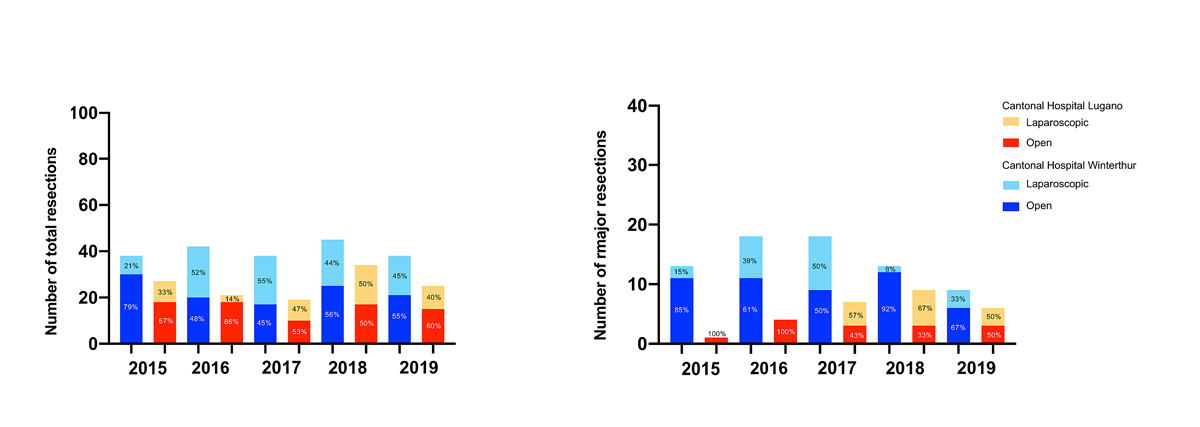
Figure 1 Number of total and major liver resections per year.
DOI: https://doi.org/10.4414/SMW.2021.w30044
Charlson Comorbity Index
Enhanced Recovery After Surgery
International Normalised Ratio
International Study Group of Liver Surgery
The first laparoscopic hepatectomy was performed 30 years ago. However, in contrast to the rapid and universal adoption of laparoscopic gallbladder, colorectal and gastric surgery, liver surgeons overall remain reluctant to fully implement the laparoscopic or robotic approach for liver resections [1]. The sophistication required for positioning of the patient for laparoscopy and the long learning curve to acquire techniques to control intraoperative bleeding allowed only a slow diffusion of the technique. The use of laparoscopy for major hepatectomy (>3 segments according to Brisbane) has become the routine approach in only a few centres worldwide [26].
Two international consensus conferences were organised to assess progress in this field. The first conference lead to the “Louisville Statement from 2009” and concluded that minor laparoscopic hepatectomies are safe in centres with experience, whereas major laparoscopic hepatectomies were still considered experimental [7]. Five years later, the second consensus conference in Morioka recommended a “cautious” introduction of major resections [3]. Since lesions requiring minor resections are more common in most centres, and new trainees are increasingly comfortable with laparoscopy, the laparoscopic technique for minor liver resections has now become a widely accepted standard using energy devices. In the meanwhile, the laparoscopic approach remains the exception for major resections.
A prospective randomised trial of laparoscopic versus open parenchymal sparing liver resections from Norway demonstrated improved clinical outcomes with less blood loss, fewer complications and shortened length of hospital stay, while oncological outcomes remain equivalent [8]. This finding had been suggested by cohort studies for a long time [9–11]. There are no randomised data for major liver resections available yet. However, a recent meta- analysis of 10 retrospective series of major laparoscopic vs open resection encompassing cohorts of 20 to 126 laparoscopic resections suggested comparable outcomes [12].
The implementation of laparoscopic liver surgery in Switzerland is difficult to assess from the published literature. Most of the available reports from Swiss hospitals are monocentric small case series, or international collaborations that do not allow identification of volume and specific patterns of practice [13, 14].
The aim of this Swiss cohort study was to compare the outcome of laparoscopic versus open major hepatectomies and correct for confounders in two cantonal hospitals that have been committed to the use of advanced laparoscopy for major hepatectomies since 2015.
The study was a retrospective cohort study in two cantonal hospitals. All consecutive patients with major hepatectomy who fulfilled the inclusion criteria were classified into laparoscopic hepatectomy and open hepatectomy groups. The data were reported according to the STROBE reporting guidelines for cohort studies [15]. Patients with colorectal liver metastases (CRLM) were evaluated as a separated subgroup. The Cantonal Ethics Commission Zurich approved analysis of anonymised patient data (approval number: 2018-02037).
All patients at either hospital who underwent liver resection of three or more segments, according to the Brisbane classification, were identified from the local institutional database between January 2015 and December 2019 [16]. Follow-up ended in March 2020.
Perihilar cholangiocarcinomas, rare large tumours and resections with biliary reconstruction were excluded from the open hepatectomy group because such patients were not considered for laparoscopic resection in either centre.
The primary outcome variable was the major complication rate (Grade IIIA or higher according to the Clavien-Dindo classification). Secondary outcomes were operation time, hospital stay, blood loss and 90-day mortality. Volume of blood loss was assessed from the anaesthesia protocol.
Secondary outcome variables were international normalised ratio (INR) and bilirubin at post-operative day 5, creatinine 48 hours after surgery, post-hepatectomy liver failure according to the definition of the International Study Group of Liver Surgery (ISGLS) [17] and bile leak according to the ISGLS definition [18].
Histopathological data about tumour stage and resection rates were based on the histological report. Mortality, recurrence, survival and follow-up were collected from direct observation or reports from other providers.
Selection bias was addressed by performing a multivariate analysis using variables with a likely impact on the main outcomes. A multivariate analysis was performed for the primary outcome,major complications. Era bias appeared unlikely across the time period of only 5 years. The analysis was performed on an intent-to-treat basis.
Study size was determined by the time period. The time period was chosen was from January 2015 to December 2019 as systematic use of laparoscopy for major resection started in 2015 in the Cantonal Hospital of Winterthur and in 2017 in the Hospital of Lugano. The cases presented here represent the initial experience with laparoscopic major hepatectomy for both lead surgeons at their respective institutions (ES and PMH).
Operations were performed using high-flow laparoscopic insufflators (Air-Seal®, Conmed, Utica, NY, USA), energy devices (Thunderbeat®, Olympus, Shinjuku, Tokyo, Japan), laparoscopic CUSA® (Integra® Excel, Plainsboro, NJ, USA) and laparoscopic bipolar forceps (Storz, Tuttlingen, Germany,and Sutter, Freiburg, Germany). Each operation was conducted by two surgeons, experienced in both hepatic and advanced laparoscopic surgery. Since 2018, all patients were enrolled in an ERAS (Enhanced Recovery After Surgery) protocol for liver surgery in Winterthur, not in Lugano.
All data in the descriptive statistics are given as means with standard deviation (SD) for parametric data and in median with interquartile range (IQR) for nonparametric data. For comparison, t-tests and the Mann-Whitney test were used for parametric and nonparametric data, respectively. Categorial variables are given as proportions and the Fisher’s exact test was used for comparisons. A two-tailed p-value less than 0.05 was defined as significant. For multivariate analysis a logistic regression was performed. Continuous variables were dichotomised by using a receiver operating characteristic (ROC) analysis and the Youden index as the cut-off. For analyses and graphics JMP® 15.0 (SAS Institute, Cary, NC, USA) and Graph Pad Prism (Graph Pad Software, La Jolla, CA, USA) were used.
Figure 1 shows the annual caseload of total liver resections and of major liver resections for each cantonal hospital from the years 2015 to 2019. The proportion of all laparoscopically performed liver resections peaked at 55% and of all laparoscopic major liver resections at 67% in the two hospitals and did not increase any further. The maximum caseloads of all liver resections achieved at Winterthur and Lugano per year were 45 and 34 resections, respectively.
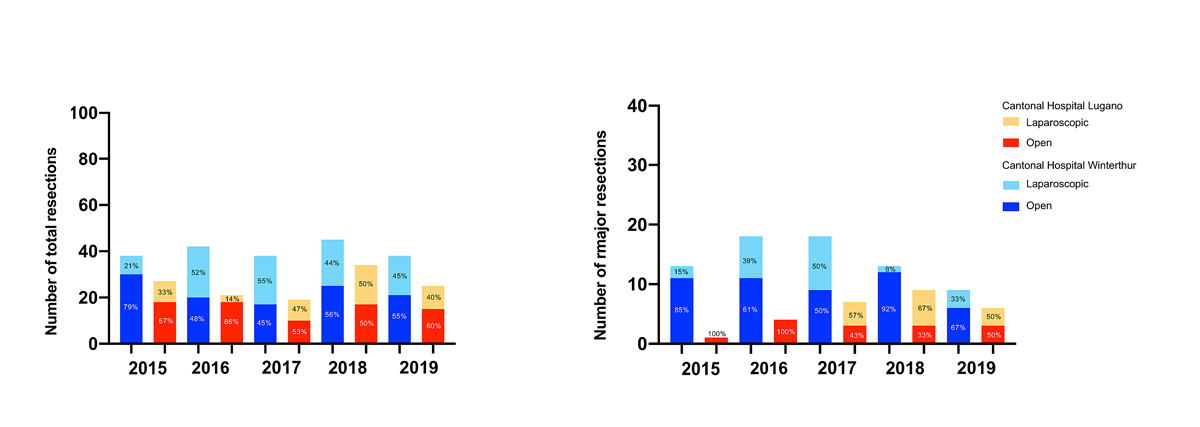
Figure 1 Number of total and major liver resections per year.
Patient selection is shown in figure 2. Among 327 patients who underwent liver resection from January 2015 to December 2019, 98 had a major hepatectomy. Eight patients with perihilar cholangiocarcinoma, a patient with a large angiosarcoma and a patient with a rare malignant fibrotic primary tumour were excluded because a laparoscopic approach would simply not be applicable to them. From the remaining 88 patients, 34 had a laparoscopic and 54 an open major hepatectomy.
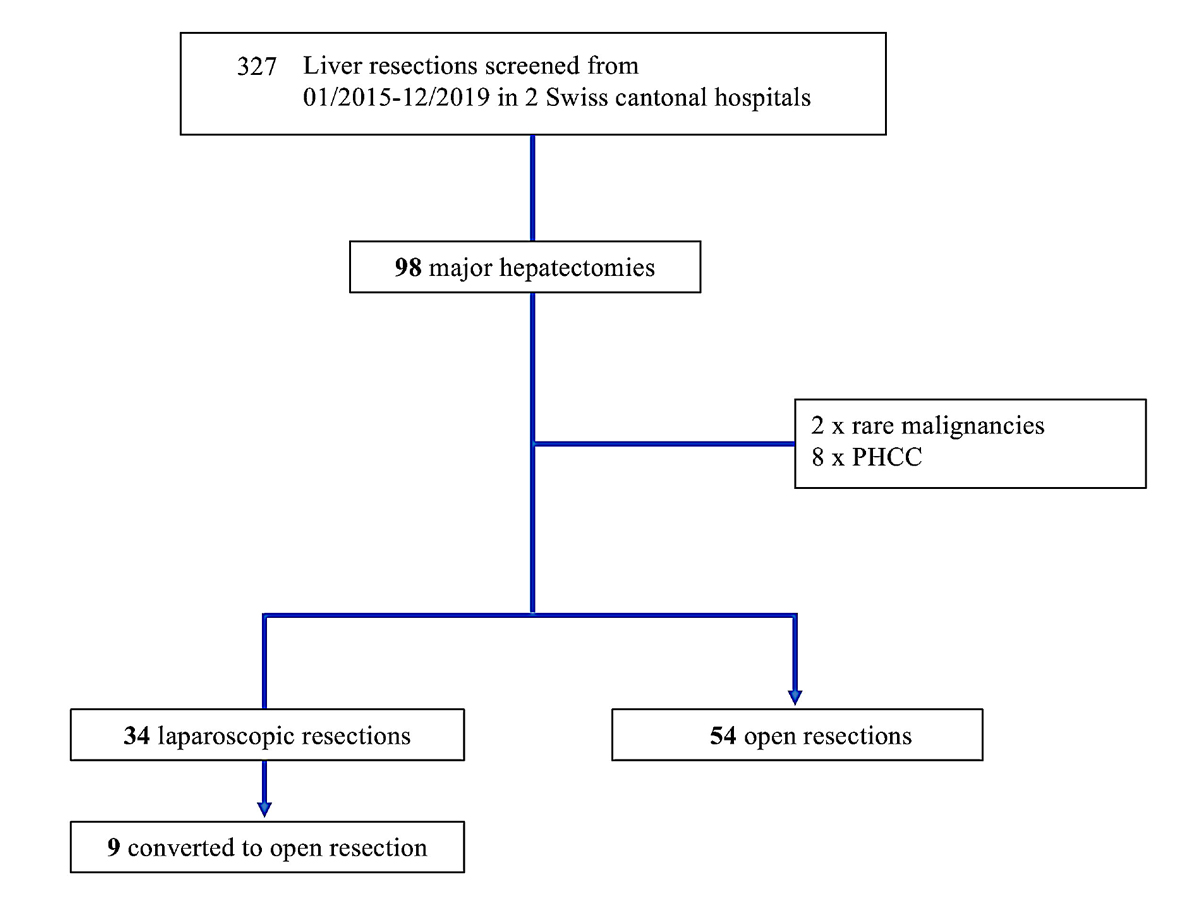
Figure 2 Flowchart.
Table 1 shows demographic and disease characteristics. Age, gender, body mass index (BMI) and the comorbidity index (CCI), bilirubin, INR and creatinine were comparable in both groups. The majority of resections were for malignancies and metastatic disease.Tumour types were equally distributed. The most common indication was colorectal liver metastases followed by neuroendocrine tumour metastases, hepatocellular carcinoma and intrahepatic cholangiocarcinoma. The number of tumours and size of the largest lesion were comparable in the two groups.
Table 1Characteristics of patients with major hepatectomy in cantonal hospitals Winterthur and Lugano 2015–2019.
| Patient characteristics | Laparoscopic (n = 34) | Open (n = 54) | p-value |
| Age, mean ± SD | 61 ± 13 | 61 ± 15 | 0.979 |
| Gender female, n (%) | 20 (59%) | 30 (56%) | 0.827 |
| BMI in kg/m2, mean ± SD | 25.8 ± 4.9 | 24.5 ± 4.5 | 0.214 |
| CCI, median (IQR) | 8 (6–9) | 7 (6–8) | 0.110 |
| INR baseline | 1.00 (0.96–1.06) | 1.00 (1.0–1.1) | 0.376 |
| Bilirubin baseline in μmol/l, mean ± SD | 12.4 (7.1–14.8) | 12.2 (6.0–12.5) | 0.051 |
| Creatinine baseline in μmol/l, mean ± SD | 78.3 (63.5–89.0) | 70.0 (62.0–74.8) | 0.253 |
| Tumour type | 0.310 | ||
| – malignant | 32 (94%) | 53 (98%) | |
| – metastatic | 25 (73%) | 41 (76%) | |
| Disease type | 0.724 | ||
| – CRLM | 18 (53%) | 32 (59%) | |
| – HCC | 3 (9%) | 3 (6%) | |
| – IHCC | 2 (6%) | 7 (13%) | |
| – NETMET | 3 (9%) | 3 (6%) | |
| – Other metastases1 | 4 (12%) | 6 (11%) | |
| – Other2 | 24 (12%) | 3 (6%) | |
| Largest lesion tumour size in mm, median (IQR) | 42 (21–80) | 30 (21–40) | 0.230 |
| Number of tumours (multiplicity), median (IQR) | 1 (1–2) | 2 (1–6) | 0.072 |
| Cirrhosis, n (%) | 0 | 0 |
SD: standard deviation; BMI: body mass index; CCI: Charlson Comorbidity Index: IQR: interquartile range; CRLM: colorectal liver metastases; HCC: hepatocellular carcinoma; IHCC: intrahepatic cholangiocarcinoma; NETMET: neuroendocrine tumour metastases; INR: international normalised ratio
1 Other metastases include mammary carcinoma, ovarian carcinoma, gastrointestinal stroma tumour, leiomyosarcoma, melanoma
2 Other includes gallbladder carcinoma, haemangioma, echinococcosis, hepatico- and choledocholithiasis
Outcome data are shown in table 2. In the laparoscopic group, right hepatectomy was the most commonly performed procedure at 74% versus 52% in the open group. There was no laparoscopic extended right hepatectomy performed and only one laparoscopic extended left hepatectomy, whereas there were 7% and 9%, respectively, in the open group. Among the 34 laparoscopic procedures, conversion to open was performed in nine cases (26%). Reasons for conversion to open were bleeding, adhesions, in one case injury of the proper hepatic artery. The proportion of two-stage hepatectomy procedures, procedures in which two stages are intended to remove an extensive tumour load, was significantly lower in the laparoscopic hepatectomy group at 6% compared with 26% in the open hepatectomy group, p = 0.018.
Table 2Surgical outcome of patients with major hepatectomy in cantonal hospitals Winterthur and Lugano 2015–2019.
| Laparoscopic (n = 34) | Open (n = 54) | p-value | |
| Resection procedure, n (%) | 0.179 | ||
| – Right hemihepatectomy | 25 (74%) | 28 (52%) | |
| – Extended right hemihepatectomy | 0 | 4 (7%) | |
| – Left hemihepatectomy | 8 (23%) | 16 (30%) | |
| – Extended left hemihepatectomy | 1 (3%) | 5 (9%) | |
| – Other | 0 | 1 (2%) | |
| Converted from laparoscopic to open | 9 (26%) | – | |
| Reason for conversion to open | |||
| – Bleeding | 6 (67%) | ||
| – Adhesions | 2 (22%) | ||
| – Injury of proper hepatic artery | 1 (11%) | ||
| Two-stage hepatectomy, n (%) | 2 (6%) | 14 (26%) | 0.018 |
| Operation time in min, median (IQR) | 433 (351–482) | 397 (296–446) | 0.222 |
| Blood loss in ml, median (IQR) | 325 (200–575) | 475 (300–800) | 0.150 |
| Hospital stay in days, median (IQR) | 9 (8–14) | 11 (9–14) | 0.411 |
| 90-day mortality, n (%) | 1 (3%) | 4 (7%) | 0.378 |
| Complications ≥IIIA, n (%) | 7 (21%) | 8 (15%) | 0.565 |
| Complications overall1, n (%) | 14 (41%) | 26 (48%) | 0.661 |
| Bile leakage, overall | 3 (9%) | 4 (7%) | >0.999 |
| – ISGLS A | 2 | 3 | |
| – ISGLS B | 1 | 0 | |
| – ISGLS C | 0 | 1 | |
| INR POD 5 | 1.10 (1.00–1.20) | 1.08 (1.03–1.12) | 0.785 |
| Bilirubin at POD 5 day in μmol/l, median (IQR) | 16 .0 (8.0–23.4) | 13.0 (9.0–19.0) | 0.447 |
| Creatinine at 48 h in μmol/l, median (IQR) | 57.0 (48.0–72.0) | 58 .0 (49.3–67.8) | 0.950 |
| Posthepatectomy liver failure (per ISGLS criteria) | 2 (6%) | 2 (4%) | 0.619 |
| R Status | 0.993 | ||
| – R0 | 29 (91%) | 48 (91%) | |
| – R1 | 3 (9%) | 5 (9%) | |
| – R2 | 0 | 0 |
IQR: interquartile range; ISGLS: International Study Group of Liver Surgery; POD: postoperative day
1 Complications overall = Grade I–V
Major complication rates were comparable in both groups (21% vs. 15%, p = 0.565).
Operation time, blood loss, hospitalisation, major and overall complications were comparable between laparoscopic and open procedures. There was one 90-day death after a laparoscopic major hepatectomy and there were four 90-day deaths after open major hepatectomies. The laparoscopic mortality was due to cardiac arrest and crash conversion after surgical injury to the middle hepatic vein in a 71-year-old patient with colorectal liver metastases. After the injury occurred, a laparoscopic sponge was used to stop the bleeding and the anaesthesia team saw a sudden fall in blood pressure and cardiac arrest. Chest compressions were started and, due to the instability of the laparoscopic visualisation, crash conversion was performed. The patient appeared severely hypovolaemic and despite aggressive resuscitation with saline and blood products, heart function could not be re-established. The lesson learned was that intra- operative normovolaemia, ability to aggressively resuscitate, and avoidance of crash conversion are important in laparoscopic liver resections.
In the open hepatectomy group, two 90-day mortalities were caused by post-hepatectomy liver failure caused by small future liver remnants (28% and 31% sFLR) in extended resections. A 63-year old patient with colorectal liver metastases developed cholestasis, synthetic dysfunction and ascites, followed by septic shock with bacteraemia which was not salvageable and died 2 weeks after resection. A 60-year old patient with colorectal liver metastases developed cholestasis, synthetic dysfunction, ascites and a biliary leak and died 5 weeks after the resection from septic shock and bacteraemia. Furthermore, a 65- year-old patient with gallbladder cancer, who had had a previous laparotomy developed a partial wound dehiscence after liver resection requiring re-exploration, mesh placement due to loss of domain and underwent gastric aspiration because of a prolonged postoperative ileus with subsequent septic shock and died 2 weeks after the operation. A 67-year-old patient with a pancreatic neuroendocrine tumour and a pre-existing Whipple procedure developed intra-abdominal sepsis after an erosion of the middle hepatic vein at the resection surface because of inadvertent injury to the Whipple limb and could not be salvaged after re-exploration, due to rapidly septic shock and deterioration of liver function after multiple blood transfusions.
Three leaks ISGLS grade A and B were observed in each group and a grade C leak occurred in the open hepatectomy group.There was no difference in postoperative laboratory markers for liver function (INR and bilirubin) at day 5 and creatinine 48 hours after resection.
Post hepatectomy liver failure occurred in two patients per group and was not significantly different. In both groups R0 resection was performed in 91% of all cases. All other patients had R1 resections (i.e., tumour at specimen margin on histological examination); there were no R2 resections (i.e., macroscopic positive margin).
A univariate and multivariate analysis was performed for the entire cohort for covariates that are of potential clinical relevance for major complications (table 3). Of these covariates, age >57 years, creatinine >66 μmol/l prior to resection and blood loss >1500 ml were found as unadjusted risk factors. The multivariate analysis revealed only blood loss >1500 ml as a relevant factor for major complications. Laparoscopic hepatectomy itself was not found to be a risk factor for complications, with an odds ratio of 0.8 (95% confidence interval 0.25–2.58, p = 0.78).
Table 3Uni- and multivariate logistic regression analysis for major complications in cantonal hospitals Winterthur and Lugano 2015–2019.
| Univariate | Multivariate | |||
| Covariate 1 | Odds ratio (CI) | p-value | Odds ratio (CI) | p-value |
| Age >57 years vs <57 years | 7.91 (0.98–63.82) | 0.025 | 9.83 (0.69–13.38) | 0.091 |
| Gender male vs female | 1.95 (0.61–6.21) | 0.255 | 0.91 (0.19–4.15) | 0.899 |
| BMI >26 kg/m2 vs <26 kg/m2 | 1.96 (0.62–6.20) | 0.253 | 1.26 (0.27–5.79) | 0.766 |
| Charlson Comorbidity Index <8 vs >8 | 2.64 (0.76–9.17) | 0.118 | 1.34 (0.13–4.27) | 0.073 |
| INR prior to resection >0.99 vs <0.99 | 2.70 (0.84–8.67) | 0.095 | 3.12 (0.71–13.64) | 0.131 |
| Bilirubin prior to resection <9 μmol/l vs >9 μmol/l | 3.94 (0.59–26.13) | 0.155 | 1.52 (0.15–15.70) | 0.724 |
| Creatinine prior to resection >66 μmol/l vs. <66 μmol/l | 4.83 (1.01–23.11) | 0.049 | 2.46 (0.43–14.03) | 0.310 |
| Blood loss >1500 ml vs <1500 ml | 8.5 (2.21–32.73) | 0.002 | 7.21 (1.23–42.25) | 0.028 |
| Operation time >336 min vs. <336 min | 2.54 (0.52–12.29) | 0.247 | 1.13 (0.12–6.34) | 0.901 |
| Two-stage hepatectomy yes vs no | 3.18 (0.89–11.29) | 0.064 | 3.01 (0.51–17.77) | 0.223 |
| Tumour type CRLM yes vs no | 2.12 (0.61–7.39) | 0.236 | 1.21 (0.20–7.15) | 0.832 |
| Group: laparoscopic yes vs no | 0.81 (0.25–2.58) | 0.724 | 0.81 (0.17–3.86) | 0.788 |
BMI: Body Mass index; INR: international normalised ratio; CRLM: colorectal liver metastases; ROC: receiver operating characteristic
1 Cutoffs for covariates were derived from logistic regression analysis using ROC curves and Youden index
In the colorectal liver metastases subgroup, 18 (53%) patients had laparoscopic and 32 (59%) had open major hepatectomy (supplementary table S1 in the appendix). Rectal cancers constituted 28% and 37% of patients in the laparoscopic hepatectomy and open hepatectomy groups, respectively. There was no difference between the two groups in the proportion of patients undergoing chemotherapy prior resection, mostly using a protocol based on FOLFOX (fluorouracil plus oxaliplatin) or XELOX (capecitabine plus oxaliplatin). The median multiplicity of lesions and the clinical risk score for recurrence established by Fong et al. were not different between the groups [19]. The median operation time was significantly prolonged in laparoscopic resections: 455, IQR 375–541 vs 397, IQR 321–432 min; p = 0.008). Volume of blood loss, hospital stay, or occurrence of major complications and 90-day mortality did not differ between the two groups. R0 resections and the 2-year survival rate (94% in both groups) were comparable. The median survival rate could not be defined because more than 50% patients were alive in both groups at the end of the study period.
This study is the first observational report from Switzerland of outcomes of major laparoscopic hepatectomy compared to open hepatectomy. Although there are randomised data on the clinical superiority of minor laparoscopic hepatectomy resections [8], there are no randomised data on major laparoscopic hepatectomy. Major laparoscopic hepatectomy resulted in comparable complication rates and 90-day mortality compared with open resection in the early learning curve experience of two regional hospitals in the Cantons of Zurich and Ticino using a multivariate analysis to correct for bias.
The clinical importance of the finding that laparoscopic procedures for major hepatectomy are feasible and safe compared with open may well encourage the adoption of major laparoscopic hepatectomy in other cantonal hospitals in Switzerland. Surprisingly little has been published about the prevalence or surgical outcomes of laparoscopic hepatectomy in this country, despite the fact that a variety of innovations in liver surgery, such as implementation of ERAS, the Rubbia-Brandt regression score in pathology of colorectal liver metastases and the “Liver-first” approach for colorectal liver metastases, originated from Switzerland [20–24]. Academic Swiss teaching hospitals are not been specifically known for laparoscopic liver surgery. One study from the University of Lausanne demonstrated an improvement of clinical outcomes by institutional adoption of ERAS guidelines. Amongst others, they reported that 25% of patients underwent laparoscopic liver resections between 2013 and 2015; however, there was no clear statement whether these laparoscopic hepatectomies included major resections [14]. The cantonal hospitals of Winterthur and Lugano have made a deliberate effort to perform laparoscopic major hepatectomies in addition to laparoscopic minor hepatectomies. Over the last 5 years, up to 67% of major hepatectomies were performed laparoscopically per year.
In 2014, a study about the practice of laparoscopic liver surgery in France, one of the pioneering countries in this field, based on data of the French Healthcare database from 2007 to 2012 was published. The study showed that laparoscopy primarily increased in the area of liver biopsies, while neither minor nor major laparoscopic hepatectomies increased over time compared with open hepatectomy. Also, it demonstrated that both minor and major laparoscopic hepatectomies were not more commonly performed in centres with more than 100 resections per year when compared with smaller centres. The study concluded that laparoscopic hepatectomy has not reached the adoption stage in liver surgery and that work in standardisation of this technique is necessary. It also showed that laparoscopic hepatectomy was performed in only 16% of cases in hospitals with a volume of 650 cases a year [25]. Most cantonal hospitals in Switzerland perform this volume of liver resections owing to the cantonal healthcare structure and only limited centralisation of highly specialised care in Switzerland. In the two cantonal hospitals analysed in the present study, the number of laparoscopic minor and major liver resections increased, and in 2017 nearly half of all liver resections were performed laparoscopically. The main reason why centres choose open resection over laparoscopic resection may be lack of familiarity with the technique and concern about bleeding control, longer operation times and potentially more complications. However, none of these outcomes were significantly different in our analysis, although the experience presented is well within the very early learning curve [26–29]. This finding is consistent with cohort studies on major laparoscopic hepatectomy from other centres [30–33]. Of course, this study, as other cohort studies, is amenable to a selection bias, where easier resections are selected for the laparoscopic approach. This bias may be reduced, but certainly not eliminated, by correcting for confounders. A recent meta-analysis, however, came to the conclusion that major laparoscopic hepatectomy is associated with decreased morbidity and length of stay and less blood loss [12]. Since the conversion rate in this cohort study was quite high, it is possible that the finding of a lack of superiority of major laparoscopic hepatectomy in this study is due to a type II error.
The majority of major liver resections in cantonal hospitals are performed for colorectal liver metastases. Among colorectal liver metastases, resection of bilobar lesions is preferentially performed open, since TSHs were more common in the open hepatectomy group. In the subgroup analysis for colorectal liver metastases a significant difference was found only for operation time and for number of lesions resected between the laparoscopic hepatectomy and open hepatectomy group. Despite the fact that there appears to be a bias for open procedures for higher numbers of colorectal liver metastases, operation time is still longer in the colorectal liver metastases subgroup. These findings may be explained by the higher difficulty of operating on multiple bilobar lesions laparoscopically due to the need for reposition and intraoperative changes of approach. In complex TSH for colorectal liver metastases there is certainly a bias towards the open approach.
The relatively high mortality of the cohort deserves comment. These cases occurred in one of the two centres, but all the authors believe that the occurrences represent real-life events that could have happened in either centre. Furthermore, Winterthur started the laparoscopic programme earlier and, for open surgery in particular, had a more open policy of accepting high-risk patients than Lugano, where hepato-pancreato-biliary surgery developed later and more conservatively.
The main limitation of this study is the retrospective study design. Reporting bias was reduced by prospective maintenance of a liver resection database. Selection bias is a concern due to a potentially cautious approach to the novel operation. The attempt to correct for this bias using variates with difference between groups and variates suspected to affect complications has intrinsic limitations. The originality of this study lies in the fact that this is the first report about the outcomes not only of major laparoscopic hepatectomy, but also of laparoscopic hepatectomy in general from Switzerland, while cohort studies on the outcomes of major laparoscopic hepatectomy vs open hepatectomy have been published before from around the world [12].
This first report from Switzerland about outcomes of laparoscopic major liver resections in two cantonal hospital shows no difference in complications and clinical non-inferiority compared to open hepatectomy.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No other potential conflict of interest was disclosed.
1. Reich H , McGlynn F , DeCaprio J , Budin R . Laparoscopic excision of benign liver lesions. Obstet Gynecol. 1991 Nov;78(5 Pt 2):956–8.
2. Ikeda T , Mano Y , Morita K , Hashimoto N , Kayashima H , Masuda A , et al. Pure laparoscopic hepatectomy in semiprone position for right hepatic major resection. J Hepatobiliary Pancreat Sci. 2013 Feb;20(2):145–50. https://doi.org/10.1007/s00534-012-0558-y
3. Wakabayashi G , Cherqui D , Geller DA , Buell JF , Kaneko H , Han HS , et al. Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg. 2015 Apr;261(4):619–29.
4. Sasaki A , Nitta H , Otsuka K , Takahara T , Nishizuka S , Wakabayashi G . Ten-year experience of totally laparoscopic liver resection in a single institution. Br J Surg. 2009 Mar;96(3):274–9. https://doi.org/10.1002/bjs.6472
5. Cherqui D , Husson E , Hammoud R , Malassagne B , Stéphan F , Bensaid S , et al. Laparoscopic liver resections: a feasibility study in 30 patients. Ann Surg. 2000 Dec;232(6):753–62. https://doi.org/10.1097/00000658-200012000-00004
6. Mbah NA , Brown RE , Bower MR , Scoggins CR , McMasters KM , Martin RC . Differences between bipolar compression and ultrasonic devices for parenchymal transection during laparoscopic liver resection. HPB (Oxford). 2012 Feb;14(2):126–31. https://doi.org/10.1111/j.1477-2574.2011.00414.x
7. Buell JF , Cherqui D , Geller DA , O’Rourke N , Iannitti D , Dagher I , et al.; World Consensus Conference on Laparoscopic Surgery . The international position on laparoscopic liver surgery: the Louisville Statement, 2008. Ann Surg. 2009 Nov;250(5):825–30. https://doi.org/10.1097/SLA.0b013e3181b3b2d8
8. Fretland AA , Dagenborg VJ , Bjørnelv GM , Kazaryan AM , Kristiansen R , Fagerland MW , et al. Laparoscopic Versus Open Resection for Colorectal Liver Metastases: The OSLO-COMET Randomized Controlled Trial. Ann Surg. 2018 Feb;267(2):199–207. https://doi.org/10.1097/SLA.0000000000002353
9. Akyuz M , Yazici P , Yigitbas H , Dural C , Okoh A , Aliyev S , et al. Oncologic results of laparoscopic liver resection for malignant liver tumors. J Surg Oncol. 2016 Feb;113(2):127–9. https://doi.org/10.1002/jso.24119
10. Andreou A , Struecker B , Raschzok N , Krenzien F , Haber P , Wabitsch S , et al. Minimal-invasive versus open hepatectomy for hepatocellular carcinoma: comparison of postoperative outcomes and long-term survivals using propensity score matching analysis. Surg Oncol. 2018 Dec;27(4):751–8. https://doi.org/10.1016/j.suronc.2018.10.005
11. Castaing D , Vibert E , Ricca L , Azoulay D , Adam R , Gayet B . Oncologic results of laparoscopic versus open hepatectomy for colorectal liver metastases in two specialized centers. Ann Surg. 2009 Nov;250(5):849–55. https://doi.org/10.1097/SLA.0b013e3181bcaf63
12. Xu H , Liu F , Li H , Wei Y , Li B . Outcomes following laparoscopic versus open major hepatectomy: a meta-analysis. Scand J Gastroenterol. 2017 Dec;52(12):1307–14. https://doi.org/10.1080/00365521.2017.1373846
13. Landi F , De’ Angelis N , Scatton O , Vidal X , Ayav A , Muscari F , et al. Short-term outcomes of laparoscopic vs. open liver resection for hepatocellular adenoma: a multicenter propensity score adjustment analysis by the AFC-HCA-2013 study group. Surg Endosc. 2017 Oct;31(10):4136–44. https://doi.org/10.1007/s00464-017-5466-4
14. Labgaa I , Jarrar G , Joliat GR , Allemann P , Gander S , Blanc C , et al. Implementation of Enhanced Recovery (ERAS) in Colorectal Surgery Has a Positive Impact on Non-ERAS Liver Surgery Patients. World J Surg. 2016 May;40(5):1082–91. https://doi.org/10.1007/s00268-015-3363-3
15. von Elm E , Altman DG , Egger M , Pocock SJ , Gøtzsche PC , Vandenbroucke JP ; STROBE Initiative . The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014 Dec;12(12):1495–9. https://doi.org/10.1016/j.ijsu.2014.07.013
16. Reddy SK , Barbas AS , Turley RS , Steel JL , Tsung A , Marsh JW , et al. A standard definition of major hepatectomy: resection of four or more liver segments. HPB (Oxford). 2011 Jul;13(7):494–502. https://doi.org/10.1111/j.1477-2574.2011.00330.x
17. Rahbari NN , Garden OJ , Padbury R , Brooke-Smith M , Crawford M , Adam R , et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011 May;149(5):713–24. https://doi.org/10.1016/j.surg.2010.10.001
18. Koch M , Garden OJ , Padbury R , Rahbari NN , Adam R , Capussotti L , et al. Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery. 2011 May;149(5):680–8. https://doi.org/10.1016/j.surg.2010.12.002
19. Fong Y , Fortner J , Sun RL , Brennan MF , Blumgart LH . Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer: analysis of 1001 consecutive cases. Ann Surg. 1999 Sep;230(3):309–18. https://doi.org/10.1097/00000658-199909000-00004
20. Melloul E , Hübner M , Scott M , Snowden C , Prentis J , Dejong CH , et al. Guidelines for Perioperative Care for Liver Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations. World J Surg. 2016 Oct;40(10):2425–40. https://doi.org/10.1007/s00268-016-3700-1
21. Rubbia-Brandt L , Giostra E , Brezault C , Roth AD , Andres A , Audard V , et al. Importance of histological tumor response assessment in predicting the outcome in patients with colorectal liver metastases treated with neo-adjuvant chemotherapy followed by liver surgery. Ann Oncol. 2007 Feb;18(2):299–304. https://doi.org/10.1093/annonc/mdl386
22. Mentha G , Roth AD , Terraz S , Giostra E , Gervaz P , Andres A , et al. ‘Liver first’ approach in the treatment of colorectal cancer with synchronous liver metastases. Dig Surg. 2008;25(6):430–5. https://doi.org/10.1159/000184734
23. Schadde E , Ardiles V , Slankamenac K , Tschuor C , Sergeant G , Amacker N , et al. ALPPS offers a better chance of complete resection in patients with primarily unresectable liver tumors compared with conventional-staged hepatectomies: results of a multicenter analysis. World J Surg. 2014 Jun;38(6):1510–9. https://doi.org/10.1007/s00268-014-2513-3
24. Prevost GA , et al. Efficiency, Accuracy and Clinical Applicability of a New Image- Guided Surgery System in 3D Laparoscopic Liver Surgery. J Gastrointest Surg. 2019. https://doi.org/10.1007/s11605-019-04395-7
25. Farges O , Goutte N , Dokmak S , Bendersky N , Falissard B ; ACHBT French Hepatectomy Study Group . How surgical technology translates into practice: the model of laparoscopic liver resections performed in France. Ann Surg. 2014 Nov;260(5):916–21. https://doi.org/10.1097/SLA.0000000000000950
26. Cai X , Li Z , Zhang Y , Yu H , Liang X , Jin R , et al. Laparoscopic liver resection and the learning curve: a 14-year, single-center experience. Surg Endosc. 2014 Apr;28(4):1334–41. https://doi.org/10.1007/s00464-013-3333-5
27. Brown KM , Geller DA . What is the Learning Curve for Laparoscopic Major Hepatectomy? J Gastrointest Surg. 2016 May;20(5):1065–71. https://doi.org/10.1007/s11605-016-3100-8
28. Komatsu S , Scatton O , Goumard C , Sepulveda A , Brustia R , Perdigao F , et al. Development Process and Technical Aspects of Laparoscopic Hepatectomy: Learning Curve Based on 15 Years of Experience. J Am Coll Surg. 2017 May;224(5):841–50. https://doi.org/10.1016/j.jamcollsurg.2016.12.037
29. Tomassini F , Scuderi V , Colman R , Vivarelli M , Montalti R , Troisi RI . The single surgeon learning curve of laparoscopic liver resection: A continuous evolving process through stepwise difficulties. Medicine (Baltimore). 2016 Oct;95(43):e5138. https://doi.org/10.1097/MD.0000000000005138
30. Dagher I , Di Giuro G , Dubrez J , Lainas P , Smadja C , Franco D . Laparoscopic versus open right hepatectomy: a comparative study. Am J Surg. 2009 Aug;198(2):173–7. https://doi.org/10.1016/j.amjsurg.2008.09.015
31. Abu Hilal M , Di Fabio F , Teng MJ , Lykoudis P , Primrose JN , Pearce NW . Single-centre comparative study of laparoscopic versus open right hepatectomy. J Gastrointest Surg. 2011 May;15(5):818–23. https://doi.org/10.1007/s11605-011-1468-z
32. Topal H , Tiek J , Aerts R , Topal B . Outcome of laparoscopic major liver resection for colorectal metastases. Surg Endosc. 2012 Sep;26(9):2451–5. https://doi.org/10.1007/s00464-012-2209-4
33. Yoon SY , Kim KH , Jung DH , Yu A , Lee SG . Oncological and surgical results of laparoscopic versus open liver resection for HCC less than 5 cm: case-matched analysis. Surg Endosc. 2015 Sep;29(9):2628–34. https://doi.org/10.1007/s00464-014-3980-1
Table S1Clinical outcome of CRLM subgroup in cantonal hospitals Winterthur and Lugano 2015-2019.
| Laparoscopic (n = 18) | Open (n = 32) | p-value | |
| Type of CRLM, n (%) | 0.697 | ||
| – Colon | 13 (72%) | 20 (63%) | |
| – Rectum | 5 (28%) | 12 (37%) | |
| Chemotherapy, n (%) | 13 (72%) | 26 (81%) | 0.362 |
| – FOLFOX/XELOX | 8 (62%) | 15 (58%) | |
| – FOLFIRI/FOLFOXIRI | 2 (15%) | 10 (42%) | |
| – Other1 | 3 (23%) | 0 | |
| T-stage of primary CRC tumour | 0.363 | ||
| – T1 | 0 | 0 | |
| – T2 | 0 | 2 (6%) | |
| – T3 | 13 (72%) | 25 (78%) | |
| – T4 | 5 (28%) | 5 (16%) | |
| N-stage of primary CRC tumour | 0.419 | ||
| – N0 | 8 (44%) | 11 (44%) | |
| – N1 | 6 (33%) | 8 (32%) | |
| – N2 | 4 (22%) | 13 (52%) | |
| Resection stage | 0.724 | ||
| – R0 | 15 (83%) | 24 (75%) | |
| – R1 | 3 /17%) | 8 (25%) | |
| Tumour size in mm, median (IQR) | 24 (20–53) | 30 (21–39) | 0.768 |
| Number of tumours, median (IQR) | 2 (1–2) | 3 (2–5) | 0.002 |
| Clinical risk score, median (IQR) | 2 (2–3) | 3 (2–3) | 0.216 |
| Operation time in min, median (IQR) | 455 (375–541) | 397 (321–432) | 0.008 |
| Blood loss in ml, median (IQR) | 375 (300–650) | 550 (300–950) | 0.216 |
| Hospital stay in days, median (IQR) | 9 (7–13) | 10 (9–13) | 0.218 |
| Complications ≥IIIA, n (%) | 4 (22%) | 6 (18%) | 0.768 |
| Complications overall2, n (%) | 6 (33%) | 17 (53%) | 0.178 |
| 90-day mortality, n (%) | 1 (5%) | 2 (6%) | 0.921 |
CRLM: colorectal liver metastases; FOLFOX: leucovorin, fluorouracil, oxaliplatin; XELOX capecitabine, oxaliplatin; FOLFIRI leucovorin, fluorouracil, irinotecan; FOLFOXIRI leucovorin, fluorouracil, irinotecan, oxaliplatin; CRC: colorectal cancer; IQR: interquartile range
1 Other includes capecitabine, cisplatin-etoposide
2 Complications overall = Grade I–V