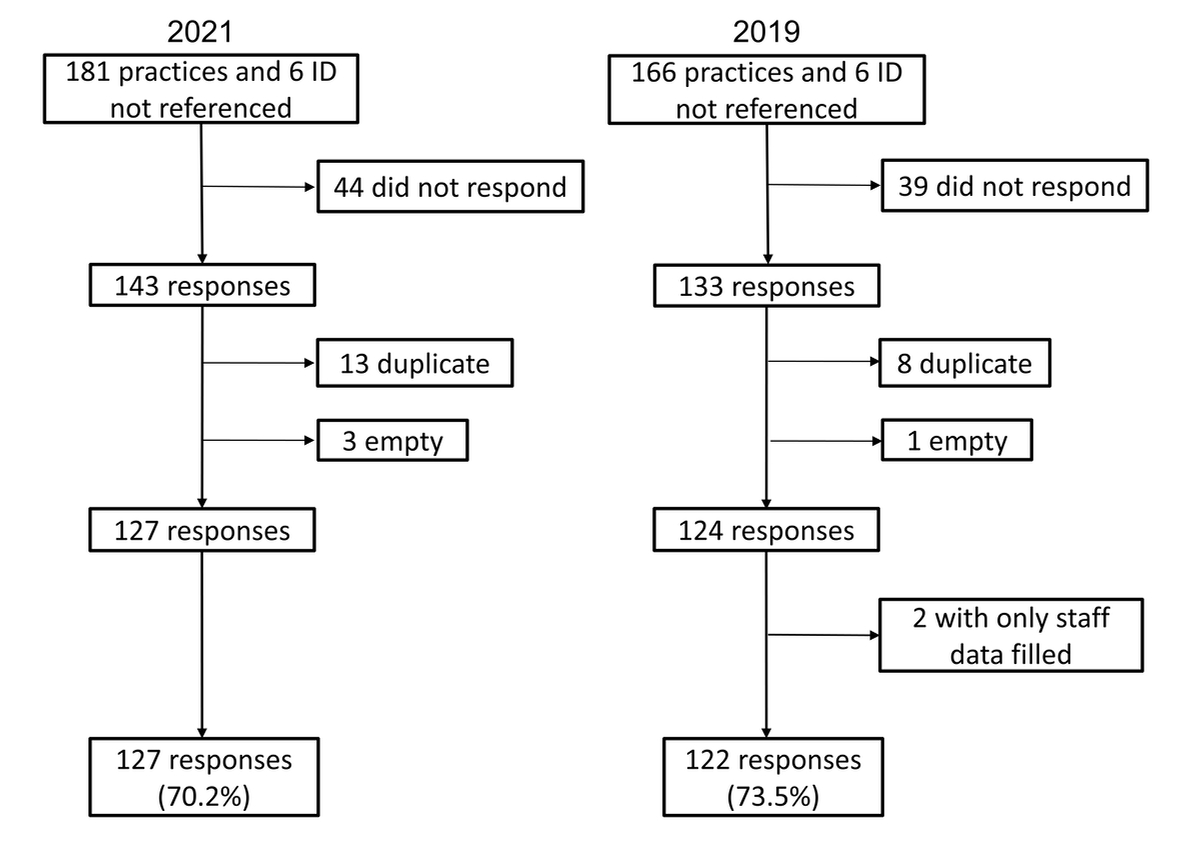
Figure 1 Flow chart showing the response rate of practices invited to participate in the surveys on infection prevention and control measures in 2021 and 2019. ID: identifier.
DOI: https://doi.org/10.4414/SMW.2022.w30170
Before the COVID-19 pandemic, evidence guiding of infection prevention and control (IPC) was limited in primary care, and recommendations consisted primarily of implementation of standard precautions [1, 2].
Specific influenza protection measures are traditionally general measures to be implemented at the time of the seasonal epidemic. In contrast, COVID-19 infection control mainly relied, prior to COVID-19 vaccination availability and immunisation through disease, on active case-finding, and putting in place isolation and quarantine measures that limit the circulation of the virus in the environment. Still, more than one third of COVID-19 infections may go undiagnosed and general protection measures, such as physical distancing, hand hygiene, mask wearing and vaccination, are also recommended [3, 4].
Our 2019 cross-sectional survey of Swiss private practices showed that primary care physicians often adhered to vaccination measures but other staff less so [1]. Adherence to hand hygiene measures was found to be suboptimal and specific facemask recommendations were not systematically in place at the time. Indeed, at the Swiss national level there were no existing nationwide general recommendations for IPC measures targeting primary care practices before the COVID-19 pandemic, and only scarce pre-existing recommendations on influenza prevention, which emphasised primarily vaccination rather than other protective measures [5]. At the beginning of the pandemic, primary care physicians and practices were in contact with COVID-19 patients and encountered logistical difficulties such as an insufficient supply of personal protective equipment, hand sanitizer and face masks for patients and staff, in the absence of vaccines against the SARS-CoV-2 virus [6]. These complications limited the possibility for practices implementing IPC measures, despite evidence from studies outside the Swiss setting that exposure to initially asymptomatic COVID-19 patients could lead to primary and hospital care-associated infections [7, 8].
The surge of COVID-19 led to the development of IPC guidelines for the private practice setting by the Centers for Disease Control and Prevention in the US and the European Centre for Disease Prevention and Control [9, 10]. Based on the European recommendations, the national Swiss Physician Federation endorsed national guidelines for COVID-19 prevention in the primary care setting [11]. European and Swiss recommendations and guidance in place on 1 March 2021, the date of distribution of the survey questionnaire, were similar except for the notable difference of the type of mask recommended for non-aerosol-generating procedures [9, 12]. The recommendation of the European Centre for Disease Prevention and Control was to use medical face masks only in case of shortage of FFP2/3 respirators, whereas the Swiss endorsed medical face masks for standard use [9].
Moreover, it was observed that the adoption of IPC measures had the unintended positive effect of reducing healthcare-related respiratory viral infections. As an example, these infections decreased from 9.69 cases per 10,000 patient-days to 0.83 cases per 10,000 patient-days (incidence-rate ratio 0.08, 95% confidence interval [CI] 0.05–0.13; p <0.05) after implementation of multimodal IPC measures in a health campus in Singapore [13]. Measures implemented at the population level also had a dramatic impact. In Switzerland in the winter of 2020 to 2021, the epidemic threshold for influenza was never reached [14].
The COVID-19 pandemic thus provides an opportunity to describe how practices adapted in the Swiss setting and to evaluate to what extent practitioners changed their way of working on integrating the recommended IPC measures. The aim of this survey was to report how the COVID-19 pandemic influenced IPC measures in private practices of the Swiss sentinel network by investigating their adherence to the recommended national protection plan and comparing the implementation of IPC measures between 2019 and 2021.
We conducted a cross-sectional survey using an online questionnaire between the 1 March and 4 May 2021, among primary care practices of the Swiss Sentinel Network (Sentinella). This network is composed of private practices of general practitioners and paediatricians from across Switzerland. The Swiss Federal Office of Public Health (FOPH) monitors influenza and other transmissible diseases nationwide using Sentinella, whose members contribute voluntarily to data collection by reporting cases of influenza-like illness and, for a subset of practices, collecting nasopharyngeal swabs analysed by the National Reference Centre for Influenza. This system was adapted for surveillance of the COVID-19 pandemic [15]. In each of the Sentinella network practices one physician was the designated responder.
Development and piloting of the initial survey in 2019 is detailed in our previous study [1]. For the 2021 study, the questionnaire included questions concerning the practice’s characteristics and organisation, including the opening date of the practice, number of physicians in the practice and their specialties, number and job titles of auxiliary staff, number of rooms and presence or not of continuous ventilation. It also inquired into the implementation of IPC measures regarding the three following topics:
French and German are the usual working languages of Sentinella. The questionnaire was written in French and translated into German with the help of the FOPH. The questionnaire was then approved by the Sentinella programme commission, comprised of Swiss university institutes of general medicine, the FOPH and regional representatives of responding physicians.
The FOPH sent a link to the online questionnaire to all Sentinella members on the 1 March 2021 and the link remained open until the 4 May 2021. During this timeframe, Sentinella members received one reminder e-mail. Participants answered on a voluntary basis via the online questionnaire. The investigators did not have access to identifying data. As the available data did not contain patient-specific information, ethical review under the scope of the Human Health research Law was not required.
Data were collected in REDCap (Research Electronic Data Capture, Vanderbilt University, Nashville, TN, USA), an electronic data capture tool hosted locally.
The proportions of physicians adhering to specific measures were estimated and compared with results of the pre-COVID-19 pandemic cross-sectional survey conducted in 2019 in the same setting and with the same methodology [1]. For some items, additional response categories were added to capture a finer description of habits. Some extra questions were added to evaluate compliance to national IPC guidelines in place at the time of the survey [11].
Finally, we carried out descriptive data analysis using Stata 15 (StataCorp, College Station, Tx, USA). Considered as duplicates and therefore excluded were the entries from a given Sentinella identification number with identical practice characteristics, for which an empty, incomplete or duplicated answer form was submitted more than once. The number of missing answers was specified for each specific item and not included in the denominator when calculating the proportion. Where comparable, proportions between 2019 and 2021 were compared by chi-square or Fisher’s exact tests where appropriate; we compared medians of count data using Wilcoxon Mann Whitney’s rank sum test. Response categories added in 2021 were regrouped for comparability with 2019 (for example, responses “more than once daily” + “at least once hourly” + “between each patient” in 2021 were compared with “more than once daily” in 2019).
The data collected within this project do not require ethical review by the Ethics Committee, as confirmed by the CER (Commission cantonale VD de l’éthique de la recherche sur l’être humain) on the 10 July 2018. The data are available in Open Access on the Unisanté repository for research purposes: https://doi.org/10.16909/dataset/29 [17].
At the time of the study, 181 practices were enlisted in Sentinella, representing 214 individual physicians (77 females). We received 143 questionnaires. After removal of duplicates and empty forms, 127 valid responses amounted to a 70.2% response rate. Given that only Sentinella member practices received the link to the questionnaire, we considered the responses received from non-referenced identifiers as valid (fig. 1). Of the 127 respondents, 72 (56.7%) had previously answered the 2019 survey, and 55 (43.3%) were new (supplementary tables S2–S5 in the appendix).
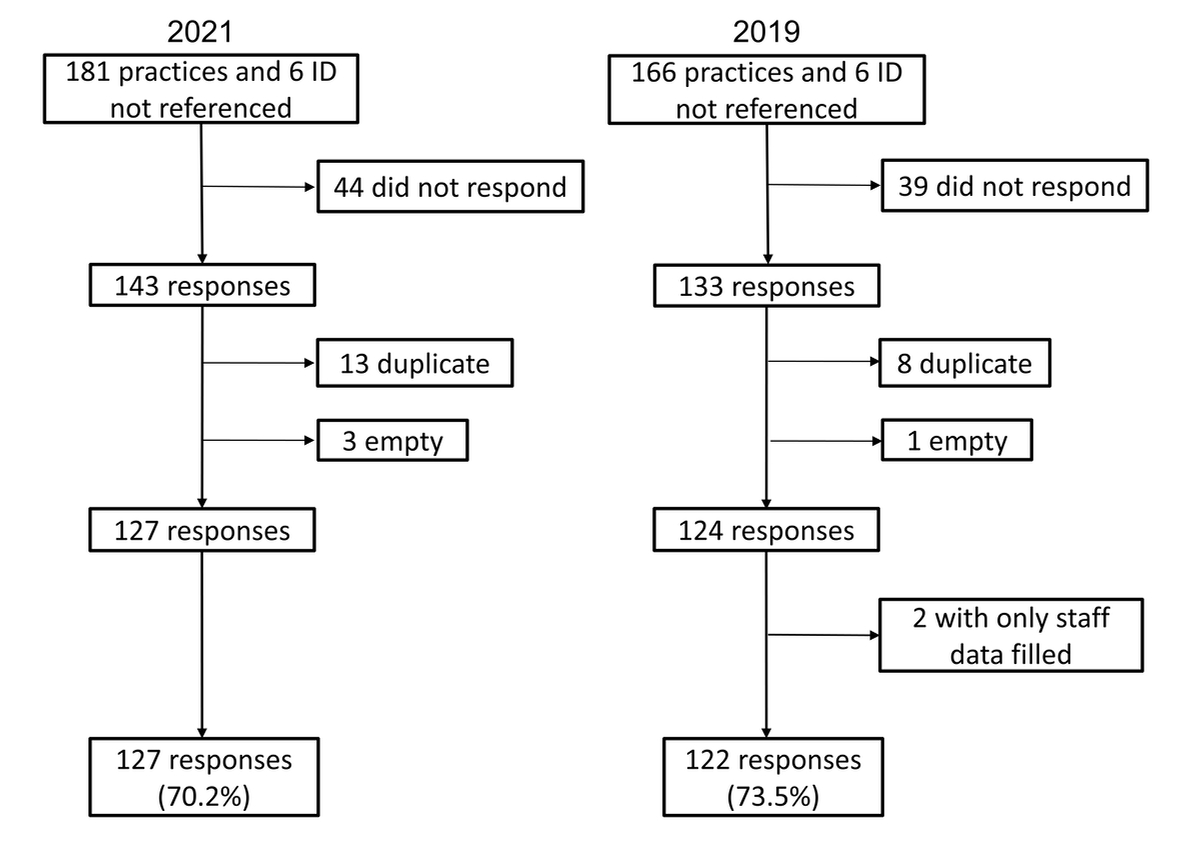
Figure 1 Flow chart showing the response rate of practices invited to participate in the surveys on infection prevention and control measures in 2021 and 2019. ID: identifier.
Table 1Practice characteristics in the Sentinella network in 2021 and 2019 (127 and 122 answering practices, respectively).
| Specialties represented in the practice (at least 1 specialist per practice) | 2021 | 2019 | p-value | |
| n (%) | n (%) | |||
| General practice* | 112 (88.2%) | 108 (88.5%) | 0.934 | |
| Paediatrics* | 20 (15.8%) | 16 (13.1%) | 0.555 | |
| Other specialties* | 22 (17.3%) | 19 (15.6%) | 0.710 | |
| Number of staff per category | median (25–75%) | median (25–75%) | p-value | |
| Physicians | Total | 2 (1–4) | 2 (1–3) | 0.221 |
| Half-days of consultation per week per physician | 7.7 (6.0–9.0) | 7.5 (5.7–9.0) | 0.686 | |
| Other staff | Total | 5 (3–8) | 4 (2–7) | 0.079 |
| Full-time equivalents(2019: 30 missing values) | 2.6 (1.4–5.0) | 2.6 (1.6–4.0) | 0.983 | |
| Physical characteristics | median, n (25–75%), % | median, n (25–75%), % | p-value | |
| Year of setting up practice | 2008 (1995–2014) | 1999 (1990–2011) | 0.014 | |
| Number of rooms | Total | 7 (6–11) | 7 (6–10) | 0.477 |
| Consultation rooms | 3 (2–5) | 3 (2–4) | 0.597 | |
| Waiting rooms | 1 (1–2) | 1 (1–1) | 0.042 | |
| Continuous ventilation | 32 (25.2%) | 26 (21.3%) | 0.426 | |
* multiple answers possible.
Practices had a median of two physicians per practice, the main specialities represented were general internal medicine (in 88.2% of practices) and paediatrics (15.8%). Physicians consulted for a median of 7.7 half days per week and had 5 additional staff on average per practice amounting to 2.6 full-time equivalents (mostly medical assistants, but also secretaries and cleaners). The median number of rooms per practice was 7, of which 3 were consultation rooms and 1 was a waiting room. Continuous ventilation was available in 25.2% of practices.
Social distancing in the waiting room complied with the 1.5 m distancing rule in 59.8% of the responding practices (table 2).
Table 2Infection prevention and control measures in the Sentinella network in 2021 and 2019 (127 and 122 answering practices, respectively).
| Measures targeting staff | 2021 | 2019 | p-value | ||
| n/N (%) | n/N (%) | ||||
| Alcohol-based disinfection for staff | Not available | 1/126 (0.8%) | 0 | N / A | |
| Available only during influenza epidemic season | 0 | 0 | |||
| Available all year round | 124/126 (99.2%) | 121/122 (99.2%) | 1.000 | ||
| Protective mask wearing for staff * | Always | 119/126 (93.7%) | N / A | N / A | |
| In the case of respiratory symptoms | 0 | 50/122 (41.0%) | <0.001 | ||
| If not vaccinated against influenza | 3/126 (2.4%) | 15/122 (12.3%) | 0.002 | ||
| During care to patients | 3/126 (2.4%) | 14/122 (11.5%) | 0.004 | ||
| No specific recommendation | 1/126 (0.8%) | 68/122 (55.7%) | <0.001 | ||
| Clothing | Reporting physician* | Wearing professional clothes washable at 60°C | 86/127 (67.7%) | N / A | N / A |
| Changing professional clothes every day | 59/127 (46.5%) | ||||
| All staff* | Wearing professional clothes washable at 60°C | 91/127 (71.7%) | |||
| Changes professional clothes every day | 52/127 (40.9%) | ||||
| No specific measures | 6/127 (4.7%) | ||||
| Measures targeting patients | n/N (%) | n/N (%) | p-value | ||
| Isolation of patients presenting with respiratory symptoms | Separation within the same waiting area | 6/127 (4.7%) | 8/122 (6.6%) | 0.517 | |
| Isolation in a separate room | 115/127 (90.6%) | 80/122 (65.6%) | <0.001 | ||
| None | 5/127 (3.9%) | 34/122 (27.9%) | <0.001 | ||
| Unknown | 1/127 (0.8%) | 0 | N / A | ||
| Minimum patient distancing in waiting room | ≥1.5 meters | 76/127 (59.8%) | N / A | N / A | |
| <1.5 meters | Total | 51/127 (40.2%) | |||
| 0 - 0.5 meter | 6/127 (4.7%) | ||||
| 0.5 – 1 meter | 12/127 (9.4%) | ||||
| 1 – 1.5 meters | 33/127 (26%) | ||||
| Alcohol-based disinfection solution | Availability (2021: at desk; 2019: any location) | Not available | 6/125 (4.8%) | 45/121 (37.2%) | <0.001 |
| During influenza epidemic season | 6/125 (4.8%) | 13/121 (10.7%) | 0.083 | ||
| All year round | 113/125 (90.4%) | 63/121 (52.1%) | <0.001 | ||
| Protective masks for patients | Availability (2021: at desk; 2019: any location) | Not available | 25/127 (19.7%) | 63/120 (52.5%) | N / A |
| During influenza epidemic season | N / A | 34/120 (28.3%) | |||
| All year round | N / A | 23/120 (19.2%) | |||
| Currently | 100/127 (78.7%) | N / A | |||
| Unknown | 2/127 (1.6%) | 0 | |||
| Condition of access * | Respiratory symptoms | 19/127 (15.0%) | 52/122 (42.6%) | <0.001 | |
| Freely | 9/127 (7.1%) | 24/122 (19.7%) | 0.003 | ||
| If no mask already | 108/127 (85.0%) | N / A | N / A | ||
| Other | 8/127 (6.3%) | 46/122 (37.7%) | <0.001 | ||
| Air humidifier in the consultation room | Yes | 4/127(3.1%) | 9/122 (7.4%) | 0.102 | |
| No | 116/127(91.3%) | 110/122 (90.2%) | 0.765 | ||
| Unknown | 7/127 (5.5%) | 3/122 (2.5%) | N / A | ||
N / A: not applicable or not assessed; * multiple answers possible.
Ventilation daily or more, often by opening the windows, was done in 85.4% of practices in waiting rooms and in 89.0% of practices in consultation rooms. Ventilating between each patient was done by 38.6% of practices (table 3).
Table 3Ventilation and cleaning frequency of various areas in the Sentinella network in 2021 and 2019 (127 and 122 answering practices, respectively).
| Ventilation | 2021 | 2019 | p-value | |
| n/N (%) | n/N (%) | |||
| Waiting room | <1x/week | 5/123 (4.1%) | 8/115 (7.0%) | 0.328 |
| 1x/week | 1/123 (0.8%) | 7/115 (6.1%) | 0.024 | |
| ≥1x/week but <1x/day | 12/123 (9.8%) | 36 / 115 (31.3%) | <0.001 | |
| ≥1x/day° | 105/123 (85.4%) | 64/115 (55.7%) | <0.001 | |
| Consultation room | <1x/week | 3/127 (2.4%) | 8/120 (6.7%) | 0.103 |
| 1x/week | 0 | 6/120 (5.0%) | 0.011 | |
| ≥1x/week but <1x/day | 11/127 (8.7%) | 30/120 (25.0%) | <0.001 | |
| ≥1x/day° | 113/127 (89.0%) | 76/120 (6.3%) | <0.001 | |
| Cleaning | n/N (%) | n/N (%) | p-value | |
| Waiting room | <1x/week | 4/123 (3.3%) | 6/117 (5.1%) | 0.487 |
| 1x/week | 3/123 (2.4%) | 33/117 (28.2%) | <0.001 | |
| ≥1x/week but <1x/day | 13/123 (10.6%) | 39/117 (33.3%) | <0.001 | |
| ≥1x/day° | 103/123 (83.7%) | 39/117 (33.3%) | <0.001 | |
| Consultation room | <1x/week | 1/126 (0.8%) | 5/120 (4.2%) | 0.086 |
| 1x/week | 3/126 (2.4%) | 21/120 (17.5%) | <0.001 | |
| ≥1x/week but <1x/day | 12/126 (9.5%) | 35/120 (29.2%) | <0.001 | |
| ≥1x/day° | 110/126 (87.3%) | 59/120 (49.2%) | <0.001 | |
| Consultation bed | <1x/week | 1/124 (0.8%) | 2/119 (1.7%) | 0.525 |
| 1x/week | 1/124 (0.8%) | 7/119 (5.9%) | 0.025 | |
| ≥1x/week but <1x/day | 3/124 (2.4%) | 20/119 (16.8%) | <0.001 | |
| ≥1x/day° | 119/124 (96.0%) | 90/119 (75.6%) | <0.001 | |
| Patients' toilet | <1x/week | 2/122 (1.6%) | N / A | N / A |
| 1x/week | 3/122 (2.5%) | |||
| ≥1x/week but <1x/day | 13/122 (10.7%) | |||
| ≥1x/day° | 104/122 (85.2%) | |||
N / A: not applicable or not assessed; ° includes “at least once hourly” and “between each patient” in 2021
Cleaning of surfaces between patients was performed at least once daily or after each patient: for the furniture in the waiting room (83.7% and 9.4%, respectively), for the furniture in the consultation room (87.3% and 27.8%), for the consultation bed (96.0% and 53.1%), and for toilets used by patients (85.2% and 2.5%) as seen in table 3.
A recommendation to wear a medical face mask at all times at work was in place (93.7%, table 2) in 2021. Hand hygiene by washing or using an alcohol-based disinfection solution was done by physicians before performing a medical act (95.3%) or patient examination (88.2%), after examining a patient (95.3%) and upon arriving at (85.8%) or leaving (77.2%) the practice (table 4).
Table 4Hand hygiene of reporting physician in the Sentinella network in 2021 and 2019 (127 and 122 answering practices, respectively).
| Situation | Method | 2021 | 2019 | p-value |
| n (%) | n (%) | |||
| Upon arrival | Soap* | 88 (69.3%) | 65 (53,3%) | 0.009 |
| Alcohol* | 76 (59.8%) | 44 (36,1%) | <0.001 | |
| Either or both | 109 (85.8%) | 78 (63,9%) | <0.001 | |
| When leaving | Soap* | 83 (65.4%) | 74 (60.7%) | 0.443 |
| Alcohol* | 72 (56.7%) | 46 (37.7%) | 0.003 | |
| Either or both | 98 (77.2%) | 83 (68.0%) | 0.106 | |
| Before examining | Soap* | 35 (27.6%) | 34 (27.9%) | 0.956 |
| Alcohol* | 106 (83.5%) | 81 (66.4%) | 0.002 | |
| Either or both | 112 (88.2%) | 91 (74.6%) | 0.006 | |
| After examining | Soap* | 63 (49.6%) | 68 (55.7%) | 0.333 |
| Alcohol* | 107 (84.3%) | 97 (79.5%) | 0.331 | |
| Either or both | 121 (95.3%) | 110 (90.2%) | 0.119 | |
| Before medical procedure | Soap* | 73 (57.5%) | 73 (59.8%) | 0.706 |
| Alcohol* | 115 (90.6%) | 94 (77.0%) | 0.004 | |
| Either or both | 121 (95.3%) | 112 (91.8%) | 0.264 | |
| After the toilet | Soap* | 115 (90.6%) | N / A | N / A |
| Alcohol* | 68 (53.5%) | |||
| Either or both | 120 (94.5%) | |||
| Other | Soap* | 41 (32.3%) | 28 (23.0%) | 0.100 |
| Alcohol* | 30 (23.6%) | 22 (18.0%) | 0.278 | |
| Either or both | 49 (38.6%) | 34 (27.9%) | 0.073 |
Alcohol: alcohol-based disinfection; N / A: Not applicable or not assessed; Soap: hand washing with soap; * multiple answers possible
Professional clothing washable at 60°C was used by all the staff in 71.7% of practices, 40.9% changing these clothes every day. In 4.7% of cases, practices declared no specific professional clothing-related measures (table 2).
At the time of the survey, SARS-CoV-2 vaccine had been administered to 51.3% of the answering physicians, with 89.5% of the unvaccinated intending to become vaccinated. In the comments sections of the survey, several physicians noted that at the time of the survey they did not yet have access to the SARS-CoV-2 virus vaccine because they were not considered a high-risk population or had already contracted the virus. Vaccination coverage rate in the practice of at least 81% was attained for 32.2% of physicians, 11.0% of medical assistants and 5.4% of other staff (suppl. material table S1).
Patients were asked to perform hand hygiene measures by the practices providing alcohol-based disinfection solution dispensers all year around at the entry desk (90.4%) and/or in the waiting room (53.6%). Compliance with the legal obligation of mask-wearing in public places was supported by practices making medical masks available at the desk (78.7%), or directly to the patient if the patient was without a mask (85.0%) (table 2).
Specific measures were implemented for the management of patients with suspected COVID-19. Specific consultation timeslots were allocated (61.6%). Further, 10.4% of practices systematically redirected patients suspected of having COVID-19, and nasopharyngeal swabs could be performed by 92.0% of practices using additional protective measures, including wearing gloves (82.7%), ventilating for 5 minutes after having performed a nasal swab (74.0%), providing a dedicated room for swabbing (73.2%), wearing protective glasses (68.5%), wearing single-use gowns (55.1%) and wearing FFP2 masks (53.5%).
Practice settings and practitioners were comparable in the 2019 and 2021 surveys (table 1). The median year of setting up a practice shifted from 1999 in 2019 to 2008 in 2021 (p = 0.014). When comparing results of 2021 to 2019, we observed that hand hygiene improved in 2021 (p <0.010, table 4) through alcohol-based disinfection solution being provided more widely to patients (table 2) and by staff improving their hand hygiene practices on arriving at and leaving the practice, before examining a patient and while performing a medical procedure (table 4). In addition, mask wearing recommendations were enhanced (table 2) in 2021 for staff when caring for patients (p = 0.004) leading to mask wearing by staff becoming almost systematic (93.7% always in 2021 vs 41.0% in case of respiratory symptoms in 2019) and masks for patients being made more available (at least 78.7% in 2021 vs 47.5% in 2019). Ventilation and cleaning frequencies in all practice areas significantly improved (p <0.001, table 3). Physical distancing of symptomatic patients became more common (p <0.001, table 2) and the impracticability of isolating patients presenting with respiratory symptoms decreased to 3.9% in 2021 from 27.9% in 2019 (table 2). New habits emerged, such as distancing waiting room chairs (59.8% >1.5 m, table 2), allocating COVID-19 patients a specific timeslot (61.6%), or redirecting them to other specialised centres (10.4%), as well as specific measures for performing nasopharyngeal swabs..
Pairwise comparison of the 72 practices who answered both the 2019 and the 2021 give similar results (supplementary tables S2–S5).
The COVID-19 pandemic brought a change in the adherence to IPC measures between 2019 and 2021 in the Swiss primary care setting. In practices with comparable characteristics, IPC measures specifically directed at staff and patients were seen to improve significantly from 2019 to 2021: mask wearing became almost systematic for the staff and masks were made more easily available to patients; alcohol-based disinfection solution was provided more consistently to patients and staff improved their hand hygiene practice, especially on arrival at work; isolation of patients with respiratory symptoms in a separate room increased drastically; ventilation of waiting rooms and cleaning frequency of all areas improved significantly. In addition, the COVID-19 pandemic brought new IPC changes such as distancing between waiting room chairs, patients with COVID-19 receiving set timeslots or being redirected to other centres, and specific measures for performing nasopharyngeal swabs.
These changes were probably introduced after introduction of a mandatory national protection plan and sanctions in cases of noncompliance as part of a special COVID-19 ordinance [12]. Also, the modifications concerning protection measures were aimed not only at practices but at the society in general. Moreover, awareness of healthcare staff vulnerability and infection risk in the overall population increased in this period of time. These changes probably had a beneficial impact, not only on COVID-19 transmission rates within practices, but also on other respiratory illnesses as shown by the influenza epidemic threshold never being reached in the 2020–2021 cold season [18].
Although infection prevention improved, our study revealed that some recommendations, such as distancing in waiting rooms and providing masks to patients not wearing one, were not universally implemented. Some of these diversions from recommendations might have been caused by structural limitations, for example the available waiting room space. On the other hand, IPC measures in practices might have been reinforced by increased protective behaviour by the Swiss population at the time of our study, with, between the 1 March and 4 May 2021, 86.06% to 93.08% of Swiss wearing personal protective masks whenever the recommended 1.5 m distancing could not be kept [19]. Vaccination was still an issue in the spring of 2021; at that time, access to SARS-CoV-2 vaccination was limited to a particular segment of the Swiss population, namely people vulnerable due to age or health conditions, or hospital professionals. In this context, responding physicians seemed willing to get vaccinated against COVID-19 and expressed frustration at not being considered among the priority groups. By contrast, auxiliary staff were less inclined to be vaccinated [20].
Multiple factors contribute to adherence of healthcare workers to IPC guidelines, such as workplace culture, understanding of the proposed measures and confidence in the guidelines themselves [21]. A better national and international coordination regarding guidelines and access to IPC measures could lead to greater effectiveness.
There are some limitations of the current study. First, Sentinella practices are not strictly representative of all Swiss practices and may have a special interest in infectious diseases, making them more aware of and willing to implement IPC. We are however confident that the observed changes can be extrapolated to most practices in the country and beyond, considering that age, gender and regional distribution of Sentinella members are comparable to characteristics of Swiss primary physicians as per national statistics (Raphael Rytz, FOPH, personal communication). Second, the lack of data on some items from the 2019 survey limits a direct comparison between the two surveys. Third, the composition of the surveillance network has evolved, with a slight increase in number of members between 2019 and 2021.Some of the observed differences between 2019 and 2021 may thus be attributed to the fact 43.3% were not the same responding practices. Caution should always be advised when interpreting comparisons with historical data as other factors may have caused the differences. However, one cannot deny that the COVID-19 pandemic was the main driver of change in healthcare practice in this period.
In conclusion, the COVID-19 pandemic was a catalyst for important advances in primary care adherence to the recommended IPC measures.
Based on our results, we would advocate maintaining and regularly updating protection plans for primary care settings. Whether the observed changes will persist after the current pandemic should be the object of further research. In addition, we suggest that primary care settings should be involved in preparedness planning.
We acknowledge the contributions of Raphael Rytz from the Federal Office of Public Health in communicating the study information to the Sentinella members and transmitting the data to the investigators.
We thank all the physicians and staff of Sentinella for collecting and reporting the data and members of the Sentinella program commission for reviewing the questionnaire.
We thank Melanie Price Hirt for English editing.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors; the authors remain independent of any funding influence and declare no support from any organization for the submitted work.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. Apart from their above-disclosed institutional membership, no potential conflict of interest was disclosed.
1. Peytremann A , Senn N , Mueller Y . Infection prevention and control measures in practices of the Swiss sentinel network during seasonal influenza epidemics. J Hosp Infect. 2020 Dec;106(4):786–92. https://doi.org/10.1016/j.jhin.2020.08.026
2. Suter P , Kermode T , Clair C , Mueller Y , Senn N . Preventive and protective measures reducing influenza transmission in general practice: a systematic review. BJGP Open. 2019;3(3). Epub 2019/10/04. doi: https://doi.org/https://doi.org/10.3399/bjgpopen19X101657. PubMed PMID: 31581114; PubMed Central PMCID: PMCPMC6970581.
3. Mohr NM , Harland KK , Krishnadasan A , Eyck PT , Mower WR , Willey J , et al. Diagnosed and Undiagnosed COVID-19 in US Emergency Department Health Care Personnel: A Cross-sectional Analysis. Ann Emerg Med. 2021;78(1):27-34. Epub 2021/03/28. doi: https://doi.org/https://doi.org/10.1016/j.annemergmed.2020.12.007. PubMed PMID: 33771413; PubMed Central PMCID: PMCPMC7746085.
4. Müller Chabloz Y , Haller-Hester D , Ziegler L . Surveillance épidémiologique du covid-19: stratégie sentinella vs coronella. Rev Med Suisse. 2020 May;16(695):1123. Available from: https://www.revmed.ch/revue-medicale-suisse/2020/revue-medicale-suisse-695/surveillance-epidemiologique-du-covid-19-strategie-sentinella-vs-coronella https://doi.org/10.53738/REVMED.2020.16.695.1123
5. Mathys P . ali. e. 5e édition actualisée : janvier 2018. OFCL, Diffusion des publications fédérales. 2018. Available from: https://www.publicationsfederales.admin.ch
6. Sotomayor-Castillo C , Nahidi S , Li C , Hespe C , Burns PL , Shaban RZ . General practitioners' knowledge, preparedness, and experiences of managing COVID-19 in Australia. Infect Dis Health. 2021;26(3):166-72. Epub 2021/03/08. doi: https://doi.org/https://doi.org/10.1016/j.idh.2021.01.004. PubMed PMID: 33676878; PubMed Central PMCID: PMCPMC7891055.
7. Buitrago-Garcia D , Egli-Gany D , Counotte MJ , Hossmann S , Imeri H , Ipekci AM , et al. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: A living systematic review and meta-analysis. PLoS Med. 2020;17(9):e1003346. Epub 2020/09/23. doi: https://doi.org/https://doi.org/10.1371/journal.pmed.1003346. PubMed PMID: 32960881; PubMed Central PMCID: PMCPMC7508369.
8. Kronbichler A , Kresse D , Yoon S , Lee KH , Effenberger M , Shin JI . Asymptomatic patients as a source of COVID-19 infections: A systematic review and meta-analysis. Int J Infect Dis. 2020;98:180-6. Epub 2020/06/21. doi: https://doi.org/https://doi.org/10.1016/j.ijid.2020.06.052. PubMed PMID: 32562846; PubMed Central PMCID: PMCPMC7832751.
9. European Centre for Disease Prevention and Control . COVID-19 infection prevention and control measures for primary care, including general practitioner practices, dental clinics and pharmacy settings: first update. ECDC: Stockholm. 2020. Available from: https://www.ecdc.europa.eu/en/publications-data/covid-19-infection-prevention-and-control-primary-care
10. CDC . Non-Hospital Settings and COVID-19: Centers for Disease Control and Prevention; [02.04.2021]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/guidance-hcf.html#outpatient-ambulatory
11. COVID-19: plan de protection de la FMH pour l’exploitation des cabinets médicaux - État au 3 novembre 2020. FMH. 2020. Available from: https://www.fmh.ch/
12. Ordonnance 3 sur les mesures destinées à lutter contre le coronavirus (COVID-19) du 19 juin 2020 (Etat le 1er mars 2021). Fedlex (online). 2021. Available from: https://fedlex.data.admin.ch/eli/cc/2020/438
13. Wee LEI , Conceicao EP , Tan JY , Magesparan KD , Amin IBM , Ismail BBS , et al. Unintended consequences of infection prevention and control measures during COVID-19 pandemic. Am J Infect Control. 2021;49(4):469-77. Epub 2020/11/07. doi: https://doi.org/https://doi.org/10.1016/j.ajic.2020.10.019. PubMed PMID: 33157180; PubMed Central PMCID: PMCPMC7610096.
14. Grippe saisonnière de l’hiver 2020/2021: L’essentiel sur la vaccination durant la pandémie de COVID-19. OFSP-Bulletin 40/20: Département fédéral de l’intérieur DFI, Office fédéral de la santé publique OFSP, Unité de direction Santé publique. 2021. Available from: https://www.bag.admin.ch/bag/fr/home/krankheiten/krankheiten-im-ueberblick/grippe.html#dokumente__content_bag_fr_home_krankheiten_krankheiten-im-ueberblick_grippe_jcr_content_par_tabs
15. Savoy M , Haller DM , Rytz R , Mueller Y . Gestion de la crise dans les cabinets de médecins du réseau Sentinella selon une étude observationnelle COVID-19 et téléconsultations. Prim Hosp Care Med Int Gen. 2021;21(02):41–5. https://doi.org/10.4414/phc-f.2021.10335
16. Peters A , Borzykowski T , Tartari E , Kilpatrick C , Mai SH , Allegranzi B , et al. “Clean care for all-it’s in your hands”: the May 5th, 2019 World Health Organization SAVE LIVES: Clean Your Hands campaign. Antimicrob Resist Infect Control. 2019 Apr;8(1):64. https://doi.org/10.1186/s13756-019-0513-7
17. Müller Y , Rytz R , Lehman I , Peytremann A , Price HM . Infection prevention and control measures implemented in Sentinella practices in 2019 and 2021. Center for Primary Care and Public Health (Unisanté), University of Lausanne, Switzerland. Version 1.0 of the licensed dataset (January 2022), provided by the Unisanté Research Data Repository. doi: https://doi.org/https://doi.org/10.16909/dataset/29
18. Adlhoch C , Mook P , Lamb F , Ferland L , Melidou A , Amato-Gauci AJ , et al. Very little influenza in the WHO European Region during the 2020/21 season, weeks 40 2020 to 8 2021. Euro Surveill. 2021;26(11). Epub 2021/03/20. doi: https://doi.org/https://doi.org/10.2807/1560-7917.Es.2021.26.11.2100221. PubMed PMID: 33739256; PubMed Central PMCID: PMCPMC7976381. https://doi.org/10.2807/1560-7917.ES.2021.26.11.2100221
19. Friemel TN , Geber S , Eisenegger M , Vogler D . Covid-Norms. Monitoring and Analyzing Preventive Behavior. University of Zurich. 2021. Available from: https://covid-norms.ch
20. Hermann M . COVID-19-Prävention: Informationsstand, Einstellungen und Verhalten In: AG SD, editor. 2021. p. 24. Available from: https://sotomo.ch/site/wp-content/uploads/2021/07/Bericht-Wirkungsmessung-BAG-Juni.pdf
21. Houghton C , Meskell P , Delaney H , Smalle M , Glenton C , Booth A , et al. Barriers and facilitators to healthcare workers' adherence with infection prevention and control (IPC) guidelines for respiratory infectious diseases: a rapid qualitative evidence synthesis. Cochrane Database Syst Rev. 2020;4(4):Cd013582. Epub 2020/04/22. doi: https://doi.org/https://doi.org/10.1002/14651858.Cd013582. PubMed PMID: 32315451; PubMed Central PMCID: PMCPMC7173761. https://doi.org/10.1002/14651858.CD013582
Table S1SARS-CoV-2 vaccination and vaccination intention in Sentinella network practices in 2021 (127 answering practices).
| Vaccination of reporting physician | 2021 | ||
| n/N (%) | |||
| Done | 60/117 (51.3%) | ||
| Intended | 51/117 (43.6%) | ||
| Not intended | 1/117 (0.8%) | ||
| Undecided | 5/117 (4.3%) | ||
| Vaccination of staff | n/N (%) | ||
| Estimated rate of vaccination | physicians | 0–20% | 61/118 (51.7%) |
| 21–40% | 5/118 (4.2%) | ||
| 41–60% | 11/118 (9.3%) | ||
| 61–80% | 3/118 (2.5%) | ||
| 81–100% | 38/118 (32.2%) | ||
| medical assistants | 0–20% | 89/118 (75.4%) | |
| 21–40% | 5/118 (4.2%) | ||
| 41–60% | 4/118 (3.4%) | ||
| 61–80% | 7/118 (5.9%) | ||
| 81–100% | 13/118 (11.0%) | ||
| other staff | 0–20% | 84/95 (88.4%) | |
| 21–40% | 2/95 (2.1%) | ||
| 41–60% | 0 | ||
| 61–80% | 4/95 (4.2%) | ||
| 81–100% | 5/95 (5.3%) | ||
| Estimated rate of intention to vaccinate | physicians | 0–20% | 3/113 (2.7%) |
| 21–40% | 5/113 (4.4%) | ||
| 41–60% | 11/113 (9.7%) | ||
| 61–80% | 11/113 (9.7%) | ||
| 81–100% | 83/113 (73.5%) | ||
| medical assistants | 0–20% | 16/112 (14.3%) | |
| 21–40% | 14/112 (12.5%) | ||
| 41–60% | 15/112 (13.4%) | ||
| 61–80% | 22/112 (19.6%) | ||
| 81–100% | 45/112 (40.2%) | ||
| other staff | 0–20% | 22/76 (28.9%) | |
| 21–40% | 6/76 (7.9%) | ||
| 41–60% | 14/76 (18.4%) | ||
| 61–80% | 7/76 (9.2%) | ||
| 81–100% | 27/76 (35.5%) | ||
Table S2Characteristics of Sentinella network practices with data for both 2021 and 2019 surveys (72 answering practices). Paired analysis with p-values from exact McNemar test (proportions) and Wilcoxon signed rank test (counts or ordinal).
| Specialties represented in the practice (at least 1 specialist per practice) | 2021 | 2019 | p-value | |
| n (%) | n (%) | |||
| General practice | 64 (88.9%) | 63 (87.5%) | 1.000 | |
| Paediatrics | 10 (13.9%) | 11 (15.3%) | 1.000 | |
| Other specialties | 11 (15.3%) | 13 (18.1%) | 0.727 | |
| Number of staff per category | median (25–75%) | median (25–75%) | p-value | |
| Physicians | Total | 2 (1–4) | 2 (1–3) | 0.439 |
| Half-days of consultation per week per physician | 8.0 (6.0–9.0) | 7.4 (5.3–9) | 0.058 | |
| Other staff | Total | 4 (3 - 7) | 4 (2 - 7) | 0.345 |
| Full-time equivalents | 2.2 (1.2 - 4.8) | 2.6 (1.5 - 4.0) | 0.551 | |
| Physical characteristics: | median, n (25–75%), (%) | median, n (25–75%), (%) | p-value | |
| Year of setting up practice | 2004 (1995–2011) | 2004 (1992–2012) | 0.978 | |
| Number of rooms | Total | 7 (6–11) | 7 (6–10) | 0.154 |
| Number of consultation rooms | 3 (2–4) | 3 (2–4) | 0.951 | |
| waiting rooms | 1 (1–1.5) | 1 (1–1) | 0.012 | |
| Continuous ventilation (2019 and 2021: 3 missing values) | 19 (27.5%) | 12 (17.4%) | 0.092 | |
* multiple answers possible
Table S3Infection prevention and control measures in the Sentinella network with data for both 2021 and 2019 surveys (72 answering practices). Paired analysis with p-values from exact McNemar test (proportions) and Wilcoxon signed rank test (counts or ordinal).
| Measures targeting staff | 2021 | 2019 | p-value | |
| n (%) | n (%) | |||
| Alcohol-based disinfection solution for staff (miss.:1) | Not available | 1 (1.4%) | 0 | 1.000 |
| All year round | 70 (98.6%) | 71 (100%) | ||
| Protective mask wearing for staff * | In the case of respiratory symptoms | 0 | 28 (38.9%) | <0.001 |
| If not vaccinated against influenza | 2 (2.8%) | 6 (8.3%) | 0.289 | |
| During care to patients | 2 (2.8%) | 7 (9.7%) | 0.180 | |
| No specific recommendation | 1 (1.4%) | 43 (59.7%) | <0.001 | |
| Measures targeting patients | n (%) | n (%) | p-value | |
| Isolation of patients presenting with respiratory symptoms (miss.: 1) | Separation within the same waiting area | 5 (7%) | 4 (5.6%) | <0.001 |
| Isolation in a separate room | 62 (87.3%) | 47 (66.2%) | ||
| None | 4 (5.6%) | 20 (28.2%) | ||
| Condition of access for protective masks for patients * | In the case of respiratory symptoms | 12 (16.7%) | 33 (45.8%) | <0.001 |
| Freely accessible | 6 (8.3%) | 12 (16.7%) | 0.210 | |
| Given if no mask already | 60 (83.3%) | N / A | N / A | |
| Other | 5 (6.9%) | 28 (38.9%) | <0.001 | |
| Presence of air humidifier in the consultation room (miss.:3) | 4 (5.8%) | 5 (7.3%) | 1.000 | |
miss.: number of missing answers; N / A: Not applicable or not assessed; * multiple answers possible
Table S4Ventilation and cleaning frequency of various areas in the Sentinella network with data for both 2021 and 2019 surveys (72 answering practices). Paired analysis with p-values from exact Mc-Nemar test (proportions) and Wilcoxon signed rank test (counts or ordinal).
| Ventilation | 2021 | 2019 | p-value | |
| n (%) | n (%) | |||
| Waiting room (miss.:4) | <1x/week | 3 (4.4%) | 4 (5.9%) | <0.001 |
| 1x/week | 1 (1.5%) | 5 (7.4%) | ||
| ≥1x/week but <1x/day | 8 (11.8%) | 19 (27.9%) | ||
| ≥1x/day° | 56 (82.4%) | 40 (58.8%) | ||
| Consultation room | <1x/week | 1 (1.4%) | 3 (4.2%) | <0.001 |
| 1x/week | 0 | 5 (6.9%) | ||
| ≥1x/week but <1x/day | 7 (9.7%) | 15 (20.8%) | ||
| ≥1x/day° | 64 (88.9%) | 49 (68.1%) | ||
| Cleaning | n (%) | n (%) | p-value | |
| Waiting room(miss.:4) | <1x/week | 0 | 0 | <0.001 |
| 1x/week | 3 (4.4%) | 3 (4.4%) | ||
| ≥1x/week but <1x/day | 2 (2.9%) | 20 (29.4%) | ||
| ≥1x/day° | 63 (82.7%) | 45 (66.2%) | ||
| Consultation room(miss.:1) | <1x/week | 0 | 0 | <0.001 |
| 1x/week | 1 (1.4%) | 3 (4.2%) | ||
| ≥1x/week but <1x/day | 1 (1.4%) | 13 (18.3%) | ||
| ≥1x/day° | 69 (97.2%) | 55 (77.5%) | ||
| Consultation bed(miss.:3) | <1x/week | 0 | 0 | 0.375 |
| 1x/week | 1 (1.4%) | 0 | ||
| ≥1x/week but <1x/day | 1 (1.4%) | 6 (8.7%) | ||
| ≥1x/day° | 67 (97.1%) | 63 (91.3%) | ||
miss.: number of missing answers; N / A: Not applicable or not assessed; ° includes “at least once hourly” and “between each patient” in 2021
Table S5Hand hygiene measures in private practices of the Sentinella network with data for both 2021 and 2019 surveys (72 answering practices). Paired analysis with p-values from exact McNemar test (proportions) and Wilcoxon signed rank test (counts or ordinal).
| Situation | Method | 2021 | 2019 | p-value |
| n (%) | n (%) | |||
| Upon arrival | Soap* | 56 (77.8%) | 43 (59.7%) | 0.019 |
| Alcohol* | 39 (54.2%) | 29 (40.3%) | 0.087 | |
| Either or both | 62 (86.1%) | 51 (70.8%) | 0.007 | |
| When leaving | Soap* | 50 (69.4%) | 24 (33.3%) | 0.839 |
| Alcohol* | 36 (50.0%) | 27 (37.5%) | 0.163 | |
| Either or both | 55 (76.4%) | 50 (69.4%) | 0.359 | |
| Before examining | Soap* | 21 (29.2%) | 17 (23.6%) | 0.503 |
| Alcohol* | 62 (86.1%) | 49 (68.1%) | 0.001 | |
| Either or both | 65 (90.3%) | 56 (77.8%) | 0.023 | |
| After examining | Soap* | 41 (56.9%) | 39 (54.2%) | 0.839 |
| Alcohol* | 61 (84.7%) | 55 (76.4%) | 0.210 | |
| Either or both | 69 (90.3%) | 64 (88.9%) | 0.125 | |
| Before medical procedure | Soap* | 43 (59.7%) | 41 (56.9%) | 0.839 |
| Alcohol* | 66 (91.7%) | 56 (77.8%) | 0.013 | |
| Either or both | 68 (94.4%) | 66 (91.7%) | 0.727 | |
| Other° | Soap* | 67 (93.1%) | 15 (20.8%) | <0.001 |
| Alcohol* | 40 (55.6%) | 11 (15.3%) | <0.001 | |
| Either or both | 69 (95.8%) | 19 (26.4%) | <0.001 |
miss.: number of missing answers; *: multiple answers possible; °: In 2021, included explicitly washing or disinfecting hands in bathroom