Ineffectiveness and unlikelihood of benefit: dealing with the concept of futility in medicine
DOI: https://doi.org/10.4414/SMW.2021.w30121
Swiss Academy of Medical Sciences
This document is available in English, French and German, cf.
https://www.sams.ch/en/Ethics/Topics-A-to-Z/Futility-in-medicine.html
. The German text is the authentic version.
1. Introduction
Any treatment should be based on the fundamental ethical values of good medical practice, including, for example, respect for patient autonomy and the principles of beneficence and non-maleficence. Also relevant are considerations of equity, e.g. in the form of the requirement that treatment is to be provided with equal care for all patients, irrespective of sex, ethnicity, social or economic status, worldview or religion.1 In everyday clinical practice, it is not always easy to observe these ethical principles. For example, medical professionals often feel obliged to offer and carry out treatments which, in their view, run counter to the patient’s welfare.2,3
Such behaviour may be attributable to various factors,4 such as:
- expectations or pressure from patients and relatives;
- a desire to avoid awkward conversations (“It’s easier just to carry on”);
-
“carrying on” because a treatment error/complication has occurred;
-
“carrying on” so that the efforts already undertaken should not have been in vain;
-
confrontation with the limits of medicine: “saving life at all costs”;
-
defensive medicine: fear of missing something, concerns about legal consequences;
-
economic interests, supply-induced overtreatment, etc.
Treatments which are ineffective or offer little or no likelihood of benefit, as well as unnecessary diagnostic investigations, do more harm than good: they do not improve quality of life or increase survival. They are not sustainable, and they tie up resources which may then not be available for other patients. This was the starting point for the “Choosing Wisely Switzerland” initiative5 launched by the Swiss Academy of Medical Sciences (SAMS) and the Swiss Society of General Internal Medicine (SSGIM). Essentially, the aim is to avoid ineffective measures – often involving overdiagnosis or overtreatment. Accordingly, various medical societies and the Swiss Association for Nursing Science have issued so-called Top-5 lists, specifying interventions which are evidently unnecessary and are thus to be avoided. The considerations given below follow on from this initiative. They explore the question of when it is justifiable to withhold or withdraw treatment from a patient. These matters are discussed under the overall heading of “futility” – a concept which, together with its content, continues to be a source of controversy; the present paper is intended to help clarify the issues.
In the medical context, futility refers to treatments which are ineffective and/or offer little or no likelihood of benefit. In principle, futility may also be discussed in relation to diagnostic investigations, particularly if such investigations have adverse effects on quality of life. In everyday clinical practice, however, attention is focused on the question of the benefits provided by treatments. For this reason, the present recommendations are primarily concerned with treatment decisions.
It is a matter of controversy to what extent assessments of futility are based on evidence and experience, and to what extent they are determined by value judgements. If a subjective dimension is admitted, the question arises who is entitled to make such value judgements and on what grounds. During the COVID-19 pandemic, discussions concerning the limits of medical expertise have intensified. Switzerland, like many other countries, has issued triage guidelines6 specifying which patients, under conditions of resource scarcity, are to be assigned priority – or considered eligible – for intensive care.7 In focusing on the short-term survival prognosis, the Swiss guidelines are based on the principle of benefit maximisation. The moral conflict arises when decisions are made as to which patients are not to receive treatment, even though they could possibly benefit from it. The guidelines gave rise to a debate as to what criteria it is permissible and justifiable to apply when decisions have to be made concerning the initiation or withdrawal of treatment. Also relevant in this context is the role to be played by the concept of medical futility.
Based on the guidelines of the SAMS, the following discussion seeks to elucidate the concept of futility and to determine how it relates not only to ineffectiveness and unlikelihood of benefit but also to the establishment of a medical indication.
2. SAMS medical-ethical guidelines
In SAMS medical-ethical guidelines – for example, those on “Management of dying and death” or “Decisions on cardiopulmonary resuscitation” – references to treatments which are no longer appropriate or offer little likelihood of benefit are generally made in connection with severe illness. In the guidelines on “Intensive-care interventions”,8 a distinction is drawn between treatments which are ineffective and those which offer little or no likelihood of benefit.9 A treatment is described as ineffective if the defined treatment goal cannot be attained, even though a short-term improvement in certain physiological parameters is possible. According to the guidelines, ineffective treatments should be discontinued or withheld altogether.
An intensive-care treatment is considered to offer little or no likelihood of benefit in cases where it must be concluded, either from the outset or in the course of therapy, that the patient will no longer be able to return to an appropriate living environment. What is meant by an appropriate living environment will depend on the patient’s wishes and preferences. However, there must at least be a prospect of the patient being able to receive long-term care outside the ICU. As stated in the guidelines, treatments offering little likelihood of benefit cannot legitimately be demanded by a patient or authorised representative, since they place burdens on the patient, relatives and the treatment team without there being any reasonable prospect of a worthwhile goal being attained. Mere survival under sustained intensive care cannot be regarded as a worthwhile goal. To this extent, not just ineffective but even effective treatments could offer little likelihood of benefit.
Even if many people presumably share the view that mere survival under sustained intensive care is not a goal worth pursuing, the guidelines do at this point make a value judgement. In order to determine that there is little likelihood of benefit, one must first consider the overarching goals of treatment and leave sufficient time to assess the situation – an assessment which often cannot in any event be made with absolute certainty. Accordingly, the guidelines do not explicitly – as in the case of ineffectiveness – call for the discontinuation of treatment offering little likelihood of benefit.
In the above-mentioned triage guidelines, issued as a supplement to those on “Intensive-care interventions”, the notion of unlikelihood of benefit is invoked not as an initial criterion for ICU admission, but in connection with triage during the ICU stay.10 However, the exclusion criteria for ICU admission listed in the guidelines are influenced by considerations concerning foreseeable failure to benefit from such treatment. Guideline-based decisions on the allocation of ICU beds ease the burden not only on health professionals but also on authorised representatives, who thus do not have to assess, under triage conditions, whether their relative (or patient) should receive one of the scarce ICU beds. They do, however – as is also the case in clinical practice under non-triage conditions – have to consider whether the patient would even have wished to receive ICU treatment.
Particular importance attaches to the concept of unlikelihood of benefit in cases where it needs to be evaluated whether patients who would in fact benefit from further ICU treatment should be transferred from an ICU in order to make room for other patients (post-ICU admission triage).11 In such cases, the intensive care specialist seeks to maximise the overall value obtained from limited ICU resources. Triage decisions thus often involve assessment of the relative benefit which can be expected for one patient compared to another. In this situation, however – critics maintain – discontinuation of treatment is only justifiable either if this is in accordance with (what can at least be presumed to be) the patient’s wishes or if the individual medical indication for continued treatment is no longer valid. But the latter, it is argued, can only be assumed to be the case if continued treatment offers such a low likelihood of benefit that it would not be undertaken even in the absence of resource scarcity. This position denies that a special ethical situation arises from resource scarcity and rejects the principle of benefit maximisation; it has not, however, gone unchallenged.12 At any rate, it is undisputed that “treatments clearly offering little likelihood of benefit should not be carried out”.13 Considerable weight thus certainly attaches to the concept of unlikelihood of benefit. At the same time, here, too, the judgements “such a low likelihood of benefit that” and “clearly offering little likelihood of benefit” highlight the interplay between medical facts and the evaluation thereof.
3. Medical ineffectiveness and unlikelihood of benefit
3.1. Historical background
The concept of medical ineffectiveness/unlikelihood of benefit can be traced back to antiquity.14 Over the centuries, it was subject to changes both in its significance and in its function. In the Hippocratic Corpus, physicians are urged not to attempt “futile treatment” in a person with an illness which is “too strong for the available remedies”.15 Therapeutic ineffectiveness/unlikelihood of benefit was thus associated with the limits of medicine. Only in the 20th century did advances in medical sciences and technology make it possible for the lives of terminally ill patients to be prolonged.16 The concept of medical ineffectiveness/unlikelihood of benefit was then linked to considerations of cost-effectiveness and the question of equity. A further shift came with the democratisation of medicine and the associated strengthening of patient autonomy.17 The idea that physicians, as experts, should make decisions on life or death was superseded by the shared decision-making model.18
3.2. Futility debate and conceptual clarifications
When the term “futility” is used, a distinction is not always clearly made between ineffectiveness and unlikelihood of benefit. However, the debate on how the term is to be understood and used can be embedded in at least three (connected) controversies:19
- How is the relationship between objective/factual and subjective/value-laden assessments and decisions to be understood?
- What weight is to be accorded to medical authority or expertise on the one hand and patient autonomy on the other?
- What happens in the event of a conflict between evaluations of outcomes on the part of physicians and the patient/relatives?
Certain authors20 seek to formulate an objective definition. The widely cited and used definitions of quantitative and qualitative futility derive from Schneiderman et al.21 Quantitative futility involves a medical judgement, based on empirical data, that the probability of treatment being successful (e.g. return of spontaneous circulation) is less than 1%. In contrast, qualitative futility refers to situations where, based on their values, patients see no benefit arising from treatment (e.g. absolute dependence on intensive care). Whereas quantitative futility relates to treatment goals, the focus with qualitative futility is on the patient’s quality of life.
Another frequently used concept is that of physiological futility.22 This relates to physiological effects and goals which cannot be achieved by means of a given treatment. This concept comes closest to the definition of ineffectiveness used in SAMS guidelines, but it can also cover unlikelihood of benefit. Thus, for example, antibiotic therapy in a case of viral infection would be ineffective, while intensive care in a patient with brain death would offer no likelihood of benefit.
Other authors raise fundamental objections to the concept of futility. They argue that the very fact that it relates to a selected goal makes it subjective and value-laden; at the same time, in their view, the concept creates an illusion of objective and factual judgement.23 The subjectivity of the goal and of the cut-off points (as regards the size or likelihood of occurrence of an effect) applies both to ineffective treatments and to those offering little likelihood of benefit. In order to highlight the dependence on a specific treatment goal and the evaluative component, alternative terms such as “inappropriate” or “non-beneficial” are therefore proposed.24 In a joint Policy Statement, a number of professional societies proposed that use of the term “futile” should be restricted to situations where a physiological goal simply cannot be achieved, and that the term “potentially inappropriate” should be used to cover all forms of ineffectiveness and unlikelihood of benefit which include an evaluative component.25 Against this view, it has been argued that the term “futility” offers the advantages of transparency and clarity, “confirm[ing] unambiguously that human beings are mortal, and medicine’s powers are limited.”26
One important result of this fundamental debate is the insight that futility relates to a defined treatment goal, which may vary according to the patient population. Thus, the ability to return to an appropriate living environment (i.e. at the very least, sustained provision of care outside the ICU), as mentioned in the SAMS guidelines on intensive-care interventions, is indeed a plausible (albeit not value-free) goal for the assessment of unlikelihood of benefit; in the first instance, however, it is only applicable in relation to ICU patients.27 Beyond the fundamental conceptual controversies, pragmatic positions have been developed which emphasise that any decision concerning the appropriateness of an intervention is taken in a broader social and medical context.28
3.3. Ethical perspective
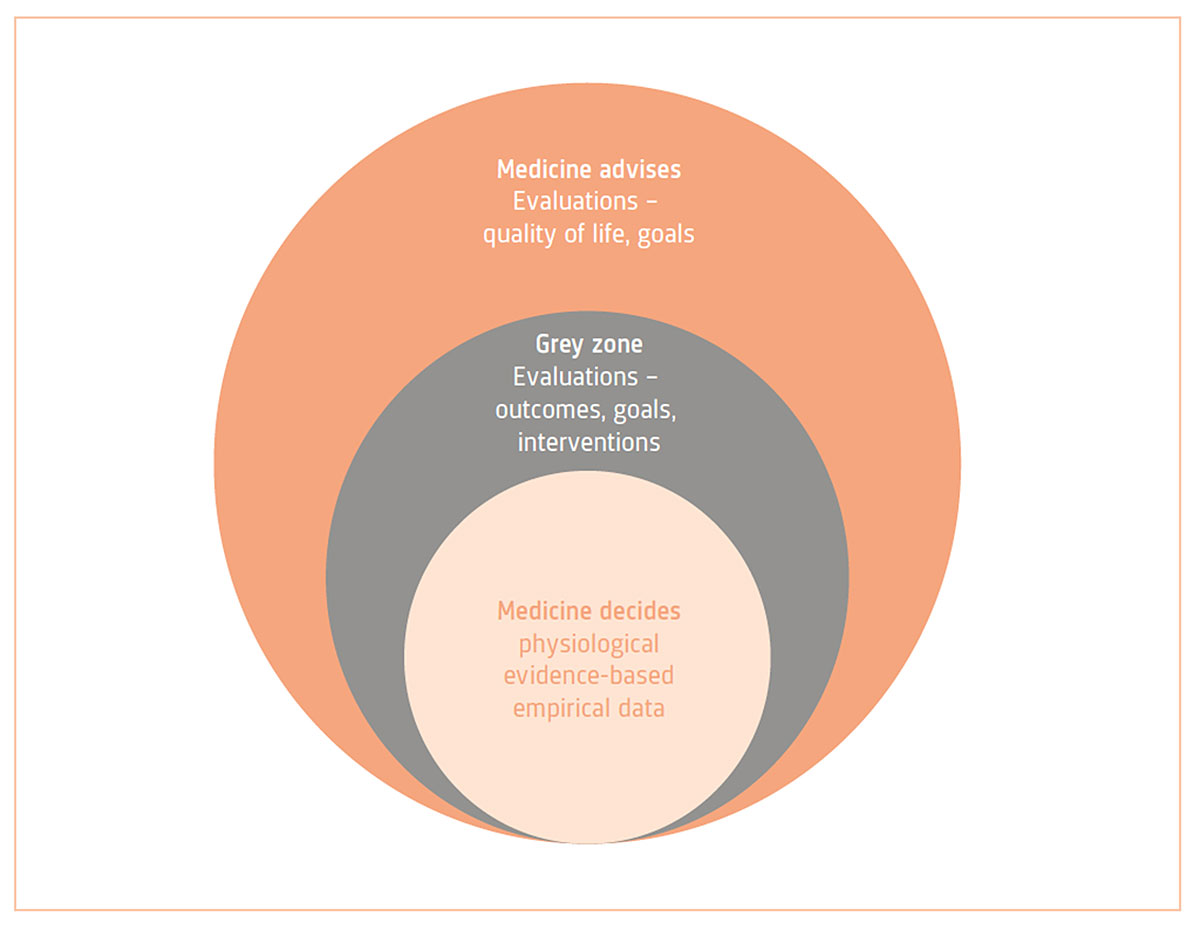
Futility is a multifaceted concept, and some authors have therefore expressed reservations about the use of this term. Medical futility has been described as “a complex, ambiguous, subjective, situation-specific, value-laden, and goal-dependent concept which is almost always surrounded by some degrees of uncertainty; hence, there is no objective and valid criterion for its determination.”29 However, such criticism appears to be unduly sweeping, as there is no doubt that some values and goals are widely shared. Consequently, it is possible in certain constellations to speak of a general consensus with regard not only to ineffectiveness but also to unlikelihood of benefit. Ultimately, however, this also involves a value-based decision, embedded in the expertise of the knowledge community and reflecting societal norms and worldviews. In the development of such consensus views, a key role can be played by authorisation procedures and health technology assessment.30 These evaluations should be made as transparent as possible, be subject to critical reflection and be integrated into a decision-making process which patients help to shape. In particular, there is also a need for public debate on the question of what effect type, size and likelihood is sufficient to justify the use of limited resources. Here, it seems legitimate to distinguish the following three categories:31
Category “Medicine decides”
In the case of physiological ineffectiveness, it can be determined empirically (even though a certain residual uncertainty or risk of error remains) that a treatment is not or would not (any longer) be effective. In such situations, medical professionals32 should be able to decide that a treatment is no longer offered (e.g. use of extracorporeal membrane oxygenation in a patient with a poor prognosis). The decision relates to the medical facts and must be based on professional expertise. In this constellation, there is a presumption of a societal consensus granting medical professionals the relevant authority. Such situations are often also regulated at the policy level, for example via professional guidelines (see also Section 5.1 “Obligation to treat or to offer a particular treatment”). In a situation of this kind, dialogue with the patient and relatives is also essential. In particular, it is important to explain the rationale for the decision to patients and relatives.
Category “Medicine advises”
This situation is the rule rather than the exception. Medical professionals inform patients (or authorised representatives) about the individual prognosis, the treatment options available, and the associated benefits and risks, and – at the patient’s request – propose one or more possible treatments. The patient accepts or rejects the proposed treatment or chooses one of the options offered. Here, the patient’s right to self-determination has priority, although it is to be borne in mind that while patients may refuse treatment at any time, they cannot generally demand particular treatments.33
Category “Grey zone”
Different weights are accorded to therapeutic goals or interventions. In this situation, the evaluation of the empirical data is influenced by worldviews and societal values. For example, should a patient be entitled to receive a treatment which has proved ineffective in the last 50, 99 or 100 cases (“Medicine decides”)?34 The normative decision lies in the determination of the cut-off (quantitative futility) or in the evaluation of the relevance of therapeutic effects (qualitative futility). These situations generally also involve efforts to determine, together with the patient, whether the treatment is desired, even though the chances of success are low (“Medicine advises”). The consequences of the treatment are not only relevant in terms of burdens for the patient and relatives (or the treatment team). In the case of high-cost treatments, possible opportunity costs must also be considered, as the resources used will no longer be available for other patients.35 In such cases, a treatment may possibly also be assigned to the “Medicine decides” category.
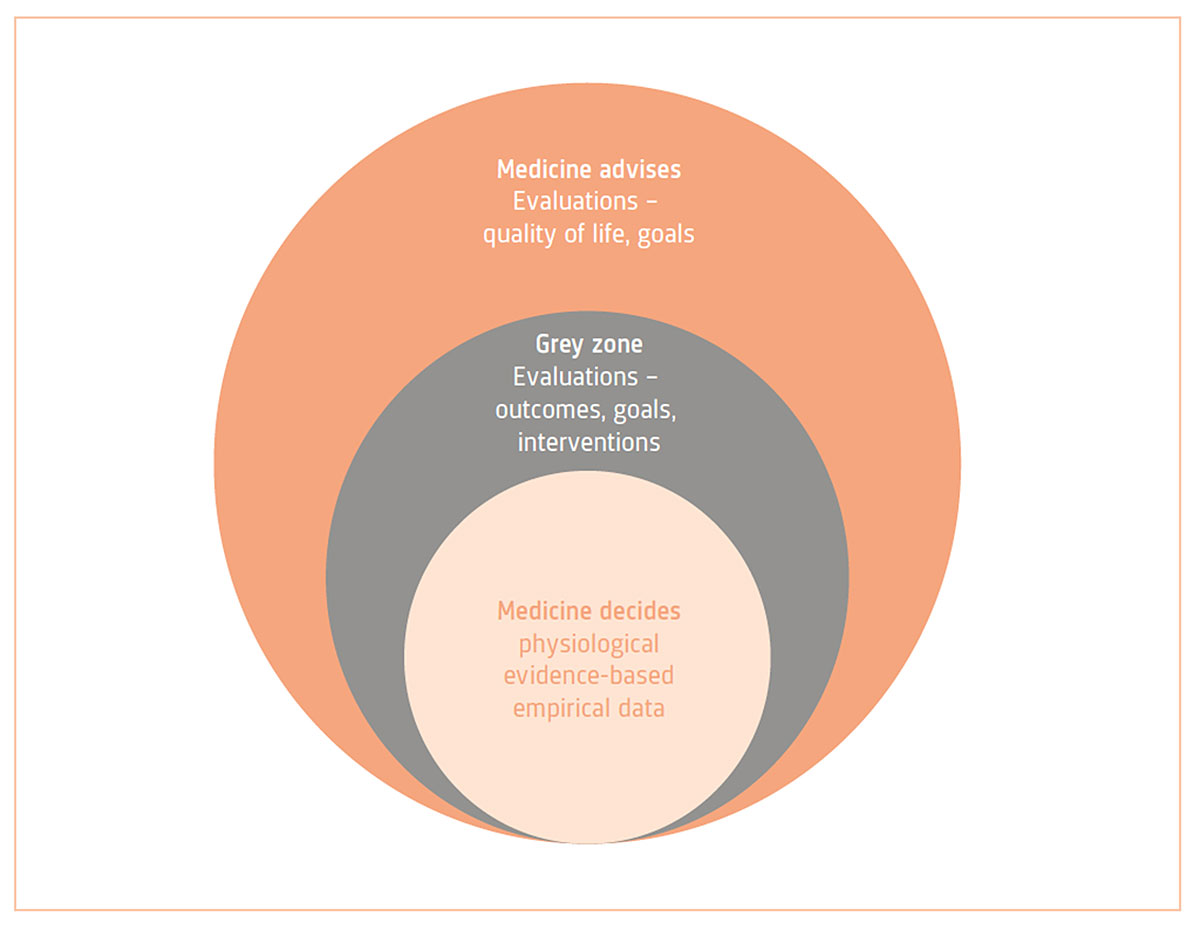
Figure 1
Futility and decision-making in medicine. While for a closely circumscribed set of medical interventions effectiveness can be clearly ruled out on the basis of physiological processes or empirical medical evidence and knowledge, a much larger area remains in which evaluations of effectiveness may vary according to the goal of treatment. Lying between these two areas is a “grey zone”, in which the question of what interventions are to be offered as therapeutic options needs to be negotiated in the specific social and economic context.
4. Medical indication
4.1. Historical background
Ineffectiveness and unlikelihood of benefit are closely related to the concept of medical indication, which – like that of futility – can be traced back to ancient medicine. Since Galen, it has assumed a deontological character, involving an obligation to take medical action.36 In the Middle Ages, there then developed the theory of indications, which was increasingly based on empirical foundations and knowledge. Diagnostic and therapeutic decisions were derived from the signs and causes of a disease. Today, the establishment of an indication is seen as a discursive and normative process.
4.2. Conceptual clarifications and controversy concerning medical indication
The medical indication serves to justify the suitability and appropriateness of a medical treatment for achieving the treatment goal jointly determined with the patient. Here, as in the case of unlikelihood of medical benefit, there is disagreement as to the extent to which the concept of medical indication transcends the purely medical or scientific. Also relevant, as well as individual aspects and value-based considerations, are societal conceptions of good medical care and of the goals of medicine.37 As with the concept of futility, the medical indication may be partly determined by factors unrelated to patient welfare or equitable resource allocation. For example, medical decisions concerning the establishment of an indication may be influenced by the economic objectives of hospital management. To make the evaluative elements explicit, some authors have therefore proposed alternative concepts, such as “balancing of benefits and harms”.38
The establishment of an indication involves two steps: firstly, the medical indication in the narrow sense offers a scientific, evidence-based justification of the suitability and appropriateness of a treatment for the agreed goal. This justification is empirical, purposive and causal and relates to the categorisation of diseases and situations.39 Secondly, the treatment is assessed in relation to the patient’s individual – medical and personal – situation. The medical indication thus has a dual character: it must be scientifically justifiable, while at the same time taking the patient’s personal and individual situation and values into account.40 However, even though the establishment of an indication “inevitably makes reference both to scientific factors and to life-world aspects of the patient in his sociocultural context”,41 this does not mean that it is arbitrary. It is embedded in well-defined decision-making structures and can be understood as a means of creating trust in scientific expertise.
Both ineffectiveness and unlikelihood of benefit thus represent a sufficient reason for a treatment not to be indicated. At the same time, an effective treatment does not automatically have to be performed. The benefits and risks of the available treatment options should first be assessed and the patient’s wishes determined.
The concept of medical indication is thus reminiscent of the Federal Supreme Court’s operationalisation of the concept of appropriateness, which is required under Art. 32 of the Federal Health Insurance Act (KVG): “Whether a medical treatment is appropriate is to be evaluated according to the diagnostic or therapeutic benefit of its application in a particular case, taking the associated risks into consideration.” Appropriateness coincides with the medical indication for a treatment, as also noted by the Federal Supreme Court: if a treatment is medically indicated, it is also appropriate.42
4.3. Ethical perspective
Like medical futility, the concept of medical indication can also be divided into various categories:43 an intervention is
- indicated,
- not indicated (ineffective and/or offering little likelihood of benefit),
- contraindicated (harmful), or
- the indication is doubtful.
The last-mentioned category corresponds roughly to the “grey zone” of medical ineffectiveness or unlikelihood of benefit. The indication for a treatment is doubtful with regard to the patient’s individual and personal situation, if the probability of success is low and/or if the benefit is marginal or not supported by adequate scientific evidence.
To separate scientific from evaluative and individual elements of a medical indication, further distinctions can be made. A medical indication sensu stricto only relates to the scientific/medical domain and is concerned with the effectiveness of a treatment.44 In this sense, whether a treatment is considered to be indicated or not depends exclusively on evidence-based judgements. In addition, indications could be assigned a degree of recommendation, according to the degree of evidence.45 With regard to these medical assessments and judgements, patients stand in a relationship of trust to medical professionals and rely on the latter’s expertise.
In the second step of the assessment, supplementing the establishment of the medical indication in the narrow sense, the concept of benefit is employed, as described above (cf. Section 4.2). The evaluations which are brought to bear in the decision-making process with the patient are thus explicitly highlighted. Here, patient autonomy and professional expertise are closely intertwined. In an additional assessment step, ethical obligations are weighed up vis-à-vis relatives, other patients and the wider health insurance community.46 Finally, the balance of benefits, risks and burdens is considered; this can be subsumed under the concept of appropriate care.
The quality of the medical indication is subject to various risks. On the one hand, a growing focus on the individuality of patients and their wishes could fuel the idea of wish-fulfilling medicine, pushing the normative, evidence-based character of the medical indication into the background.47 On the other hand, economic incentives could induce medical professionals to focus not on the patient’s interests but on other, medically irrelevant factors when establishing an indication.48
5. Legal aspects
In order to provide a legal assessment of treatments which are ineffective or offer little likelihood of benefit, it is necessary to consider the various issues which may arise in this connection.49 To be examined, firstly, are the questions under what conditions an obligation to treat or an obligation to offer a particular treatment exists (Section 5.1); what the position is if an offer of treatment is refused (5.2); and how to proceed in the event of an unclear indication (5.3). Not to be considered here, in the first instance, is the question under what conditions a treatment must be reimbursed by a health insurer.
If agreement exists between the physician and the duly informed patient (or authorised representative) that a treatment is to be carried out, not carried out, or discontinued, no further difficulties arise from a legal perspective. Accordingly, only situations of conflict are explored below.
5.1. Obligation to treat or to offer a particular treatment
Conflicts may arise if patients demand a treatment which they have not been offered. This raises the question under what conditions a physician is legally obliged to offer a treatment. In the legal literature, it is widely agreed that treatments which are not indicated do not have to be offered, either by a hospital or by a physician. The concept of medical indication is therefore of substantial importance. As shown in Section 4.2, the physician retains a degree of discretion. However, the indication established on the basis of the physician’s professional expertise and experience (with consideration being given to specialist guidelines, where appropriate) sets the framework within which a patient can exercise his or her right to self-determination – understood as a right to refuse control by others (cf. Section 5.2).50 Thus, in the case of treatments which, according to medical criteria, offer “little likelihood of benefit”, there is no obligation to treat and the physician is not required to offer the patient (or authorised representative) any such treatment. Equally, the physician is not required to refer the patient to a colleague or an institution where such treatment may be available.
For the sake of completeness, it should be noted that, for physicians, an actual obligation to treat is in any case the exception rather than the rule, being confined to the provision of assistance in an emergency.51 Even when such an obligation exists, treatments which are not indicated do not have to be offered.52
5.2. Refusal of treatment offered or recommended
Treatment must not be carried out if a duly informed patient with capacity (or authorised representative) decides to refuse an intervention specifically offered or not to undergo treatment of any kind.53 In such cases, the only point to note is that such a decision should be made freely and not on the basis of one-sided, directive information or non-objective reasoning on the part of health professionals (pseudo-futility). A decision on the discontinuation or refusal of treatment made under pressure or as a result of non-impartial information would not be legally valid, so that the question of liability could then arise. Otherwise, the refusal of medical interventions is to be respected, regardless of the underlying motives, with exceptions to be made only (in exceptional cases) for child protection measures54 or – in the case of patients lacking capacity or where their interests are jeopardised by an authorised representative – for adult protection measures.55
5.3. Conflict in cases of doubtful indication (“grey zone”)
From a legal perspective, the situation is most difficult in cases where there are doubts as to whether a treatment which has been requested is indicated or not, and the physician or treatment team take the view that it would be better if the treatment were withheld. It is true that a refusal by a patient (even of a clearly indicated treatment, all the more so for one which is not unequivocally indicated) is legally unproblematic and to be respected, while treatment which is (clearly) not indicated need not be offered in the first place. However, the question arises what role is to be played by the patient’s wishes within the “grey zone”. Court practice is rarely concerned with such cases, and if it is, then generally only with regard to the reimbursement of costs by health insurers. Since the efficacy, appropriateness and cost-effectiveness of a treatment are a prerequisite for mandatory reimbursement, this can also serve as a starting point in the dialogue between physician and patient to determine whether an obligation to offer treatment exists.56 If no agreement is reached in discussions between the medical professionals involved and the patient or authorised representative, the following cases need to be distinguished: if the resources required for the requested treatment are essentially available and if at the same time a requirement exists for reimbursement of costs by the health insurer, then – in doubtful cases – treatment should be carried out (or attempted) as requested. If, however, one or both of these conditions are not met, the treatment should generally not be carried out, or treatment already initiated should be discontinued and, if appropriate, the focus should be shifted to palliative care.
6. Conclusions
The concept of futility is complex, and the associated terms “ineffectiveness”, “unlikelihood of benefit” and “indication” are used and distinguished from each other in different ways. The present recommendations provide a basis for the clear and consistent application of these terms.
Both ineffectiveness and unlikelihood of benefit represent a sufficient reason for the absence of an indication (treatment not indicated). This does not, however, mean that any treatment which may be effective is necessarily indicated, for the benefits and risks (negative aspects for the patient, appropriateness) also need to be assessed and the patient’s wishes taken into consideration.
The question when something is or is not to be classified as “futile” depends essentially on what is defined as a satisfactory outcome. Remaining of central importance, therefore, is the question what an appropriate treatment goal is. Who determines the treatment goal? Can this be adequately achieved by means of the intervention? Is the ratio of benefits to risks and burdens acceptable for the patient? Of crucial importance is the distinction between those decisions which clearly rest with medical professionals (cf. Section 3.3: “Medicine decides”) and those which need to be made jointly with the patient (cf. Section 3.3: “Medicine advises”/“Grey zone”). Some areas exist in which there is a robust social consensus in support of decisions being made independently by medical professionals even against the wishes of those concerned – for example, in cases where patients, authorised representatives or relatives demand treatments which are not part of recognised medical practice, or are opposed to the withdrawal of a treatment even though the continuation thereof is to be regarded, on medical grounds, as offering little likelihood of benefit (e.g. discontinuation of treatment in refractory heart failure or in persistent vegetative state). In such constellations, the concept of futility strengthens the autonomy and expertise of the medical treatment team. At the same time, the concept of unlikelihood of benefit can help relatives to accept a withdrawal of treatment which is also based on sound legal foundations (cf. Section 5.1) and to consent to palliative care.57 In all constellations, however, dialogue with the patient and relatives remains central.
According to the SAMS guidelines “Decisions on cardiopulmonary resuscitation”, for example, CPR offers little or no likelihood of benefit in cases where a short- or medium-term extension of life, with a quality of life tolerable from the patient’s perspective, can almost certainly be ruled out. At the same time, the guidelines also define criteria for situations in which the initiation of CPR is not indicated (or negotiable) because there is clear evidence that it would offer little or no likelihood of benefit.58
The following Table – supplementing the text – shows how the concepts of ineffectiveness, unlikelihood of benefit and indication relate to each other.
|
Futility
|
|
Ineffectiveness
|
Unlikelihood of benefit
|
|
Ineffective
|
Probably ineffective
|
No likelihood of benefit
|
Little likelihood of benefit
|
| Specific therapeutic goal cannot be achieved with treatment, i.e. therapeutic success is not possible (e.g. antibacterial treatment of a viral infection). |
Probability of specific therapeutic success unclear or low, with at best the prospect of a limited effect (e.g. prescription of digoxin in refractory heart failure). |
Even if treatment is potentially effective, there is little prospect of achieving the overarching therapeutic goal (e.g. cure, survival with acceptable quality of life) desired by the patient (e.g. experimental chemotherapy in advanced metastatic cancer with a low probability of extension of survival by a few months). |
Even if treatment is potentially effective, the overarching therapeutic goal (e.g. cure, survival with acceptable quality of life) desired by the patient cannot be achieved (e.g. resuscitation after interruption of oxygen supply for several minutes in a patient with end-stage COPD). |
|
Not indicated (or contraindicated, if harmful) |
Doubtful indication (potentially inappropriate). For indication, assessment of appropriateness is required. → Evaluation of the ratio of the size and likelihood of benefit to risks and adverse effects. For reimbursability (in the area of compulsory health insurance), assessment of cost-effectiveness is required. → Evaluation of cost-effectiveness (Health Technology Assessment) |
Not indicated (or contraindicated, if harmful) |
| Remaining essential in all types of situation is dialogue with the patient concerning the overarching and specific therapeutic goals and the treatment options available. If the indication is doubtful, the patient is to be involved in the decision-making process (shared decision-making).
|
7. Recommendations
If the ineffectiveness or unlikelihood of benefit of a treatment is clearly established, then there is no medical indication for it (“Medicine decides”). The following recommendations are designed to encourage all concerned to deal consciously with the concept of futility, especially in those situations where – irrespective of the patient’s preferences – ineffectiveness or unlikelihood of benefit is not clearly established (“Medicine advises”/”Grey zone”). Here, the following recommendations are relevant:
7.1. Defining the goal of treatment
The overarching goal of treatment must be jointly defined with the patient or authorised representative. This requires medical professionals to take into consideration the patient’s ideas and level of knowledge, needs, wishes and fears, and to enquire about the patient’s preferences. Professionals are to be guided by the treatment goal and to assess whether the proposed procedure is in accordance with the goal. The results are to be documented in an appropriate form.
Example: A patient with cervical cancer develops obstructive kidney failure which, if untreated, can be rapidly fatal. The patient would like to live to see the birth of her grandchild in two months’ time. Dialysis can extend life without, however, affecting the underlying malignancy. But as it makes it possible for the patient to live to see her grandchild born, it may be appropriate.
7.2. Acknowledging personal bias
The establishment of an indication is not only based on objective facts, but is frequently influenced by non-scientific factors. For example, professional judgement may be coloured by subjective, emotional evaluations of disease situations or patient groups, or by anxiety about awkward conversations, but also by conflicts of interest. Such influences are to be acknowledged and subjected to critical reflection.
Example: Medical professionals are aware that, for certain patient groups, they may tend to dismiss a treatment more rapidly as ineffective or offering little prospect of benefit and thus not offer or perform it, e.g. in the case of people with diabetes or addiction disorders.
59
7.3. Interprofessionality
Indications should be established in an interdisciplinary and multiprofessional manner (within the team). Specialists are to be involved in the assessment of ineffectiveness or unlikelihood of benefit.
Example: Hospital physicians and nurses who need to assess whether or not dialysis should be performed in a patient discuss the situation with the nephrologist and GP responsible, as well as with the patient and relatives.
7.4. Biopsychosocial approach to the patient
The decision on the appropriateness and/or effectiveness of a treatment should take into consideration not just physiological but also psychological and social aspects.
Example: A treatment is assessed not “atomistically” with regard to a specific problem to be dealt with (e.g. a surgical procedure requiring bed rest for wound healing in a frail patient with psychomotor agitation), but holistically, considering the patient as a whole. This means that other diseases and the patient’s general situation are also taken into account.
7.5. Taking account of patients' values and worldviews
Patients’ personal values and worldviews or cultural characteristics influence their conception of autonomy, affect their understanding of disease and cure, and may lead to different weights being accorded to treatment options or a prognosis. This needs to be taken into account insofar as indications which are negotiated or lie within the “grey zone” are concerned.
Example: Parents who, for reasons of worldview, insist on the continuation of ICU treatment in a child with multi-organ failure and severe CNS damage, with no prospect of improvement, are offered psychological support. If religious motives are predominant, it may be helpful – with the parents’ consent – to involve representatives of the religious community in the dialogue.
7.6. Focusing on dialogue
Communication/dialogue makes it possible to identify the needs of patients and relatives, create trust and arrive at good decisions. It should be borne in mind that, for example, the role of medical professionals and also of patients may change in the course of severe illness. If it becomes apparent that treatments are proving ineffective, it is important to negotiate subsequent steps acceptable to all parties through dialogue.
Example: In an elderly ICU patient with severe Covid-19, the prognosis is deteriorating. By talking to the relatives, it is possible to address their concern that the proposed discontinuation of treatment may be due to a shortage of beds, with their relative now having to make room for a younger patient.
7.7. Transparency
Indications should be established on the basis of scientific evidence, medical experience and the patient’s situation. If the effectiveness of a treatment or the prognosis cannot be assessed with certainty, this should be explained transparently and taken into consideration in the decision-making process (subjective evaluation of the patient). A seemingly objective statement to the effect that an intervention would be of no benefit is not permissible (pseudo-futility)60.
Example: A surgeon confronts the patient with a decision which has been made (rejection of a surgical procedure based on poor prognosis) and provides information on the background to the decision (poor prognosis).
7.8. Integrating palliative care at an early stage
It is important to explain clearly to the patient that the withholding or withdrawal of therapies does not mean that treatment will no longer be provided, but that the focus is to be shifted to palliative care. Even if therapies offer “little or no likelihood of benefit” in terms of survival with an acceptable quality of life, effective and highly appropriate interventions are available if the goal of treatment is shifted to palliation.
Example: In the context of persistent severe illness (e.g. COPD, severe neurodegenerative disease such as amyotrophic lateral sclerosis, or severe psychiatric disease such as anorexia nervosa), unlikelihood of benefit means that intensive care or other treatments aimed at extending life are no longer indicated and palliative care becomes of prime importance.
Professional societies, nursing organisations and patient associations are urged to engage in the debate on this complex issue.
Footnotes
1 Cf., for example, the Code of the Swiss Medical Association (FMH), Art. 4.
2 Cf. OECD (2017).
3 Cf. Fässler et al. (2015).
4 Cf. Position paper of the Ethics Section of the DIVI and the Ethics Section of the DGIIN (Michalsen et al. 2021).
5 Cf. SAMS recommendations on the management of conflicts of interest in the development of guidelines and Choosing Wisely lists (2017; available in French and German); www.smartermedicine.ch
6 Cf. “Intensive care triage under exceptional resource scarcity”. Guidelines issued by the SAMS and SSICM (2020, updated 2021).
7 Cf. Joebges & Biller-Andorno (2020); Joebges et al. (2020).
8 Cf. SAMS Medical-ethical guidelines “Intensive-care interventions” (2013, supplement issued in 2020 and 2021).
9 Cf. Section 5.4 of the guidelines “Intensive-care interventions”. In these guidelines, the term “futility” is mentioned only as a rough equivalent of these two notions but is not subsequently used, given the inconsistent and controversial nature of existing definitions.
10 Cf. “Intensive care triage under exceptional resource scarcity”. Guidelines issued by the SAMS and SSICM (2020, updated 2021).
11 Cf. Fateh-Moghadam & Gutmann (2020).
12 Cf., for example, the responses from Hans Pargger and Stefan Felder (2020).
13 Cf. Picecchi (2020).
14 Cf. Schneiderman (2011).
15 Cf. Schneiderman (2011); Aghabarary & Dehghan Nayeri (2016).
16 Cf. Aghabarary & Dehghan Nayeri (2016).
17 Cf. Misak et al. (2016).
18 Cf. Rosca et al. (2020).
19 Cf. Wolfe (2019).
20 Cf. Brody et al. (1995); Schneiderman (2011).
21 Cf. Schneiderman et al. (1990).
22 Cf. Aghabarary & Dehghan Nayeri (2016); Brody et al. (1995).
23 Cf. Kyriakopoulos et al. (2017); Truog & White (2013); Wilkinson & Savulescu (2011).
24 Cf. Brett & McCullough (2017); Kyriakopoulos et al. (2017); Truog & White (2013).
25 Cf. Bosslet et al. (2015); Pope (2017).
26 Cf. Schneiderman et al. (2017).
27 Cf. SAMS Medical-ethical guidelines “Intensive-care interventions” (2013, supplement issued in 2020 and 2021).
28 Cf. Misak et al. (2016); Misak et al. (2014); Krones & Monteverde (2013).
29 Cf. Aghabarary & Dehghan Nayeri (2016); Nair-Collins (2015).
30 Cf. www.swissmedicalboard.ch
31 Cf. Misak et al. (2016), where three types of cases are distinguished – “straightforward unnegotiated”, “straightforward negotiated” and “non-straightforward”.
32 Cf. Truog (2018).
33 Cf. Aebi-Müller (2021).
34 Cf. Brett & McCullough (2017); Kyriakopoulos et al. (2017); Truog (2018).
35 Cf. Niederman & Berger (2010).
36 Cf. Gahl (2015).
37 Cf. Dörries, Lipp (2015); Maio (2015).
38 Cf. Dörries (2015); Marckmann (2015).
39 Cf. Raspe (2015).
40 Cf. Neitzke (2015); Marckmann (2015).
41 Maio (2015).
42 “Lorsque l’indication médicale est clairement établie, le caractère approprié de la prestation l’est également” (Federal Supreme Court ruling BGE 130 V 532 S. 536).
43 Cf. Neitzke (2015).
44 Cf. Marckmann (2015).
45 Cf. Raspe (2015).
46 Cf. Marckmann (2015).
47 Cf. Maio (2015); Raspe (2015).
48 Cf. Dörries (2015); Maio (2015); Raspe (2015).
49 Not covered in the following discussion are triage situations in the narrow sense, i.e. resource scarcity in relation to ICU beds (cf., for example, Aebi-Müller 2021).
50 Cf. Aebi-Müller (2016).
51 Cf. Art. 40 let. g of the Medical Professions Act (SR 811.11): They shall provide aid in urgent cases and participate in emergency services in accordance with cantonal requirements.
52 Cf. Aebi-Müller (2016).
53 Cf. Aebi-Müller et al. (2016). § 2, margin no. (Rz) 94, with additional references.
54 Cf. Pfister Piller (2016).
55 Cf. SAMS Medical-ethical guidelines “Coercive measures in medicine” (2015).
56 Cf. Aebi-Müller (2021).
57 Cf. Šarić et al. (2017); Truog (2018).
58 Clear evidence: unwitnessed cardiac arrest, absence of hypothermia, asystole, no first-responder CPR, emergency medical services response time >10 minutes. The guidelines point out that, in practice, for the relatives’ sake, CPR is sometimes attempted for a limited period – above all, to demonstrate that every effort was made; however, it is noted that this is ethically problematic.
59 Cf. Lorentzon et al. (2019); Bernstein et al. (2013).
60 Cf. Geppert (2021); Wilkinson & Savulescu (2011).
Information on the preparation of these recommendations
The preparation of these recommendations was prompted by discussions which took place from 2018 onwards in connection with the revision of the SAMS medical-ethical guidelines “Decisions on cardiopulmonary resuscitation” (issued in 2021). These discussions concerned the balance to be struck between strictly medical considerations and values as a basis for decision making. The question of equity was additionally addressed in 2020, during the preparation of the ICU triage guidelines.
The topic was discussed in depth at four meetings of an advisory group. On the basis of the first discussions, the authors (see below) drafted a text which was discussed and approved at the advisory group meetings. The text was submitted to selected experts for comment, and their feedback was taken into account in the final version. The recommendations were discussed and approved by the Executive Board of the SAMS at a meeting held on 16 September 2021, and by the Central Ethics Committee (CEC) on 28 September 2021.
Authors
Professor Nikola Biller-Andorno, Zürich
Professor Regina Aebi-Müller, Luzern
lic. iur. Michelle Salathé, MAE, Basel
Jana Sedlakova, MA, Zürich
Members of the advisory group
Professor Nikola Biller-Andorno, Zürich (Chair)
Professor Regina Aebi-Müller, Luzern (CEC member)
PD Dr Klaus Bally, Basel (CEC member)
PD Dr Eva Bergsträsser, Zürich (CEC member)
Professor Paul Hoff, Zürich (CEC Chair)
Professor Anja Lorch, Zürich (CEC member)
Dr Valerie Luyckx, Zürich (CEC member)
Dr Madeleine Mirabaud, Genève (CEC member)
lic. iur. Michelle Salathé, MAE, Basel (scientific support)
Bianca Schaffert, MSN, Schlieren (CEC Vice Chair)
Dr Ewald Schorro, Fribourg (CEC member)
Experts
PD Dr Peter Berchtold, Bern
Dr Lars Clarfeld, Bern
Dr Antje Heise, Thun
Dr Damian König, Sion
Professor Tanja Krones, Zürich
Professor Sophie Pautex, Genève
Professor Reto Stocker, Zürich
PD Dr Manuel Trachsel, Basel
Dr Anna Westermair, Zürich
References
–
Aebi-Müller RE
. Behandlungspflichten und Behandlungsentscheide bei Ressourcenknappheit. Jusletter 1. Februar 2021.
–
Aebi-Müller RE
,
Fellmann W
,
Gächter T
et al.
Arztrecht. Bern: Stämpfli Verlag; 2016.
–
Aghabarary M
,
Dehghan Nayeri N
. Medical futility and its challenges: a review study. J Med Ethics Hist Med. 2016 Oct;9:11.
–
Bernstein SL
,
Yu S
,
Post LA
,
Dziura J
,
Rigotti NA
. Undertreatment of tobacco use relative to other chronic conditions. Am J Public Health. 2013 Aug;103(8):e59–65. https://doi.org/10.2105/AJPH.2012.301112
–
Bosslet GT
,
Pope TM
,
Rubenfeld GD
,
Lo B
,
Truog RD
,
Rushton CH
, et al.; American Thoracic Society ad hoc Committee on Futile and Potentially Inappropriate Treatment; American Thoracic Society; American Association for Critical Care Nurses; American College of Chest Physicians; European Society for Intensive Care Medicine; Society of Critical Care
. An official ATS/AACN/ACCP/ESICM/SCCM policy statement: responding to requests for potentially inappropriate treatments in intensive care units. Am J Respir Crit Care Med. 2015 Jun;191(11):1318–30. https://doi.org/10.1164/rccm.201505-0924ST
–
Brett AS
,
McCullough LB
. Getting Past Words: Futility and the Professional Ethics of Life-Sustaining Treatment. Perspect Biol Med. 2017;60(3):319–27. https://doi.org/10.1353/pbm.2018.0003
–
Brody BA
,
Halevy A
. Is futility a futile concept? J Med Philos. 1995 Apr;20(2):123–44. https://doi.org/10.1093/jmp/20.2.123
–
Dörries A.
Die medizinische Indikation: Begriffsbestimmung und Rahmenbedingungen. In: Dörries A., Lipp V. (Hrsg.) Medizinische Indikation. Ärztliche, ethische und rechtliche Perspektiven. Grundlagen und Praxis. Kohlhammer; 2015; 13–23.
–
Dörries A
,
Lipp V.
(Hrsg.)
. Medizinische Indikation. Ärztliche, ethische und rechtliche Perspektiven. Grundlagen und Praxis. Kohlhammer; 2015.
–
Fässler M
,
Wild V
,
Clarinval C
,
Tschopp A
,
Faehnrich JA
,
Biller-Andorno N
. Impact of the DRG-based reimbursement system on patient care and professional practise: perspectives of Swiss hospital physicians. Swiss Med Wkly. 2015 Feb;145:w14080. https://doi.org/10.4414/smw.2015.14080
–
Fateh-Moghadam B
,
Gutmann T.
Gleichheit vor der Triage. Rechtliche Rahmenbedingungen der Priorisierung von COVID-19-Patienten in der Intensivmedizin. Verfassungsblog; 2020. https://verfassungsblog.de/gleichheit-vor-der-triage (accessed on 10 August 2020).
–
Gahl K.
Zur Geschichte des Begriffs der medizinischen Indikation. In: Dörries A, Lipp V. (Hrsg.) Medizinische Indikation. Ärztliche, ethische und rechtliche Perspektiven. Grundlagen und Praxis. Kohlhammer; 2015; 24–35.
–
Geppert C.
Psychotherapeutic Futility. In: Trachsel M, Gaab J, Biller-Andorno N, Tekin S, Sadler JZ (Hrsg.). Oxford Handbook of Psychotherapy Ethics. Oxford University Press; 2021; 447–60.
–
Joebges S
,
Biller-Andorno N
. Ethics guidelines on COVID-19 triage-an emerging international consensus. Crit Care. 2020 May;24(1):201. https://doi.org/10.1186/s13054-020-02927-1
–
Jöbges S
,
Vinay R
,
Luyckx VA
,
Biller-Andorno N
. Recommendations on COVID-19 triage: international comparison and ethical analysis. Bioethics. 2020 Nov;34(9):948–59. https://doi.org/10.1111/bioe.12805
–
Kieser U.
Zweckmässigkeitsprüfungen bei Arzneimitteln, v.a. beim Bestehen einer Limitation. Pflegerecht. 2019; 26–32.
–
Krones T
,
Monteverde S
. Medical futility from the Swiss Perspective. In: Bagheri, Alireza (ed.) Medical futility: a cross-national study. Medical Futility. 2013; 205–26.
–
Kuhn MW
,
Poledna T
. (Hrsg.)
. Arztrecht in der Praxis. 2. Aufl., Zürich: Schulthess; 2007 (insbes. S. 722 ff. zur strafrechtlichen Beurteilung der Ressourcenverteilung).
–
Kyriakopoulos P
,
Fedyk M
,
Shamy M
. Translating futility. CMAJ. 2017 Jun;189(23):E805–6. https://doi.org/10.1503/cmaj.161354
–
Lorentzon M
,
Nilsson AG
,
Johansson H
,
Kanis JA
,
Mellström D
,
Sundh D
. Extensive undertreatment of osteoporosis in older Swedish women. Osteoporos Int. 2019 Jun;30(6):1297–305. https://doi.org/10.1007/s00198-019-04872-4
–
Maio G.
Die Indikation als Vertrauensgrundlage der Medizin. In: Dörries A, Lipp V. (Hrsg.) Medizinische Indikation. Ärztliche, ethische und rechtliche Perspektiven. Grundlagen und Praxis. Kohlhammer; 2015; 74–82.
–
Marckmann G.
Wirksamkeit und Nutzen als alternative Konzepte zur medizinischen Indikation. In: Dörries A, Lipp V. (Hrsg.) Medizinische Indikation. Ärztliche, ethische und rechtliche Perspektiven. Grundlagen und Praxis. Kohlhammer; 2015; 113–24.
–
Michalsen A
,
Neitzke G
,
Dutzmann J
,
Rogge A
,
Seidlein AH
,
Jöbges S
, et al.
Überversorgung in der Intensivmedizin: erkennen, benennen, vermeiden. Med Klin Intensivmed Notf Med. 2021;116(4):281–94. https://doi.org/10.1007/s00063-021-00794-4
–
Misak CJ
,
White DB
,
Truog RD
. Medical futility: a new look at an old problem. Chest. 2014 Dec;146(6):1667–72. https://doi.org/10.1378/chest.14-0513
–
Misak CJ
,
White DB
,
Truog RD
. Medically Inappropriate or Futile Treatment: Deliberation and Justification. J Med Philos. 2016 Feb;41(1):90–114.
–
Nair-Collins M
. Laying Futility to Rest. J Med Philos. 2015 Oct;40(5):554–83. https://doi.org/10.1093/jmp/jhv019
–
Neitzke G.
Medizinische und ärztliche Indikation – zum Prozess der Indikationsstellung. In: Dörries A, Lipp V. (Hrsg.) Medizinische Indikation. Ärztliche, ethische und rechtliche Perspektiven. Grundlagen und Praxis. Kohlhammer; 2015; 83–93.
–
Niederman MS
,
Berger JT
. The delivery of futile care is harmful to other patients. Crit Care Med. 2010 Oct;38(10 Suppl):S518–22. https://doi.org/10.1097/CCM.0b013e3181f1cba5
–
OECD
. Tackling Wasteful Spending on Health. Paris: OECD Publishing; 2017.
–
Pargger H
,
Felder S.
Uni Research News. Universität Basel. 2020. Covid-19 und Intensivmedizin: Zwei Repliken. www.unibas.ch/de/Aktuell/News/Uni-Research/Corona-und-Triage--Wer-soll-behandelt-werden--wer-nicht--Zwei-Repliken.html (accessed on 10 August 2020)
–
Pfister Piller B.
Kindesschutz in der Medizin. Elterliche und staatliche Bestimmungsrechte bei der medizinischen Behandlung des Kindes. Schulthess; 2016.
–
Pope TM
. Medical Futility and Potentially Inappropriate Treatment: better ethics with more precise definitions and language. Perspect Biol Med. 2017;60(3):423–7. https://doi.org/10.1353/pbm.2018.0018
–
Picecchi D.
Die Zuteilung knapper medizinischer Ressourcen. sui generis. 2020; 297–307.
–
Raspe H.
Die medizinische Indikation und ihre Regulierung in Zeiten der evidenzbasierten Medizin. In: Dörries A, Lipp V. (Hrsg.) Medizinische Indikation. Ärztliche, ethische und rechtliche Perspektiven. Grundlagen und Praxis. Kohlhammer; 2015; 94–112.
–
Rosca A
,
Krones T
,
Biller-Andorno N
. Shared decision making: patients have a right to be informed about possible treatment options and their risks and benefits. Swiss Med Wkly. 2020 Jul;150:w20268. https://doi.org/10.4414/smw.2020.20268
–
Šarić L
,
Prkić I
,
Jukić M
. Futile Treatment-A Review. J Bioeth Inq. 2017 Sep;14(3):329–37. https://doi.org/10.1007/s11673-017-9793-x
–
Schneiderman LJ
,
Jecker NS
,
Jonsen AR
. Medical futility: its meaning and ethical implications. Ann Intern Med. 1990 Jun;112(12):949–54. https://doi.org/10.7326/0003-4819-112-12-949
–
Schneiderman LJ
. Defining medical futility and improving medical care. J Bioeth Inq. 2011 Jun;8(2):123–31. https://doi.org/10.1007/s11673-011-9293-3
–
Schneiderman LJ
,
Jecker NS
,
Jonsen AR
. The Abuse of Futility. Perspect Biol Med. 2017;60(3):295–313. https://doi.org/10.1353/pbm.2018.0001
–
Truog RD
. The Concept of Futility: Recognizing the Importance of Context. Perspect Biol Med. 2018;60(3):428–32. https://doi.org/10.1353/pbm.2018.0019
–
Truog RD
,
White DB
. Futile treatments in intensive care units. JAMA Intern Med. 2013 Nov;173(20):1894–5. https://doi.org/10.1001/jamainternmed.2013.7098
–
Wilkinson DJ
,
Savulescu J
. Knowing when to stop: futility in the ICU. Curr Opin Anaesthesiol. 2011 Apr;24(2):160–5. https://doi.org/10.1097/ACO.0b013e328343c5af
–
Wolfe I
. A Critical Analysis of Futility Discourse in Pediatric Critical Care. Journal of Pediatric Ethics. 2019;1(2):82–90.