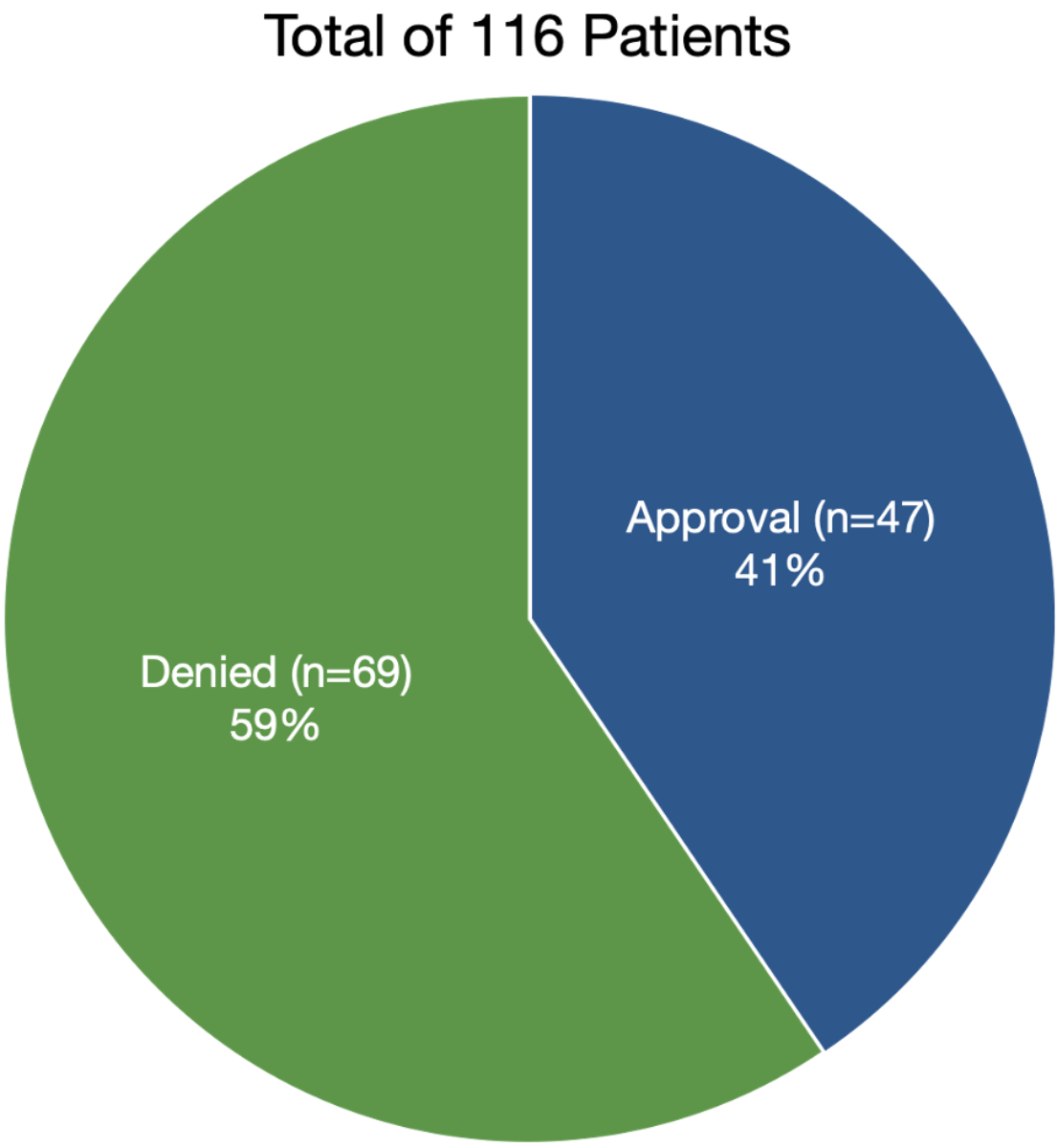
Figure 1 Denial and acceptance rates.
DOI: https://doi.org/10.4414/SMW.2022.w30131
In Switzerland, within the last 25 years, the proportion of obese (body mass index [BMI] >30 kg/m2) people has doubled. For men, we have seen an increase from 6% in 1992 to 12% in 2017, whereas women had an increase from 5% in 1992 to 10% in 2017 in the general population [1]. This has led to a dramatic increase in bariatric surgery, in order to lose weight. After massive weight loss, the patients find themselves with contour deformities and/or redundant skin. It is scientifically proven that bariatric surgery has considerable advantages for patients, such as resolution of type 2 diabetes and improvement of arterial hypertension [2]. The long-term benefit of modest and moderate weight loss in established type 2 diabetes and diabetes prevention, as well as improvement in cardiovascular risk factors is well established [3]. The resulting redundant excess skin can lead to difficulty in mobilisation and exercising, intertrigo and infections. Furthermore, patients report being dissatisfied with their appearance, which consequently leads to decreased psychosocial well-being [4]. The only possible treatment for excess skin is surgery. However, body contouring surgery is considered by some as cosmetic rather than reconstructive surgery and therefore should not be reimbursed by insurance companies [5]. Today, these procedures are often considered cosmetic by health insurance companies and therefore not reimbursed. There is little scientific evidence regarding benefits of these procedures and hence the insurers also put their efficacy in question. Moreover, they also simply ignore the fact that redundant skin is an expected outcome of bariatric surgery [6].
However, several studies have shown that patients undergoing body contouring surgery maintain a significantly lower average weight than patients who undergo only bariatric surgery [7]. Patients undergoing body contouring surgery are in fact very satisfied with the results and have an improvement in self-esteem and quality of life in many cases [8, 9]. Despite an appropriate diagnosis-related group (DRG)-code, coverage of post-bariatric surgery by insurance companies remains low. There is little guidance for coverage by insurance companies for body contouring procedures [5, 10]. A negative decision for reimbursement in redundant skin and body deformities by the federal court (Decision K135/04 of 17 January 2006, Bundesgericht) makes it an even harder task for doctors to get financial help for the patient, despite the fact that surgeons can clearly identify the medical indications for the surgery. The decision on coverage remains random.
The aim of our study was to identify objective criteria in application letters submitted to insurance companies leading to a positive answer for body contouring surgery.
All patients requesting body contouring surgery (arms, breast, abdomen, thighs) after bariatric surgery between January 2013 and December 2018 in the Department of Plastic and Reconstructive Surgery, University Hospital in Bern, Switzerland were included in this study. No patients requested gluteal or facelift surgery after massive weight loss. The following patient-related data in the application letters were retrospectively collected for each patient:
All postoperative weight losses and BMI values were recorded at the time of writing the letter to the insurance company.
The application letters from our department to the insurance companies were searched for objective criteria leading to approval for body contouring surgery. The following keywords were collected from the application letters for each patient:
In order to analyse which factors influence the approval or the refusal of insurance companies, the retrospectively collected continuous data were analysed with the student's t-test or the Mann-Whitney U-test if the data were not normally distributed; the Pearson’s χ2 test and the Fischer’s exact test were used for the categorical variables. A p-value <0.05 was considered statistically significant. A univariate statistical analysis was performed for multiple independent variables. All the factors with a significance of p <0.2 in the univariate analysis were included in the multivariate logistic regression model to identify independent predictors for the approval of the insurance companies. Statistical analysis was performed using SPSS 24.0 (SPSS Inc., Chicago, USA).
The study was conducted according to the Declaration of Helsinki principles and was approved by the local Research Ethics Committees (BASEC-Nr: Req-2020-01274).
The study included 150 consecutive patients seen in the outpatient clinic between January 2013 and December 2018. From this total of 150 patients, 116 (77.3%) could be included in the study; the excluded patients are summarised in table 1. The specific demographic data of the patients included are summarised in table 2. We considered medical indications as follows:
Table 1Excluded patients.
| Reason for exclusion | Number of patients |
| Missing data | 10 |
| Missing answer from insurance companies | 2 |
| No medical indication | 18 |
| Referred to the psychiatrist | 4 |
Table 2Demographic data.
| Mean | Min. | Max. | |
| Age (years) | 46.3 | 24 | 79 |
| Men (n) | 22 | ||
| Women (n) | 94 | ||
| Time from bariatric operation to first plastic surgery consultation (months) | 49.2 | 0 | 221 |
| Height (cm) | 165.4 | 145 | 192 |
| Weight (kg) | 127.4 | 83.9 | 230 |
| BMI before bariatric operation (kg/m2) | 46.6 | 31.7 | 94.6 |
| Weight after bariatric operation (kg) | 80.9 | 55 | 137 |
| BMI after bariatric operation (kg/m2) | 29.6 | 20.7 | 46.3 |
| Weight loss (kg) | 46.9 | 12 | 124 |
| BMI loss (kg/m2) | 17.2 | 4.4 | 55.9 |
| Stability of weight (months) | 15.2 | 0 | 126 |
| Time from bariatric operation to application letter (months) | 51.6 | 0 | 221 |
| Number of application letters | 1.3 | 1 | 3 |
BMI: body mass index
An average of 1.3 application letters were written per patient, with a range from 1 application letter to a maximum number of 3 per patient, with a total number of 148 application letters. Ninety patients had one letter of request for reimbursement to the insurance company, of which only 38 (32.8%) were approved (table 3).
Table 3Number of application letters.
| Number of application letters | Total applications | % applications | Accepted | % accepted |
| 1 | 90 | 77.6% | 38 | 32.8% |
| 2 | 20 | 17.2% | 5 | 4.3% |
| 3 | 6 | 5.2% | 4 | 3.4% |
Twenty patients had a supplementary letter of recommendation and an additional six patients had a third letter of recommendation. That brings the overall approval for post-bariatric body contouring surgery to 47 patients or 40.52%, as shown in fig. 1.
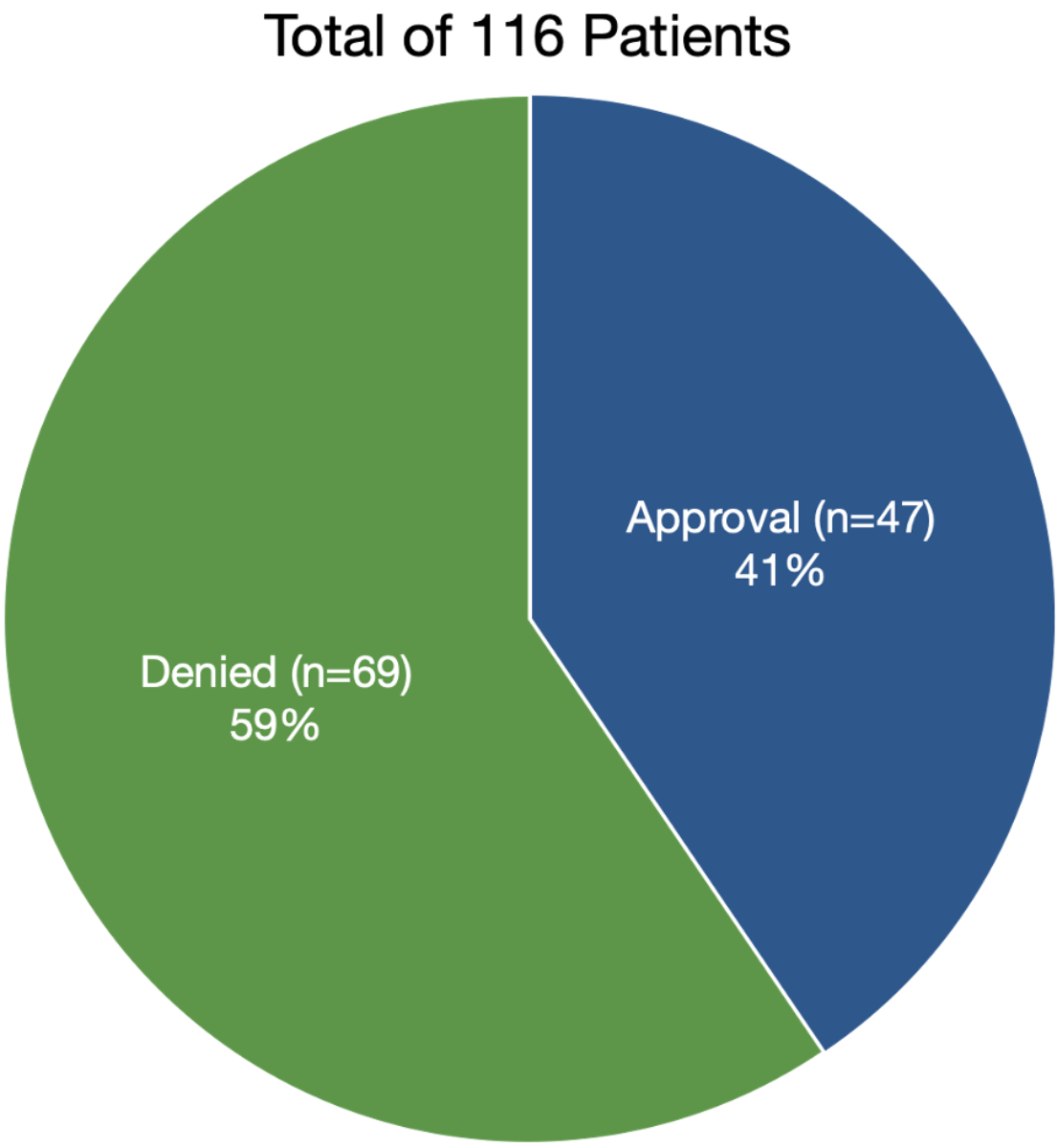
Figure 1 Denial and acceptance rates.
In total, 45 patients were finally operated on at our department for plastic and hand surgery. One patient declined surgery for personal reasons. Another patient was redirected to another plastic surgery unit because of the lack of insurance coverage in our canton.
The phrase "medical indication" was mentioned in 101 application letters out of the total 148 sent to the insurance companies. The second most mentioned phrase was "mechanical restriction". A mechanical restriction was considered to exist when mentioned by the referring physician or the patient indicated a shearing stress between body parts, for example between the legs, through the abdominal apron or between the upper body and upper arms. The frequency of the terms mentioned in the application letters is summarised in table 4.
Table 4Number of keywords searched in application letters.
| Keyword | Number |
| Medical indication | 101 |
| Mechanical/functional restrictions | 83 |
| Mental suffering | 42 |
| Pain | 37 |
| Stable weight over a year | 34 |
| Unreasonable/abnormal body condition | 31 |
| Additional application letters | 20 |
| Disfigurement | 17 |
| Stigmatising | 8 |
| Weight history | 4 |
| Reconstructive intervention | 3 |
| Lawyer | 2 |
| Painful scar | 2 |
| Photodocumentation | 113 |
| Eczema - consequence | 90 |
| Pain - consequence | 30 |
The results of the univariate analysis are summarised in table 5. Including an additional application letter to the insurance company (p <0.024), either from the family doctor or from another medical department, as well as mentioning mechanical restriction (p <0.022), were associated with a positive response from the insurance companies.
Table 5Univariate analysis of the data for the approval of the insurance company.
| Caracteristic | Refusal | Approval | p-value | |
| Medical indication | 0.130 | |||
| No | 11 (78.6%) | 3 (21.4%) | ||
| Yes | 58 (57.4%) | 43 (42.6%) | ||
| Mechanical restriction | 0.022 | |||
| No | 27 (75.0%) | 9 (25.0%) | ||
| Yes | 42 (52.5%) | 38 (47.5%) | ||
| Mental suffering | 0.133 | |||
| No | 40 (54.8%) | 33 (45.2%) | ||
| Yes | 29 (69.0%) | 13 (31%) | ||
| Pain | 0.625 | |||
| No | 48 (61.5%) | 30 (38.5%) | ||
| Yes | 21 (56.8%) | 16 (43.2%) | ||
| Stable weight over a year | 0.055 | |||
| No | 53 (66.3%) | 27 (33.8%) | ||
| Yes | 16 (47.1%) | 18 (52.9%) | ||
| Unreasonable/abnormal body condition | 0.123 | |||
| No | 54 (64.3%) | 30 (35.7%) | ||
| Yes | 15 (48.4%) | 16 (51.6%) | ||
| Additional application letters | 0.024 | |||
| No | 62 (64.6%) | 34 (35.4%) | ||
| Yes | 7 (36.8%) | 12 (63.2%) | ||
| Disfigurement | 0.086 | |||
| No | 62 (63.3%) | 36 (36.7%) | ||
| Yes | 7 (41.2%) | 10 (58.8%) | ||
| Stigmatising | 0.263 | |||
| No | 66 (61.7%) | 41 (38.3%) | ||
| Yes | 3 (37.5%) | 5 (62.5%) | ||
| Weight history | 0.299 | |||
| No | 68 (61.8%) | 42(38.2%) | ||
| Yes | 1 (25.0%) | 3 (75.0%) | ||
| Reconstructive intervention | 1.000 | |||
| No | 67 (59.8%) | 45 (40.2%) | ||
| Yes | 2 (66.7%) | 1 (33.3%) | ||
| Lawyer | 0.158 | |||
| No | 69 (61.1%) | 44 (38.9%) | ||
| Yes | 0 (0.0%) | 2 (100%) | ||
| Photo documentation | 1.000 | |||
| No | 1 (100%) | 0 (0.0%) | ||
| Yes | 67 (59.3%) | 46 (40.7%) | ||
| Eczema | 0.486 | |||
| No | 17 (65.4%) | 9 (34.6%) | ||
| Yes | 52 (57.8%) | 3 (42.2%) | ||
| Gender | 0.600 | |||
| Male | 12 (54.5%) | 10 (45.5%) | ||
| Female | 57 (60.6%) | 37 (39.4%) | ||
| Number of application letters (in total) | 0.149 | |||
| 1 | 52 (57.8%) | 83 (42.2%) | ||
| 2 | 15 (75.0%) | 5 (25.0%) | ||
| 3 | 2 (33.3%) | 4 (66.7%) |
Looking at the demographic data, we found that a high BMI before the bariatric operation (p <0.009), a high weight before the bariatric operation (p <0.039), a high weight loss (p <0.027), as well as a high BMI reduction (p <0.021) were associated with a higher approval rate by insurance companies (table 6).
Table 6Mean and the standard deviation for every variable and for each response from the insurance company (No/Yes). Univariate analysis of the data for the approval of the insurance companies.
| Characteristics | Number | Mean | Standard deviation | p-value | |
| Time after operation (first seen) | 0.403 | ||||
| No | 69 | 46.07 | 49.67 | ||
| Yes | 47 | 53.83 | 47.64 | ||
| Height | 0.416 | ||||
| No | 67 | 165.95 | 8.28 | ||
| Yes | 47 | 164.56 | 9.73 | ||
| Weight before operation | 0.039 | ||||
| No | 67 | 122.94 | 20.39 | ||
| Yes | 46 | 133.64 | 33.92 | ||
| BMI before operation | 0.009 | ||||
| No | 67 | 44.72 | 7.52 | ||
| Yes | 46 | 49.55 | 11.82 | ||
| Weight after operation | 0.375 | ||||
| No | 67 | 79.78 | 13.89 | ||
| Yes | 47 | 82.55 | 19.39 | ||
| BMI after operation | 0.162 | ||||
| No | 67 | 28.98 | 4.83 | ||
| Yes | 47 | 30.46 | 6.39 | ||
| Weight loss | 0.027 | ||||
| No | 67 | 43.17 | 16.27 | ||
| Yes | 46 | 51.60 | 23.72 | ||
| BMI loss | 0.021 | ||||
| No | 67 | 15.74 | 6.25 | ||
| Yes | 46 | 19.10 | 9.04 | ||
| Percentage excess BMI loss | 0.136 | ||||
| No | 67 | 34.48 | 9.50 | ||
| Yes | 46 | 37.41 | 11.13 | ||
| Stability of weight until submission of application letter | 0.054 | ||||
| No | 67 | 12.94 | 9.92 | ||
| Yes | 46 | 18.78 | 21.43 | ||
| Time in months after first bariatric operation and submission of application letter | 0.376 | ||||
| No | 69 | 48.74 | 49.38 | ||
| Yes | 46 | 56.91 | 46.78 |
BMI: body mass index
To further clarify the importance of a reduction in BMI we separated the patients into four categories, depending on the degree of reduction: a first group with a BMI reduction of 0–10 kg/m2, a second group with a BMI reduction of 10.1–20 kg/m2, a third group with a BMI reduction of 20.1–30 kg/m2 and a last group (group 4) with a BMI reduction of >30 kg/m2. We did a logistic regression to compare groups 2–4 with the first BMI reduction group (0–10 kg/m2).
The second group with 10.1–20 kg/m2 BMI reduction did not show a statistically significant difference when compared with the first group (p <0.697). However, the 20.1–30 kg/m2 group had 4.889 times higher chance than the 0–10 kg/m2 BMI reduction group to have their application letters accepted (p <0.027).The group with >30.1 kg/m2 BMI reduction had a 16.5 times higher chance than the 0–10 kg/m2 group to have an accepted application letter from the insurance company (p <0.022; table 7)
Table 7BMI groups 1–4 with statistical significance (p-Value) and the added chance (Exp(B)) in comparison to group 1.
| Group | BMI loss (kg/m2) | p-Value | Odds ratio (Exp(B)) | Confidence interval | |
| Lower limit | Upper limit | ||||
| 1 | 0–10 | 0.006 | |||
| 2 | 10.1–20 | 0.697 | 1.283 | 0.365 | 4.507 |
| 3 | 20.1–30 | 0.027 | 4.889 | 1.199 | 19.942 |
| 4 | >30.1 | 0.022 | 16.5 | 1.487 | 183.070 |
A logistic regression was performed to ascertain the effects of the variables with a p-value <0.2 on the approval or denial of the insurance companies. The logistic regression model was statistically significant, χ2(21) = 62.968, p <0.0001. The model explained 61.0% (Nagelkerke R2) of the variance in the approval of the insurance companies and correctly classified 80.8% of cases. Of all the predictor variables, only two were statistically significant: the mention of medical indication and of mental suffering. Patients where medical indication was mentioned had a 15.2 times higher chance of receiving a positive answer (p <0.001). Patients who had mental suffering included in the letter had 82.3% less chance of getting a positive response from the insurance company (p <0.001). A detailed risk factor table including all odd ratios, 95% confidence intervals and associated p-values are presented as table 8. All reports of mental suffering were confirmed by a professional.
Table 8Multivariate analysis for factors predicting insurance approval.
| Standard error | Odds ratio | pvalue) | 95% confidence interval | ||
| Lower limit | Upper limit | ||||
| Medical indication | 1.603 | 15.253 | 0.049 | 0.659 | 352.886 |
| Mechanical restriction | 0.687 | 1.471 | 0.574 | 0.382 | 5.659 |
| Mental suffering | 0.725 | 0.215 | 0.034 | 0.052 | 0.891 |
| Stable weight over a year | 0.758 | 2.470 | 0.233 | 0.559 | 10.914 |
| Unreasonable/abnormal body condition | 0.697 | 1.597 | 0.502 | 0.407 | 6.262 |
| Additional application letters | 1.502 | 1.613 | 0.750 | 0.085 | 30.606 |
| Disfigurement | 0.971 | 1.296 | 0.789 | 0.193 | 8.697 |
| Weight history | 162.318 | 26584.412 | 0.999 | 0.000 | |
| Lawyer | 230.419 | 15136.720 | 0.999 | 0.000 | |
| Stability of weight (in months) | 0.489 | 0.568 | 0.248 | 0.218 | 1.483 |
| Number of application letters (1) | 0.133 | ||||
| – 2 | 1.869 | 0.023 | 0.044 | 0.001 | 0.911 |
| – 3 | 1.661 | 0.436 | 0.618 | 0.017 | 11.316 |
| Lost BMI (0–10 kg/m2) | 0.294 | ||||
| – 10.1–20 kg/m2 | 1.061 | 2.952 | 0.307 | 0.369 | 23.601 |
| – 20.1–30 kg/m2 | 1.292 | 10.632 | 0.067 | 0.844 | 133.886 |
| – >30.1 kg/m2 | 1468.080 | 2411387.616 | 0.999 | 0.000 | |
| Constant | 17.992 | 1520957.253 | 0.152 | ||
There was no statistical significant difference in the approval rate by the insurance companies between the different surgical procedures (arms, breast, abdomen, thighs). In addition, due to our small sample size there was no statistical difference in our study for requesting one or more surgical procedure. The type of body contouring surgery that was planned, approved and performed is shown in detail in table 9.
Table 9Procedures requested, approved and performed.
| Abdomen requested (n) | Thigh requested (n) | Arms requested (n) | Breast requested (n) |
| 100 | 44 | 14 | 24 |
| Abdomen approved (n) | Thigh approved (n) | Arms approved (n) | Breast approved (n) |
| 42 | 6 | 3 | 4 |
| Abdomen performed (n) | Thigh performed (n) | Arms performed (n) | Breast performed (n) |
| 42 | 6 | 3 | 4 |
Sparse data exist in Switzerland regarding insurance coverage for post-bariatric procedures. We reached an approval rate of approximately 40% in our single centre review at the University Hospital in Bern. The reimbursement rate found in our study is comparable to other reimbursement rates found in the literature [4, 5, 10, 12, 13]. The decision-making processes of insurance companies worldwide appear to be random at best. Some USA and UK insurance companies even insert an exclusion clause for bariatric surgery in their policies [5, 10, 14].
In the review of Gurunluoglu et al. in the USA, the refusal rate based on the authors' experience was 40–50% [10], whereas in England, the denial rate reached 60% in the Primary Care Trusts that allow or exclude bariplastic surgery on the National Health Service [5]. In the study of Sati et al. there was a reimbursement rate of 35% by insurance companies in patients with massive weight loss and going through body-contouring surgery [12]. Another study showed that out of the 47 patients undergoing body contouring procedures after gastric bypass surgery, only 47% of the 17 abdominoplasties and 33.3% of the 6 breast lifts had been paid for by insurance [13]. In the study of Sioka et al only 16.7% of a total of 167 patients were approved by insurance company for body contouring procedures in Greece [4].
The goal of this study was not to investigate different insurance companies body contouring approval rates, but to evaluate whether there are any set criteria for approval and to assess if using certain keywords in the correspondence with the insurance company influences the decision-making process. Interestingly, our study identified keywords such as “medical indication” (a positive factor) and “mental suffering” (a negative factor) that had an impact on the insurance companies decision. In addition, multiple letters to the insurance companies influence the decision in favour of the patient. Our study is unique in this respect, as we could not find any data in the medical literature regarding the correspondence with insurance companies. Insurance systems vary between European countries and are therefore hard to compare.
In our study, a higher BMI reduction also showed a higher acceptance rate by insurance companies. Losing more than 30 kg/m2 in BMI value gave a 16.5 times higher chance to obtain an approval by the insurance company (p <0.022). Furthermore, losing an equivalent of 20.1 to 30 kg/m2 resulted in a 4.9 times higher approval rate from the insurance company (p <0.027). There are different criteria that have been proposed by Samrat Mukherjee [5], Raffi Gurunluoglu [10] and the British association of Plastic and Reconstructive and Aesthetic Surgery Commission (BAPRAS) [15] for body contouring surgery after massive weight loss. These guidelines have been followed by some insurance companies, but there are, however, major differences between them [16–21]. The guidelines of some insurance companies distinguish between patients requesting body contouring surgery after natural weight loss versus weight loss after bariatric surgery [5]. Furthermore, most of the criteria are often very hard for patients to meet after bariatric surgery. For example, there is a guideline that suggests the patient should reach a BMI lower than 30 kg/m2 or even a stable BMI between 18 and 27 kg/m2 [5, 15]. A meta-analysis assessing the cost-effectiveness of bariatric surgery compared with conservative treatment in patients with massive weight loss in the Swiss Medical Weekly demonstrated that nearly all studies assessing patients with a BMI >35 kg/m2 indicated bariatric surgery to be cost-saving or cost-effective [22]. Coon et al. also showed that the BMI has an influence on complications after bariatric surgery [23]. This was confirmed by the study of Au et al., which reported the (post-weight loss) BMI at the time of body contouring surgery to be a predictor for postoperative complications [24]. Another possible reason why patients with a high weight or a high BMI reduction received a positive response for body contouring procedures from the insurance companies is that a lower BMI gives a lower complication rate after a body contouring procedure [23–25]. A meta-analysis showed that there was a 60% increase in the risk of complications after body contouring procedures in the post-bariatric patient group compared with a non-bariatric group [25]. It is as yet difficult to set a cut-off BMI at which the patient should be reimbursed for body contouring procedures or not. In the authors experience, the most common reason provided by insurance companies for refusal was a high BMI.
Very few physical criteria seem to influence the insurance companies approval positively. In our study, “mechanical restrictions”, as judged by the surgeon, appears to have a positive outcome. In other studies, abdominoplasties were covered by insurance only if the pannus reached or was below the level of the symphysis pubis [ 12, 19 ]. Problems with gait, especially osteoarthritis of the knee joint, is commonly associated with an increase in BMI. Studies have shown that a five unit increase in BMI was associated with a 35% increase in risk of knee osteoarthritis [11].
Worldwide insurance approval trends for body contouring surgery suggest that a high rejection rate based on ill-defined criteria seems to be a common occurrence. Insurance companies appear to have a positive attitude to rewarding people with a high BMI reduction. Obese patients considering any bariatric surgery should be treated by a multidisciplinary team including a general practitioner, a visceral surgeon, a plastic surgeon, a psychologist and a dietitian. Additionally, the patient should discuss what exactly will be paid by an insurance company and what he or she would need to cover by themselves from the array of body contouring procedures. Our study confirmed that an additional application letter sent to the insurance company renders a higher chance for approval for a body contouring procedure. Closer cooperation between different medical disciplines is therefore required.
The psychological well-being of the patients is clearly impacted by the extent of disfigurement after massive weight loss [9], with body contouring procedures significantly improving satisfaction and quality of life in patients after gastric bypass [26]. Moreover, the study of Smith et al. suggested that patients undergoing body contouring surgery were able to lose more weight and maintain a better BMI than patients undergoing bariatric surgery alone [7]. Insurance companies often consider body contouring procedures cosmetic surgery and therefore there is no reimbursement for this type of operation. Each insurance company should have a set of objective criteria that can be applied universally to all patients. It would be of even greater benefit if a national Swiss guideline for these procedures could be agreed upon by all insurance companies. A consensus conference between all Swiss insurance companies to decide on objective criteria might be helpful. In our opinion, a person with a high BMI (>40 kg/m2) prior to the massive weight loss and with a high BMI reduction (>20 kg/m2) will definitely have more redundant skin and, in consequence, more mechanical restrictions. In such a case, the body contouring procedure should be considered reconstructive. On the other hand, a patient with a lower BMI before bariatric surgery and a lower BMI reduction will have only moderate redundant skin and mechanical restrictions. In this particular situation, the body contouring procedure would be seen more as an aesthetic operation. This outlook was confirmed by our study on the approvals of different insurance companies.
We recommend that all patients are seen in an interdisciplinary team. The most important objective criteria appear to be related to the patients' BMI. We recommend that insurance companies adopt a universal BMI policy that it would make clear to patients and referring physicians whether they will qualify for body contouring surgery after bariatric surgery. This would significantly reduce the administrative workload of both the treating physicians and insurance companies. In addition, it would then be clear for patients before going on the bariatric surgery road whether they will be able to have body contouring surgery paid for by the insurance companies.
The broad term "medical indication" in correspondence to the insurance companies appears to have a positive effect. Surprisingly, the only specific medical indication that is constantly associated with a positive response appears to be mechanical restrictions. Again, an objective list of physical symptoms that may lead to a positive outcome and universally adopted by insurance companies would be extremely helpful to the patients.
The mental suffering of morbidly obese patients pre- and post-bariatric surgery is generally unappreciated and underestimated. Denying patients body contouring surgery after bariatric surgery can add to their psychological stress and mental suffering.
We do not question that some body contouring procedures can be considered to be cosmetic. However, in the patients with massive weight loss the procedures have significant medical and functional benefits.
The authors received no financial support for the research, authorship and publication of this article.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
1. Sektionen Gesundheitsversorgung G der B. Bundesamt für Statistik . https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/determinanten/uebergewicht.html. Published 2018. Accessed September 23, 2019.
2. Buchwald H , Avidor Y , Braunwald E , Jensen MD , Pories W , Fahrbach K , et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004 Oct;292(14):1724–37. https://doi.org/10.1001/jama.292.14.1724
3. Ryan DH , Yockey SR . Weight Loss and Improvement in Comorbidity: differences at 5%, 10%, 15%, and Over. Curr Obes Rep. 2017 Jun;6(2):187–94. https://doi.org/10.1007/s13679-017-0262-y
4. Sioka E , Tzovaras G , Katsogridaki G , Bakalis V , Bampalitsa S , Zachari E , et al. Desire for Body Contouring Surgery After Laparoscopic Sleeve Gastrectomy. Aesthetic Plast Surg. 2015 Dec;39(6):978–84. https://doi.org/10.1007/s00266-015-0561-1
5. Mukherjee S , Kamat S , Adegbola S , Agrawal S . Funding for postbariatric body-contouring (bariplastic) surgery in England: a postcode lottery. Plast Surg Int. 2014;2014:153194. https://doi.org/10.1155/2014/153194
6. Ngaage LM , Rose J , Pace L , Kambouris AR , Rada EM , Kligman MD , et al. A Review of National Insurance Coverage of Post-bariatric Upper Body Lift. Aesthetic Plast Surg. 2019 Oct;43(5):1250–6. https://doi.org/10.1007/s00266-019-01420-7
7. Smith OJ , Hachach-Haram N , Greenfield M , Bystrzonowski N , Pucci A , Batterham RL , et al. Body contouring surgery and the maintenance of weight-loss following Roux-En-Y gastric bypass: A retrospective study. Aesthet Surg J. 2018 Feb;38(2):176–82. https://doi.org/10.1093/asj/sjx170
8. Kinzl JF , Traweger C , Trefalt E , Biebl W . Psychosocial consequences of weight loss following gastric banding for morbid obesity. Obes Surg. 2003 Feb;13(1):105–10. https://doi.org/10.1381/096089203321136683
9. Al-Hadithy N , Aditya H , Stewart K . Does the degree of ptosis predict the degree of psychological morbidity in bariatric patients undergoing reconstruction? Plast Reconstr Surg. 2014 Nov;134(5):942–50. https://doi.org/10.1097/PRS.0000000000000695
10. Gurunluoglu R . Insurance coverage criteria for panniculectomy and redundant skin surgery after bariatric surgery: why and when to discuss. Obes Surg. 2009 Apr;19(4):517–20. https://doi.org/10.1007/s11695-008-9752-z
11. Jiang L , Tian W , Wang Y , Rong J , Bao C , Liu Y , et al. Body mass index and susceptibility to knee osteoarthritis: a systematic review and meta-analysis. Joint Bone Spine. 2012 May;79(3):291–7. https://doi.org/10.1016/j.jbspin.2011.05.015
12. Sati S , Pandya S . Should a panniculectomy/abdominoplasty after massive weight loss be covered by insurance? Ann Plast Surg. 2008 May;60(5):502–4. https://doi.org/10.1097/SAP.0b013e31816fcac4
13. Mitchell JE , Crosby RD , Ertelt TW , Marino JM , Sarwer DB , Thompson JK , et al. The desire for body contouring surgery after bariatric surgery. Obes Surg. 2008 Oct;18(10):1308–12. https://doi.org/10.1007/s11695-008-9557-0
14. Gurunluoglu R . Panniculectomy and redundant skin surgery in massive weight loss patients: current guidelines and recommendations for medical necessity determination. Ann Plast Surg. 2008 Dec;61(6):654–7. https://doi.org/10.1097/SAP.0b013e3181788e63
15. Singh, Mr Masha MMS. Your Guide to Body Contouring Surgery after Weight Loss. British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS); 2014.
16. Human MSEO of H and . Guidelines for medical necessity determination for occupational therapy. Guidel Massachusetts Heal. 2011(January 29):5-7. http://www.mass.gov/?pageID=eohhs2terminal&L=6&L0=Home&L1=Provider&L2=Insurance+(including+MassHealth)&L3=MassHealth&L4=Guidelines+for+Clinical+Treatment&L5=Guidelines+for+Medical+Necessity+Determination&sid=Eeohhs2&b=terminalcontent&f=masshealth_provider
17. Guidelines M. Mahp guidelines for panniculectomy/abdominoplasty purpose: Guidel Mahp. 2017;(July 2011).
18. Health P. Medical Policy No. 91444-R7 Panniculectomy/abdominoplasty. Prior Heal. 2015;(Review date 8/17):1-3.
19. Pratt JH , Irons GB . Panniculectomy and abdominoplasty. Am J Obstet Gynecol. 1978 Sep;132(2):165–8. https://doi.org/10.1016/0002-9378(78)90919-5
20. Poyatos JV , Del Castillo JM , Sales BO , Vidal AA . Post-bariatric surgery body contouring treatment in the public health system: cost study and perception by patients. Plast Reconstr Surg. 2014 Sep;134(3):448–54. https://doi.org/10.1097/PRS.0000000000000428
21. Soldin M , Mughal M , Al-Hadithy N ; Department of Health; British association of Plastic, Reconstructive and Aesthetic Surgeons; Royal College of Surgeons England . National commissioning guidelines: body contouring surgery after massive weight loss. J Plast Reconstr Aesthet Surg. 2014 Aug;67(8):1076–81. https://doi.org/10.1016/j.bjps.2014.04.031
22. Ademi Z , Tomonaga Y , van Stiphout J , Glinz D , Gloy V , Raatz H , et al. Adaptation of cost-effectiveness analyses to a single country: the case of bariatric surgery for obesity and overweight. Swiss Med Wkly. 2018 Jun;148(June):w14626. https://doi.org/10.4414/smw.2018.14626
23. Coon D , Gusenoff JA , Kannan N , El Khoudary SR , Naghshineh N , Rubin JP . Body mass and surgical complications in the postbariatric reconstructive patient: analysis of 511 cases. Ann Surg. 2009 Mar;249(3):397–401. https://doi.org/10.1097/SLA.0b013e318196d0c6
24. Boustred AM , Dyer A , Mackay DR , Miraliakbari R , Hazard SW . Correlation of Complications of Body Contouring Surgery With Increasing Body Mass Index. Aesthetic Surg J. 2008;28.
25. Hasanbegovic E , Sørensen JA . Complications following body contouring surgery after massive weight loss: a meta-analysis. J Plast Reconstr Aesthet Surg. 2014 Mar;67(3):295–301. https://doi.org/10.1016/j.bjps.2013.10.031
26. Modarressi A , Balagué N , Huber O , Chilcott M , Pittet-Cuénod B . Plastic surgery after gastric bypass improves long-term quality of life. Obes Surg. 2013 Jan;23(1):24–30. https://doi.org/10.1007/s11695-012-0735-8