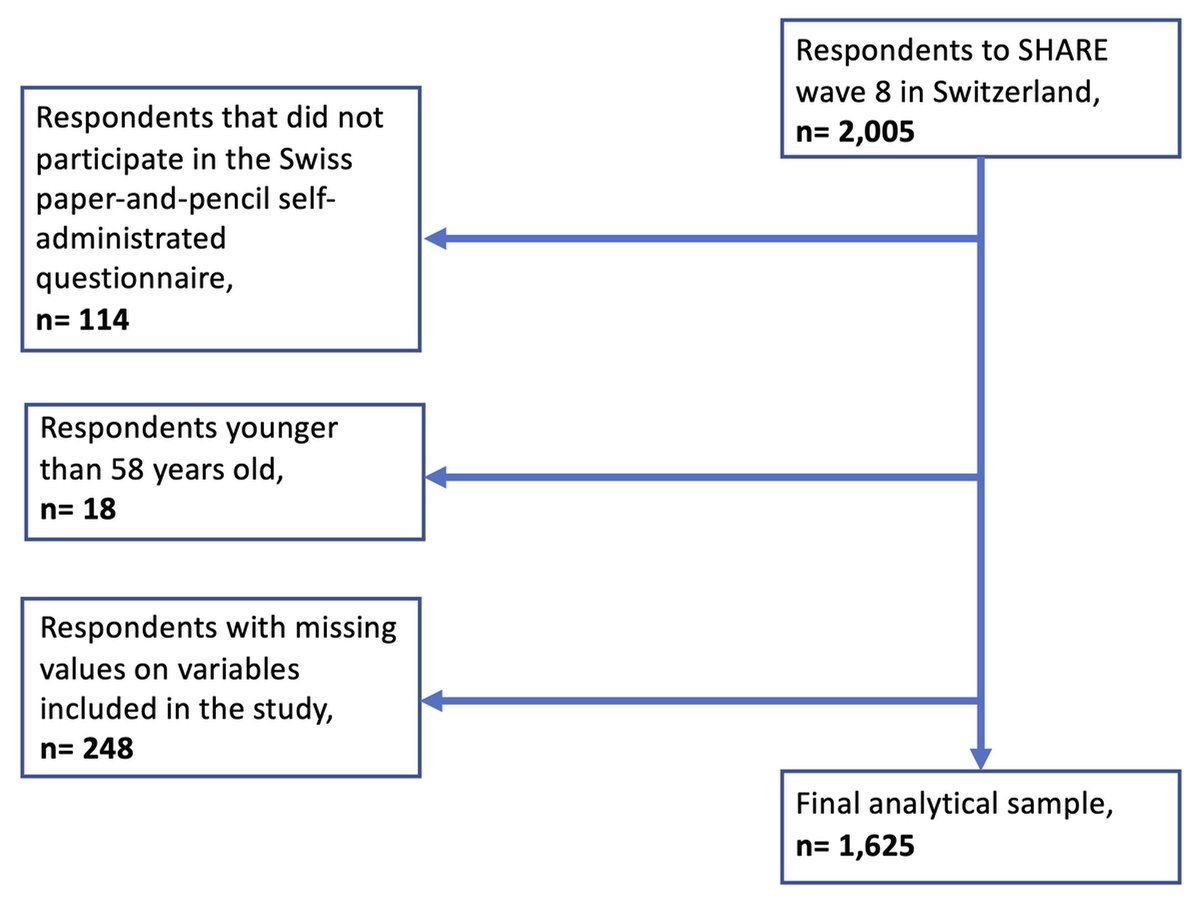
Figure 1 Flow chart.
DOI: https://doi.org/10.4414/SMW.2022.w30158
Individuals differ in their ability to deal with health-related issues, which influences their health-related behaviour and decisions. A common measure of skills regarding health-related issues is health literacy. Health literacy refers to “the degree to which individuals have the ability to find, understand, and use information and services to inform health-related decisions and actions for themselves and others” [1]. Health literacy skills enable individuals to engage in behaviour beneficial to their health, such as adopting a healthier lifestyle, seeking more appropriate healthcare services, and empowering them in the event of illness [2].
During the past few years, policymakers, researchers, and practitioners have moved the growing attention from functional health literacy measures to broader subjective instruments [3]. The focus was on comprehensively measuring health literacy in the general population to capture individuals' competencies to seek, understand, appraise and use health-related information for making judgments and decisions in everyday life [4]. This approach allows measuring the autonomy and empowerment of citizens regarding the health care system [2]. Recent studies implementing this concept found that low health literacy levels are associated with poor health status, lower use of preventive healthcare interventions, and key barriers to medical conversations [5]. Low health literacy is associated with advanced age, a migration background, and low self-assessed social status [6]. Moreover, varying health literacy is a strong predictor of health disparities between individuals, related to factors such as age, language, education, and socioeconomic status [7, 8]. Therefore, improving health literacy in disadvantaged groups may contribute to reducing social inequalities in health and raising patient empowerment.
At the population level, measuring health literacy is an instrument of public health that allows identifying vulnerable sub-groups to follow the main goals of the health system regarding accessibility, responsiveness, and solidarity [9].
Switzerland aims to pursue these goals to give all citizens equal opportunities for good health. Yet, implementing health equity remains a challenge as several socially disadvantaged groups face challenges due to language, origin, social status, or education level [10]. The Swiss Federal Office of Public Health (FOPH) aims to promote health equity by creating effective policies and interventions targeted at these socially disadvantaged population groups. The FOPH recently conducted a national health literacy survey on citizens over the age of 15; the results of the study from 2020 revealed that health literacy in Switzerland is generally poor, with approximately 38% of the population having problematic health literacy. However, the problem is not that deep as only 11% of respondents displayed inadequate health literacy [11]. This study also indicated that low health literacy was associated with poor financial means, lower education level and lower health status. The FOPH study focused on the entire population; however, health literacy skills are particularly relevant in aging populations with large chronic and severe diseases burdens. Health literacy influences how older individuals perceive their health problems, communicate with health professionals and make medical decisions [12]. These results highlight the need to increase the knowledge of social patterns of health literacy in older populations to better understand the corresponding inequalities in health literacy and its potential consequences. Yet, there has not been a comprehensive and representative health literacy survey on Switzerland's older adults' population. The study we present begins to close this gap, and aims to (a) measure the level of health literacy in older adults living in Switzerland and (b) identify its association with the individuals’ social, regional, and health characteristics.
We use data from the Survey of Health, Ageing and Retirement in Europe (SHARE), a biennial population-based longitudinal study of Europeans aged 50 years and older that started in 2004 [13]. SHARE collects information on health, socioeconomic status, and social networks of targeted respondents and their partners in 27 European countries and Israel, using Computer-Assisted Personal Interviewing (CAPI). In Switzerland, a random sample of older individuals were invited to participate in the longitudinal SHARE sample and have been invited to participate in the survey every two years. During each survey round, respondents give their consent to participate in the SHARE study twice: when they accept the invitation to schedule a personal interview and when they take part in the face-to-face interview. In addition to an internationally harmonised in-person interview, respondents answer a country-specific paper-and-pencil self-administered questionnaire. Our database thus combined the Swiss questionnaire containing a short health literacy assessment with the variables from the main interview. These data were collected for the 8th wave of SHARE, between October 2019 and the beginning of March 2020. SHARE wave 8 included 2,005 participants in Switzerland, either as targeted respondents or their partners. Among them, 1,891 individuals also completed the self-administrated questionnaire, resulting in a cooperation rate of 94.3%. The Swiss SHARE sample was designed to be nationally representative of individuals aged 50 years and older and their partners. It is periodically refreshed to maintain its representativeness of the target population. Since the last refreshment sample for SHARE Switzerland took place in 2011, the Swiss SHARE sample of wave 8 (2019/2020) is no longer representative of the population of adults aged 50 to 58. Therefore, our study only includes respondents aged 58 and older to be representative of Swiss citizens. Finally, after eliminating 18 respondents younger than 58 years old and 248 respondents with missing responses on some variables included in this study, our analytical sample comprises 1,625 participants (Figure 1).
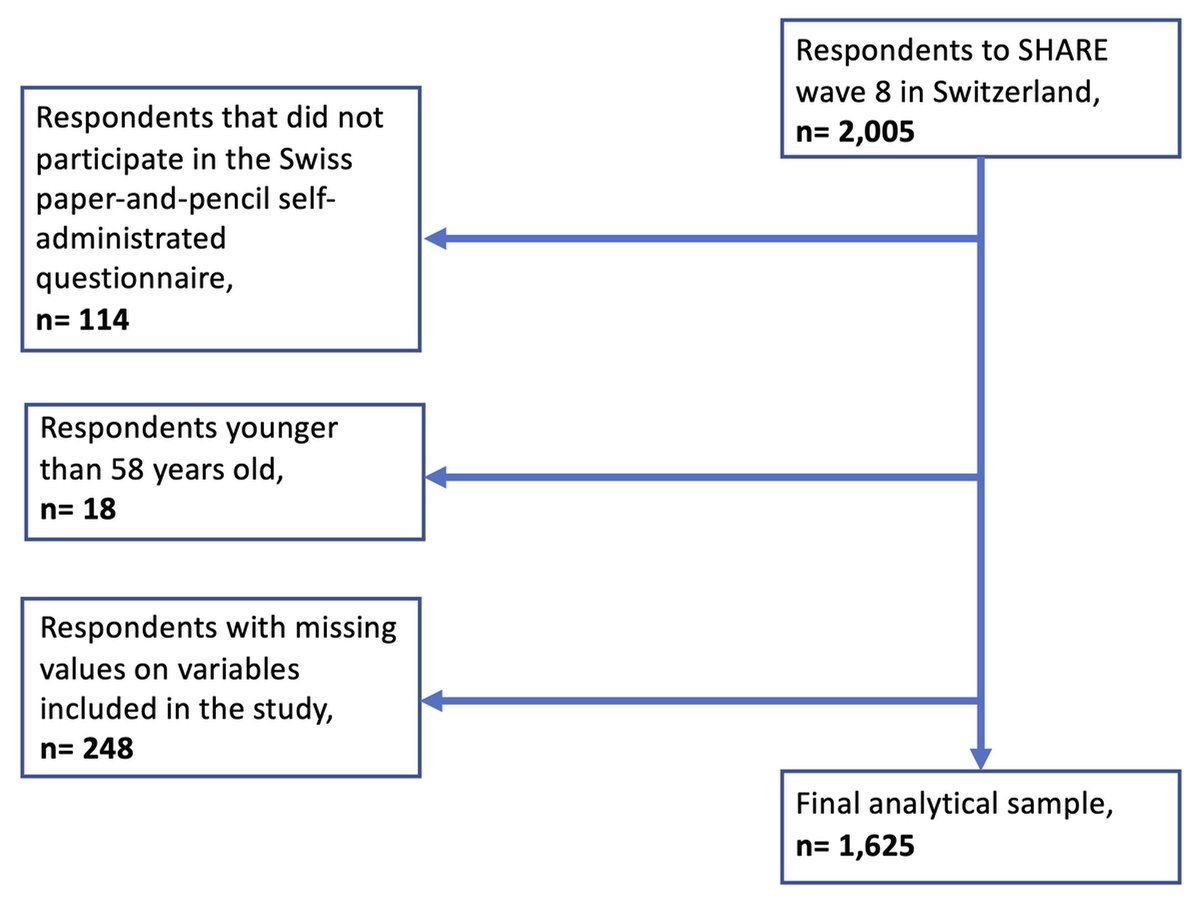
Figure 1 Flow chart.
HLS-EU-Q16. The Swiss drop-off questionnaire included the 16 items of the short version of the European Health Literacy Survey questionnaire developed by the HLS-EU consortium [5]. The scale consists of 16 items (see Appendix) measuring health literacy within three domains: health care, disease prevention, health promotion, and four stages of information processing, which includes accessing health information, understanding health information, processing health information, applying health information. Each item consists of concrete health-relevant tasks or situations that respondents rate on a 4-point Likert scale with answers ranging from "very easy," "fairly easy," "fairly difficult," to "very difficult." Following an approach suggested by Pelikan, Ganahl, Van den Broucke and Sorensen on how to measure health literacy in the general populations [3], each answer is dichotomised with a value of "0" for "fairly difficult" and "very difficult" and a value of "1" for the categories "very easy" and "fairly easy" [3]. Missing values were treated as 0, and the final health literacy score only includes respondents with no more than two missing values on the items. In total, 123 respondents (7.6%) had one or two missing values on the 16 items. The final health literacy score ranges from 0 to 16 and can be divided into three categories: inadequate (0–8), problematic (9–12), and sufficient (13–16) or in a binary variable combining the two upper categories [i.e., 0: not inadequate (9–16), 1: inadequate (0–8)]. In addition to the health literacy scores, seven sub-indices were constructed based on the different items pertaining to the three health domains and four literacy information processing stages. To make our analysis more comparable to previous studies, the health literacy score and the seven sub-indices were standardised on a scale from a minimum of 0 to a maximum of 50 following the formula: Index = (mean – 1) x 50/3 [7]. The standardisation consists of putting the indices constructed with a different number of items on the same scale; this process allows comparing the scores between all the indices.
To assess social differences in health literacy, our statistical models include information on gender (0 = male, 1 = female), age group (58–64 years, 65–74 years, 75+ years), and education level, which was grouped into three categories based on the International Standard Classification of Education (ISCED) of 2017 [14] (low = ISCED levels 0-1–2, secondary = ISCED levels 3–4, tertiary = ISCED levels 5–6). Our measure of partnership status considered all types of partnership rather than just focusing on legal marriage (0 = has a partner, 1 = has no partner). Respondents' perceived financial situation was measured based on the question: "Is your household able to make ends meet?" with permissible answers being recoded into three groups (1 = easily, 2 = fairly easily, 3 = with difficulty), merging the two highest categories "with some difficulty" and "with great difficulty" into the category "with difficulty." We also used information on the major linguistic regions of Switzerland based on the language of the questionnaire (German, French, or Italian) and on the living environment, namely whether respondents lived in an urban or rural area (0 = urban, 1 = rural). Finally, we assessed respondents' self-rated health status; for brevity, the original five-point Likert scale to measure self-rated health (5 = excellent, 4 = very good, 3 = good, 2 = fair, 1 = poor) was recoded by combining the two outer categories to obtain a three-point scale (1 = poor/fair health, 2 = good health, 3 = very good/excellent health).
We used unweighted number counts and weighted proportion estimation to assess the relative frequencies of all variables used in our final analytical sample of adults aged 58 and older residing in Switzerland. Specifically, to obtain descriptive statistics representative of the population of interest, we calibrated the sample using cross-sectional weights provided in the SHARE data. Survey weights can help to address challenges related to nonresponse and sample attrition. SHARE calibration of the weight relies on the approach Deville and Särndal (1992), which aligns the sample and population distributions [15]. The internal consistency and reliability for the HLS-EU-Q16 measure were assessed using Cronbach's alpha. Moreover, the distribution of the health literacy score per category of each covariate also used weighted proportion. In addition, we conducted a bivariate analysis with Pearson's chi-squared test (X2) between the health literacy score and each covariate. Partial associations between health literacy outcomes and respondents' characteristics were estimated using unweighted ordinary least squares regression (HL score), probit regression (HL binary), and multivariable ordered probit model (HL grouped), whose results are reported in terms of average marginal effects. Testing these associations on three statistical models permits a robustness check of the estimates. Finally, adjusted associations of the overall standardised health literacy score and its seven sub-indices with respondent's sociodemographic characteristics were assessed using unweighted multivariable ordinary least squares regression. The estimated standard errors were adjusted to account for the possibility of dependencies in the observations as both partners of the same couple may participate in our study, which increases the chances of similar responses. The regressions were hence clustered at the household level using the command option “cluster” of STATA to account for such potential dependencies. All estimations were performed using STATA/SE 17.0 software (STATA Corporation, College Station, TX).
Our study obtained ethical approval number 66/14 from the ethics committee of the canton of Vaud, Switzerland, in March 2014.
Regarding the measurement instrument of health literacy, the HLS-EU-Q16, Cronbach's alpha indicated a high internal consistency and reliability as the coefficients were above 0.9. Table 1 presents the key characteristics of our weighted analytical sample. The proportion of women in our sample was 50%, the mean age was 73.4 years old (SD: 8.5), and the majority of respondents ranged between the age of 58 and 64 years (45%). Almost three-quarters of respondents had a partner (72%), and 63% had a secondary educational degree. Most of the respondents reported that it was "easy" (57%) or "fairly easy" (30%) to make ends meet at the end of the month. Regarding regional characteristics, (70%) of the respondents lived in the German-speaking part of Switzerland, and 59% lived in a rural area. Most respondents reported being healthy, with only 16% indicating having "poor" or "fair" health.
Table 1Characteristics of the study population, adults aged 58+, SHARE Switzerland, 2019/2020, n = 1,625.
| Unweighted | Weighted | |||
| n | % | CI | ||
| Gender | Male | 762 | 50.4 | [46.2–54.6] |
| Female | 863 | 49.6 | [45.4–53.8] | |
| Age groups | 58–64 years | 263 | 45.3 | [40.0–50.7] |
| 65–74 years | 678 | 27.5 | [24.5–30.8] | |
| 75+ years | 684 | 27.2 | [24.2–30.4] | |
| Education | Low | 289 | 16.0 | [13.1–19.4] |
| Secondary | 1,015 | 63.1 | [58.5–67.4] | |
| Tertiary | 321 | 20.9 | [17.2–25.2] | |
| Partnership status | Has a partner | 1,218 | 72.1 | [67.7–76.1] |
| No partner | 407 | 27.9 | [23.9–32.3] | |
| Make ends meet | Easily | 896 | 56.9 | [52.2–61.5] |
| Fairly easily | 517 | 30.5 | [26.5–34.9] | |
| With difficulty | 212 | 12.6 | [9.9–15.9] | |
| Language | German | 1,152 | 70.5 | [65.7–74.9] |
| French | 414 | 26.6 | [22.3–31.4] | |
| Italian | 59 | 2.9 | [1.9–4.2] | |
| Living area | Urban | 743 | 41.3 | [36.7–46.0] |
| Rural | 882 | 58.7 | [54.0–63.3] | |
| Self–rated health | Poor/fair health | 308 | 16.5 | [13.5–19.9] |
| Good health | 685 | 37.6 | [33.3–42.2] | |
| Very good/excellent health | 632 | 45.9 | [40.9–50.9] | |
Note: unweighted and weighted number of observations for the whole sample. n = number; CI = confidence interval.
Figure 2 displays the weighted proportion of answers for each health literacy item grouped by their respective health domain. Overall, less than 35% of respondents systematically reported finding it "very difficult" or "fairly difficult" to deal with one of the seven items from the health care domain. Only 2.3% reported having difficulties understanding doctors’ or pharmacists’ instructions on how to take a prescribed medication, 3.4% reported difficulties in following instructions from doctors or pharmacists, 6.6% in understanding what doctors say, 8.4% in finding out where to get professional help in case of illness, 9.6% in finding information on treatments of illnesses that concern the person, 13.9% in using information the doctor gives to make decisions, and 34.3% in judging when there is a need to get a second opinion from another doctor.
Less than 46% of responded reported difficulties with any of the five related HLS-EU-Q16 items concerning disease prevention. The proportion of respondents stating that it was "very difficult" or "fairly difficult" to understand health warnings about behaviour such as smoking, low physical activity, and drinking too much was 2.7%, while 6.2% reported difficulties in understanding the need for health screening, 24.5% in finding information on how to manage mental health problems like stress or depression, 37.9% in deciding how to protect oneself from illness based on information in the media, and 45.6% to judge if the information on health risks in the media is reliable.
Finally, less than 25% found it "very difficult" or "fairly difficult" to deal with different types of issues/aspects related to health promotion. A minority of 10.4% of respondents had difficulties judging which everyday behaviours are related to the person's health, 12.1% understanding health advice from family or friends, 12.4% learning about activities that benefit mental well-being, and 24.4% understanding information in the media on healthy living.

Figure 2 Short version of the European Health Literacy Survey questionnaire (HLS-EU-Q16), percentage of respondents per categories, adults aged 58+, SHARE Switzerland, 2019/2020, n = 1,625.
Table 2 shows the overall distribution of the three-category health literacy score and its bivariate distribution by key respondent characteristics. Overall, 6.8% of the respondents had inadequate health literacy, 24.6% problematic health literacy, and 68.6% sufficient health literacy. The bivariate analysis between health literacy and respondents’ characteristics showed statistically significant correlations for gender (p <0.008), age (p <0.004), education (p <0.001), financial situation (p <0.001), and self-rated health (p <0.001). Women had higher levels of health literacy than men. Being older was correlated with lower health literacy levels, while higher education, better financial situation, and higher self-rated health were positively correlated with health literacy. Respondents' partnerships status, language, and the living area were not shown to be correlated with health literacy.
Table 2Distribution of the three-category health literacy on the covariates, adults aged 58+, SHARE Switzerland, 2019/2020,n = 1,625
| Health literacy scores (grouped) | p-value | ||||
| Inadequate | Problematic | Sufficient | |||
| % [95% CI] | % [95% CI] | % [95% CI] | |||
| Total | 6.8 [5.0–9.1] | 24.6 [20.6–29.1] | 68.6 [64.0–72.9] | ||
| Gender | Male | 7.8 [5.1–11.9] | 24.3 [18.3–31.6] | 67.8 [60.4–74.4] | |
| Female | 5.7 [3.9–8.3] | 24.9 [20.4–30.1] | 69.4 [64.2–74.2] | <0.008 | |
| Age groups | 55–64 years | 5.4 [2.5–11.2] | 25.0 [17.1–35.1] | 69.6 [59.5–78.1] | |
| 65–74 years | 5.8 [4.2–8.0] | 22.7 [19.5–26.2] | 71.5 [67.8–75.0] | ||
| 75+ years | 10.1 [8.0–12.8] | 25.9 [22.7–29.5] | 64.0 [60.1–67.7] | <0.004 | |
| Education | Low | 14.3 [9.1–21.7] | 26.4 [18.8–35.8] | 59.3 [49.1–68.8] | |
| Secondary | 6.6 [4.4–9.9] | 27.4 [22.2–33.4] | 65.9 [60.0–71.4] | ||
| Tertiary | 1.5 [0.7–3.1] | 14.7 [9.9–21.3] | 83.8 [77.0–88.8] | <0.001 | |
| Partnership status | Has a partner | 5.9 [4.4–8.0] | 24.5 [19.6–30.0] | 69.6 [64.1–7.47] | |
| No partner | 9.0 [4.8–16.3] | 25.0 [18.5–33.0] | 66.0 [57.4–73.6] | <0.595 | |
| Make ends meet | Easily | 5.3 [3.1–9.0] | 20.0 [15.5–25.5] | 74.6 [68.8–79.7] | |
| Fairly easily | 6.8 [4.2–10.7] | 29.5 [22.5–37.6] | 63.7 [55.7–71.0] | ||
| With difficulty | 13.2 [8.4–20.2] | 33.6 [22.1–47.4] | 53.3 [40.6–65.5] | <0.001 | |
| Language | German | 6.3 [4.2–9.2] | 21.3 [17.3–26.1] | 72.4 [67.3–76.9] | |
| French | 7.1 [4.2–11.7] | 32.6 [23.3–43.5] | 60.3 [50.1–69.7] | ||
| Italian | 16.1 [5.2–40.3] | 30.7 [16.0–50.7] | 53.2 [36.0–69.7] | <0.272 | |
| Living area | No | 6.7 [4.8–9.1] | 23.6 [18.6–29.4] | 69.8 [63.8–75.1] | |
| Yes | 6.9 [4.3–10.7] | 25.4 [19.7–32.2] | 67.8 [61.0–73.9] | <0.273 | |
| Self–rated health | Poor/fair health | 15.2 [9.9–22.8] | 35.6 [25.6–47.0] | 49.2 [39.3–59.2] | |
| Good health | 6.9 [5.2–9.1] | 25.1 [19.8–31.3] | 68.0 [61.7–73.7] | ||
| Very good/excellent health | 3.6 [1.4–9.1] | 20.3 [14.6–27.4] | 76.1 [68.6–82.3] | <0.001 | |
Note: all proportions are weighted, CI = confidence interval. HLS-EU-Q16 Score: 0–8 = inadequate, 9–12 = problematic, 13–16 = sufficient.
Table 3 presents adjusted partial associations between health literacy and respondent characteristics based on multivariable regression, probit, and ordered probit models depending on the outcome under consideration. Overall, women were more likely to have higher health literacy scores (p <0.001) and were less likely to have inadequate and problematic levels of health literacy than men (p <0.001). Respondents with a secondary (p <0.05) or tertiary (p <0.001) level of education were more likely to have higher health literacy scores and less likely to have inadequate and problematic levels of health literacy than respondents with a low level of education. Respondents who stated that they were able to make ends meet easily were more likely to have higher health literacy scores (p <0.01) and less likely to have inadequate and problematic health literacy levels than those reporting difficulties in making ends meet (p <0.05). Finally, respondents with good/very good or excellent self-rated health (p <0.001) were more likely to have a higher health literacy score and less likely to have inadequate and problematic levels of health literacy than those who reported being in poor or fair health. There was no statistically significant partial association between health literacy and respondent's age, partnership status, and language once other characteristics were accounted for in our models.
Table 3 Partial associations of health literacy with respondents’ sociodemographic characteristics; health literacy score (0–16), two-category (0: not inadequate, 1: inadequate) and three-category (1: inadequate, 2: problematic, 3: sufficient), adults aged 58+, SHARE Switzerland, 2019/2020, n = 1,625.
| OLS regression (HL score) | Probit regression [Inadequate AME (SE)] | Oprobit regression [Inadequate – Problematic AME (SE)] | |||
| Gender (male) | Female | 0.67*** | –0.05*** | –0.03*** | –0.06*** |
| (0.14) | (0.01) | (0.01) | (0.01) | ||
| Age group (58–64 years) | 65–74 years | 0.11 | –0.03 | –0.00 | –0.00 |
| (0.19) | (0.02) | (0.01) | (0.02) | ||
| 75+ years | –0.13 | –0.01 | 0.01 | 0.02 | |
| (0.21) | (0.02) | (0.01) | (0.02) | ||
| Education (low) | Secondary | 0.44* | –0.05* | –0.03 | –0.04* |
| (0.22) | (0.02) | (0.01) | (0.02) | ||
| Tertiary | 1.22*** | –0.10*** | –0.07*** | –0.12*** | |
| (0.24) | (0.02) | (0.02) | (0.02) | ||
| Partnership status (has a partner) | No partner | 0.07 | 0.00 | –0.00 | –0.01 |
| (0.18) | (0.02) | (0.01) | (0.02) | ||
| Make ends meet (easily) | Fairly easily | –0.19 | –0.01 | 0.01 | 0.02 |
| (0.17) | (0.01) | (0.01) | (0.02) | ||
| With difficulty | –0.81** | 0.05* | 0.03* | 0.05* | |
| (0.27) | (0.02) | (0.02) | (0.02) | ||
| Language [German (ch)] | French (ch) | 0.04 | –0.00 | 0.01 | 0.01 |
| (0.18) | (0.02) | (0.01) | (0.02) | ||
| Italian (ch) | –0.48 | 0.04 | 0.03 | 0.04 | |
| (0.50) | (0.05) | (0.03) | (0.04) | ||
| Living area (urban) | Rural | –0.12 | 0.01 | 0.01 | 0.02 |
| (0.15) | (0.01) | (0.01) | (0.01) | ||
| Self-rated health (poor/fair health) | Good health | 0.97*** | –0.03 | –0.05*** | –0.06*** |
| (0.23) | (0.02) | (0.02) | (0.02) | ||
| Very good/excellent health | 1.59*** | –0.09*** | –0.08*** | –0.12*** | |
| (0.23) | (0.02) | (0.02) | (0.02) | ||
| Observations | 1625 | 1625 | 1625 | 1625 | |
Note: this table shows an Ordinary Least Squares (OLS) regression of the Health Literacy (HL) score on the covariates, a probit regression of the two-category HL variable on the covariates, and an oprobit regression of the three-category HL score on the covariates. The table shows average marginal effects (AMEs) and standard errors in brackets with significance level ∗p <0.05, ∗∗p <0.01, ∗∗∗p <0.001. Concerning the interpretation of the average marginal effects, the AME for gender in the probit regression in bold above, for instance, means that women have a 5-percentage point smaller probability of inadequate health literacy compared to men.
Table 4 shows multivariable regressions of the overall standardised health literacy score and the seven standardised sub-indices on the covariates. The adjusted partial associations of health literacy with gender, education, financial situation, and self-rated health are generally similar to those documented above. There were also statistically significant results among linguistic regions on a few sub-indices.
Table 4Partial associations of standardised health literacy score and sub-indices with respondents’ sociodemographic characteristics, adults aged 58+, SHARE Switzerland, 2019/2020, n = 1,625
| HL score | Healthcare (hc_hl) | Disease prevention (dp_hl) | Health promotion (hp_hl) | Access (oi) | Understanding (ui) | Process (pi) | Apply (ai) | ||
| Gender (male) | Female | 2.03*** | 1.84*** | 1.95*** | 2.46*** | 2.36*** | 1.84*** | 2.31*** | 1.69*** |
| (0.35) | (0.37) | (0.41) | (0.45) | (0.42) | (0.36) | (0.48) | (0.43) | ||
| Age group (58–64 years) | 65–74 years | 0.01 | 0.26 | –0.01 | –0.39 | 0.05 | 0.15 | –0.04 | –0.26 |
| (0.53) | (0.54) | (0.64) | (0.65) | (0.61) | (0.53) | (0.71) | (0.64) | ||
| 75+ years | –0.40 | 0.71 | –0.91 | –1.71* | –0.87 | –0.38 | –0.34 | 0.12 | |
| (0.55) | (0.56) | (0.69) | (0.69) | (0.65) | (0.56) | (0.74) | (0.66) | ||
| Education (low) | Secondary | 1.37* | 1.25* | 1.45* | 1.48* | 1.34* | 1.69** | 1.10 | 1.04 |
| (0.54) | (0.56) | (0.64) | (0.68) | (0.64) | (0.55) | (0.70) | (0.63) | ||
| Tertiary | 4.03*** | 3.79*** | 3.86*** | 4.68*** | 3.84*** | 4.77*** | 3.34*** | 3.52*** | |
| (0.65) | (0.66) | (0.79) | (0.85) | (0.78) | (0.66) | (0.87) | (0.78) | ||
| Partnership status (has a partner) | No partner | 0.67 | 0.41 | 0.81 | 0.94 | 0.22 | 0.99* | 0.75 | 0.55 |
| (0.47) | (0.49) | (0.54) | (0.58) | (0.56) | (0.47) | (0.61) | (0.57) | ||
| Make ends meet (easily) | Fairly easily | –0.90* | –0.95* | –1.11* | –0.55 | –1.24* | –0.85* | –1.01 | –0.46 |
| (0.43) | (0.44) | (0.51) | (0.54) | (0.52) | (0.43) | (0.56) | (0.51) | ||
| With difficulty | –2.20*** | –2.73*** | –1.51* | –2.12* | –3.71*** | –2.24*** | –1.06 | –1.23 | |
| (0.66) | (0.69) | (0.77) | (0.84) | (0.82) | (0.66) | (0.83) | (0.77) | ||
| Language [German (ch)] | French (ch) | –0.69 | –1.10* | 0.06 | –0.91 | –1.17* | –1.31** | 0.86 | –0.37 |
| (0.47) | (0.48) | (0.54) | (0.57) | (0.57) | (0.46) | (0.60) | (0.54) | ||
| Italian (ch) | –2.02 | –1.02 | –2.95* | –2.59 | –2.80 | –3.05* | 0.27 | –1.21 | |
| (1.24) | (1.24) | (1.36) | (1.54) | (1.48) | (1.38) | (1.43) | (1.23) | ||
| Living area (urban) | Rural | –0.31 | –0.15 | –0.33 | –0.57 | –0.14 | –0.50 | –0.01 | –0.47 |
| (0.39) | (0.40) | (0.46) | (0.48) | (0.47) | (0.39) | (0.50) | (0.46) | ||
| Self-rated health (poor/fair health) | Good health | 1.85*** | 1.73** | 1.71** | 2.24*** | 2.44*** | 1.52** | 1.84** | 1.74** |
| (0.55) | (0.60) | (0.63) | (0.67) | (0.67) | (0.57) | (0.70) | (0.65) | ||
| Very good/excellent health | 4.00*** | 3.56*** | 3.77*** | 5.07*** | 4.51*** | 3.51*** | 4.90*** | 3.42*** | |
| (0.58) | (0.63) | (0.67) | (0.71) | (0.72) | (0.59) | (0.75) | (0.70) | ||
| Constant | 31.96*** | 33.53*** | 30.31*** | 31.27*** | 31.77*** | 35.14*** | 26.42*** | 31.39*** | |
| (0.96) | (0.98) | (1.15) | (1.24) | (1.13) | (0.97) | (1.26) | (1.11) | ||
| Observations | 1625 | 1625 | 1625 | 1625 | 1625 | 1625 | 1625 | 1625 | |
Note: this table shows the regressions of the standardised health literacy score and the sub-indices on covariates. Sub-indices abbreviations: health care (hc_hl), disease prevention (dp_hl), health promotion (hp_hl), access health information (oi), understanding health information (ui), process health information (pi), apply health information (ai). Estimates and standard errors in parentheses, significance level: ∗p <0.05, ∗∗p <0.01, ∗∗∗p <0.001.
To the best of our knowledge, our study is the first nationally representative population-based study of health literacy of adults aged 58 and older in Switzerland. The HLS-EU-Q16 allows us to draw a comprehensive picture of health literacy based on individuals' self-assessed competencies to seek, understand, process and use health information to make decisions in everyday life. In addition, as the HLS-EU-Q16 is an instrument that is used internationally, it allows for comparisons between countries. The analysis showed that about one-third of older adults in Switzerland had inadequate or problematic levels of health literacy. Specifically, 6.8% had an inadequate level of health literacy, and 24.6% had a problematic level of health literacy. Multivariable analyses indicated that — holding other characteristics fixed — health literacy was lower in men, individuals with low levels of education and people who reported difficult in making their ends meet, and those with bad self-rated health. Most older adults in Switzerland found it easy to navigate the health care system and use appropriate health information. The health-related aspects where respondents perceived more difficulties were managing mental health problems, asking for a second opinion from another doctor, protecting oneself from illness based on information in the media, judging if the information on health risks in the media is reliable, and understanding information in the media on how to get healthier.
In comparison to previous nationwide studies of health literacy in Switzerland in 2020 [11], our study indicates a relatively higher level of health literacy. However, the age range differs considerably from our study population as the one from the FOPH, which included individuals 15 years old and above. Older adults tend to have more experience and are more likely to be confronted with health issues which may help them be more familiar with the healthcare system. Moreover, the study from the FOPH included more respondents with a migration background and difficulties with the local language than there are in our research. Additionally, the method of data collection was not the same; our study uses face-to-face interviews (CAPI) while the one from the FOPH uses a mix of online interviews (CAWI) and telephone interviews (CAPI). We feel the best option for interviewing older adults is in person as it avoids potential challenges with using a laptop and lessens the chance of hearing problems, which could occur over the phone. Some variations may also come from the fact that the study from the FOPH had 47 items while our study only included 16 items; in comparison, the shorter scale presents easier questions on health issues that are more common, which may allow individuals to have a better score [16, 17]. Compared to other European countries, our results are close to those with high health literacy distribution, such as Austria [18]. A potential explanation for the high levels of health literacy present in our results could be that older adults in Switzerland are often well-educated individuals with relatively good health and few financial difficulties.
The general health literacy score varied significantly between respondents depending on their sociodemographic characteristics such as gender, education, financial situation, and self-rated health status. We found that women had better health literacy scores than men. This result was statistically significant with the general measures of health literacy and through the different sub-indices. Other studies on general populations also found that women perceived fewer difficulties regarding health-related aspects than men [17, 19]. Gender differences in attitudes toward health and use of healthcare services are well documented: women have, on average, better overall adherence to health screening and prevention programs, and they make greater use of medical consultation [20]. The gender gap in health could be explained by women’s traditional role as caregivers, which remains relevant today and contributes to women’s increased knowledge and skills in attention to health [21].
Our analyses showed a strong positive association between education and health literacy scores and sub-indices. This result is not surprising as education develops transversal skills measured in the health literacy scale and applied to health-related issues [4]. Previous research demonstrated that communicating health information is not enough to improve health literacy, and educating individuals is fundamental [22–24]. For older adults, the conservation and development of an adequate level of health literacy depend mainly on whether or not they practice lifelong learning activities such as formal education, reading practices, internet use, and social or volunteering actions [2, 25].
Better health literacy is also associated with better phyical health; in our analyses, respondents with better self-rated health, a good predictor of individuals’ health status [26], were more likely to have a higher health literacy score. Although we don’t know exactly in which direction this association goes, it is likely that health literacy indirectly impacts health through multiple mechanisms; for instance, increased health literacy can lead to better behaviour such as more exercise or lower smoking rate or drinking, which will ultimately improve health status [5]. Moreover, there is a positive association between education level, health literacy, and self-rated health. A Dutch study showed that health literacy mediates the associations between education and self-reported health and concludes that improving health literacy could be a useful strategy to reduce health inequalities related to education [27].
Another important factor associated with low health literacy in our study is financial strain. Compared to individuals for whom it was easy to make ends meet, respondents with financial difficulty had lower health literacy. The HLS-EU consortium that developed the European Health Literacy Survey questionnaire found similar results concerning the negative association between health literacy and financial deprivation [7]. Similarly, in the 2020 nationwide study on health literacy in Switzerland by the FOPH, financial deprivation was one of the strongest drivers of low health literacy levels [28]. In another study, the authors describe the associations between individuals' sociodemographic characteristics such as education level or financial limitation, health-related behaviour, and health literacy, and attest that globally individuals with higher socioeconomic status tend to have better self-management regarding health issues [29]. Our findings outline a social gradient in health literacy in older adults living in Switzerland that may produce health inequality. Individuals with lower education, more limited financial resources and poor health status are at risk of being disadvantaged in accessing and using health services. Public health policies should use health literacy measures such as the European Health Literacy Survey questionnaire to target individuals affected by this triple burden. Health literacy interventions could include the use of simplified health information and accessible and easy-to-use eHealth tools [30]. However, although digitalization radically changes how individuals find information on health issues, policies should be particularly careful with older adults as they tend to display more difficulties with accessing digital information and lower levels of digital health literacy [11]. Improving patient-provider communication could also increase the shared decision-making and help the individuals to manage their health better. Moreover, a policy that would ask all citizens to answer a health literacy questionnaire periodically and offer specific intervention to respondents with an inadequate level of health literacy could help alleviate remaining social health inequalities in the Swiss population.
Our study has several limitations. First, the HLS-EU-Q16 questionnaire is a subjective measure that can include reporting bias where respondents would overrate their skills and underrate their problems. Nevertheless, the short version of the HLS-EU questionnaire also presents some advantages: it is more convenient as it is quicker for older adults to answer and is also a validated instrument [31, 32]. Second, our study findings may be challenged by remaining concerns about the representativeness of SHARE or issues related to missing data, which may bias our estimates. The selection effects and attrition might underrepresent a vulnerable group of very old adults or individuals in bad health disposition who did not participate in the main SHARE study due to their low literacy, education, unwillingness to participate, or health conditions. In addition, even if the study SHARE follows individuals in nursing homes, when necessary, such interviews remain challenging and not always feasible. In the study, missed participations were not a significant concern as the number of respondents who did not participate in the drop-off questionnaire was extremely low. Then, no critical tendency appeared when regressing on the set of covariates those who were not included due to missing values on the variables used in the analysis. Finally, the current design of the study does not allow us to determine a causal effect.
Despite a good level of health in Switzerland, which has one of the longest life expectancies in the world [33], one-third of older citizens report having difficulty managing their health. Our findings showed that men, individuals with low education, financial difficulties, and poor self-assessed health status are particularly at risk of presenting inadequate health literacy levels. The combination of social and health vulnerability with a low level of health literacy makes these population groups more likely to experience health inequalities. These findings emphasise that public health policies are needed to overcome this social gradient regarding health inequalities in the population. Accordingly, the FOPH provides teaching materials for individuals with low health literacy and information for healthcare providers on how they can promote the health literacy level of their patients [34]. With regards to the older adult population, health literacy screening for patients seems beneficial to overcome poor compliance with treatment and inappropriate health care decisions [35]. In addition, the promotion of lifelong learning activities and the simplification of health information accessible on the Internet could help reduce the share of individuals with inadequate health literacy levels [25].
This paper uses data from Börsch-Supan, A. (2020). Survey of Health, Ageing and Retirement in Europe (SHARE) Wave 8. Release version: 1.0.0. SHARE-ERIC. Data set. DOI: 10.6103/SHARE.w8.100. Study data already de-identified are available to the scientific community upon submitting a data requestion application to the SHARE study.
The authors are grateful to Dr Valérie-Anne Ryser and Dr Robert Reinecke for their precious advice and support.
Clément Meier
University of Lausanne
Bâtiment Géopolis, FORS
1015 Lausanne, Switzerland
clement.meier[at]unil.ch
SNSF funding for the EOL project. Healthy Ageing in the Face of Death: Preferences, Communication, Knowledge and Behaviors Regarding End of Life and End-of-life Planning Among Older Adults in Switzerland (grant number: 10001C_188836).
The SHARE data collection has been funded by the European Commission, DG RTDthrough FP5 (QLK6-CT-2001-00360), FP6 (SHARE-I3: RII-CT-2006-062193, COMPARE: CIT5-CT-2005-028857, SHARELIFE: CIT4-CT-2006-028812), FP7 (SHARE-PREP: GA N°211909, SHARE-LEAP: GA N°227822, SHARE M4: GA N°261982, DASISH: GA N°283646) andHorizon 2020(SHARE-DEV3: GA N°676536, SHARE-COHESION: GA N°870628,SERISS: GA N°654221, SSHOC: GA N°823782) and by DG Employment, Social Affairs & Inclusion through VS 2015/0195, VS 2016/0135, VS 2018/0285, VS 2019/0332, and VS 2020/0313. Additional funding from the German Ministry of Education and Research, the Max Planck Society for the Advancement of Science, the U.S. National Institute on Aging (U01_AG09740-13S2, P01_AG005842, P01_AG08291, P30_AG12815, R21_AG025169, Y1-AG-4553-01, IAG_BSR06-11, OGHA_04-064, HHSN271201300071C, RAG052527A) and from various national funding sources is gratefully acknowledged(see).
The authors declare that they have no competing interests.
1. Santana S , Brach C , Harris L , Ochiai E , Blakey C , Bevington F , et al. Updating Health Literacy for Healthy People 2030: Defining Its Importance for a New Decade in Public Health. J Public Health Manag Pract. 2021 Nov-Dec;27 Suppl 6:S258–64. https://doi.org/10.1097/PHH.0000000000001324 Edifix has not found an issue number in the journal reference. Please check the volume/issue information. (Ref. 1 "Santana, Brach, Harris, Ochiai, Blakey, Bevington, et al., 2021")
2. Kickbusch I , Pelikan JM , Apfel F , Tsouros AD . World Health Organization, editors. Health literacy: the solid facts. Copenhagen: World Health Organization Regional Office for Europe; 2013. 73 p. (The solid facts).
3. Pelikan J , Ganahl K , Van den Broucke S , Sorensen K . Measuring health literacy in Europe: Introducing the European Health Literacy Survey Questionnaire (HLS-EU-Q). 2019 [cited 2021 Aug 6]; Available from: https://dial.uclouvain.be/pr/boreal/object/boreal:219963
4. Sørensen K , Van den Broucke S , Fullam J , Doyle G , Pelikan J , Slonska Z , et al.; (HLS-EU) Consortium Health Literacy Project European . Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012 Jan;12(1):80. https://doi.org/10.1186/1471-2458-12-80
5. Okan O, Bauer U, Levin-Zamir D, Pinheiro P, Sørensen K. International Handbook of Health Literacy : Research, practice and policy across the lifespan [Internet]. Policy Press; 2019 [cited 2021 Jul 12]. Available from: https://library.oapen.org/handle/20.500.12657/24879
6. Schaeffer D , Berens EM , Vogt D . Health Literacy in the German Population. Dtsch Arztebl Int. 2017 Jan;114(4):53–60.
7. Sørensen K , Pelikan JM , Röthlin F , Ganahl K , Slonska Z , Doyle G , et al.; HLS-EU Consortium . Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health. 2015 Dec;25(6):1053–8. https://doi.org/10.1093/eurpub/ckv043
8. Levin-Zamir D , Baron-Epel OB , Cohen V , Elhayany A . The Association of Health Literacy with Health Behavior, Socioeconomic Indicators, and Self-Assessed Health From a National Adult Survey in Israel. J Health Commun. 2016;21(sup2):61–8.
9. Murray CJ , Frenk J . Policy WHOGP on E for H. A WHO framework for health system performance assessment [Internet]. World Health Organization; 1999 [cited 2021 Oct 22]. Available from: https://apps.who.int/iris/handle/10665/66267
10. Spycher, J., Morisod, K., Eggli, Y., Moschetti, K., Le Pogam, M.-A., Peytremann-Bridevaux, I., Bodenmann, P., & Marti, J. Indicators on Healthcare Equity in Switzerland. New Evidence and Challenges. Report commissioned by the Federal Office of Public Health. Bern: FOPH [Internet]. 2021 [cited 2022 Feb 10]. Available from: https://www.bag.admin.ch/bag/en/home/strategie-und-politik/nationale-gesundheitsstrategien/gesundheitliche-chancengleichheit/chancengleichheit-in-der-gesundheitsversorgung/chancengerechtigkeit-messen.html
11. De Gani SM , Jaks R , Bieri U , Kocher JP . Health Literacy Survey Schweiz 2019-2021. Schlussbericht im Auftrag des Bundesamtes für Gesundheit BAG. Zürich, Careum Stiftung. [Internet]. 2021 [cited 2022 Jan 12]. Available from: https://www.bag.admin.ch/bag/en/home/strategie-und-politik/nationale-gesundheitspolitik/gesundheitskompetenz.html
12. Ladin K , Buttafarro K , Hahn E , Koch-Weser S , Weiner DE . “End-of-Life Care? I’m not Going to Worry About That Yet.” Health Literacy Gaps and End-of-Life Planning Among Elderly Dialysis Patients. Gerontologist. 2018 Mar;58(2):290–9. https://doi.org/10.1093/geront/gnw267
13. Börsch-Supan A , Brandt M , Hunkler C , Kneip T , Korbmacher J , Malter F , et al.; SHARE Central Coordination Team . Data Resource Profile: the Survey of Health, Ageing and Retirement in Europe (SHARE). Int J Epidemiol. 2013 Aug;42(4):992–1001. https://doi.org/10.1093/ije/dyt088
14. Hoffmeyer-Zlotnik JH , Wolf C , editors . International Standard Classification of Education, ISCED 1997. In: Advances in Cross-National Comparison: A European Working Book for Demographic and Socio-Economic Variables [Internet]. Boston, MA: Springer US; 2003 [cited 2021 Aug 7]. p. 195–220. Available from: https://doi.org/https://doi.org/10.1007/978-1-4419-9186-7_10
15. The Survey of Health . Ageing and Retirement in Europe (SHARE): Release Guides [Internet]. [cited 2019 Aug 3]. Available from: http://www.share-project.org/data-documentation/release-guides.html
16. Tiller D , Herzog B , Kluttig A , Haerting J . Health literacy in an urban elderly East-German population - results from the population-based CARLA study. BMC Public Health. 2015 Sep;15(1):883. https://doi.org/10.1186/s12889-015-2210-7
17. Svendsen MT , Bak CK , Sørensen K , Pelikan J , Riddersholm SJ , Skals RK , et al. Associations of health literacy with socioeconomic position, health risk behavior, and health status: a large national population-based survey among Danish adults. BMC Public Health. 2020 Apr;20(1):565. https://doi.org/10.1186/s12889-020-08498-8
18. The HLS19 Consortium of the WHO Action Network M-POHL . (2021): International Report on the Methodology, Results, and Recommendations of the European Health Literacy Population Survey 2019-2021 (HLS19) of M-POHL. Austrian National Public Health Institute, Vienna [Internet]. [cited 2022 Feb 10]. Available from: https://m-pohl.net/node/42
19. van der Heide I , Rademakers J , Schipper M , Droomers M , Sørensen K , Uiters E . Health literacy of Dutch adults: a cross sectional survey. BMC Public Health. 2013 Feb;13(1):179. https://doi.org/10.1186/1471-2458-13-179
20. Jean-Yves Le Talec, Danièle Authier, Sylvie Tomolillo. La promotion de la santé au prisme du genre : Guide théorique et pratique - Livre [Internet]. Les Presses de l’EHESP. [cited 2021 Aug 2]. Available from: https://www.presses.ehesp.fr/produit/promotion-de-sante-prisme-genre/
21. Colombo F , Llena-Nozal A , Mercier J , Tjadens F . Help Wanted?: Providing and Paying for Long-Term Care [Internet]. OECD; 2011 [cited 2021 Aug 2]. (OECD Health Policy Studies). Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/help-wanted_9789264097759-en
22. Nutbeam D . Health literacy as a public health goal: a challenge for contemporary health education and communication strategies into the 21st century. Health Promot Int. 2000 Sep;15(3):259–67. https://doi.org/10.1093/heapro/15.3.259
23. Nutbeam D , McGill B , Premkumar P . Improving health literacy in community populations: a review of progress. Health Promot Int. 2018 Oct;33(5):901–11. https://doi.org/10.1093/heapro/dax015
24. Nutbeam D . Health education and health promotion revisited. Health Educ J. 2019 Oct;78(6):705–9. https://doi.org/10.1177/0017896918770215
25. Wister AV , Malloy-Weir LJ , Rootman I , Desjardins R . Lifelong educational practices and resources in enabling health literacy among older adults. J Aging Health. 2010 Sep;22(6):827–54. https://doi.org/10.1177/0898264310373502
26. Wu S , Wang R , Zhao Y , Ma X , Wu M , Yan X , et al. The relationship between self-rated health and objective health status: a population-based study. BMC Public Health. 2013 Apr;13(1):320. https://doi.org/10.1186/1471-2458-13-320
27. van der Heide I , Wang J , Droomers M , Spreeuwenberg P , Rademakers J , Uiters E . The relationship between health, education, and health literacy: results from the Dutch Adult Literacy and Life Skills Survey. J Health Commun. 2013;18(sup1 Suppl 1):172–84. https://doi.org/10.1080/10810730.2013.825668
28. Bieri U , Kocher JP , Gauch C , Tschöpe S , Venetz A , Hagemann M , et al. Study commissioned by the Swiss Federal Office of Public Health FOPH, Health Strategies Division. :8.
29. Goldman DP , Smith JP . Can patient self-management help explain the SES health gradient? Proc Natl Acad Sci USA. 2002 Aug;99(16):10929–34. https://doi.org/10.1073/pnas.162086599
30. Visscher BB , Steunenberg B , Heijmans M , Hofstede JM , Devillé W , van der Heide I , et al. Evidence on the effectiveness of health literacy interventions in the EU: a systematic review. BMC Public Health. 2018 Dec;18(1):1414. https://doi.org/10.1186/s12889-018-6331-7
31. Eronen J , Paakkari L , Portegijs E , Saajanaho M , Rantanen T . Assessment of health literacy among older Finns. Aging Clin Exp Res. 2019 Apr;31(4):549–56. https://doi.org/10.1007/s40520-018-1104-9
32. Lorini C , Lastrucci V , Mantwill S , Vettori V , Bonaccorsi G ; Florence Health Literacy Research Group . Measuring health literacy in Italy: a validation study of the HLS-EU-Q16 and of the HLS-EU-Q6 in Italian language, conducted in Florence and its surroundings. Ann Ist Super Sanita. 2019 Jan-Mar;55(1):10–8.
33. OECD/WHO (2011), OECD Reviews of Health Systems: Switzerland 2011, OECD Publishing. [Internet]. Paris: Organisation for Economic Co-operation and Development; 2011 [cited 2021 Oct 27]. Available from: http://dx.doi.org/https://doi.org/10.1787/9789264120914-en
34. FOPH FO of PH . Strengthening health literacy of disadvantaged groups [Internet]. [cited 2021 Oct 27]. Available from: https://www.bag.admin.ch/bag/en/home/strategie-und-politik/nationale-gesundheitsstrategien/gesundheitliche-chancengleichheit/gesundheitskompetenz-von-benachteiligten-staerken.html
35. Chesser AK , Keene Woods N , Smothers K , Rogers N . Health Literacy and Older Adults: A Systematic Review. Gerontol Geriatr Med. 2016 Mar;2:2333721416630492. https://doi.org/10.1177/2333721416630492
The questions with the 16 items from the HLS-EU-Q16 scale
First, we would like to ask you how comfortable you feel when dealing with health-related information.
For you, how easy or difficult is it to…
Answer categories: "Very easy", "Fairly easy", "Fairly difficult", "Very difficult"
Health care
Disease prevention
8. Understand health warnings about behaviour such as smoking, low physical activity, and excessive drinking?
9. Understand why you need health screenings?
10. Find information on how to manage mental health problems like stress or depression?
11. Decide how you can protect yourself from illness based on information in the media?
12. Judge if the information on health risks in the media is reliable?
Health promotion
13. Understand advice on health from family members or friends?
14. Judge which everyday behaviour is related to your health?
15. Find out about activities that benefit your mental well-being?
16. Understand information in the media on how to be healthier?