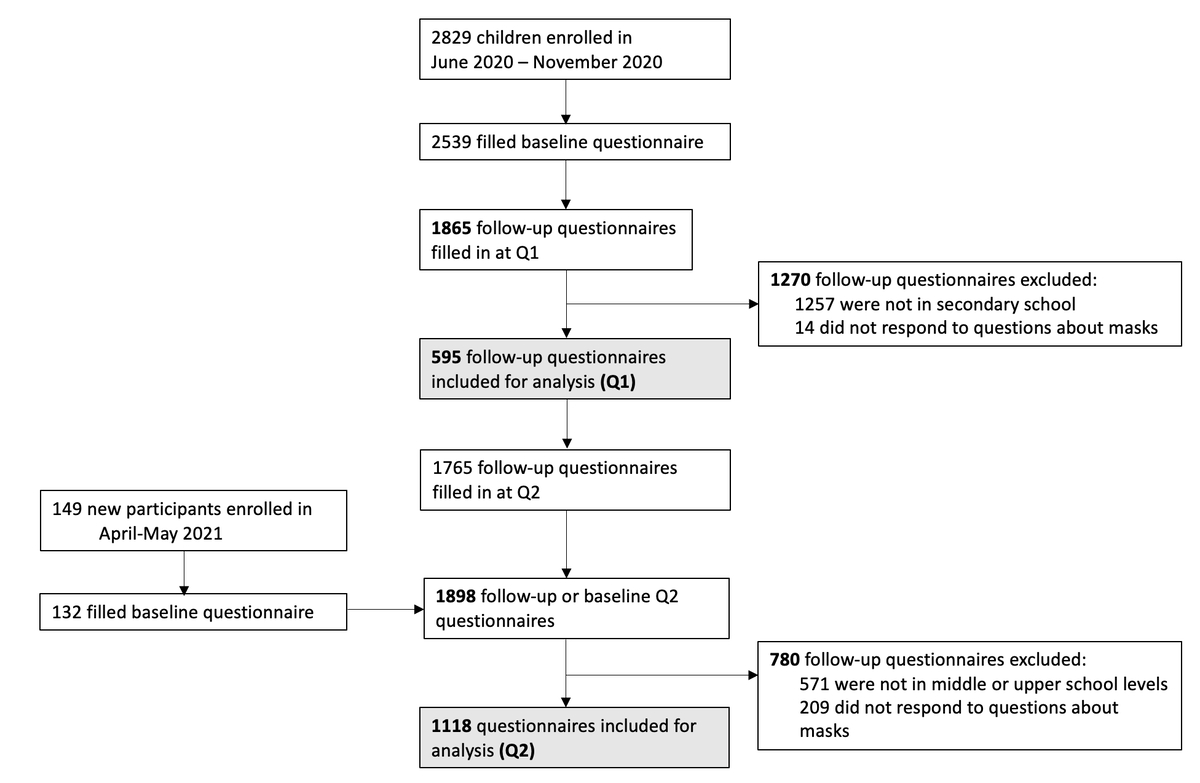
Figure 1 Flowchart of study participants and questionnaires, T1: testing in June-July 2020, T2: testing in October-November 2020, T3: testing in March-April 2021. * Exclusion due to missing values in mask usefulness questions.
DOI: https://doi.org/10.4414/SMW.2022.w30165
The contribution of school children to the spread of SARS-CoV-2 remains a controversial topic. In 2020–2021, school policy decisions ranged internationally from complete closure over many months to fully maintained in-person attendance throughout the pandemic [1, 2]. Although children rarely develop severe health outcomes [3–5], SARS-CoV-2 infection rates among children and adolescents are generally similar to those in adults [6, 7]. However, major outbreaks of clustered SARS-CoV-2 infections in schools were rare in the first year of the pandemic [7–9]. Lower viral load, more frequent asymptomatic or mildly symptomatic infections, as well mitigation measures in schools, including mask wearing of adults and children, could have contributed to the limited spread in schools and communities [10–15]. Nevertheless, numerous countries implemented nationwide school closures to confine the diffusion of SARS-CoV-2 infections [2, 16]. Worldwide, about 150 countries fully closed their schools at some point in 2020–202 [17]. Prolonged school closures may be associated with detrimental long-term consequences for children’s mental and physical health, and learning outcomes [18, 19].
In Switzerland, schools were open with preventive measures in place, except during a 6-week nationwide lockdown from 16 March to 10 May 10 2020. Subsequently, schools reopened with implemented protective measures (e.g., social distancing, frequent hand washing, reduced mixing of classes). Face masks became compulsory in public transport and in situations where physical distance (2 metres and subsequently 1.5 metres) could not be maintained from July 2020 for persons from 12 years age. From November 2020, masks became compulsory for adults and secondary school children (grade 7 and higher) in educational settings. From February 2021, wearing of masks was extended to children in middle school level (grades 4–6).
Although masks were reported to be linked with reduced SARS-CoV-2 community transmission [20–24] and school outbreaks [14], prolonged wearing of masks may be perceived as a burden and can be associated with side effects such as headaches or skin irritation in adults and children [25, 26]. Willingness to wear masks is influenced by perceived benefits and social norms, and refusal by negative attitudes or side effects [27, 28]. The authors were unaware of any study investigating the perceived usefulness and attitudes towards mask wearing in children and adolescents at the time of this study.
This exploratory study reports descriptive measures of school children’s perceptions of the usefulness of masks in- and outside the school setting from randomly selected schools in the canton of Zürich, Switzerland. In a second step, we examined associations between perception of usefulness and school level (secondary versus primary school), gender, and parents’ educational attainment [29], in order to uncover potential relationships with sociodemographic characteristics and thus inform further focused research projects in the future. Finally, we documented the changes in perception over time in secondary school children.
Ciao Corona is a prospective cohort study investigating SARS-CoV-2 seroprevalence in school children in the Canton of Zurich, Switzerland, described in detail previously [7, 30]. Zurich has 1.5 million ethnically diverse residents who live in urban and rural settings and comprise 18% of the Swiss population. Roughly 27% of residents in the Canton of Zurich are of foreign nationalities [31], and approximately 8% of the population receive some social benefits [32]. The study is embedded in a nationally coordinated SARS-CoV-2 research network in Switzerland, Corona Immunitas [33]. Briefly, randomly selected schools were invited to participate in the study in May-June 2020, with the target number of enrolled schools proportional to the population size within the 12 districts of the canton. School authorities were provided with study information and the link to the study website by email. After agreeing to participate, schools received the consent forms and access codes to the online baseline questionnaire, to be forwarded along with the study information for the parents of the children of the randomly selected participating classes.
Approximately 2500 school children aged 6 to 16 years from 55 primary and secondary schools (from a total of 600 schools in the Canton of Zurich) participated in each testing phase of the study. The study was structured around three seroprevalence testing phases in June/July 2020, October/November 2020, and March/April 2021. At each testing phase, venous blood samples were taken for SARS-CoV-2 serological analysis. Seroprevalence in children who were ever seropositive by October/November 2020 was 6.6% (95% credible interval 4.0–8.9%), and increased to 16.4% (12.1–19.5%) by March/April 2021 [15].
Online questionnaires were distributed to parents of the participating children by email upon enrolment to assess children’s symptoms, possible SARS-CoV-2 infections and lifestyle. Parents were asked to fill the questionnaires together with their child. Subsequently, parents and children received further bi-monthly online follow-up questionnaires until March/May 2021.
The current study focused on questions on mask wearing, which were incorporated into the online questionnaires at two time-points: in the follow-up questionnaire in winter of 2021 (Q1: 12 January to 24 March 2021), and in late spring of 2021 (Q2: 10 March to 16 May 2021. For participants who were enrolled and completed the baseline questionnaire around the third testing phase in March-April 2021, Q2 questions regarding mask wearing were incorporated into the baseline questionnaire. A flowchart of participants and questionnaires included in this study is shown in figure 1.
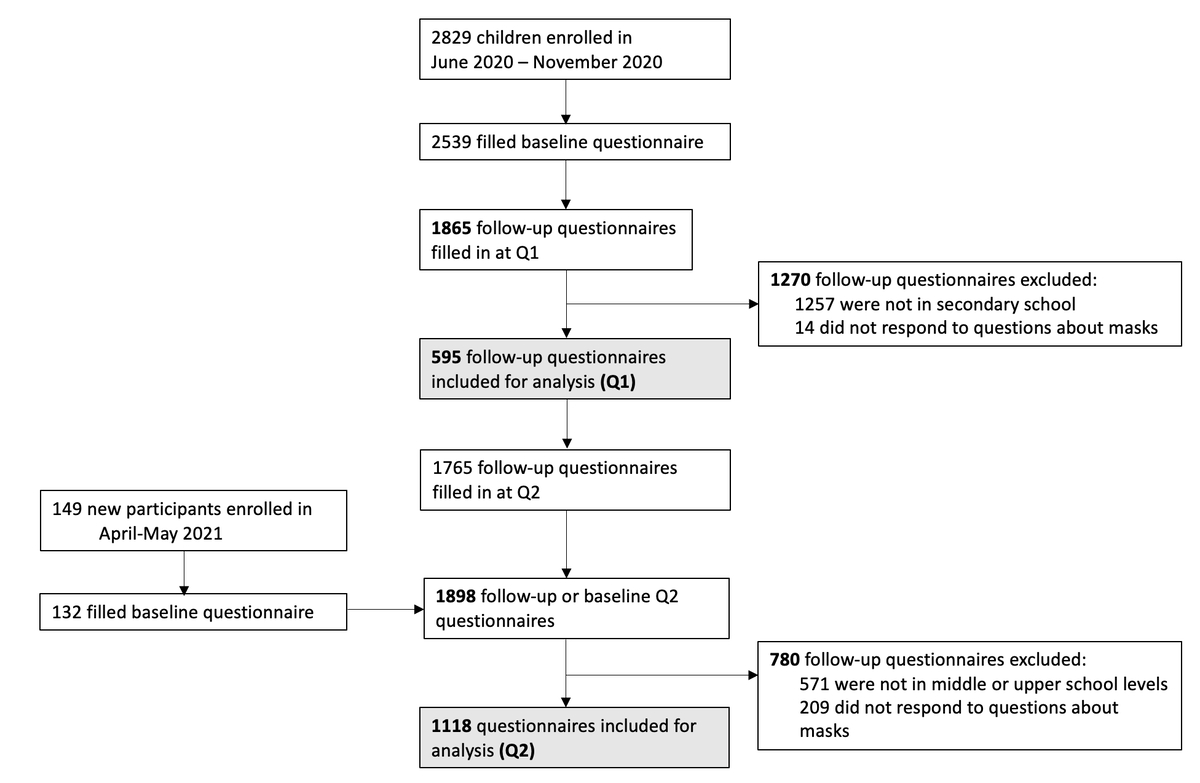
Figure 1 Flowchart of study participants and questionnaires, T1: testing in June-July 2020, T2: testing in October-November 2020, T3: testing in March-April 2021. * Exclusion due to missing values in mask usefulness questions.
Survey questions were developed by the study team based on iterative discussions and were not formally validated. Questions included children’s perception of the usefulness of masks in the school setting and in public, mask wearing practices (i.e., type of mask, storage and wear time), and an open question for comments on masks (see supplementary table S1 in the appendix). Masks were compulsory for primary school children in grades 4–6 only from the end of January 2021. Therefore, at each survey, we addressed the questions on masks only to the children attending school levels with compulsory mask wearing: only secondary school children (grades 8–9, age 13–17 years) at Q1; and both primary (grades 5–6, age 10–13 years) and secondary school children at Q2. In the online questionnaire, we explicitly asked parents to have their child complete the questions about masks.
The study was approved by the Ethics Committee of the Canton of Zurich, Switzerland (2020-01336). Written informed consent was obtained from parents or legal guardians of participating children. Children aged 14 years and older could confirm the consent themselves after consultation with a parent or legal guardian.
A total of 1302 of 2974 (44%) children who participated in at least one of the Ciao Corona testing rounds completed at least one question about masks in at least one of the Q1 and Q2 questionnaires. Variables extracted from the questionnaires were perceived usefulness of masks (5-point Likert scale: 1: not at all useful, 2: somewhat useful 3: neither useful nor useless, 4: quite useful, and 5: very useful) at school and in public, school level (middle or upper), child’s gender and parents’ highest educational attainment as well as residence (urban/rural). For the analysis, we further merged the 5-point Likert scale into three categories: “somewhat or not useful” (Likert scale values 1-2), “neutral” (Likert scale value 3), and “useful” (Likert scale values 4-5). High educational attainment was defined as at least one parent having at least a technical college or university degree.
Two authors (PA, TR) developed six categories for the free-text comments by identifying homogenous themes in the responses: (1) general rejection and frustration; (2) general acceptance; (3) side effects and discomfort; (4) uncertainty and mistrust; (5) situation-specific complaints (e.g., during sports); and (6) not categorisable. These two authors independently categorised the responses into the defined categories. When necessary, discrepancies were resolved among the two authors and consensus achieved through discussion.
Descriptive statistics included a summary of participants’ key characteristics (age, gender, school level, rural or urban residence, and parents’ highest educational attainment). Associations between school level, gender, parents’ highest educational attainment and perceived usefulness of masks were investigated with Pearson’s and McNemar’s chi-square tests. In addition, we examined the differences in perceived usefulness between the two measurement points Q1 and Q2 on population (cross-sectional) and individual (longitudinal) levels. Data from Q2 were used for the main cross-sectional analyses, with data from Q1 presented in the appendix. Data analysis was performed using base packages of R version 4.1.0 (R Core Team, 2020) [34], supplemented with packages tidyverse and gtsummary [35,36].
Participant characteristics are given in table 1. A total of 595 (54% girls) study participants responded to at least one question on masks in the online survey at Q1, and 1118 (52% girls) participants at Q2. At Q2, 596 middle level school children and 522 upper level school children completed the questionnaire. The majority of children had at least one parent with Swiss nationality, and at least one parent with a higher educational attainment.
Table 1Participant characteristics.
| January – March 2021 (Q1) | April – May 2021 (Q2) | ||
| n = 595 | n = 1118 | ||
| Age (years) | 14.3 ± 0.7 | 12.8 ± 1.6 | |
| Gender | Girls, n (%)* | 320 (54%) | 580 (52%) |
| Boys, n (%)* | 272 (46%) | 536 (48%) | |
| RT-PCR confirmed SARS-CoV-2 infection, n (%)** | 21 (4%) | 43 (4%) | |
| School location | Urban, n (%) | 239 (46%) | 427 (46%) |
| Rural, n (%) | 356 (54%) | 691 (54%) | |
| School level *** | Middle level (grades 5–6) | – | 596 (53%) |
| Upper level (grades 8–9) | 595 (100%) | 522 (47%) | |
| Socioeconomic status | Either parent with Swiss nationality, n (%)a | 503 (85%) | 974 (87%) |
| Either parent with high educational attainment, n (%)b | 349 (60%) | 783 (71%) | |
Data are presented as mean ± standard deviation (SD) or count (%). There were no missing data on age, gender, confirmed SARS-CoV-2 infection, school location or level.
RT-PCR: real time polymerase chain reaction; SARS-CoV-2: severe acute respiratory syndrome coronavirus 2.
* 3 (Q1) and 2 (Q2) children reported “other” as their gender.
** RT-PCR confirmed SARS-CoV-2 infection was defined as at least one RT-PCR positive test reported in any questionnaire by 24 March 2021 (Q1), or by 16 May (Q2).
*** For school children, mask use was compulsory from October 29, 2020, for grade 7 and higher, and from January 25, 2021, for grade 4 and higher.
a Parents of 13 (Q1) and 16 (Q2) children did not report their nationality.
b Parents of 16 (Q1) and 21 (Q2) children did not report their highest education.
At Q1, the majority of children and adolescents perceived masks as useful, both at school (n = 357, 60%) and in public (n = 408, 69%). At Q2, 57% (638) participants perceived masks as useful at school, and 60% (675) in public. At Q2, masks were perceived as useful at school by 354 (59%) of primary and 284 (55%) of secondary school children (p = 0.2), and in public by 366 (61%) of primary and 309 (59%) of secondary school children (p = 0.2). Detailed responses to the questions of mask usefulness at Q1 and Q2 are provided in supplementary table S2 (appendix).
At Q2, girls perceived mask wearing as useful more often than boys both at school (61% vs 53%, p = 0.018; fig. 2A) and in public (64% vs 57%, p = 0.026); supplementary fig. S1). The difference between girls and boys was similar at Q1 (at school: 63% vs 56%, p = 0.2; in public: 71% vs 67%, p = 0.3; table S3). Moreover, the perception of mask usefulness at school and in public did not differ between middle level and upper level school children (fig. S2).
At Q2, 71% (781 of 1095 with reported information) of participating children had at least one parent with high educational attainment. Children of parents with higher educational attainment were more likely to perceive mask wearing as useful at school (61% vs 49%, p < 0.001; fig. 2B) and in public (63% vs 54%, p = 0.019; fig. S1). At Q1, the difference was somewhat smaller for perceived usefulness at school (63% vs 57%, p = 0.3), and similar to that in Q2 for usefulness in public (74% vs 63%, p = 0.026; table S3).
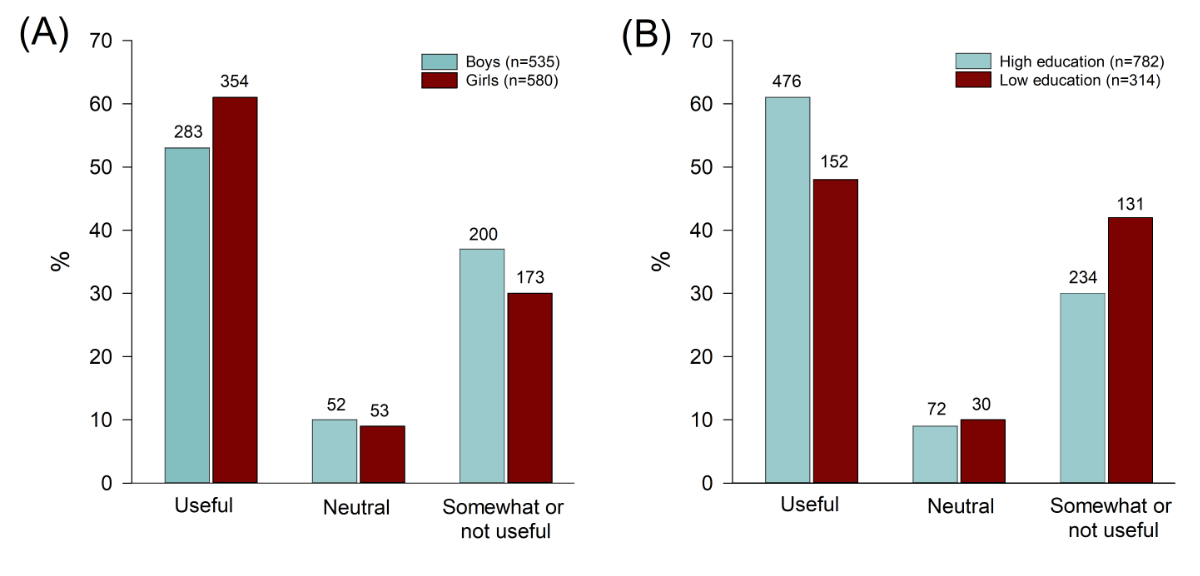
Figure 2 Comparison of perceived usefulness of mask wearing at school between boys and girls (A) and according to parents’ educational attainment (B) at Q2. Higher educational attainment was defined as at least one parent having at least a technical college or university degree. One boy did not answer the question about mask usefulness at school.
From the secondary school children participating at Q1, 75% (446 of 595) answered the question on perceived usefulness of mask wearing at school and 75% (447 of 595) on mask wearing in public at Q2. Overall, the proportion of children perceiving masks as useful was smaller at Q2 than at Q1 ( pschool = 0.06, ppublic <0.001; table 2). Some 17% of children reported a lower perception of mask usefulness at school at Q2 than at Q1, and 12% reported a higher perception of mask usefulness. A total of 23% reported a lower perception of mask usefulness in public at Q2 than at Q1, and 10% reported a higher perception of mask usefulness.
Table 2Comparison of perceived usefulness of mask wearing at school (n = 446) and in public (n = 447) between secondary school children at Q1 and Q2.
| Q2* | ||||||
| Useful | Neutral | Somewhat or not useful | p-value** | |||
| Q1 | School | Useful | 206 (46%) | 20 (4%) | 46 (10%) | 0.06 |
| Neutral | 13 (3%) | 5 (1%) | 11 (2%) | |||
| Somewhat or not useful | 26 (6%) | 14 (3%) | 105 (24%) | |||
| Public | Useful | 230 (52%) | 21 (5%) | 66 (15%) | <0.001 | |
| Neutral | 10 (2%) | 5 (1%) | 14 (3%) | |||
| Somewhat or not useful | 23 (5%) | 11 (2%) | 67 (15%) | |||
* A total of 595 secondary school children answered the questions on mask usefulness at Q1, and 521 children at Q2. Of these, 446 and 447 children, respectively, answered the questions on mask usefulness at school and in public at both time points.
** McNemar’s chi-squared test.
A total of 120 (20%) children provided a free-text comment about masks at Q1, and 228 (20%) at Q2. Children who perceived mask wearing as somewhat or not useful both at school and in public were more likely to leave a comment, both at Q1 (ppublic = 0.02, pschool <0.001), and Q2 (ppublic = 0.006, p school = 0.001). At Q1, 95 (80%) comments were categorised as either general or situation-specific mask rejection, complaints or mistrust, in comparison with 140 (61%) such comments at Q2. Most comments mentioned side effects and discomfort (36% at Q1, 7% of all children; 18% at Q2, 4% of all children) and general rejection/frustration (23% at Q1, 21% at Q2), see table 3. At Q2, the proportion of children reporting side effects and discomfort was slightly lower among middle level compared with upper level school children (15% versus 21%), and situation-specific complaints about masks were more frequently reported by middle level compared to upper level children (24% versus 11%). Table 3 shows examples of comments for each of the six categories.
Table 3Examples of free-text comments on an open question on mask wearing at Q1 and Q2.
| Response category and comment examples* | Q1 | Q2 | |||
| All | Middle Level | Upper Level | |||
| N = 120 | N = 228 | N = 126 | N = 102 | ||
| General rejection and frustration | “Masks are annoying” | 28 (23%) | 48 (21%) | 27 (21%) | 21 (21%) |
| “Hopefully, there will soon be a life without masks!” | |||||
| “I hate masks” | |||||
| “All the students are annoyed by the masks” | |||||
| Uncertainty and mistrust | “Masks make no sense, everything is just fear mongering” | 12 (10%) | 10 (4%) | 6 (4%) | 4 (4%) |
| “Completely useless” | |||||
| “Why do we have to wear masks in class but not in school sports? There, the distance can also not be maintained...” | |||||
| “Masks are useless against viruses and have no effect on infection!” | |||||
| General acceptance | “For me, wearing masks in everyday life makes a lot of sense. The only thing that bothers me are people who think it is not important, because they believe they won’t get sick. In school, I find that wearing masks would need to be better controlled, because many do not follow the rules or see each other at lunch without a mask and share food or drinks.” | 15 (13%) | 37 (16%) | 22 (18%) | 15 (15%) |
| “They do not look nice, but are currently the least evil, so there is worse.” | |||||
| Side-effects and discomfort | “I get too little air, so that I have headaches more often.” | 43 (36%) | 41 (18%) | 19 (15%) | 22 (21%) |
| “My skin is very unclean. I miss seeing the whole face of people around me.” | |||||
| “Because of the masks, I have skin rashes and my ears hurt.” | |||||
| “I think that wearing masks is very bad. You can hardly breathe, and I can concentrate less and less in school. I find this idea very bad, because in your free time children talk to each other without a mask anyway”. | |||||
| Situation-specific complaints | “Very annoying while doing sports!!!!!” | 12 (10%) | 41 (18%) | 30 (24%) | 11 (11%) |
| “It's unbearable in gym class!” | |||||
| “It is very uncomfortable to breathe during sports” | |||||
| Not categorizable | “More fabric masks” | 10 (8%) | 51 (22%) | 22 (18%) | 29 (28%) |
* Individual responses were translated from German.
The majority of children reported using disposable masks (69% at Q1 and 76% at Q2) or a combination of disposable and fabric masks (21% at Q1 and 15% at Q2) (see supplementary table S4). When not worn, masks were most commonly carried in a pocket or fastened around the arm, and less frequently stored in a plastic or fabric bag. Mean reported daily wear times of masks were about 6 hours for middle level school children, and 7 hours for upper level school children (table S4).
In this study of children and adolescents from randomly selected schools in the canton of Zurich, Switzerland, approximately 60% of participants perceived wearing of masks as useful both at school and in public in the first half of 2021. Girls valued the usefulness of masks higher than boys, and children of at least on parent with a higher education perceived masks as more useful. Perceived usefulness of wearing masks in public, but not at school, decreased over time. A small proportion of school children reported general side effects and discomfort (7% at Q1 and 4% at Q2) or situation-specific complaints (2% at Q1 and 4% at Q2) associated with masks.
Some survey participants provided free-text comments on the necessity of wearing masks to protect others and even complained about others not wearing their masks according to school rules. On the other hand, roughly one third of the survey participants did not perceive masks in school-settings as useful; these participants provided free-text comments about masks significantly more frequently, indicating a bias towards negative comments. These comments ranged from generic (“masks are useless”, “I hate masks”) to specifically pointing towards physical discomfort and side effects, such as fatigue, decreased concentration, headaches, or acne. Mandatory wearing of masks was often criticised for specific situations, such as physical education classes and breaks.
Complaints about masks, particularly their side effects, need to be considered on an individual basis. In settings with potential widespread transmission and where physical distance cannot be guaranteed, the use of masks for children aged 6 years and older is recommended by the World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) [37]. In this study, the proportion of children reporting side effects and discomfort was slightly lower among middle level compared with upper level school children (15% versus 21%), whereas situation-specific complaints about masks were more frequently reported by middle level than to upper level children (24% versus 11%). Various reasons might explain these age group differences in self-reported side effects and situation-specific complaints. For example, potentially longer mask exposure times in upper level school children could have resulted in more frequently reported side effects. Importantly, current evidence on the benefit-harm balance of the use of masks during the SARS-CoV-2 pandemic in the paediatric population is limited. Laboratory-based experimental studies investigating short-term effects of various types of masks (e.g., surgical mask, FFP2, or N95 respirators) worn at rest and during exercise on physiological variables and individuals’ perception of breathing are controversial [38–40]. Masks are usually only one of several implemented mitigation measures, making it challenging to tease out the unique effect of masks on infection control as documented in a few studies [13, 14].
Children whose parents had a higher educational background and girls perceived masks as more useful. In contrast, we did not see a difference between perception of middle and upper school level (i.e., younger and older) children. Associations between gender and education with the willingness to wear masks has been shown in previous adult studies [29, 41, 42]. In a large analysis of shoppers, female gender, older age and urban location were associated with higher odds of an individual wearing a mask [29]. Schools could provide tailored information about masks to reach different groups of children, and to actively engage them in a dialogue about potential benefits and harms.
Although the absolute difference was small, the proportion of school children rating masks as useful in public was higher than the proportion rating masks useful at school (60% versus 57% at Q2). One potential explanation could stem from the prolonged wearing of masks in school settings: masks were reported to be worn between six and eight hours a day (supplementary table S4). Outside the school setting, masks are usually only required temporarily, such as in public transport or supermarkets. Second, children and adolescents may feel safer in a classroom environment than in public because of the implementation of various additional measures as part of a school’s protection concept, and thus may perceive mask wearing there as relatively less useful. In addition, the proportion of children perceiving mask wearing as useful slightly decreased from January to April 2021, at school from 60% to 57% and in public from 69% to 60%, respectively. This could be related to the longer overall exposure of wearing masks at Q2 compared with Q1, as well as to the lower community incidence of SARS-CoV-2 infections at Q2.
This study has several limitations. First, the online questionnaires of the Ciao Corona study were usually completed by parents or legal guardians. Although parents were explicitly encouraged to complete the questions on masks together with their children or to let their child respond on their own, we cannot confirm that this was followed. Parent-reported responses might be subject to social desirability bias. Second, children’s behaviour and perceptions are largely influenced by their parents’, teachers’, and peers’ beliefs and behaviour [43, 44]. Thus, it is also likely that children of parents who were sceptical towards certain restrictions and measures implemented during the SARS-CoV-2 pandemic did not take part in the Ciao Corona study, resulting in potential selection bias. Third, the questionnaire was developed internally by the study authors, not formally validated, and the concept of usefulness was not explicitly defined for participants, potentially leading to heterogeneous interpretation of the question. The authors were not aware of a validated questionnaire capturing children’s perceptions of mask wearing at the time of running the study. The somewhat straightforward manner of the questions, as well as the urgency to administer the questionnaire promptly, led to authors’ omitting the formal validation of the questionnaire. Owing to the exploratory nature of the study, we instead supplemented the questionnaire with an open-ended question on attitudes towards mask wearing and relied on extracting the themes emerging in the free-text responses. The questionnaire, translated from the original German to English, is provided in supplemental table S1 for readers’ judgement. Furthermore, we did not investigate the role of perception of, attitude to and knowledge of mask wearing practice of children, and did not conduct interviews or focus-group discussions to probe themes identified in the free-text comments. Hence, the understanding of mask wearing practices in our study population might be incomplete. However, perceived usefulness and benefits of masks have been shown to increase intention and willingness to wear masks in adults [27, 45]. Therefore, it could be regarded as an important first proxy to understanding such practices. Fourth, side effects reported by some survey participants cannot be (clinically) verified and would require a different study design. Finally, our study sample consisted predominantly of families with Swiss nationality, and a larger proportion of parents had a higher educational background (60% at Q1 and 71% at Q2) than would be expected in the general population [46]. We did not specifically tailor our recruitment strategy towards children/families of different ethnicities, for example by providing study information in several languages. Consequently, our study includes a selective cohort and the findings likely do not reflect the entire spectrum of perceptions about the usefulness of masks in the general population, and may to some extent overestimate the perceived value of masks in schools and public.
In summary, our findings suggest that 60% of children perceived masks as useful in the winter and spring of 2021 during the SARS-CoV-2 pandemic at school and in public, with slightly higher perception of usefulness among girls and families of higher socioeconomic background. Certain complaints of some children, such as physical discomfort and side effects due to the prolonged wearing of masks, should be addressed in order to ensure the maintenance of mask wearing, and ultimately protect the health and well-being of children and adults at schools and beyond. Efforts should also be taken to validate questionnaires to assess perceptions in mask wearing.
The raw data supporting the conclusions of this article will be made available by the authors, on reasonable request.
We kindly thank all children and their parents for their participation in this study and for completing the online surveys.
Contributors: SK and MAP initiated the cohort study in which this study is embedded. AU, PA, TR and SK designed the research questions and the study, and were responsible for the study organization and procedures. PA was responsible for the organization of testing at schools in 2021. PA and TR were responsible for the online surveys and provided guidance to participants, if needed. AU, SRH, and PA carried out the statistical analysis. All authors contributed to the interpretation of study findings. PA and TR wrote the first draft of the manuscript, and all authors critically reviewed and approved the final version of the manuscript.
This study is part of Corona Immunitas research network, coordinated by the Swiss School of Public Health (SSPH+), and funded by fundraising of SSPH+ that includes funds of the Swiss Federal Office of Public Health and private funders (ethical guidelines for funding stated by SSPH+ will be respected), by funds of some Cantons of Switzerland and by institutional funds of the Universities. Additional funding, specific to this study is available from the University of Zurich Foundation. The funder/sponsor did not have any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Goldstein E , Lipsitch M , Cevik M . On the Effect of Age on the Transmission of SARS-CoV-2 in Households, Schools, and the Community. J Infect Dis. 2021 Feb;223(3):362–9. https://doi.org/10.1093/infdis/jiaa691
2. Viner RM , Russell SJ , Croker H , Packer J , Ward J , Stansfield C , et al. School closure and management practices during coronavirus outbreaks including COVID-19: a rapid systematic review. Lancet Child Adolesc Health. 2020 May;4(5):397–404. https://doi.org/10.1016/S2352-4642(20)30095-X
3. Hoang A , Chorath K , Moreira A , Evans M , Burmeister-Morton F , Burmeister F , et al. COVID-19 in 7780 pediatric patients: A systematic review. EClinicalMedicine. 2020 Jun;24:100433. https://doi.org/10.1016/j.eclinm.2020.100433
4. Levin AT , Hanage WP , Owusu-Boaitey N , Cochran KB , Walsh SP , Meyerowitz-Katz G . Assessing the age specificity of infection fatality rates for COVID-19: systematic review, meta-analysis, and public policy implications. Eur J Epidemiol. 2020 Dec;35(12):1123–38. https://doi.org/10.1007/s10654-020-00698-1
5. Shekerdemian LS , Mahmood NR , Wolfe KK , Riggs BJ , Ross CE , McKiernan CA , et al.; International COVID-19 PICU Collaborative . Characteristics and Outcomes of Children With Coronavirus Disease 2019 (COVID-19) Infection Admitted to US and Canadian Pediatric Intensive Care Units. JAMA Pediatr. 2020 Sep;174(9):868–73. https://doi.org/10.1001/jamapediatrics.2020.1948
6. Stringhini S , Wisniak A , Piumatti G , Azman AS , Lauer SA , Baysson H , et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies in Geneva, Switzerland (SEROCoV-POP): a population-based study. Lancet. 2020 Aug;396(10247):313–9. https://doi.org/10.1016/S0140-6736(20)31304-0
7. Ulyte A , Radtke T , Abela IA , Haile SR , Berger C , Huber M , et al. Clustering and longitudinal change in SARS-CoV-2 seroprevalence in school children in the canton of Zurich, Switzerland: prospective cohort study of 55 schools. BMJ. 2021 Mar;372(616):n616. https://doi.org/10.1136/bmj.n616
8. Armann JP , Kirsten C , Galow L , Kahre E , Haag L , Dalpke A , et al. SARS-CoV-2 transmissions in students and teachers: seroprevalence follow-up study in a German secondary school in November and December 2020. BMJ Paediatr Open. 2021 Mar;5(1):e001036. https://doi.org/10.1136/bmjpo-2021-001036
9. Li X , Xu W , Dozier M , He Y , Kirolos A , Theodoratou E ; UNCOVER . The role of children in transmission of SARS-CoV-2: A rapid review. J Glob Health. 2020 Jun;10(1):011101. https://doi.org/10.7189/jogh.10.011101
10. Davies NG , Klepac P , Liu Y , Prem K , Jit M , Eggo RM ; CMMID COVID-19 working group . Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med. 2020 Aug;26(8):1205–11. https://doi.org/10.1038/s41591-020-0962-9
11. Lee B , Raszka WV Jr . COVID-19 in Children: Looking Forward, Not Back. Pediatrics. 2021 Jan;147(1):e2020029736. https://doi.org/10.1542/peds.2020-029736
12. Zimmerman KO , Akinboyo IC , Brookhart MA , Boutzoukas AE , McGann KA , Smith MJ , et al.; ABC SCIENCE COLLABORATIVE . Incidence and Secondary Transmission of SARS-CoV-2 Infections in Schools. Pediatrics. 2021 Apr;147(4):e2020048090. https://doi.org/10.1542/peds.2020-048090
13. Chernozhukov V , Kasahara H , Schrimpf P . The association of opening K-12 schools with the spread of COVID-19 in the United States: county-level panel data analysis. Proc Natl Acad Sci USA. 2021 Oct;118(42):e2103420118. https://doi.org/10.1073/pnas.2103420118
14. Jehn M , McCullough JM , Dale AP , Gue M , Eller B , Cullen T , et al. Association Between K-12 School Mask Policies and School-Associated COVID-19 Outbreaks - Maricopa and Pima Counties, Arizona, July-August 2021. MMWR Morb Mortal Wkly Rep. 2021 Oct;70(39):1372–3. https://doi.org/10.15585/mmwr.mm7039e1
15. Ulyte A , Radtke T , Abela IA , Haile SR , Ammann P , Berger C , et al. Evolution of SARS-CoV-2 seroprevalence and clusters in school children from June 2020 to April 2021 reflect community transmission: prospective cohort study Ciao Corona. Swiss Med Weekly 2021: 2021;151:w30092. https://doi.org/https://doi.org/10.4414/smw.2021.w30092 https://doi.org/10.4414/SMW.2021.w30092
16. Walsh S , Chowdhury A , Braithwaite V , Russell S , Birch JM , Ward JL , et al. Do school closures and school reopenings affect community transmission of COVID-19? A systematic review of observational studies. BMJ Open. 2021 Aug;11(8):e053371. https://doi.org/10.1136/bmjopen-2021-053371
17. UNICEF . COVID-19 and School Closures. One year of education disruption n.d. https://data.unicef.org/resources/one-year-of-covid-19-and-school-closures/ (accessed 4 July 2021).
18. Buonsenso D , Roland D , De Rose C , Vásquez-Hoyos P , Ramly B , Chakakala-Chaziya JN , et al. Schools Closures During the COVID-19 Pandemic: A Catastrophic Global Situation. Pediatr Infect Dis J. 2021 Apr;40(4):e146–50. https://doi.org/10.1097/INF.0000000000003052
19. Engzell P , Frey A , Verhagen MD . Learning loss due to school closures during the COVID-19 pandemic. Proc Natl Acad Sci USA. 2021 Apr;118(17):e2022376118. https://doi.org/10.1073/pnas.2022376118
20. Brooks JT , Butler JC . Effectiveness of Mask Wearing to Control Community Spread of SARS-CoV-2. JAMA. 2021 Mar;325(10):998–9. https://doi.org/10.1001/jama.2021.1505
21. Rader B , White LF , Burns MR , Chen J , Brilliant J , Cohen J , et al. Mask-wearing and control of SARS-CoV-2 transmission in the USA: a cross-sectional study. Lancet Digit Health. 2021 Mar;3(3):e148–57. https://doi.org/10.1016/S2589-7500(20)30293-4
22. Lopes H , Middleton J , De Guchtenaere A , Hadjipanayis A ; Statement From the Association of Schools of Public Health in the European Region and the European Academy of Paediatrics . COVID-19 and the Use of Masks by Children. Front Pediatr. 2021 Jan;9:580150. https://doi.org/10.3389/fped.2021.580150
23. Howard J, Huang A, Li Z, Tufekci Z, Zdimal V, Westhuizen H-M van der, et al. An evidence review of face masks against COVID-19. Proc Natl Acad Sci 2021;118. https://doi.org/https://doi.org/10.1073/pnas.2014564118.
24. Chu DK , Akl EA , Duda S , Solo K , Yaacoub S , Schünemann HJ , et al.; COVID-19 Systematic Urgent Review Group Effort (SURGE) study authors . Physical distancing, face masks, and eye protection to prevent person-to-person transmission of SARS-CoV-2 and COVID-19: a systematic review and meta-analysis. Lancet. 2020 Jun;395(10242):1973–87. https://doi.org/10.1016/S0140-6736(20)31142-9
25. Lazzarino AI , Steptoe A , Hamer M , Michie S . Covid-19: important potential side effects of wearing face masks that we should bear in mind. BMJ. 2020 May;369:m2003. https://doi.org/10.1136/bmj.m2003
26. Rosner E . Adverse Effects of Prolonged Mask Use among Healthcare Professionals during COVID-19. J Infect Dis Epidemiol. 2020;6(3):130. https://doi.org/10.23937/2474-3658/1510130
27. Irfan M , Akhtar N , Ahmad M , Shahzad F , Elavarasan RM , Wu H , et al. Assessing Public Willingness to Wear Face Masks during the COVID-19 Pandemic: Fresh Insights from the Theory of Planned Behavior. Int J Environ Res Public Health. 2021 Apr;18(9):4577. https://doi.org/10.3390/ijerph18094577
28. Taylor S , Asmundson GJ . Negative attitudes about facemasks during the COVID-19 pandemic: the dual importance of perceived ineffectiveness and psychological reactance. PLoS One. 2021 Feb;16(2):e0246317. https://doi.org/10.1371/journal.pone.0246317
29. Haischer MH , Beilfuss R , Hart MR , Opielinski L , Wrucke D , Zirgaitis G , et al. Who is wearing a mask? Gender-, age-, and location-related differences during the COVID-19 pandemic. PLoS One. 2020 Oct;15(10):e0240785. https://doi.org/10.1371/journal.pone.0240785
30. Ulyte A , Radtke T , Abela IA , Haile SR , Braun J , Jung R , et al. Seroprevalence and immunity of SARS-CoV-2 infection in children and adolescents in schools in Switzerland: design for a longitudinal, school-based prospective cohort study. Int J Public Health. 2020 Dec;65(9):1549–57. https://doi.org/10.1007/s00038-020-01495-z
31. Migration im Kanton Zürich . 2020. Kanton Zür Migr 2021. https://www.zh.ch/content/dam/zhweb/bilder-dokumente/organisation/sicherheitsdirektion/migrationsamt/Zahlen%20und%20Fakten%202020.pdf (accessed 2 December 2021).
32. Statistisches Amt des Kantons Zürich. Statistisches Jahrbuch des Kantons Zürich 2018 2018. https://www.zh.ch/de/news-uebersicht/medienmitteilungen/2018/04/statistisches-jahrbuch-des-kantons-zuerich-2018-schwerpunkt-armut.html (accessed 2 December 2021).
33. West EA , Anker D , Amati R , Richard A , Wisniak A , Butty A , et al.; Corona Immunitas Research Group . Corona Immunitas: study protocol of a nationwide program of SARS-CoV-2 seroprevalence and seroepidemiologic studies in Switzerland. Int J Public Health. 2020 Dec;65(9):1529–48. https://doi.org/10.1007/s00038-020-01494-0
34. R Core Team . R: A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria: 2020.
35. Wickham H , Averick M , Bryan J , Chang W , McGowan LD , François R , et al. Welcome to the Tidyverse. J Open Source Softw. 2019;4(43):1686. https://doi.org/10.21105/joss.01686
36. Sjoberg DD , Whiting K , Curry M , Lavery JA , Larmarange J . Reproducible Summary Tables with the gtsummary Package. R J. 2021;13(1):570–80. https://doi.org/10.32614/RJ-2021-053
37. World Health Organization (WHO) and United Nations Children’s Fund . Advice on the use of masks for children in the community in the context of COVID-19: annex to the advice on the use of masks in the context of COVID-19 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-IPC_Masks-Children-2020.1
38. Goh DY , Mun MW , Lee WL , Teoh OH , Rajgor DD . A randomised clinical trial to evaluate the safety, fit, comfort of a novel N95 mask in children. Sci Rep. 2019 Dec;9(1):18952. https://doi.org/10.1038/s41598-019-55451-w
39. Smart NR , Horwell CJ , Smart TS , Galea KS . Assessment of the Wearability of Facemasks against Air Pollution in Primary School-Aged Children in London. Int J Environ Res Public Health. 2020 Jun;17(11):3935. https://doi.org/10.3390/ijerph17113935
40. Eberhart M , Orthaber S , Kerbl R . The impact of face masks on children-A mini review. Acta Paediatr. 2021 Jun;110(6):1778–83. https://doi.org/10.1111/apa.15784
41. Chuang Y , Liu JC . Who wears a mask? Gender differences in risk behaviors in the COVID-19 early days in Taiwan. Econ Bull. 2020;40:2619–27.
42. Rieger MO . To wear or not to wear? Factors influencing wearing face masks in Germany during the COVID-19 pandemic. Soc Health Behav. 2020;3(2):50. https://doi.org/10.4103/SHB.SHB_23_20
43. Shelus VS , Frank SC , Lazard AJ , Higgins IC , Pulido M , Richter AP , et al. Motivations and Barriers for the Use of Face Coverings during the COVID-19 Pandemic: Messaging Insights from Focus Groups. Int J Environ Res Public Health. 2020 Dec;17(24):9298. https://doi.org/10.3390/ijerph17249298
44. Wilson RF , Sharma AJ , Schluechtermann S , Currie DW , Mangan J , Kaplan B , et al. Factors Influencing Risk for COVID-19 Exposure Among Young Adults Aged 18-23 Years - Winnebago County, Wisconsin, March-July 2020. MMWR Morb Mortal Wkly Rep. 2020 Oct;69(41):1497–502. https://doi.org/10.15585/mmwr.mm6941e2
45. Zhang B , Li Z , Jiang L . The Intentions to Wear Face Masks and the Differences in Preventive Behaviors between Urban and Rural Areas during COVID-19: An Analysis Based on the Technology Acceptance Model. Int J Environ Res Public Health. 2021 Sep;18(19):9988. https://doi.org/10.3390/ijerph18199988
46. Statista Research Department . Bildungsstand der Wohnbevölkerung im Kanton Zürich nach höchster abgeschlossener Ausbildung im Jahr 2019. Bild Wohnbevölk Im Kanton Zür Nach Höchster Abgeschloss Ausbild Im Jahr 2019 2021. https://de.statista.com/statistik/daten/studie/1241630/umfrage/bildungsstand-der-bevoelkerung-im-kanton-zuerich/ (accessed July 15, 2021).
The supplementary tables and figures are available in the PDF version of this article.