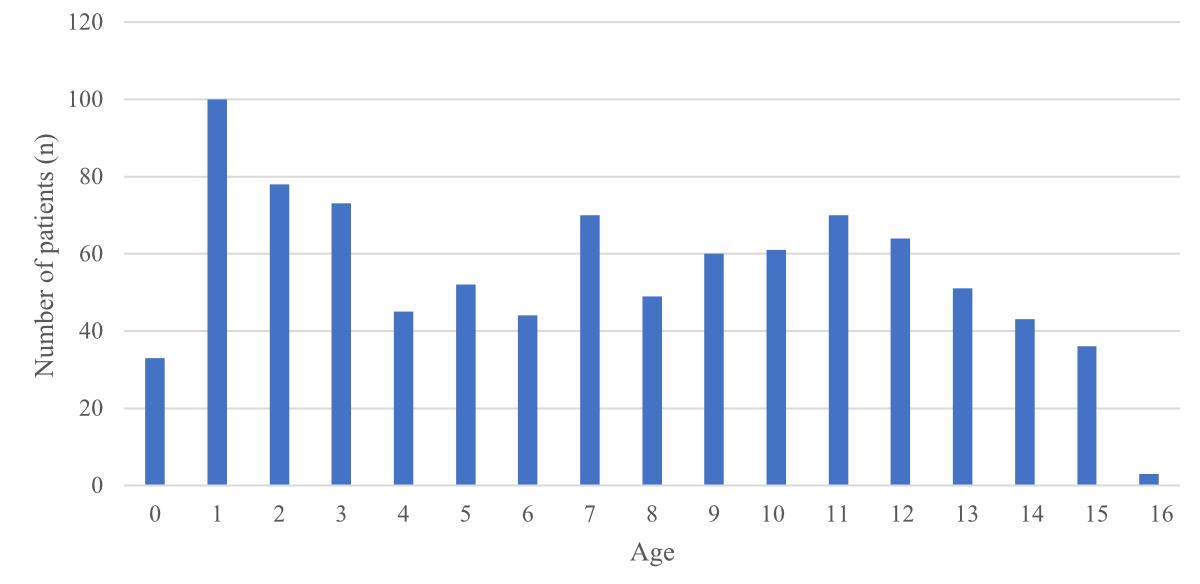
Figure 1 Age distribution of patients with hand and finger injuries.
DOI: https://doi.org/10.4414/SMW.2022.w30134
Hand and finger injuries in children are frequent reasons for presentation and account for 1.16–1.8% of presentations to the paediatric emergency department [1, 2]. Previous studies have examined incidence, pattern and location of hand and finger injuries as well as patient demographics in the paediatric population [3–5].
In contrast, there is a research gap regarding the association between subspecialty involvement in the management of these injuries and length of stay, patient flow and patient care in the paediatric emergency department.
Similar to adult surgery, paediatric surgery is becoming increasingly subspecialised owing to technological advances in diagnostics and treatment, as well as increasing patient and parental expectations. However, as pathologies might intersect, this division into, for example paediatric urology and paediatric orthopaedics, may in certain cases challenge the straightforward allocation of patients to treating teams [6]. In clinical practice, inconsistent subspecialty referral processes in the paediatric emergency department may considerably delay treatment and adequate care by the definitive surgeon and thus impact negatively on patient outcome. Obstruction of patient flow and emergency department crowding may have a detrimental influence on patient care and patient safety [7, 8]. In Switzerland, no general referral guidelines exist for children presenting to the emergency department with finger and hand injuries. These are currently treated by either paediatric emergency medicine physicians, paediatric surgeons or hand surgeons, depending on injury severity or skills of the involved physicians. The current informal local standard implies treatment of injuries requiring minor procedures by paediatric emergency medicine physicians. Children with injuries to the dorsum of the hand needing surgery are treated by paediatric surgeons, whereas children with injuries to the palm of the hand and more complex injuries are treated by the department of hand surgery. This study set out to examine the association of current, non-guideline-based multiple subspecialty consultation practice for this patient group, and paediatric emergency department length of stay and patient flow. We aimed to identify obstacles and enablers for timely patient referral and management and to suggest what best practice should be.
This was a cross-sectional study with retrospective chart review of the hospital electronic medical records from visits to a Swiss tertiary paediatric emergency department (26,000 presentations/year) for the treatment of hand and finger injuries conducted as a clinical audit service. Clinical audits allow review of the quality of care and significant events. Audits generate findings that will benefit patient care but may also create new scientific knowledge that may change practice and improve future patient care.
Patients under 17 years of age presenting to the paediatric emergency department with hand or finger injuries or infections from November 2015 to March 2017 were included fin the analysis.
Patients aged <17 years, with hand and finger injuries distal to the distal radius were included.
Exclusion criteria were fractures including and proximal to the distal radius, multiple trauma, systemic infections and allergic reactions to the hand or finger.
Association between current subspecialty referral practice and paediatric emergency department length of stay was the primary outcome.
Current subspecialty referral practice, hand and finger injury type, pattern, incidence, cause and treatment modality were secondary outcomes.
Patient demographics (age, gender, date, type, cause and treatment modality of injury, disposition from paediatric emergency department) and study data (length of stay in the paediatric emergency department, type of subspecialty referral, number of different subspecialty reviews per patient, final patient ownership and treatment) were retrieved from the hospital electronic medical records. Length of stay was defined as the period between admission and discharge from the paediatric emergency department. Missing, conflicting and ambiguous chart elements were coded as missing data. The abstractors were not blinded to the study question.
IBM SPSS (version 28.0.0.0) and Microsoft Excel (version 16.51) were used for data analysis. Because of the relatively small sample size, a non-normal distribution was assumed and confirmed using the Shapiro-Wilk test. Comparisons between multiple groups of both metric and ordinal scaled data were conducted using the Kruskal-Wallis test for independent samples. Pairwise comparisons were performed using the Mann-Whitney-U-test for independent samples. To determine whether the distributions of the categorical variables differed from each other, a contingency table analysis (Fisher’s exact test) was performed. The level of significance was set at α = 0.05. To evaluate where the statistical significant effect occurred, a subsequent adjusted standardised residuals analysis [9] was carried out. To avoid the occurrence of a type I Error, a Bonferroni correction was applied to the p-values. To determine if an association between metric and nominal data existed, an eta-correlation was calculated. Continuous variables were described as median or mean (with confidence interval (CI), interquartile range, or standard deviation) and categorical variables by frequency and percentage.
Over 17 months, we identified 932 paediatric emergency department visits for hand and finger injuries, accounting for 2.2% (932/41,729) of all consultations, with a male preponderance (n = 517, 56%; females n = 415, 44%) and a mean age of 7.08 years (95% CI 6.79–7.37). There were peaks of injuries in children under 2 years, aged 6 to 7 years or 10 to 14 years as compared with the remainder of the patients; however this was not statistically significant (p = 0.187; fig. 1). Whereas typical lesions in infants included burns and finger injures (e.g., jamming/crush injuries), more complex hand lesions and injuries affecting multiple digits mostly occurred in older children. With increasing age, sports-associated injuries were more frequent, peaking at ages 7 and 11 years (table 1).
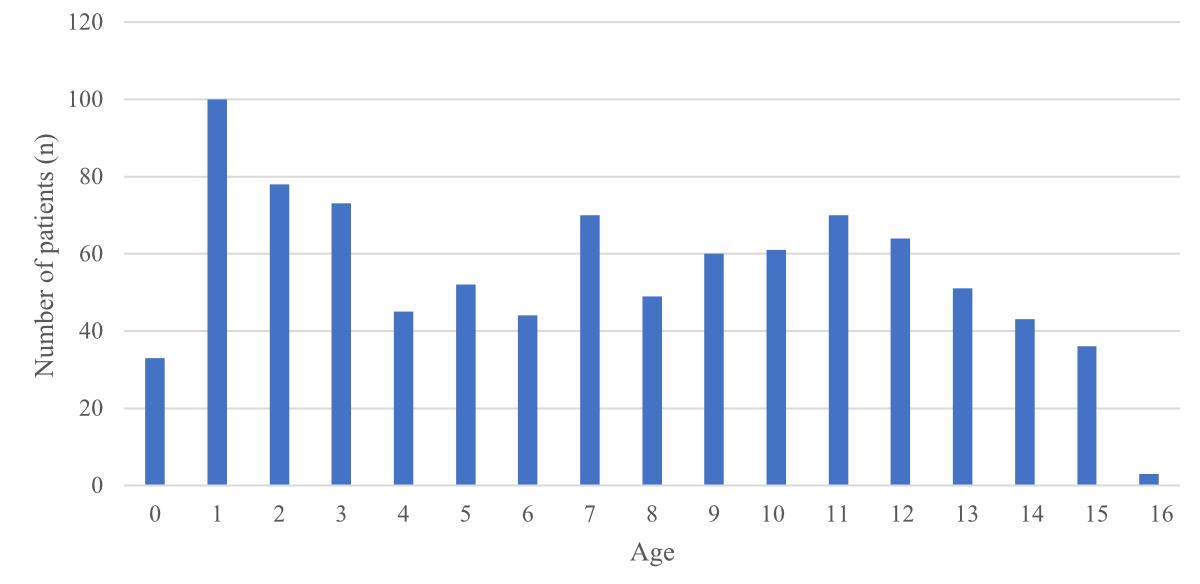
Figure 1 Age distribution of patients with hand and finger injuries.
Table 1Frequency and type of injury according to age.
| Infants | Preschool children | School children | Teenagers/adolescents | Total | ||||||
| (0–1 yr) | (2–5 yr) | (6–12 yr) | (12–16 yr) | |||||||
| n | % | n | % | n | % | n | % | n | % | |
| Superficial laceration | 27 | 20.3% | 49 | 19,8% | 52 | 12.4% | 9 | 6.8% | 137 | 14.7% |
| Extensor tendon injury | 1 | 0.8% | 2 | 0.8% | 6 | 1.4% | 3 | 2.3% | 12 | 1.3% |
| Flexor tendon injury | 1 | 0.8% | 0 | 0.0% | 0 | 0.0% | 0 | 0.0% | 1 | 0.1% |
| Nerve lesion | 0 | 0.0% | 1 | 0.4% | 1 | 0.2% | 0 | 0.0% | 2 | 0.2% |
| Contusion | 15 | 11.3% | 42 | 16.9% | 140 | 33.5% | 51 | 38.3% | 248 | 26.6% |
| (Meta-)carpal fracture | 0 | 0.0% | 0 | 0.0% | 14 | 3.3% | 12 | 9.0% | 26 | 2.8% |
| Single digital fracture | 6 | 4.5% | 30 | 12.1% | 99 | 23.7% | 33 | 24.8% | 168 | 18.0% |
| Fingertip amputation | 3 | 2.3% | 10 | 4.0% | 7 | 1.7% | 2 | 1.5% | 22 | 2.4% |
| Joint sprain | 2 | 1.5% | 1 | 0.4% | 3 | 0.7% | 8 | 6.0% | 14 | 1.5% |
| Nail- and nail bed injury | 9 | 6.8% | 30 | 12.1% | 30 | 7.2% | 2 | 1.5% | 71 | 7.6% |
| Infection | 8 | 6.0% | 27 | 10.9% | 29 | 6.9% | 3 | 2.3% | 67 | 7.2% |
| Dermabrasio | 1 | 0.8% | 6 | 2.4% | 2 | 0.5% | 2 | 1.5% | 11 | 1.2% |
| Burn | 45 | 33.8% | 32 | 12.9% | 8 | 1.9% | 4 | 3.0% | 89 | 9.5% |
| Bite | 9 | 6.8% | 3 | 1.2% | 6 | 1.4% | 0 | 0.0% | 18 | 1.9% |
| Complex injury | 1 | 0.8% | 5 | 2.0% | 6 | 1.4% | 2 | 1.5% | 14 | 1.5% |
| Amputation | 1 | 0.8% | 2 | 0.8% | 0 | 0.0% | 1 | 0.8% | 4 | 0.4% |
| Other | 4 | 3.0% | 8 | 3.2% | 15 | 3.6% | 1 | 0.8% | 28 | 3.0% |
| Total | 133 | 100% | 248 | 100% | 418 | 100% | 133 | 100% | 932 | 100% |
Distribution of injuries listed for each age group. The remainder is summarisd under “Other”.
The most frequent injuries were contusions (n = 248, 27%) and fractures (n = 194, 21%) (table 2). Border rays were affected more frequently, but this was not statistically significant. About one in ten children (n = 99, 11%) had sustained multiple digit injuries (fig. 2). The right (n = 455, 49%) and left (n = 456, 49%) hands were affected equally often in unilateral injuries, and bilateral injuries were recorded in 14 cases (1.5%) (n = 7, 0.8% missing). The leading causes were direct falls onto the hand (n = 237, 25%) and crushing or jamming (n = 203, 22%), followed by lacerations (n = 139, 15%), direct impact (n = 134, 14%), burns (n = 89, 9.5%), infections (n = 41, 4.4%), foreign body penetrations (n = 26, 2.8%), animal (n = 25, 2.7%) or insect bites (n = 12, 1.3%) and other (n = 26, 2.8%).
Table 2Causes for presentation to paediatric emergency department and admission to hospital per injury type.
| Patients treated in paediatric emergency department (%) (paediatric emergency medicine / paediatric surgery / hand surgery) | Admissions to hospital (% of injury type) (paediatric surgery / hand surgery) | |
| Overall number of patients | 932 (817 / 75 / 40) | 87 (50 / 37) |
| Contusion | 248 (26.6%) (248 / 0 / 0) | 0 (0%) (0 / 0) |
| Single digital fracture | 168 (18.0%) (146 / 19 / 3) | 11 (6.5%) (8 /3) |
| Superficial laceration | 137 (14.7%) (126 / 9 / 2) | 3 (2.2%) (2 / 1) |
| Burn | 89 (9.5%) (79 / 10 / 0) | 8 (9.0%) (8 / 0) |
| Nail and nail bed injury | 71 (7.6%) (67 / 3 / 1) | 2 (2.8%) (1 / 1) |
| Infection | 67 (7.2%) (49 / 12 / 6) | 16 (23.9%) (10 / 6) |
| Various | 28 (3.0%) (26 / 2 / 0) | 2 (7.1%) (2 / 0) |
| (Meta-)carpal fracture | 26 (2.8%) (25 / 1 / 0) | 1 (3.8%) (1 / 0) |
| Fingertip amputation | 22 (2.4%) (10 / 8 / 4) | 10 (45.5%) (7 / 3) |
| Bite | 18 (1.9%) (16 / 2 / 0) | 2 (11.1%) (2 / 0) |
| Complex injury | 14 (1.5%) (0 / 1 / 13) | 14 (100%) (1 / 13) |
| Joint sprain | 14 (1.5%) (12 / 1 / 1) | 2 (14.3%) (1 / 1) |
| Extensor tendon lesion | 12 (1.3%) (2 / 6 / 4) | 9 (75.0%) (6 / 3) |
| Dermabrasion | 11 (1.2%) (11 / 0 / 0) | 0 (0%) (0 / 0) |
| Amputation/devascularisation | 4 (0.4%) (0 / 0 / 4) | 4 (100%) (0 / 4) |
| Nerve lesion | 2 (0.2%) (0 / 1 / 1) | 2 (100%) (1 / 1) |
| Flexor tendon lesion | 1 (0.1%) (0 / 0 / 1) | 1 (100%) (0 / 1) |
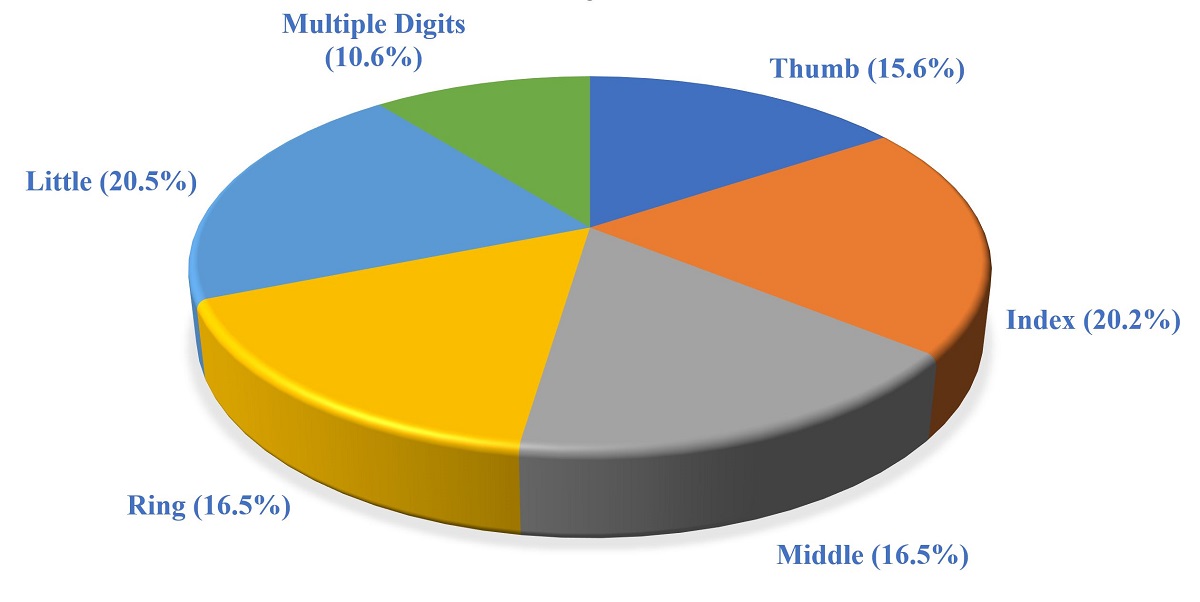
Figure 2 Frequency of fingers affected in paediatric hand and finger injuries.
More injuries were treated by paediatric emergency medicine physicians (n = 817) compared with paediatric surgeons (n = 75, p <0.001) or hand surgeons (n = 40, p <0.001). This was statistically significant. No significant difference was seen between paediatric or hand surgery as leading discipline (p = 0.242). Of those children receiving definitive treatment by hand surgeons, 37.5% (n = 15) were seen by all three disciplines and 62.5% (n = 25) by paediatric emergency medicine and hand surgery specialists only. Among those patients receiving definitive treatment by paediatric surgeons, 98.7% (n = 74) were seen by paediatric emergency medicine and paediatric surgery only and 1.3% (n = 1) by all three disciplines. A statistically significant difference was found between involvement of different subspecialties with respect to type of injury (p <0.001, Fisher’s exact test). Adjusted standardised residuals analysis with Bonferroni correction showed that the statistical significance was largely due to a higher than expected number of extensor and flexor tendon injuries, complex injuries and amputations treated by hand surgeons, whereas paediatric surgeons treated a higher than expected percentage of extensor tendon injuries and fingertip amputations, based on the null hypothesis of no difference between the three disciplines (fig. 3).
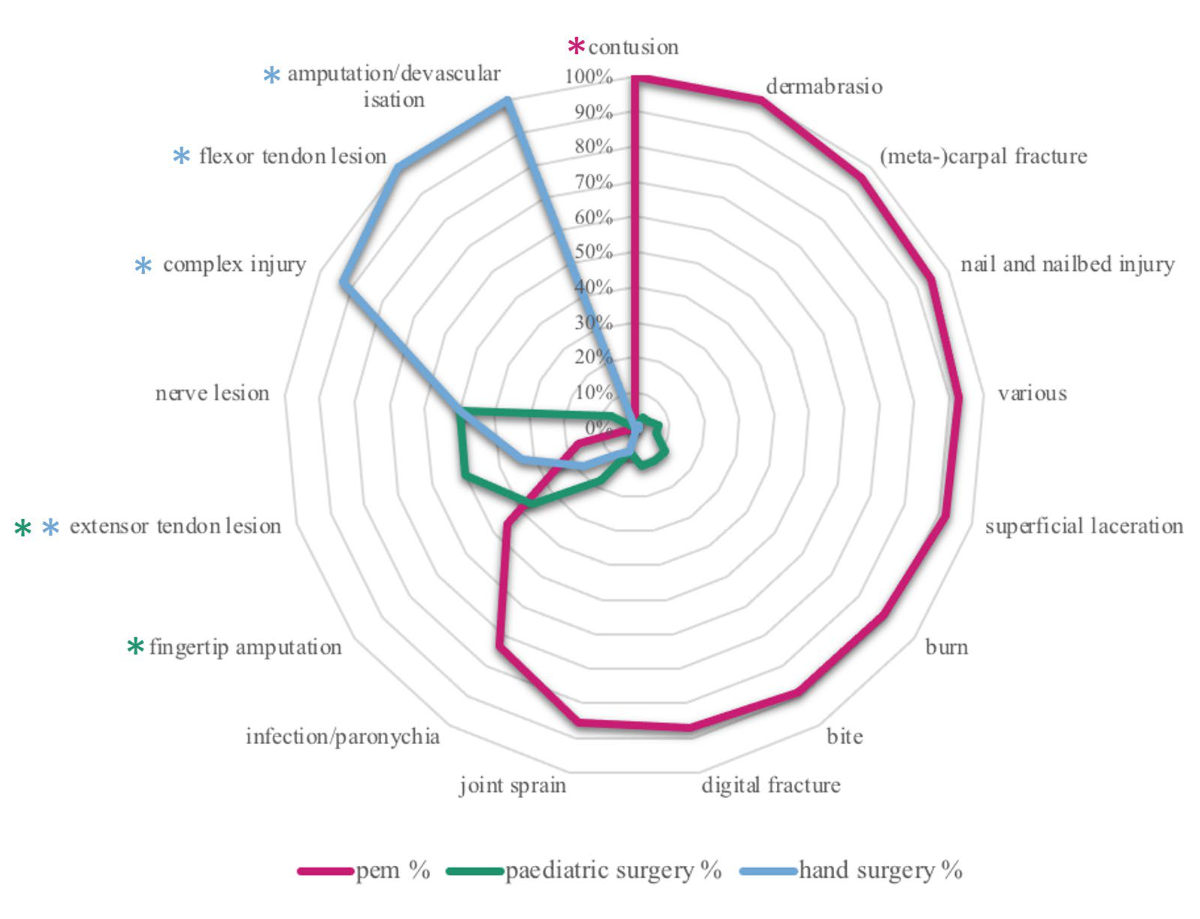
Figure 3 Distribution of injury patterns by treating discipline.
* Higher than expected (p <0.001) (adjusted standardised residuals analysis with Bonferroni correction). For a clearer presentation of the data, only those injuries where the frequency of treatment was higher than expected were marked.
Mean length of stay for all patients was 154 min (95% CI 146–162). There was a statistically significant difference in mean length of stay for patients treated by paediatric emergency medicine physicians alone (142 min, 95% CI 134–150) versus those requiring specialist involvement (241 min, 95% CI 215–268; 249 min, 95% CI 219–280; p <0.01 when paediatric surgery was involved, vs 228 min, 95% CI 175–281; p <0.01 when hand surgery was involved). In contrast, there was no significant difference between length of stay for patients treated by paediatric surgeons vs hand surgeons (p = 0.079). When treated by two disciplines, mean length of stay was 243 min (95% CI 213–273) and when treated by three disciplines, mean length of stay was 235 min (95% CI 169–301). This difference was not statistically significant (p = 1).
When admission to the operating theatre or ward was required, mean length of stay was 234 min (95% CI 202–265) with a minimally longer length of stay for paediatric surgery (mean 236 min, 95% CI 199–273) versus hand surgery (mean 231 min, 95% CI 174–289) patients. This difference was not statistically significant (p = 0.31). Mean length of stay for patients suffering multiple injuries to the hand was 188 min (95% CI 114–261) and for patients with isolated trauma was 154 min (95% CI 145–162). This difference was not statistically significant (p = 0.32). Length of stay was shortest for patients with amputations (mean 102 min, 95% CI 24–179). There was a poor correlation between length of stay and type of injury (eta2 = 0.073).
Nearly one in ten children (n = 87, 9.3%) required hospital admission (see table 1), in most cases for treatment of local infections (18%) and multiple hand and finger injuries (16%), and less frequently for single finger fractures (13%) and fingertip amputations (12%). Fifty-one admitted patients were treated by paediatric surgeons (59%) and 36 (41%) by hand surgeons, with surgery rates of 78% (40/51) and 100%, respectively. This difference was statistically significant (p <0.05). There was no statistically significant difference in type of treatment or subspecialty involvement in relation to age groups.
This study examined the association between current non-guideline-based consultation practice for children with hand and finger injuries presenting to a tertiary paediatric emergency department and length of stay and patient flow in the emergency department. Mean length of stay in the emergency department was significantly shorter for patients requiring minor treatment by paediatric emergency medicine physicians alone, constituting the majority of children in our study. Length of stay was significantly longer when any surgical subspecialty provided definitive treatment, thus confirming previous findings [10]. Patients treated by one or two subspecialties spent twice as much time in the emergency department, most likely due to the more complex nature of the injuries on one hand, but also organisational shortcomings in the consultation process such as allocation to busy operating theatre lists and associated reduced presence of surgical staff whilst on call for the emergency department and increased waiting time for surgical subspecialty consultation. Of note, surgical treatment time in the operating theatre was added to the emergency department length of stay. We can only speculate that timely patient flow may also have been blocked by issues such as reduced operating theatre availability, readiness of anaesthetic staff, bed block and lack of a more rigorous referral process. Interestingly, length of stay was shorter, although not significantly, for patients managed by hand surgeons (mean 228 min) compared with those seen by paediatric surgeons (mean 249 min). This may possibly be explained by higher triage categories given to these patients triggered by the severity of injury and risk of ischaemic compromise, thus ensuing earlier patient review and referral to hand surgery.
In this study, disposition was direct discharge from the emergency department for 9 in 10 children who required minor procedures only, such as wound repair, closed fracture reduction or plaster application. Of these, only 28 (3%) required subspecialty involvement. One in 10 patients, however, was admitted to hospital, with a ratio of paediatric vs hand surgery involvement of approximately 3:2. Disposition from the emergency department was individually decided on a case-by-case basis. Likewise, subspecialty referral practice was heterogeneous, but we found a recurrent pattern of hospital admission under paediatric surgery or less complex injuries (e.g., burns, simple finger fractures, fingertip amputations, injuries to the dorsum of the hand) and under hand surgery for more complex lesions (amputations, injuries to the palm of the hand (see fig. 3).
Surgical subspecialist consultation remains a challenge in teaching hospitals with high fluctuations of paediatric emergency medicine, paediatric surgery and hand surgery trainees, and where different disciplines might be responsible for the same anatomical region. Untargeted or redundant subspecialty reviews of hand and finger injuries may lead to repeated opening of wound dressings until review by the appropriate specialist, increased patient stress and pain, delay of definitive surgery, longer emergency department length of stay and, possibly, poor patient outcome and emergency department crowding. The latter has been found to be linked to ineffective administration of antibiotics and pain management, long waiting times and patient and staff dissatisfaction [11]. The delivery of high-quality care to children is a statutory obligation for healthcare organisations subject to the Health Act and clinical governance [12, 13]. It is an ethical imperative to strive for optimal patient care including timely consultation by the most appropriate surgeon and high-quality repair of hand and finger injuries with excellent outcomes. We observed a relatively short length of stay for mild and extremely severe injuries where allocation to treating disciplines seemed evident from the time of admission to the emergency department. For all other injuries requiring surgical care this seemed less clearly defined and consequently prolonged the length of stay.
In the light of our data, we therefore suggest the implementation of clear referral guidelines for the treatment of hand and finger injuries in Swiss paediatric emergency departments, for example including direct involvement of the appropriate surgical subspecialty at triage or standardised joint consultations for predefined injuries.
This study reported an occurrence of 2.2% of hand and finger injuries in the emergency department, approximately two cases per day. This represents a larger number than previously reported [1, 2], possibly due to the fact that parents preferred to be seen in the emergency department directly, as opposed to primary care, even with minor injuries [14]. In contrast to a previously reported bimodal injury distribution with mainly crush injuries in under 2-year-olds and more complex injuries in 10–14-year-old children in a study from the US [2], we observed a third, statistically not significant increase in frequency of injuries at six to seven years, with injury patterns similar to those of adolescents. We can only speculate that this additional peak may be explained by a higher risk for sport injuries in Swiss children as compared with other cultures. Consistent with earlier reports, border rays were more often affected than central rays, complexity of injuries increased with age [15] and the majority of injuries were minor [2–4] and treatable in the outpatient paediatric emergency department.
Because of the retrospective nature of our study, we did not investigate the true times to subspecialty consultation, anaesthesiology review and operating theatre / ward transfer, and we did not examine whether there are specific drivers, enablers or obstacles for referral to paediatric versus hand surgery, and patient transfer to the ward / operating theatre as this is not routinely documented in our institution. The actual reasons for delay in disposition from the emergency department were not assessed in this study and should be explored in future research. Collecting this information would be highly useful for future clinical practice.
These results suggest that the implementation of standardised referral guidelines for effective and safe clinical practice and decision-making in the management of hand and finger injuries in Swiss paediatric emergency departments might not only substantially shorten length of stay in the emergency department but result in faster, high-quality care and optimal patient outcome. Process mapping (or flow charting) has been shown to help visualise the specific steps of any process in a working environment [16]. Analysis and improvement of patient flow may be applied to any other patient group in the emergency department and future studies are required to obtain evidence for their efficacy.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
No funding sources declared by the authors
1. Doraiswamy NV , Baig H . Isolated finger injuries in children—incidence and aetiology. Injury. 2000 Oct;31(8):571–3. https://doi.org/10.1016/S0020-1383(00)00052-8
2. Shah SS , Rochette LM , Smith GA . Epidemiology of pediatric hand injuries presenting to United States emergency departments, 1990 to 2009. J Trauma Acute Care Surg. 2012 Jun;72(6):1688–94. https://doi.org/10.1097/TA.0b013e31824a4c5b
3. Bhende MS , Dandrea LA , Davis HW . Hand injuries in children presenting to a pediatric emergency department. Ann Emerg Med. 1993 Oct;22(10):1519–23. https://doi.org/10.1016/S0196-0644(05)81251-X
4. Ljungberg E , Rosberg HE , Dahlin LB . Hand injuries in young children. J Hand Surg [Br]. 2003 Aug;28(4):376–80. https://doi.org/10.1016/S0266-7681(03)00101-3
5. Vadivelu R , Dias JJ , Burke FD , Stanton J . Hand injuries in children: a prospective study. J Pediatr Orthop. 2006 Jan-Feb;26(1):29–35. https://doi.org/10.1097/01.bpo.0000189970.37037.59
6. Davis TR , Stothard J . Why all finger fractures should be referred to a hand surgery service: a prospective study of primary management. J Hand Surg [Br]. 1990 Aug;15(3):299–302. https://doi.org/10.1016/0266-7681_90_90008-R
7. Fee C , Weber EJ , Maak CA , Bacchetti P . Effect of emergency department crowding on time to antibiotics in patients admitted with community-acquired pneumonia. Ann Emerg Med. 2007 Nov;50(5):501–9. https://doi.org/10.1016/j.annemergmed.2007.08.003
8. Hwang U , Richardson L , Livote E , Harris B , Spencer N , Sean Morrison R . Emergency department crowding and decreased quality of pain care. Acad Emerg Med. 2008 Dec;15(12):1248–55. https://doi.org/10.1111/j.1553-2712.2008.00267.x
9. MacDonald PL , Gardner RC , Type I . Error Rate Comparisons of Post Hoc Procedures for I j Chi-Square Tables. Educ Psychol Meas. 2000 Oct;60(5):735–54. https://doi.org/10.1177/00131640021970871
10. Richardson D . Progress towards reducing crowding. Am J Emerg Med. 2018 Oct;36(10):1880. https://doi.org/10.1016/j.ajem.2018.08.006
11. Pines JM , Hilton JA , Weber EJ , Alkemade AJ , Al Shabanah H , Anderson PD , et al. International perspectives on emergency department crowding. Acad Emerg Med. 2011 Dec;18(12):1358–70. https://doi.org/10.1111/j.1553-2712.2011.01235.x
12. Kraszewski S . Clinical audit in general practice. Pract Nurs. 2005;30(10):51–5.
13. Ashmore S , Ruthven T . Clinical audit: a guide. Nurs Manag (Harrow). 2008 Apr;15(1):18–22. https://doi.org/10.7748/nm2008.04.15.1.18.c6489
14. Löflath V , Hau E-M , Garcia D , Berger S , Löllgen R . Parental satisfaction with waiting time in a Swiss tertiary paediatric emergency department. Emerg Med J. 21. Dezember 2020;emermed-2019-208616.
15. Rosberg HE , Carlsson KS , Dahlin LB . Prospective study of patients with injuries to the hand and forearm: costs, function, and general health. Scand J Plast Reconstr Surg Hand Surg. 2005;39(6):360–9. https://doi.org/10.1080/02844310500340046
16. Eitel DR , Rudkin SE , Malvehy MA , Killeen JP , Pines JM . Improving service quality by understanding emergency department flow: a White Paper and position statement prepared for the American Academy of Emergency Medicine. J Emerg Med. 2010 Jan;38(1):70–9. https://doi.org/10.1016/j.jemermed.2008.03.038