Paediatric and adolescent athletes in Switzerland: age-adapted proposals for pre-participation cardiovascular evaluation
DOI: https://doi.org/10.4414/SMW.2022.w30128
Maciej
Albińskiabc, Christian
Balmera, Matthias
Wilhelmd, Philippe
Meyere, Matthias
Gassa, Christian
Schmiedf, Andrea
Menafogliog, Susanne
Kriemlerh, Yvan
Mivelazi, Dominik
Stambachj, Mathieu
Saubadekl, Vincent
Gremeauxkm, Boris
Gojanovicno, Josep
Brugadap, Aaron
Baggishq, Vincent
Gabusrs
aDepartment of Paediatric Cardiology, University Children's Hospital Zurich, Zurich, Switzerland
bDivision of Paediatrics, Lausanne University Hospital, Lausanne, Switzerland
cDepartment of Paediatrics, Hôpital Riviera-Chablais, Rennaz, Switzerland
dDepartment of Cardiology, Cardiovascular Centre, Inselspital, Bern University Hospital, University of Bern, Switzerland
eService of Cardiology, Department of Medicine, Geneva University Hospitals, Geneva, Switzerland
f
Department of Cardiology, University Heart Center Zurich, University of Zurich, Zurich, Switzerland
g
Department of Cardiology, San Giovanni Hospital Bellinzona, Bellinzona, Switzerland
hEpidemiology, Biostatistics and Prevention Institute, University of Zurich, Zurich, Switzerland
i
Department of Woman-Mother-Child, Paediatric Cardiology Unit, Lausanne University Hospital, Lausanne, Switzerland
j
Paediatric Cardiology, Ostschweizer Kinderspital, St. Gallen, Switzerland
kSwiss Olympic Medical Center, Sports Medicine Unit, Lausanne University Hospital, Lausanne, Switzerland
l
Center for Primary Care and Public Health (Unisanté), University of Lausanne, Lausanne, Switzerland
mInstitute of Sport Sciences, University of Lausanne, Switzerland
n
Centre SportAdo, Woman-mother-child Department (DFME), Lausanne University and Hospital, Switzerland
oSwiss Olympic Medical Center, Hôpital de la Tour, Meyrin, Switzerland
pCardiovascular Institute, Hospital Clínic, Paediatric Arrhythmia Unit, Hospital Sant Joan de Déu, University of Barcelona, Spain
qDivision of Cardiology, Massachusetts General Hospital, Boston, Massachusetts, USA
rDepartment of Cardiology, Hôpital Riviera-Chablais, Rennaz, Switzerland
s
Department of Cardiology, Lausanne University Hospital, Lausanne, Switzerland
Summary
High-level sports competition is popular among Swiss youth. Even though preparticipation evaluation for competitive athletes is widespread, screening strategies for diseases responsible for sudden death during sport are highly variable. Hence, we sought to develop age-specific preparticipation cardiovascular evaluation (PPCE) proposals for Swiss paediatric and adolescent athletes (under 18 years of age). We recommend that all athletes practising in a squad with a training load of at least 6 hours per week should undergo PPCE based on medical history and physical examination from the age of 12 years on. Prior to 12 years, individual judgement of athletic performance is required. We suggest the inclusion of a standard 12-lead electrocardiogram (ECG) evaluation for all post-pubertal athletes (or older than 15 years) with analysis in accordance with the International Criteria for ECG Interpretation in Athletes. Echocardiography should not be a first-line screening tool but rather serve for the investigation of abnormalities detected by the above strategies. We recommend regular follow-up examinations, even for those having normal history, physical examination and ECG findings. Athletes with an abnormal history (including family history), physical examination and/or ECG should be further investigated and pathological findings discussed with a paediatric cardiologist. Importantly, the recommendations provided in this document are not intended for use among patients with congenital heart disease who require individualised care according to current guidelines.
Why screen paediatric and adolescent athletes?
The number of children and adolescents in Switzerland performing sports remains at a high level. According to the last federal sports report of the young from 2014, two thirds of the Swiss youth between 10 and 19 years of age are physically active for more than three hours per week and one third even for more than seven hours [1]. Cardiac adaptions to intensive exercise, termed “the athlete’s heart”, represent a benign physiological response to training [2]. However, distinguishing cardiac adaptions to sport from pathology remains challenging [3]. In presence of an underlying cardiac disease, sudden cardiac death (SCD) may occur. SCD remains the leading medical cause of death across all sports among young athletes (<35 years) with a strong male predominance [4]. Before implementation of a mandatory screening programme, athletes in the Italian region of Veneto had an increased risk of SCD compared with non-athletes [5]. The SCD incidence then decreased by 89% following implementation of preparticipation cardiovascular screening [6]. Data characterising the incidence of SCD among paediatric athletes are sparse despite the fact that a US-based sudden death registry reported 65% of all victims to be younger than 18 years [7].
In Switzerland, preparticipation evaluation has been performed for several years, promoting several aspects of the athlete’s health and wellbeing [8]. This review focuses on the cardiovascular part, termed preparticipation cardiovascular examination (PPCE). Nevertheless, we acknowledge the importance of a comprehensive screening of the young performing high level sports.
Proposal: Identification of individuals at risk of SCD is of paramount importance during the preparticipation cardiovascular evaluation (PPCE) of competitive athletes, not only in adults, but also in the paediatric/adolescent age range.
How to define the “paediatric/adolescent athlete”?
The development of a universally acceptable definition of paediatric and adolescent athletes presents numerous challenges. The term “athlete” refers to an individual who participates in competitive sports on a high level [9], but defining competitive sports performance under the age of 12 years may require individual judgement [9], as regular training can start from the age of six years [10]. However, general physical activity levels are higher in children than adults. The World Health Organization recommendation on physical activity in children advocates an average of 60 minutes daily, including at least three days a week of vigorous-intensity and strengthening activities [11]. Therefore, in order to differentiate paediatric and adolescent athletes from recreational “exercisers” and normally active children, we suggest including individuals practising in a squad with a training load of at least six hours of structured training per week beyond leisure activities. Intensive exercise for at least four hours a week induces adaptive cardiac changes in adults [3]. Limited data suggest that similar adaptations can be observed in adolescents [12].
Even though biological age determined by puberty stages according to Tanner [13, 14] is more appropriate than chronological age and should be used in the young athlete’s assessment, we suggest an upper cut-off age of 18 years for the definition of paediatric and adolescent athletes. The lower cut-off is based on the onset of athletic performance, as mentioned above [9].
Proposal: Paediatric/adolescent athletes (younger than 18 years) are defined by competitive sports participation on high level, practising in a squad for at least six hours per week.
Whom do we need to screen?
A key issue is the cut-off age for the implementation of PPCE in paediatric and adolescent athletes. SCD-related cardiac pathologies develop with age, resulting in a relatively low risk of SCD before puberty [15]. The incidence of SCD in the general population between 1 and 35 years of age in Australia and New Zealand was 1.3/100,000, with a nadir between 6 and 15 years. However, unexplained SCD (i.e., unidentified by comprehensive autopsy) peaked between 16 and 20 years [16]. Comparable data in Europe were found in Denmark [17] and Sweden [18]. Sports-related SCD rates are generally lower [19, 20]. Nevertheless, in a UK-based registry, the so-called “sudden arrhythmic death” accounted for more than half of all sports-related cases under 18 years [21]. This entity may be related to primary arrhythmias including genetic channelopathies and congenital pre-excitation that are detectable by 12-lead electrocardiography (ECG) [21]. Although PPCE in pre-pubertal paediatric athletes can detect occult disease associated with SCD, there are currently no data to support starting screening before puberty. The economic implications are considerable: in an Italian study, cost per diagnosis in PPCE was more than three times higher among children (7–11 years) than among adolescents (12–18 years) [15]. Due to the high variability between biological and chronological age in the process of puberty, notably between male and female athletes, it is practically impossible to set numerical cut-offs for paediatric and adolescent athletes. In order to distinguish pre- from post-pubertal athletes, we recommend evaluation of the biological age by the use of Tanner stages (table 1). Although we acknowledge that some may advocate PPCE at younger ages, we suggest starting screening from 12 years on with a medical history and physical examination, corresponding to the lower age range on regional level for Swiss Olympic Talent Card holders in most sports categories [22]. Prior to that age, athletic performance requires individual judgement [9]. We recommend the inclusion of a 12-lead ECG among athletes who are post-pubertal according to Tanner stages or from 15 years, corresponding to the starting age on national level for Swiss Olympic Talent Card holders in most sports categories [22].
Table 1Tanner stages evaluating maturity stages [13, 14].
|
Male
|
Female
|
| 1 |
No pubic hair |
No pubic hair |
| Testis of childhood size |
Elevated papilla |
| 2 |
Sparse, long hair |
Sparse, long hair |
| Testis enlarged |
Breast buds present |
| 3 |
Darker, curled hair |
Darker, curled hair |
| Penis enlarged |
Areolar diameter enlarged |
| 4 |
Small area of adult-type hair |
Small area of adult-type hair |
| Scrotum darkened |
Secondary mound |
| 5 |
Mature male |
Mature female |
The incidence of SCD is consistently higher for males in both the general population [16] and among competitive athletes [20, 23]. Despite an increasing participation of women in competitive sports, this gap persists [24]. The degree to which this sex difference is applicable to the paediatric and adolescent age range, remains to be definitively determined, although one UK-based study including children reported lower SCD rates among females than males [21]. However, an argument supporting ECG screening in females was shown in young Swiss females (<35 years), where the leading cause of SCD were cardiomyopathies that are potentially identifiable by 12-lead ECG [25]. As long as the impact of female sex on SCD risk in paediatric and adolescent athletes is not established, we recommend that male and female paediatric and adolescent competitive athletes be screened in an identical fashion.
Ethnicity also plays a role on SCD risk, as shown in the US, where African-American athletes and other non-Caucasian ethnicities demonstrate a nearly five-fold increased death rate compared with Caucasians [23]. In the absence of data defining markedly high-risk ethnic groups in Switzerland, we recommend equal screening policies in Swiss paediatric and adolescent athletes of all ethnicities.
Patients with congenital heart disease who wish to participate in competitive sports may be at the highest risk of SCD during exercise [26]. These patients require an individualised shared decision-making approach involving experts in paediatric cardiology, congenital heart disease and sports medicine. Importantly, regular exercise in accordance with physical activity guidelines is recommended for individuals with stable forms of congenital heart disease [27].
Proposal: From the age of 12 years on, we suggest screening by history and physical examination. Prior to this age, individual judgement of athletic performance is required. Post-pubertal athletes (or older than 15 years) should have ECG-inclusive PPCE, independently of sex and ethnicity. Patients with congenital heart disease should be managed individually by their attending paediatric cardiologist.
Which is the best screening tool?
Medical history and physical examination remain the cornerstones of PPCE. Importantly, standardised questionnaires such as the American Heart Association 14-Element Screening [28], the American Academy of Pediatrics 5th PPE Monograph [29] or equivalent should be used in order to ensure comprehensive and consistent evaluation, including blood pressure measurement (table 2). Importantly, any abnormal finding on history and/or physical examination including abnormal prior cardiovascular testing results and a positive family history including premature death (<50 years) and/or known genetic cardiomyopathy in a first degree relative requires further investigations, as suggested by large international guidelines [27, 30, 31].
Table 2Comprehensive evaluation by medical history and physical examination according to the American Heart Association 14-Element Screening (AHA-14) [28] or the American Academy of Pediatrics 5th PPE Monograph (5th PPE Monograph) [29].
|
AHA-14
|
5th PPE Monograph
|
| Personal History |
Exertional chest pain/discomfort |
Exertional chest pain/discomfort |
| Unexplained syncope or near-syncope |
Exertional syncope or near-syncope |
| Exertional dyspnoea/fatigue/palpitations |
Exertional tachycardia/palpitations |
| Priorly known heart murmur |
Priorly known cardiac disease |
| Elevated systemic blood pressure |
Exertional dyspnoea/numbness |
| Prior restriction from sports |
Prior seizure |
| Prior heart testing by a physician |
Prior heart testing by a physician |
| Family History |
Premature cardiac death in a relative (<50 years) |
Sudden death in a relative (<35 years) |
| Disability from heart disease in a relative (<50 years) |
Pacemaker or implanted defibrillator in a relative (<35 years) |
| Specific cardiac conditions in family members: hypertrophic or dilated cardiomyopathy, long-QT syndrome or other ion channelopathies, Marfan syndrome, clinically significant arrhythmias, genetic cardiac conditions |
Specific cardiac conditions in family members: hypertrophic or arrhythmogenic right ventricular cardiomyopathy, long-QT syndrome, short-QT syndrome, Marfan syndrome, Brugada syndrome, catecholaminergic polymorphic ventricular tachycardia |
| Physical Exam |
Heart murmur |
Heart murmur |
| Femoral pulses |
Pulse |
| Physical stigmata of Marfan syndrome |
Physical stigmata of Marfan syndrome |
| Brachial artery blood pressure |
Brachial artery blood pressure |
ECG has proven to increase sensitivity and negative predictive value for SCD-related cardiac pathologies in PPCE of athletes [32]. The European Society of Cardiology (ESC) recommends ECG as an inherent part of preparticipation screening [31]. Interestingly, although the American Heart Association (AHA) does not recommend routine ECG-inclusive screening, it still states that ECG “may be considered in relatively small cohorts of young healthy people 12 to 25 years of age” underlining the peculiarity of this age group [28]. ECG evaluation is currently widely used during PPCE among Swiss athletes (table 3). However, as described previously, the risk of SCD is lowest in individuals before they reach puberty [16]. Hence, instead of using a numerical cut-off for chronological age, we strongly recommend evaluation of the pubertal status of an athlete by the use of Tanner stages (table 1). This is particularly important when considering the earlier pubertal onset in females. Only if Tanner stages cannot be used for major reasons (self-determination, pudency, legal implications), we suggest a chronological cut-off of 15 years or older. Taken together, we recommend that ECG be considered standard of care for all post-pubertal athletes (or from 15 years on).
Table 3Current PPCE standards for major sport types in paediatric and adolescent athletes in Switzerland.
|
Sport type
|
Method
|
Starting age
|
Follow-up interval
|
| Football |
H&P 1×/year |
“junior elite” (≈ 14–16 years) |
At transfer to “elite” |
| ECG 1×/2 years |
| Unihockey* |
H&P 1×/2 years |
"U19" (17–18 years) |
1×/2 years |
| ECG 1×/2 years |
| Blood tests 1×/2 years |
| Ice Hockey |
H&P 1×/year |
"U17" (14–16 years) |
1×/year |
| ECG 1×/year |
| Swimming |
H&P 1×/year |
regional: boys: 13 years, girls: 12 years |
1×/year |
| national: boys: 15 years, girls: 14 years |
Echocardiographic screening in healthy adolescents with a mean age of 13 years demonstrated a 3.6% rate of previously unknown cardiac abnormalities of which the vast majority are not known to increase the risk of SCD during sports [33]. Several studies suggest that echocardiography does not provide any additional diagnostic value to medical history, physical examination and ECG during PPCE [34, 35]. In a study on Italian male paediatric football players, ECG proved to be a powerful diagnostic tool for detecting cardiomyopathies and identified all athletes requiring sports disqualification, thus limiting the value of echocardiography as first-line tool [36]. In line with current ESC and American Society of Echocardiography guidelines [27, 37], we suggest reserving echocardiography for second-line evaluation.
Proposal: PPCE relies on a comprehensive medical history and physical examination, as well as a 12-lead ECG in post-pubertal athletes (or from age 15 years).
Do we have appropriate ECG criteria for PPCE in paediatric and adolescent athletes?
Appropriate, age-specific criteria are required to differentiate benign, training-induced (“normal”) from potentially malignant, training-unrelated (“abnormal”) ECG findings. In 2016, Perrin et al. demonstrated a low prevalence (1.4%) of abnormal findings in a cohort of young Swiss athletes (≥14 years) including adults [38]. In the interim, ECG interpretation criteria for athletes have been revised and now achieve high values of specificity (93.0%) and sensitivity (95.9%) in adults [39].
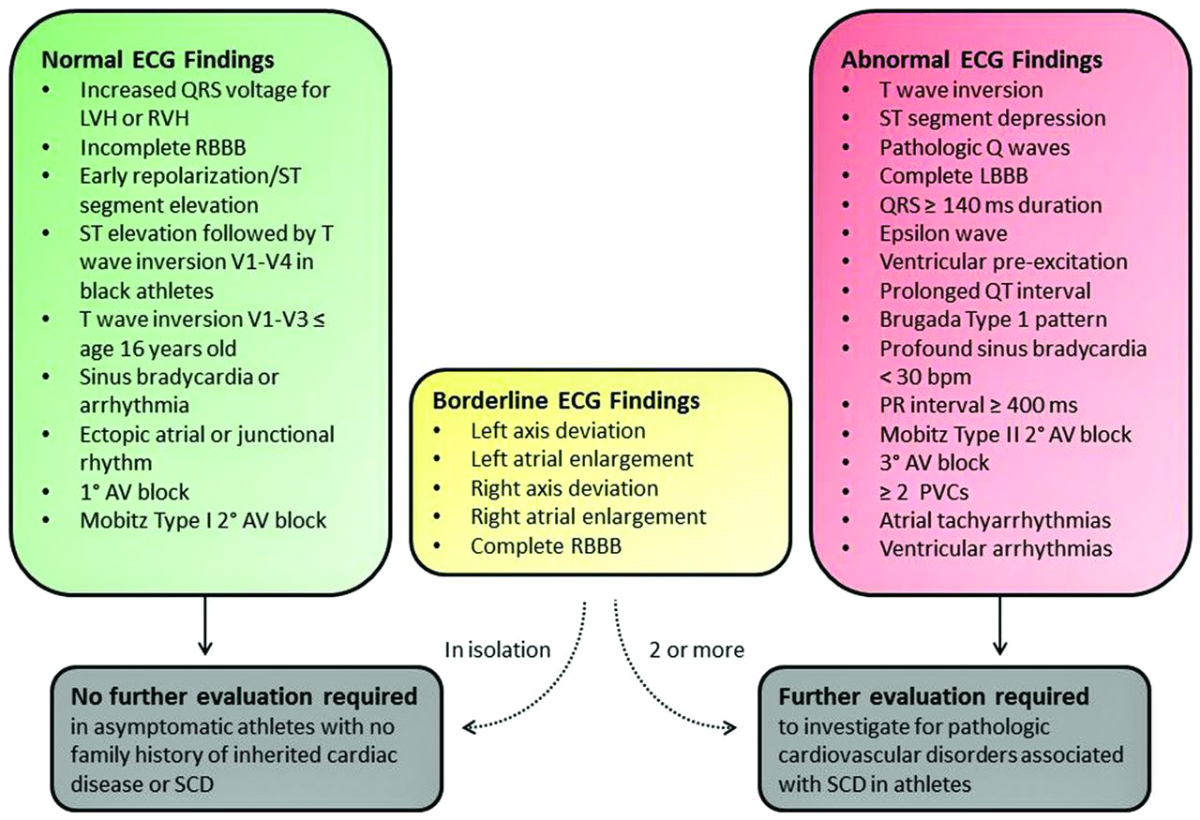
The latest version of athlete specific ECG interpretation criteria, the International Criteria for Electrocardiographic Interpretation in Athletes (2017) (fig. 1), were developed for use among asymptomatic athletes aged 12–35 years [30].
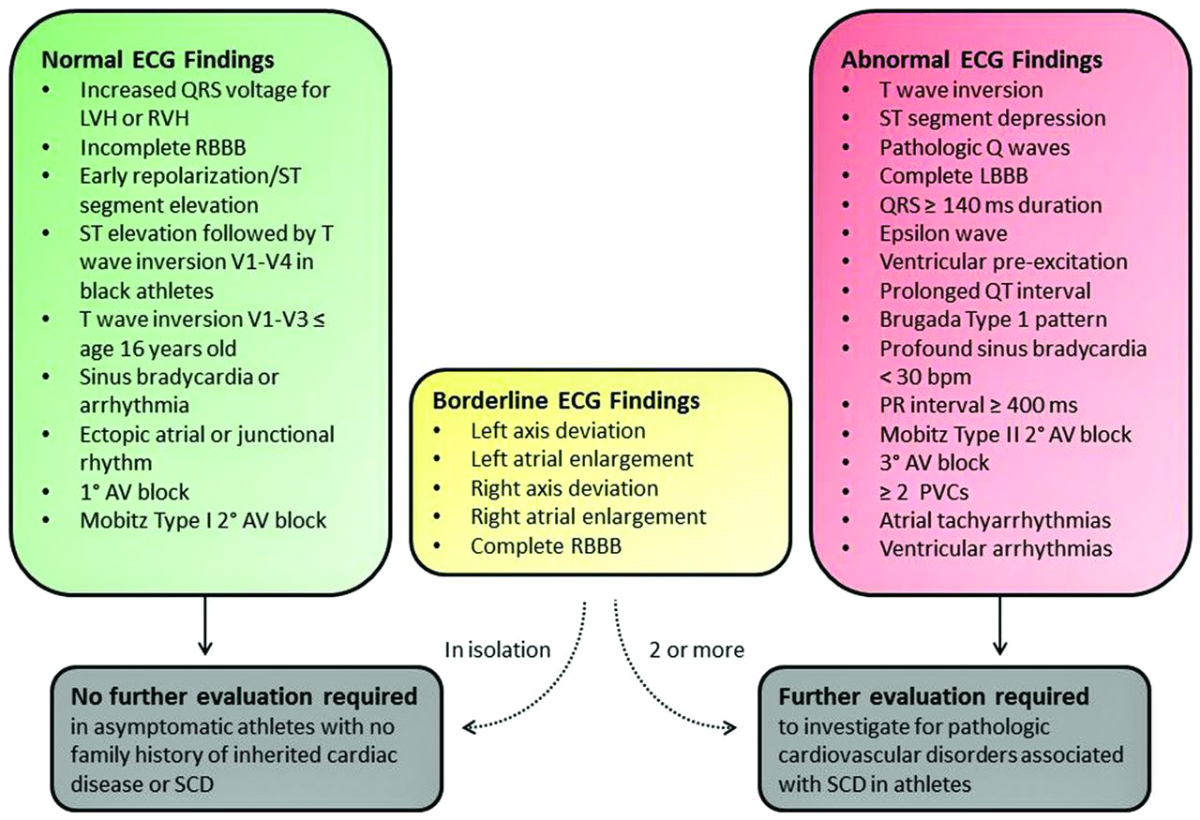
Figure 1 International consensus standards for ECG interpretation in athletes, reprinted with permission from: Drezner JA, Sharma S, Baggish A, Papadakis M, Wilson MG,
Prutkin JM, et al. International criteria for electrocardiographic interpretation
in athletes: consensus statement. Br J Sports Med.
2017 May;51(9):704–31 [30].
AV: atrioventricular; LBBB: left bundle branch block; LVH: left ventricular hypertrophy; PVC: premature ventricular contraction; RBBB: right bundle branch block; RVH: right ventricular hypertrophy; SCD: sudden cardiac death.
An initial study performed in paediatric athletes demonstrated only moderate values of diagnostic accuracy for these criteria [40]. However, this study was realised in Middle Eastern and African athletes, who are known to exhibit more abnormal findings on ECG [41]. Further, the diagnostic value of modern ECG interpretation standards highly depends on appropriately educated medical staff [42]. This implies a critical need for age-specific knowledge in ECG interpretation as part of paediatric and adolescent athletes’ screening, given the presence of specific paediatric electrocardiographic variants, such as isolated complete right bundle branch block in patients with Ebstein’s anomaly [43]. High inter-observer agreement using the International Criteria for Electrocardiographic Interpretation in Athletes was demonstrated in Swiss athletes [44]. Application of these criteria to 891 Swiss paediatric athletes from 45 different sports demonstrated a low rate (2.1%) of abnormal ECG findings [45], congruent to results from Italian male peri-pubertal football players [36]. A recent study in Caucasian paediatric athletes showed a low false-positive rate (2.2%) [43]. In sum, the International Criteria for Electrocardiographic Interpretation in Athletes appear to perform with sufficient accuracy to use among paediatric and adolescent athletes.
Proposal: The International Criteria for Electrocardiographic Interpretation in Athletes are appropriate to use in paediatric/adolescent athletes.
What is the cost of ECG-inclusive PPCE?
Frequently cited arguments against ECG-inclusive PPCE include enlarged financial burden and increased need for downstream testing to address ECG findings [46]. Paediatric athlete data from Switzerland revealed costs of CHF 103 per athlete for basic ECG-inclusive PPCE, which increased to CHF 116 when further investigations of abnormal findings were included [64]. PPCE without ECG reduced the costs from CHF 116 to CHF 72, owing to less expensive baseline screening and a lower rate of abnormal findings requiring further evaluation. However, large-scale trials in young athletes from the US and Italy demonstrated that ECG-inclusive PPCE was more cost-effective than history and physical examination alone [47]. Data from Italy in a mixed paediatric-adult population demonstrated costs of approximately EUR 80 per athlete, including second-line investigations [15]. This is comparable to figures from the UK and Canada [15]. Nevertheless, children had the highest cost per diagnosis because of the low disease prevalence in this age group [15].
Proposal: Costs for PPCE in Switzerland are comparable to other countries and seem appropriate to potentially decrease the SCD rate among young athletes.
What are the limits of PPCE?
The limits of one-time PPCE were demonstrated in a study among adolescent football players (n = 11,168; age = 16.4 ± 1.2 years; 95% male) from the UK screened by ECG and echocardiography [48]. First, there was a low prevalence (0.38%) of SCD-associated cardiac disorders diagnosed, of which 86% were identified by ECG, 29% by echocardiography and less than 10% by history and physical examination. Second, 2% of screened athletes had abnormal or borderline abnormal ECG findings for which no explanatory cardiac diagnosis could be established. This is similar to the results observed in a cohort of Swiss paediatric athletes [45]. Third, over a mean follow-up period of over 10 years, there were eight cases of SCD, resulting in an SCD incidence in screened athletes of 6.8 per 100,000 athletes. Out of the eight SCD victims, seven had a post-mortem diagnosis of cardiomyopathy. Importantly, six of the eight athletes had been cleared for sports participation on initial PPCE, suggesting subsequent emergence of phenotypic disease. Taken together, this study substantiates the critical need for follow-up screenings, as a one-time PPCE may miss individuals at risk of SCD. Even though only two thirds of SCDs manifest by abnormal ECG [31], ECG detects substantially more pathologies than medical history and physical examination alone, as presented in this large-scale study [48].
Proposal: The main limit of ECG-inclusive PPCE is a low prevalence (<1%) of findings with one single screening, highlighting the substantial need for follow-up ECGs.
Do we need follow-up examinations?
The heart continues to develop during childhood and adolescence with major developmental steps taking place during puberty [49]. This includes the phenotypic emergence of several cardiomyopathies. Whereas congenital cardiomyopathies such as Noonan syndrome [50], offspring of mothers suffering from diabetes [51] or related to metabolic disorders are usually diagnosed before and in part are only transient, two of the major cardiomyopathies with risk of SCD (hypertrophic and arrhythmogenic right ventricular cardiomyopathies) may manifest only after the onset of puberty [52]. One of the electrocardiographic findings of cardiomyopathies, a T-wave inversion in the anterior precordial leads, is considered a physiological (“juvenile pattern”) in athletes younger than 16 years [30]. Therefore, follow-up is of crucial importance in the screening process of paediatric and adolescent athletes. The best example is stated by the UK football players mentioned above [48]. Hence, the potential of relevant cardiovascular conditions to cause SCD in athletes and their emergence over time imply a need for regular follow-up. Furthermore, follow-up allows prevention of complications arising from pathologies without immediate risk of cardiac mortality [36]. Based on experience from professional football players in the UK, Speers et al. suggested follow-up at a maximum 2-year interval even for the lowest risk category with completely normal screening results [53]. As mentioned above, data on SCD in the paediatric age range are scarce. This implies a lack of evidence for exact determination of adequate follow-up intervals.
Proposal: Follow-up should be performed regularly because of the emergence of SCD-related pathologies over time, notably during growth of paediatric and adolescent athletes.
Athlete counselling and shared decision making
Even the best PPCE does not fully eliminate the remaining risk of SCD in athletes. Athletes and their caregivers should therefore be educated about the limitations of screening including the risk of false positive and false negative findings.
There are mounting data to suggest that numerous cardiac conditions previously associated with SCD indicate minimal and non-prohibitive risk during sport participation [54, 55]. Accordingly, clinicians are increasingly utilising shared decision-making models to educate patients about the risks and benefits of sport participation following a cardiac diagnosis. Examples include hypertrophic cardiomyopathy without any markers of increased risk [27], frequent ventricular arrhythmias with no underlying structural heart disease, asymptomatic Brugada syndrome or selected pacemaker/implantable cardioverter defibrillator carriers [15]. In the paediatric age range, there is a similar trend regarding simple shunting lesions or aortic stenosis [26]. This trend is of importance as many competitive athletes may choose to accept some levels of risk in order to continue participating in sport. However, we admit the legal peculiarities of this process, as illustrated previously [56]. Furthermore, the importance of self-determination and autonomy of adolescents, as well as the role of parents, should be considered. Hence, the long-term outcomes associated with shared decision making with the concerned athletes and their parents, both favourable and adverse, have yet to be documented and represent an important area of future research.
Following the 2019 COVID-19 pandemic, a number of considerations emerged on the resumption of high-level physical activity in general [57–59] and specifically for children and adolescents [60]. Furthermore,
Sport & Exercise Medicine Switzerland edited a specific flowchart for return to play after COVID-19 [61].
Proposal: Individualised counselling with shared decision making including parents’ advice and close follow-up may enable athletes with abnormal findings to continue their sport on a lower level considering their own benefit-harm balance.
Further efforts to prevent SCD in athletes
Prevention in the form of emergency action planning should extend beyond screening to encompass training in cardiopulmonary resuscitation and the use of an automated external defibrillator. The benefit of a prompt response is evidenced by data documenting that survival after sports-related sudden cardiac arrest is 1.7–2.7 more common than in the general population [34]. However, survival to hospital discharge in trained athletes with a median age of 17 years remained low at 25%, even though resuscitation was initiated within three minutes, compared with 3% when this time delay was longer [32].
Proposal: Other preventive measures such as resuscitation training and use of automated external defibrillator remain of paramount importance.
Swiss Paediatric Athletes Database (Swiss PAED)
In this rapidly evolving field, more data are required not only to elucidate the clinical implications of cardiac adaptation in pre-, peri- and post-pubertal athletes, but notably to identify markers of increased risk. Therefore, the national registry Swiss Paediatric Athletes ECG Database (Swiss PAED) was initiated as a collaborative project between paediatrics, paediatric cardiology, cardiology and sports medicine. It is anticipated that this registry will serve as a common platform for further research topics in this area. All stakeholders implied in the care for paediatric and adolescent athletes are encouraged to join this database for research purposes relevant to the safety of sports.
Proposal: The Swiss Paediatric Athletes ECG Database (Swiss PAED) will serve as national registry for athletes younger than 18 years.
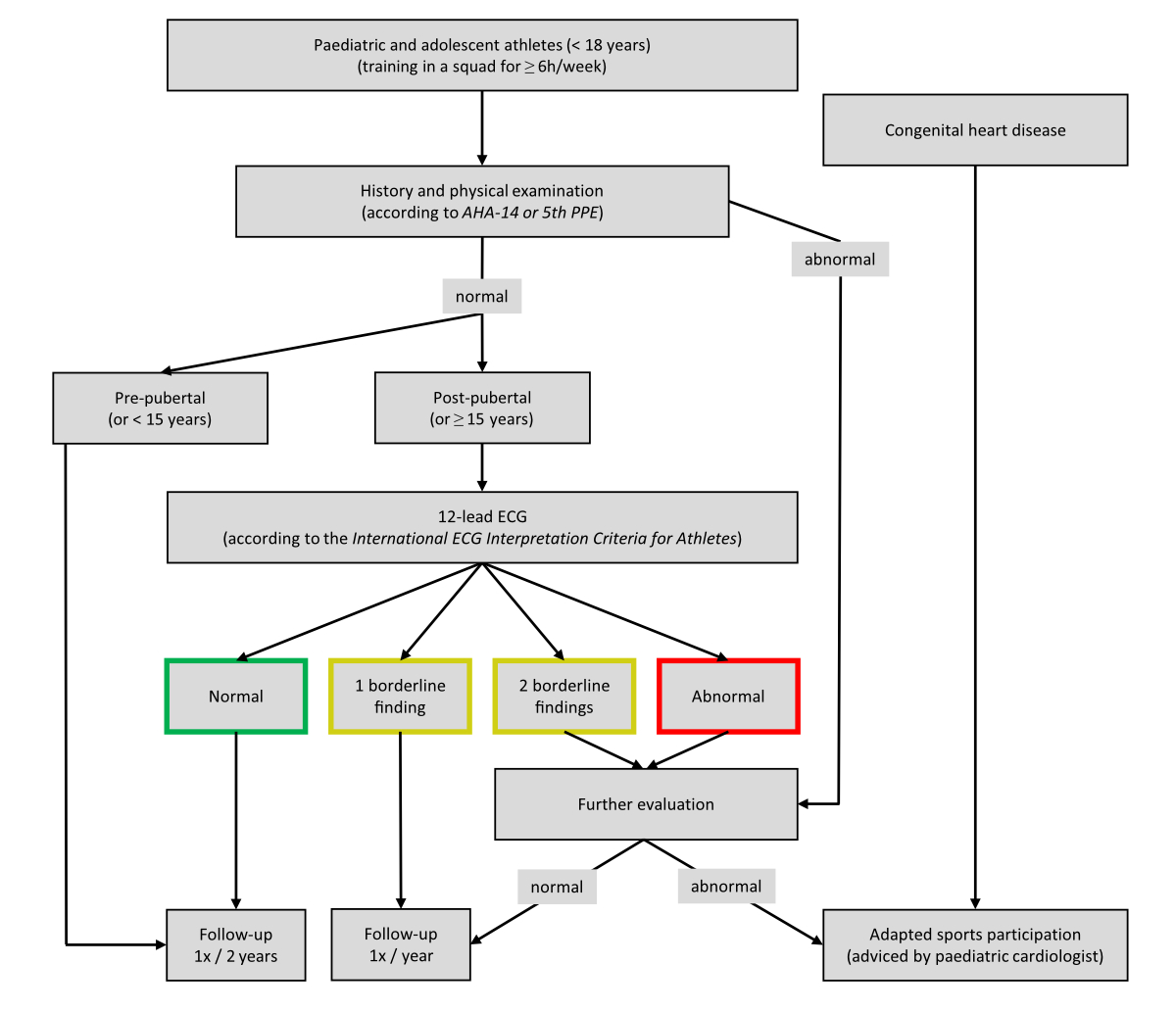
Suggested PPCE and follow-up algorithm
Based on the presented findings, we suggest an algorithm for PPCE and follow-up in paediatric and adolescent competitive athletes in Switzerland (fig. 2). We recommend screening of all athletes under 18 years of age with medical history and physical examination utilising comprehensive questionnaires, such as the American Heart Association 14-Element Screening [28] or the American Academy of Paediatrics 5th PPE Monograph [29]. Abnormal findings on history and physical examination should be further evaluated by a paediatric cardiologist, which may include an ECG if indicated. Among pre-pubertal athletes as measured by Tanner stages, or younger than 15 years, PPCE should be limited to history and physical examination and be conducted serially at 2-year intervals. Given the low incidence of SCD in pre-pubertal individuals, we suggest ECG-inclusive PPCE, using the International ECG Interpretation Criteria for Athletes [30] be applied in post-pubertal athletes according to Tanner stages, or from 15 years. Among athletes with normal ECG findings, we recommend repeat ECG-inclusive PPCE at 2-year intervals. In the case of an isolated borderline ECG finding, we suggest yearly follow-up including ECG. In cases of two borderline or any abnormal ECG finding, we recommend a comprehensive evaluation under the supervision of a paediatric cardiologist. Of note, the detailed investigation of these assessments must be individualised as a function of the nature of the suspected pathology and go beyond the scope of this article [30]. For athletes with abnormal ECG findings that are not found to have explanatory pathology after comprehensive evaluation, we recommend yearly follow-up to rule out the emergence of phenotypic cardiomyopathic disease [30]. Athletes with abnormal findings on further investigations are subject to treatment according to the ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease [27]. Depending on the type of pathology, limiting sports participation or even temporary restriction from athletic activity may be indicated as advised by a paediatric cardiologist and/or sports medicine physician [30]. As mentioned above, this document is not intended for use among patients with congenital heart disease who require individualised risk stratification and activity prescription under the supervision of a paediatric cardiologist. Of note, these proposals (table 4) are confined to how and when to perform the PPCE. Alternative screening topics including nutritional behaviour, psychological impact, substance abuse, etc. may best be approached by different strategies. For individuals older than 18 years, we suggest transition to adult sports cardiology institutions listed by Sport & Exercise Medicine Switzerland or the Swiss Working Group for Cardiovascular Prevention, Rehabilitation and Sports Cardiology.
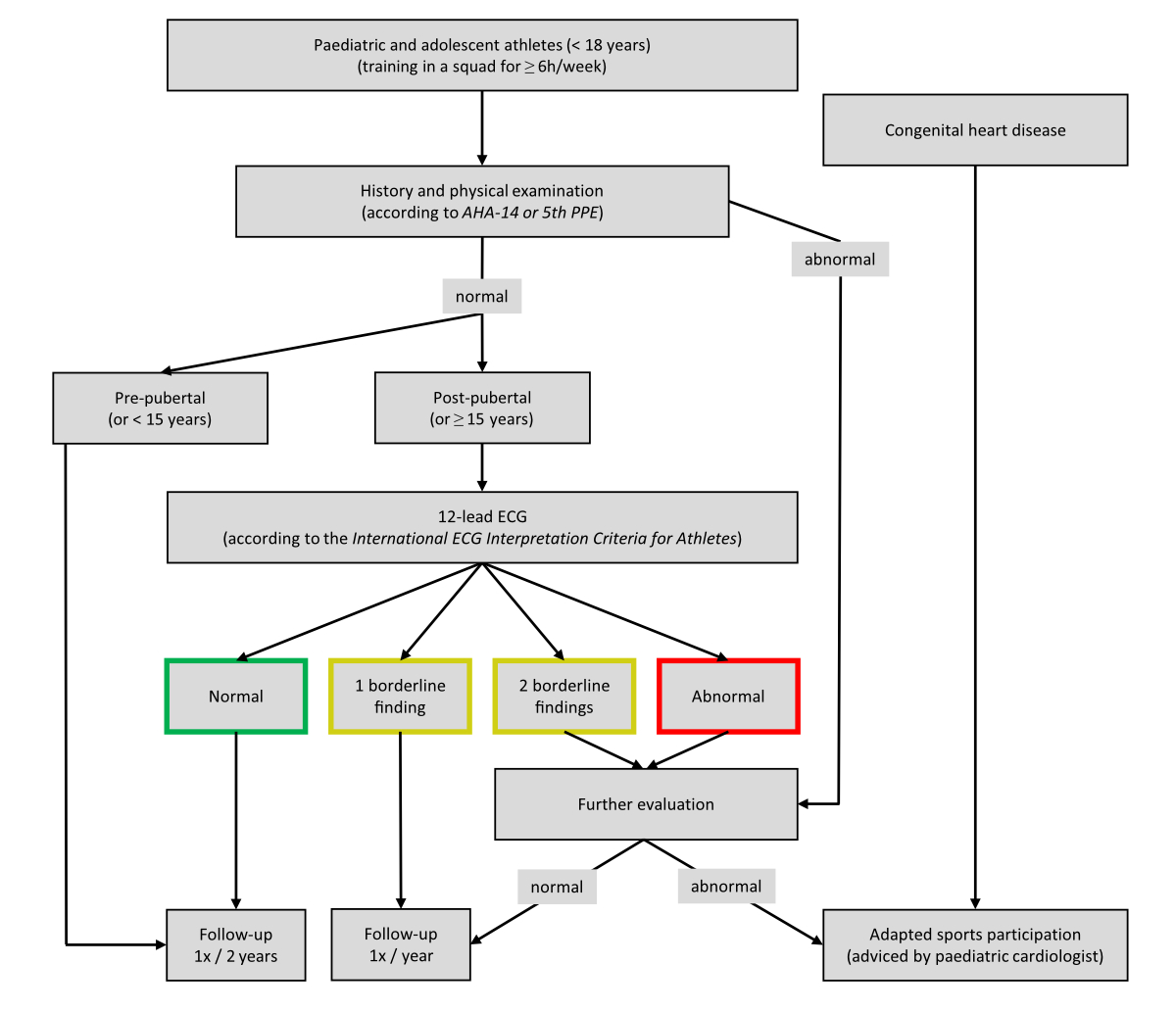
Figure 2 Preparticipation cardiovascular evaluation and follow-up algorithm for paediatric and adolescent athletes in Switzerland.
Table 4Overview of proposals for preparticipation evaluation in Swiss paediatric and adolescent athletes.
|
Issue
|
Proposal
|
| Indication |
Identification of paediatric/adolescent athletes at risk for SCD |
| Definition |
Competitive sports participation in a squad for at least 6h/week |
| Target group |
Under 18 years, any sex, any ethnicity, excluding patients with CHD |
| Methods |
Under 15 years: medical history and physical examination |
| From 15 years on: ECG-inclusive screening |
| ECG criteria |
International Criteria for Electrocardiographic Interpretation in Athletes
|
| Costs |
Comparable to other countries, appropriate to avoid SCD in the young |
| Limits |
Low prevalence of SCD requires regular follow-up |
| Follow-up |
Regularly due to emergence of pathologies over time and with growth |
| Counselling |
Individualised approach and shared decision-making |
| SCD prevention |
Resuscitation training and AED use on the field |
| Swiss PAED |
National electrocardiographic registry for athletes under 18 years |
Conclusion
Guidelines delineating PPCE among adults have evolved over several decades and now represent clinically accepted standard of care [31]. The use of routine ECG for screening remains the major controversy between the ESC approach [31] and American protocols [62]. With the development of new ECG criteria, identification of individuals at risk becomes more accurate [39]. In contrast, PPCE protocols for use among paediatric and adolescent aged athletes (< 18 years) have yet to be universally established. A first model was presented by the Association of European Paediatric Cardiology [63]. In our proposals, we precise the target group, analyse costs and limits and evolve the algorithm with a focus on follow-up and further investigations among paediatric and adolescent athletes in Switzerland (fig. 2).
Class of recommendation: IIa (should be considered)
Level of evidence: C (expert opinion)
Endorsed by the Swiss Society of Paediatric Cardiology, the Sport & Exercise Medicine Switzerland and the Swiss Working Group for Cardiovascular Prevention, Rehabilitation and Sports Cardiology (branch of the Swiss Society of Cardiology)
Acknowledgement
We thank Dr Roland Grossen (Swiss Football Association), Dr Gery Büsser (Swiss Ice Hockey Federation), Remo Manser (Swiss Unihockey) and David Burckhardt (Swiss Aquatics) for providing information regarding current screening procedures in their sports federations. Furthermore, we thank Mrs Staubli from the Children’s Hospital Zürich for graphical assistance.
Dr Maciej Albiński
Service de pédiatrie
Centre Hospitalier Universitaire Vaudois
Rue du Bugnon 46
CH-1011 Lausanne
maciej.albinski[at]chuv.ch
References
1.
Lamprecht M
,
Fischer, A.
,
Wiegand, D
&
Stamm, H.P.
(2015). Sport Schweiz 2014: Kinder- und Jugendbericht. Magglingen: Bundesamt für Sport BASPO.
2.
Morganroth J
,
Maron BJ
,
Henry WL
,
Epstein SE
. Comparative left ventricular dimensions in trained athletes. Ann Intern Med. 1975 Apr;82(4):521–4. https://doi.org/10.7326/0003-4819-82-4-521
3.
Merghani A
,
Malhotra A
,
Sharma S
. The U-shaped relationship between exercise and cardiac morbidity. Trends Cardiovasc Med. 2016 Apr;26(3):232–40. https://doi.org/10.1016/j.tcm.2015.06.005
4.
Maron BJ
. Sudden death in young athletes. N Engl J Med. 2003 Sep;349(11):1064–75. https://doi.org/10.1056/NEJMra022783
5.
Corrado D
,
Basso C
,
Rizzoli G
,
Schiavon M
,
Thiene G
. Does sports activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol. 2003 Dec;42(11):1959–63. https://doi.org/10.1016/j.jacc.2003.03.002
6.
Corrado D
,
Basso C
,
Pavei A
,
Michieli P
,
Schiavon M
,
Thiene G
. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006 Oct;296(13):1593–601. https://doi.org/10.1001/jama.296.13.1593
7.
Maron BJ
,
Doerer JJ
,
Haas TS
,
Tierney DM
,
Mueller FO
. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation. 2009 Mar;119(8):1085–92. https://doi.org/10.1161/CIRCULATIONAHA.108.804617
8.
Kriemler S BD
,
Camathias C
,
Hasler C
,
Schmid C
,
Stambach D
,
Gojanovic B
. Annual preparticipation examination in youth athletes. Sport and Exercise Medicine Switzerland journal. 2019.
9.
Maron BJ
,
Zipes DP
. Introduction: eligibility recommendations for competitive athletes with cardiovascular abnormalities-general considerations. J Am Coll Cardiol. 2005 Apr;45(8):1318–21. https://doi.org/10.1016/j.jacc.2005.02.006
10.
Pieles GE
,
Stuart AG
. The adolescent athlete’s heart; A miniature adult or grown-up child? Clin Cardiol. 2020 Aug;43(8):852–62. https://doi.org/10.1002/clc.23417
11.
WorldHealthOrganisation
. Physical activity. 2020.
12.
Churchill TW
,
Groezinger E
,
Loomer G
,
Baggish AL
. Exercise-induced cardiac remodeling during adolescence. Eur J Prev Cardiol. 2020 Dec;27(19):2148–50. https://doi.org/10.1177/2047487319869691
13.
Marshall WA
,
Tanner JM
. Variations in pattern of pubertal changes in girls. Arch Dis Child. 1969 Jun;44(235):291–303. https://doi.org/10.1136/adc.44.235.291
14.
Marshall WA
,
Tanner JM
. Variations in the pattern of pubertal changes in boys. Arch Dis Child. 1970 Feb;45(239):13–23. https://doi.org/10.1136/adc.45.239.13
15.
Vessella T
,
Zorzi A
,
Merlo L
,
Pegoraro C
,
Giorgiano F
,
Trevisanato M
, et al.
The Italian preparticipation evaluation programme: diagnostic yield, rate of disqualification and cost analysis. Br J Sports Med. 2020 Feb;54(4):231–7. https://doi.org/10.1136/bjsports-2018-100293
16.
Bagnall RD
,
Weintraub RG
,
Ingles J
,
Duflou J
,
Yeates L
,
Lam L
, et al.
A Prospective Study of Sudden Cardiac Death among Children and Young Adults. N Engl J Med. 2016 Jun;374(25):2441–52. https://doi.org/10.1056/NEJMoa1510687
17.
Winkel BG
,
Risgaard B
,
Sadjadieh G
,
Bundgaard H
,
Haunsø S
,
Tfelt-Hansen J
. Sudden cardiac death in children (1-18 years): symptoms and causes of death in a nationwide setting. Eur Heart J. 2014 Apr;35(13):868–75. https://doi.org/10.1093/eurheartj/eht509
18.
Wisten A
,
Krantz P
,
Stattin EL
. Sudden cardiac death among the young in Sweden from 2000 to 2010: an autopsy-based study. Europace. 2017 Aug;19(8):1327–34.
19.
Landry CH
,
Connelly KA
,
Dorian P
. Cardiac Arrest during Competitive Sports. N Engl J Med. 2018 Apr;378(15):1464–5.
20.
Wisten A
,
Börjesson M
,
Krantz P
,
Stattin EL
. Exercise related sudden cardiac death (SCD) in the young - Pre-mortal characterization of a Swedish nationwide cohort, showing a decline in SCD among athletes. Resuscitation. 2019 Nov;144:99–105. https://doi.org/10.1016/j.resuscitation.2019.09.022
21.
Finocchiaro G
,
Papadakis M
,
Robertus JL
,
Dhutia H
,
Steriotis AK
,
Tome M
, et al.
Etiology of Sudden Death in Sports: Insights From a United Kingdom Regional Registry. J Am Coll Cardiol. 2016 May;67(18):2108–15. https://doi.org/10.1016/j.jacc.2016.02.062
22.
SwissOlympic
. Card Report 2020. 2020.
23.
Maron BJ
,
Haas TS
,
Ahluwalia A
,
Murphy CJ
,
Garberich RF
. Demographics and Epidemiology of Sudden Deaths in Young Competitive Athletes: From the United States National Registry. Am J Med. 2016 Nov;129(11):1170–7. https://doi.org/10.1016/j.amjmed.2016.02.031
24.
Colombo CS
,
Finocchiaro G
. The Female Athlete’s Heart: facts and Fallacies. Curr Treat Options Cardiovasc Med. 2018 Nov;20(12):101. https://doi.org/10.1007/s11936-018-0699-7
25.
Asatryan B
,
Vital C
,
Kellerhals C
,
Medeiros-Domingo A
,
Gräni C
,
Trachsel LD
, et al.
Sports-related sudden cardiac deaths in the young population of Switzerland. PLoS One. 2017 Mar;12(3):e0174434. https://doi.org/10.1371/journal.pone.0174434
26.
Van Hare GF
,
Ackerman MJ
,
Evangelista JA
,
Kovacs RJ
,
Myerburg RJ
,
Shafer KM
, et al.; American Heart Association Electrocardiography and Arrhythmias Committee of Council on Clinical Cardiology, Council on Cardiovascular Disease in Young, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, and American College of Cardiology
. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 4: Congenital Heart Disease: A Scientific Statement From the American Heart Association and American College of Cardiology. Circulation. 2015 Dec;132(22):e281–91. https://doi.org/10.1161/CIR.0000000000000240
27.
Pelliccia A
,
Sharma S
,
Gati S
,
Bäck M
,
Börjesson M
,
Caselli S
, et al.; ESC Scientific Document Group
. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021 Jan;42(1):17–96. https://doi.org/10.1093/eurheartj/ehaa605
28.
Maron BJ
,
Friedman RA
,
Kligfield P
,
Levine BD
,
Viskin S
,
Chaitman BR
, et al.; American Heart Association Council on Clinical Cardiology, Advocacy Coordinating Committee, Council on Cardiovascular Disease in the Young, Council on Cardiovascular Surgery and Anesthesia, Council on Epidemiology and Prevention, Council on Functional Genomics and Translational Biology, Council on Quality of Care and Outcomes Research, and American College of Cardiology
. Assessment of the 12-lead ECG as a screening test for detection of cardiovascular disease in healthy general populations of young people (12-25 Years of Age): a scientific statement from the American Heart Association and the American College of Cardiology. Circulation. 2014 Oct;130(15):1303–34. https://doi.org/10.1161/CIR.0000000000000025
29.
American Academy of Family Physicians AAoP, American College of Sports Medicine, American Medical Society for Sports Medicine, American Orthopaedic Society for Sports Medicine, American Osteopathic Academy of Sports Medicine
. 5th edn. Preparticipation physical evaluation. American Academy of Pediatrics. 2019.
30.
Drezner JA
,
Sharma S
,
Baggish A
,
Papadakis M
,
Wilson MG
,
Prutkin JM
, et al.
International criteria for electrocardiographic interpretation in athletes: consensus statement. Br J Sports Med. 2017 May;51(9):704–31. https://doi.org/10.1136/bjsports-2016-097331
31.
Mont L
,
Pelliccia A
,
Sharma S
,
Biffi A
,
Borjesson M
,
Brugada Terradellas J
, et al.; Reviewers
. Pre-participation cardiovascular evaluation for athletic participants to prevent sudden death: position paper from the EHRA and the EACPR, branches of the ESC. Endorsed by APHRS, HRS, and SOLAECE. Eur J Prev Cardiol. 2017 Jan;24(1):41–69. https://doi.org/10.1177/2047487316676042
32.
DeFroda SF
,
McDonald C
,
Myers C
,
Cruz AI
,
Owens BD
,
Daniels AH
. Sudden Cardiac Death in the Adolescent Athlete: History, Diagnosis, and Prevention. Am J Med. 2019 Dec;132(12):1374–80. https://doi.org/10.1016/j.amjmed.2019.05.025
33.
Steinberger J
,
Moller JH
,
Berry JM
,
Sinaiko AR
. Echocardiographic diagnosis of heart disease in apparently healthy adolescents. Pediatrics. 2000 Apr;105(4 Pt 1):815–8. https://doi.org/10.1542/peds.105.4.815
34.
Berge HM
,
Andersen TE
,
Bahr R
. Cardiovascular incidents in male professional football players with negative preparticipation cardiac screening results: an 8-year follow-up. Br J Sports Med. 2019 Oct;53(20):1279–84. https://doi.org/10.1136/bjsports-2018-099845
35.
Magalski A
,
McCoy M
,
Zabel M
,
Magee LM
,
Goeke J
,
Main ML
, et al.
Cardiovascular screening with electrocardiography and echocardiography in collegiate athletes. Am J Med. 2011 Jun;124(6):511–8. https://doi.org/10.1016/j.amjmed.2011.01.009
36.
Calò L
,
Martino A
,
Tranchita E
,
Sperandii F
,
Guerra E
,
Quaranta F
, et al.
Electrocardiographic and echocardiographic evaluation of a large cohort of peri-pubertal soccer players during pre-participation screening. Eur J Prev Cardiol. 2019 Sep;26(13):1444–55. https://doi.org/10.1177/2047487319826312
37.
Baggish AL
,
Battle RW
,
Beaver TA
,
Border WL
,
Douglas PS
,
Kramer CM
, et al.
Recommendations on the Use of Multimodality Cardiovascular Imaging in Young Adult Competitive Athletes: A Report from the American Society of Echocardiography in Collaboration with the Society of Cardiovascular Computed Tomography and the Society for Cardiovascular Magnetic Resonance. J Am Soc Echocardiogr. 2020 May;33(5):523–49. https://doi.org/10.1016/j.echo.2020.02.009
38.
Perrin T
,
Trachsel LD
,
Schneiter S
,
Menafoglio A
,
Albrecht S
,
Pirrello T
, et al.
Prevalence of abnormal electrocardiograms in Swiss elite athletes detected with modern screening criteria. Swiss Med Wkly. 2016 Dec;146:w14376. https://doi.org/10.4414/smw.2016.14376
39.
Zorzi A
,
Calore C
,
Vio R
,
Pelliccia A
,
Corrado D
. Accuracy of the ECG for differential diagnosis between hypertrophic cardiomyopathy and athlete’s heart: comparison between the European Society of Cardiology (2010) and International (2017) criteria. Br J Sports Med. 2018 May;52(10):667–73. https://doi.org/10.1136/bjsports-2016-097438
40.
McClean G
,
Riding NR
,
Pieles G
,
Watt V
,
Adamuz C
,
Sharma S
, et al.
Diagnostic accuracy and Bayesian analysis of new international ECG recommendations in paediatric athletes. Heart. 2019 Jan;105(2):152–9. https://doi.org/10.1136/heartjnl-2018-313466
41.
Riding NR
,
Sheikh N
,
Adamuz C
,
Watt V
,
Farooq A
,
Whyte GP
, et al.
Comparison of three current sets of electrocardiographic interpretation criteria for use in screening athletes. Heart. 2015 Mar;101(5):384–90. https://doi.org/10.1136/heartjnl-2014-306437
42.
MacLachlan H
,
Drezner JA
. Cardiac evaluation of young athletes: time for a risk-based approach? Clin Cardiol. 2020 Aug;43(8):906–14. https://doi.org/10.1002/clc.23364
43.
Halasz G
,
Cattaneo M
,
Piepoli M
,
Romano S
,
Biasini V
,
Menafoglio A
, et al.
Pediatric athletes’ ECG and diagnostic performance of contemporary ECG interpretation criteria. Int J Cardiol. 2021 Jul;335:40–6. https://doi.org/10.1016/j.ijcard.2021.04.019
44.
Schneiter S
,
Trachsel LD
,
Perrin T
,
Albrecht S
,
Pirrello T
,
Eser P
, et al.
Inter-observer agreement in athletes ECG interpretation using the recent international recommendations for ECG interpretation in athletes among observers with different levels of expertise. PLoS One. 2018 Nov;13(11):e0206072. https://doi.org/10.1371/journal.pone.0206072
45.
Albiński M
,
Saubade M
,
Benaim C
,
Menafoglio A
,
Meyer P
,
Capelli B
, et al.
Impact of early sports specialisation on paediatric ECG. Scand J Med Sci Sports. 2021 Jun;31(6):1335–41. https://doi.org/10.1111/sms.13942
46.
Franklin BA
,
Thompson PD
,
Al-Zaiti SS
,
Albert CM
,
Hivert MF
,
Levine BD
, et al.; American Heart Association Physical Activity Committee of the Council on Lifestyle and Cardiometabolic Health; Council on Cardiovascular and Stroke Nursing; Council on Clinical Cardiology; and Stroke Council
. Exercise-Related Acute Cardiovascular Events and Potential Deleterious Adaptations Following Long-Term Exercise Training: Placing the Risks Into Perspective-An Update: A Scientific Statement From the American Heart Association. Circulation. 2020 Mar;141(13):e705–36. https://doi.org/10.1161/CIR.0000000000000749
47.
Papadakis M
,
Sharma S
. Electrocardiographic screening in athletes: the time is now for universal screening. Br J Sports Med. 2009 Sep;43(9):663–8. https://doi.org/10.1136/bjsm.2008.054874
48.
Malhotra A
,
Dhutia H
,
Finocchiaro G
,
Gati S
,
Beasley I
,
Clift P
, et al.
Outcomes of Cardiac Screening in Adolescent Soccer Players. N Engl J Med. 2018 Aug;379(6):524–34. https://doi.org/10.1056/NEJMoa1714719
49.
Guasch E
,
Mont L
. Endurance training in young athletes: what happens in childhood, stays in childhood? Eur J Prev Cardiol. 2019 Dec;26(18):1998–2000. https://doi.org/10.1177/2047487319871649
50.
Gelb BD
,
Roberts AE
,
Tartaglia M
. Cardiomyopathies in Noonan syndrome and the other RASopathies. Prog Pediatr Cardiol. 2015 Jul;39(1):13–9. https://doi.org/10.1016/j.ppedcard.2015.01.002
51.
Øyen N
,
Diaz LJ
,
Leirgul E
,
Boyd HA
,
Priest J
,
Mathiesen ER
, et al.
Prepregnancy Diabetes and Offspring Risk of Congenital Heart Disease: A Nationwide Cohort Study. Circulation. 2016 Jun;133(23):2243–53. https://doi.org/10.1161/CIRCULATIONAHA.115.017465
52.
Migliore F
,
Zorzi A
,
Michieli P
,
Perazzolo Marra M
,
Siciliano M
,
Rigato I
, et al.
Prevalence of cardiomyopathy in Italian asymptomatic children with electrocardiographic T-wave inversion at preparticipation screening. Circulation. 2012 Jan;125(3):529–38. https://doi.org/10.1161/CIRCULATIONAHA.111.055673
53.
Speers C
,
Seth AN
,
Patel KC
,
Rakhit DJ
,
Gillett MJ
. Defining the Process of a Cardiovascular Risk Assessment Program: Lessons Learnt From Cardiac Assessment of Elite Soccer Players in the United Kingdom. Clin J Sport Med. 2017;Publish Ahead of Print. https://doi.org/10.1097/JSM.0000000000000534
54.
Johnson JN
,
Ackerman MJ
. Return to play? Athletes with congenital long QT syndrome. Br J Sports Med. 2013 Jan;47(1):28–33. https://doi.org/10.1136/bjsports-2012-091751
55.
Pelliccia A
,
Lemme E
,
Maestrini V
,
Di Paolo FM
,
Pisicchio C
,
Di Gioia G
, et al.
Does Sport Participation Worsen the Clinical Course of Hypertrophic Cardiomyopathy? Clinical Outcome of Hypertrophic Cardiomyopathy in Athletes. Circulation. 2018 Jan;137(5):531–3. https://doi.org/10.1161/CIRCULATIONAHA.117.031725
56.
https://www.reuters.com/article/us-olympics-triathlon-gomez-idUSL0380004820080625
57.
Baggish A
,
Drezner JA
,
Kim J
,
Martinez M
,
Prutkin JM
. Resurgence of sport in the wake of COVID-19: cardiac considerations in competitive athletes. Br J Sports Med. 2020 Oct;54(19):1130–1. https://doi.org/10.1136/bjsports-2020-102516
58.
Baggish AL
,
Levine BD
. Icarus and Sports After COVID 19: Too Close to the Sun? Circulation. 2020 Aug;142(7):615–7. https://doi.org/10.1161/CIRCULATIONAHA.120.048335
59.
Kim JH
,
Levine BD
,
Phelan D
,
Emery MS
,
Martinez MW
,
Chung EH
, et al.
Coronavirus Disease 2019 and the Athletic Heart: Emerging Perspectives on Pathology, Risks, and Return to Play. JAMA Cardiol. 2021 Feb;6(2):219–27. https://doi.org/10.1001/jamacardio.2020.5890
60.
https://sems-journal.ch/10717
61.
https://sems.ch/fileadmin/user_upload/Covid-19_Flow-Charts/COVID19_Flowcharts_DE_060421.pdf
62.
Maron BJ
,
Levine BD
,
Washington RL
,
Baggish AL
,
Kovacs RJ
,
Maron MS
; American Heart Association Electrocardiography and Arrhythmias Committee of Council on Clinical Cardiology, Council on Cardiovascular Disease in Young, Council on Cardiovascular and Stroke Nursing, Council on Functional Genomics and Translational Biology, and American College of Cardiology
. Eligibility and Disqualification Recommendations for Competitive Athletes With Cardiovascular Abnormalities: Task Force 2: Preparticipation Screening for Cardiovascular Disease in Competitive Athletes: A Scientific Statement From the American Heart Association and American College of Cardiology. Circulation. 2015 Dec;132(22):e267–72.
63.
Fritsch P
,
Ehringer-Schetitska D
,
Dalla Pozza R
,
Jokinen E
,
Herceg-Cavrak V
,
Hidvegi E
, et al.; European Paediatric Cardiology Working Group Cardiovascular Prevention
. Cardiovascular pre-participation screening in young athletes: Recommendations of the Association of European Paediatric Cardiology. Cardiol Young. 2017 Nov;27(9):1655–60. https://doi.org/10.1017/S1047951117001305
64.
Albiński M
,
Saubade M
,
Menafoglio A
,
Meyer P
,
Capelli B
,
Perrin T
, et al.
Diagnostic yield and cost analysis of electrocardiographic screening in Swiss paediatric athletes. J Sci Med Sport. 2021 Nov 18;S1440-2440(21)00516-8. doi: https://doi.org/10.1016/j.jsams.2021.11.039.