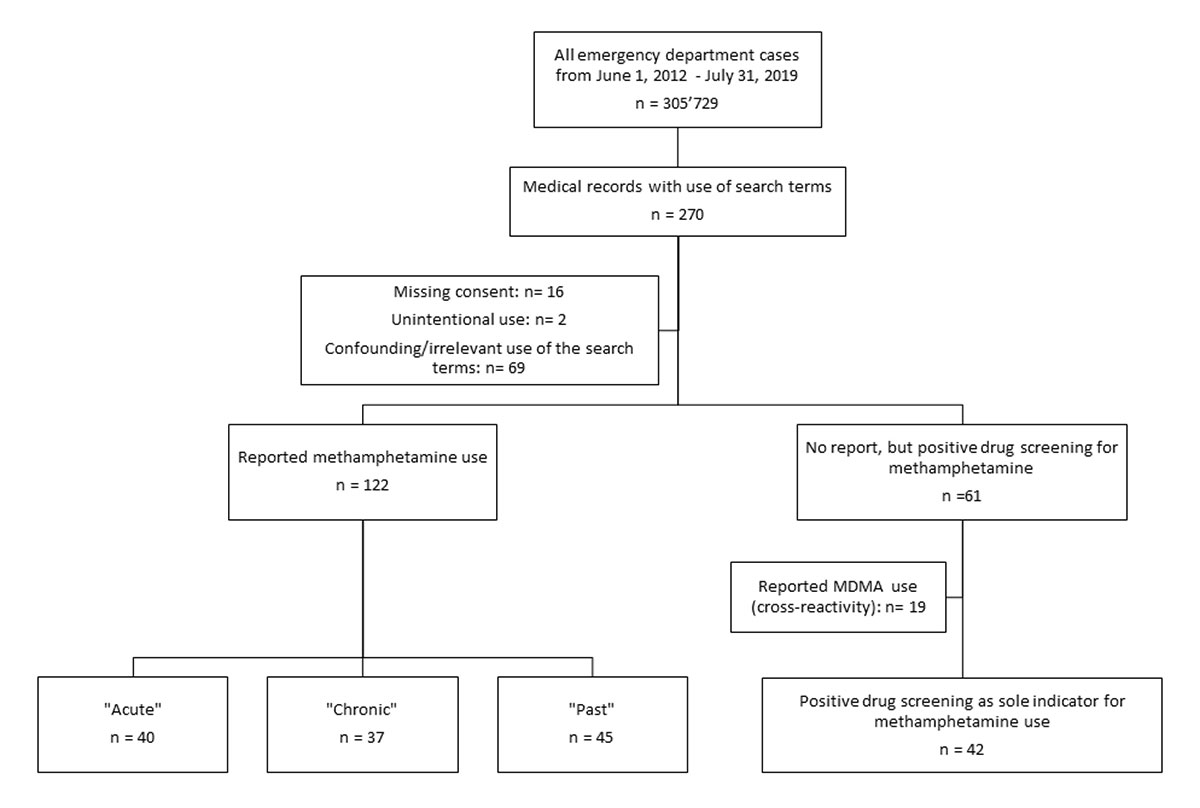
Figure 1 Flow-chart of included and excluded cases with reported methamphetamine use and cases with positive drug screening test for methamphetamine during the study period.
DOI: https://doi.org/10.4414/SMW.2021.w30099
Methamphetamine is a potent sympathomimetic substance and a highly addictive drug of abuse. It is the most widely used stimulant and second most commonly used illicit drug after cannabis worldwide [1]. Methamphetamine use is most prevalent in North America, Oceania and South-East Asia, but its global market has seen a steady increase and a geographical expansion over the past two decades [2, 3]. Its synthesis is fairly simple, resulting in numerous small-scale producers and leading to an affordable and widely available product [4]. It is a member of the phenylethylamine class and is a methylated derivative of amphetamine, but has more marked and longer lasting effects on the central nervous system than some other amphetamines, due to its high lipophilicity [5]. Methamphetamine can be used as crystals (“crystal meth”, “ice”), powder (“speed”, “crank”) [4] or tablets (“yaba”, “Pervitin” [6], “Thai pills” [7]), and can be orally ingested, snorted, inhaled (smoked) or injected intravenously [4, 5].
By increasing the intra-synaptic concentrations of dopamine, noradrenaline and serotonin in the central nervous system, methamphetamine causes physical and psychological arousal [8]. Effects include decreased appetite and drowsiness, increased alertness and concentration at low doses, and euphoria, psychomotor activation and sexual arousal at higher doses [4, 9, 10]. Physical effects of methamphetamine are a typical dose-dependent sympathomimetic toxidrome with mydriasis, hyperthermia, vasoconstriction, tachycardia and hypertension [4, 5]. This can lead to hyperthermic or hypertensive crises, haemorrhagic or ischaemic stroke, seizures, renal failure, vascular dissection, myocardial ischaemia, arrhythmia and sudden cardiac death [4, 9, 11, 12]. The half-life of methamphetamine is approximately 9–12 hours, but can vary considerably, and many users consume it in “binges” (repetitive use every few hours over several days) [4, 5]. Afterwards, a phase called “tweaking” follows, which is characterised by anxiety, short-temper, compulsive behaviour, delusions and paranoia [4, 8]. If no repeated administration follows, patients enter the “crash” phase, a period with prolonged, restless sleep, which can last more than a day [4]. Withdrawal symptoms, such as depressed mood, suicidal ideation, anxiety, disturbed sleep, strong drug craving and cognitive impairment are most severe 24–72 hours after the last administration, and gradually improve over 7–10 days [9, 12, 13]. Quick development of drug tolerance often leads to use of higher doses or more potent forms of the drug (crystals rather than powder or tablet) and to transitioning from ingestion or smoking to injection [12]. Chronic methamphetamine use impairs executive function and coping skills, which often presents with irritability, aggression, impulsivity and disorganisation [8]. Both intoxication and withdrawal can produce symptoms resembling psychiatric disorders, such as psychosis and paranoia, and significant agitation and aggression [14–16]. It is often such behavioural changes that lead to presentations to the emergency department (ED) [11].
In Western and Central Europe, methamphetamine use has historically been high in the Czech Republic and Slovakia, but increasing use of the drug has been reported throughout Europe, especially in the eastern part of Germany, Greece, Turkey and Northern Europe [17–21]. Since 2012, criminal offences (including use, possession, dealing, production and trafficking) related to methamphetamine have seen an increase in Switzerland [22]. A study assessing wastewater data and criminal offences showed a highly regional distribution, with Neuchâtel, Biel, Zurich and St Gallen showing the highest rates [23]. In 2013, two laboratories manufacturing methamphetamine were dismantled in the Cantons of Bern and Aargau, which indicates a local market for the product [7]. To our knowledge, no Swiss study has previously used an ED database as a source of insight specifically into methamphetamine users and their health problems, and ED-based studies about methamphetamine are sparse in Europe in general. The main objective of this study was to collect systematic data on the prevalence, susceptible groups and patterns of ED presentations with reported methamphetamine use at an urban ED in Switzerland.
This retrospective single-centre study involved a review of medical records of all patients admitted to the ED at the University Hospital of Bern with reported methamphetamine use between June 2012 and July 2019. The study was approved by the local ethics committee (No. KEK-BE/072/2015).
The ED of the University Hospital of Bern treats approximately 50,000 adult patients (age ≥16 years) a year (2019) and is both a tertiary (referral) and a primary care clinic. Patients younger than 16 years old are usually treated in a separate specialised emergency department for children and adolescents. Patients are most often seen by the interdisciplinary (surgical and internal) medicine emergency team, but can also be directly referred to an emergency physician of other disciplines, e.g., psychiatry or neurology. Treating physicians routinely ask patients about drug consumption habits, albeit not in a standardised manner. Urine drug screening tests are commonly obtained if drug use is suspected or clinically relevant.
Cases were retrieved from the electronic patient chart database (E.care 3.1.0, BVBA, ED 2.1.3.0, Turnhout, Belgium) using the search terms “crystal”, "methamphetamine", and street names for methamphetamine such as “ice” or “crank”, including misspelled and abbreviated terms (e.g., “crystel”, “crysthal”, “cristal”, “cristel”, “cristhal”, “methamp”, “metamp”, “methamf”, “metamf”). The search was conducted electronically in the diagnosis, medical history, clinical findings, consultations, evaluation, triage information and medical course fields of the reports, and was carried out by a clinical data manager. The retrieved cases were reviewed by one of the authors of the study (medical professional), and unclear cases were additionally reviewed with a senior physician who is also an author of the study. Irrelevant or confounding uses of the search terms in reference to another diagnosis or condition (e.g., “calcium pyrophosphate crystal deposition”) were removed manually. Included were patients presenting at the ED of the University Hospital of Bern with reported methamphetamine use. Methamphetamine use was identified on the basis of the patient’s self-report, information retrieved from witnesses or the judgement of the treating physician. Patients who reported unintentional methamphetamine consumption (e.g., spiked drinks) were excluded regardless of the result of the urine drug screening immunoassay. We also excluded cases in which patients had denied the hospital’s general consent to process their medical data for research purposes. Cases with a positive methamphetamine urine drug screening test with no further information available were described separately.
Based on the patient history, the included cases were categorised into three groups: “acute”, if patients presented within 72 hours of last reported use (main focus of the study), “chronic” in cases of regular use but not within the previous 72 hours, and “past” in cases of discontinued consumption, i.e., one-time, occasional or regular use in the past, but not within the previous 72 hours and no current regular use. The time window for the “acute” cases was chosen since acute effects, but also withdrawal symptoms such as depression and anxiety, can lead to ED presentation shortly after methamphetamine use, with the latter being most severe 24–72 hours after last administration [9, 13, 15].
The analysis included patient demographics (age, sex, psychiatric co-morbidities) and ED visit characteristics (hour and weekday of ED admission, ED primary care discipline, mode of ED admission, chief complaints, consulting services and triage level). The triage level was measured by a specially trained nurse using the Swiss Emergency Triage Scale, which classifies the urgency of treatment for patients presenting to an ED in five levels: 1. acute life-threatening problem; 2. high urgency; 3. urgency; 4. less urgency; 5. non-urgent problem. Methamphetamine use characteristics (form and route of use) and clinical outcome were analysed for the acute, chronic and past groups. For the acute group, clinical variables, laboratory results and required treatment (intubation, sedation, other) were also reported. Alcohol levels were measured either in blood serum, with alcohol breathalyser tests, or calculated from the osmolar gap [24, 25]. Clinical variables (if available) included reported and/or recorded symptoms, vital signs including peripheral capillary oxygen saturation, body temperature, and the Glasgow Coma Scale score. For the laboratory tests, the in-hospital laboratory normal value ranges were applied. Hypertension was defined as systolic blood pressure ≥140 mm Hg [26], hypotension as systolic blood pressure ≤100 mm Hg, tachycardia as heart rate ≥100/min, tachypnoea as respiratory rate >20/min and bradypnoea as respiratory rate <12/min [27]. The severity of intoxication was assessed by one of the authors of the study (medical professional) using the Poisoning Severity Score, a standardised scheme for grading severity of poisoning by taking the most severe clinical features into account and classifying outcomes as none, minor, moderate or severe toxicity, and death [28]. Data were analysed descriptively using Microsoft Excel software. Numerical data are presented as arithmetic mean and standard deviation (SD) or median and range, nominal data as proportion (%).
A urine drug screening immunoassay test (Triage® TOX Drug Screen, Alere Inc, since 2017 Quidel Inc, USA) [29] was used to screen for methamphetamine, as well as amphetamines, barbiturates, benzodiazepines, cocaine, methadone, opiates, phencyclidine, tricyclic antidepressants and tetrahydrocannabinol (THC). According to the manufacturer, the cut-off for methamphetamine detection was 1000 ng/ml for d-methamphetamine and 30,500 ng/ml for l-methamphetamine. Other substances that can also yield positive test results for methamphetamine (cross-reactivity) include 3,4-methylenedioxymethamphetamine (MDMA) (1500 ng/ml), 3,4-methylenedioxy-N-ethylamphetamine (MDEA) (4600 ng/ml), ethylamphetamine (12,500 ng/ml), isometheptine (100,000 ng/ml) and propylamphetamine (>200,000 ng/ml) [29].
From 1 June 2012 to 31 July 2019, 305,729 admissions to the ED were recorded in total; 122 cases with reports of methamphetamine use were included in the final analysis, corresponding to 0.04% of all ED presentations in this time period. The flow-chart of the included cases is provided in figure 1. Of the two cases with reported unintentional methamphetamine consumption, one suspected poisoning by a neighbour, and one (with positive drug screening test for amphetamines but not for methamphetamine) suspected a methamphetamine spiked-drink. Nineteen of the 61 patients with methamphetamine mentioned in their medical record solely due to a positive urine drug screening immunoassay test clearly stated they had used MDMA (cross-reactivity) and were not investigated further. The other 42 cases are described separately.
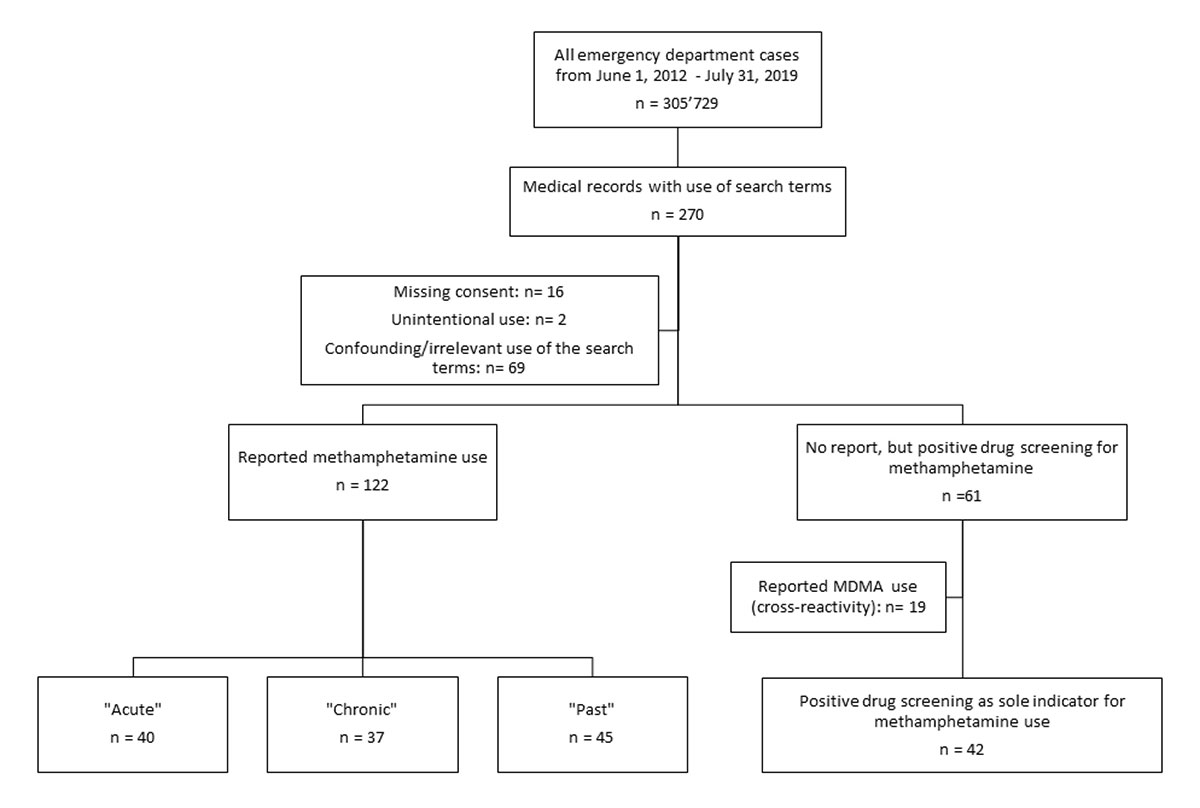
Figure 1 Flow-chart of included and excluded cases with reported methamphetamine use and cases with positive drug screening test for methamphetamine during the study period.
Some patients presented more than once within the study period, resulting in a total of 122 cases among 96 individuals. The annual distribution is shown in figure 2.
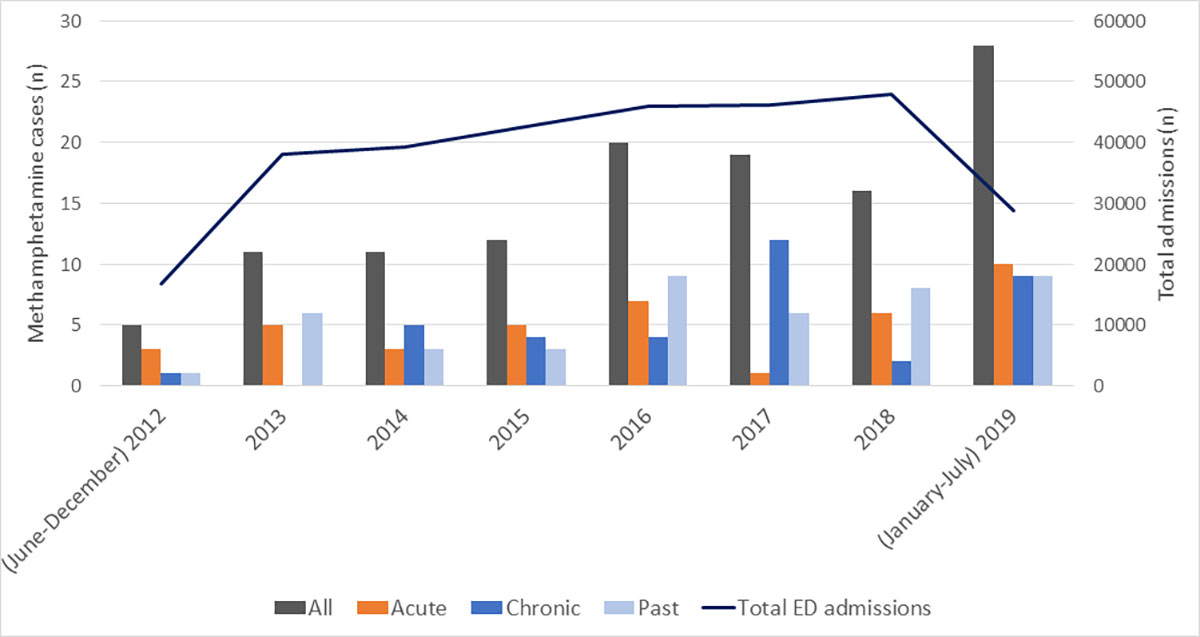
Figure 2 Annual distribution of total emergency department (ED) presentations (n = 305,729) and acute, chronic and past cases with reported methamphetamine use (n = 122).
In 40 cases, methamphetamine use in the past 72 hours was recorded. In 38 (95.0%) cases, patients self-reported methamphetamine use. In one case (2.5%) the ED triage had received information about methamphetamine intoxication from the pre-hospital emergency team, and in one case (2.5%) the patient was unable to provide any information, but the treating emergency physicians diagnosed methamphetamine intoxication. Two individuals presented twice and one patient presented five times within the observed time period, resulting in a total of 40 cases among 34 individuals. In most cases (n = 25, 62.5%), patients reported using crystal meth. Six patients (15%) reported using “Thai pills”, of whom four also consumed crystal meth. In 65% of all cases (n = 26), no information about the route of exposure was provided. Seven patients (17.5%) reported inhalation, four oral ingestion (10.0%), two snorting (5.0%) and one (2.5%) intravenous use. The mean age of the acute methamphetamine intoxication group was 29.5 years (SD 8.7, range 16–48), and they were predominantly male (75.0%). The demographic data and the ED visit characteristics of this group are described in table 1.
Table 1Demographics and emergency department (ED) visit characteristics of acute methamphetamine cases (n = 40).
| Sex, n (%) | Male | 30 (75.0) |
| Female | 10 (25.0) | |
| Age (years) mean ± SD | 29.5 ± 8.7 | |
| Age groups (years), n (%) | <20 | 6 (15.0) |
| 21–30 | 17 (42.5) | |
| 31–40 | 13 (32.5) | |
| >40 | 4 (10.0) | |
| Time of presentation, n (%) or median (range) | Night arrival (20:00 h – 08:00 h) | 19 (47.5) |
| Weekend arrival (Friday 17:00 h – Monday 08:00 h) | 15 (37.5) | |
| Average duration of ED visit | 3h 49 min (47 min – 10h 18min)* | |
| ED discipline, n (%) | Medicine | 14 (35.0) |
| Psychiatry | 13 (32.5) | |
| Surgery | 9 (22.5) | |
| Other | 4 (10.0) | |
| Triage level, n (%) | 1: acute life-threatening problem | 4 (10.0) |
| 2: high urgency | 17 (42.5) | |
| 3: urgency | 18 (45.0) | |
| 4: less urgency | 1 (2.5) | |
| 5: non-urgent problem | 0 (0) | |
| Mode of admission, n (%) | Ambulance | 9 (22.5) |
| Self-presentation | 16 (40.0) | |
| Police | 10 (25.0) | |
| Physician referral | 6 (15.0) |
SD: standard deviation
* Not recorded in one case
Eighteen (45.0%) patients had one or more documented psychiatric disorders. Most common was a previously recorded or newly diagnosed substance dependence disorder (n = 12, 30.0%). Five patients (12.5%) had borderline personality disorder and three (7.5%) had a diagnosis of depression (past or present). Other recorded psychiatric co-morbidities included attention deficit hyperactive disorder (n = 2, 5.0%), anxiety disorder (n = 2, 5.0%), schizophrenia, eating disorder, suicidal ideation, and post-traumatic stress disorder (each n = 1, 2.5%).
Six patients (15.0%) reported exclusive methamphetamine use, one no substance use (2.5%), and the majority (n = 33, 82.5%) multiple substance use (whether current or in general). The most commonly reported co-used substances were alcohol (55.0%), cocaine (50.0%) and cannabis (37.5%) (table 2).
Table 2Reported co-used substances (current and/or in general) in acute methamphetamine cases (n = 40).
| No. of cases (%) | |
| Alcohol | 22 (55.0) |
| Cocaine | 20 (50.0) |
| Cannabis | 15 (37.5) |
| Amphetamines (excluding methamphetamine and MDMA) | 6 (15.0) |
| Heroin | 6 (15.0) |
| Benzodiazepines | 4 (10.0) |
| Methadone | 2 (5.0) |
| ᵞ-Hydroxybutyric acid (GHB) | 2 (5.0) |
| Lysergic acid diethylamide (LSD) | 2 (5.0) |
| MDMA | 2 (5.0) |
| Opiates/opioids (excluding methadone and heroin) | 1 (2.5) |
| Poppers | 1 (2.5) |
MDMA: 3,4-methylenedioxymethamphetamine
The chief complaints noted by the triage were signs of intoxication (n = 13, 32.5%) and psychiatric symptoms (n = 13, 32.5%). Seven patients (17.5%) presented because of trauma and seven (17.5%) because of other medical complaints. Three patients (7.5%) required immediate medical care in the shock room with the trauma team or other specialists (anaesthesiologist, radiologist, cardiologist or others) standing by, and one patient (2.5%) with mixed intoxication (crystal meth, alcohol and heroin) had to be intubated. The psychiatric emergency team was consulted in five cases (12.5%) where they were not the primary care discipline, and the internal medicine and the gastroenterology teams were consulted in one case each (2.5%).
The clinical data of these patients are presented in table 3; hypertension (27.5%), tachycardia (27.5%), agitation (27.5%) and sleeping disturbance (25.0%) were the most frequent symptoms. Behavioural disturbances (restlessness, agitation and/or aggression) were documented in 16 cases (40.0%) overall.
Table 3Reported or recorded symptoms and clinical characteristics in acute methamphetamine cases (n = 40).
| No. of cases (%) | ||
| Cardiovascular | Hypertension1 | 11 (27.5) |
| Tachycardia1 | 11 (27.5) | |
| Chest pain | 3 (7.5) | |
| Hypotension1 | 1 (2.5) | |
| Arrhythmia | 1 (2.5) | |
| Pulmonary | Dyspnoea | 3 (7.5) |
| Hypoxia requiring supplemental oxygen2 | 2 (5.0) | |
| Apnoea/bradypnoea3 | 1 (2.5) | |
| Tachypnoea3 | 1 (2.5) | |
| Psychiatric | Agitation | 11 (27.5) |
| Sleeping disturbance | 10 (25.0) | |
| Aggression | 8 (20.0) | |
| Restlessness | 6 (15.0) | |
| Hallucinations | 5 (12.5) | |
| Paranoia | 5 (12.5) | |
| Suicidal ideation | 3 (7.5) | |
| Fear | 2 (5.0) | |
| Self-mutilation | 1 (2.5) | |
| Depression | 1 (2.5) | |
| Neurological | Mydriasis | 6 (15.0) |
| Impaired consciousness (GCS score 9–14)4 | 4 (10.0) | |
| Miosis | 3 (7.5) | |
| Confusion | 3 (7.5) | |
| Dizziness | 3 (7.5) | |
| Impaired gait | 2 (5.0) | |
| Paraesthesia | 2 (5.0) | |
| Amnesia | 1 (2.5) | |
| Visual disturbance | 1 (2.5) | |
| Unconsciousness (GCS score <9)4 | 1 (2.5) | |
| Gastrointestinal | Impaired appetite | 7 (17.5) |
| Emesis | 6 (15.0) | |
| Nausea | 3 (7.5) | |
| Gastrointestinal bleeding | 2 (5.0) | |
| Abdominal pain | 1 (2.5) | |
| Constipation | 1 (2.5) | |
| Miscellaneous | Trauma | 6 (15.0) |
| Exhaustion | 1 (2.5) | |
| Generalised pain | 1 (2.5) | |
| Epistaxis | 1 (2.5) | |
| Urinary retention | 1 (2.5) |
GCS: Glasgow Coma Scale
1 Blood pressure and heart rate not recorded in 17 cases; 2 oxygen saturation not recorded in 18 cases; 3 respiratory rate not recorded in 32 cases; 4 GCS not recorded in 20 cases
A urine drug screening test was performed in 14 (35.0%) cases and was positive for methamphetamine in nine cases (64.3% of the samples, 22.5% of all acute cases). Other analytically detected substances were amphetamines (eight cases), benzodiazepines and THC (four cases each), cocaine (three cases) and opiates (one case). The urine immunoassay was positive for more than one substance in 10 of the cases, positive for one substance in three and negative for all tested substances in one case. In 11 cases, alcohol levels were documented. In three of those, no alcohol was detected, and in eight cases alcohol was detected with a median concentration of 1.12‰ (range 0.06–2.82‰), though the method of detection was not indicated in all cases.
In 18 cases, further laboratory analyses were performed. Noteworthy results included high white blood cell count and elevated serum creatinine (nine cases each), high red blood cell count, decreased potassium and elevated creatine kinase (four cases each, though results for potassium were not available in 12 and for creatine kinase in 11 cases with laboratory analysis), elevated transaminases (three cases, not available in 13 cases with laboratory analysis), and decreased glucose (one case, not available in three cases with laboratory analysis), though it could not be evaluated whether these values were pre-existing or due to acute methamphetamine intoxication.
Twenty-nine patients (72.5%) required some form of treatment, of whom seven (17.5% of all acute cases) had to be sedated with benzodiazepines. Twenty-five patients (62.5%) required some other form of treatment, including analgesics, antiemetics, antibiotics, tetanus-boosters or further treatment during hospitalisation. The severity of poisoning and the outcome of the acute cases are shown in table 4; among the three severe cases, one had reportedly consumed only crystal meth, whereas the other two had consumed multiple substances.
Table 4Severity of poisoning and mode of release in acute methamphetamine cases (n = 40).
| No. of cases (%) | ||
| Severity of poisoning | None | 6 (15.0) |
| Minor | 12 (30.0) | |
| Moderate | 19 (47.5) | |
| Severe | 3 (7.5) | |
| Fatal | 0 (0) | |
| Mode of release | Medically discharged | 22 (55.0) |
| Admission to psychiatric clinic | 14 (35.0) | |
| Admission to intensive care unit | 1 (2.5) | |
| Admission to cardiology intermediate care unit | 1 (2.5) | |
| Admission to another hospital ward | 1 (2.5) | |
| Admission to prison ward of the University Hospital | 1 (2.5) |
In 37 cases, patients reported regular methamphetamine use, but not within the past 72 hours. Two patients presented three times and one presented twice, resulting in 31 individuals among the 37 cases. Five of these patients also presented in the “acute” group. Twenty-three (62.2%) reported using crystal meth and two (5.4%) reported “Thai pill” consumption (one consumed both), whereas the rest (n = 12, 32.4%) did not specify what form of methamphetamine they used. Oral ingestion and inhalation were reported in two cases (5.4%) each, and the route of exposure remained unclear in the rest (n = 33, 89.2%). Thirty-five (94.6%) patients reported multiple substance use, most commonly alcohol (n = 8, 21.6%) and cocaine (n = 6, 16.2%). Twenty-six patients (70.3%) were male and the mean age was 30.9 years (SD 11.0, range 16–63). Fifteen patients (40.5%) presented on the weekend and 16 (43.2%) at night. Seventeen patients (45.9%) presented due to psychiatric symptoms, nine (24.3%) because of medical problems, eight (12.6%) because of intoxication and three (8.1%) due to trauma. Patients were most often admitted to the medical emergency team (n = 15, 40.5%) or the psychiatric emergency physician (n = 14, 37.8%). If admitted to a different ED discipline, psychiatric consulting services were required in eight cases (21.6%). In 27 cases (73.0%), patients had one or more documented psychiatric disorders, of whom 19 (51.4%) had a diagnosed substance dependence disorder. Other common diagnoses were emotionally unstable personality disorder (n = 7, 18.9%), schizophrenia (n = 5, 13.5%) and mood disorders (n = 4, 10.8%). Twenty patients (54.1%) were medically discharged, 10 (27.0%) were admitted to a psychiatric clinic, 4 (10.8%) were hospitalised, 2 (5.4%) were taken into police custody, and one (2.7%) was transferred to an intensive care unit at another hospital.
In 45 cases, patients reported methamphetamine consumption at least once in the past, but no longer regular use, and not within the past 72 hours. Four patients presented twice and one three times, resulting in 39 individuals among these 45 cases. None of these patients presented in the “acute” group. In 33 cases (73.3%), patients reported having used crystal meth, one (2.2%) reported “Thai pill” consumption (as well as crystal meth), and 12 (26.7%) did not further specify the form of methamphetamine used. Inhalation was reported in two cases (4.4%) and intravenous use once (2.2%), and the route of exposure remained unclear in 42 (93.3%) cases. Thirty-nine patients (86.7%) reported multiple substance use, most commonly alcohol and cocaine (n = 12, 26.7% each). These patients too were mostly male (n = 31, 68.9%), with a mean age of 29.8 years (SD 8.6, range 17–58). Sixteen patients (35,6%) presented on the weekend and 15 (33,3%) at night. In 22 cases (48.9%) medical problems (e.g., abdominal pain, dyspnoea, or headache) prompted presentation to the medical emergency team (n = 18, 40%). Psychiatric symptoms were the reason for admission in 11 cases (24.4%), and patients required psychiatric services, either as the primary care discipline or as a consulting service, in 12 (26.7%) and 9 (20%) cases, respectively. Psychiatric disorders were documented in 27 cases (60.0%), most commonly substance dependence disorder (n = 20, 44.4%) and mood disorders (n = 10, 22.2%). Twenty-eight patients (62.2%) were medically discharged, nine patients (20.0%) were admitted to a psychiatric clinic, six (13.3%) were hospitalised, one (2.2%) was transferred to the hospital prison ward of the university hospital, and one (2.2%) was discharged to a normal prison.
In 42 cases, a positive urine immunoassay was the sole indicator for methamphetamine use (i.e., no reported/documented use of methamphetamine or MDMA, which can yield false positive results for methamphetamine with the immunoassay used in this study). In these cases, it was unclear which substance the patients had used, often because they themselves were not certain what drug they had consumed. These patients most commonly presented at night (n = 22, 52.4%) and on weekends (n = 29, 69.0%), and were typically young (mean age 28.4 years, SD 9.4, range 18–49 years) and male (n = 29, 69.0%). Fourteen patients (33.3%) presented due to intoxication, 11 (26.2%) due to trauma, and nine (21.4%) due toother medical symptoms (e.g., confusion, loss of consciousness or vomiting).
Based on our findings, despite a slight increase in the yearly ED presentations of patients reporting methamphetamine use (corresponding in part to an increase in the total of ED admissions), the overall numbers remained low and a considerable number of individuals presented more than once during the study period. The typical patient was young and male and required psychiatric services – either as the primary care discipline or as a consulting service – in approximately half of all cases. Patients in the acute group most commonly presented with psychiatric symptoms and/or a sympathomimetic toxidrome, were frequently aggressive or agitated, and often required pre-hospital resources such as police and ambulance services. Pharmacological treatment, mostly sedatives, was often required, but very few cases needed shock room treatment or intubation. Nearly half of the acute cases had a psychiatric diagnosis and a great majority were polydrug users, with cocaine and cannabis being the most frequently co-used illicit substances. The majority of all patients were medically discharged, but admissions to a psychiatric clinic were frequent (highest in the acute group and lowest in the past group).
Previous studies investigating methamphetamine-related ED presentations were mostly set in the Unites States and Australia, where methamphetamine-related health problems account for 1–2.4% of all ED visits [14, 15, 30]. In line with such reports [11, 14, 30–35], patients in this study were mostly young males and not infrequently required police accompaniment or ambulance services in the acute group [11, 14, 33, 35]. The substantial use of pre-hospital resources is likely due to the adverse behavioural effects of methamphetamine, such as agitation and aggression, which have been shown to be prominent in methamphetamine-related ED presentations [11, 14, 35, 36]. These behavioural disturbances also put a strain on in-hospital resources, such as staff and security services [11]. Methamphetamine is known to induce psychosis with paranoia and hallucinations [12, 37], which was also encountered in our patients in the acute group. A quarter of all patients in the acute group reported sleeping disturbances, which is another well-described problem among methamphetamine users [13]. These psychiatric problems may account for the high rate of direct admissions to the psychiatric emergency team – as has also been shown by several other studies from areas where methamphetamine use is common [10, 16, 30, 36]. Chronic methamphetamine use has previously been shown to be associated with psychiatric disorders, including mood and anxiety disorders, psychosis, and cognitive impairment [12]. In a study interviewing regular methamphetamine users with psychotic symptoms, 70% reported a previously diagnosed psychiatric disorder [10]. However, it is difficult to discern the relationship between pre-existing psychiatric disorders with concurrent methamphetamine use and methamphetamine-induced psychiatric disorders [10].
Rhabdomyolysis and subsequent renal failure due to excessive muscular activity during periods of agitation has been reported [5, 11]. Considering the elevated red blood cell count in some cases in the acute group, dehydration due to hyperthermia might be another explanation for impaired kidney function. Elevated white blood cell count has been described in a study analysing amphetamine intoxication, and might be explained by the stress response induced by stimulants. Interestingly, cocaine does not appear to cause leucocytosis, possibly because of cocaine’s shorter half-life or other pharmacological differences [38].
Compared with another study with a similar design, a urine drug screening test was performed in a relatively high percentage of our acute cases (35% vs 10%) [11], which might be due to differences in routinely performed diagnostic procedures in various hospitals and regions. The negative methamphetamine test results in some of the acute cases in our study may be explained by the limited time frame for detectability [39], concentrations below the cut-off value of the assay [40], or because patients had falsely believed they had consumed methamphetamine. The limitations of the immunoassay have also been shown in a study comparing the detection of psychoactive substances with immunoassays and mass spectrometry, which found a relatively high discrepancy for amphetamine-type substances [40]. Although additional analytical methods (e.g., liquid or gas chromatography combined with mass spectrometry) can provide valuable information in cases with equivocal immunoassay results, those methods are more costly and time-consuming than the rapid immunoassay tests and thus of limited use in an ED setting [40]. Detection of benzodiazepines may be explained in some cases by having sampled urine after iatrogenic administration.
Methamphetamine has not been the focus of studies analysing drug-related ED visits in Switzerland so far. Cannabis and cocaine are the most widely used illicit drugs in Europe [18] and also the most frequently reported substances in drug-related ED presentations in other Swiss studies [31, 41, 42]. In line with these findings, methamphetamine users in this study also most frequently reported co-use of cocaine and cannabis, which have previously been found to be the most commonly co-used substances in methamphetamine users [10]. Compared with users of other substances, patients in the acute methamphetamine group in this study were more often admitted to a psychiatric clinic (35%) than patients with ED visits related to use of cocaine (19%) [43] and other substances (2-–22%) [31, 41, 42]. ED admissions in the acute group were fairly evenly distributed throughout the day and week, suggesting that methamphetamine users are not predominantly weekend party-drug users. This correlates with wastewater findings throughout Europe, possibly reflecting more regular consumption habits among methamphetamine users [44]. Methamphetamine users are known to most often be polydrug users [10, 11, 32, 34, 36]. Although combining other drugs with methamphetamine does not produce a more toxic metabolite (as is the case with cocaethylene when combining alcohol and cocaine), co-use of other substances can amplify toxic effects and increase the likelihood for complications [12].
Analysing the extent of methamphetamine use leading to ED visits in Switzerland in the past is challenging, since most other studies did not analyse methamphetamine use separately. In previous Swiss studies, use of amphetamines, including methamphetamine , was reported in 3–9% of cases presenting to an ED because of recreational drug use [31, 41, 42]. Since use of other amphetamines is currently more common in Western and Central Europe [18], it is likely that only a small number of these were methamphetamine users, but changes in trends may potentially be missed. From 1997–2009 the Swiss Toxicological Information Centre was consulted in only 41 cases with methamphetamine intoxication, which suggests that methamphetamine has not been a common drug of choice in Switzerland in the past [45]. However, it should be noted that the spread of crystal meth from Czechia to Eastern Germany has increased its availability in Switzerland in the past two decades [7], and that the majority of patients in this study reported using crystal meth, the most potent form of methamphetamine associated with a higher likelihood of dependence [9]. A considerable number of patients also reported consuming methamphetamine powder compressed into tablets, locally known as “Thai pills” [7]. A practice known as “slamming”, which involves injecting methamphetamine during “chemsex” parties, currently does not appear to be common in Switzerland [7].
Although the spread of methamphetamine appears to be impeded by the availability and popularity of other stimulant drugs, most notably cocaine, but also amphetamine and MDMA [19], stimulant drugs can coexist in some markets by acting as substitutes for each other [2]. If the availability, price, or quality of other stimulant drugs such as amphetamine, cocaine and MDMA should change, methamphetamine could quickly gain popularity [7]. The European market for stimulant drugs is large, and these substances may be interchangeable to a certain degree, with users sometimes being unaware which particular drug they are consuming. Data suggest that methamphetamine use is spreading in Europe, and many of the indicators of drug use – such as urine immunoassay drug screening tests – are ill-adapted to distinguish between different amphetamines and methamphetamine [1]. Considering the significant acute and chronic health problems associated with methamphetamine use and the quick shifts in drug markets, continued drug monitoring and education for healthcare professionals should be a priority in the near future.
The findings in this study are limited by its retrospective design, the low number of cases and the quality of documentation. A reporting bias cannot be excluded, since patients were not asked about drug use in a standardised manner and some may have given incorrect reports, either because they wrongly believed they had consumed methamphetamine or were unwilling to report methamphetamine use. Certain clinical parameters (e.g., Glasgow Coma Scale score, respiratory rate) and laboratory values were not always obtained (e.g., in the case of patients who were assessed by a psychiatric emergency physician only), and the laboratory data cannot be conclusively interpreted, as they were not compared with previous values. A number of patients were excluded from the analysis because of withheld consent. Causality between methamphetamine use and ED visits was sometimes difficult to ascertain in the acute group, despite the reported temporal relation (maximum 72 hours after last use). The number of cases with confirmation by a urine immunoassay was relatively low and the majority of the cases were diagnosed based on their medical history. However, this is in line with current clinical practice in an ED setting, where laboratory results are not always readily available and patient management is mainly based on the patient’s report and clinical presentation. The high incidence of multiple substance use may also give a skewed impression of the clinical presentation. The number of ED presentations with reports of methamphetamine use does not necessarily indicate trends of use in the general population.
Strengths of this study include the long observation period and the large patient population. We had access to detailed documentation of patient and clinical data, which allowed for more insight than studies based on coded diagnoses or analysis of poison centre data. By combining the patient’s self-report, urine drug screening tests and clinicians’ judgement, we used every method available to increase the quality of the results, as suggested by Jones et al. in their literature review on methamphetamine-related ED presentations [15].
In conclusion, this retrospective study at a large urban ED in Bern, Switzerland over a 7-year study period revealed only a small number (0.04%) of ED presentations with reports of methamphetamine use. The global popularity of methamphetamine and the significant pre- and in-hospital resources often required may warrant further research in other parts of Switzerland and Europe to estimate the prevalence of methamphetamine use and prepare EDs for methamphetamine -related health problems (most commonly sympathomimetic and psychiatric symptoms).
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
We thank David Fagerdahl for proofreading and language editing.
1. European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) and Europol . Methamphetamine in Europe: EMCDDA-Europol Threat assessment 2019. Luxembourg: Publications Office of the European Union. 2019. doi: https://www.emcdda.europa.eu/publications/joint-publications/methamphetamine-threat-assessment_en
2. United Nations Office on Drugs and Crime (UNODC) . World Drug Report 2020: Executive Summary. Vienna: United Nations publications. 2020. doi: https://reliefweb.int/report/world/unodc-world-drug-report-2020
3. United Nations Office on Drugs and Crime (UNODC) . World Drug Report 2020: Drug Supply. Vienna: United Nations publications. 2020. doi: https://reliefweb.int/report/world/unodc-world-drug-report-2020
4. Logan BK . Methamphetamine - Effects on human performance and behavior. Forensic Sci Rev. 2002 Feb;14(1-2):133–51.
5. Schep LJ , Slaughter RJ , Beasley DM . The clinical toxicology of metamfetamine. Clin Toxicol (Phila). 2010 Aug;48(7):675–94. https://doi.org/10.3109/15563650.2010.516752
6. European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) and Europol . Methamphetamine – A European Union perspective in the global context. Luxembourg: Publications Office of the European Union. 2009.
7. Zobel F , Schneider C . (fedpol), Marthaler M. Neue Tendenzen im Drogenbereich (NTD) - Methamphetamin in der Schweiz. Lausanne: Sucht Schweiz. 2015.
8. Panenka WJ , Procyshyn RM , Lecomte T , MacEwan GW , Flynn SW , Honer WG , et al. Methamphetamine use: a comprehensive review of molecular, preclinical and clinical findings. Drug Alcohol Depend. 2013 May;129(3):167–79. https://doi.org/10.1016/j.drugalcdep.2012.11.016
9. Cruickshank CC , Dyer KR . A review of the clinical pharmacology of methamphetamine. Addiction. 2009 Jul;104(7):1085–99. https://doi.org/10.1111/j.1360-0443.2009.02564.x
10. Lecomte T , Mueser KT , MacEwan WG , Laferrière-Simard MC , Thornton AE , Buchanan T , et al. Profiles of individuals seeking psychiatric help for psychotic symptoms linked to methamphetamine abuse – baseline results from the MAPS (methamphetamine and psychosis study). Ment Health Subst Use. 2010;3(3):168–81. https://doi.org/10.1080/17523281.2010.504645
11. Isoardi KZ , Ayles SF , Harris K , Finch CJ , Page CB . Methamphetamine presentations to an emergency department: management and complications. Emerg Med Australas. 2019 Aug;31(4):593–9. https://doi.org/10.1111/1742-6723.13219
12. Darke S , Kaye S , McKetin R , Duflou J . Major physical and psychological harms of methamphetamine use. Drug Alcohol Rev. 2008 May;27(3):253–62. https://doi.org/10.1080/09595230801923702
13. McGregor C , Srisurapanont M , Jittiwutikarn J , Laobhripatr S , Wongtan T , White JM . The nature, time course and severity of methamphetamine withdrawal. Addiction. 2005 Sep;100(9):1320–9. https://doi.org/10.1111/j.1360-0443.2005.01160.x
14. Bunting PJ , Fulde GW , Forster SL . Comparison of crystalline methamphetamine (“ice”) users and other patients with toxicology-related problems presenting to a hospital emergency department. Med J Aust. 2007 Nov;187(10):564–6. https://doi.org/10.5694/j.1326-5377.2007.tb01417.x
15. Jones R , Woods C , Usher K . Rates and features of methamphetamine-related presentations to emergency departments: an integrative literature review. J Clin Nurs. 2018 Jul;27(13-14):2569–82. https://doi.org/10.1111/jocn.14493
16. Cloutier RL , Hendrickson RG , Fu RR , Blake B . Methamphetamine-related psychiatric visits to an urban academic emergency department: an observational study. J Emerg Med. 2013 Jul;45(1):136–42. https://doi.org/10.1016/j.jemermed.2012.11.094
17. United Nations Office on Drugs and Crime (UNODC) . World Drug Report 2020: Drug Use an Health Consequences. Vienna: United Nations publications. 2020. doi: https://reliefweb.int/report/world/unodc-world-drug-report-2020
18. European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) . European Drug Report 2020: Trends and Developments. Luxembourg: Publications Office of the European Union; 2020. 2020.
19. Griffiths P , Mravcik V , Lopez D , Klempova D . Quite a lot of smoke but very limited fire—the use of methamphetamine in Europe. Drug Alcohol Rev. 2008 May;27(3):236–42. https://doi.org/10.1080/09595230801932588
20. Ort C , van Nuijs AL , Berset JD , Bijlsma L , Castiglioni S , Covaci A , et al. Spatial differences and temporal changes in illicit drug use in Europe quantified by wastewater analysis. Addiction. 2014;109(8):1338-52. doi: https://www.ncbi.nlm.nih.gov/pubmed/24861844. PubMed PMID: 24861844; PubMed Central PMCID: PMCPMC4204159.
21. European Monitoring Center for Drugs and Drug Addiction (EMCDDA) . Exploring methamphetamine trends in Europe. EMCDDA Papers Luxembourg: Publications Office of the European Union; 2014. 2014.
22. Gamma A , Schleifer R , Weinmann W , Buadze A , Liebrenz M. Could Google trends be used to predict methamphetamine-related crime? An analysis of search volume data in Switzerland, Germany, and Austria. PLoS One. 2016;11(11):e0166566. doi: https://doi.org/10.1371/journal.pone.0166566. PubMed PMID: 27902717; PubMed Central PMCID: PMCPMC5130206.
23. Been F , Bijlsma L , Benaglia L , Berset JD , Botero-Coy AM , Castiglioni S , et al. Assessing geographical differences in illicit drug consumption—A comparison of results from epidemiological and wastewater data in Germany and Switzerland. Drug Alcohol Depend. 2016 Apr;161:189–99. https://doi.org/10.1016/j.drugalcdep.2016.02.002
24. Lynd LD , Richardson KJ , Purssell RA , Abu-Laban RB , Brubacher JR , Lepik KJ , et al. An evaluation of the osmole gap as a screening test for toxic alcohol poisoning. BMC Emerg Med. 2008;8:5. doi: https://doi.org/10.1186/1471-227X-8-5. PubMed PMID: 18442409; PubMed Central PMCID: PMCPMC2390580.
25. Aderjan R , Daldrup T , Käferstein H , Krause D , Musshoff F , Paul LD . Richtlinien zur Bestimmung der Blutalkoholkonzentration (BAK) für forensische Zwecke der Deutschen Gesellschaft für Rechtsmedizin. Gesellschaft für Toxikologische und Forensische Chemie und Deutschen Gesellschaft für Verkehrsmedizin. 2011;48(3):137–43.
26. Williams B , Mancia G , Spiering W , Agabiti Rosei E , Azizi M , Burnier M , et al.; ESC Scientific Document Group . 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018 Sep;39(33):3021–104. https://doi.org/10.1093/eurheartj/ehy339
27. Park SB , Khattar D . Tachypnea. StatPearls. Treasure Island (FL)2021.
28. Persson HE , Sjöberg GK , Haines JA , Pronczuk de Garbino J . Poisoning severity score. Grading of acute poisoning. J Toxicol Clin Toxicol. 1998;36(3):205–13. https://doi.org/10.3109/15563659809028940
29. Alere TM . Triage® TOX Drug Screen Product Insert. Rapid qualitative simultaneous detection of drug and/or the major urinary metabolites of 10 different drug classes (11 unique assays). Available from: https://www.quidel.com/sites/default/files/2972E8590A6600494C.pdf. ed2016.
30. Hendrickson RG , Cloutier R , McConnell KJ . Methamphetamine-related emergency department utilization and cost. Acad Emerg Med. 2008 Jan;15(1):23–31. https://doi.org/10.1111/j.1553-2712.2007.00006.x
31. Liakoni E , Muller S , Stoller A , Ricklin M , Liechti ME , Exadaktylos AK . Presentations to an urban emergency department in Bern, Switzerland associated with acute recreational drug toxicity. Scand J Trauma Resusc Emerg Med. 2017;25(1):26. doi: https://doi.org/10.1186/s13049-017-0369-x. PubMed PMID: 28264690; PubMed Central PMCID: PMCPMC5340017.
32. Swanson SM , Sise CB , Sise MJ , Sack DI , Holbrook TL , Paci GM . The scourge of methamphetamine: impact on a level I trauma center. J Trauma. 2007 Sep;63(3):531–7. https://doi.org/10.1097/TA.0b013e318074d3ac
33. Richards JR , Bretz SW , Johnson EB , Turnipseed SD , Brofeldt BT , Derlet RW . Methamphetamine abuse and emergency department utilization. West J Med. 1999;170(4):198-202. PubMed PMID: 10344172; PubMed Central PMCID: PMCPMC1305548.
34. Mattson ME . Emergency department visits involving methamphetamine: 2007 to 2011. The CBHSQ report. 2013:1-7. PubMed PMID: 27606402; PubMed Central PMCID: PMCPMID27606402.
35. Jones R , Woods C , Barker R , Usher K . Patterns and features of methamphetamine-related presentations to emergency departments in QLD from 2005 to 2017. Int J Ment Health Nurs. 2019 Aug;28(4):833–44. https://doi.org/10.1111/inm.12618
36. Toles M , Jiang CS , Goebert D , Lettich L . Methamphetamine in emergency psychiatry. Addict Disord Their Treat. 2006;5(4):191–9. https://doi.org/10.1097/01.adt.0000210076.53993.05
37. Pasic J , Russo JE , Ries RK , Roy-Byrne PP . Methamphetamine users in the psychiatric emergency services: a case-control study. Am J Drug Alcohol Abuse. 2007;33(5):675–86. https://doi.org/10.1080/00952990701522732
38. Richards JR , Farias VF , Clingan CS . Association of leukocytosis with amphetamine and cocaine use. ScientificWorldJournal. 2014;2014:207651. doi: https://doi.org/10.1155/2014/207651. PubMed PMID: 24578625; PubMed Central PMCID: PMCPMC3919105.
39. Swiss Guidelines Committee for Drugs of Abuse Testing (SCDAT) . Richtlinien für Suchtstoffanalytik. 2021(Version EN). Epub 2021-03-25.
40. Liakoni E , Yates C , Dines AM , Dargan PI , Heyerdahl F , Hovda KE , et al. Acute recreational drug toxicity: Comparison of self-reports and results of immunoassay and additional analytical methods in a multicenter European case series. Medicine (Baltimore). 2018;97(5):e9784. doi: https://doi.org/10.1097/MD.0000000000009784. PubMed PMID: 29384873; PubMed Central PMCID: PMCPMC5805445.
41. Liakoni E , Dolder PC , Rentsch K , Liechti ME . Acute health problems due to recreational drug use in patients presenting to an urban emergency department in Switzerland. Swiss Med Wkly. 2015 Jul;145:w14166. https://doi.org/10.4414/smw.2015.14166
42. Liakoni E , Dolder PC , Rentsch KM , Liechti ME . Presentations due to acute toxicity of psychoactive substances in an urban emergency department in Switzerland: a case series. BMC Pharmacol Toxicol. 2016;17(1):25. doi: https://doi.org/10.1186/s40360-016-0068-7. PubMed PMID: 27228985; PubMed Central PMCID: PMCPMC4882845.
43. Bodmer M , Enzler F , Liakoni E , Bruggisser M , Liechti ME . Acute cocaine-related health problems in patients presenting to an urban emergency department in Switzerland: a case series. BMC Res Notes. 2014;7:173. doi: https://doi.org/10.1186/1756-0500-7-173. PubMed PMID: 24666782; PubMed Central PMCID: PMCPMC3987164.
44. European Monitoring Center for Drugs and Drug Addiction (EMCDDA) . Wastewater analysis and drugs: a European multi-city study. Perspectives on Drugs 2020. 2020. doi: https://www.emcdda.europa.eu/publications/html/pods/waste-water-analysis_en
45. Bruggisser M , Ceschi A , Bodmer M , Wilks MF , Kupferschmidt H , Liechti ME . Retrospective analysis of stimulant abuse cases reported to the Swiss Toxicological Information Centre during 1997-2009. Swiss Med Wkly. 2010 Oct;140:w13115. https://doi.org/10.4414/smw.2010.13115