) and with surgical face masks (green). (b) Results with face masks and HEPA filtration (blue: 2.5 air changes per hour (ACH)/400 m3h-1; green: 5 ACH/800 m3h-1). (c) Results with natural ventilation (two windows 20 cm open all day long during winter) and face masks and HEPA filtration (blue: 2.5 ACH/400 m3h-1; green: 5 ACH/800 m3h-1).
Since around 15% of individuals are responsible for 80% of secondary transmissions [29], we evaluated the impact of interventions when the infectious individual is a super-spreader. Since the cumulative dose absorbed by an exposed occupant in our model is strongly influenced by the viral load of the infectious occupant, we looked at the highest percentiles of the cumulative dose distributions (fig. S2). Under baseline conditions, the 95th percentile cumulative dose was 5-fold higher than the mean (~900 virions in spring/summer and ~1300 virions in winter) and the 99th percentile 16-fold higher (~2,700 virions in spring/summer and ~3900 virions in winter). In winter, when natural ventilation (20-cm opening of two windows all day) was combined with the universal use of surgical face masks (fig. S2n), the 99th percentile cumulative dose remained lower than the mean cumulative dose under baseline conditions (159 virions). When all three interventions were combined (fig. S2n), the 99th percentile cumulative dose remained below 100 virions (96 virions for 2.5 ACH/400 m3h-1 CADR and 69 virions for 5 ACH/800 m3h-1 CADR). These results suggest that combined interventions remain highly effective against super-spreaders.
Discussion
Using the COVID Airborne Risk Assessment (CARA) modeling tool [20], we found that surgical face masks, HEPA filters and strategic natural ventilation are effective strategies to reduce the cumulative dose of virions absorbed by exposed individuals in a classroom setting. We also showed that these interventions have cumulative effects and should be implemented together for maximum benefit. This is in agreement with the results of a recent study of the US CDC that — using a breathing aerosol source simulator — showed that HEPA filtration combined with face masks can reduce the mean aerosol concentration by 90% [30].
We found natural ventilation to be most effective in winter. This result was expected since the fresh air flow for single-sided natural ventilation is proportional to √∆T, with
∆T representing the difference between outdoor and indoor temperatures [20]. However, the cumulative dose in the baseline scenario (windows closed) was 1.5-fold times higher in winter than in spring/summer. This difference comes from a lower decay rate of the aerosolised viral particles when relative humidity is low (~30%), as is often the case when heating systems are turned on in the winter. As a consequence, even if natural ventilation is more effective in winter, given the high baseline values, opening windows during yard and lunch breaks remains insufficient. In winter, intermediate ventilation strategies such as the full opening of six windows at the end of each teaching period (“hourly breaks”) or a 20-cm opening of two windows all day reduced the cumulative dose 2.7- and 3-fold, respectively. In summer, similar results could be obtained through the full opening of six windows at the end of each teaching period (1.8-fold decrease) or the full opening of one or several windows all day long (with decreases ranging from 2- to 7-fold depending on the number of windows). Although humidity had a strong impact in the absence of mitigation measures, making at first indoor airborne transmission more likely in winter, the effect of ventilation quickly became dominant, leading to lower cumulative doses in winter compared with summer when all windows were maintained open throughout the day. The effectiveness of natural ventilation could be further improved through the opening of windows located on opposite sides of the room, but it was not modelled in this paper since most classrooms have windows on one side only.
Although natural ventilation through the opening of windows at all times is an effective strategy to decrease the concentration of virions in the air, it can be inadvisable when outdoor temperatures are too extreme or when the outdoor air is too polluted. In addition, when the outdoor temperature equals the indoor temperature, natural ventilation is less effective. This prompted us to consider alternative strategies to reduce virion concentration such as the use of high efficiency particulate air (HEPA) filtration devices, whose performance is unaffected by the season. The effectiveness of HEPA filters is measured in air changes per hour (ACH) of the device’s clean air delivery rate (CADR) [31] and must be calculated based on the volume of the room and the specifications of the device. However, “HEPA” per se is not a certification label and might not be enough to guarantee the desired performance. We suggest installing filters labelled H13 (≥99.95% efficiency) or H14 (≥99.995% efficiency), according to EN 1822 standard [32].
We found HEPA filtration to be an effective strategy to decrease the cumulative dose of virions absorbed by exposed individuals, with the 2.5 ACH (400 m3h-1 CADR) option leading to a 2.5- to 3-fold decrease in cumulative dose and the 5 ACH (800 m3h-1 CADR) option to a 4- to 5-fold decrease. The main disadvantage of HEPA filters compared with face masks or natural ventilation strategies is their cost — H13 and H14 HEPA filters can be expected to cost USD ~1000 and filters need to be replaced at least every two years, or according to manufacturer’s instruction, at a cost of USD ~300. Other disadvantages include noise, draught, energy consumption, and extra care that must be taken to replace and dispose of the filters. One of the main advantages of these portable devices is their mobility, meaning that they can be moved from one room to another depending on the needs.
CO2 sensors, which are more affordable (USD ~160), can be used to assess the level of natural ventilation to identify rooms that are poorly ventilated and would most benefit from the addition of HEPA filters, favouring a targeted investment for the school structure. However, there is no direct correlation between CO2 levels and virion concentration since the latter is influenced by the number of infected hosts and their viral load. No CO2 concentration can guarantee occupants’ safety, but current recommendations are to keep CO2 levels below 1000 ppm to reduce the risk of transmission of SARS-CoV-2 during sedentary activities such as classes [33–35]. Rooms where that threshold cannot be reached by natural ventilation should be prioritised for complementary measures such as HEPA filtration or the installation of a mechanical ventilation system. Levels as high as 4400 ppm have been observed in densely occupied, poorly ventilated spaces such as schools, highlighting the importance of establishing a ventilation strategy in classrooms [11, 27]. Importantly, although HEPA devices filter particulate matter, they do not filter gaseous molecules. As a consequence, CO2 sensors cannot be used to assess the efficacy of HEPA filters and HEPA filtration devices should be combined with natural or mechanical ventilation to ensure that CO2 concentrations do not exceed levels that have been found to interfere with students’ performance. CO2 levels are influenced by the number of people occupying the room, but the viral concentration is influenced only by the number of infectious individuals, their viral load and their physical and expiratory activities. In this paper, we assumed a homogeneous viral concentration in a classroom containing one infectious individual, meaning that all other room occupants have an equal exposure to virions.
The universal use of surgical face masks was one of the most effective interventions to reduce the cumulative dose absorbed by exposed individuals (8-fold decrease in both seasons). However, similar to HEPA devices, what is crucial is to guarantee the desired filtration performance with the proper certification. We suggest to use well fit surgical masks labelled with a material filtration performance of at least Type I (≥95% bacterial filtration efficiency), according to EN 14683 standard [36].
Combined interventions — i.e., natural ventilation in combination with surgical face masks and HEPA filters — remained highly effective in the presence of a super-spreader. Heterogeneity in transmission is a characteristic feature of SARS-CoV-2, with around 15% of infected individuals responsible for 80% of secondary infections [29]. This high heterogeneity in transmission has been traced back to heterogeneity in both the number of contacts and in individuals’ viral loads — with 2% of individuals harbouring up to 90% of virions [37]. This effect has been proposed as an explanation for the apparent discrepancies in the literature regarding transmission of SARS-CoV-2 in school settings, with most children not transmitting the disease to anyone and a handful being responsible for large outbreaks [38]. In addition, viral load distributions were found to be similar between children, youths and adults as well as between symptomatic and asymptomatic individuals [37], with around half of transmissions occurring during the presymptomatic phase [29]. Since highly contagious individuals cannot be identified based on age or symptoms, mitigation strategies such as ventilation and face masks are especially important in crowded, closed settings such as classrooms.
One important limitation of our model comes from the lack of consensus regarding the infectious dose. Hence, we cannot predict, on a quantitative level, what measures are sufficient to keep the occupants of the room safe. Nonetheless, reducing the number of inhaled virions will result in an exponential reduction in the probability of contracting the disease. Therefore, estimating the mean cumulative dose absorbed in each scenario and by how much it varies based on the interventions can already provide actionable information. Furthermore, the infectious dose is hypothesised to vary depending on the SARS-CoV-2 variant. Since no significant change in viral load was observed between the original variant and the alpha variant [39], the most likely hypothesis to explain the increased infectivity of the alpha variant was a genetic mutation in the spike protein enabling it to more effectively bind to the ACE2 receptor [40], thereby decreasing the amount of viral particles needed to infect a susceptible host. With the rise of new variants such as omicron, which became dominant in Switzerland within one month and is spreading faster among children and young adults [10, 41], we can expect the infectious dose to decrease, making new outbreaks more difficult to contain. Even with vaccination now reaching the youngest age groups, the ability of the omicron variant to evade immunity has shown that mitigation strategies such as ventilation and face masks remain crucial to decrease the number of infections and hence prevent the rise of new and potentially more dangerous SARS-CoV-2 variants.
Another major limitation of our model is the assumption of a homogeneous viral concentration throughout the room, as it does not account for the proximity to the infectious individual. A well-mixed model has the advantage of simplicity and requires lower computing power, which can be an asset when performing a rapid assessment for each room in a school. However, it only evaluates the effectiveness of interventions against long-range airborne transmission. Additional hygiene and distancing measures remain necessary to prevent short-range transmission. Among the interventions that we tested, the universal use of face masks was one of the most effective at preventing long-range transmission and is the only one that also protects against short-range transmission. In June 2021, several countries lifted requirements for face coverings in secondary schools despite increasing infection rates in educational settings [42, 43]. In an opinion piece, Gurdasani and colleagues “argued that this was ill-advised given the clear evidence for the role of children and schools in transmission of SARS-CoV-2 and the rise of the new (delta) variant” [44]. Our results further support this position since universal face masks decreased 8-fold the cumulative dose absorbed by exposed individuals.
Besides primary and secondary education settings, the CARA tool can also be used to assess the effectiveness of mitigation measures in other settings, such as universities, other higher education institutions, and other indoor spaces. Beyond the current COVID-19 crisis, maintaining a proper level of ventilation in classrooms is also recommended for the children’s health and performance [45]. Some of the most pathogenic viruses such as influenza, respiratory syncytial virus, adenovirus, coronavirus and measles are transmitted through aerosols, and elevated levels of CO2 have been found to interfere with intellectual concentration and, thus, students’ performance. HEPA filtration devices could also be useful beyond the pandemic as they might capture larger airborne particles such as pollen or outdoor atmospheric pollutants, which were found to be associated with increased susceptibility to respiratory diseases such as COVID-19 [46, 47].
Executive summary
- Surgical face masks, HEPA filters and window opening are effective strategies to reduce the risk of airborne transmission and have cumulative effects.
- Among feasible interventions tested in our model, mask wearing is the most effective against airborne transmission (8-fold reduction in cumulative dose absorbed) and is the only one that also protects against short-range transmission.
- Opening windows only during yard and lunch breaks is not effective at decreasing risk (from 1.1 to 1.5-fold reduction in cumulative dose absorbed).
- Opening several windows on one side of the room during the whole teaching period is effective in summer (3-fold reduction with two windows, 7-fold reduction with six windows).
- It is even more effective in winter (7.5-fold reduction with two windows, 20-fold reduction with six windows) but inadvisable (energy waste and thermal discomfort).
- The partial opening (20 cm) of two windows during the whole teaching period or the full opening of six windows for 10 minutes at the end of each teaching period (every 45 minutes) can be effective measures in winter (3- and 2.7-fold reduction, respectively), especially if combined with surgical face masks (25-fold reduction).
- Two air filters correctly placed in the room with an air flow rate of 5 times the room volume (CADR = 800 m
- Inexpensive CO
- CO
Data sharing statement
CARA is an Open Source software under an APACHE License, Version 2.0. The code repository can be accessible here: https://gitlab.cern.ch/cara/cara. Other information can be obtained from the corresponding author.
Acknowledgements
The authors thank Sabina Rodriguez Velásquez for improving the use of English in the manuscript.
Contributors: JV, AH, SC, and OK conceived and planned the numerical experiments. AH, MR, NM, JD, GA, PE, MA, and NT designed the model and the computational framework. AH carried out the simulations. JV, AH, SC, CV, and OK interpreted the results. JV and AH designed the figures. JV drafted the manuscript and AH, CV, and OK revised it critically. OK supervised the project. All authors reviewed and approved the final manuscript.
Andre Henriques
European Organization for Nuclear Research (CERN)
CH-1211 Geneva 23
andre.henriques[at]cern.ch
References
1.
Swiss National COVID-19 Science Task Force
. The role of children (≤12 years of age) and adolescents (13-17 years of age) in the SARS-CoV-2 pandemic: A rapid review. 27 April 2021. https://sciencetaskforce.ch/en/policy-brief/the-role-of-children-and-adolescents-0-18-years-of-age-in-the-transmission-of-sars-cov-2-a-rapid-review-09-04-2021/
2.
Hyde Z.
COVID‐19, children and schools: overlooked and at risk. Medical Journal of Australia. 2020;213(10):444-446. e1.
3.
Szablewski CM
,
Chang KT
,
Brown MM
,
Chu VT
,
Yousaf AR
,
Anyalechi N
, et al.
SARS-CoV-2 transmission and infection among attendees of an overnight camp—Georgia, June 2020. MMWR Morb Mortal Wkly Rep. 2020 Aug;69(31):1023–5. https://doi.org/10.15585/mmwr.mm6931e1
4.
Stein-Zamir C
,
Abramson N
,
Shoob H
,
Libal E
,
Bitan M
,
Cardash T
, et al.
A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020. Euro Surveill. 2020 Jul;25(29):2001352. https://doi.org/10.2807/1560-7917.ES.2020.25.29.2001352
5.
Yoon J.
27 cases of COVID-19 confirmed at Boucherville day camp. CBC News. 29 July 2020;
6.
Torres JP
,
Piñera C
,
De La Maza V
, et al.
SARS-CoV-2 antibody prevalence in blood in a large school community subject to a Covid-19 outbreak: a cross-sectional study. Clin Infect Dis. 2020.
7.
Otte im Kampe E
. Lehfeld A-S, Buda S, Buchholz U, Haas W. Surveillance of COVID-19 school outbreaks, Germany, March to August 2020. Euro Surveill. 2020;25(38):2001645.
8.
Public Health England
. SARS-CoV-2 variants of concern and variants under investigation in England, Technical briefing 16. 18 June 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/997414/Variants_of_Concern_VOC_Technical_Briefing_16.pdf
9.
Office of National Statistics
. Coronavirus (COVID-19) Infection Survey, UK: 29 October 2021 - 11 February 2022. 2021-2022.
10.
Swiss Federal Office of Public Health
. COVID-19 Switzerland. Information on the current situation, as of 14 February 2022. Laboratory-confirmed cases. 2022. https://www.covid19.admin.ch/en/epidemiologic/case
11.
Marr L
,
Miller S
,
Prather K
, et al.
FAQs on Protecting Yourself from COVID-19 Aerosol Transmission. Vol. Version: 1.87. 9 December 2020. https://tinyurl.com/FAQ-aerosols
12.
Moschovis PP
,
Yonker LM
,
Shah J
,
Singh D
,
Demokritou P
,
Kinane TB
. Aerosol transmission of SARS-CoV-2 by children and adults during the COVID-19 pandemic. Pediatr Pulmonol. 2021 Jun;56(6):1389–94. https://doi.org/10.1002/ppul.25330
13.
Jones E
,
Young A
,
Clevenger K
, et al.
Healthy schools: risk reduction strategies for reopening schools. Harvard TH Chan School of Public Health Healthy Buildings program. 2020;
14.
Greenhalgh T
,
Jimenez JL
,
Prather KA
,
Tufekci Z
,
Fisman D
,
Schooley R
. Ten scientific reasons in support of airborne transmission of SARS-CoV-2. Lancet. 2021 May;397(10285):1603–5. https://doi.org/10.1016/S0140-6736(21)00869-2
15.
Wang CC
,
Prather KA
,
Sznitman J
, et al.
Airborne transmission of respiratory viruses. Science. 08 27 2021;373(6558)doi:https://doi.org/10.1126/science.abd9149
16.
World Health Organization
. Roadmap to Improve and Ensure Good Indoor Ventilation in the Context of COVID-19. 2021. https://www.who.int/publications/i/item/9789240021280
17.
Centers for Disease Control and Prevention
. Guidance for COVID-19 Prevention in K-12 Schools. 13 January 2022. https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/k-12-guidance.html#ventilation
18.
Gov.uk
. Schools COVID-19 operational guidance. 19 January 2022. https://www.gov.uk/government/publications/actions-for-schools-during-the-coronavirus-outbreak/schools-coronavirus-covid-19-operational-guidance
19.
Swiss Federal Office of Public Health
. Coronavirus: Measures and ordinances. 3 February 2022. https://www.bag.admin.ch/bag/en/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/massnahmen-des-bundes.html
20.
Henriques A
,
Mounet N
,
Aleixo L
,
Elson P
,
Devine J
,
Azzopardi G
, et al.
Modelling airborne transmission of SARS-CoV-2 using CARA: risk assessment for enclosed spaces. Interface Focus. 2022 Feb;12(2):20210076. https://doi.org/10.1098/rsfs.2021.0076
21.
Jacot D
,
Greub G
,
Jaton K
,
Opota O
. Viral load of SARS-CoV-2 across patients and compared to other respiratory viruses. Microbes Infect. 2020 Nov - Dec;22(10):617–21. https://doi.org/10.1016/j.micinf.2020.08.004
22.
Johnson G
,
Morawska L
,
Ristovski Z
,
Hargreaves M
,
Mengersen K
,
Chao CY
, et al.
Modality of human expired aerosol size distributions. J Aerosol Sci. 2011;42(12):839–51. https://doi.org/10.1016/j.jaerosci.2011.07.009
23.
van Doremalen N
,
Bushmaker T
,
Morris DH
,
Holbrook MG
,
Gamble A
,
Williamson BN
, et al.
Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020 Apr;382(16):1564–7. https://doi.org/10.1056/NEJMc2004973
24.
Yang W
,
Elankumaran S
,
Marr LC
. Relationship between humidity and influenza A viability in droplets and implications for influenza’s seasonality. 2012;
25.
Watanabe T
,
Bartrand TA
,
Weir MH
,
Omura T
,
Haas CN
. Development of a dose-response model for SARS coronavirus. Risk Anal. 2010 Jul;30(7):1129–38. https://doi.org/10.1111/j.1539-6924.2010.01427.x
26.
Department of Homeland Security (DHS) Science and Technology Directorate
. (S&T). Master question list for COVID-19 (caused by SARS-CoV-2), required information for effective infectious disease outbreak response. Accessed March 12, 2021, https://www.dhs.gov/publication/st-master-question-list-covid-19
27.
Vassella CC
,
Koch J
,
Henzi A
,
Jordan A
,
Waeber R
,
Iannaccone R
, et al.
From spontaneous to strategic natural window ventilation: improving indoor air quality in Swiss schools. Int J Hyg Environ Health. 2021 May;234:113746. https://doi.org/10.1016/j.ijheh.2021.113746
28.
Allen J
,
Spengler J
,
Jones E
,
Cedeno-Laurent J
. 5-step guide to checking ventilation rates in classrooms. August, 2020. https://schools.forhealth.org/wp-content/uploads/sites/19/2020/08/Harvard-Healthy-Buildings-program-How-to-assess-classroom-ventilation-08-28-2020.pdf
29.
Sun K
,
Wang W
,
Gao L
,
Wang Y
,
Luo K
,
Ren L
, et al.
Transmission heterogeneities, kinetics, and controllability of SARS-CoV-2. Science. 2021 Jan;371(6526):eabe2424. https://doi.org/10.1126/science.abe2424
30.
Lindsley WG
,
Derk RC
,
Coyle JP
,
Martin SB Jr
,
Mead KR
,
Blachere FM
, et al.
Efficacy of Portable Air Cleaners and Masking for Reducing Indoor Exposure to Simulated Exhaled SARS-CoV-2 Aerosols - United States, 2021. MMWR Morb Mortal Wkly Rep. 2021 Jul;70(27):972–6. https://doi.org/10.15585/mmwr.mm7027e1
31.
Nazaroff WW
. Effectiveness of air cleaning technologies. SIY Indoor Air Information Oy Helsinki, Finland; 2000:49-54.
32.
European Committee for Standardization
. EN 1882:2019, High efficiency air filters (EPA, HEPA and ULPA) - Part 1: Classification, performance testing, marking. Brussels: standard, CEN; 2019.
33.
Swiss National COVID-19 Science Task Force
. On the use of CO2 sensors in schools and other indoor environments -. Policy Brief. 2021 Apr;19:•••. Available from: https://sciencetaskforce.ch/en/policy-brief/on-the-use-of-co2-sensors-in-schools-and-other-indoor-environments/
34.
Federation of European Heating Ventilation and Air-conditioning Associations (REHVA)
. REHVA COVID-19 guidance document. 15 April 2021.
35.
Gov.uk
. EMG and SPI-B: Application of CO2 monitoring as an approach to managing ventilation to mitigate SARS-CoV-2 transmission, 27 May 2021. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/992966/S1256_EMG_SPI-B_Application_of_CO2_monitoring_as_an_approach_to_managing_ventilation_to_mitigate_SARS-CoV-2_transmission.pdf
36.
European Committee for Standardization
. EN 14683:2019+AC:2019, Medical face masks - Requirements and test methods. Brussels: standard, CEN; 2019.
37.
Yang Q
,
Saldi TK
,
Gonzales PK
,
Lasda E
,
Decker CJ
,
Tat KL
, et al.
Just 2% of SARS-CoV-2-positive individuals carry 90% of the virus circulating in communities. Proc Natl Acad Sci USA. 2021 May;118(21):e2104547118. https://doi.org/10.1073/pnas.2104547118
38.
Tupper P
,
Colijn C
. COVID-19's unfortunate events in schools: mitigating classroom clusters in the context of variable transmission. medRxiv. 2020 https://doi.org/10.1101/2020.10.20.20216267
39.
Walker AS
,
Vihta KD
,
Gethings O
, et al.
Increased infections, but not viral burden, with a new SARS-CoV-2 variant. medRxiv. 2021 https://doi.org/10.1101/2021.01.13.21249721
40.
Public Health England
. Investigation of novel SARS-COV-2 variant: Variant of concern 202012/01, technical briefing 1. 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/959438/Technical_Briefing_VOC_SH_NJL2_SH2.pdf
41.
Swiss Federal Office of Public Health
. COVID-19 Switzerland. Information on the current situation, as of 14 February 2022. Virus variants. 2022. https://www.covid19.admin.ch/en/epidemiologic/virus-variants
42.
UK Department for Education
. Guidance: Face coverings in education. 24 May 2021. https://www.gov.uk/government/publications/face-coverings-in-education/face-coverings-in-education
43.
Swiss Federal Council
. Federal Council eases measures against the coronavirus from June 26. 23 June 2021. https://www.newsd.admin.ch/newsd/message/attachments/67283.pdf
44.
Gurdasani D
,
Ziauddeen H
,
Reicher S
,
McKee M.
Covid-19 and the delta variant—we need an urgent focus on mitigations in schools. BMJ Opinion. 11 June 2021;
45.
Swiss Federal Office of Public Health
. Comment bien aérer sa classe. Accessed 11 July 2021, https://www.schulen-lueften.ch/fr/accueil
46.
Damialis A
,
Gilles S
,
Sofiev M
,
Sofieva V
,
Kolek F
,
Bayr D
, et al.; COVID-19/POLLEN study group
. Higher airborne pollen concentrations correlated with increased SARS-CoV-2 infection rates, as evidenced from 31 countries across the globe. Proc Natl Acad Sci USA. 2021 Mar;118(12):e2019034118. https://doi.org/10.1073/pnas.2019034118
47.
Ali N
,
Islam F
. The effects of air pollution on COVID-19 infection and mortality—A review on recent evidence. Front Public Health. 2020 Nov;8:580057. https://doi.org/10.3389/fpubh.2020.580057
Appendix: Supplementary data
The appendix is available in the pdf version of the article.