
Figure 1 QR code at the vaccination centre Winterthur (Source: Impfzentrum Winterthur, 2021).
DOI: https://doi.org/10.4414/SMW.2022.w30156
Herd immunity for COVID-19 is critical to get the pandemic under control [1]. Like adults, children and adolescents infected with COVID-19 can transmit the virus to others [2, 3]. There is an ongoing public and scientific debate on the need for and relevance of vaccinating children, while vaccination of adolescents is strongly recommended and generally accepted. Although the disease burden in children and adolescents has been reasonably mild [4], COVID-19 vaccines can prevent them from becoming seriously ill (e.g., multisystem inflammatory syndrome in children) [5]. Evidence also indicates that long COVID occurs in children and adolescents [6–8] and that vaccination should protect against long COVID in this age group [9].
In Switzerland, COVID-19 vaccines have been authorised for young people aged 12 years and older since 4 June 2021 [10, 11], and only recently in December 2021 were vaccines approved for 5–11-year-olds [12]. The COVID-19 vaccination is recommended for children and adolescents to protect them from frequent mild and very rare severe cases of COVID-19. This applies especially to children and adolescents with a chronic illness and who are in close contact with people at high risk, such as people with a weakened immune system [10]. In addition, increasing the general vaccination coverage will reduce infection risk and cases overall. Protecting others, avoidance of negative effects of measures (e.g., isolation, quarantine), and regaining mobility and access to free-time activities are additional motives for adolescents and young people, especially [13, 14].
Nevertheless, vaccine hesitancy forms a critical barrier to the uptake of the COVID-19 vaccine. The reasons why people do not get vaccinated are often complex. Regarding COVID-19 vaccines, the novelty of the vaccines and the use of new technologies such as messenger RNA are major contributors to public uncertainty and scepticism. In general, psychological factors and traits are decisive for individuals' opinion on vaccinations. For example, the 5C model, which comprises several psychological theories for predicting preventive behaviour and is based on established theoretical models of vaccine hesitancy and acceptance, includes five psychological antecedents of vaccination: first, confidence, defined as trust in safety and effectiveness of vaccines and the system that delivers them; second, complacency, which reflects the perceived risks of vaccine-preventable diseases; third, constraints, which refers to perceived structural or psychological barriers to vaccination; fourth, calculation, which relates to weighing the risks and benefits of vaccination and individuals’ engagement in extensive information seeking about vaccination; and finally, collective responsibility, which reflects the willingness to protect others by one’s own behaviour [15].
Concerning routine vaccinations for children, parental attitudes and beliefs are strongly associated with vaccination intention [1, 16]. In general, positive attitudes towards vaccination are associated with the decision to vaccinate [17]. This applies also to COVID-19 vaccines. Studies show that the most important psychological drivers of parental COVID-19 vaccination intention are beliefs that vaccination against COVID-19 is necessary [18–20] (complacency), confidence in the safety of the vaccine [18–20], and trust in public health authorities and health sciences [19]. Furthermore, several studies found that parents’ COVID-19 vaccination or likelihood of vaccination was the most important factor independently associated with the likelihood of children getting the vaccine [18, 20–22]. Other influencing factors are parental vaccination history [2, 23], sex [2, 21, 24] and education level [23] as well as characteristics of the child such as age [2, 22], presence of a chronic illness [2], and status of the childhood vaccination schedule [22]. Particularly with regard to gender, findings are consistent, highlighting a major gap between mothers and fathers, with mothers being more vaccine hesitant than fathers [2, 21, 24].
In Switzerland, little is known about parents’ intentions to have their child vaccinated against COVID-19 and associated factors. Therefore, this study investigated the association between the psychological antecedents of standard vaccinations, measured with the 5C scale [15], in parents who received the COVID-19 vaccination themselves and their intention to have their child vaccinated against COVID-19, once available. Further, we wished to understand how previous parental vaccination history and the conviction of the benefits of the Swiss vaccination recommendations for children and adolescents are associated with the child vaccination intention, and where and by whom parents would like to have the COVID-19 vaccination to be performed.
We conducted a cross-sectional study at the COVID-19 vaccination centre Winterthur, Switzerland.
The COVID-19 vaccination centre Winterthur provides COVID-19 vaccination services for the residents of the city of Winterthur and the surrounding area with the capability to administer over 5000 vaccinations per day. The study was in accordance with the Declaration of Helsinki and was submitted to the Cantonal Ethics Committee of the Canton of Zurich, Switzerland. The study does not fall under the Human Research Act and an exemption of an ethical review was received (BASEC-Nr. Req-2021-00347). This manuscript was prepared in compliance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist [25].
The study population corresponded to a self-selected sample of individuals vaccinated against COVID-19 at the vaccination centre Winterthur between 13 April and 30 September 2021. All individuals at the vaccination centre had access to a flyer with information about the study and a web link / QR code to access the survey. Further, a QR code on the floor in front of the seats in the waiting area led to the online landing page with main study information and online consent as well as the online questionnaire (fig. 1).

Figure 1 QR code at the vaccination centre Winterthur (Source: Impfzentrum Winterthur, 2021).
For this analysis, we included survey participants having received the first dose of the vaccine between 16 May and 30 September 2021, and who had children under 16 years. We did not foresee the inclusion of respondents after the second dose of vaccine; firstly, we assumed the intention would not change in such a short interval (4 weeks), and secondly, the anonymity of the data did not allow a linkage of individual data sets. Respondents answering the questionnaire before 16 May 2021 were excluded because the question regarding children’s age was added to the questionnaire on that date.
The questionnaire included sociodemographic factors, vaccination history (parents and children), psychological antecedents of vaccination (5C scale: confidence, constraints, complacency, calculation and collective responsibility), motifs for COVID-19 vaccination, service experience in the vaccination centre (infrastructure of the vaccination centre, process of vaccination, satisfaction with staff), side effects of the COVID-19 vaccination (first and second dose), preferred vaccination location (parents and children), parental COVID-19 vaccination intention, self-rated health status, previous COVID-19 infection and stress factors caused by the pandemic(containment measures, contracting COVID-19, COVID-19 infection, COVID-19 testing). Participants had to actively provide their consent online before accessing the online questionnaire. The anonymity of participants was always guaranteed.
The primary outcome variable was parents’ intention to vaccinate their child against COVID-19, which was measured with a single item, used in the HES-C study [26] and the Swiss National Corona Immunitas Study [15] to measure vaccination intention in students and the general population, respectively. Respondents were asked the following: “Once the COVID-19 vaccine is approved for adolescents/children, will you get your child/children vaccinated?”, using a 6-point Likert scale (1 = no, 2 = probably no, 3 = undecided, 4 = yes, after others, 5 = probably yes, 6 = yes). For the analysis, the responses were recoded into binary categories 0 = low vaccination intention (“no”, “probably no”, and “undecided”) and 1 = strong vaccination intention (“yes”, “probably yes”, “yes, after others”). A secondary outcome was the location in which parents preferred to have their child vaccinated, should vaccination against COVID-19 become necessary in the future.
Parental psychological antecedents of standard vaccination were measured using the validated 5C scale [15]. The 5C scale is a self-assessment questionnaire that measures five different antecedents of vaccine hesitancy: (1) confidence (trust in the effectiveness and safety of vaccines and in the providers/system), (2) complacency (perceived disease risk), (3) constraints (perceived structural or psychological barriers to vaccination), (4) calculation (risk-benefit calculation), and (5) collective responsibility (willingness to benefit others by receiving vaccination). The questionnaire comprised 15 items to be rated on a 5-point Likert scale (from “strongly disagree” to “strongly agree”). Scores on each sub-scale represent the mean scores of the scale’s items and range from 1 to 5, with higher values representing more agreement with the antecedent, e.g., more confidence or more perceived constraints.
Previous parental vaccination history was assessed for influenza vaccination (0 = no, 1 = yes) and for travel vaccinations as a medical precaution (0 = no, 1 = yes). Participants were also asked to indicate on a 10-point scale the extent to which they were convinced of the benefits of the Swiss vaccination recommendations for children and adolescents.
Parental sociodemographic covariates included age, sex (0 = women, 1 = men) and highest education level (0 = low: no educational qualification, compulsory schooling, apprenticeship; 1 = middle: grammar school, professional maturity, higher technical and vocational training; 3 = high: university, university of applied sciences, ETH). Data on children were restricted to the age range of the oldest child under 16 years (0 = 0–5 years, 1 = 6–11 years, 2 = 12–15 years). Since COVID-19 vaccines were approved for adolescents aged 12 years and older on 4 June 2021 [11], we controlled for time of authorisation (0 = before vaccine authorisation, 1 = after vaccine authorisation).
The analytic sample consisted of complete cases only. We used the Stata mdesc and mvpatterns commands to assess incomplete cases. We detected no systematic patterns in the missing data. Missing values of individual variables were in the range between 0% and 0.82%. Descriptive statistics were run concerning the sample characteristics, and univariate t-tests and chi-square tests were used to assess univariate group differences by gender and vaccination intention (supplemental table S1 in the appendix).
Multivariable logistic regression models were applied to estimate the association between psychological antecedents (5C scale: confidence, complacency, constraints, calculation, collective responsibility) and parental COVID-19 vaccination intention regarding their child. In a first model, we included the 5C vaccination antecedents. Further models were adjusted for vaccination history (travel vaccination and influenza vaccination), the conviction of the benefits of the Swiss vaccination recommendations for children and adolescents (model 2), and age, sex, education level, children age group, and time of vaccine authorisation (model 3, full model). We report adjusted odds ratios (AORs) with corresponding 95% confidence intervals (95% CIs) for the single components of the 5C scale and the model covariates. Statistical significance was established at p <0.05. We used Stata version 15.1 (StataCorp, College Station, TX, USA) for statistical analyses.
In total, 6500 people completed the survey after the first dose of COVID-19 vaccination, of whom 1604 (24.7%) had a child under 16 years of age. A total of 257 parents were excluded because they answered the questionnaire before 16 May 2021 and therefore had missing values for the variable children’s age. This left 1347 (20.7%) parents who fulfilled the inclusion criteria. Information on parental COVID-19 vaccination intention, our primary outcome, was provided by 1344 respondents (99.8%) and complete data for all variables used in our model were available for 1318 respondents (97.9%).
The analytic sample of 1318 parents consisted of 590 mothers (44.8%) and 728 fathers (55.2%) (table 1). The mean age of the parents was 41 years (standard deviation [SD] 6.5). The mean ages for mothers and fathers differed significantly (p = 0.004) and were 41 years (SD 6.4) and 42 years (SD 6.5), respectively. Regarding the psychological antecedents of vaccination (5C scale), compared with fathers, mothers expressed significantly higher levels of collective responsibility (p <0.001) and significantly lower complacency (p = 0.015). Overall, 36.2% of the parents had been vaccinated in the past against seasonal influenza and 60.5% reported a previous travel vaccination. The conviction of the benefits of the Swiss vaccination recommendations for children and adolescents was generally high among the parents with a mean value of 7.9 on a 10-point scale (SD 2.2). Mothers’ conviction was slightly higher than fathers’ (8.0 vs. 7.8, p = 0.065). In 26.6% of the participants, the oldest child under 16 years was between 12 and 15 years old, in 35.3% between 6 and 11 years old, and in 38.1% between 0 and 5 years old. Three-fifths of the parents reported a high education level. There was a significant difference regarding the education level (p <0.001) between the genders.
Table 1Characteristics of the study population (n = 1318).
Data are n (%) unless otherwise stated. n: number of observations
a Strong vaccination intention: Yes = combined categories "Yes, after others", "Probably yes", "Yes"; No = combined categories "Undecided", "Probably no", "No"
b 5C vaccination antecedents: scale from 1 = strongly disagree to 5 = strongly agree
c Conviction of the benefits of the Swiss vaccination recommendation for children and adolescents: scale from 1 = not convinced at all to 10 = very convinced
d COVID-19 vaccines for children aged ≥ 12 years were approved in Switzerland on 4 June 2021
Overall, 58.7% of the parents expressed an intention to have their child vaccinated against COVID-19 (“yes”, “probably yes”, “yes after others”). Vaccination intention was significantly lower in mothers than fathers (p = 0.011) (table 1). 17.4% of the parents indicated that they would have their child vaccinated against COVID-19 (“yes”), and 4.1% responded they would not have their child vaccinated (“no”); 78.4% were not absolutely sure (“probably yes” 32.2%, “probably no” 16.7%), undecided (20.5%), or wished to wait for others to vaccinate their children first (9.0%).
Parental vaccination intention differed significantly by child age group (fig. 2). The vaccination intention of parents with older children was significantly higher than those of parents with younger children (“strong vaccination intention” 12–15 years = 72.0%, 6–11 years = 55.9%; 0–5 years = 52.1%; p <0.001).

Figure 2 Parental COVID-19 vaccination intention, by child age group (in %); n = 1318
Among parents willing to have their child vaccinated against COVID-19 (“yes”, “probably yes”, “yes after others”), 70.3% would, in future, prefer to have their child vaccinated at their paediatrician or family doctor practice, 25.6% at a COVID-19 vaccination centre and 4.2% at a pharmacy (fig. 3). No significant difference was found by parental gender. Parents of children aged 12–15 years showed a higher preference to vaccinate their child in a vaccination centre than parents of children aged 0–5 and 6–11 years (p <0.001).
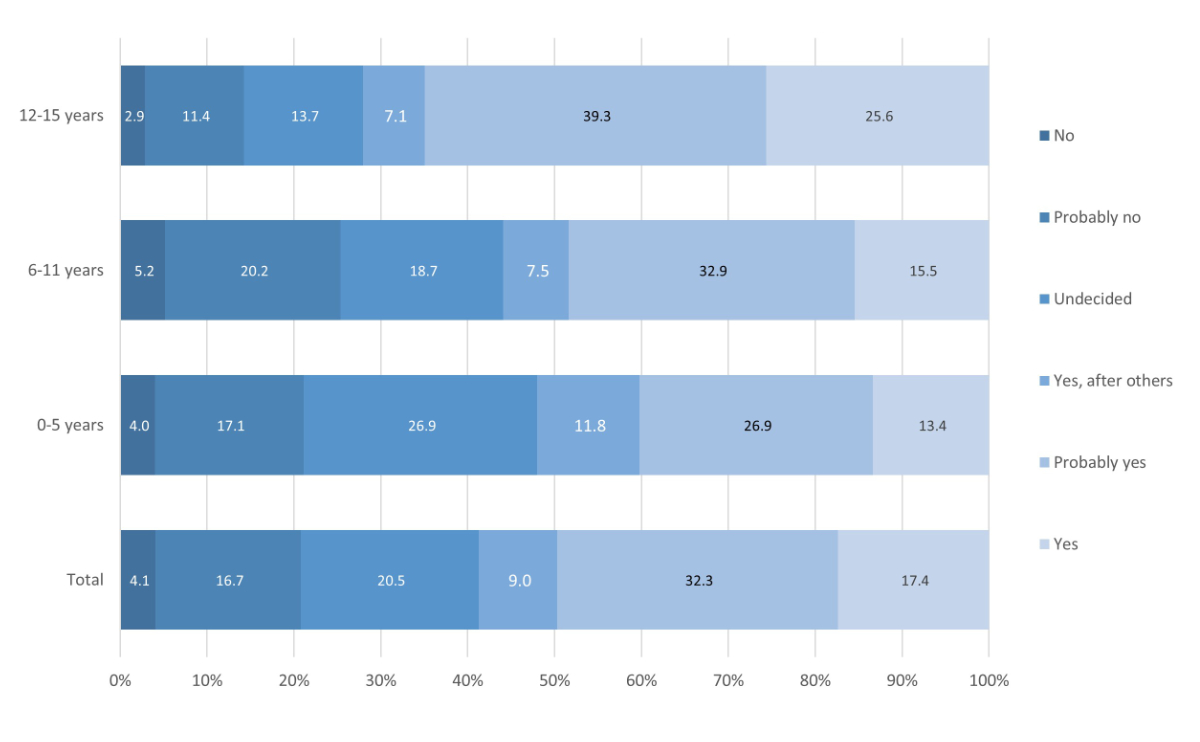
Figure 3 Parental preferred COVID-19 vaccination location for their child, by child age group (in %); n = 771.
The multivariable logistic regression (table 2) yielded significant associations with the 5C vaccination antecedents both in the unadjusted and adjusted models. In the unadjusted model (model 1), four of the 5C dimensions were significantly associated with vaccination intention. Adjusting for previous influenza and travel vaccination (model 2) led to an attenuation of the effect and the significance level of the 5C domains, but remained statistically significant. In the fully adjusted model (model 3), confidence turned borderline significant. Parents who expressed more confidence in vaccinations were more likely to be willing to vaccinate their child against COVID-19 (OR 1.33, 95% CI 1.00–1.76). Collective responsibility and calculation showed no change in effect size or significance level in the fully adjusted model. Collective responsibility, i.e., willingness to protect others, remained significantly associated with vaccination intention (OR 1.93, 95% CI 1.47–2.52), whereas calculation, i.e., risk-benefit calculation, was associated with lower vaccination intention (OR 0.68, 95% CI 0.58–0.81).
Table 2Parental COVID-19 vaccination intention for children: logistic regression models.
| Variable | Model 1 | Model 2 | Model 3 | |||
| AOR | 95% CI | AOR | 95% CI | AOR | 95% CI | |
| 5C vaccination antecedents | ||||||
| – Confidence | 2.29*** | 1.80–2.91 | 1.41* | 1.081.85 | 1.33† | 1.001.76 |
| – Complacency | 0.76** | 0.620.93 | 0.94 | 0.751.17 | 0.93 | 0.741.17 |
| – Constraints | 0.99 | 0.811.22 | 1.00 | 0.811.24 | 1.01 | 0.811.27 |
| – Calculation | 0.75*** | 0.650.87 | 0.78** | 0.670.91 | 0.68*** | 0.580.81 |
| – Collective responsibility | 1.96*** | 1.542.49 | 1.79*** | 1.402.29 | 1.93*** | 1.472.52 |
| Influenza vaccination (ref = No) | ||||||
| – Yes | 1.32* | 1.011.72 | 1.53** | 1.152.03 | ||
| Travel vaccination (ref = No | ||||||
| – Yes | 1.09 | 0.841.41 | 1.05 | 0.801.39 | ||
| Conviction of the benefits of the vaccination recommendation | 1.39*** | 1.301.50 | 1.40*** | 1.291.51 | ||
| Age (years) | 1.04** | [1.011.07 | ||||
| Sex (ref = Women) | ||||||
| – Men | 1.66*** | 1.262.18 | ||||
| Education level (ref = Low) | ||||||
| – Middle | 1.14 | 0.741.76 | ||||
| – High | 1.44† | 0.972.14 | ||||
| Age oldest child under 16 years (ref = 0–5 years) | ||||||
| – 6–11 years | 1.14 | 0.811.60 | ||||
| – 12–15 years | 2.93*** | 1.844.67 | ||||
| Time of vaccine authorisation (ref = Before authorization) | ||||||
| – After authorisation | 0.63** | 0.480.83 | ||||
| Number of observations | 1344 | 1340 | 1318 | |||
| P-value (chi-square) | <0.001 | <0.001 | <0.001 | |||
ref = reference category; AOR = adjusted odds ratio; 95% CI = 95% confidence interval; † p <0.1, * p <0.05, ** p <0.01, *** p <0.001
Furthermore, in the full model (model 3) parental COVID-19 vaccination intention was positively associated with parents’ previous influenza vaccination (OR 1.53, 95% CI 1.15–2.03), but not with travel vaccination, and with a higher conviction of the benefits of the Swiss vaccination recommendations for children and adolescents (OR 1.40, 95% CI 1.29–1.51).
Vaccination intention was higher among parents whose oldest child was between 12 and 15 years old (OR 2.93, 95% CI 1.84–4.67), fathers (OR 1.66, 95% CI 1.26–2.18), older parents (OR 1.04, 95% 1.01–1.07). Educational level was not statistically significant. Among parents who participated after the authorisation of the vaccine for children aged 12 years and older, vaccination intention was lower than in parents responding before this date (OR 0.63, 95% CI 0.48–0.83).
In a sample of Swiss German-speaking parents who got vaccinated themselves against COVID-19, we found a relatively high level of parental intention to vaccinate their child against COVID-19. Overall, 58.7% of the parents reported the intention to have their child vaccinated against COVID-19 once the vaccine was available. Calculation and collective responsibility proved to be the strongest psychological antecedents associated with the vaccination intention.
To our knowledge, this is the first Swiss study on child vaccination intention in parents not opposed to COVID-19 vaccination as such. Most studies on parental vaccination intention in the general public showed a similar result to ours. Humble et al. [18] found that 63.1% of Canadian parents intended to vaccinate their child against COVID-19 and Altenbuchner et al. [24] reported 52.3 % for German parents. Skjefte et al. [19] observed the highest rate of vaccination intention (69.2%) in an international study for young mothers from 16 different countries. Our finding might overestimate the vaccination intention of parents in Switzerland, as the parental COVID-19 vaccination intention could be higher in vaccinated parents than in the non-vaccinated population. In fact, previous studies showed that the vaccination status of parents is a main predictor of the intention to vaccinate their child [18, 20–22]. Current vaccination rates indicate a lower vaccination rate of 44% in 12–15-year-olds and 3% in 5–11-year-olds than these early intention data suggested [27]. Our study found that 72% of parents of 12–15-year-olds and 55.9% of parents of 6–11-year-olds would have their child vaccinated, but these data stem from a population of vaccinated parents. In addition, the late authorisation of the vaccine for children aged 5–11 years (December 2021) and high COVID-19 cases in children may contribute to the current low vaccination rate.
Regarding the psychological antecedents (5C scale), we found a positive association of the dimensions confidence and collective responsibility, and a negative association with the dimension calculation. However, no significant association was found for complacency and constraints.
The dimension confidence was asked in the context of general vaccinations recommended for adults, and measures trust in the effectiveness and safety of vaccinations as well as in the system that delivers them. It seems intuitive that such trust would increase vaccination willingness, and our data imply that confidence in vaccinations for oneself is associated with trust in child vaccinations. After the variable “conviction of the benefits of the vaccination recommendations for children and adolescents”, the dimension confidence was attenuated in strength and significance level. The parental conviction of the benefits of the vaccination recommendations was associated with 40% higher odds of vaccinating one’s child. This indicates that the trust in the vaccination recommendations is of higher relevance than the psychological antecedent confidence.
It seems that the aspect of collective responsibility is crucial regarding the intention not only to vaccinate oneself but also to vaccinate children [28–32]. This interpretation is affirmed by the association found between parents’ past influenza vaccination and vaccination intention, whereas travel vaccination was not positively associated with child vaccination intention. Indeed, travel vaccinations are mainly for self-protection, while the influenza vaccination has both aspects, personal and collective gain.
With respect to the dimension calculation, high scores were associated with 30% lower odds of child vaccination. Understandably, parents might carefully weigh the benefits and risks regarding their child, as children were reported to be at little risk for severe COVID-19 infections and little information on child vaccinations was available at the time of the study. The more information a person seeks in order to weigh the risks and benefits of vaccination, the higher the likelihood of encountering vaccine-critical information [15].
These findings emphasise that it is important to address the dimension of calculation when developing public health campaigns fostering COVID-19 vaccination for children from different angles and for different sub-groups. The parents indicating strong vaccination intentions (so-called innovators) should be reinforced in their conclusion, whereas the parents waiting for others to vaccinate their child first or who are yet undecided may react to positive experiences of the innovators in their decision-making process [33, 34]. Lastly, the ones who are against might need facts and figures, and background information to build trust in the recommendations.
Looking further into the covariates included in the full model (model 3), we found that being a father yields a significantly higher vaccination intention than being a mother. This is in line with results from Teasdale et al. [35], indicating that mothers were less likely to report plans to vaccinate their child against COVID-19. According to Bono et al. [36], women more often fear side effects and believe that the COVID-19 vaccine was designed to harm them or that the vaccine is not effective. These concerns may explain why women also tend to be more hesitant than men to get vaccinated against COVID-19 [28, 37–40].
A higher education level was positively associated with parental COVID-19 vaccination intention. A systematic review by Robinson et al. [41] indicated that generally, persons with a low education level are less likely to vaccinate against COVID-19. For parents with low education, some studies regarding childhood vaccinations (e.g., routine childhood, or influenza vaccinations) also showed a higher hesitancy than parents with high education level [42, 43]. Nevertheless, Hudson and Motelpare [44] stressed that vaccine hesitancy is an issue across all social classes and vaccine campaigns should not be reduced to focus on lower socioeconomic status.
Our study showed that parents whose oldest child was between 12 and 15 years old have higher COVID-19 vaccination intention than parents with younger children. Parents whose child was over 11 years old had three-fold higher odds of intending to vaccinate their child. Our results must be viewed against the background of the absence of authorisation of the vaccine for children under 12 years at the time of the data collection in Switzerland and the limited availability of clinical study data for younger children. Similar findings were reported by Temsah et al. [45] as well as Teasdale et al. [35] and support our interpretation.
The COVID-19 vaccine was approved for 12-year-olds and older during the study in June 2021. We could thus investigate the impact of the authorisation on a change in intention. We found that parental COVID-19 vaccination intention decreased after the vaccine was approved for adolescents. This is contradictory to the hypothesis that the authorisation of the vaccine has a decisive role in vaccination intention. On the other hand, as time passed, people who attended the vaccination centre probably were different in their beliefs and attitudes toward the COVID-19 vaccination. The social pressure to get vaccinated against COVID-19 increased in the second half of 2021 [46] and as more restrictions came into force and the COVID certificate was introduced [47], people might have felt more inclined to be vaccinated for reasons other than collective responsibility or calculation.
Our study participation rate was rather low, which can be explained by the recruiting method. The population invited to the vaccination centre was not informed about the study prior to their visit, nor were the individuals addressed directly at the centre. The QR code to the online link was placed on the floor in front of the seats and participants could find a leaflet next to the complimentary water bottles in the waiting zone. This cautious approach was taken to avoid any additional uncertainty regarding the vaccination at the centre. Therefore, our data are based on a self-selected sample, which limits the generalisability of our research findings. Since participants did not know we would also ask about child vaccinations, we see no major selection bias regarding parents’ participation. Our 5C results show a variance, implying both vaccination hesitant and less hesitant parents participated in the study.
Our results imply that collective responsibility and calculation are strong drivers for parental vaccination intention. Campaigns on COVID-19 vaccination for children may reach parents better when addressing these psychological antecedents. Campaigns should also consider mothers as a specific target group because of their increased hesitancy. Strengthening confidence in official paediatric vaccination recommendations will increase compliance with recommendations in general, and is also predictive of a higher parental intention to vaccinate their child against COVID-19. Further, taking parental views on the setting for vaccination, paediatrician / family doctor practice or vaccination centres, into account may also have an effect on future parental vaccination willingness.
We would like to thank the parents who participated in this study. Furthermore, we thank Thomas Kraft, Kate Schmitt, and Hanni Wipf Stengele, and the employees of the vaccination centre Winterthur for their support and the opportunity to conduct this study at the center.
There was no specific funding for this project.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Wang Q , Xiu S , Zhao S , Wang J , Han Y , Dong S , et al. Vaccine Hesitancy: COVID-19 and Influenza Vaccine Willingness among Parents in Wuxi, China-A Cross-Sectional Study. Vaccines (Basel). 2021 Apr;9(4):342. https://doi.org/10.3390/vaccines9040342
2. Goldman RD , Yan TD , Seiler M , Parra Cotanda C , Brown JC , Klein EJ , et al.; International COVID-19 Parental Attitude Study (COVIPAS) Group . Caregiver willingness to vaccinate their children against COVID-19: cross sectional survey. Vaccine. 2020 Nov;38(48):7668–73. https://doi.org/10.1016/j.vaccine.2020.09.084
3. Wiedenmann M , Goutaki M , Keiser O , Stringhini S , Tanner M , Low N . The role of children and adolescents in the SARS-CoV-2 pandemic: a rapid review. Swiss Medical Weekly. 2021 Sep 17;(37).
4. Obaro S . COVID-19 herd immunity by immunisation: are children in the herd? Lancet Infect Dis. 2021 Jun;21(6):758–9. https://doi.org/10.1016/S1473-3099(21)00212-7
5. Feldstein LR , Rose EB , Horwitz SM , Collins JP , Newhams MM , Son MB , et al.; Overcoming COVID-19 Investigators; CDC COVID-19 Response Team . Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N Engl J Med. 2020 Jul;383(4):334–46. https://doi.org/10.1056/NEJMoa2021680
6. Buonsenso D , Munblit D , De Rose C , Sinatti D , Ricchiuto A , Carfi A , et al. Preliminary evidence on long COVID in children. Acta Paediatr. 2021 Jul;110(7):2208–11. https://doi.org/10.1111/apa.15870
7. Asadi-Pooya AA , Nemati H , Shahisavandi M , Akbari A , Emami A , Lotfi M , et al. Long COVID in children and adolescents. World J Pediatr. 2021 Oct;17(5):495–9. https://doi.org/10.1007/s12519-021-00457-6
8. Brackel CL , Lap CR , Buddingh EP , van Houten MA , van der Sande LJ , Langereis EJ , et al. Pediatric long-COVID: an overlooked phenomenon? Pediatr Pulmonol. 2021 Aug;56(8):2495–502. https://doi.org/10.1002/ppul.25521
9. Schleiss MR , John CC , Permar SR . Children are the key to the Endgame: A case for routine pediatric COVID vaccination. Vaccine. 2021 Sep;39(38):5333–6. https://doi.org/10.1016/j.vaccine.2021.08.005
10. Federal Office of Public Health FOPH . Coronavirus: Vaccination [Internet]. bag.admin.ch. 2021 [cited 2021 Jul 5]. Available from: https://www.bag.admin.ch/bag/en/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/impfen.html
11. Swissmedic. Covid-19 Impfstoff von Pfizer/BioNTech in der Schweiz für Jugendliche freigegeben [Internet]. www.swissmedic.ch. 2021 [cited 2021 Oct 29]. Available from: https://www.swissmedic.ch/swissmedic/de/home/news/coronavirus-covid-19/covid-19-impfstoff-pfizer-biontech-fuer-jugendliche.html
12. Swissmedic. Swissmedic genehmigt Covid-19 Impfstoff von Pfizer/BioNTech für Kinder von 5 bis 11 Jahren [Internet]. www.swissmedic.ch. 2021 [cited 2021 Dec 15]. Available from: https://www.swissmedic.ch/swissmedic/de/home/news/coronavirus-covid-19/covid-19-impfstoff-pfizer-biontec-kinder-5-11-jahren-genehmigt.html
13. Nilsson S , Mattson J , Berghammer M , Brorsson AL , Forsner M , Jenholt Nolbris M , et al. To be or not to be vaccinated against COVID-19 - The adolescents’ perspective - A mixed-methods study in Sweden. Vaccine X. 2021 Dec;9:100117. https://doi.org/10.1016/j.jvacx.2021.100117
14. Hermann M. Spezialauswertung COVID-19-Impfung: Informationsstand, Einstellungen und Verhalten. Auszug aus der periodischen Wirkungsmessung März 2021 im Auftrag des Bundesamts für Gesundheit BAG. Bern: Forschungsstelle sotomo; 2021.
15. Betsch C , Schmid P , Heinemeier D , Korn L , Holtmann C , Böhm R . Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS One. 2018 Dec;13(12):e0208601. https://doi.org/10.1371/journal.pone.0208601
16. Shapiro GK , Kaufman J , Brewer NT , Wiley K , Menning L , Leask J , et al.; BeSD Working Group . A critical review of measures of childhood vaccine confidence. Curr Opin Immunol. 2021 Aug;71:34–45. https://doi.org/10.1016/j.coi.2021.04.002
17. Waller J , Forster A , Ryan M , Richards R , Bedford H , Marlow L . Decision-making about HPV vaccination in parents of boys and girls: A population-based survey in England and Wales. Vaccine. 2020 Jan;38(5):1040–7. https://doi.org/10.1016/j.vaccine.2019.11.046
18. Humble RM , Sell H , Dubé E , MacDonald NE , Robinson J , Driedger SM , et al. Canadian parents’ perceptions of COVID-19 vaccination and intention to vaccinate their children: results from a cross-sectional national survey. Vaccine. 2021 Dec;39(52):7669–76. https://doi.org/10.1016/j.vaccine.2021.10.002
19. Skjefte M , Ngirbabul M , Akeju O , Escudero D , Hernandez-Diaz S , Wyszynski DF , et al. COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries. Eur J Epidemiol. 2021 Feb;36(2):197–211. https://doi.org/10.1007/s10654-021-00728-6
20. Choi SH , Jo YH , Jo KJ , Park SE . Pediatric and Parents’ Attitudes Towards COVID-19 Vaccines and Intention to Vaccinate for Children. J Korean Med Sci. 2021 Aug;36(31):e227. https://doi.org/10.3346/jkms.2021.36.e227
21. Zhang MX , Lin XQ , Chen Y , Tung TH , Zhu JS . Determinants of parental hesitancy to vaccinate their children against COVID-19 in China. Expert Rev Vaccines. 2021 Oct;20(10):1339–49. https://doi.org/10.1080/14760584.2021.1967147
22. Szilagyi PG , Shah MD , Delgado JR , Thomas K , Vizueta N , Cui Y , et al. Parents’ Intentions and Perceptions About COVID-19 Vaccination for Their Children: Results From a National Survey. Pediatrics. 2021 Oct;148(4):e2021052335. https://doi.org/10.1542/peds.2021-052335
23. Hetherington E , Edwards SA , MacDonald SE , Racine N , Madigan S , McDonald S , et al. SARS-CoV-2 vaccination intentions among mothers of children aged 9 to 12 years: a survey of the All Our Families cohort. CMAJ Open. 2021 May;9(2):E548–55. https://doi.org/10.9778/cmajo.20200302
24. Altenbuchner A , Haug S , Schnell R , Scharf A , Weber K . Impfbereitschaft von Eltern mit einem COVID-19-Vakzin: Die Rolle von Elternschaft und Geschlecht. Padiatr Padol. 2021 Oct;56(5):230–4. https://doi.org/10.1007/s00608-021-00925-2
25. von Elm E , Altman DG , Egger M , Pocock SJ , Gøtzsche PC , Vandenbroucke JP ; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008 Apr;61(4):344–9. https://doi.org/10.1016/j.jclinepi.2007.11.008
26. Studie zur Gesundheit von Studierenden in Zeiten der Corona-Pandemie . [Internet]. ZHAW Gesundheit. [cited 2021 Aug 19]. Available from: https://www.zhaw.ch/de/gesundheit/forschung/gesundheitswissenschaften/projekte/studierendengesundheit/
27. Federal Office of Public Health FOPH . COVID-19 Switzerland | Coronavirus | Dashboard [Internet]. www.covid19.admin.ch. [cited 2022 Feb 14]. Available from: https://www.covid19.admin.ch/en/vaccination/persons?geoAge=A_5_11
28. Dratva J , Wagner A , Zysset A , Volken T . To Vaccinate or Not to Vaccinate-This Is the Question among Swiss University Students. Int J Environ Res Public Health. 2021 Aug;18(17):9210. https://doi.org/10.3390/ijerph18179210
29. Al-Sanafi M , Sallam M . Psychological Determinants of COVID-19 Vaccine Acceptance among Healthcare Workers in Kuwait: A Cross-Sectional Study Using the 5C and Vaccine Conspiracy Beliefs Scales. Vaccines (Basel). 2021 Jun;9(7):701. https://doi.org/10.3390/vaccines9070701
30. Kwok KO , Li KK , Wei WI , Tang A , Wong SY , Lee SS . Editor’s Choice: Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: A survey. Int J Nurs Stud. 2021 Feb;114:103854. https://doi.org/10.1016/j.ijnurstu.2020.103854
31. Kwok KO , Li KK , Tang A , Tsoi MT , Chan EY , Tang JW , et al. Psychobehavioral Responses and Likelihood of Receiving COVID-19 Vaccines during the Pandemic, Hong Kong. Emerg Infect Dis. 2021 Jul;27(7):1802–10. https://doi.org/10.3201/eid2707.210054
32. Sherman SM , Smith LE , Sim J , Amlôt R , Cutts M , Dasch H , et al. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. Hum Vaccin Immunother. 2021 Jun;17(6):1612–21. https://doi.org/10.1080/21645515.2020.1846397
33. Mo PK , Luo S , Wang S , Zhao J , Zhang G , Li L , et al. Intention to Receive the COVID-19 Vaccination in China: Application of the Diffusion of Innovations Theory and the Moderating Role of Openness to Experience. Vaccines (Basel). 2021 Feb;9(2):129. https://doi.org/10.3390/vaccines9020129
34. Rosen B , Waitzberg R , Israeli A , Hartal M , Davidovitch N . Addressing vaccine hesitancy and access barriers to achieve persistent progress in Israel’s COVID-19 vaccination program. Isr J Health Policy Res. 2021 Aug;10(1):43. https://doi.org/10.1186/s13584-021-00481-x
35. Teasdale CA , Borrell LN , Kimball S , Rinke ML , Rane M , Fleary SA , et al. Plans to Vaccinate Children for Coronavirus Disease 2019: A Survey of United States Parents. J Pediatr. 2021 Oct;237:292–7. https://doi.org/10.1016/j.jpeds.2021.07.021
36. Bono SA , Faria de Moura Villela E , Siau CS , Chen WS , Pengpid S , Hasan MT , et al. Factors Affecting COVID-19 Vaccine Acceptance: An International Survey among Low- and Middle-Income Countries. Vaccines (Basel). 2021 May;9(5):515. https://doi.org/10.3390/vaccines9050515
37. Murphy J , Vallières F , Bentall RP , Shevlin M , McBride O , Hartman TK , et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021 Jan;12(1):29. https://doi.org/10.1038/s41467-020-20226-9
38. Thaker J . The Persistence of Vaccine Hesitancy: COVID-19 Vaccination Intention in New Zealand. J Health Commun. 2021 Feb;26(2):104–11. https://doi.org/10.1080/10810730.2021.1899346
39. Schwarzinger M , Watson V , Arwidson P , Alla F , Luchini S . COVID-19 vaccine hesitancy in a representative working-age population in France: a survey experiment based on vaccine characteristics. Lancet Public Health. 2021 Apr;6(4):e210–21. https://doi.org/10.1016/S2468-2667(21)00012-8
40. Ruiz JB , Bell RA . Predictors of intention to vaccinate against COVID-19: results of a nationwide survey. Vaccine. 2021 Feb;39(7):1080–6. https://doi.org/10.1016/j.vaccine.2021.01.010
41. Robinson E , Jones A , Lesser I , Daly M . International estimates of intended uptake and refusal of COVID-19 vaccines: A rapid systematic review and meta-analysis of large nationally representative samples. Vaccine. 2021 Apr;39(15):2024–34. https://doi.org/10.1016/j.vaccine.2021.02.005
42. Kempe A , Saville AW , Albertin C , Zimet G , Breck A , Helmkamp L , et al. Parental Hesitancy About Routine Childhood and Influenza Vaccinations: A National Survey. Pediatrics. 2020 Jul;146(1):e20193852. https://doi.org/10.1542/peds.2019-3852
43. Rammohan A , Awofeso N , Fernandez RC . Paternal education status significantly influences infants’ measles vaccination uptake, independent of maternal education status. BMC Public Health. 2012 May;12(1):336. https://doi.org/10.1186/1471-2458-12-336
44. Hudson A , Montelpare WJ . Predictors of Vaccine Hesitancy: Implications for COVID-19 Public Health Messaging. Int J Environ Res Public Health. 2021 Jul;18(15):8054. https://doi.org/10.3390/ijerph18158054
45. Temsah MH , Alhuzaimi AN , Aljamaan F , Bahkali F , Al-Eyadhy A , Alrabiaah A , et al. Parental Attitudes and Hesitancy About COVID-19 vs. Routine Childhood Vaccinations: A National Survey. Front Public Health. 2021 Oct;9:752323. https://doi.org/10.3389/fpubh.2021.752323
46. Begleitstudie COVID-Impfzentrum Winterthur [Internet]. ZHAW Gesundheit. [cited 2021 Nov 5]. Available from: https://www.zhaw.ch/de/gesundheit/forschung/gesundheitswissenschaften/projekte/begleitstudie-covid-impfzentrum-winterthur/
47. Bundesamt für Gesundheit BAG. Coronavirus: Massnahmen und Verordnungen [Internet]. bag.admin.ch. [cited 2021 Nov 5]. Available from: https://www.bag.admin.ch/bag/de/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/massnahmen-des-bundes.html
Table S1Characteristics of the study population (n = 1318).
| (Strong) vaccination intention a | ||||
| Total n (%) | No n (%) | Yes n (%) | p-value | |
| Total | 1318 (100.0) | 544 (41.3) | 774 (58.7) | |
| Vaccination intention | ||||
| – No | 54 (4.1) | - | - | |
| – Probably no | 220 (16.7) | - | - | |
| – Undecided | 270 (20.5) | - | - | |
| – Yes, after others | 119 (9.0) | - | - | |
| – Probably yes | 426 (32.2) | - | - | |
| – Yes | 229 (17.4) | - | - | |
| 5C vaccination antecedents (mean) b | ||||
| – Confidence | 4.43 | 4.19 | 4.60 | <0.001 |
| – Complacency | 1.91 | 2.11 | 1.77 | <0.001 |
| – Constraints | 1.44 | 1.45 | 1.41 | 0.014 |
| – Calculation | 3.87 | 4.04 | 3.75 | <0.001 |
| – Collective responsibility | 4.52 | 4.28 | 4.69 | <0.001 |
| Influenza vaccination | <0.001 | |||
| – No | 841 (63.8) | 391 (71.9) | 450 (58.1) | |
| – Yes | 477 (36.2) | 153 (28.1) | 324 (41.9) | |
| Travel vaccination | 0.009 | |||
| – No | 521 (39.5) | 238 (43.8) | 283 (36.6) | |
| – Yes | 797 (60.5) | 306 (56.3) | 491 (63.4) | |
| Conviction in the benefits of the vaccination recommendation (mean, SD) c | 7.9 (2.2) | 6.8 (2.4) | 8.7 (1.6) | <0.001 |
| Sex | 0.011 | |||
| – Women | 590 (44.8) | 266 (48.9) | 324 (41.9) | |
| – Men | 728 (55.2) | 278 (51.1) | 450 (58.1) | |
| Age (mean, SD) | 41 (6.5) | 39.7 (6.1) | 42.1 (6.5) | <0.001 |
| Education level | ||||
| – Low | 204 (15.5) | 111 (20.4) | 93 (12.0) | <0.001 |
| – Middle | 316 (24.0) | 152 (27.9) | 164 (21.2) | |
| – High | 798 (60.6) | 281 (51.7) | 517 (66.8) | |
| Age of oldest child under 16 years | <0.001 | |||
| – 0–5 years | 502 (38.1) | 241( 44.3) | 261 (33.7) | |
| – 6–11 years | 465 (35.3) | 205 (37.7) | 260 (33.6) | |
| – 12–15 years | 351 (26.6) | 98 (18.0) | 253 (32.7) | |
| Time of vaccine authorisation d | <0.001 | |||
| – Before authorisation | 521 (39.5) | 148 (27.2) | 373 (48.2) | |
| – After authorisation | 797 (60.5) | 396 (72.8) | 401 (51.8) | |
| Preferred vaccination location (only participants willing to vaccinate their child) | ||||
| – Vaccination centre | 197 (25.6) | - | - | |
| – Paediatrician or family doctor | 542 (70.3) | - | - | |
| – Pharmacy | 32 (4.2) | - | - | |
Data are n (%) unless otherwise stated. n: number of observations
a Strong vaccination intention: Yes = combined categories "Yes", "Yes, after others", "Probably yes"; No = combined categories "Undecided", "Probably no", "No"
b 5C vaccination antecedents: scale from 1 = strongly disagree to 5 = strongly agree
c Conviction in the benefits of the Swiss vaccination recommendation for children and adolescents: scale from 1 = not convinced at all to 10 = very convinced
d COVID-19 vaccines for children aged ≥12 years were approved in Switzerland on 4 June 2021