In-hospital cost analysis of aquablation compared with transurethral resection of the prostate in the treatment of benign prostatic enlargement
DOI: https://doi.org/10.4414/SMW.2022.w30136
Gautier
Müllhaupta, Pavel
Lyatoshinskya, Anne
Neuenschwandera, Sabine
Güsewellb, Hans-Peter
Schmida, Dominik
Abta
aDepartment of Urology, School of Medicine, University of St Gallen, Switzerland
bClinical Trials Unit, School of Medicine, University of St Gallen, Switzerland
Summary
PURPOSE: To compare in-hospital treatment costs of aquablation and transurethral resection of the prostate (TURP) in the treatment of benign prostatic enlargement.
PATIENTS AND METHODS: Patient data and procedural details were derived from a prospective database. In-hospital costs were calculated using detailed expenditure reports provided by the hospital accounts department. Total costs including those arising from surgical procedures, consumables, personnel and accommodation were analysed for 24 consecutive patients undergoing aquablation and compared with 24 patients undergoing TURP during the same period. Mean total costs and mean costs for individual expense items were compared between treatment groups with t-tests.
RESULTS: Mean total costs per patient (± standard deviation) were higher for aquablation at EUR 10,994 ± 2478 than for TURP at EUR 7445 ± 2354. The mean difference of EUR 3549 was statistically significant (p <0.001). Although the mean procedural costs were significantly higher for aquablation (mean difference EUR 3032; p <0.001), costs apart from the procedure were also lower for TURP, but the mean difference of EUR 1627 was not significant (p <0.327). Medical supplies were mainly responsible (mean difference EUR 2057; p <0.001) for the difference in procedural costs.
CONCLUSIONS: In-hospital costs are significantly higher for aquablation than for TURP, mainly due to higher costs of medical supplies for the procedure. This difference should be taken into consideration, at least in patients for whom the different side effect profiles of both treatments are irrelevant.
Abbreviations
- LUTS/BPO
-
Lower urinary tract symptoms secondary to benign prostatic obstruction
- TURP
-
Transurethral resection of the prostate
Introduction
Benign prostatic hyperplasia is one of the most common diseases in men and is often associated with bladder outlet obstruction and lower urinary tract symptoms (LUTS/BPO). Approximately 50% of men aged 50–60 years and ~90% of men aged ≥85 years are affected [1]. The estimated annual treatment costs were already USD 4 billion in the United States in 2006, and EUR 858 per patient in Europe in 2003 [2, 3]. As a result of demographic change, the costs of treating LUTS/BPO will increase significantly in the future, making treatment of LUTS/BPO a lucrative market for the industry. Therefore, the high number of novel treatment options entering the market in recent years does not seem surprising.
One of these novel treatments is aquablation [4], a technique that uses real-time ultrasound imaging combined with a robotically executed surgeon-guided high-velocity water jet to resect prostate tissue. After the first animal trial in 2015 in a canine model [5] by Faber and its first clinical application in 2016 [4], aquablation has been routinely applied in multiple urology departments worldwide and cohort studies have confirmed its clinical safety as well as its efficiency in relieving LUTS/BPO [6-9]. In addition, a randomised double-blind controlled trial (WATER study) compared aquablation with transurethral resection of the prostate (TURP) [10]. Follow-up data after 1 year [11], 2 years [12] and 3 years [13] have been released so far and efficacy outcomes after TURP and aquablation were similar with advantages for aquablation in terms of short operation time, preservation of ejaculation and short learning curve. A comparison of the costs of aquablation and TURP, which still represents a reference standard in surgical treatment of benign prostatic hyperplasia, is not yet available.
In view of the high economic burden of LUTS/BPO treatment and the considerable differences between technical aspects of aquablation and traditional transurethral surgical treatments such as TURP, cost analyses seem to be of particular interest.
As aquablation offers some obvious advantages compared with TURP, the aim of this study was to perform a comparison of in-hospital costs of both treatments in a Swiss tertiary care centre.
Patients and methods
Patient data were derived from a prospective database for the assessment of efficacy and safety of benign prostatic hyperplasia treatment registered at ClinicalTrials.gov: NCT03521648. This database, introduced in 2017, prospectively collects data of patients undergoing a variety of surgical treatments for LUTS/BPO. Clinical, patient-reported and imaging data that are assessed in clinical routine are collected from all patients providing written informed consent. Informed consent to data analysis (general informed consent) was obtained from all individual participants included in the study.
The study was performed according to the World Medical Association Declaration of Helsinki [14] and the Guidelines for Good Clinical Practice [15] and was approved by the local ethics committee (EKOS 20/042). The present analysis included the first 24 consecutive patients treated by aquablation at our department starting from September 2019. To compare costs, 24 patients treated with TURP during the same period were consecutively selected from the database; the patients had to be histologically free of prostate cancer and TURP had to be performed by a board certified surgeon.
Intervention
Aquablation is a minimally invasive surgical technology for the therapy of benign prostate enlargement first introduced by Gilling et al. [4] in 2016 using the AquaBeam® device (Procept BioRobotics, Redwood Shores, CA, USA). The AquaBeam system includes a planning unit, a robotic hand-piece and a surgeon console [16]. By means of a high-pressure saline stream, parenchymal tissue of the prostate is removed endoscopically through a heat-free mechanism called hydrodissection. The intervention is supported by live ultrasound guidance and the required depth and angle of the resection is planned out prior to the resection [16] (fig. 1). The bladder is accessed using a 24-Fr hand-piece, which accommodates the scope [5]. The handpiece is supported by an articulating arm attached to the operation table. Once placed in the optimal position, the system automatically adjusts the alignment as necessary [16].

Figure 1 Aquablation. The AquaBeam system includes a planning unit, a robotic hand-piece and a surgeon console. By means of a high-pressure saline stream, parenchymal tissue of the prostate (arrowhead) is removed (arrow) endoscopically through a heat-free mechanism called hydrodissection. The intervention is supported by live ultrasound guidance and the required depth and angle of the resection is planned out prior to the resection.
Haemostasis is achieved through diathermy and after the procedure, a threeway catheter is inserted and bladder irrigation is initiated.
Aquablation was performed using AquaBeam® according to the manufacturer’s instructions for use.
To ensure treatment quality and safety, the first 18 procedures were supervised by experts from the company. All the procedures were performed by two surgeons (GM, DA) experienced in various treatments of LUTS/BPO.
TURP was performed under spinal or general anaesthesia by a total of seven board certified physicians using a monopolar or bipolar technique according to the surgeon’s preference. For monopolar and bipolar resection 24-Fr resectoscopes with reusable cutting wire loops (Karl Storz Endoskope, Binningen, Switzerland) were used. Resection was performed according to established techniques [17] with the surgical capsule serving as a landmark.
After both procedures, a three-way bladder catheter was inserted for bladder irrigation and left for at least 2 days according to the degree of postoperative haematuria. Patients were discharged from the hospital on the day of catheter removal or the day after, according to the clinical course and patient’s preference.
Financial data
Detailed expense reports based on work records of activities and services performed by the medical and nursing staff, medical consumables used, medications administered, and costs for accommodation, rooms, and equipment were provided by the accounts department of the hospital for each patient. These data were used to compare in-hospital costs arising from aquablation and TURP. The calculations of the costs of the surgical facilities (technical staff, premises and equipment) were based on average personnel costs per minute, fixed charges for room costs and proportionate depreciation of equipment. Fixed charges were also applied for the calculation of administrative costs.
Costs were divided into procedural costs and costs arising from the hospital stay. Procedural costs included professional charges of the urologist, costs of operation facilities (technical staff, premises and equipment), medical supplies required for the procedure (e.g., handpiece [aquablation], resection loop, irrigation solution, tissue evacuation system), costs for anaesthesia (anaesthesiology staff and medical supplies, recovery room) and histological tissue examination if performed [18]. Costs of the inpatient stay included physician’s professional charges, services by nursing specialists, medical supplies (e.g., irrigation solutions), medication, laboratory services, administration and accommodation (premises, housekeeping and catering). The latter was based on fixed sums calculated by the accounts department.
Expense reports were provided in Swiss francs and converted to euros as a more widely used currency based on the average exchange rate over the period that aquablation was performed (September 2020 to end of March 2020; EUR 1 = 1.084 Swiss francs).
Statistics
Data were summarised with descriptive statistics separately for the two treatment groups. Patient characteristics and procedural details were compared between groups using Wilcoxon rank sum tests for numeric (continuous or discrete) variables, and Fisher's exact test for categorical variables. Mean total costs (primary endpoint) were compared between groups with a two-sided t-test after checking for normal distribution, and 95% confidence intervals (CIs) for the difference in means was derived from the test. T-tests were also performed for individual cost items. The dependence of procedural costs on effective operation time in the aquablation group was analysed with linear regression to estimate how much total costs could potentially be reduced if increased experience of the surgeons leads to shorter operation time. All analyses were performed using the R programming language (R version 4.0.2; R Foundation for Statistical Computing, Vienna, Austria, 2020).
Results
Baseline characteristics of the 48 study patients, perioperative data and postoperative results are summarised in table 1. Both groups were similar regarding patients’ age and comorbidities. However, prostate volume was larger in the aquablation group (61.9 ± 22.6 ml vs 50.0 ± 25.7 ml; p = 0.046).
Table 1Patient characteristics, procedural details and postoperative results by treatment group, with p-values from Wilcoxon rank sum tests or Fisher's exact tests for differences between groups.
|
Aquablation (n = 24)
|
TURP (n = 24)
|
p-value
|
|
Baseline characteristics (mean ± SD)
|
| Age (years) |
68.1 ± 6.9 |
68.4 ± 10.1 |
>0.99 |
| Prostate volume (ml) |
61.9 ± 22.6 |
50.0 ± 25.7 |
0.046 |
| PSA level (ng/ml) |
4.6 ± 5.1 |
2.2 ± 1.8 |
0.064 |
| Charlson comorbidity index |
3.2 ± 1.2 |
3.9 ± 2.5 |
0.548 |
| IPSS |
19.2 ± 6.9 |
17.8 ± 6.5 |
0.609 |
| QoL |
3.7 ± 1.3 |
3.0 ± 1.9 |
0.281 |
| Qmax (ml/s) |
7.2 ± 4.6 |
6.0 ± 4.8 |
0.481 |
| PVR (ml) |
100.2 ± 95.9 |
171.9 ± 151.3 |
0.149 |
|
Perioperative data (n and % or mean ± SD)
|
| Anaesthesia |
| – General |
14 (58.3%) |
11 (45.8%) |
0.564 |
| – Spinal |
10 (41.7%) |
13 (54.2%) |
|
| Oral anticoagulant * |
| – None |
19 (79.2%) |
20 (83.3%) |
> 0.99 |
| – Apixaban |
2 (8.3%) |
1 (4.2%) |
|
| – Rivaroxaban |
3 (12.5%) |
2 (8.3%) |
|
| – Phenprocoumon |
0 (0.0%) |
1 (4.2%) |
|
| Need for revision (persistent gross haematuria) |
2 (8.3%) |
0 (0.0%) |
0.490 |
| Quantity of tissue sent for histology (g) |
2.0 ± 2.3 |
16.0 ± 11.6 |
< 0.001 |
| Total procedure time (min)** |
99.6 ± 22.1 |
79.8 ± 21.0 |
0.001 |
| Time until start of surgery (min)*** |
19.4 ± 5.2 |
12.3 ± 4.5 |
< 0.001 |
| Effective surgery time (min)**** |
61.8 ± 20.5 |
62.9 ± 21.5 |
0.918 |
| Duration aquablation cycle 1 (min) |
3.6 ± 0.9 |
|
|
| Duration aquablation cycle 2 (min)***** |
3.3 ± 0.9 |
|
|
| Time for cystoscopy and coagulation (min) |
19.5 ± 17.2 |
|
|
|
Recovery parameters (mean ± SD)
|
| Haemoglobin decrease 24 h (g/l) |
18.3 ± 12.0 |
18.9 ± 12.1 |
0.706 |
| Postoperative hospital stay (days) |
3.8 ± 1.0 |
3.4 ± 0.7 |
0.097 |
| Bladder catheter indwelling time (days) |
2.8 ± 0.9 |
2.3 ± 0.6 |
0.022 |
|
Follow up 6 months postoperatively (mean ± SD)
|
| IPSS decrease |
8.4 ± 8.5 |
10.9 ± 7.4 |
0.510 |
| QoL improvement |
2.6 ± 1.2 |
1.7 ± 2.8 |
0.292 |
| Qmax increase (ml/s) |
10.6 ± 7.4 |
11.2 ± 10.6 |
0.863 |
| PVR decrease (ml) |
75.9 ± 108.2 |
140.0 ± 135.4 |
0.267 |
| PSA reduction (ng/ml) |
1.3 ± 1.3 |
0.9 ± 0.8 |
0.458 |
Time for surgery was similar for both treatments, but procedural time was significantly longer for aquablation if patient positioning and technical preparations were included in the analyses. Postoperative bladder catheter indwelling time was significantly longer after aquablation compared with TURP. However, the difference in length of the hospital stay was not significant. Regarding postoperative outcomes, there were no significant differences between the two treatments 6 months after intervention (table 1).
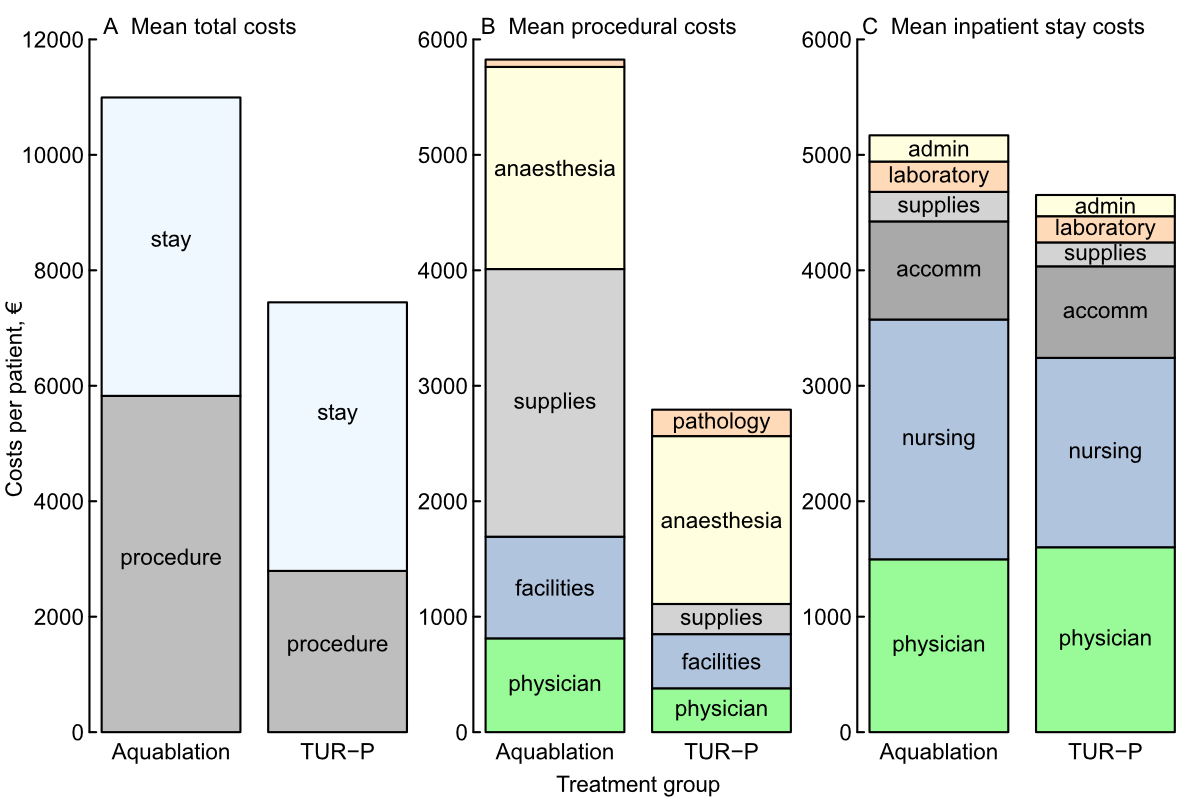
Costs for aquablation and TURP are categorised in table 2 and illustrated in figure 2. Mean total costs per patient were lower for TURP (EUR 7445 ± 2354) than for aquablation (EUR 10,994 ± 2478). The mean difference (md) of EUR 3549 (95% CIEUR 2144–4953) was statistically significant (p <0.001).
Table 2Cost breakdown for in-hospital costs arising from aquablation and TURP.
|
Expense item
|
Mean costs per patient ± SD
(EUR)
|
p-value
|
|
Aquablation (n = 24)
|
TURP (n = 24)
|
| Surgical procedure (total) |
5825 ± 1346 |
2793 ± 725 |
<0.001 |
| – Physician professional charges |
812 ± 384 |
380 ± 116 |
<0.001 |
| — Operation facilities (Technical staff, premises, equipment) |
880 ± 397 |
469 ± 133 |
<0.001 |
| — Medical supplies |
2318 ± 106 |
261 ± 21 |
<0.001 |
| — Anaesthesia (anaesthesiology staff, medical supplies needed for anaesthesia, recovery room) |
1750 ± 752 |
1454 ± 513 |
0.119 |
| — Pathology |
64 ± 43 |
229 ± 104 |
<0.001 |
| Inpatient stay (total) |
5169 ± 1568 |
4652 ± 2015 |
0.327 |
| — Physician professional charges |
1497 ± 1111 |
1601 ± 1246 |
0.761 |
| — Services by nursing specialists |
2077 ± 439 |
1640 ± 418 |
0.001 |
| — Medical supplies and medication |
256 ± 55 |
207 ± 78 |
0.017 |
| — Accommodation (including housekeeping and catering) |
850 ± 333 |
793 ± 436 |
0.616 |
| — Laboratory services |
263 ± 88 |
227 ± 66 |
0.116 |
| — Administrative costs |
227 ± 74 |
184 ± 75 |
0.050 |
|
Total in-hospital costs
|
10994 ± 2478 |
7445 ± 2354 |
<0.001 |
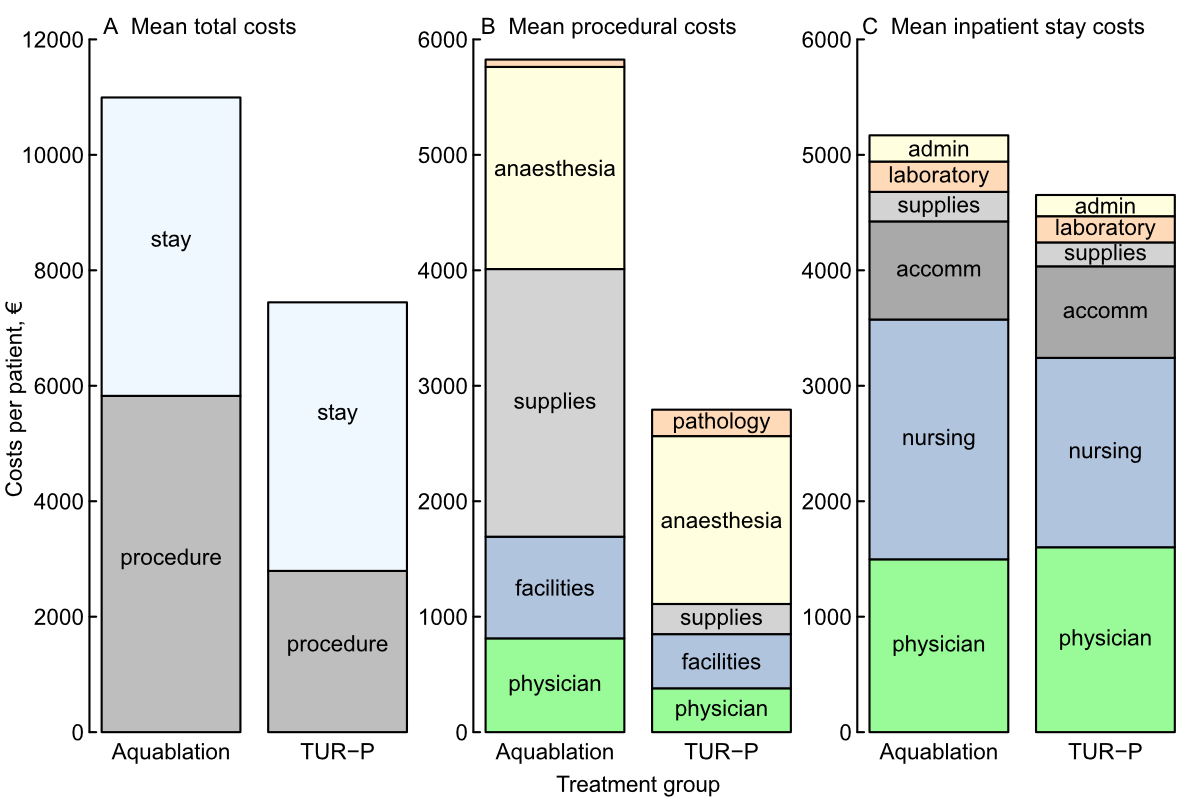
Figure 2 Cost summary for aquablation and TURP grouped by mean total (A), procedural (B), and inpatient stay (C).
stay: inpatient stay; procedure: surgical procedure; supplies: medical supplies; facilities: operation facilities; physician: physician professional charges; anaesthesia: anaesthesia; pathology: pathology; laboratory: laboratory services; supplies: medical supplies and medication; accomm: accommodation; nursing: services by nursing specialists; admin: administrative costs
Mean costs for the surgical procedure alone were EUR 5825 ± 1346 for aquablation and EUR 2793 ± 725 for TURP (mean difference EUR 3032, p <0.001). The main cost factor for the surgical procedure for TURP was anaesthesia (mean costs EUR 1454 ± 513). In contrast, medical supplies (EUR 2318 ± 106) was the most important cost factor for the surgical procedure of aquablation.
Mean costs of the inpatient stay were EUR 5169 ± 1568 for aquablation and EUR 4652 ± 2015 for TURP (mean difference EUR 517, p= 0.327). Services provided by the nursing staff were one of the main cost factors for the hospital stay for both aquablation (EUR 2077 ± 439) and TURP (EUR 1640 ± 418).
As operation time might further decrease with a higher patient volume and increasing experience of surgeons and nursing staff, and as operation times largely vary between different studies, we further assessed the impact of surgical times on the procedural costs. Across all aquablation patients, mean procedural costs increased on average by EUR 41 per minute additional operation time. Mean procedural costs at 45 and 90 minutes effective surgery time were EUR 5131 and 6987, respectively. Predicted mean procedural costs at 30 minutes effective surgery time were EUR 4512.
Discussion
This study shows that total in-hospital costs are significantly higher for aquablation than for TURP. At a Swiss centre of tertiary care total treatment costs for TURP were 67.7% of those arising from aquablation.
The cost breakdown shows that this difference is mainly caused by the costs arising from the surgical procedure. Thus, expenses for medical supplies represent the most pronounced difference between the two treatments, followed by costs arising from greater efforts for the operation room staff. Although the postoperative costs for services by nursing specialists, medical supplies and medications and administrative costs were also significantly in favour of TURP, the difference in total costs for postoperative care was not statistically significant.
The prospective data collection is the main strength of this study. All financial data used in this analysis were routinely and independently assessed by the hospital accounts department. However, the study has also several drawbacks, including its non-randomised setting with limited precision due to the small sample size and possible selection bias, and the fact that it is an exploratory analysis.
Moreover, the 24 aquablation procedures were the first to be performed at our hospital, which is likely to be associated with a longer surgical procedure time and, therefore, also higher costs for aquablation. Therefore, we analysed the dependence of surgery time and costs. According to linear regression, a reduction of the effective operation time by 1 minute could save EUR 41. Assuming that, based on current literature [19, 6, 10, 12, 20], the effective surgical time could be reduced to 30 minutes, mean procedural costs would be reduced from EUR 5825 to 4512, so that EUR 1313 could be saved per procedure.
However, despite these savings, the mean difference in favour of TURP in procedural and total costs would still be EUR 1719 and 2236, respectively. Thus, the total treatment costs of TURP still would only be 76.3% of those arising from aquablation. In this context, it also has to be mentioned that the definition of surgical time differs widely between the available studies (e.g., inclusion of transrectal ultrasound setup in surgical time or not) and that the recommended procedure for haemostasis changed from a catheter tensioning device to electrocautery, with the latter being clearly more time-consuming
Prostate volumes in our study were significantly larger in patients treated by aquablation (61.9 ± 22.6 ml vs 50.0 ± 25.7 ml; p = 0.046). Although this difference would have hardly affected the operation time for aquablation, treating larger prostates by TURP is likely to be more time-consuming.
However, according to our data, reducing the procedural costs of aquablation to those of TURP by reducing the time of surgery would not be possible. Thus, a time reduction of 74 minutes would be required, which is above the mean effective operating time of 61.8 minutes.
Some of the costs included, such as premises and depreciation of equipment, can only be estimated. The fixed sums used for the calculations are based on standard calculations used by the hospital accounts department. Costs that arose from in-hospital complications (see table 1) could not be filtered out separately by the accounts department of the hospital and, therefore, were not available for our analysis.
As healthcare systems vary widely between different countries, our results will not be generalisable to countries with clearly different health care structures.
TURP still represents a reference standard in the surgical treatment of LUTS/BPO, but a variety of other treatment options are now available. Some of these treatments have been shown to be more expensive than TURP [21–23], but still have their role in the treatment of LUTS/BPO due to specific advantages. However, including various treatment techniques was beyond the scope of the present cost analysis.
Our study focused on in-hospital costs. Postoperative incapacity for work, management of post-hospitalization adverse events, and re-interventions and medical treatment for LUTS/BPH during long-term follow-up would have to be included to estimate the actual economic burden for the healthcare system and cost-effectiveness of the intervention. Such data are not available yet.
On the other hand, patients’ expectations and acceptance of specific surgical complications should not be balanced against costs. Thus, the cost difference might be of subordinate importance in patients interested in preserving ejaculatory function.
Conclusions
In-hospital costs are significantly higher for aquablation than for TURP, mainly due to higher costs of medical supplies for the procedure. This difference should be taken into consideration, at least in patients for whom the different side effect profiles of both treatments are irrelevant.
Data sharing statement
Requests for an anonymised, full dataset of physician level data will be considered if the proposed use aligns with public good purposes, does not conflict with other requests, does not conflict with the use by the authors and contingent on approval from the local ethics committee (EKOS). Requests can be addressed to the corresponding author.
Acknowledgements and author contributions
Yáscara Donath-Schmal from the accounts department provided the expense reports and important help with the analyses.
Author contributions: Protocol/project development: Müllhaupt, Abt; data collection or management: Müllhaupt, Lyatoshinsky, Neuenschwander; data analysis: Müllhaupt, Güsewell, Abt; manuscript writing/editing: Müllhaupt, Güsewell, Abt; critical revision of the manuscript: Schmid, Lyatoshinsky, Neuenschwander
Gautier Müllhaupt, MD
Klinik für Urologie, Institut für Medizin
Universität St. Gallen
Rorschacherstrasse 95
CH-9007 St. Gallen
gautier.muellhaupt[at]kssg.ch
References
1.
Berry SJ
,
Coffey DS
,
Walsh PC
,
Ewing LL
. The development of human benign prostatic hyperplasia with age. J Urol. 1984 Sep;132(3):474–9. https://doi.org/10.1016/s0022-5347(17)49698-4 https://doi.org/10.1016/S0022-5347(17)49698-4
2.
Taub DA
,
Wei JT
. The economics of benign prostatic hyperplasia and lower urinary tract symptoms in the United States. Curr Urol Rep. 2006 Jul;7(4):272–81. https://doi.org/10.1007/s11934-996-0006-0
3.
van Exel NJ
,
Koopmanschap MA
,
McDonnell J
,
Chapple CR
,
Berges R
,
Rutten FF
; TRIUMPH Pan-European Expert Panel
. Medical consumption and costs during a one-year follow-up of patients with LUTS suggestive of BPH in six european countries: report of the TRIUMPH study. Eur Urol. 2006 Jan;49(1):92–102. https://doi.org/10.1016/j.eururo.2005.09.016
4.
Gilling P
,
Reuther R
,
Kahokehr A
,
Fraundorfer M
. Aquablation - image-guided robot-assisted waterjet ablation of the prostate: initial clinical experience. BJU Int. 2016 Jun;117(6):923–9. https://doi.org/10.1111/bju.13358
5.
Faber K
,
de Abreu AL
,
Ramos P
,
Aljuri N
,
Mantri S
,
Gill I
, et al.
Image-guided robot-assisted prostate ablation using water jet-hydrodissection: initial study of a novel technology for benign prostatic hyperplasia. J Endourol. 2015 Jan;29(1):63–9. https://doi.org/10.1089/end.2014.0304
6.
Gilling P
,
Anderson P
,
Tan A
. Aquablation of the Prostate for Symptomatic Benign Prostatic Hyperplasia: 1-Year Results. J Urol. 2017 Jun;197(6):1565–72. https://doi.org/10.1016/j.juro.2017.01.056
7.
Yassaie O
,
Silverman JA
,
Gilling PJ
. Aquablation of the Prostate for Symptomatic Benign Prostatic Hyperplasia: early Results. Curr Urol Rep. 2017 Oct;18(12):91. https://doi.org/10.1007/s11934-017-0743-2
8.
Bach T
,
Giannakis I
,
Bachmann A
,
Fiori C
,
Gomez-Sancha F
,
Herrmann TR
, et al.
Aquablation of the prostate: single-center results of a non-selected, consecutive patient cohort. World J Urol. 2019 Jul;37(7):1369–75. https://doi.org/10.1007/s00345-018-2509-y
9.
Desai MM
,
Singh A
,
Abhishek S
,
Laddha A
,
Pandya H
,
Ashrafi AN
, et al.
Aquablation therapy for symptomatic benign prostatic hyperplasia: a single-centre experience in 47 patients. BJU Int. 2018 Jun;121(6):945–51. https://doi.org/10.1111/bju.14126
10.
Gilling P
,
Barber N
,
Bidair M
,
Anderson P
,
Sutton M
,
Aho T
, et al.
WATER: A Double-Blind, Randomized, Controlled Trial of Aquablation® vs Transurethral Resection of the Prostate in Benign Prostatic Hyperplasia. J Urol. 2018 May;199(5):1252–61. https://doi.org/10.1016/j.juro.2017.12.065
11.
Kasivisvanathan V
,
Hussain M
. Aquablation versus transurethral resection of the prostate: 1 year United States - cohort outcomes. Can J Urol. 2018 Jun;25(3):9317–22.
12.
Gilling P
,
Barber N
,
Bidair M
,
Anderson P
,
Sutton M
,
Aho T
, et al.
Two-Year Outcomes After Aquablation Compared to TURP: Efficacy and Ejaculatory Improvements Sustained. Adv Ther. 2019 Jun;36(6):1326–36. https://doi.org/10.1007/s12325-019-00952-3
13.
Gilling P
,
Barber N
,
Bidair M
,
Anderson P
,
Sutton M
,
Aho T
, et al.
Three-year outcomes after Aquablation therapy compared to TURP: results from a blinded randomized trial. Can J Urol. 2020 Feb;27(1):10072–9.
14.
World Medical Association
. Declaration of Helsinki - ethical principles for medical research involving human subjects [Internet]. 1964 [cited 25 August 2018]. Available from: https://www.wma.net/en/
15. International conference on harmonisation: Good clinical practice guideline [Internet]. [cited 25 August 2018]. Available from: www.compendium.ch. http://www.ich.org/products/guidelines/efficacy/article/efficacyguidelines
16.
MacRae C
,
Gilling P
. How I do it: aquablation of the prostate using the AQUABEAM system. Can J Urol. 2016 Dec;23(6):8590–3.
17.
Milam DF
. Transurethral resection of the prostate. In: Smith JA, Howards SS, McGuire EJ, Preminger GM, eds. Hinman’s atlas of urologic surgery. Elsevier, 2012. doi:https://doi.org/10.1016/B978-1-4160-4210- 5.00080-3 https://doi.org/10.1016/B978-1-4160-4210-5.00080-3
18.
Müllhaupt G
,
Enzler-Tschudy A
,
Horg K
,
Bubendorf L
,
Pratsinis M
,
Schmid HP
, et al.
Informative value of histological assessment of tissue acquired during aquablation of the prostate. World J Urol. 2021 Jun;39(6):2043–7. https://doi.org/10.1007/s00345-020-03426-2
19.
Bach T
,
Gilling P
,
El Hajj A
,
Anderson P
,
Barber N
. First Multi-Center All-Comers Study for the Aquablation Procedure. J Clin Med. 2020 Feb;9(2):E603. https://doi.org/10.3390/jcm9020603
20.
Roehrborn CG
,
Teplitsky S
,
Das AK
. Aquablation of the prostate: a review and update. Can J Urol. 2019 Aug;26(4 Suppl 1):20–4.
21.
Fayad AS
,
Sheikh MG
,
Zakaria T
,
Elfottoh HA
,
Alsergany R
. Holmium laser enucleation versus bipolar resection of the prostate: a prospective randomized study. Which to choose? J Endourol. 2011 Aug;25(8):1347–52. https://doi.org/10.1089/end.2011.0059
22.
Mathieu R
,
Lebdai S
,
Cornu JN
,
Benchikh A
,
Azzouzi AR
,
Delongchamps NB
, et al.
Perioperative and economic analysis of surgical treatments for benign prostatic hyperplasia: A study of the French committee on LUT. Prog Urol. 2017 May;27(6):362–8. https://doi.org/10.1016/j.purol.2017.03.010
23.
Müllhaupt G
,
Hechelhammer L
,
Engeler DS
,
Güsewell S
,
Betschart P
,
Zumstein V
, et al.
In-hospital cost analysis of prostatic artery embolization compared with transurethral resection of the prostate: post hoc analysis of a randomized controlled trial. BJU Int. 2019 Jun;123(6):1055–60. https://doi.org/10.1111/bju.14660