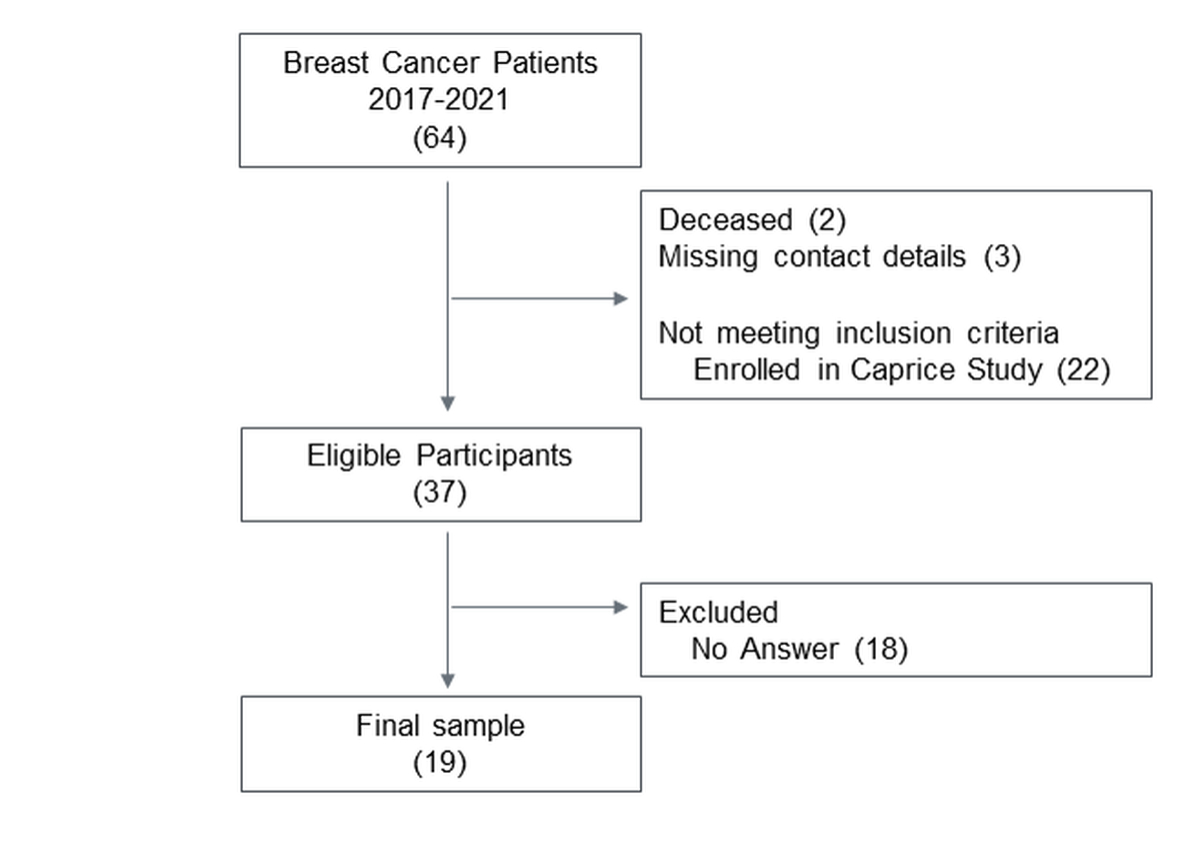
Figure 1 Patient flow diagram. Numbers in brackets indicates number of patients.
DOI: https://doi.org/10.4414/SMW.2022.w30155
Among women in Switzerland, breast cancer is the most common cancer type and accounts for nearly one in three new cancer cases and almost one in five cancer-related deaths. As a result of progress in prevention, early detection and treatment, the mortality rate has been declining in the last decades, consequently leading to an increase in the number of cancer survivors [1].
With the growing number of cancer survivors, there is a need to discuss the specific health problems that cancer survivors face as a result of the diagnosis, care and comorbid conditions [2]. One example of a common side effect of cancer treatment is cancer-related fatigue. In 25% of cancer survivors fatigue may persist even after cancer treatment has ended, making it difficult for them to return to work and live independently, hence having a severe impact on their quality of life not only during but also after treatment [3].
There is evidence suggesting that exercise for cancer patients is safe and effective in improving fatigue, quality of life, physical function and cardiorespiratory fitness both during and after cancer treatment [4, 5]. Comparing the effects of centre-based supervised, and home-based unsupervised exercise on quality of life and physical function, Buffart et al. (2017) found effects twice as large for supervised exercise [5]. Moreover, cancer patients have an increased risk of cardiovascular) disease, resulting from direct effects of cancer therapies and the accumulation of cardiovascular risk factors such as hypertension, smoking, the loss of cardiorespiratory fitness or weight gain [6]. To prevent and/or mitigate cardiovascular events, most developed countries, including Switzerland, offer structured supervised exercise as part of cardio-oncological rehabilitation programmes [6].
The positive effects of exercise in both supervised and unsupervised settings for cancer-specific health outcomes are evident [2]. Yet the majority of breast cancer survivors do not meet the physical activity recommendations of 150 min/week of moderate-to-vigorous aerobic exercise [7, 8]. Furthermore, activity levels of breast cancer survivors declined from 18 to 42 months after treatment [9]. Cancer survivors encounter a number of barriers that make it challenging to exercise. Understanding the barriers that limit, and facilitators that further exercise participation may help to curb the problem of low physical activity levels in cancer survivors [10]. In previous reviews, frequently reported facilitators included social support from peers, physical motivators such as improved physical fitness and the reduction of side effects, mental well-being and enjoyment of exercise [10, 11]. Previous studies in cancer patients identified physical and treatment-related barriers, psychological and motivation-related barriers and contextual, environmental or other life-related barriers [10–13]. The transition from supervised exercise to maintaining exercise participation in everyday life, according to a recent study, is a key obstacle for breast cancer survivors [14]. To date, data are lacking from Switzerland on barriers, facilitators and the transition from centre- to home-based exercise. Although previous studies have assessed barriers and facilitators, none of them addressed the difficulties that may arise with the transition from structured, supervised programmes to everyday life and no previous study evaluated strategies to overcome these obstacles.
The aim of the present study was to identify barriers, facilitators and strategies used to manage barriers of breast cancer survivors in Switzerland towards: (a) centre-based exercise within a cardio-oncological rehabilitation programme at a tertiary referral centre (University Hospital Bern) in Switzerland; and (b) home-based exercise during and after the completion of the centre-based exercise programme. The separate assessment of barriers to supervised exercise (centre-based) and unsupervised exercise (at home, outside or at another exercise facilities) will indicate which barriers may arise with this transition.
This study used a qualitative approach with thematic analysis of semi-structured telephone interviews [15]. Eligible candidates were contacted by mailed invitation letter (January to March 2021) asking them to participate in a telephone interview. Consenting patients were contacted by telephone to make an appointment for the telephone interview.
At the beginning of the interview, the participants were asked for consent to be audio-recorded. The questions about the facilitators, barriers and strategies to manage barriers were open-ended to encourage the flow of speech and not restrict participants to pre-formulated responses. The interviews were held in Swiss German to create a pleasant and natural atmosphere for the participants and lasted between 25 and 45 minutes.
Women with breast cancer diagnosis, aged 18 years and older who participated in the structured centre-based exercise programme at the Inselspital in Bern between January 2017 and March 2021 were eligible for this study. The current examination was conducted as a substudy of the Caprice study (NCT03850171), which is a randomised controlled trial assessing the importance of exercise therapy timing with regard to cardiotoxicity and patient preference in breast cancer and lymphoma patients. For this reason, we excluded women who were already enrolled in the Caprice study. Excluding Caprice study patients from the present study is unlikely to have introduced a bias in that it was determined mainly by the time period of enrolling into the rehabilitation programme, with patients enrolling after 2019 mostly volunteering for Caprice. Further, women, who had deceased according to the in-house clinical database or could not be contacted due to missing contact details were removed from the study.
The cardio-oncological rehabilitation programme is a 12-week ambulatory multidisciplinary programme, including 24 supervised exercise sessions, counselling on physical activity, psychosocial aspects, nutrition, cardiovascular risk factors, and pain management. The exercise training is offered twice weekly to groups of at most10 cancer patients with exercise sessions lasting 90 min, supervised by experienced exercise therapists. Sessions start with approximately 30–40 min of cycling on an ergometer at moderate intensity, increasing on a weekly basis if possible. After the cycling training, patients continue the exercise session with 45 min of strength, coordination and/or balance training. During the first COVID-19 lockdown in Switzerland (March to May 2020), training sessions at the centre were suspended. In June, group exercise sessions took place once a week in smaller groups and patients completed the second weekly training session at home. From July to September 2020, training sessions were offered twice weekly with up to 10 patients. From October 2020 to May 2021, group exercise sessions were replaced by individual sessions once weekly, which were scheduled according to patient preference and availability of the exercise therapists. The second exercise session was performed at home and supervised via an activity tracking device (Fitbit, San Francisco, USA).
Demographic and disease-specific characteristics of patients participating in the interview study were compared with those of patients not participating in the study by unpaired t-tests and Fisher’s exact test, as appropriate. The interviews were audio-recorded and transcribed verbatim according to the recommendations by Braun and Clarke for thematic analysis [15]. Swiss dialect was translated into Standard German. Patients’ answers were coded by assigning statements to an already existing code [15] or by generating a new code when needed to capture all answers. For each item coded, it was noted in which context the statement was made in order to later identify possible context-specific patterns and to compare the different contexts. Barriers and facilitators were specified according to exercise in the centre-based and in the home-based setting. Home-based exercise included any exercise outside the centre, e.g., at home, outdoors, in fitness centres, clubs or classes, organised by patients independently. A table was created to group statements according to their codes. After coding was applied to the transcripts of the first two interviews, the coding table was reviewed by a co-author, and disagreements in coding were discussed amongst four co-authors until agreement was reached. Then, codes allocated to at least two patients and used for related facilitators and barriers were grouped together to generate subthemes and themes. For the barriers, previously suggested categorisations by Hefferon et al. [13] and Courneya et al. [12] served as an orientation and were used when they fitted the answers of the patients.
Current physical activity recommendations for general health state that adults should engage in 150 min of moderate or 75 min of vigorous physical activity per week or an equivalent combination thereof [16]. Current physical activity levels of the participants were quantified using the global physical activity questionnaire (GPAQ) administered by telephone to calculate the proportion of patients fulfilling these guidelines. GPAQ data were analysed according to the analysis guide provided [17].
Of the 64 breast cancer patients who completed a structured, centre-based exercise programme during the screening period, 37 were eligible for this study and 19 patients consented to be interviewed (fig. 1).
Figure 1 Patient flow diagram. Numbers in brackets indicates number of patients.
Characteristics of the study population as well as the patients who did not participate in the study are shown in table 1. Baseline characteristics were defined according to studies presenting similar data [14, 18]. For the participating patients, there were no missing data. None of the characteristics of the study populations differed from the characteristics of the non-participating patients; however it should be noted that relatively few of the included women were on hormone treatment. In qualitative research, a common method to determine sample size is based on the achievement of data saturation. Since we did not obtain new information that added to the understanding of our categories in the last patient interviews, our sample consisting of 19 patients can be deemed sufficient for this type of exploratory analysis [19].
Table 1Characteristics of the study population.
| Total population (n = 64) | Study participants (n = 19) | Screened, non-participating patients (n = 45) | ||
| Demographic variables | Age (yrs) | 47.0 ± 11.2 | 48.9 ± 9.7 | 46.3 ± 11.8 |
| BMI (kg/m2 | 26.3 ± 5.1 | 25.5 ± 4.8 | ||
| Health-related variables | VO2 peak (ml/kg/min | 23.7 ± 7.0 | 23.9 ± 6.0 | |
| Work-related PA (min/week | 502 ± 634 | |||
| Transport-related PA (min/week | 92 ± 103 | |||
| Recreation-related PA (min/wk) | 312 ± 178 | |||
| Received cancer treatment | Chemotherapy | 53 (82.8) | 14 (73.7) | 39 (86.7) |
| Radiotherapy | 34 (53.1) | 14 (73.7) | 20 (44.4) | |
| Immune therapy | 10 (15.6) | 4 (21.1) | 6 (13.3) | |
| Hormone therapy | 24 (37.5) | 5 (26.3) | 19 (42.2) | |
| Breast cancer stage | Stage I | 14 (21.9) | 4 (21.1) | 10 (22.2) |
| Stage II | 33 (51.6.) | 10 (52.6) | 23 (51.1) | |
| Stage III | 14 (21.9) | 3 (15.8) | 11 (24.4) | |
| Stage IV | 2 (3.1) | 1 (5.3) | 1 (2.2) | |
| Exercise programme participation | Completion during cancer therapy | 23 (35.9) | 4 (21.1) | 19 (42.2) |
| Completion after cancer therapy | 41 (64.1) | 15 (78.9) | 26 (57.8) | |
| Duration of exercise programme (weeks) | 12.6 ± 3.3 | 12.5 ± 4.0 | 12.6 ± 3.0 | |
BMI: body mass index; PA: physical activity; VO2: oxygen consumption
Data are presented as mean ± standard deviation or number of patients (% of group).
The majority of the study participants (n = 15, 79%) attended the centre-based exercise programme after completion of their treatment (chemo- and/or radiotherapy), except for four women (21%), who completed the exercise programme during their cancer treatment. For the women who participated in the programme after their therapy, the average time between end of therapy and start of the programme was 6 months (range 0.5–48). The average duration of the exercise programme was 12.5 weeks with a range from 2 weeks (dropout from the programme) to 22 weeks. Nearly half of the participants (n = 9, 47%) completed the exercise programme during the COVID-19 pandemic, during which the programme had to be adapted as described in the methods.
According to data from the GPAQ [17], the study participants performed a total of 907 min ± standard deviation 677 min of physical activity per week. The total amount of physical activity consisted of three different domains, namely weekly work-related (502 ± 634 min), weekly transport-related with (92 ± 103 min, and weekly recreational-related with 312 ± 178 min. The average moderate-intensity recreational-related was 192 ± 169 min and the average vigorous-intensity recreational-related per week was 120 ± 92 min. All study participants fulfilled the current physical activity recommendations. Fifty-eight percent and 42% reported doing more or the same amount, respectively, of moderate-intensity physical activity than before their diagnosis; and 53% and 21% reported doing more or the same amount, respectively, of vigorous-intensity physical activity. Twenty-six percent of the interviewed women reported doing less vigorous-intensity physical activity than before their cancer diagnosis.
Facilitators could be grouped into four major themes, namely: (1) social support; (2) benefits of exercise on health status; (3) benefits of binding and structured exercise; and (4) enjoyment of exercise. The most commonly named facilitators for home-based exercise were the anticipated benefits of exercise to prevent the recurrence of breast cancer (32% of 19 patients), the motivation to improve current health status (32%) and the enjoyment of exercise (32%). The most frequently cited facilitators for centre-based exercise were fixed appointments (63%), improvements in physical fitness (53%) and explanations/support from a trained supervisor (53%).
Table 2Facilitators for exercise participation in home-based exercise and in centre-based exercise.
| Facilitator | Centre-based exercise (ECB) | Home-based exercise (EHB) | |
| S ocial support | 18 | 7 | |
| Peers | Positive group dynamics | 9 | 5 |
| Contact with people with the same illness | 7 | NA | |
| Therapist | Support from trained supervisor | 10 | 1 |
| Family/Friends | Support from family/ friends | NA | 3 |
| Benefits of exercise on health status | 12 | 15 | |
| Anticipated benefits | Prevent recurrence of breast cancer | NA | 6 |
| Motivation to improve current health status | NA | 6 | |
| Knowing that exercise is good for one’s health | 3 | 4 | |
| Exercising to maintain body weight | NA | 3 | |
| Exercising to stay vital in later life | NA | 3 | |
| Experienced benefits | Improvements in physical fitness | 10 | 4 |
| Good feeling from exercising | 1 | 9 | |
| Combating the after-effects of therapy | 3 | 5 | |
| Autonomy and mindfulness | NA | 3 | |
| Regain confidence in own body | 2 | NA | |
| Switch off from daily routine | 1 | 2 | |
| Benefits of binding and structured exercise | 15 | ||
| fixed appointment | 12 | NA | |
| regularity/routine | 4 | NA | |
| Programme as an initiator to start exercising | 4 | NA | |
| structured exercise with training schedule | 2 | NA | |
| Enjoyment of exercise | 7 | 7 | |
| Enjoyment of movement | 2 | 6 | |
| Intrinsic motivation | 2 | 2 | |
| Enjoying activities in the programme | 3 | NA | |
ECB: number of women reporting this facilitator exclusively for exercise in centre-based setting; EHB: number of women reporting this facilitator for home-based exercise (at home, outside or another exercise facility, organized by patients independently).
The theme social support was the most frequently named facilitator regarding centre-based exercise. Exercising as a group and the resulting group dynamic was found to be very motivating.
Some women explained that exercising in a group or arranging with other people to meet for sports has motivated them to maintain their physical activity also after completion of the centre-based exercise programme. Supportive friends and family were also mentioned as facilitators for exercise in general.
A main facilitator for centre-based exercise was the support from trained supervisors. The assistance of trained therapists and receiving specific information about exercising that was specific to people with a cancer diagnosis gave the women a feeling of safety and helped them to understand the benefits of exercise during their cancer journey.
Many women were motivated to improve their current health status. Their motivation originated both from positive outcome expectancies (the belief that exercise is effective in improving their health) as well as from positive outcome experiences (prior exercise participation has already had a positive effect on their health).
Many women explained that they really enjoyed being physically active and some women pointed out that they enjoyed the activities from the centre-based exercise programme, which motivated them to continue exercising.
This theme was reported exclusively for centre-based exercise. The majority of the women pointed out that exercise with a fixed appointment was a main facilitator for them to maintain their exercise participation during the centre-based programme. Other participants liked that the exercise programme gave them a daily structure and routine.
The reported barriers were grouped into three major themes, which are consistent with previous research [12, 13]. The barriers were categorised into physical barriers (treatment and non-treatment-related), psychological barriers and environmental barriers (natural, built and social environment). The most frequently named barriers for centre-based exercise were fatigue (26% of 19 patients), doctor’s appointments (21%) and work responsibilities (21%). The most common barriers for home-based exercise was lack of willpower/self-discipline (63%), fatigue (37%) and bad weather (32%).
Table 3Barriers toward exercise participation.
| Barriers | Centre-based | Home-based | |
| Physical barriers | |||
| Treatment-related | Fatigue | 5 | 7 |
| Pain | 2 | 2 | |
| Other side effects | NA | 2 | |
| Non-treatment-related | Injury / medical conditions | 3 | 2 |
| Psychological barriers | |||
| Lack of willpower | NA | 12 | |
| Exercise ‘not a priority’ | NA | 4 | |
| No-one to exercise with | NA | 3 | |
| Lack of time | 1 | 3 | |
| Enough activity elsewhere | NA | 3 | |
| Not being ‘the sporty type’ | NA | 2 | |
| Environmental barriers | |||
| Natural environment | Bad weather | NA | 6 |
| Built environment | Distance to rehab centre | 3 | NA |
| No space and equipment to exercise | NA | 2 | |
| Social environment | COVID- pandemic | NA | 4 |
| Work responsibilities | 3 | 2 | |
| Childcare duties | NA | 4 | |
| Doctor’s appointment | 4 | 1 | |
| Vacation | 3 | NA | |
| Irregular work hours | NA | 2 | |
The women reported both treatment-related (fatigue and/or pain) and non-treatment-related physical barriers (injuries and medical conditions) that prevented them from or made it more difficult to exercise. Fatigue was the most common treatment-related barrier.
Psychological barriers originated from the women’s lack of motivation or lack of volition (the successful pursuit of defined goals [20]). The most cited psychological barrier was the lack of willpower/self-discipline. This barrier was mentioned only in the context of home-based unsupervised exercise both during and after completion of the centre-based exercise programme.
This theme included barriers that originated from the natural, built and social environment that surround an individual. Specific to this study’s time period (year of 2020) were the barriers that arose owing to the COVID-19 pandemic. Because all sporting and fitness facilities were closed for several months, some women were not able to pursue their usual exercise activities and were forced to adapt their habits.
The comparison of barriers to exercise in the centre-based versus the home-based setting showed large differences with regard to psychological barriers, which were much greater for home-based exercise (fig. 2). Physical and environmental barriers regarding exercise in the home-based and centre-based setting were comparable.
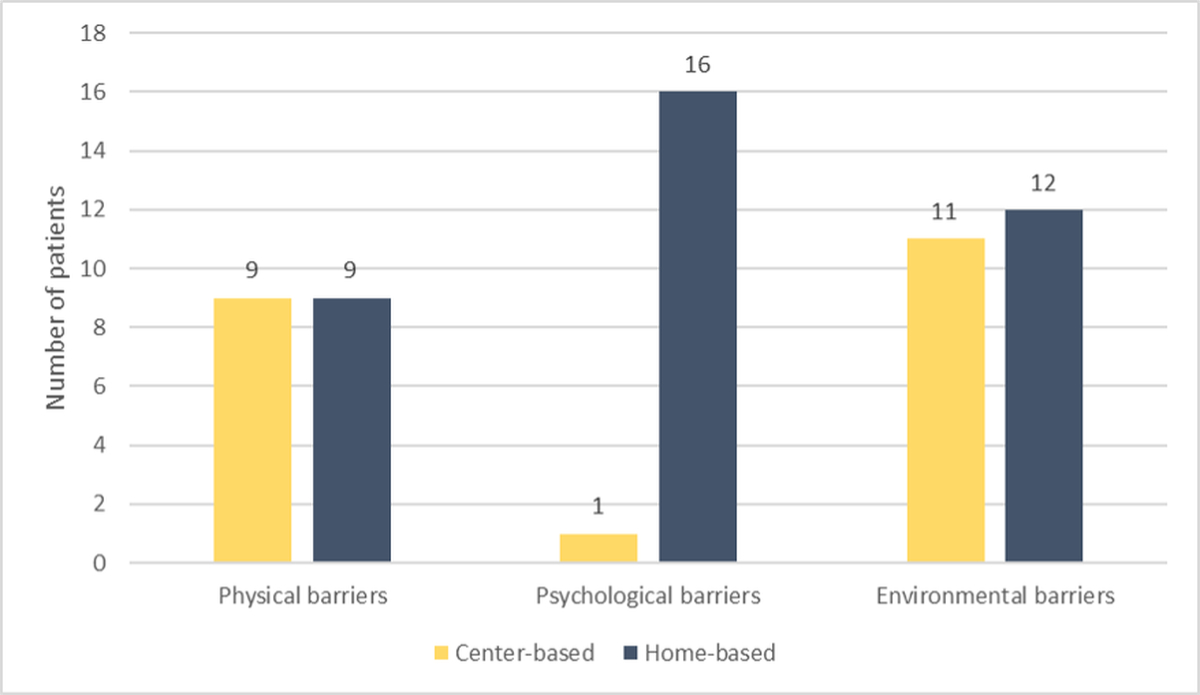
Figure 2 Comparison of barriers to centre- vs. home-based exercise training.
Strategies to overcome barriers to exercise training were grouped into three major themes, namely adaptation of training circumstances, behaviour change strategies and strategies to deal with side effects. The strategies used by the women to overcome or manage their barriers were highly individual (fig. 3), meaning that for one specific barrier many different strategies were named, whereas one specific strategy could be used against several different barriers. The two most frequently used strategies to manage or overcome barriers were planning the exercise sessions in advance (47%) and creating a commitment (37%). These strategies were mainly used against the psychological barrier lack of willpower/self-discipline. The common barrier fatigue was addressed with many different strategies, but most frequently by exercising at lower intensity or for a shorter duration (26%).
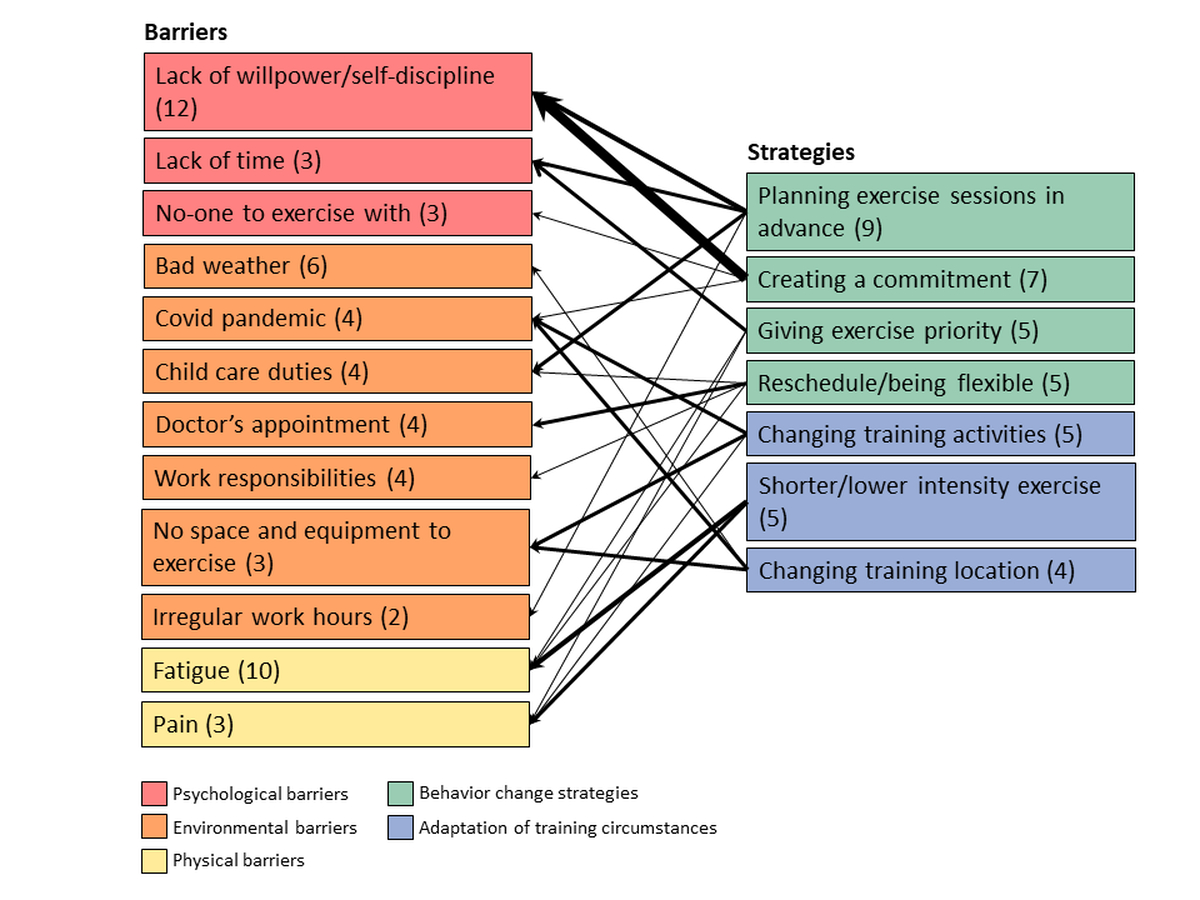
Figure 3 Frequently named strategies to overcome certain barriers, with number of patients reporting specific barriers and strategies indicated in brackets.
To overcome barriers, some women adapted their training circumstances by altering training modalities or by making exercise sessions more appealing. Some women changed their training activities or training location to address their barriers (e.g. pain, COVID pandemic, no space and equipment to exercise, bad weather). Women who struggled with the lack of willpower or the lack of an exercise partner tried to make their exercise sessions more appealing by distracting themselves with music or podcasts, or added a social component by arranging their exercise sessions with other people.
This theme included cognitive and behavioural strategies, which are part of common behaviour change models [21]. The women’s strategies were grouped into three subthemes: (1) prioritisation of exercise, (2) action planning, (3) action control and 4) coping planning.
To summarise the findings, figure 4 shows all the themes and subthemes that emerged from the content analysis and reflects their possible influence on exercise participation.
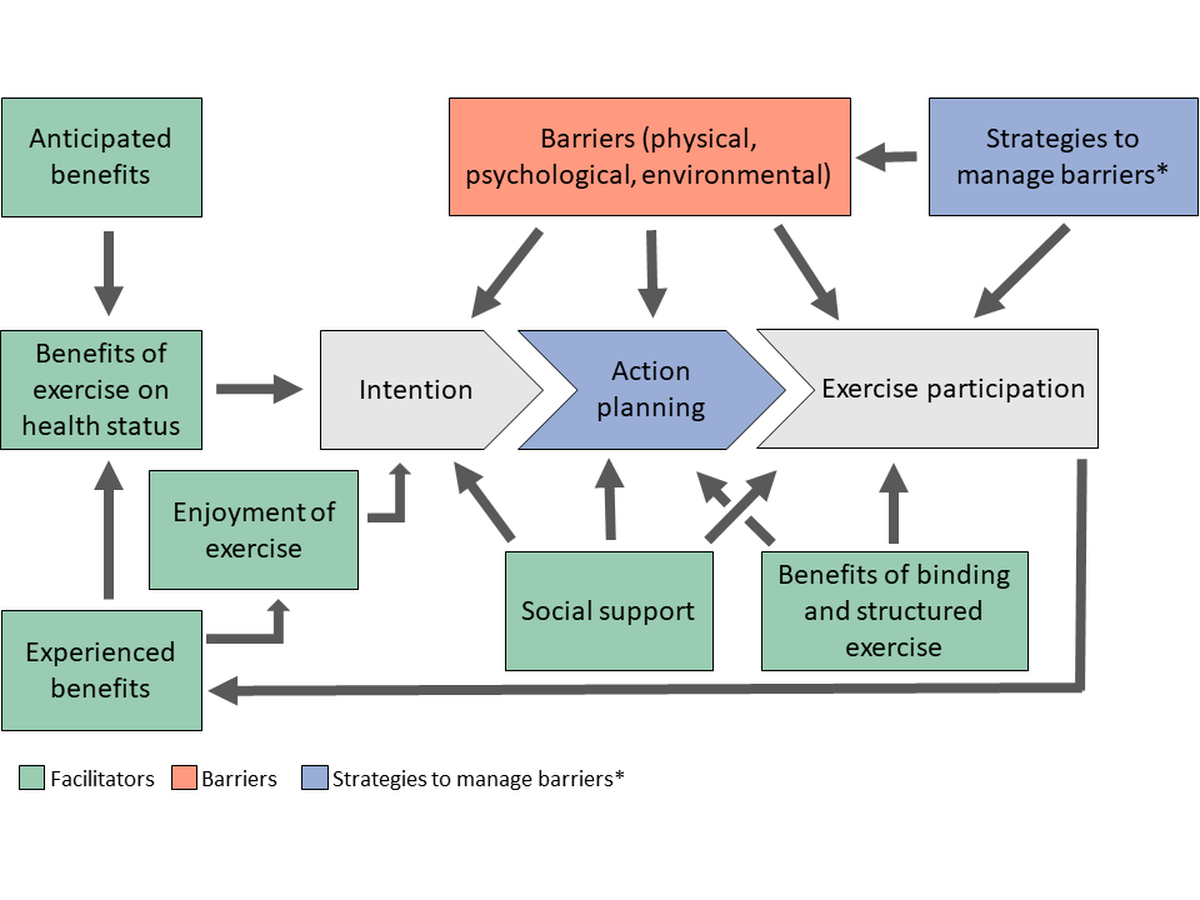
Figure 4 Overview of the emerged themes and their possible influence on exercise participation.
This is the first study in Switzerland identifying barriers, facilitators and strategies used to manage barriers of breast cancer survivors to exercise in (a) a supervised centre-based setting integrated into a cardio-oncological rehabilitation programme and (b) a self-organised home-based setting during and/or after the completion of the centre-based exercise programme. Main facilitators were social support, benefits of exercise on health status, enjoyment of exercise and benefits of binding and structured exercise. Barriers included physical, psychological and environmental barriers. Strategies to manage such barriers were adaptation of training settings, behaviour change strategies and strategies to deal with side effects of cancer therapy. There were more facilitators and fewer barriers to exercise participation in the centre-based than the home-based setting. These differences may contribute to understanding the difficulty of maintaining exercise participation beyond the duration of a rehabilitation programme and to providing targeted recommendations.
Facilitators for and barriers to engagement in a structured centre-based exercise programme reported in this study were similar to those described in previous studies from the US, Canada, Australia and the European Union [10, 11, 14, 22]. The benefits of exercise experienced, such as improvements in physical fitness and positive effects on mental well-being, were also the most important and commonly cited facilitators in the review by Clifford et al. [10]. Browall et al. [11] and Ferri et al. [14] also found improved social, physiological and psychological health to be highly valued benefits of physical activity by cancer patients. Several women in our study pointed out their enjoyment of exercising. Such positive affective states during exercising have been shown to improve adherence to physical activity in non-cancer populations [23, 24]. Hence, increasing positive affective states during the centre-based exercise programme may be an effective measure to positively influence the exercise behaviour of breast and probably other cancer survivors in the longer term.
Context-specific facilitators for supervised, centre-based exercise were social support from peers and trained therapists, the input by the therapists in the form of structured exercise, as well as the obligation to turn up to scheduled training sessions. The facilitating role of social support from other breast cancer patients and trained exercise therapists has been described in previous studies [11, 18, 25]. Yet only a few studies reported that making a commitment to scheduled exercise training sessions acts as a facilitator [26, 27]. In contrast, in our study almost two thirds of the patients (n = 12; 63%) stated that the commitment to participate in the centre-based exercise programme was a major facilitator. This commitment may be an important factor in preventing the emergence of psychological barriers or in overcoming physical barriers that arise from side effects of cancer therapy. Psychological barriers were predominant for exercising in the unsupervised, home-based setting.
In particular, the lack of willpower was the most often named barrier for unsupervised exercise. Previous studies have found the lack of motivation to be the main psychological barrier to exercise participation in breast cancer survivors in both settings (supervised, centre-based and unsupervised, home-based) [13, 28]. For our patients, not motivational but rather volitional barriers to putting intention into action were predominant. Many women struggled with the implementation of their own exercise goals in an unsupervised setting at home more than in the supervised exercise programme. These findings are in line with previous studies that found larger effects for several health outcomes in supervised exercise programmes compared with unsupervised home-based exercise [5, 29]. In summary, centre-based and supervised exercise programmes for cancer patients are important to facilitate exercise participation during as well as after the programme.
Treatment-related physical barriers were less common and diverse than in previous studies. In the study of Courneya et al. [12], disease and treatment-related barriers accounted for half of all reported barriers and in the review from Clifford et al. [10], treatment-related side effects were the most frequently cited barriers to exercise participation. A possible explanation for the reduced frequency of treatment-related barriers may be that the majority of the study participants (n = 15, 79%) participated in the centre-based exercise programme after completion of their cancer treatment (chemo- and/or radiotherapy), when acute side effects are less common.
The prevalence of environmental barriers between centre-based and home-based exercise appeared to be similar, but the barriers themselves seemed to vary by context. Centre-specific barriers arose primarily because the exercise programme was tied to a certain place and time. The combination of both centre-based and guided home-based exercise may be an effective strategy to address centre-specific barriers.
The differences in barriers between the two settings may also explain difficulties in the transition from supervised to self-organised exercise after the completion of the centre-based exercise programme, as described in a previous study [14]. To facilitate this transition and the integration of regular physical activity into daily life, centre-based exercise programmes should include psycho-educational training. The positive effect of motivational constructs (e.g., positive outcome expectancies, intention formation) and volitional constructs (e.g., action planning, coping planning, maintenance self-efficacy) on health behaviour change has previously been described for non-cancer populations [30–32]. To promote different types of health behaviour change, motivational interviewing has been shown to be a promising technique both in cancer and non-cancer populations [33, 34].
An important aim of the supervised centre-based exercise programme is to improve the understanding of the disease and the importance of physical activity for cancer-specific as well as general health outcomes. Therefore, psycho-educational training should not primarily focus on enhancing motivation, but rather on volition and therefore promote behaviour change techniques such as coping planning and action control [13, 21]. Hybrid rehabilitation models with a combination of centre-based and home-based exercise may provide the personal experience of the barriers that may arise in an unsupervised, home-based setting. In such a model, the patients could get professional assistance on how to cope with emerging barriers also for self-organised training at home. For survivors, maintenance of self-organised exercise training is of particular importance in the years to follow.
All the study participants reported a high amount of total weekly physical activity, fulfilling the WHO recommendations of at least 150 min of moderate-intensity or 75 min of vigorous-intensity physical activity [35]. Our results differ from those of previous studies that assessed self-reported physical activity in breast cancer survivors [7, 8]. The high volume of activity by our patients probably reflects a selection bias towards physically active patients and may not be representative for the Swiss breast cancer survivor population. It may partly reflect a positive effect of the centre-based programme; however, most of our study participants were self-referrals to the exercise programme, indicating that they had a strong interest in physical activity and were already active before their cancer diagnosis. Only six (32%) out of the 19 study participants were referred to the exercise programme by their oncologist, confirming the results of a previous study reporting that only few clinicians refer their patients to exercise specialists [36]. Some women pointed out that they wished to have learned about the centre-based exercise programme earlier, namely at the time of diagnosis or during their cancer treatment. Interestingly, even in this cohort of physically active breast cancer patients, barriers towards home-based exercise existed, highlighting the need for structured supervised exercise programmes. We can only speculate that these barriers may even be greater in less physically active patients. This is a call to action to oncologists and cancer nurses to encourage and refer cancer patients, and in particular physically inactive patients who would benefit most, to available structured and supervised exercise programmes [37]. There is sufficient evidence that exercise training reduces adverse and undesired side effects of chemotherapy and may improve survival [2].
This study was conducted with breast cancer survivors who had previously participated in an established structured centre-based exercise programme, hence outcomes can be transferred to clinical practice. The inclusion of cancer survivors who completed the exercise programme at various points in time within the screening period (January 2017 to March 2021) and under different circumstances (during or after the completion of their cancer treatment, before or during the COVID-19 pandemic) yielded a broad spectrum of experiences with exercise participation. A recall bias is possible, since the time between completion of the exercise programme and the research interview varied between the study participants. Physical activity volume per week was not measured objectively by an accelerometer but was self-reported using a validated questionnaire [17]. Because of the rather small sample size (n = 19) we could conduct in-depth and comprehensive interviews. Ceasing recruitment upon data saturation is an established practice in qualitative research and indicates that a suitable sample size was obtained. The demographic and health-related characteristics of the study participants did not differ from the other non-participating breast cancer patients who completed an exercise programme at our centre (n = 47). Thus, it can be assumed that our findings can be generalised to the population of breast cancer patients enrolling in a centre-based exercise programme.
The major limitation of this study was that the identified facilitators and barriers relate to a population of breast cancer survivors who voluntarily chose to complete a centre-based exercise programme and far exceeded physical activity recommendations. Therefore, our findings may not be extrapolated to cancer survivors who do not volunteer to complete an exercise programme or to survivors of other cancers.
This first study on facilitators and barriers toward exercise in breast cancer patients in Switzerland identified more barriers, particularly psychological barriers, for unsupervised, home-based exercise than for supervised, centre-based exercise. Benefits of exercise on physical and mental health and enjoyment of exercise motivated the women to be physically active and benefits of structured and scheduled exercise as well as social support from peers and exercise therapists were the main facilitators for centre-based exercise.
These findings support the importance of providing structured supervised exercise programmes for cancer patients and suggest that a special focus should be directed at the transition from supervised to self-organised exercise in order to enhance and maintain long-term exercise participation.
All data generated or analysed during this study are included in this published article (and the appendix).
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
Financial support was received by Swiss Cancer Research for the Caprice study under grant number HSR-4360-11-2017.
1. Jones LW , Peddle CJ , Eves ND , Haykowsky MJ , Courneya KS , Mackey JR , et al. Effects of presurgical exercise training on cardiorespiratory fitness among patients undergoing thoracic surgery for malignant lung lesions. Cancer. 2007 Aug;110(3):590–8. https://doi.org/10.1002/cncr.22830
2. Campbell KL , Winters-Stone KM , Wiskemann J , May AM , Schwartz AL , Courneya KS , et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med Sci Sports Exerc. 2019 Nov;51(11):2375–90. https://doi.org/10.1249/MSS.0000000000002116
3. Bower JE . Management of cancer-related fatigue. Clin Adv Hematol Oncol. 2006 Nov;4(11):828–9.
4. Schmitz KH , Courneya KS , Matthews C , Demark-Wahnefried W , Galvão DA , Pinto BM , et al.; American College of Sports Medicine . American College of Sports Medicine roundtable on exercise guidelines for cancer survivors. Med Sci Sports Exerc. 2010 Jul;42(7):1409–26. https://doi.org/10.1249/MSS.0b013e3181e0c112
5. Buffart LM , Kalter J , Sweegers MG , Courneya KS , Newton RU , Aaronson NK , et al. Effects and moderators of exercise on quality of life and physical function in patients with cancer: an individual patient data meta-analysis of 34 RCTs. Cancer Treat Rev. 2017 Jan;52:91–104. https://doi.org/10.1016/j.ctrv.2016.11.010
6. Gilchrist SC , Barac A , Ades PA , Alfano CM , Franklin BA , Jones LW , et al.; American Heart Association Exercise, Cardiac Rehabilitation, and Secondary Prevention Committee of the Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; and Council on Peripheral Vascular Disease . Cardio-Oncology Rehabilitation to Manage Cardiovascular Outcomes in Cancer Patients and Survivors: A Scientific Statement From the American Heart Association. Circulation. 2019 May;139(21):e997–1012. https://doi.org/10.1161/CIR.0000000000000679
7. Blanchard CM , Courneya KS , Stein K ; American Cancer Society’s SCS-II . Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society’s SCS-II. J Clin Oncol. 2008 May;26(13):2198–204. https://doi.org/10.1200/JCO.2007.14.6217
8. Irwin ML , McTiernan A , Bernstein L , Gilliland FD , Baumgartner R , Baumgartner K , et al. Physical activity levels among breast cancer survivors. Med Sci Sports Exerc. 2004 Sep;36(9):1484–91.
9. Emery CF , Yang HC , Frierson GM , Peterson LJ , Suh S . Determinants of physical activity among women treated for breast cancer in a 5-year longitudinal follow-up investigation. Psychooncology. 2009 Apr;18(4):377–86. https://doi.org/10.1002/pon.1519
10. Clifford BK , Mizrahi D , Sandler CX , Barry BK , Simar D , Wakefield CE , et al. Barriers and facilitators of exercise experienced by cancer survivors: a mixed methods systematic review. Support Care Cancer. 2018 Mar;26(3):685–700. https://doi.org/10.1007/s00520-017-3964-5
11. Browall M , Mijwel S , Rundqvist H , Wengström Y . Physical Activity During and After Adjuvant Treatment for Breast Cancer: An Integrative Review of Women’s Experiences. Integr Cancer Ther. 2018 Mar;17(1):16–30. https://doi.org/10.1177/1534735416683807
12. Courneya KS , McKenzie DC , Reid RD , Mackey JR , Gelmon K , Friedenreich CM , et al. Barriers to supervised exercise training in a randomized controlled trial of breast cancer patients receiving chemotherapy. Ann Behav Med. 2008 Feb;35(1):116–22. https://doi.org/10.1007/s12160-007-9009-4
13. Hefferon K , Murphy H , McLeod J , Mutrie N , Campbell A . Understanding barriers to exercise implementation 5-year post-breast cancer diagnosis: a large-scale qualitative study. Health Educ Res. 2013 Oct;28(5):843–56. https://doi.org/10.1093/her/cyt083
14. Ferri A , Gane EM , Smith MD , Pinkham EP , Gomersall SR , Johnston V . Experiences of people with cancer who have participated in a hospital-based exercise program: a qualitative study. Support Care Cancer. 2021 Mar;29(3):1575–83. https://doi.org/10.1007/s00520-020-05647-y
15. Braun V , Clarke V . Thematic analysis: APA handbook of research methods in psychology. 2012; 2: 57–71. ISBN-139781433810039.
16. Bull FC , Al-Ansari SS , Biddle S , Borodulin K , Buman MP , Cardon G , et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020 Dec;54(24):1451–62. https://doi.org/10.1136/bjsports-2020-102955
17. Armstrong T , Bull F . Development of the world health organization global physical activity questionnaire (GPAQ). Z Gesundhwiss. 2006;14(2):66–70. https://doi.org/10.1007/s10389-006-0024-x
18. Balneaves LG , Van Patten C , Truant TL , Kelly MT , Neil SE , Campbell KL . Breast cancer survivors’ perspectives on a weight loss and physical activity lifestyle intervention. Support Care Cancer. 2014 Aug;22(8):2057–65. https://doi.org/10.1007/s00520-014-2185-4
19. Creswell JW , Poth CN . Qualitative inquiry and research design: Choosing among five approaches: Sage publications; 2016.
20. Achtziger A, Gollwitzer PM. Dorsch Lexikon der Psychologie; 2021 [updated 8 March 2021; cited 14 July 2021]. Available from: https://dorsch.hogrefe.com/stichwort/volition
21. Schwarzer R . Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. 2008;57(1):1–29. https://doi.org/10.1111/j.1464-0597.2007.00325.x
22. Schmid J , Gut V , Conzelmann A , Sudeck G . Bernese motive and goal inventory in exercise and sport: validation of an updated version of the questionnaire. PLoS One. 2018 Feb;13(2):e0193214. https://doi.org/10.1371/journal.pone.0193214
23. Jekauc D . Enjoyment during exercise mediates the effects of an intervention on exercise adherence. Psychology (Irvine). 2015;6(01):48–54. https://doi.org/10.4236/psych.2015.61005
24. Rhodes RE , Fiala B , Conner M . A review and meta-analysis of affective judgments and physical activity in adult populations. Ann Behav Med. 2009 Dec;38(3):180–204. https://doi.org/10.1007/s12160-009-9147-y
25. Backman M , Browall M , Sundberg CJ , Wengström Y . Experiencing health - Physical activity during adjuvant chemotherapy treatment for women with breast cancer. European journal of oncology nursing : the official journal of European Oncology Nursing Society. 2016;21:160-7.
26. Lavallée JF , Abdin S , Faulkner J , Husted M . Barriers and facilitators to participating in physical activity for adults with breast cancer receiving adjuvant treatment: A qualitative metasynthesis. Psychooncology. 2019 Mar;28(3):468–76. https://doi.org/10.1002/pon.4980
27. Ee C , Cave AE , Naidoo D , Bilinski K , Boyages J . Weight management barriers and facilitators after breast cancer in Australian women: a national survey. BMC Womens Health. 2020 Jul;20(1):140. https://doi.org/10.1186/s12905-020-01002-9
28. Ottenbacher AJ , Day RS , Taylor WC , Sharma SV , Sloane R , Snyder DC , et al. Exercise among breast and prostate cancer survivors—what are their barriers? J Cancer Surviv. 2011 Dec;5(4):413–9. https://doi.org/10.1007/s11764-011-0184-8
29. Sweegers MG , Altenburg TM , Chinapaw MJ , Kalter J , Verdonck-de Leeuw IM , Courneya KS , et al. Which exercise prescriptions improve quality of life and physical function in patients with cancer during and following treatment? A systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2018 Apr;52(8):505–13. https://doi.org/10.1136/bjsports-2017-097891
30. Zhang CQ , Zhang R , Schwarzer R , Hagger MS . A meta-analysis of the health action process approach. Health Psychol. 2019 Jul;38(7):623–37. https://doi.org/10.1037/hea0000728
31. Hattar A , Pal S , Hagger MS . Predicting physical activity‐related outcomes in overweight and obese adults: A health action process approach. Appl Psychol Health Well-Being. 2016 Mar;8(1):127–51. https://doi.org/10.1111/aphw.12065
32. Scholz U , Sniehotta FF , Schwarzer R . Predicting physical exercise in cardiac rehabilitation: the role of phase-specific self-efficacy beliefs. J Sport Exerc Psychol. 2005;27(2):135–51. https://doi.org/10.1123/jsep.27.2.135
33. Frost H , Campbell P , Maxwell M , O’Carroll RE , Dombrowski SU , Williams B , et al. Effectiveness of Motivational Interviewing on adult behaviour change in health and social care settings: A systematic review of reviews. PLoS One. 2018 Oct;13(10):e0204890. https://doi.org/10.1371/journal.pone.0204890
34. Spencer JC , Wheeler SB . A systematic review of Motivational Interviewing interventions in cancer patients and survivors. Patient Educ Couns. 2016 Jul;99(7):1099–105. https://doi.org/10.1016/j.pec.2016.02.003
35. Bull FC , Al-Ansari SS , Biddle S , Borodulin K , Buman MP , Cardon G , et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020 Dec;54(24):1451–62. https://doi.org/10.1136/bjsports-2020-102955
36. Demark-Wahnefried W , Peterson B , McBride C , Lipkus I , Clipp E . Current health behaviors and readiness to pursue life-style changes among men and women diagnosed with early stage prostate and breast carcinomas. Cancer. 2000 Feb;88(3):674–84. https://doi.org/10.1002/(SICI)1097-0142(20000201)88:3<674::AID-CNCR26>3.0.CO;2-R
37. Balneaves LG , Truant TL , Van Patten C , Kirkham AA , Waters E , Campbell KL . Patient and Medical Oncologists’ Perspectives on Prescribed Lifestyle Intervention-Experiences of Women with Breast Cancer and Providers. J Clin Med. 2020 Aug;9(9):E2815. https://doi.org/10.3390/jcm9092815
A manual was drafted in advance to serve as a guide for the semi-structured interviews (Appendix 1). The manual was structured as follows:
Questions about diagnosis, treatment regime, timing and assignment to COR program;
Questions about satisfaction with COR program;
Questions about facilitators, barriers and strategies to manage barriers regarding center-based and home-based exercise during the COR program;
Assessment of current physical activity (GPAQ; Armstrong & Bull, 2006; Appendix 3);
Questions about current facilitators, barriers and strategies to manage barriers regarding home-based exercise.
The interviews were audio-recorded and transcribed verbatim according to the recommendations by Braun and Clarke (2012) for thematic analysis (TA). Swiss dialect was translated into Standard German. Expressions that could not be translated without changing their meaning were written in dialect and marked “…”. Three dots in brackets (…) signals editing of the transcript. Editing was applied for brevity, leaving out dialogue out of context and not relevant for answering the research questions. According to Braun and Clarke (2012) this level of detail for transcription is more than adequate for TA. TA is a method to systematically identify meaning units and organize a data set into patterns (themes). The first step, the familiarization with the data, as proposed by Braun and Clarke (2012) for TA, was initiated with the transcription of the interviews (Appendix 4). Once all the transcripts were completed, each transcript was re-read to get a first overview of potentially interesting themes. Paragraphs of interest regarding the research questions were highlighted. As last patient interviews did not provide new findings, it can be assumed that data saturation was reached. As a next step, initial codes were generated with the specific research question in mind, meaning that only data segments were coded if they seemed potentially relevant to answering the research question.
The theme social support was the most frequently named facilitator regarding center-based exercise. Exercising together in a group and the resulting group dynamic was found to be very motivating. Many women pointed out that exercising together with other breast cancer patients/survivors who had experienced the same situation motivated them to continue with the COR program and stabilized them mentally.
«The group was certainly also motivating, so um, the commonality, so with other people who are in the same situation, um, to do it together.» T15; code: contact with people with the same illness.
Some women explained that exercising in a group or arranging with other people to meet for sports has motivated them to maintain their PA also after completion of the COR program. Supportive friends and family were also mentioned as facilitators for exercise in general.
«That I motivate myself and say 'someone else is coming along' or we go together, then it just simplifies things tremendously for me.» T5; code: positive group dynamics.
«Um, with my husband, that helps that he also participates, that we do this together. That is a great support.» T16; code: support from friends/family.
A main facilitator for center-based exercise was the support from trained supervisors. The continuous assistance of trained therapists and receiving specific information about exercising gave the women a feeling of safety and helped them to understand the benefits of exercise.
«(...) They looked after you very well, and also encouraged you.» T10; code: explanations/support from trained supervisor.
«Because at the end of the day, they always asked how you were doing and that already motivated you and they have- the physiotherapists have also clearly shown you the benefits.» T11; code: explanations/support from trained supervisor.
Many women were motivated to improve their current health status. Their motivation originated both from positive outcome expectancies (the belief that exercise is effective to improve their health) as well as from positive outcome experiences (prior exercise participation has already had a positive effect on their health).
Anticipated benefits
A positive belief that exercise is effective for improving one’s health status is an important factor influencing motivation (e.g. Schwarzer, 2004). Women reported that they ‘realized that exercise is important’ or that they ‘knew that exercise is good for them’.
«We also learned that the exercise activity is apparently important for health, that is indeed a motivation.» T2; code: knowing that exercise is good for my health.
«So the great thing was, that you also understood how important it is that you have to do something.» T8; code: knowing that exercise is good for my health.
The belief that exercise is effective in preventing the recurrence of breast cancer was another commonly named motivator.
«The main motivator has been really um to prevent the recurrence if possible» T11; code: prevent recurrence of breast cancer.
Beside cancer-related health issues, some women were motivated to improve their physical health status in general, exercised to maintain their body weight and to stay vital and mobile in later life.
« I want to get fit again (...) I also want to regain my strength.», T6; code: motivation to improve current health status.
« Yes, just that relaxed feeling, feeling fit, that's what I want to achieve»; T12; code: motivation to improve current health status.
«The risk of falling, so I notice, you can see that with older people or- how that turns out then, if you do nothing, that you are then so wobbly on your feet.»; T10; code: exercising to stay vital in later life.
Experienced benefits
A main motivator for many women to keep up the participation in the COR program was the experience of improvements in physical fitness. They found it very motivating to see objectively what they have achieved and to feel the positive effect on their body.
«I have noticed that the fitness is improving, so that I especially with the bike have been able to increase levels or add minutes or so, that I have really noticed 'yes, it has an effect'.» T18; code: improvements in physical fitness.
Some women experienced that exercise helps to reduce negative side effects, most commonly fatigue.
«I have also felt quite strong fatigue and lack of strength and through the exercise- the exercise has given me back the strength. I have felt more awake and comfortable, stronger, yes.» T12; code: combating the after-effects of therapy.
«At the beginning I had extreme pain and then through the movement it has become better.» T10; code: combating the after-effects of therapy.
Many women also experienced that exercise has had positive effects not only on their physical health but also on their mental well-being. Some women explained that exercising makes them feel good, while others highlighted the good feeling they have after exercising.
«Yes the good feeling that it gives you (...) feelings of happiness (...) the good body feeling that I have afterwards, I feel my body, I feel alive, I can breathe better, I am more awake.» T13; code:good feeling from exercising.
«When exercising I always have a good feeling when I've finished it, you've sweated, and you have the feeling 'whoa now I've done something', so the reward from the endorphins and from the body.»; T14; code: good feeling from exercising.
Exercise also helped some women to switch off from their daily routine and to regain confidence into their own body.
«That it also does me good mentally and psychologically, so as if the body is ventilated (…) that's why I think I also move a lot in everyday life, the thoughts that settle so rather, like digesting, you know what I mean, digesting the thoughts.»; T1; code: switch off from daily routine.
Many women explained that they really enjoyed being physically active and some women pointed out that they enjoyed the activities from the COR program, which has motivated them to continue. Some women were intrinsically motivated to exercise because of the enjoyment they experienced while exercising and because it was important to them to attend the COR program. Some women pointed out that if they really liked the exercise activities, and the fact that attending organized exercise freed them from having to ‘force themselves’ to exercise.
«Of course the walking with the poles, the Nordic walking, uh I liked that so much, that was so beautiful» T9; code: enjoying the activities in the program.
«And at the same time it's fun for me of course, so movement, I also need that, so that's also good for me and I'm like a little addicted to being able to move (...) it's the urge to move, the urge to act.»; T6; code: enjoyment of movement.
This theme was reported exclusively for center-based exercise. The majority of the women pointed out that exercise with a fixed appointment was a main facilitator for them to maintain their exercise participation during the COR program. Other participants liked that the COR program gave them a daily structure and routine and that the exercise sessions were according to a training schedule. Also, the COR program helped several women to re-initiate exercising after their cancer treatment.
«It's like the same thing with strength training, I have an appointment, then I go (...) it's like clear, like a business appointment (...) That also makes it easier for me.» T6; code: fixed appointment.
«That of course it has been regular (...) just getting back into the rhythm like that» T8; code: regularity/routine.
«It [the COR program] has indeed made me a little bit eager to move again, so the inner- the inner urge to move a little bit awakened again» T13; code: COR as an initiator to start exercising.
The women reported both treatment-related and non-treatment-related physical barriers (injuries and medical conditions) that prevented them from or made it more difficult to exercise. Fatigue was the most common treatment-related barrier. Furthermore, some women were impaired by pain in joints, muscles, bones or at the side of breast surgery. Other side effects like nausea and neuropathy were reported less frequently than pain and fatigue.
« During these 10 days I did nothing, I was happy if I could somehow walk to the toilet or to the kitchen. » T6; code: fatigue.
«Yes, due to the Tamoxifen I have joint problems (...) ankle and the whole back hurts, so I have severe muscle soreness afterwards (...) the muscle soreness and the joint problems slow me down when I do sports» T13; code: pain.
Psychological barriers reflect barriers that originated from the women’s lack of motivation or lack of volition (the successful pursuit of defined goals; Achtziger & Gollwitzer, 2021). The most cited psychological barrier was the lack of willpower/self-discipline. This barrier was mentioned only in the context of home-based, unsupervised exercise both during and after completion of the COR program.
«And if I don't do it at home, then there is the problem with my ‘inner demons’.» T2; code: lack of willpower/self-discipline.
«Because at home you would just- you always have a reason to put it off a little longer (...).» T10; code: lack of willpower/self-discipline.
«I think it's just structural (...) I didn't manage to make an appointment and then do it at home, I absolutely didn’t feel like it (...) it didn't motivate me at home.» T6; code: lack of willpower/self-discipline.
Some women explained that they did not have enough time to exercise or when they had a lot of things to deal with, exercise was not a priority.
«You want to do other things as well (...). Until you have finished the whole program that you actually want to do, then yes, of course you want to cut out what you like to do the least (...).» T10; code: exercise ‘not a priority’.
A few women struggled to maintain their exercise because they did not really enjoy it and identified themselves as not being a ‘sporty type’.
«Yes, where I just realize, I'm just not the sporty type, or otherwise it wouldn't be so difficult for me» T10; code: not being ‘the sporty type’.
This theme included barriers that originated from the natural, built and social environment that surrounded an individual. The only but frequently mentioned barrier from the natural environment was bad weather.
«Then the winter arrives and then I stop running»T7; code: bad weather.
«When it's so gruesomely cold, I'd rather sit inside»T9; code: bad weather.
Specific to this time period (year of 2020) were the barriers that arose due to the Covid-19 pandemic. Because all sporting and fitness facilities were closed for several months, some women were not able to pursue their usual exercise activities and were forced to adapt their habits.
«Yes, Covid, so I also went to a fitness center for a while, I actually like to go swimming, but now I can't do all that. » T14, code: Covid pandemic.
Other quite frequently named barriers from the social environment were work-related time constraints and childcare duties. Scheduling conflicts and time burden arose due to work responsibilities and doctor’s appointments; work irregularities made it difficult to plan ahead. Childcare duties was a barrier mentioned specifically for home-based exercise, because it was more difficult to exercise at home with the children around.
«I don't have time, I don't have time, I have 2 kids, I almost work 100%, I absolutely can't» T8; codes: childcare duties / work responsibilities.
«Yes, it [exercising at home] was difficult in terms of the environment, because then I had the children» T14; code: childcare duties.
A barrier from the built environment for the women that lived outside of the city and specific to center-based exercise was the distance to the rehabilitation center. To take on this ‘long way to travel’, especially with public transport, made it more difficult to attend the exercise sessions. On the other hand, a barrier from the built environment for home-based exercise was the lack of space and suitable exercise equipment.
The comparison of barriers towards center-based and home-based exercise showed large differences with regard to psychological barriers, which were much greater for home-based exercise (Figure 3). Physical and environmental barriers regarding home-based and center-based exercise were about the same.
Strategies to manage barriers to exercise training. Number of patients reporting strategies are indicated in brackets.
Adapting training modalities
Making exercise sessions more appealing
Prioritization of exercise
Action planning
Action control
Coping planning
To overcome barriers, some women adapted their training circumstances by adapting training modalities or by making exercise sessions more appealing.
Some women changed their training activities or training location to address their barriers (e.g. pain, Covid pandemic, no space and equipment to exercise, bad weather). A common cited strategy to deal with fatigue and pain was shorter/lower intensity exercise.
«I just made sure I went outside every day somehow, even if I could only crawl 100 meters.» T3; code: shorter/lower intensity exercise.
«More repetitions but less weight, this helped me to adapt the training to the challenges, to the health situation, precisely. » T6; code: shorter/lower intensity exercise.
A strategy specific to the barriers that arose due to the Covid-19 pandemic was the organization of exercise sessions at home. Some women joined online exercise sessions or bought equipment for weight training at home.
Women who struggled with the lack of willpower/self-discipline or the lack of an exercise partner tried to make their exercise sessions more appealing by distracting themselves with music or podcasts or added a social component by arranging their exercise sessions with other people.
«Yes that I bring some colleagues on board to also motivate the others and um myself also, so that my training sessions have a bit of variety so that I have more motivation.» T12; code: arranging training with other people.
This theme included cognitive and behavioral strategies, which are part of common behavior change models (e.g. Schwarzer, 2014). The women’s strategies were grouped into three subthemes: prioritization of exercise, action planning and action control. Action planning is a prospective approach, in which behavioral plans are established before encountering the situation, and action control is a synchronous self-regulatory approach with continuous evaluation of the current behavior (Schwarzer, 2008).
To have more time and energy to exercise, some women cut down on other activities and gave exercise a higher priority than other, competing activities or tried to have a good balance between different activities.
«I have to manage my strength somehow and this rehabilitation program and the sports activities at home are important, so other things that are not that important have to take a back seat.» T19; code: cutting down on other activities.
«To find a bit of a balance like that (…) It's more just that, it's like the balance between social networking and my own activities.» T3; code: finding a balance between exercise and other activities.
«I say to myself that I would rather do sports than cleaning and outsource the strenuous household work, I then have a cleaning lady or have the groceries delivered so that I can use the energy to do sports.»T6; code: cutting down on other activities.
Action planning describes strategies that include the planning of the when, where and how the exercise session will take place. Action planning strategies were most often applied for motivational barriers (e.g. lack of willpower/self-discipline) but were also used for environmental barriers like childcare duties. Many women found it helpful to plan exercise sessions in advance, to create a commitment and to make it a routine.
«Also that I have already made an agreement, a fixed appointment, then I go, no matter if it is raining or snowing or windy or cold.» T6; code: creating a commitment.
«Making definite weekly plans (...) if I use these weekly plans realistically, then I can actually stick to them better and that also helps to keep the pace.» T2; code: planning exercise sessions in advance.
«Exactly, firmly scheduled on Friday or so (...) that it becomes a routine and that it really is an appointment, something like that.» T4; code: making exercise a routine.
Some women also explained that setting goals and self-monitoring like writing down their own progress has helped them to keep themselves motivated and to remain physically active.
«I even have like a table everyday I’m taking the activity done, so you know to keep me motivated in this way.» T17; code: write down activities/progress.
«I have learned to set the goals more realistically.»T2; code: setting goals.
The subtheme action control includes strategies that are used when an already planned exercise session cannot be carried out due to internal or external barriers or to shield already planned sessions from other courses of action (Schwarzer, 2014). A strategy that was used by women when confronted with overlapping appointments or sudden fatigue was to be flexible and to reschedule the planned exercise session. The possibility to reschedule the exercise sessions from the COR program was pointed out by women to have facilitated the regular attendance. For a few women it was important not to postpone their planned exercise session, because they knew they would probably then not do it at all.
«I do (...) my gymnastic exercises on Saturday and then things came up at short notice, vet appointments or something that I said, 'ok I'll do it on Sunday' and postponed it by a day.» T19; code: reschedule/being flexible.
Some women explained that formulating plans with alternative exercise options were helpful to maintain their activity when barriers emerged. This strategy is referred to as coping planning in the literature (Scholz et al., 2005).
To deal with ongoing fatigue some women pointed out the importance of a balance between resting and exercising. Some women addressed side effects like neuropathy or joint and muscular pain by seeking medical attention or treatments with alternative medicine.
«I already knew that I would get lazy in the winter and because it is too cold to run and then we planned together where I could do this exercise, for example at the Inselspital [tertiary center] up and down the stairs or so.» T1; code: planning alternative exercise options.
« Yes I went to the family doctor (...) and the idea is that I get a cortisone injection and that I treat it [neuropathy] with medication. » T6; code: doctor’s visit / medical attention.