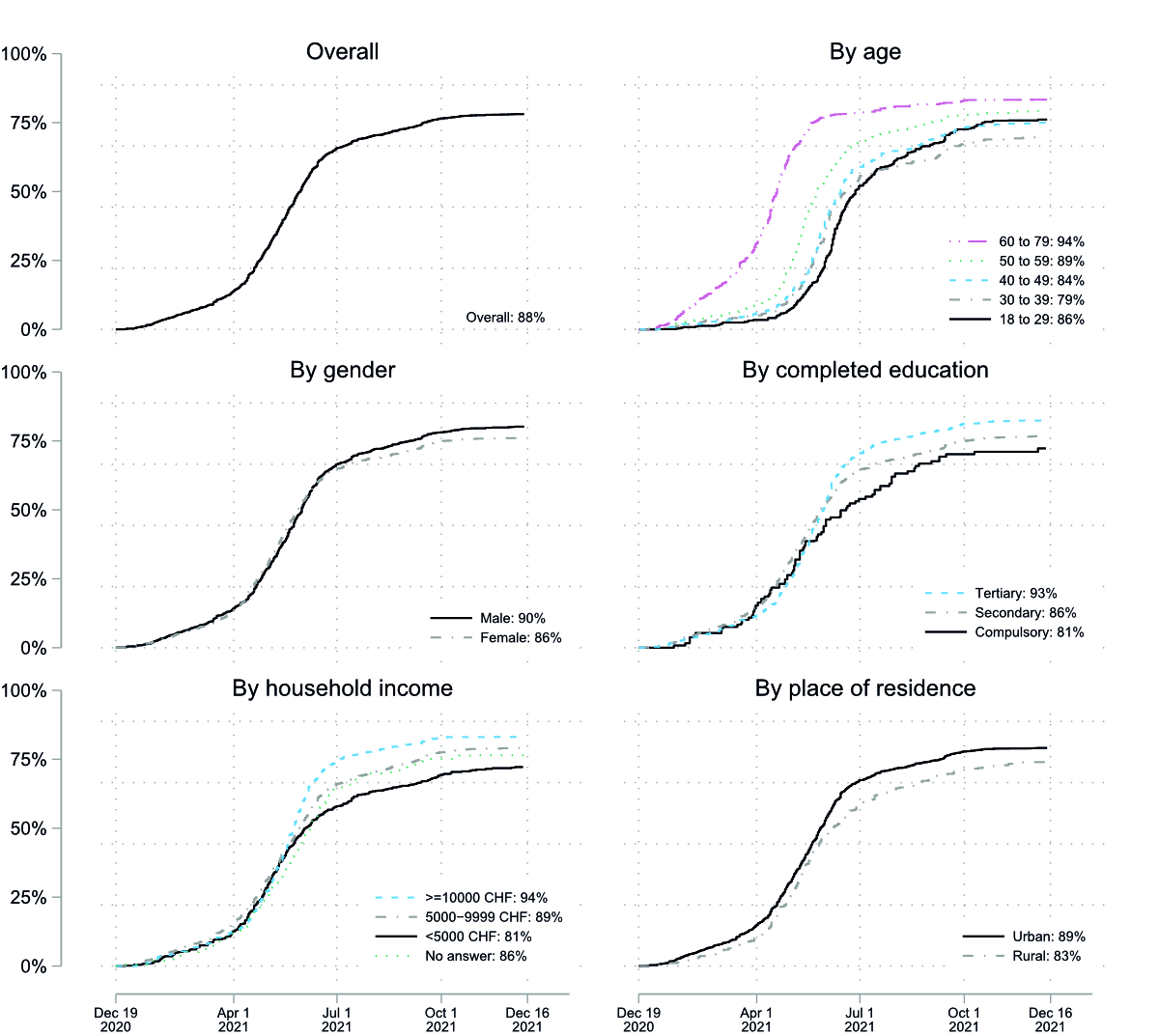
Figure 1 COVID-19 vaccine uptake over time (first vaccine dose), overall and by subgroups. Kaplan-Meier curves.
DOI: https://doi.org/10.4414/SMW.2022.w30162
SARS-CoV-2 infection numbers and associated morbidity and mortality are still on the rise worldwide. However, the rapid development of effective vaccines against COVID-19 has been a fundamental step towards controlling the pandemic and protecting health systems. Infections, hospitalisations and mortality rates have been shown to be mitigated by vaccinating large parts of the population [1]. Thus, widespread uptake of vaccines is key [2]. However, uptake progressed differently between and within countries owing to challenges in production and distribution of the vaccine, affordable pricing, global allocation and administration of doses [3]. Early in 2021, Israel had administered the most vaccines against COVID-19 per capita worldwide [4]. Also, the UK as well as Canada conducted fast vaccination campaigns [5]. In Europe, by 30 November 2021, Iceland and Portugal show the highest and the Western Balkan countries the lowest vaccination rates. Switzerland, however, shows the lowest vaccination rates compared with other countries in Western and Central Europe. These low rates are similar to the ones found in the United States [6].
After vaccines had become widely available, many countries faced the issue of widespread vaccine hesitancy. Vaccine hesitancy delays immunisation of the population and leads to substantial parts of the population not being vaccinated. Consequently, the benefits of vaccination in terms of containing the spread of the pandemic, protecting vulnerable groups and mitigating severe outcomes cannot be fully realised and future outbreaks of COVID-19 might be amplified [7, 8]. The most frequently identified reasons related to vaccine hesitancy include the desire to wait and see if the vaccine is safe, fear of side effects, belief in the superiority of natural immunity, and lack of trust in government and health authorities [9–11]. Sociodemographic differences are important determinants of vaccine acceptance [12, 13]. Systematic reviews found that being female, younger, of lower income and having a lower education level, belonging to an ethnic minority group and living in a rural area were consistently associated with lower intentions to get vaccinated [14, 15].
Compared with Israel or the UK, Switzerland had a rather late and slow start to the vaccination campaign. The canton of Lucerne was one of the first to administer vaccines, on 23 December 2020 [16]; the other cantons followed shortly. Priority was given to the elderly and the chronically ill, and, secondly, to healthcare workers and those living with people at risk [17]. By about May 2021, access to vaccines was opened to the general population aged 16 and over, and by the beginning of June 2021, children and adolescents aged 12 to 15 could get vaccinated. Different national and cantonal campaigns were set in place to inform people about the vaccine and to motivate the public and certain subgroups such as the young or foreigners to get vaccinated. From September 2021 on, a “COVID certificate” similar to the EU-issued “Green Pass” for the vaccinated, recovered or negatively tested was declared mandatory to access indoor hospitality venues, cultural, sporting and leisure activities indoors, and large-scale outdoor events [18], putting more pressure on the unvaccinated. Other measures were a national vaccination week at the beginning of November consisting of around 170 additional mobile vaccination centres and personalised advisory services [19]. By 20 December, 69% of the total Swiss population (including children) had received one dose of vaccine according to official statistics, and 67% had been fully vaccinated (generally, two doses; those recovered from COVID-19, one dose) [20]. This places Switzerland among the countries with lower vaccination rates in Europe.
Previous Swiss studies focused on vaccination attitudes and willingness to vaccinate, but not on vaccination uptake itself [21–23]. The aim of this study was to investigate the detailed development of COVID-19 vaccination uptake in Switzerland and subgroup heterogeneities over time. The results give detailed insights into socioeconomic and other differences in uptake. Findings contribute to the understanding of the challenges related to widespread vaccine hesitancy and may provide a valuable basis to inform future COVID-19 vaccination or other health prevention campaigns.
We used data from the COVID-19 Social Monitor, a large cohort study of the Swiss resident population aged 18 to 79 years with online access [24, 25]. The study covers various public health issues and started surveying the population at the beginning of the COVID-19 pandemic. The questionnaire used includes mostly validated items from established population surveys, mainly the Swiss Health Survey (SHS, https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/erhebungen/SHS.html), the Swiss Household Panel (SHP, https://forscenter.ch/projekte/swiss-household-panel), and the Study on Health, Ageing and Retirement (SHARE, http://www.share-project.org). Some items were adapted to fit the context of the pandemic. Questions regarding the COVID-19 pandemic and COVID-19 vaccination uptake were newly developed, expert-reviewed and closely coordinated with another major Swiss COVID-19 population survey, the Corona Immunitas Digital Follow-Up eCohort [26].
Participants were randomly sampled from an online panel whose members have been actively recruited using random probability sampling based on national landline telephone directories and random digit dialing of mobile phone numbers. The sampling process was stratified by age, gender and language region, and is representative of the Swiss resident population (census of 2018) in this regard. An initial sample of 2026 respondents participated in the survey, beginning in March 2020, and was complemented with an additional sample of 1355 from December 2020 onwards. Respondents were surveyed approximately every five to eight weeks during the study period. The last responses included in this analysis were from survey wave 20 with a data-collection period from 6 to 16 December 2021. Table 1 shows the sample size and non-participation rates of the different survey waves. We included 2553 study participants with at least one response to the item on vaccination uptake we introduced on 7 June 2021. We excluded 85 cases (3.3%) because of one or more missing covariates (1 case with missing migration status, 7 for health literacy, 76 for trust in government and trust in science, 2 for trust in science only). Our final analysis sample consists of 2448 cases.
Table 1Overview of COVID-19 Social Monitor sample size and nonparticipation by wave.
| Survey wave | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
| Survey start | 30 March 2020 | 6 April 2020 | 14 April 2020 | 27 April 2020 | 11 May 2020 | 25 May 2020 | 15 June 2020 |
| No. of initial sample | 2026 | 2026 | 2026 | 2026 | 2026 | 2026 | 2026 |
| No. of additional sample | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| No. of combined sample | 2026 | 2026 | 2026 | 2026 | 2026 | 2026 | 2026 |
| No. of participants | 2026 | 1537 | 1540 | 1729 | 1673 | 1616 | 1522 |
| Nonparticipation (%) | 0 | 24 | 24 | 15 | 17 | 20 | 25 |
| Survey wave | 8 | 9 | 10 | 11 | 12 | 13 | 14 |
| Survey start | 14 July 2020 | 17 August 2020 | 28 September 2020 | 9 November 2020 | 14 December 2020 | 25 January 2021 | 22 February 2021 |
| No. of initial sample | 2026 | 2026 | 2026 | 2026 | 2026 | 2026 | 2026 |
| No. of additional sample | 0 | 0 | 0 | 0 | 1355 | 1355 | 1355 |
| No. of combined sample | 2026 | 2026 | 2026 | 2026 | 3381 | 3381 | 3381 |
| No. of participants | 1508 | 1532 | 1511 | 1492 | 2802 | 2564 | 2346 |
| Nonparticipation (%) | 26 | 24 | 25 | 26 | 17 | 24 | 31 |
| Survey wave | 15 | 16 | 17 | 18 | 19 | 20 | |
| Survey start | 29 March 2021 | 3 May 2021 | 7 June 2021 | 30 August 2021 | 18 October 2021 | 6 December 2021 | |
| No. of initial sample | 2026 | 2026 | 2026 | 2026 | 2026 | 2026 | |
| No. of additional sample | 1355 | 1355 | 1355 | 1355 | 1355 | 1355 | |
| No. of combined sample | 3381 | 3381 | 3381 | 3381 | 3381 | 3381 | |
| No. of participants | 2219 | 2154 | 2095 | 1921 | 1947 | 1951 | |
| Nonparticipation (%) | 34 | 36 | 38 | 43 | 42 | 42 |
The survey was pseudonymised. The identity of the participants is known only to the panel provider and strictly separated from data collection and the researchers. De-anonymisation of the data was prevented by legal restrictions.Further details on the study methodology and design, as well as baseline characteristics of the sample, are presented in a previously published paper [24]. The data are available under https://doi.org/10.48620/22. Vaccination dates were removed from the published data to protect respondents’ privacy. We provide the rounded time (in days) from study entry to vaccination, upon request. The research question analysed in this paper had not been anticipated when planning the study and no protocol has been registered.
COVID-19 vaccine uptake was elicited from wave 17 onwards (7 June 2021) by asking respondents retrospectively whether and when they received their first vaccine dose (“Have you been vaccinated against the coronavirus (at least one dose)?”, “When have you received your first dose?”). First-dose vaccination is a valid measure of vaccine uptake as there is so far no evidence of any non-uptake of second doses on a relevant scale. Further, this operationalisation also fits for those with a prior SARS-CoV-2 infection who were recommended to get only one dose of vaccine, and to those few receiving the Johnson and Johnson vaccine that requires only one dose. Respondents who had not received a first dose of the vaccine when last surveyed were asked about the reasons for not being vaccinated.
For subgroup comparisons and as potential determinants for uptake, we included three sets of predictors, which we selected a priori based on theoretical considerations. Besides basic sociodemographics we included health literacy, adherence to COVID-19 prevention measures, and trust, which are all highlighted as important determinants of COVID-19 vaccine uptake in the literature:
1. Basic sociodemographics: age (18 to 29; 30 to 39; 40 to 49; 50 to 59; 60 to 79), gender (male; female), completed education (compulsory schooling; secondary degree II; tertiary degree), household income (CHF <5000; CHF 5000–9999; CHF ≥10,000; no answer), place of residence (urban; rural), language region (German-, French-, Italian-speaking), and migration background (Swiss-born; foreign-born), chronic condition (yes; no) including hypertension, cardiovascular diseases, diabetes, respiratory diseases, cancer and renal disease, excluding mental health disorders and arthrosis/arthritis.
2. Health literacy (problematic/inadequate; sufficient; excellent) measured with an adapted version of the HLS-EU-Q12 scale [27, 28] and, as an indicator for adherence to COVID-19 prevention measures, whether respondents refrained from domestic visits to friends and relatives to protect themselves and others from the coronavirus (rarely; sometimes; mostly). We used responses elicited in December 2020, a time with high infection rates and partial lockdown, when vaccines were not yet available in Switzerland. For respondents not participating in that survey wave, we used responses from previous waves (210 cases).
3. Trust in government and trust in science (“Regarding the COVID-19 pandemic, how much do you trust the following sources?” Swiss government (e.g. Federal Office of Public Health); Science) with the categories low (“little”/“very little”), middle (“moderately”), and high (“strongly”/“very strongly”). We used responses elicited in December 2020, just before the start of the vaccination campaign. For respondents not participating in that survey wave, we used responses from previous waves, or, if none were available, from subsequent follow-up waves (133 cases for trust in government, 134 cases for trust in science).
We calculated COVID-19 vaccine uptake rates as the proportion of participants having received a first dose at a particular point in time up to the end of the study period on 16 December 2021 using Kaplan-Meier estimation. Results are reported as Kaplan-Meier curves and as rates by the end of the study period.
We then compared uptake rates over time of the above-specified subgroups using Cox regression survival analysis. Cox regression allows for a relative comparison of uptake rates at different points in time and accounts for right-censoring. The observation period under consideration started on 19 December 2020, the day when vaccines first became available in Switzerland. The observation period ended with an individual’s last survey participation, i.e., at the latest with the end of the study period on 16 December 2021, or the date of vaccination, whichever came first. To account for the age-specific availability of vaccines and vaccination progress, we stratified all analyses by age (categorised by 18 to 29, 30 to 39, 40 to 49, 50 to 59, and 60 to 79 years). This allows for different baseline hazard ratios (HRs) by age group, while keeping HRs for other predictors equal. We estimated three multivariable models using the described predictor sets. We report unadjusted (from univariable regression models) HRs and adjusted (from multivariable) HRs with 95% confidence intervals (CIs). We tested the proportional-hazards assumption using Schoenfeld’s test. We found a violation of the assumption for gender (p = 0.02), the Italian vs the German language region (p = 0.04), and for excellent vs problematic/inadequate health literacy (p = 0.04); the global p-value was <0.001. Consequently, we carried out separate analyses by gender to check the robustness of our results (see supplementary tables S1 and S2 in the appendix).
Finally, we report the reasons for not being vaccinated as proportions of the nonvaccinated according to responses in the last survey wave (overall, and by gender). Data analysis was carried out with Stata/SE version 17.0, the analysis do-files are provided in the supplement S4.
We used weights to correct for sampling and attrition bias as described in Moser et al. [25]. In brief, sampling weights were constructed using variables age, gender, and language region and the 2018 Swiss census data as reference. Attrition weights used additional information about employment status, living with a partner or not, and highest attained education. Details on the weighting strategy including a sensitivity analysis regarding alternative modelling strategies are provided in supplement S3.
The Cantonal Ethics Commission of Zurich concluded that the current study does not fall within the scope of the Human Research Act (BASEC-Nr. Req-2020-00323). The study is a pseudonymised survey. Participants gave their general consent to be part of research studies when accepting the panel provider’s invitation to the online panel from which we sampled respondents. Explicit informed consent was therefore not needed from participants for this study. Participation in the study was voluntary and participants could always withdraw.
Table 2 shows the characteristics of study participants and the resulting proportions when applying sampling weights. We analysed responses from 2448 study participants. Half of the study population was 50 years or older (54%) with an equal distribution of men and women. A majority of study participants had secondary school as the highest achieved education level (68%), reported a monthly income of below CHF 10,000 (70%), had no chronic disease condition (65%) and lived in an urban area (80%).
Table 2Characteristics of study population (n = 2448).
* Using weighted sample
By the end of the study period on 16 December 88% of the study population had received their first dose of COVID-19 vaccine (fig. 1). Vaccinations had started by the end of December 2020; rates progressed slowly until April and then increased steeply until the end of June when progress (first dose) slowed down considerably after having reached an overall prevalence of about 70% of the study population. The slowdown began earlier and was particularly marked among the elderly who had early access to vaccination, whereas rates for the younger with delayed eligibility continued to soar until about October. After October, rates continued to increase constantly but only slowly until the end of the study period.
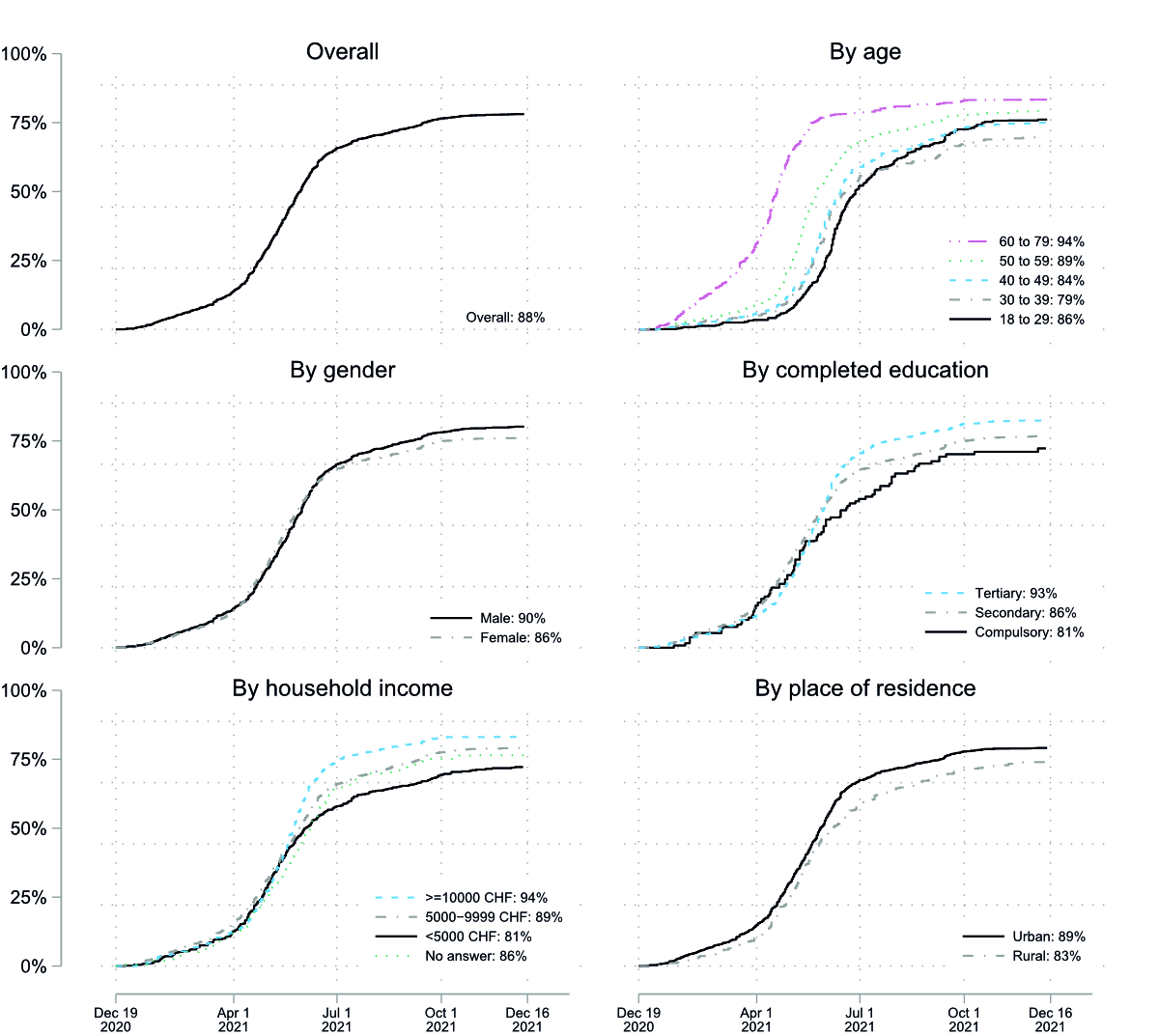
Figure 1 COVID-19 vaccine uptake over time (first vaccine dose), overall and by subgroups. Kaplan-Meier curves.
Vaccination uptake differed considerably between age groups; in particular, the elderly aged 60 to 79 years showed a much earlier and faster uptake. Between other soci-demographic groups there were differences too, albeit on a smallerscale: respondents with compulsory schooling, with lower household income as well as those living in rural regions showed a slower uptake and a lower rate at the end of the study period. Respondents with compulsory schooling showed the lowest rate at 81%, those in the income group CHF ≥10,000 the highest at 94%.
Compared to official data provided by the Federal Office of Public Health [20], our sample showed considerably higher vaccination rates. Depending on age group, rates were between 4 (age group 70 to 79 years) and 15 percentage points (20 to 29) higher than the official vaccination rates (table 3).
Table 3COVID-19 vaccine uptake of the study population and of the general population according to official vaccination rates provided by the Federal Office of Public Health (FOPH) by age group as of 16 December 2021.
| Age groups (in years) | ||||||
| 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | |
| Official rates (FOPH) | 71% | 73% | 77% | 81% | 86% | 91% |
| Study sample | 86% | 79% | 84% | 89% | 93% | 95% |
Rates for study sample are based on weighted Kaplan-Meier estimates.
Table 4 shows uptake rates and HRs from age-stratified univariable and age-stratified multivariable analysis of the three models, including different sets of predictors. Unadjusted HRs from the age-stratified univariable analysis, without additional covariates, showed that uptake was lower for females than males (HR 0.89, 95% CI 0.81–0.97), increased with educational level (secondary: HR 1.39, 95% CI 1.10–1.76; tertiary: HR 1.94, 95% CI 1.52–2.47) and household income (CHF 5000–9999, HR 1.42, 95% CI 1.25–1.61; CHF ≥10,000: HR 1.99, 95% CI 1.72–2.30), and was lower for respondents residing in rural vs in urban regions (HR 0.79, 95% CI 0.70–0.88). No differences could be found for migration background and language region. Individuals with a chronic condition showed a higher uptake rate than those without (HR 1.38, 95% CI 1.25–1.53).
Table 4COVID-19 vaccine uptake and Cox proportional hazard ratios from univariable and multivariable analyses (N=2,448).
| Uptake a (%) | Unadj HR b | (95% CI) | Adj HR Model 1 c | (95% CI) | Adj HR Model 2 c | (95% CI) | Adj HR Model 3 c | (95% CI) | |
| Gender | |||||||||
| Male | 90 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Female | 86 | 0.89 | (0.81–0.97) | 0.97 | (0.88–1.06) | 0.94 | (0.86–1.03) | 0.92 | (0.84–1.01) |
| Education | |||||||||
| Compulsory | 81 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Secondary | 86 | 1.39 | (1.10–1.76) | 1.23 | (0.98–1.55) | 1.23 | (0.97–1.56) | 1.12 | (0.89–1.41) |
| Tertiary | 93 | 1.94 | (1.52–2.47) | 1.59 | (1.25–2.02) | 1.58 | (1.24–2.03) | 1.32 | (1.03–1.68) |
| Household income | |||||||||
| CHF <5000 | 81 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| CHF 5000–9999 | 89 | 1.42 | (1.25–1.61) | 1.37 | (1.21–1.56) | 1.35 | (1.19–1.54) | 1.28 | (1.13–1.46) |
| CHF ≥10,000 | 94 | 1.99 | (1.72–2.30) | 1.81 | (1.55–2.10) | 1.76 | (1.51–2.05) | 1.69 | (1.45–1.98) |
| No answer | 86 | 1.39 | (1.16–1.66) | 1.40 | (1.17–1.67) | 1.38 | (1.15–1.65) | 1.36 | (1.14–1.63) |
| Migration background | |||||||||
| Swiss-born | 88 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Foreign-born | 88 | 1.04 | (0.90–1.20) | 0.99 | (0.86–1.14) | 0.97 | (0.84–1.12) | 0.95 | (0.83–1.10) |
| Place of residence | |||||||||
| Urban | 89 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Rural | 83 | 0.79 | (0.70–0.88) | 0.80 | (0.72–0.90) | 0.79 | (0.70–0.88) | 0.78 | (0.70–0.88) |
| Language region | |||||||||
| German | 88 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| French | 89 | 1.04 | (0.93–1.16) | 1.00 | (0.89–1.12) | 1.03 | (0.92–1.15) | 0.99 | (0.88–1.11) |
| Italian | 89 | 0.94 | (0.84–1.05) | 0.90 | (0.79–1.01) | 0.88 | (0.78–1.00) | 0.89 | (0.79–1.00) |
| Chronic condition | |||||||||
| No | 85 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 94 | 1.38 | (1.25–1.53) | 1.41 | (1.27–1.56) | 1.39 | (1.25–1.53) | 1.38 | (1.25–1.53) |
| Health literacy | |||||||||
| Problematic/inadequate | 85 | 1.00 | 1.00 | 1.00 | |||||
| Sufficient | 91 | 1.13 | (0.98–1.29) | 1.07 | (0.93–1.23) | 1.01 | (0.88–1.16) | ||
| Excellent | 90 | 1.21 | (1.10–1.34) | 1.19 | (1.08–1.32) | 1.10 | (0.99–1.21) | ||
| Adherence to prevention measures (refrained from visits) | |||||||||
| Rarely | 75 | 1.00 | 1.00 | 1.00 | |||||
| Sometimes | 88 | 1.56 | (1.33–1.84) | 1.56 | (1.32–1.85) | 1.36 | (1.15–1.61) | ||
| Mostly | 91 | 1.67 | (1.46–1.91) | 1.67 | (1.46–1.91) | 1.42 | (1.24–1.62) | ||
| Trust in government | |||||||||
| Low | 63 | 1.00 | 1.00 | ||||||
| Middle | 81 | 1.76 | (1.45–2.14) | 1.41 | (1.14–1.74) | ||||
| High | 94 | 2.70 | (2.28–3.20) | 1.74 | (1.42–2.14) | ||||
| Trust in science | |||||||||
| Low | 65 | 1.00 | 1.00 | ||||||
| Middle | 81 | 1.69 | (1.39–2.05) | 1.32 | (1.06–1.65) | ||||
| High | 94 | 2.65 | (2.21–3.17) | 1.64 | (1.31–2.05) | ||||
CI confidence interval; HR hazard ratio.
a Uptake based on weighted Kaplan-Meier estimates as of last common censoring date across all subgroups (8 December); b stratified by age; c stratified by age and adjusted for all the other variables included in the model as shown.
A separate analysis by gender (see supplementary tables S1 and S2) showed some few gender-specific differences: women living in rural areas had an even lower vaccination uptake than their male counterparts; men with lower health literacy showed a lower uptake than those with higher health literacy, whereas there was no statistically significant difference for females in this regard. For other predictors, we see no substantial differences.
Results from the multivariable model including basic sociodemographic predictors (model 1) are comparable to the ones from the univariable analysis with some slightly smaller hazard ratios. In model 2, after adjustment for sociodemographics, a higher level of health literacy showed a positive association with uptake (sufficient: HR 1.07, 95% CI 0.93–1.23; excellent: HR 1.19, 95% CI 1.08–1.32; reference category: problematic/inadequate), as did stronger adherence to COVID-19 prevention measures (refrained from domestic visits). In multivariable model 3, which additionally included trust in government and science, a strong positive association with both trust in government and trust in science was found.
The 12% of respondents not being vaccinated according to the last survey wave with responses collected from 6 to 16 December indicated fears of side effects (reported by 57% of the not vaccinated), doubts regarding the effectiveness of the vaccine (57%), and a preference for natural/traditional remedies (36%) as main reasons against the vaccine. Twenty-one percent reported having had a COVID-19 infection as a reason against a vaccination (fig. 2). Only 4% mentioned medical reasons. Separate analysis by gender showed a similar pattern, with females reporting slightly more often fears of side effects and having had a COVID-19 infection and with males questioning more frequently the vaccines’ effectiveness and whether COVID-19 posed an actual threat to them (“A COVID-19 infection is not dangerous for me.”).
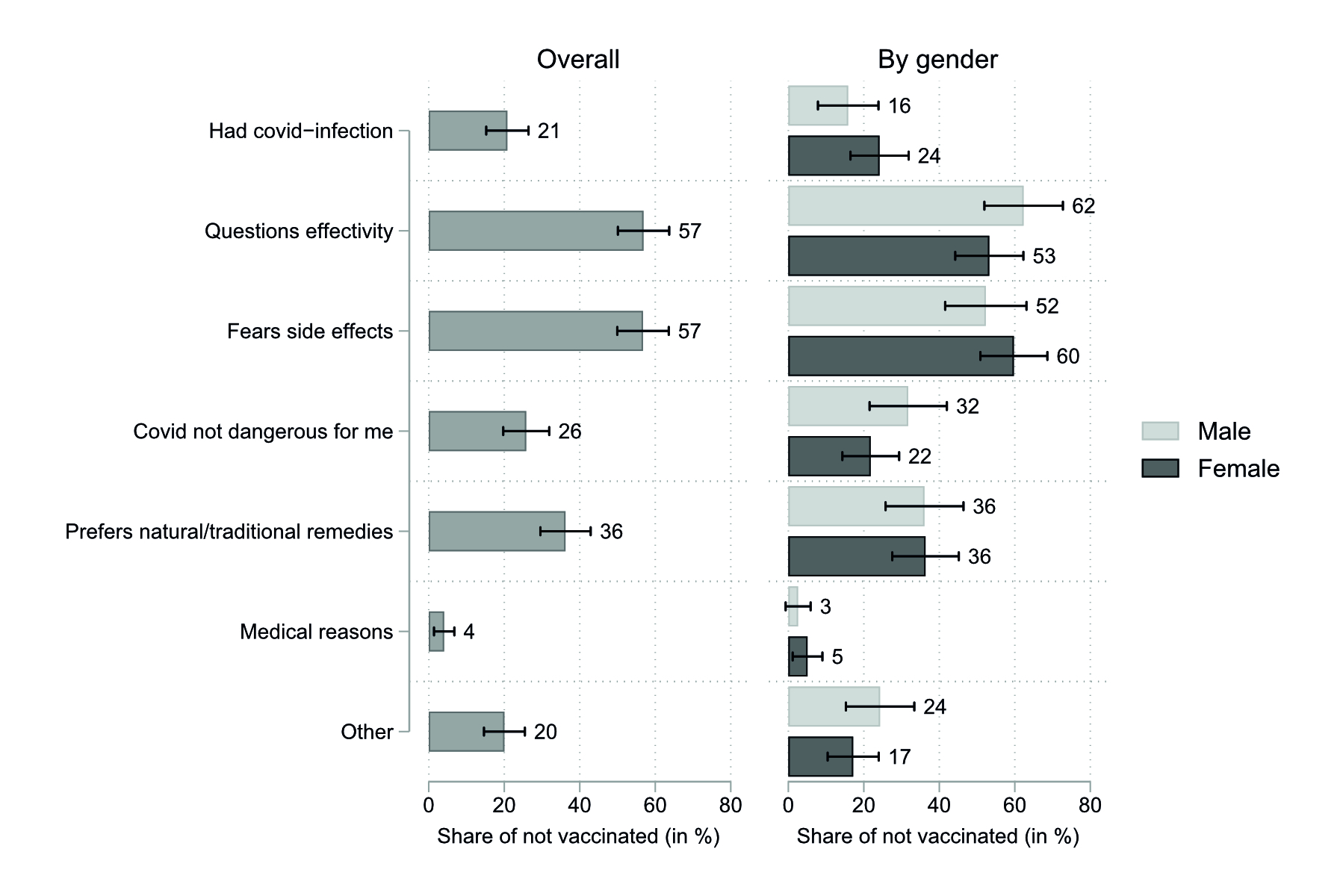
Figure 2 Stated reasons for not being vaccinated at the end of study period overall and by gender. Multiple responses possible. n = 227 (94 males, 133 females), cases weighted to correct for sampling and wave-nonresponse.
Although vaccine uptake in Switzerland progressed quickly after a slow beginning due to a lack of vaccine availability, uptake slowed down by the end of June 2021, when about 70% in our study population had received their first dose. Vaccine availability was no longer an issue at that time, but significant vaccine hesitancy, indifference and, possibly, implicit accessibility barriers among all age groups curbed the further increase in uptake rates. Most apparent differences in uptake could be found between respondents with low and high levels of completed education, low and high household income, rural vs urban regions of residence, and between those with and without a chronic condition. None or only small differences could be found between genders, the language regions and between respondents with and without migration background. Lower vaccine uptake was associated with lower health literacy (for males, but not for females), lower adherence to COVID-19 prevention measures, as well as with low levels of trust in government and science.
Similar patterns regarding age groups, household income, education level, gender and migration background were observed in analyses based on data from a nationwide Swiss seroprevalence study [29]. Moreover, widespread vaccine hesitancy has been observed in Switzerland for other vaccines , such as human papillomavirus (HPV) [7, 30], measles [31] and influenza [32]. These studies found a pattern similar to our results with regard to lower vaccination uptake in rural compared with urban areas [30–32]. For HPV vaccines, fear of side effects and general opposition to vaccination were two main reasons for not being vaccinated [33], but also accessibility to HPV vaccines, i.e. the existence and the scope of cantonal vaccination programmes led to differences in vaccination rates [34, 35]. Accessibility has likely played a role in COVID-19 vaccination uptake too. (Online) registration procedures, as well as problems with getting time off work to get vaccinated, might have posed something of a hurdle to persons with lower education levels or a migration background, in particular when coupled with a lack of social support or a nonexistent established primary care relationship.
Interestingly, we did not find systematic differences between the language regions, even though pronounced differences between Swiss cantons exist, with the vaccination rate for the total population ranging from 55.9–70.7% [20]. Such differences might be explained by local context and the federal organisation of the vaccination programmes in Switzerland. Neighbouring countries show large differences in vaccination rates: Germany (71.2%) and Austria (70.1%) have lower vaccination rates for the total population compared with Italy (74.3%) and France (73.6%) (see [36]). This, however, does not seem to translate into sizeable differences between the Swiss language regions. Whereas raw uptake rates are almost identical between the language regions, hazard ratios for the Italian language region are <1 (albeit not significantly different from unity at the 5% level). This is a result of a seemingly lower vaccination rate in the Ticino after control for age (age-stratified univariable model) and other covariates (age-stratified multivariable models).
In the case of COVID-19, extensive misinformation since the beginning of the pandemic nourished mistrust in science and public health authorities [37]. Hence, the type of sources trusted and used to obtain vaccination-related information plays a crucial role in decisions about COVID-19 vaccination as the association between misinformation and vaccine hesitancy is well documented [12, 38]. Furthermore, even though the relationship between health literacy and uptake of childhood vaccines or influenza vaccination remains unclear [39], levels of low health literacy have been shown to be related to COVID-19 vaccine hesitancy [37].
Our data provide no information about the effectiveness of public health measures intended to increase vaccination rates. Presently, using incentives and penalties to encourage vaccination is intensively debated. Research has shown that even small financial incentives can strongly increase the usage of a COVID-19 contact tracing app [40]. Incentives such as remunerations, vaccination possibilities at local doctors’ practices or providing more freedom have been shown in a hypothetical factorial survey experiment in Germany to be effective, but to different degrees depending on the age of respondents [41]. Also, mandatory COVID-19 certificates seem to increase vaccination uptake, especially among the young [42]. However, the overall effect of such measures is highly context-specific and hard to predict for the current Swiss situation.
The fact that individuals with lower educational levels and lower health literacy show a lower COVID-19 vaccination uptake, and that fears of side effects and doubts about the efficacy of the vaccine are prominent reasons against vaccination suggests that the risk and benefits of being vaccinated should be communicated more broadly and in a more comprehensible way. Also, vaccination campaigns require a determined effort from local/cantonal authorities and should be planned from early on to be as accessible as possible for the whole population, including persons with poor local language and/or reading skills, limited time availability, or in otherwise disadvantaged situations that might pose barriers to vaccination [43]. As lower uptake is associated with low trust in government and science, actors other than government agencies and scientists might be more successful in communicating the benefits of being vaccinated to subgroups with low uptake rates. Local doctors and local politicians or other recognised public persons might be better suited. Implementing strategies based on behavioural science insights such as nudge techniques or giving people a choice (between various vaccines) might be options to consider [44].
A strength of this study is that not much pressure was put on the unvaccinated in Switzerland; hence, our data reflect well the study populations’ preferences and attitudes towards vaccination. Of course, our study has several limitations such as the selectivity of the sample, which is restricted to persons with online access, good knowledge of Italian, French or German, and capabilities as well as willingness to participate in an online survey on health and other topics related to the pandemic. Persons with migration experience are underrepresented. This selectivity might explain our relatively higher overall vaccination rate compared with official data. Selectivity might have increased with study duration, due to non-random dropouts. Also, self-reporting of the vaccination status might be prone to social desirability bias, even though this might be less of a problem in an online survey and for a behaviour far from being marginal in the surveyed population [45].
After one year of vaccine availability, the COVID-19 vaccine uptake in Switzerland reached a plateau in Switzerland. Uptake rates differed considerably between population subgroups with the less educated, less well-off, and rural population showing the lowest rates. To increase uptake rates and to strengthen future vaccination booster campaigns, efforts should be continued to mitigate fears of unwanted vaccine effects and doubts regarding vaccine effectiveness, and to point out the individual and societal benefits of vaccination – also for healthy, younger individuals. Specifically, targeted measures communicating the risk and benefits of being vaccinated relative to not being vaccinated in a comprehensible way and by trusted individuals might help to counteract low vaccination rates among these subgroups.
We thank Paul Kelly for proofreading the manuscript and two anonymous reviewers for their very good comments which helped us to improve the manuscript.
The study has received funding from the Swiss Federal Office of Public Health and from Health Promotion Switzerland. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Omer SB , Benjamin RM , Brewer NT , Buttenheim AM , Callaghan T , Caplan A , et al. Promoting COVID-19 vaccine acceptance: recommendations from the Lancet Commission on Vaccine Refusal, Acceptance, and Demand in the USA. Lancet. 2021 Dec;398(10317):2186–92. https://doi.org/10.1016/S0140-6736(21)02507-1
2. Strategic Advisory Group of Experts on Immunization SAGE . “WHO SAGE Roadmap for Prioritizing uses of Covid-19 Vaccines in the Context of Limited Supply.” World Health Organization, Oct. 20, 2020. Accessed: 24 Sep. 2021. Online. Available: https://www.who.int/publications/i/item/who-sage-roadmap-for-prioritizing-uses-of-covid-19-vaccines-in-the-context-of-limited-supply
3. Wouters OJ , Shadlen KC , Salcher-Konrad M , Pollard AJ , Larson HJ , Teerawattananon Y , et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. 2021 Mar;397(10278):1023–34. https://doi.org/10.1016/S0140-6736(21)00306-8
4. Our World in Data . “Israel: What share of the population has received at least one dose of the COVID-19 vaccine?” Israel: Coronavirus Pandemic Country Profile, Jul. 24, 2021. https://ourworldindata.org/coronavirus/country/israel#what-share-of-the-population-has-received-at-least-one-dose-of-the-covid-19-vaccine (accessed 26 Jul. 2021).
5. Our World in Data . “Coronavirus (COVID-19) Vaccinations,” Our World in Data, Jul. 24, 2021. https://ourworldindata.org/covid-vaccinations (accessed 26 Jul. 2021).
6. Our World in Data . “Share of people vaccinated against COVID-19 Nov 30, 2021,” Our World in Data, Nov. 30, 2021. https://tinyurl.com/ydncz85s (accessed 02 Feb. 2021).
7. Deml MJ , Jafflin K , Merten S , Huber B , Buhl A , Frau E , et al. Determinants of vaccine hesitancy in Switzerland: study protocol of a mixed-methods national research programme. BMJ Open. 2019 Nov;9(11):e032218. https://doi.org/10.1136/bmjopen-2019-032218
8. Johnson NF , Velásquez N , Restrepo NJ , Leahy R , Gabriel N , El Oud S , et al. The online competition between pro- and anti-vaccination views. Nature. 2020 Jun;582(7811):230–3. https://doi.org/10.1038/s41586-020-2281-1
9 S. H. Adams , J. P. Schaub , J. M. Nagata , M. J. Park , C. D. Brindis , and C. E. Irwin , “Young Adult Perspectives on COVID-19 Vaccinations,” J. Adolesc. Health, p. S1054139X21002858, Jul. 2021, doi: https://doi.org/10.1016/j.jadohealth.2021.06.003.
10. Brandt EJ , Rosenberg J , Waselewski ME , Amaro X , Wasag J , Chang T . National Study of Youth Opinions on Vaccination for COVID-19 in the U.S. J Adolesc Health. 2021 May;68(5):869–72. https://doi.org/10.1016/j.jadohealth.2021.02.013
11. Jennings W , Stoker G , Bunting H , Valgarðsson VO , Gaskell J , Devine D , et al. Lack of Trust, Conspiracy Beliefs, and Social Media Use Predict COVID-19 Vaccine Hesitancy. Vaccines (Basel). 2021 Jun;9(6):593. https://doi.org/10.3390/vaccines9060593
12. Malik AA , McFadden SM , Elharake J , Omer SB . Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine. 2020 Sep;26:100495. https://doi.org/10.1016/j.eclinm.2020.100495
13. Murthy BP , Sterrett N , Weller D , Zell E , Reynolds L , Toblin RL , et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties - United States, December 14, 2020-April 10, 2021. MMWR Morb Mortal Wkly Rep. 2021 May;70(20):759–64. https://doi.org/10.15585/mmwr.mm7020e3
14. Cascini F , Pantovic A , Al-Ajlouni Y , Failla G , Ricciardi W . Attitudes, acceptance and hesitancy among the general population worldwide to receive the COVID-19 vaccines and their contributing factors: A systematic review. EClinicalMedicine. 2021 Oct;40:101113. https://doi.org/10.1016/j.eclinm.2021.101113
15. Robinson E , Jones A , Lesser I , Daly M . International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021 Apr;39(15):2024–34. https://doi.org/10.1016/j.vaccine.2021.02.005
16. Schweizer Radio und Fernsehen SRF . “Luzernerin erhält erste Impfung – auch weitere Kantone gestartet,” Schweizer Radio und Fernsehen SRF, Dec. 2020. https://www.srf.ch/news/schweiz/impfstart-in-der-schweiz-luzernerin-erhaelt-erste-impfung-auch-weitere-kantone-gestartet (accessed 04 Oct. 2021).
17. Federal Office of Public Health . “Covid-19-Impfstrategie: Besonders gefährdete Personen sollen zuerst geimpft werden,” Bundesamt für Gesundheit BAG, Dec. 17, 2020. https://www.bag.admin.ch/bag/de/home/das-bag/aktuell/medienmitteilungen.msg-id-81667.html (accessed 21 Jul. 2021).
18. Federal Office of Public Health . “Coronavirus: Measures and ordinances,” Oct. 06, 2021. https://www.bag.admin.ch/bag/en/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/massnahmen-des-bundes.html#850493620 (accessed 02 Dec. 2021).
19. Federal Office of Public Health . “Coronavirus: Federal Council plans new vaccination drive,” Bundesamt für Gesundheit BAG, Oct. 01, 2021. https://www.admin.ch/gov/en/start/documentation/media-releases.msg-id-85336.html (accessed 02 Dec. 2021).
20. Federal Office of Public Health . “COVID-19 Switzerland Information on the current situation - Vaccinations,” Jan. 07, 2022. https://www.covid19.admin.ch/en/vaccination/persons (accessed 07 Jan. 2022).
21. Zürcher K , et al. “Vaccination willingness for COVID-19 among health care workers in Switzerland,” Jul. 2021. doi: https://doi.org/10.1101/2021.07.04.21255203
22. Fadda M , Suggs LS , Albanese E . Willingness to vaccinate against Covid-19: A qualitative study involving older adults from Southern Switzerland. Vaccine X. 2021 Aug;8:100108. https://doi.org/10.1016/j.jvacx.2021.100108
23. Leos-Toro C , Ribeaud D , Bechtiger L , Steinhoff A , Nivette A , Murray AL , et al. Attitudes Toward COVID-19 Vaccination Among Young Adults in Zurich, Switzerland, September 2020. Int J Public Health. 2021 May;66:643486. https://doi.org/10.3389/ijph.2021.643486
24. Moser A , Carlander M , Wieser S , Hämmig O , Puhan MA , Höglinger M . The COVID-19 Social Monitor longitudinal online panel: real-time monitoring of social and public health consequences of the COVID-19 emergency in Switzerland. PLoS One. 2020 Nov;15(11):e0242129. https://doi.org/10.1371/journal.pone.0242129
25. Moser A , von Wyl V , Höglinger M . Health and social behaviour through pandemic phases in Switzerland: regional time-trends of the COVID-19 Social Monitor panel study. PLoS One. 2021 Aug;16(8):e0256253. https://doi.org/10.1371/journal.pone.0256253
26 A. Speierer et al. , “Original article: The Corona Immunitas digital follow-Up eCohort to monitor impacts of the SARS-CoV-2 pandemic in Switzerland: Study protocol and first results,” Int. J. Public Health, vol. online first, 2022, doi: https://doi.org/10.3389/ijph.2022.1604506.
27. Finbråten HS , Wilde-Larsson B , Nordström G , Pettersen KS , Trollvik A , Guttersrud Ø . Establishing the HLS-Q12 short version of the European Health Literacy Survey Questionnaire: latent trait analyses applying Rasch modelling and confirmatory factor analysis. BMC Health Serv Res. 2018 Jun;18(1):506. https://doi.org/10.1186/s12913-018-3275-7
28 S. M. De Gani , R. Jaks , U. Bieri , and J. Ph. Kocher , “Health Literacy Survey Schweiz 2019-2021,” Careum Stiftung, Zürich, Sep. 2021.
29 V. Von Wyl and Corona Immunitas Research Group , “Report on status of vaccination in Switzerland,” Swiss School of Public Health (SPPH+), Zürich, Dec. 2021.
30. Riesen M , Konstantinoudis G , Lang P , Low N , Hatz C , Maeusezahl M , et al. Exploring variation in human papillomavirus vaccination uptake in Switzerland: a multilevel spatial analysis of a national vaccination coverage survey. BMJ Open. 2018 May;8(5):e021006. https://doi.org/10.1136/bmjopen-2017-021006
31. Richard JL , Mäusezahl M , Basler S , Eckert N . Approaching measles elimination in Switzerland: changing epidemiology 2007-2018. Swiss Med Wkly. 2019 Jun;149(Jun):w20102. https://doi.org/10.4414/smw.2019.20102
32. Zürcher K , Zwahlen M , Berlin C , Egger M , Fenner L . Losing ground at the wrong time: trends in self-reported influenza vaccination uptake in Switzerland, Swiss Health Survey 2007-2017. BMJ Open. 2021 Feb;11(2):e041354. https://doi.org/10.1136/bmjopen-2020-041354
33. Federal Office of Public Health . “Die HPV-Impfung in der Schweiz: Resultate einer nationalen Befragung im Jahr 2014,” Federal Office of Public Health, Bulletin 23, 2015. Accessed: 11 Oct. 2021. Online. Available: https://www.bag.admin.ch/bag/de/home/krankheiten/krankheiten-im-ueberblick/hpv.html
34. Lang P , Sinniger P , Spaar A , Born R , Hatz C . “Evolution of the HPV vaccination coverage in Switzerland, 2008-2016,” presented at the Poster 4441, presented at the Swiss Public Health Conference 2017, Basel 22–23 November 2017, 2017. Online. Available: https://organizers-congress.org/frontend/index.php?page_id=4145&additions_conferenceschedule_action=detail&additions_conferenceschedule_controller=paperList&pid=4441&hash=f49071bb2676ff88f7aec864a67f329c1fde52556e03f405c0b67e1d268c0707
35. Tarr PE , Deml MJ , Huber BM . Measles in Switzerland - progress made, but communication challenges lie ahead. Swiss Med Wkly. 2019 Jun;149(Jun):w20105. https://doi.org/10.4414/smw.2019.20105
36. European Centre for Disease Prevention and Control . “Data on COVID-19 vaccination in the EU/EEA,” Jan. 07, 2022. https://tinyurl.com/3nmn8bkt (accessed 07 Jan. 2022).
37. Montagni I , Ouazzani-Touhami K , Mebarki A , Texier N , Schück S , Tzourio C ; CONFINS group . Acceptance of a Covid-19 vaccine is associated with ability to detect fake news and health literacy. J Public Health (Oxf). 2021 Dec;43(4):695–702. https://doi.org/10.1093/pubmed/fdab028
38. Carrieri V , Madio L , Principe F . Vaccine hesitancy and (fake) news: quasi-experimental evidence from Italy. Health Econ. 2019 Nov;28(11):1377–82. https://doi.org/10.1002/hec.3937
39. Lorini C , Santomauro F , Donzellini M , Capecchi L , Bechini A , Boccalini S , et al. Health literacy and vaccination: A systematic review. Hum Vaccin Immunother. 2018 Feb;14(2):478–88. https://doi.org/10.1080/21645515.2017.1392423
40. Munzert S , Selb P , Gohdes A , Stoetzer LF , Lowe W . Tracking and promoting the usage of a COVID-19 contact tracing app. Nat Hum Behav. 2021 Feb;5(2):247–55. https://doi.org/10.1038/s41562-020-01044-x
41. Klüver H , Hartmann F , Humphreys M , Geissler F , Giesecke J . Incentives can spur COVID-19 vaccination uptake. Proc Natl Acad Sci USA. 2021 Sep;118(36):e2109543118. https://doi.org/10.1073/pnas.2109543118
42. Mills MC , Rüttenauer T . The effect of mandatory COVID-19 certificates on vaccine uptake: synthetic-control modelling of six countries. Lancet Public Health. 2021 Dec;0(0): https://doi.org/10.1016/S2468-2667(21)00273-5
43. Masserey Spicher V , Weiss MG . Policy and socio-cultural differences between cantons in Switzerland with high and low adolescent vaccination coverage for hepatitis B and HPV. Vaccine. 2019 Dec;37(52):7539–46. https://doi.org/10.1016/j.vaccine.2019.09.085
44. Wood S , Schulman K . Beyond Politics - Promoting Covid-19 Vaccination in the United States. N Engl J Med. 2021 Feb;384(7):e23. https://doi.org/10.1056/NEJMms2033790
45. Höglinger M , Jann B , Diekmann A . Sensitive Questions in Online Surveys: An Experimental Evaluation of Different Implementations of the Randomized Response Technique and the Crosswise Model. Surv Res Methods. 2016 Dec;10(3):171–87. https://doi.org/10.18148/srm/2016.v10i3.6703
Table S1Males – COVID-19 vaccine uptake and Cox proportional hazard ratios from univariable and multivariable analyses (n = 1263).
| Uptake a (%) | Unadj HR b | (95% CI) | Adj HR Model 1 c | (95% CI) | Adj HR Model 2 c | (95% CI) | Adj HR Model 3 c | (95% CI | |
| Education | |||||||||
| Compulsory | 81 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Secondary | 89 | 1.49 | (1.05–2.11) | 1.44 | (1.00–2.07) | 1.44 | (0.99–2.09) | 1.32 | (0.91–1.92) |
| Tertiary | 94 | 2.16 | (1.51–3.10) | 1.98 | (1.37–2.87) | 1.97 | (1.34–2.90) | 1.66 | (1.13–2.44) |
| Household income | |||||||||
| CHF <5000 | 87 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| CHF 5000–9999 | 90 | 1.23 | (1.04–1.45) | 1.18 | (1.00–1.40) | 1.16 | (0.97–1.38) | 1.13 | (0.94–1.35) |
| CHF ≥10,000 | 94 | 1.75 | (1.45–2.11) | 1.56 | (1.28–1.90) | 1.53 | (1.25–1.87) | 1.54 | (1.25–1.90) |
| No answer | 91 | 1.49 | (1.11–1.98) | 1.52 | (1.15–2.02) | 1.47 | (1.12–1.95) | 1.53 | (1.17–2.01) |
| Migration background | |||||||||
| Swiss-born | 90 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Foreign-born | 92 | 1.11 | (0.93–1.32) | 1.09 | (0.91–1.31) | 1.05 | (0.88–1.26) | 1.00 | (0.83–1.20) |
| Place of residence | |||||||||
| Urban | 90 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Rural | 90 | 0.88 | (0.76–1.02) | 0.87 | (0.75–1.01) | 0.84 | (0.72–0.98) | 0.83 | (0.71–0.96) |
| Language region | |||||||||
| German | 91 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| French | 89 | 1.03 | (0.88–1.21) | 0.98 | (0.83–1.15) | 1.01 | (0.86–1.19) | 0.96 | (0.81–1.13) |
| Italian | 90 | 0.88 | (0.74–1.03) | 0.80 | (0.66–0.96) | 0.80 | (0.67–0.96) | 0.79 | (0.67–0.94) |
| Chronic condition | |||||||||
| No | 88 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 94 | 1.32 | (1.15–1.52) | 1.41 | (1.22–1.62) | 1.36 | (1.19–1.57) | 1.35 | (1.18–1.55) |
| Health literacy | |||||||||
| Problematic/inadequate | 86 | 1.00 | 1.00 | 1.00 | |||||
| Sufficient | 96 | 1.32 | (1.10–1.59) | 1.25 | (1.04–1.51) | 1.17 | (0.97–1.42) | ||
| Excellent | 93 | 1.38 | (1.21–1.58) | 1.31 | (1.14–1.50) | 1.19 | (1.05–1.36) | ||
| Adherence to prevention measures (refrained from visits) | |||||||||
| Rarely | 77 | 1.00 | 1.00 | 1.00 | |||||
| Sometimes | 90 | 1.62 | (1.29–2.04) | 1.63 | (1.29–2.06) | 1.48 | (1.17–1.85) | ||
| Mostly | 94 | 1.72 | (1.43–2.05) | 1.71 | (1.42–2.05) | 1.48 | (1.23–1.79) | ||
| Trust in government | |||||||||
| Low | 70 | 1.00 | 1.00 | ||||||
| Middle | 84 | 1.68 | (1.31–2.16) | 1.38 | (1.05–1.83) | ||||
| High | 96 | 2.48 | (2.01–3.06) | 1.60 | (1.22–2.09) | ||||
| Trust in science | |||||||||
| Low | 71 | 1.00 | 1.00 | ||||||
| Middle | 86 | 1.61 | (1.25–2.08) | 1.30 | (0.96–1.76) | ||||
| High | 95 | 2.44 | (1.93–3.09) | 1.58 | (1.16–2.16) | ||||
CI: confidence interval; HR: hazard ratio.
a Uptake based on weighted Kaplan-Meier estimates as of last common censoring date across all subgroups (8 December)
b Stratified by age
c Stratified by age and adjusted for all the other variables included in the model as shown.
Table S2Females – COVID-19 vaccine uptake and Cox proportional hazard ratios from univariable and multivariable analyses (N=1,185).
| Uptakea (%) | Unadj HRb | (95% CI) | Adj HR Model 1c | (95% CI) | Adj HR Model 2c | (95% CI) | Adj HR Model 3c | (95% CI) | |
| Education | |||||||||
| Compulsory | 83 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Secondary | 84 | 1.31 | (0.96–1.79) | 1.12 | (0.83–1.52) | 1.13 | (0.83–1.53) | 1.01 | (0.74–1.39) |
| Tertiary | 91 | 1.70 | (1.22–2.38) | 1.35 | (0.97–1.88) | 1.34 | (0.96–1.86) | 1.10 | (0.78–1.54) |
| Household income | |||||||||
| CHF <5000 | 77 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| CHF 5000–9999 | 88 | 1.56 | (1.30–1.87) | 1.57 | (1.31–1.89) | 1.55 | (1.30–1.86) | 1.43 | (1.19–1.72) |
| CHF ≥10,000 | 94 | 2.19 | (1.76–2.72) | 2.06 | (1.63–2.61) | 2.00 | (1.58–2.52) | 1.79 | (1.41–2.28) |
| No answer | 83 | 1.39 | (1.10–1.75) | 1.38 | (1.10–1.74) | 1.38 | (1.10–1.74) | 1.30 | (1.03–1.65) |
| Migration background | |||||||||
| Swiss-born | 86 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Foreign-born | 84 | 0.97 | (0.77–1.21) | 0.90 | (0.71–1.13) | 0.88 | (0.70–1.12) | 0.92 | (0.74–1.16) |
| Place of residence | |||||||||
| Urban | 88 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Rural | 78 | 0.73 | (0.61–0.86) | 0.75 | (0.63–0.89) | 0.74 | (0.62–0.88) | 0.74 | (0.62–0.88) |
| Language region | |||||||||
| German | 85 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| French | 88 | 1.06 | (0.90–1.24) | 1.01 | (0.86–1.18) | 1.03 | (0.88–1.20) | 1.01 | (0.86–1.18) |
| Italian | 89 | 1.00 | (0.86–1.18) | 1.00 | (0.85–1.18) | 0.98 | (0.83–1.15) | 1.00 | (0.85–1.18) |
| Chronic condition | |||||||||
| No | 82 | 1.00 | 1.00 | 1.00 | 1.00 | ||||
| Yes | 93 | 1.42 | (1.22–1.65) | 1.41 | (1.22–1.64) | 1.41 | (1.22–1.63) | 1.43 | (1.23–1.65) |
| Health literacy | |||||||||
| Problematic/Inadequate | 84 | 1.00 | 1.00 | 1.00 | |||||
| Sufficient | 87 | 1.01 | (0.83–1.23) | 0.94 | (0.77–1.16) | 0.91 | (0.74–1.11) | ||
| Excellent | 87 | 1.10 | (0.95–1.27) | 1.08 | (0.94–1.25) | 1.02 | (0.88–1.18) | ||
| Adherence to prevention measures (refrained from visits) | |||||||||
| Rarely | 73 | 1.00 | 1.00 | 1.00 | |||||
| Sometimes | 86 | 1.53 | (1.20–1.94) | 1.47 | (1.16–1.87) | 1.23 | (0.97–1.57) | ||
| Mostly | 89 | 1.62 | (1.33–1.99) | 1.58 | (1.30–1.93) | 1.31 | (1.07–1.60) | ||
| Trust in government | |||||||||
| Low | 53 | 1.00 | 1.00 | ||||||
| Middle | 78 | 2.05 | (1.50–2.82) | 1.60 | (1.13–2.28) | ||||
| High | 92 | 3.27 | (2.45–4.37) | 2.04 | (1.46–2.86) | ||||
| Trust in science | |||||||||
| Low | 57 | 1.00 | 1.00 | ||||||
| Middle | 78 | 1.86 | (1.38–2.53) | 1.37 | (0.98–1.92) | ||||
| High | 93 | 2.99 | (2.26–3.96) | 1.73 | (1.25–2.40) | ||||
CI: confidence interval; HR: hazard ratio.
a Uptake based on weighted Kaplan-Meier estimates as of last common censoring date across all subgroups (8 December)
b Stratified by age
c Stratified by age and adjusted for all the other variables included in the model as shown.
Available in the pdf version of the article.
Available for download at DOI: 10.4414/smw.2022.w30134.