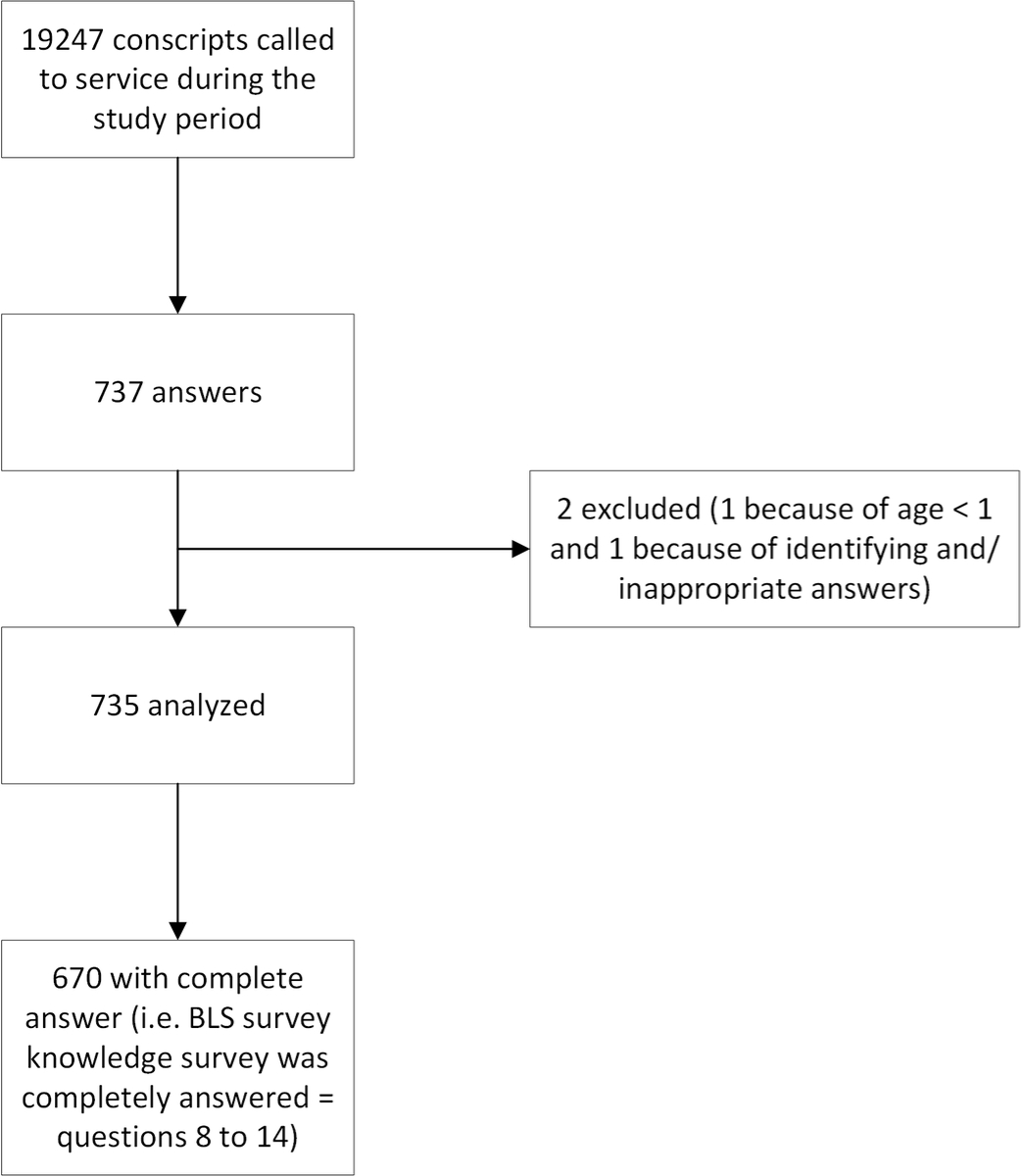
Figure 1 Flow chart.
DOI: https://doi.org/10.4414/SMW.2022.w30147
Basic life support (BLS) is a systematic approach recommended to assess and treat a (un)conscious person with a potential life-threatening emergency. The aim is to provide a standardised approach to recognising cardiac arrest and promptly initiating cardiopulmonary resuscitation (CPR) [1]. These measures include the following: (1) checking one's own safety, (2) recognising a possible cardiac arrest according to assessment with the systematic sequential mnemonic C – A – B ("Circulation – Airways – Breathing"), (3) calling for help and alerting out-of-hospital emergency services, and (4) initiating resuscitation measures such as CPR, ventilation, and defibrillation (if indicated) [2].
In Switzerland, BLS is currently taught to those who aim to obtain a driving license, health and rescue professionals, people wishing to train voluntarily, and army recruits during military general basic training (Instruction de Base Générale) [3]. In 2017, the Touring Club Suisse and the Alliance Suisse des Samaritains, the two main promoters of these courses, encouraged BLS training in the population after a survey showed that in a representative sample of the Swiss population, only 7% were able to give first aid effectively [4]. Interestingly, no independent scientific study in Switzerland has evaluated the knowledge of the population before and after formal BLS training, or estimated the willingness and/or ability of the population to provide first aid.
Training as many people as possible in BLS is still the subject of public and political debate in Switzerland, particularly the cost-effectiveness of training laypersons with a low probability of requiring such skills. In fact, both the usefulness and the cost/benefit ratio of extensive training given to the population are questioned by some experts, who consider such one-off courses as not effective in the medium to long term. Although training strategies involving BLS have been taught multiple times in schools or in professional contexts in other countries [5–9], such strategies are nonetheless still rare and isolated in Switzerland.
Currently, in case of a cardiac arrest, the strategy commonly applied by Swiss emergency call centres when a witness calls the emergency number is based on a systematic proposal to start phone-guided CPR, with some exceptions: an indication that the patient had “not to be resuscitated” orders, injuries incompatible with life, or definite signs of death [10]. An alternative solution would be to allocate all resources to skilled dispatchers, who would work with a dense network of first responders followed by professional emergency medical services (EMS) / helicopter-based EMS teams.
The correct and rapid recognition of cardiac arrest and quick initiation of CPR by bystanders is an important public health issue, as there are 8000 cardiac arrests per year in Switzerland [11] and cardiac arrest is the third leading cause of death in Europe [12]. It therefore seems useful to focus research on this topic, particularly among the younger generations, in order to precisely understand their level of knowledge and to optimise future training programmes. In this context, the conscript population is an interesting one to study in order to evaluate BLS competences of a semi-representative sample of Swiss young adults.
Our objective was to evaluate BLS knowledge among Swiss conscripts during the recruitment process and to identify characteristics related to performance.
We developed a 22-item survey with SurveyMonkey® software. The conscripts in this study were enrolled in the six Swiss Armed Forces recruitment centres through information posters printed in the three languages corresponding to the linguistic regions (French, German and Italian). Inclusion criteria for this study were: being called for duty as a conscript to one of the recruitment centres, having a smartphone, and agreeing to answer the survey. Exclusion criteria were: age below 18 years, answers that allowed identification of the conscript, and inappropriate answers. Employees of the centres were also excluded, although internal restrictions were given to limit this bias.
A quick-response code on the posters needed to be scanned with the conscript’s smartphone to link directly to the online survey. Due to military requirements, the candidates’ recruitment for the study was very passive. We were allowed to display two A0 posters per centre and there was no formal presentation of the study. To ensure an optimal and homogeneous recruitment process among all of the above-mentioned centres, coordination meetings were organised with each recruitment centre head to find the best solution to present our study to the conscripts, according to the specific organisation of each centre. In this context, a paper version of the survey was provided to two recruitment centres: one because of poor network coverage and the absence of Wi-Fi and the other because of low poster visibility and an insufficient number of answers in this French-speaking centre. These handwritten answers were added to the online database by one of the investigators (DD). The start of the study was planned for 11February 2019, without any deadline, and we estimated that 643 complete answers were needed to provide a margin of error of 5% in a total population of 20,000 conscripts with a confidence level of 99%. The study ended on 27 September 2019, when the sample size was reached.
Participation in the study was voluntary and did not provide any benefits; a conscript’s lack of participation was unknown to the officers and recruitment centre heads. Conscripts were considered to have given their consent to be enrolled in this study by logging into the online questionnaire with their own smartphone or by filling in the handwritten form. No informed consent is available. Although the IP number of the smartphone was temporarily recorded by the software to prevent the same device from participating twice, in order to ensure complete anonymity, this number was never transmitted during data extraction. Similarly, there was no question or information on the paper questionnaires that could be used to identify any of the respondents.
A 22-item survey was initially created in French with SurveyMonkey® software, and then translated into German and Italian and made available directly on the platform (appendix 2). To minimise translation bias, German and Italian questionnaires were compared and proofread by three independent bilingual persons before the start of our study. Each questionnaire had the same structure, consisting of three parts. The first part focused on demographic data (gender, age, place of residence, education level). The second so-called technical part aimed to evaluate BLS theoretical knowledge, as well as knowledge of the Swiss medical emergency phone number “144.” Of the six technical questions, four (Items 8 to 11; appendix 1) dealt with one of the four “secure-examine-alarm-assist” phases of BLS, and two were closed questions (Items 14 and 15; appendix 2). This part was based on the algorithms published by the European Resuscitation Council in 2015 and validated for the year 2018 [13]. To compare the technical answers with the demographic data collected, we implemented a 6-point scoring system. For statistical analysis of the technical part, points were awarded for each correct answer to the six questions assessed. The method used to score and grade the questions is detailed in table 1. Each correct answer was worth 1 point, an incorrect answer was worth 0 points, and the maximum number of points that could be awarded was 6. For two questions (medical emergency number and cardiac arrest identification), it was possible to be awarded 0.5 points if the answer was defined as partially correct (table 1).
Table 1Correction grid.
| Multiple-choice question | 1 point | 0.5 points | 0 points |
| 8: “In Switzerland, what is the emergency number to call in case of a health problem?” | 144 | 112 | 117, 118, other |
| 9: “A person is unconscious on the ground in a pedestrian crossing. What is your first action?” | Security | Other answer | |
| 10: “A person is unconscious on the floor, on her back and breathing normally. What do you do after trying to wake her up and calling for help?” | Recovery position | Other answer | |
| 11: “How do you recognise when someone is in cardiac arrest?” | Apnoea/gasping + unconsciousness | 1 error (omission or addition) | 2 errors (omission or addition) |
| 13: “By performing CPR, I can make the person's condition worse.” | False | True | |
| 14: “By performing CPR, I risk criminal prosecution.” | False | True |
CPR: cardiopulmonary resuscitation
The third part of the questionnaire probed the conscript’s personal experience about a potential cardiac arrest situation as a bystander or lay first responder. In addition, conscripts were asked to self-assess their knowledge/skills of CPR (1 = very bad, 5 = excellent; see appendix 2). The conscripts were then asked about the usefulness – in their opinion – of introducing generalised BLS training for the whole population, as well as what the ideal environment would be to implement such an approach.
At the request of the Swiss Armed Forces for both organisational reasons and ease of participation, this survey was not to take more than 10 minutes to complete. The questionnaire therefore consisted of 17 closed multiple-choice questions and 3 open questions. Three questions were based on a previous answer (Items 7, 12b, and 18b; appendix 1) and thus the total number of questions to be answered by the conscript varied between 17 and 20. The order of answers in the multiple-choice questionnaire was systematically randomised by computer for each conscript and each question. However, the overall sequence of predefined related questions was not randomised in order to maintain the three-part structure as described above. Each conscript could answer the online survey only once. It was tested multiple times by the authors before the start of the study to ensure a failure-free and user-friendly experience for the conscript.
Twenty-nine subcategories were defined before the start of the study in order to use regression models to test the association between our primary outcome and 29 predictors of interest. The categories included age, gender, socio-economic status, language, and time since the last BLS training.
Continuous variables having a Gaussian distribution are described by mean and standard deviation. In the case of non-Gaussian distribution, the median and interquartile range were calculated. Categorical variables are expressed as percentages and 95% confidence intervals (CIs). Comparisons were performed by using the Student t-test or the Mann-Whitney U-test, as appropriate. Categorical data are expressed as numbers and percentages and were compared by using Pearson’s chi-square test or Fisher's exact test, as appropriate. We performed ordinal logistic regression to assess associations between our primary outcome and potential predictors such as age, sex, socioeconomic status, language, and time since the last BLS training. Linearity for continuous variables was assessed graphically. We included polynomial terms in cases of departure from linearity. We assessed agreement between knowledge score and self-assessment knowledge with weighted Cohen’s kappa. The value of 1 was given in cases of exact agreement or with a difference of 1 point.
A bilateral p-value of <0.05 was considered significant. All analyses were performed using STATA software (version 16.0; Stata Corp, College Station, TX, USA).
The Human Research Ethics Committee of the Canton of Vaud was contacted prior to the start of the study. As this study was performed on anonymously collected data and according to federal regulations, the Research Ethics Committee ruled on 3 October 2018 to waive the need for full ethical approval.
Between 11 February and 27 September 2019, a total of 19,247 conscripts went through the recruitment process. Of these, 737 responded to the survey (3.8% of study sample).Two were excluded because age was <18 years (1), and identifying answers and/or inappropriate answers (1). Hence, 735 were included in the analyses.
Among included respondents, 718 (98%) were male and 696 (95%) were between 18 and 25 years of age, with a median age of 19 years (±1.2) (table 2). Five hundred and eighty-seven (80%) of responders had attended at least one BLS course prior to recruitment.
Table 2Demographic data.
| Age, mean ± standard deviation | 19.5 ± 1.5 | |
| Sex, n (%) | Male | 718 (98) |
| Female | 17 (2) | |
| Socio-professional status, n (%) | Without Education and unemployed | 4 (1) |
| Unemployed | 20 (3) | |
| Employed | 246 (33) | |
| Apprenticeship | 258 (35) | |
| High school | 132 (18) | |
| University | 75 (10) | |
| Language, n (%) | French | 371 (50) |
| German | 345 (47) | |
| Italian | 19 (3) | |
| Recruiting centre, n (%) | Payerne | 278 (38) |
| Rüti | 169 (23) | |
| Aarau | 129 (18) | |
| Sumiswald | 85 (11) | |
| Mels | 52 (7) | |
| Monte Ceneri | 22 (3) | |
| Time since last BLS course, n (%) | <1 year | 133 (18) |
| 1 year | 88 (12) | |
| 2 years | 120 (16) | |
| 3 years | 98 (13) | |
| >3 years ago | 148 (20) | |
| Never | 144 (20) | |
| Not available | 4 (1) | |
BLS: basic life support
The second part of the questionnaire was designed to assess the level of knowledge of BLS. An answer to these questions was not mandatory. The BLS knowledge survey was completely answered by 670 participants (91%). Of the 670, 157 (23%) scored 5 or 6 points on the questionnaire (fig. 1). The results of the six questions assessed are detailed in table 3.
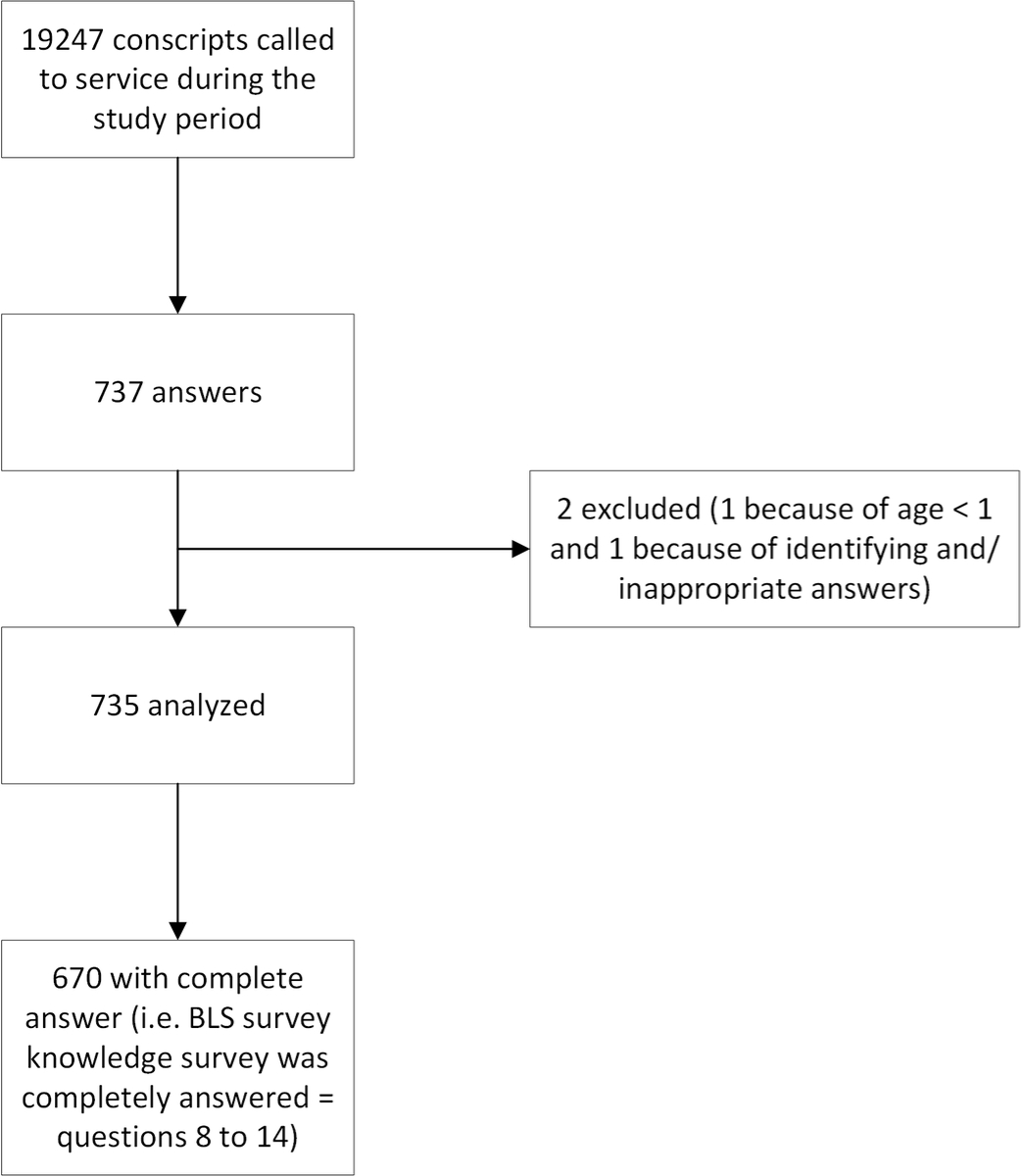
Figure 1 Flow chart.
Table 3Results of the technical part of the survey.
| Multiple-choice question | n | Possible answers | n (%) |
| 8: “In Switzerland, what is the emergency number to call in case of a health problem?” | 695 | 144 | 553 (80) |
| 112 | 32 (5) | ||
| 118 | 21 (3) | ||
| 117 | 18 (3) | ||
| 114 | 41 (6) | ||
| 115 | 3 (<1) | ||
| 911 | 4 (<1) | ||
| 41 | 2 (<1) | ||
| Does not know | 13 (2) | ||
| Other numbers (793, 318, 122, 44, 108, 311, 116, 411) | 8 (1) | ||
| 9: “A person is unconscious on the ground in a crosswalk. What is your first action?” | 695 | Alert emergency services | 372 (54) |
| Ensure your own safety (correct answer) | 266 (38) | ||
| Start CPR immediately | 51 (7) | ||
| Get an automated external defibrillator (AED) | 6 (1) | ||
| 10: “A person is unconscious on the floor, on his/her back and breathing normally. What do you do after trying to wake him/her up and calling for help?” | 695 | Put the victim in the recovery position (correct answer) | 598 (86) |
| Do not touch the victim and wait for help | 55 (8) | ||
| Start CPR immediately | 27 (4) | ||
| Put the victim on his/her stomach to prevent vomiting | 15 (2) | ||
| 11: "How do you recognise when someone is in cardiac arrest? (one or multiple answers possible)" | 695 | The patient is apnoeic and/or gasping (correct answer) | 501 (72) |
| The patient is unconscious (correct answer) | 363 (52) | ||
| The patient is pale | 188 (27) | ||
| The patient’s hemi-body is paralyzed | 126 (18) | ||
| 13: "By performing CPR, I can make the person's condition worse” | 670 | True | 364 (54) |
| False (correct answer) | 306 (46) | ||
| 14: "By performing CPR, I risk criminal prosecution" | 670 | False (correct answer) | 581 (87) |
| True | 89 (13) |
CPR: cardiopulmonary resuscitation
Of the 670 conscripts who completely answered questions 8 to 14, 108 (16%) scored 3.5 points, 93 (14%) scored 4 points, 108 (16%) scored 4.5 points, 66 (10%) scored 5 points and 21 (8%) scored 5.5 points. Only 40 (6%) answered the six questions correctly (fig. 2). Those who answered in German obtained significantly better results than those who answered in French or Italian. Detailed results are available in appendix 1.

Figure 2 Distribution of conscripts' results by test score (n = 670).
Of 670 conscripts, 585 (87%) thought that BLS training should be mandatory for the whole population; 413 (62%) believed that primary/secondary school and 218 (33%) believed that the workplace were the most suitable places to provide this type of education. Regarding the self-assessment of their ability to provide well-performed CPR, 316 (47%) felt that they had good skills, with a mean score of 2.9 (1: very bad, 5: excellent). Finally, 31 (5%) of the 670 respondents indicated that they had already performed CPR in a real cardiac arrest situation. Of these 31 respondents, 16 (52%) of them had performed CPR on a stranger, 8 (26%) on a friend and/or colleague, 4 (13%) on a patient, 3 (10%) on a family member, 1 (3%) during a mission as a firefighter, and 1 (3%) on a neighbour.
We compared conscript’s scores and their self-assessment, and found substantial agreement between them (weighted kappa 0.22 with 74% agreement; fig. 3).

Figure 3 Conscripts' knowledge of basic life support linked to their self-assessment.
Being German speaking (odds ratio [OR] 1.3, 95% confidence interval [CI] 1.0–1.8), prior receipt of BLS training (OR 3.1, 95% CI 2.0–4.8), and female gender (OR 5.8, 95% CI 2.0–17.2) were associated with a higher BLS knowledge score. Time to last BLS training of ≥3 years (OR 0.5, 95% CI 0.4–0.7) (fig. 4) and unemployment (OR 0.3, 95% CI 0.1–0.9) were associated with a lower BLS knowledge score.

Figure 4 Conscripts' knowledge of basic life support (BLS) by time since last BLS course.
Table 4Univariate and multivariate analysis.
| Univariate | Multivariate | ||||
| Odds ratio (95% CI) | p-value | Odds ratio (95% CI) | p-value | ||
| Age | 0.95 (0.89–1.01) | 0.099 | 0.96 (0.89–1.04) | 0.279 | |
| Sex | Male | 1 | – | 1 | – |
| Female | 5.00 (1.75–14.3) | 0.003 | 5.85 (1.99–17.3) | 0.001 | |
| Occupation | Employee | 1 | 1 | – | |
| Apprentice | 1.11 (0.81–1.52) | 0.517 | 0.95 (0.67–1.32) | 0.743 | |
| Secondary school | 1.25 (0.84–1.84) | 0.268 | 1.05 (0.69–1.60) | 0.815 | |
| Student | 0.83 (0.51–1.34) | 0.435 | 0.80 (0.49–1.32) | 0.388 | |
| Unemployed | 0.31 (0.11–0.91) | 0.033 | 0.41 (0.13–1.31) | 0.133 | |
| BLS training | No | 1 | – | 1 | – |
| Yes | 4.16 (2.94–5.88) | <0.001 | 8.56 (5.33–13.76) | <0.001 | |
| Time from training | <1 year | 1 | – | 1 | – |
| 1 year | 0.44 (0.27–0.73) | 0.001 | 0.45 (0.27–0.74) | 0.002 | |
| 2 years | 0.55 (0.35–0.88) | 0.012 | 0.60 (0.38–0.96) | 0.032 | |
| 3 years | 0.33 (0.20–0.54) | <0.001 | 0.36 (0.22–0.58) | <0.001 | |
| >3 years | 0.33 (0.21–0.52) | <0.001 | 0.38 (0.23–0.61) | <0.001 | |
| No training | 0.11 (0.07–0.18) | <0.001 | – | – | |
| Language | French | 1 | – | 1 | – |
| German | 1.52 (1.17–2.00) | 0.002 | 1.29 (0.97–1.72) | 0.077 | |
| Italian | 1.40 (0.58–3.36) | 0.449 | 0.80 (0.32–2.00) | 0.632 | |
CI: confidence interval
The originality of this study lies in the fact that it considered the willingness of the group studied to be better trained in BLS, a problem that, to our knowledge, has not been investigated previously in the literature. Although the response rate was limited, our study is indirectly representative of the Swiss conscript population, and revealed generally heterogeneous BLS knowledge among Swiss conscripts. One fourth only had good BLS knowledge. Most of them believed that BLS training should be mandatory for the whole population. Being female, German speaking and having previous BLS training were associated with good BLS knowledge. On the contrary, being unemployed, and increased time since last BLS training were associated with worse BLS knowledge. The results shown in figure 4 are consistent with those from similar previously published studies [14–16].
Women scored significantly higher than did their male counterparts. This result should be interpreted with caution in view of the large difference in the number of answers between these two subgroups and the selection bias inherent in the Swiss federal law on army and military administration, as Swiss women are integrated only through voluntary military service [17]. To date, the role of gender as a positive predictor for BLS theoretical knowledge is still debated [18]. Although the results of previous studies seem to be congruent with some of our results, such as emergency number knowledge [9] (women: 94% in the Kanstad et al. study vs 94% in our study; men: 85% in the Kanstad aet nd al. study vs 79% in our study) and higher scores on the theoretical test for women [19], further well-designed studies should be conducted to validate these trends. Indeed, several publications with similar questionnaires and a higher representation of women have shown no statistically significant differences in answers between men and women [18, 20, 21].
One potential reason for the observed association between good BLS knowledge and German speaking is that Swiss cantons and cities have a lot of freedom in terms of education and public health. It is possible that the number of schools offering first aid training to their students is higher in Swiss-German and/or bilingual cantons. Similarly, it is possible that companies based in the German-speaking part of Switzerland have a greater awareness of BLS training for their employees. To our knowledge, no database is currently available to verify these hypotheses.
Swiss-German and Italian-speaking conscripts were under-represented compared with national percentages (German: 50% conscripts vs 62% nationally, Italian: 3% conscripts vs 8% nationally), whereas French-speaking conscripts were over-represented (47% conscripts vs 23% nationally) (table 2). One of the reasons for this discrepancy may be the over-abundant number of answers obtained that were written in French. Another reason may be the non-negligible number of conscripts who are perfectly bilingual and who were therefore able to use the language of their choice when answering the online questionnaire. Nevertheless, a possible selection bias cannot be excluded.
Despite a marked tendency for unemployed people to perform less well on the questionnaire, no epidemiological variables collected in this study could shed light on why they scored significantly lower than did the overall sample. Being unemployed, by definition, removes the chance to be trained in BLS at the workplace, may also select participant with a lower socioeconomic background and could explain why this subgroup had greater difficulty in answering the questionnaire correctly.
Knowledge of the Swiss emergency phone number “144” by only 79.6% (552) of the sample and of “112” (European emergency number) by only 4.6% (32) is concerning. Indeed, since calling the emergency number is part of the first link in the emergency chain of survival, it is essential that the entire population is able to call for help as quickly as possible. The validity of our results is supported by a recent Swiss national study that reported similar results throughout all age categories [22].
For comparison, in 2002, 95.7% of 18- to 29-year-olds in Queensland, Australia, were aware of the national emergency number “000.” [23] One reason for this result could be that all Australian emergency services (fire-police-emergency health) are grouped under a single number. In Switzerland, the existence of many emergency numbers (144 and 112: EMS, 118: firefighters, 117: law enforcement, 1414: air ambulance) can be confusing. Unfortunately, dialling valid but incorrect emergency numbers or invalid numbers (114, 115...) will at best result in a answer delay, but at worst in nonachievement of the request for help.
The studied population was aware of their abilities by judging them appropriately. Although previous studies have shown that self-assessment does not necessarily reflect real knowledge [24–26], good correlation between self-estimation and actual BLS skills has recently been reported [26], as was the case in our study.
Motivation is one of the keys to successful learning and long-term retention of information [27]. In view of the mixed performances of the conscripts in the questionnaire, their good capacity for self-assessment, and, above all, their very strong desire to implement mandatory BLS training for all, the usefulness of a mandatory approach appears to be a strong and viable option. Nevertheless, the implementation of such a significant public health action would require the support of a more powerful and ambitious additional study to confirm that the population as a whole is in favour of this paradigm shift. Indeed, although recent studies have been published concerning knowledge of the general population in terms of BLS, in particular in Switzerland [22], none of these studies have included the motivation to be better educated as a key point. From our results, we are confident that there is a potential public health benefit to be gained from the implementation of mandatory and repeated BLS training for the entire youth population.
The answers to the question about whether CPR can worsen a patient’s condition (item 13, appendix 1) by our sample seem to show confusion between worsening health and potential complications caused by CPR. Indeed, half of conscripts answered the question correctly. The nuance regarding worsening of the patient’s health versus complications secondary to CPR is subtle but crucial in the key messages of BLS training in order to systematically encourage the initiation of CPR in case of doubt about the patient's health status (cardiac arrest or not).
Although there is a real risk of life-threatening secondary injuries developing during CPR with patients who achieved a return of spontaneous circulation, it is low (1%) and probably not associated with a reduced chance of survival [28, 29]. Thus, the risk of inflicting potential iatrogenic injuries on the patient should not limit the first aid that must be undertaken immediately in the event of a cardiac arrest.
Interestingly, although the majority (70–80%) of out-of-hospital cardiac arrests in Switzerland occur in a patient's home [30], half of the conscripts who had ever performed CPR did not know the victim, and only two conscripts performed CPR on a family member.
Although the number of answers represents about 4% of the sample, the study nevertheless made it possible to obtain a large number of answers (735 usable answers) with a sample of conscripts presenting a great socioeconomic and cultural mix. To our knowledge, this study is the first of its kind in Switzerland. Our sample might not be fully representative of the conscript population, especially in terms of the proportion of language regions or gender distribution. Similarly, results from this study cannot be directly extrapolated to the entire Swiss young adult population. Certain population groups could not be included in this study, such as foreigners residing in Switzerland, the majority of Swiss women, or young Swiss who were exempt from recruitment because of medical or psychosocial conditions. An important selection bias was therefore inherent in the format of the study.
Another potential limitation in this type of study is the uncertainty that all conscripts understood the questions in the same way. The questionnaire was self-administered, without assistance or supervision. In addition, we cannot exclude the possibility of differences in the energy devoted to the promotion of the study between the different recruitment centres. As the six centres worked independently from each other (both organisationally and logistically), it was not possible to standardise the locations where the posters were put up and the way the study was promoted by their respective staff.
The technical part of the study was intended to test only the most basic and indispensable knowledge for a Swiss citizen. It was by no means intended to be exhaustive or to cover all the technical and theoretical knowledge expected at the end of a full BLS-automated external defibrillator course recognised by the Swiss Resuscitation Council [31]. Furthermore, the modest number of questions used to assess the conscripts prevented us from examining their knowledge in more detail.
In order to assess the knowledge of the Swiss population, it would have been optimal to carry out a telephone survey with a random sample that was representative of the population. This type of survey is frequently done for marketing surveys or for public health investigations and would be the ideal method to conduct a future well-designed study with the same outcomes as ours. The resources required for such an approach, in particular the financial resources inherent in the method of collecting this information, were not available for this study.
As expected, the results of the questionnaires completed by the conscripts show significant potential for improvement, which makes it possible to envisage corrections in terms of training and dissemination of information. Not only are there various possibilities for improving the BLS skills of the general population [9, 32–41], but the majority of the group surveyed was also in favour of stronger implementation of BLS training, in particular by making it compulsory to attend such training, preferably in schools. Notably, this solution has been supported by numerous publications in the field [7, 32–34, 42, 43]. According to our data and in line with current recommendations, such training can only be effective if it is provided repeatedly over time in order to maintain a level of knowledge over the long term. Although several studies have demonstrated the positive cost/benefit ratio of such courses [44–46], their high costs and the divergent expert opinions about them are important barriers to nationwide implementation of BLS courses in the population. We are pleased to note, however, that this strong demand to extend BLS training to the entire population is consistent with the Swiss Resuscitation Council's National Survival Strategy for cardiac arrest, including measures "influencing employers and schools to achieve as high a proportion as possible of the population initially trained in BLS before the age of 20” [47].
It will be crucial to make an additional effort to increase awareness of the health emergency number, with the aim of having 95% of the Swiss population able to dial this number. Although further studies need to be undertaken in order to define the best methods to achieve this goal, it would be interesting to start by (re-)questioning the usefulness of a common emergency number for all emergency services, following the example of other European health systems (e.g., Romania or Portugal). Another way to improve the management of cardiac arrest in Switzerland would be to systematically propose telephone-guided resuscitation by the regulator when someone calls “144.” Indeed, there is currently no harmonisation between the different Swiss emergency call centres, each of them using their own protocols concerning remote-guided CPR.
Theoretical knowledge of BLS among Swiss conscripts is heterogeneous. In particularly regarding the medical emergency phone number “144”, which is unknown to 20% of conscripts, or in the recognition of the signs and symptoms of a cardiac arrest. These shortcomings must be weighed against the strong motivation of the conscripts to be better trained, particularly in their professional environment or school. Carrying out a similar study including a larger sample, representative of the Swiss population, would be useful to confirm the trends explored in this work.
We acknowledge the assistance of the Centre of Competence for Military and Disaster Medicine, Swiss Armed Forces Medical Service, Federal Department of Defence, Civil Protection and Sport DDPS and Barbara Every, ELS, of BioMedical Editor, for English language editing.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
This study was financed by the Faculty of Biology and Medicine of the University of Lausanne (FBM-UNIL) and by the Department of Emergency Medicine of the Lausanne University Hospital (CHUV).
1. American Heart Association . HIGHLIGHTS of the 2015 American Heart Association Guidelines Update for CPR and ECC. 2015.
2. Khalid U , Juma AA . Paradigm shift: ‘ABC’ to ‘CAB’ for cardiac arrests. Scand J Trauma Resusc Emerg Med. 2010 Nov;18(1):59. https://doi.org/10.1186/1757-7241-18-59
3. Déroulement et dates des écoles de recrues [Internet]. [cité 25 févr 2018]. Disponible sur: https://www.vtg.admin.ch/fr/mon-service-militaire/recrues.html
4. TCS suisse, ASS alliance suisse des samaritains. Test premiers secours - TCS Suisse [Internet]. [cité 26 nov 2017]. Disponible sur: https://www.tcs.ch/fr/tests-conseils/conseils/tous-les-themes/test-premiers-secours.php
5. Rasmus A , Czekajlo MS . A national survey of the Polish population’s cardiopulmonary resuscitation knowledge. Eur J Emerg Med. 2000 Mar;7(1):39–43. https://doi.org/10.1097/00063110-200003000-00008
6. Chen M , Wang Y , Li X , Hou L , Wang Y , Liu J , et al. Public Knowledge and Attitudes towards Bystander Cardiopulmonary Resuscitation in China. BioMed Res Int. 2017;2017.
7. Siebenpfund P, Kaufmann G, Roman B, Ummenhofer W. La réanimation par des secouristes volontaires. BMS. 2015;33(96):1124–6.
8. Lukas RP , Van Aken H , Mölhoff T , Weber T , Rammert M , Wild E , et al. Kids save lives: a six-year longitudinal study of schoolchildren learning cardiopulmonary resuscitation: Who should do the teaching and will the effects last? Resuscitation. 2016 Apr;101:35–40. https://doi.org/10.1016/j.resuscitation.2016.01.028
9. Kanstad BK , Nilsen SA , Fredriksen K . CPR knowledge and attitude to performing bystander CPR among secondary school students in Norway. Resuscitation. 2011 Aug;82(8):1053–9. https://doi.org/10.1016/j.resuscitation.2011.03.033
10. Ghuysen A , Collas D , Stipulante S , Donneau AF , Hartstein G , Hosmans T , et al. Dispatcher-assisted telephone cardiopulmonary resuscitation using a French-language compression-only protocol in volunteers with or without prior life support training: A randomized trial. Resuscitation. 2011 Jan;82(1):57–63. https://doi.org/10.1016/j.resuscitation.2010.09.014
11. Fondation Suisse de Cardiologie . Arrêt cardio-circulatoire - Fondation Suisse de Cardiologie [Internet]. [cited 2021 juill 21]. Disponible sur: https://www.swissheart.ch/fr/prevention/comportement-en-cas-durgence/arret-cardio-circulatoire.html
12. Gräsner JT , Herlitz J , Tjelmeland IB , Wnent J , Masterson S , Lilja G , et al. European Resuscitation Council Guidelines 2021: epidemiology of cardiac arrest in Europe. Resuscitation. 2021 Apr;161:61–79. https://doi.org/10.1016/j.resuscitation.2021.02.007
13. Perkins GD , Handley AJ , Koster RW , Castrén M , Smyth MA , Olasveengen T , et al.; Adult basic life support and automated external defibrillation section Collaborators . European Resuscitation Council Guidelines for Resuscitation 2015: Section 2. Adult basic life support and automated external defibrillation. Resuscitation. 2015 Oct;95:81–99. https://doi.org/10.1016/j.resuscitation.2015.07.015
14. Plant N , Taylor K . How best to teach CPR to schoolchildren: a systematic review. Resuscitation. 2013 Apr;84(4):415–21. https://doi.org/10.1016/j.resuscitation.2012.12.008
15. de Ruijter PA , Biersteker HA , Biert J , van Goor H , Tan EC . Retention of first aid and basic life support skills in undergraduate medical students. Med Educ Online. 2014 Nov;19(1):24841. https://doi.org/10.3402/meo.v19.24841
16. Binkhorst M , Coopmans M , Draaisma JM , Bot P , Hogeveen M . Retention of knowledge and skills in pediatric basic life support amongst pediatricians. Eur J Pediatr. 2018 Jul;177(7):1089–99. https://doi.org/10.1007/s00431-018-3161-7
17. Confédération Suisse . Loi fédérale sur l’armée et l’administration militaire. Sect. Titre deuxième, Chap 1, Art. 3 févr 3, 1995.
18. Finke SR , Schroeder DC , Ecker H , Wingen S , Hinkelbein J , Wetsch WA , et al. Gender aspects in cardiopulmonary resuscitation by schoolchildren: A systematic review. Resuscitation. 2018 Apr;125:70–8. https://doi.org/10.1016/j.resuscitation.2018.01.025
19. Lester C , Donnelly P , Weston C . Is peer tutoring beneficial in the context of school resuscitation training? Health Educ Res. 1997 Sep;12(3):347–54. https://doi.org/10.1093/her/12.3.347
20. Papalexopoulou K , Chalkias A , Dontas I , Pliatsika P , Giannakakos C , Papapanagiotou P , et al. Education and age affect skill acquisition and retention in lay rescuers after a European Resuscitation Council CPR/AED course. Heart Lung. 2014 Jan-Feb;43(1):66–71. https://doi.org/10.1016/j.hrtlng.2013.09.008
21. Fischer H , Strunk G , Neuhold S , Kiblböck D , Trimmel H , Baubin M , et al. The effectiveness of ERC advanced life support (ALS) provider courses for the retention of ALS knowledge. Resuscitation. 2012 Feb;83(2):227–31. https://doi.org/10.1016/j.resuscitation.2011.09.014
22. Bühler G , Bütikofer S , Craviolini J , Hermann M , Krähenbühl D , Eliane M , et al. Was tun im Notfall? Befragung zum Verhalten und den Kompetenzen in Erster Hilfe in der Schweiz. Zürich: Sotomo, Schweizerisches Rotes Kreuz. Helsana. 2020;(août):43.
23. Clark MJ , Enraght-Moony E , Balanda KP , Lynch M , Tighe T , FitzGerald G . Knowledge of the national emergency telephone number and prevalence and characteristics of those trained in CPR in Queensland: baseline information for targeted training interventions. Resuscitation. 2002 Apr;53(1):63–9. https://doi.org/10.1016/S0300-9572(01)00486-5
24. Davis DA , Mazmanian PE , Fordis M , Van Harrison R , Thorpe KE , Perrier L . Accuracy of physician self-assessment compared with observed measures of competence: a systematic review. JAMA. 2006 Sep;296(9):1094–102. https://doi.org/10.1001/jama.296.9.1094
25. Lynn DJ , Holzer C , O’Neill P . Relationships between self-assessment skills, test performance, and demographic variables in psychiatry residents. Adv Health Sci Educ Theory Pract. 2006 Feb;11(1):51–60. https://doi.org/10.1007/s10459-005-5473-4
26. Lund-Kordahl I , Mathiassen M , Melau J , Olasveengen TM , Sunde K , Fredriksen K . Relationship between level of CPR training, self-reported skills, and actual manikin test performance-an observational study. Int J Emerg Med. 2019 Jan;12(1):2. https://doi.org/10.1186/s12245-018-0220-9
27. Seli P , Wammes JD , Risko EF , Smilek D . On the relation between motivation and retention in educational contexts: the role of intentional and unintentional mind wandering. Psychon Bull Rev. 2016 Aug;23(4):1280–7. https://doi.org/10.3758/s13423-015-0979-0
28. Boland LL , Satterlee PA , Hokanson JS , Strauss CE , Yost D . Chest Compression Injuries Detected via Routine Post-arrest Care in Patients Who Survive to Admission after Out-of-hospital Cardiac Arrest. Prehosp Emerg Care. 2015 Jan-Mar;19(1):23–30. https://doi.org/10.3109/10903127.2014.936636
29. Krischer JP , Fine EG , Davis JH , Nagel EL . Complications of cardiac resuscitation. Chest. 1987 Aug;92(2):287–91. https://doi.org/10.1378/chest.92.2.287
30. Carron PN , Dami F , Niquille M , Frei O , Valloton L , Yersin B . Médecine d’urgence préhospitalière. Éditions médecine & hygiène; 2013. 637 p.
31. SRC - Swiss Resuscitation Council . Directives de cours 2015 Guide pour l’obtention du label SRC pour les cours Basic Life Support - version 2.0. 2015.
32. . American Academy of Pediatrics Committee on School Health. Basic life support training school. Pediatrics. 1993 Jan;91(1):158–9. https://doi.org/10.1542/peds.91.1.158
33. Vetter VL , Haley DM . Secondary prevention of sudden cardiac death: does it work in children? Curr Opin Cardiol. 2014 Jan;29(1):68–75. https://doi.org/10.1097/HCO.0000000000000022
34. Bohn A , Lukas RP , Breckwoldt J , Böttiger BW , Van Aken H . ‘Kids save lives’: why schoolchildren should train in cardiopulmonary resuscitation. Curr Opin Crit Care. 2015 Jun;21(3):220–5. https://doi.org/10.1097/MCC.0000000000000204
35. Song KJ , Shin SD , Park CB , Kim JY , Kim DK , Kim CH , et al. Dispatcher-assisted bystander cardiopulmonary resuscitation in a metropolitan city: a before-after population-based study. Resuscitation. 2014 Jan;85(1):34–41. https://doi.org/10.1016/j.resuscitation.2013.06.004
36. Mathiesen WT , Bjørshol CA , Høyland S , Braut GS , Søreide E . Exploring How Lay Rescuers Overcome Barriers to Provide Cardiopulmonary Resuscitation: A Qualitative Study. Prehosp Disaster Med. 2017 Feb;32(1):27–32. https://doi.org/10.1017/S1049023X16001278
37. Reder S , Cummings P , Quan L . Comparison of three instructional methods for teaching cardiopulmonary resuscitation and use of an automatic external defibrillator to high school students. Resuscitation. 2006 Jun;69(3):443–53. https://doi.org/10.1016/j.resuscitation.2005.08.020
38. Semeraro F , Frisoli A , Loconsole C , Mastronicola N , Stroppa F , Ristagno G , et al. Kids (learn how to) save lives in the school with the serious game Relive. Resuscitation. 2017 Jul;116:27–32. https://doi.org/10.1016/j.resuscitation.2017.04.038
39. Cuijpers P , Kicken W , Gorgels A . Effectiveness of a blended learning approach for CPR training in secondary schools for different education level groups. Resuscitation. 2012 Oct;83:e112. https://doi.org/10.1016/j.resuscitation.2012.08.289
40. Langlais BT , Panczyk M , Sutter J , Fukushima H , Wu Z , Iwami T , et al. Barriers to patient positioning for telephone cardiopulmonary resuscitation in out-of-hospital cardiac arrest. Resuscitation. 2017 Jun;115:163–8. https://doi.org/10.1016/j.resuscitation.2017.03.034
41. Hsieh MJ , Bhanji F , Chiang WC , Yang CW , Chien KL , Ma MH . Comparing the effect of self-instruction with that of traditional instruction in basic life support courses-A systematic review. Resuscitation. 2016 Nov;108:8–19. https://doi.org/10.1016/j.resuscitation.2016.08.021
42. Meissner TM , Kloppe C , Hanefeld C . Basic life support skills of high school students before and after cardiopulmonary resuscitation training: a longitudinal investigation. Scand J Trauma Resusc Emerg Med. 2012 Apr;20(1):31. https://doi.org/10.1186/1757-7241-20-31
43. Böttiger BW , Van Aken H . Kids save lives—training school children in cardiopulmonary resuscitation worldwide is now endorsed by the World Health Organization (WHO). Resuscitation. 2015 Sep;94:A5–7.
44. Bouland AJ , Risko N , Lawner BJ , Seaman KG , Godar CM , Levy MJ . The Price of a Helping Hand: Modeling the Outcomes and Costs of Bystander CPR. Prehosp Emerg Care. 2015;19(4):524–34. https://doi.org/10.3109/10903127.2014.995844
45. Friesen J , Patterson D , Munjal K . Cardiopulmonary Resuscitation in Resource-limited Health Systems-Considerations for Training and Delivery. Prehosp Disaster Med. 2015 Feb;30(1):97–101. https://doi.org/10.1017/S1049023X14001265
46. Nichol G , Huszti E , Birnbaum A , Mahoney B , Weisfeldt M , Travers A , et al. Cost-effectiveness of lay responder defibrillation for out-of-hospital cardiac arrest. Ann Emerg Med. août 2009;54(2):226-235.e1-2.
47. Burkart R , Regener H . Stratégie nationale de survie relative aux arrêts circulatoires. Bull Médecins Suisses. 2019 Nov;100(48):1615–7.
Table S1Detailed answers of the survey.
| Item | Question | Details (%) | Ntot | Remarks (n) |
| 0a | Language | French (50), German (47), Italian (3) | 735 | |
| 0b | Recruitment centers | Payerne (37), Rüti (23), Aarau (18), Sumiswald (12), Mels (7) Monte Ceneri (3) | 735 | Data extrapolated from Item #3 |
| 1 | Age | 18 (27), 19 (34), 20 (17), 21 (7), 22 (4), 23 (3), 24 (2), 25 (1), >25 (5) | 735 | |
| 2 | Type | Male (98), female (2) | 735 | |
| 3 | Postcode/Home address | - | 735 | |
| 4 | Currently you are... (education/job) | No education and no job (<1), no job (3), employment (33), apprenticeship (35), secondary school (18), university/high school (10) | 735 | |
| 5 | Please specify your [Item 4] | - | 735 | |
| 6 | Have you ever taken a first aid course? | Yes (80), No (20) | 731 | |
| 7 | Your first aid training was done… | Less than 1 year ago (23), 1 year ago (15), 2 years ago (21), 3 years ago, (17), Over 3 years ago (24) | 587 | |
| 8 | In Switzerland, what is the emergency number to call in case of a health problem? | 144 (79.6), 112 (4.6), 118 (3.0), 117 (2.6), 114 (5.9), 115(0.4) 911 (0.6), 41 (0.3), don't know (1.9), Other number * (1.1) | 695 | * 793 (1), 318 (1), 122 (1), 44 (1), 108 (1)311 (1), 116 (1), 411 (1) |
| 9 | A person is unconscious on the ground in a pedestrian crossing. What is your first action? | Start CPR immediately (7), get an AED (1), ensure safety (38), alert emergency services (54) | 695 | |
| 10 | A person is unconscious on the floor, on her back and breathing normally. What do you do after trying to wake her up and calling for help? | Start CPR immediately (4), do nothing (8), put in recovery position(1) (86) Put on stomach to avoid vomiting (2) | 695 | |
| 11 | How do you recognize when someone is in cardiac arrest? | Apnea or gasping (72), Unconsciousness (52), pallor (27), paralysis of half the body (18) | 695 | Multiple answers possible |
| 12 | If faced with a person in cardiac arrest, would you agree to perform CPR? | Yes (87), no (13) | 695 | |
| 12b | What are the reasons you could not perform CPR? | Fear of doing harm (45), don’t know what to do (36), against nature (7), Risk of criminal/legal prosecution (3), fear of not doing right (2), other* (8) | 81(2) | Multiple answers possible; not comfortable (1), not his problem (1), too tiring (1), not the right thing to do (4) |
| 13 | By performing CPR, I can make the person's condition worse. | True (54), false (46) | 670 | |
| 14 | By performing CPR, I risk criminal prosecution. | True (13), false (87) | 670 | |
| 15 | In your opinion, should first aid training be made mandatory for the whole population? | Yes (87), no (13) | 670 | |
| 16 | Where do you think would be the best place to teach first aid to the maximum number of people? | Primary/secondary school (61), workplace (33), sports club (7), private first aid companies (11), army/recruitment (6), other* (2) | 670 | Multiple answers possible; * when obtaining a driving license (3), days organized by the Confederation (1), supermarket (1), community hall (1), fire station (1), at home (1) |
| 17 | How would you rate your resuscitation (CPR) skills? | Very poor (6), poor (22), fair (47), good (21), excellent (3) | 670 | |
| 18 | Have you ever performed CPR on a real person? | Yes (5), no (95) | 670 | |
| 18b | Please specify who this person is in relation to you: | Unknown person (52), family (10), patient (13), friend/colleague (26), other* (6) | 31(2) | Multiple responses possible; * firefighter intervention (1), neighbor (1) |
This appendix is available in the PDF version of the article.