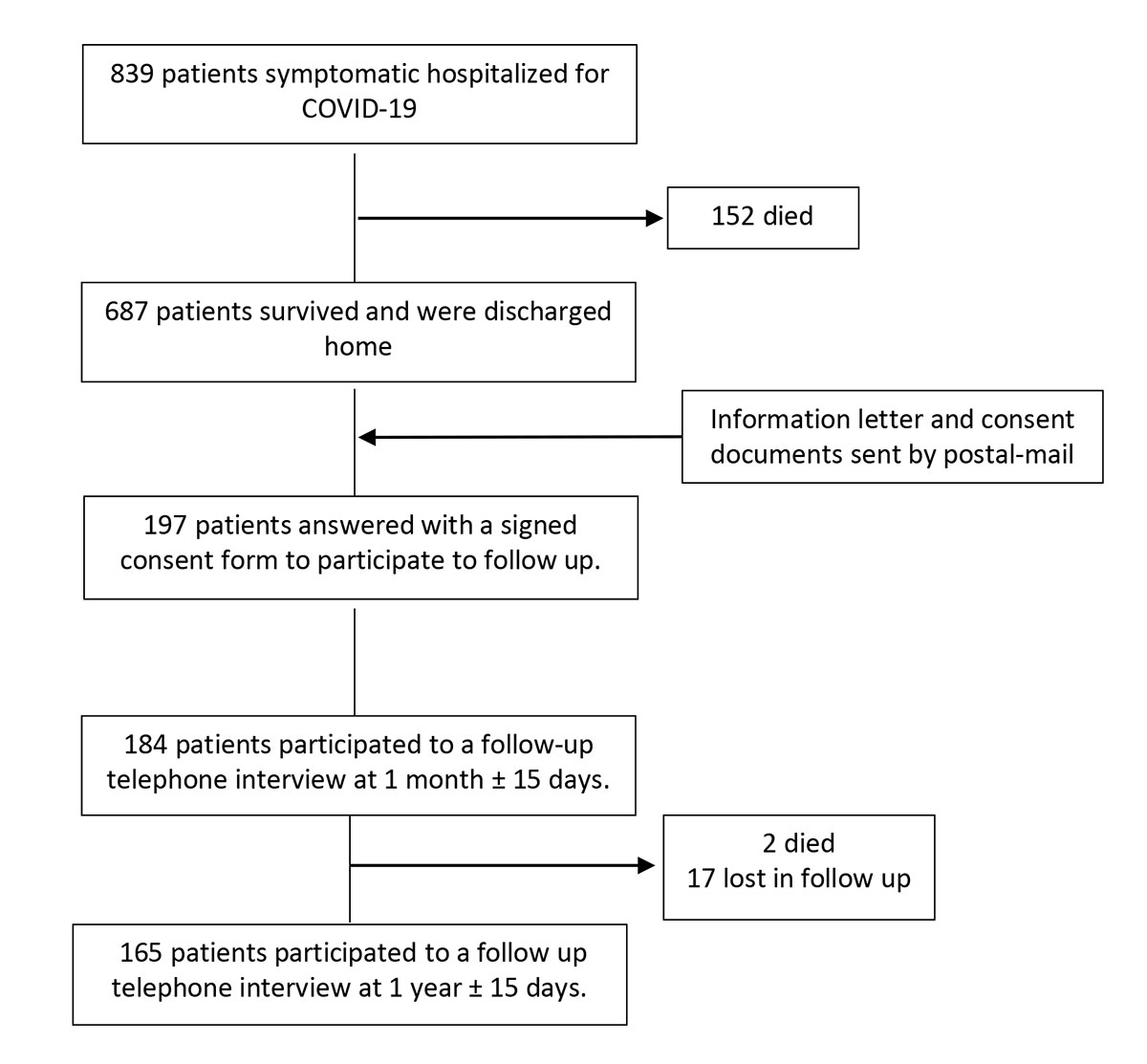
Figure 1 Patient selection and follow-up flowchart.
DOI: https://doi.org/10.4414/SMW.2021.w30093
Over 190 million people have recovered from coronavirus disease 2019 (COVID-19) worldwide [1] and a wide range of short- and long-term complaints have been reported. In the majority of cases, lung damage caused by COVID-19 is reversible, but in some cases symptoms persist [2].
The impact of the COVID-19 pandemic on quality of life (QoL) and its effects on the social and human level have been reported [3]. The consequences and burden of COVID-19 on the emotional and clinical status of hospitalised patients discharged after an acute infection are important, and they deserve explicit attention from healthcare professionals, not only to improve symptoms in post-COVID-19 syndromes, but also to restore quality of life and work productivity.
In discharged survivors of COVID-19, impairment of diffusion capacity is the most common persisting abnormality of lung function, followed by restrictive respiratory defects, both of which are associated with severity of the disease [4]. A history of cardiovascular diseases (CVD) is associated with increased mortality, and a high risk of major events in patients with COVID-19, and has long-term implications for the cardiovascular (CV) system, impacting global quality-of-life [5]. In addition to respiratory and CV sequelae, physical and psychological impairment have been reported in patients hospitalised for COVID-19 at 1 month after discharge [6]. Multiorgan symptoms after COVID-19 and complications related to “long -COVID-19” are increasing [7].
In this study we aimed to investigate symptoms, emotional status and QoL, after discharge among COVID-19 survivors.
The Geneva COVID-19 CVD study (ClinicalTrials.gov Identifier: NCT04384029) is an observational, monocentric cohort study of patients hospitalised for COVID-19 at the University Hospitals of Geneva.
The study was approved by the Ethical Committee of Geneva, Switzerland (Commission cantonale d'éthique de la recherche sur l'être humain, protocol 2020-00610) and complies with the Declaration of Helsinki.
Inclusion criteria were: all patients ≥18 years tested positive for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by polymerase chain reaction (PCR) and exhibiting typical COVID-19 symptoms according to the World Health Organization (WHO) guidelines [8] who were hospitalised for COVID-19 at the University Hospitals of Geneva between 26 February 2020, and 26 April 2020.
We excluded all patients who were found positive for SARS-CoV-2 during hospitalisation (swab taken for screening) without COVID-19 symptoms or who were hospitalised for other reasons than COVID-19.
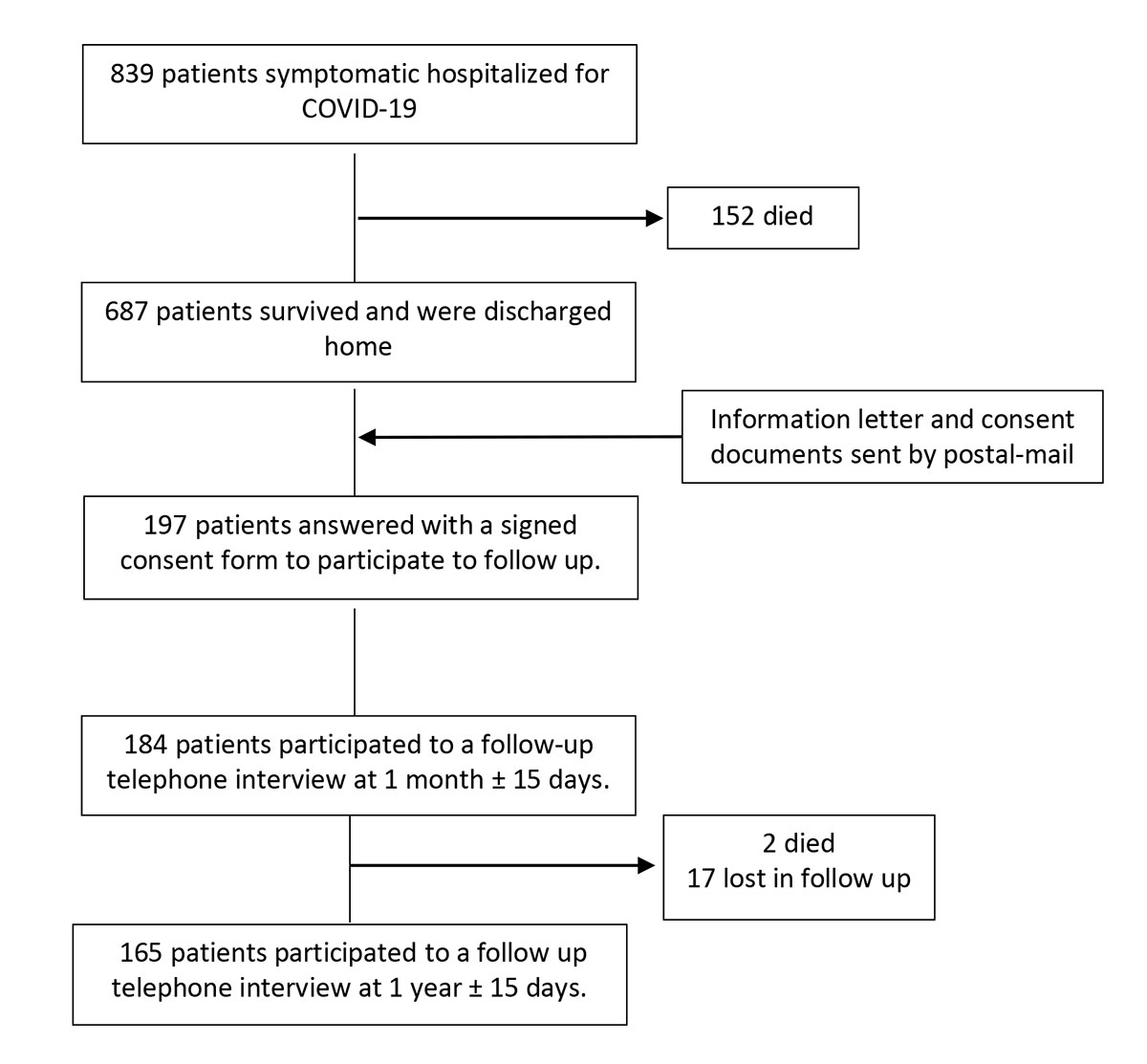
Figure 1 Patient selection and follow-up flowchart.
Hospitalisation data were extracted through validated automated feeds form electronic health records, as well as manually by a study team trained in cardiology on uniform sources for the study variables. After hospital discharge, we prospectively contacted patients by postal mail to propose a 30-day and 1-year follow-up evaluation. Follow-up was by telephone at 30 days ± 15 days and at 1 year ± 15 days after discharge among patients who accepted and signed the consent form.
We inquired about the patient’s general health status, with questions based on their symptoms, and then administered the HeartQoL questionnaire (total or partial), at the 1- month and at 1-year follow-up, and the EQ-5D-5L was completed at 1-year follow up to derive patient-reported outcome measures (PROM). The interviewer was the same for all phone calls, and for both time points (at 1-month and 1-year follow-up), asking questions in a standardised way for symptoms, the Heart QoL questionnaire and the EQ-5D-5L questionnaire, using the same approach for everyone.
Data were entered into REDCap®, a secure free web application for building and managing databases.
MACE (major adverse cardiovascular events) during COVID hospitalisation were defined as: CV death, heart failure (defined as acute heart failure in a patient with or without a past medical history of heart failure, with transthoracic echocardiography showing left ventricle ejection fraction < 50%, heart failure symptoms and elevated N-terminal pro-Btype natriuretic peptide [NT-pro BNP] according to European guidelines [9]), non-fatal MI (myocardial infarction) with or without ST segment elevation (STEMI or NSTEMI) as defined by the ESC) [10], nonfatal stroke (ischaemic or haemorrhagic stroke); major arrhythmia (defined as any of the following: atrial fibrillation, atrial flutter, ventricular tachycardia, ventricular fibrillation).
Patients with CVD were those with either a past medical history of CVD or a new onset of CVD during hospitalisation for COVID-19. CVD was defined as: history of acute coronary syndrome (either STEMI, NSTEMI or unstable angina), as well as history of any of the following: stable angina, coronary artery bypass, history of arrhythmia (atrial fibrillation, atrial flutter, or ventricular tachycardia), heart failure.
QoL was assessed using HeartQol, as well as EQ-5D-5L questionnaire and visual analogue scale. Considering the language used during the telephone interview, French and the English version were offered, and patients could choose between the two according to their preference.
HeartQoL is a recognised questionnaire developed by the ESC, assessing patient-reported outcomes in ischaemic heart disease [11–13], as well as in patients with atrial fibrillation [14] and after valve heart surgery [15]. The HeartQoL questionnaire consists of 14 items, of which 10 pertain to a physical subscale (1–8, 13, 14) and 4 to an emotional subscale (9–12).
For patients with CVD as described above, all 14 items with the respective answering scale were used (10 physical items + 4 emotional items), whereas patients with no CVD were only asked to respond to the 4 items relating to emotional status (items 9–12), both at 1-month and 1-year follow-up.
The EQ-5D-5L questionnaire was used at the 1-year follow-up phone call. It is a validated tool that assesses health related QoL and it comprises five dimensions: mobility, self-care, usual activities, pain/discomfort and anxiety/depression [16]. Each dimension has five levels: no problems, slight problems, moderate problems, severe problems and extreme problems. This decision results in a 1-digit number that expresses the level selected for that dimension. The digits for the five dimensions can be combined into a 5-digit number that describes the patient’s health state. The EuroQuol approach is reliable [17], with an average test-re-test reliability using inter-class coefficients with mean of 0.78 and 0.73 [18].
This tool also has an overall health EQ visual analogue scale (EQ-VAS) where the patient selects a number between 0 and 100. The value records patient’s self-reported health on a vertical visual analogue scale, where the endpoints are labelled "The best health you can imagine" (100) and "The worst health you can imagine" (0). The EQ-VAS is a subjective measure of health outcome that reflects the patient’s own judgement. Convergent validity was demonstrated by a correlation between EQ-5D-5L and the dimensions of WHO 5, ( r= 0.43, p <0.001) [19].
Patient and hospital stay characteristics were described as counts and percentages for qualitative data and as mean (standard deviation, SD) or median (interquartile range) for quantitative data. Patient and hospital stay characteristics were compared between participants and non-participants using the chi-square test for qualitative variables and Wilcoxon-Mann-Whitney tests for quantitative variables. Symptoms, emotional status and the EQ-5D-5L were described as count and percentage. The EQ-VAS score (theoretical range 0 to 100) was graphically represented using a histogram. In CVD patients, the HeartQoL global score was graphically represented at 30 days and one year, using an empirical cumulative distribution function plot.
Statistical significance was set at a two-sided 0.05 level for all analyses. All analyses were performed using R software, version 4.0.2 (R Foundation for Statistical Computing, Vienna: www.R-project.org).
Among 839 patients hospitalized for COVID-19 between February 26, 2020 and April 26, 2020, 687 (82%) survived and were discharged. We obtained signed consent forms back from 197 patients. Of these, 184 patients were reached by phone at one month (+/–15 days) follow up and 165 patients at one year (+/–15 days) follow up (figure 1). Patients’ characteristics are described in table 1. Followed-up patients had a median age of 58 years, 62% were male, and 21% had a past medical history of heart disease. Compared to patients who did not proceed with the follow-up interview, participants were younger (mean difference = 5.1 years [95%CI 2.5 to 7.7], p <0.001), presented less frequently with a new onset of Major Adverse Cardiovascular Events (MACE) during their hospital stay (6% vs. 12%, p = 0.024), but were more frequently admitted to the Intensive Care Unit (ICU) (16% vs. 8%, p=0.007) or to the Intermediate Care Unit (IMCU) (21% vs. 12%, p = 0.006). Their length of hospital stay (LoS) was shorter (mean LoS 11.1 vs. 14.1 days, p = 0.002).
Table 1Patient and hospital stay characteristics.
| Refused follow-up (n = 503) | Followed up (n = 184) | p-value 1 | |
| Patient characteristics | |||
| Male, n (%) | 243 (48) | 114 (62) | 0.002 |
| Age (y), median (IQR) | 65 (52–80) | 58 (50–69) | <0.001 |
| BMI* (kg/m2), median (IQR) | 26 (2330) | 27 (2431) | 0.026 |
| Comorbidities | |||
| Hypertension | 232 (46) | 65 (35) | 0.015 |
| Dyslipidaemia | 113 (22) | 45 (24) | 0.655 |
| Diabetes type II** | 93 (18) | 29 (16) | 0.474 |
| History of heart failure | 25 (5) | 2 (1) | 0.036 |
| Chest CT with COVID-19 signs*** | 74 (15) | 38 (21) | 0.080 |
| Hospitalization-related characteristics | |||
| MACE, n (%) | 62 (12) | 11 (6) | 0.024 |
| Length of stay (days), mean (sd) | 14.1 (12.2) | 11.1 (9.1) | 0.002 |
| Rehabilitation, n (%) | 123 (24) | 19 (10) | <0.001 |
| ICU admission, n (%) | 42 (8) | 29 (16) | 0.007 |
| IMCU admission, n (%) | 60 (12) | 38 (21) | 0.006 |
1 Wilcoxon-Mann-Whitney test for quantitative variables, chi-square test for qualitative variables.
BMI: body mass index; CVD: cardiovascular disease; MACE: major adverse cardiovascular events; ICU: intensive care Unit; IMCU: intermediate care unit; IQR = interquartile range; CT = computed tomography;
* Missing data for BMI value = 86;
** Diabetes type II, either treated with or without insulin
*** Chest CT scan with typical radiological signs of COVID-19 pneumonia
At admission the most common symptom was fever (77%), followed by dyspnoea (76%) and cough (72%). At 30 days and 1 year post-discharge, respectively, 143 (78%) patients and 91 (55%) patients reported some symptoms. In particular, at 30-day and 1-year follow-up, respectively, 61% (113/184) and 27% (45/165) patients reported symptoms of fatigue, 28% (52/184) and 14% (23/165) dyspnoea, 10% (19/184) and 6% (10/165) olfactory and gustatory disorders, 9% (16/184) and 17% (28/165) neurological symptoms (table 2).
Table 2Symptoms and emotional status in discharged COVID-19 patients.
| At hospital admission (n = 184) | 1-month follow-up after discharge (n = 184) | 1-year follow-up after discharge (n = 165) | |
| Symptoms | |||
| Fever | 141 (77%) | 1 (1%) | 1 (1%) |
| Dyspnoea | 139 (76%) | 52 (28%) | 23 (14%) |
| Cough | 132 (72%) | 17 (9%) | 5 (3%) |
| Myalgia | 66 (36%) | 15 (8%) | 10 (6%) |
| Tiredness/fatigue | 63 (34%) | 113 (61%) | 45 (27%) |
| Other** | 54 (29%) | 25 (14%) | 26 (16%) |
| GI symptoms | 46 (25%) | 6 (3%) | 4 (2%) |
| Headache | 35 (19%) | 12 (7%) | 8 (5%) |
| Expectorations | 35 (19%) | 5 (3%) | 1 (1%) |
| Altered smell or taste sensation | 20 (11%) | 19 (10%) | 10 (6%) |
| Runny nose | 16 (9%) | 9 (5%) | 1 (1%) |
| Neurological symptoms* | 5 (3%) | 16 (9%) | 28 (17%) |
| Emotional status | |||
| Not feeling relaxed and free of tension | |||
| No | 109 (59%) | 95 (58%) | |
| A little/sometimes | 65 (35%) | 66 (40%) | |
| A lot | 10 (5%) | 4 (2%) | |
| Feeling depressed | |||
| No | 138 (75%) | 109 (66%) | |
| A little/sometimes | 37 (20%) | 51 (31%) | |
| A lot | 9 (5%) | 5 (3%) | |
| Being frustrated | |||
| No | 129 (70%) | 113 (68%) | |
| A little/sometimes | 50 (27%) | 47 (28%) | |
| A lot | 5 (3%) | 5 (3%) | |
| Being worried | |||
| No | 90 (49%) | 88 (53%) | |
| A little/sometimes | 80 (43%) | 71 (43%) | |
| A lot | 14 (8%) | 6 (4%) | |
* Neurological problem included: memory loss, concentration problems, sleep disorders, syncope and dizziness.
** Other symptoms included: weight loss, back pain, rheumatic disease, hair loss, lack of appetite, palpitations.
The four items on emotional status of the HeartQoL were completed by all patients reached by telephone (table 2). Globally, the percentage of patients expressing a problem ranged between 2% (felt “a lot” not relaxed at 1 year) and 8% (being “a lot” worried at 30 days). Specifically, at 1 month after discharge, 8% of patients (14/184) reported being worried (answered “a lot”), 5% (10/184) felt “not relaxed” (answered “a lot”), 5% (9/184) felt depressed (answered “a lot”) and 3% (5/184) felt frustrated (answered “a lot”). At 1 year after discharge, 4% of patients (6/165) reported being worried (answered “a lot”), 3% (5/165) reported feeling depressed (answered “a lot”), 3% (5/165) reported feeling frustrated (answered “a lot”) and 2% (4/165) feeling “not relaxed” (answered “a lot”).
The EQ-5D-5L was answered by all patients (n = 165) reached by telephone at the 1-year follow-up interview (table 3).
Table 3Quality of life assessment (EQ-5D-5L) at 1-year follow up.
| 1-year follow up after discharge (n = 165) | |
| Mobility | |
| No problems | 148 (90) |
| Slight–moderate | 14 (8) |
| Severe–unable | 3 (2) |
| Self-care | |
| No problems | 162 (98) |
| Slight–moderate | 3 (2) |
| Severe–unable | - |
| Usual activities | |
| No problems | 131 (79) |
| Slight–moderate | 32 (19) |
| Severe–unable | 2 (1) |
| Pain/discomfort | |
| No problems | 95 (58) |
| Slight–moderate | 66 (40) |
| Severe–extreme | 4 (2) |
| Anxiety/depression | |
| No problems | 90 (55) |
| Slight–moderate | 56 (34) |
| Severe–extreme | 19 (12) |
We have grouped together “slight” and “moderate”, as well as “severe” and “extreme”/“unable”.
The most affected dimension of the EQ-5D-5L was anxiety/depression with 19 (12%) patients being severely or extremely anxious or depressed. No more that 2% of the patients expressed a severe or extreme difficulty in the other four domains. The mean value of the EQ-VAS score was 78.4 (SD 16.1), with a range between 30 and 100. The median was 80 (IQR 70–90) (fig. 2).
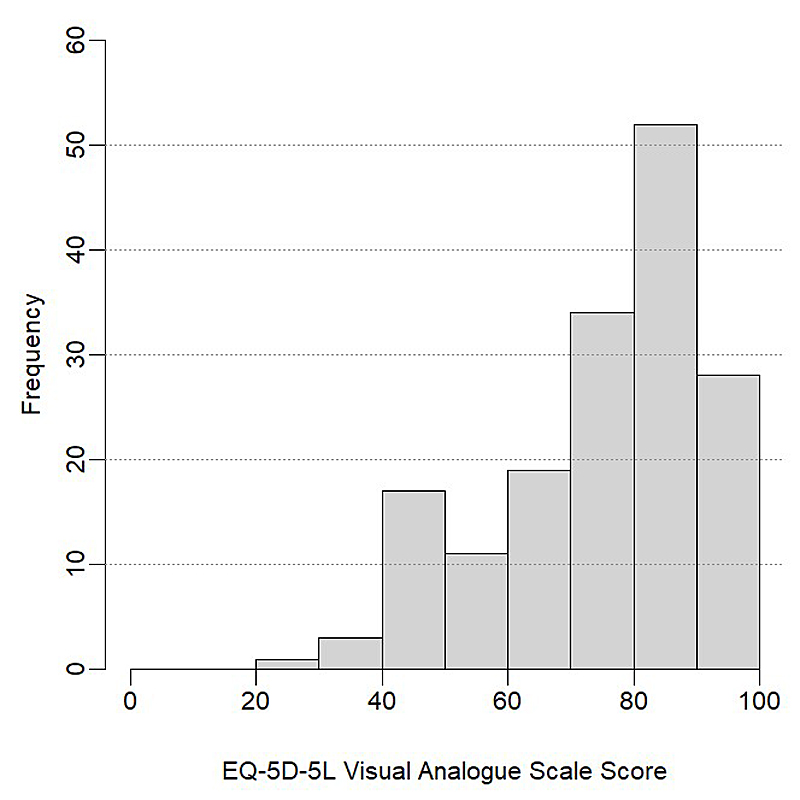
Figure 2 EQ-5D-5L Visual Analogue Scale (VAS) scores one-year after discharge after acute COVID-19 episode.
Scores on the EQ-5D-5L VAS in 165 patients at 1-year follow up (patient’s own judgment on quality of life in a scale range from 0 to 100, with higher scores indicating better health status). Bars are right closed and left opened. Median score was 80 (IQR 70–90).
Only 22 of 184 patients followed up had a history of CVD, (19/22 had a history of CVD at admission, and a further 6/22 had a new event during hospitalisation: three heart failure and three myocardial infarction).
The 14 items of the HeartQoL questionnaire were answered by these 22 patients. Distribution of the HeartQoL global score is shown in figure 3. The 14-item HeartQoL score ranged from 1.4 to 3, with a median score of 2.2 (IQR 1.8–2.5) at 1-month follow up, and 2.4 (IQR 1.8–2.9) at 1 year follow up. The HeartQoL items showed acceptable levels of internal consistency (Cronbach’s Alpha: 0.89).
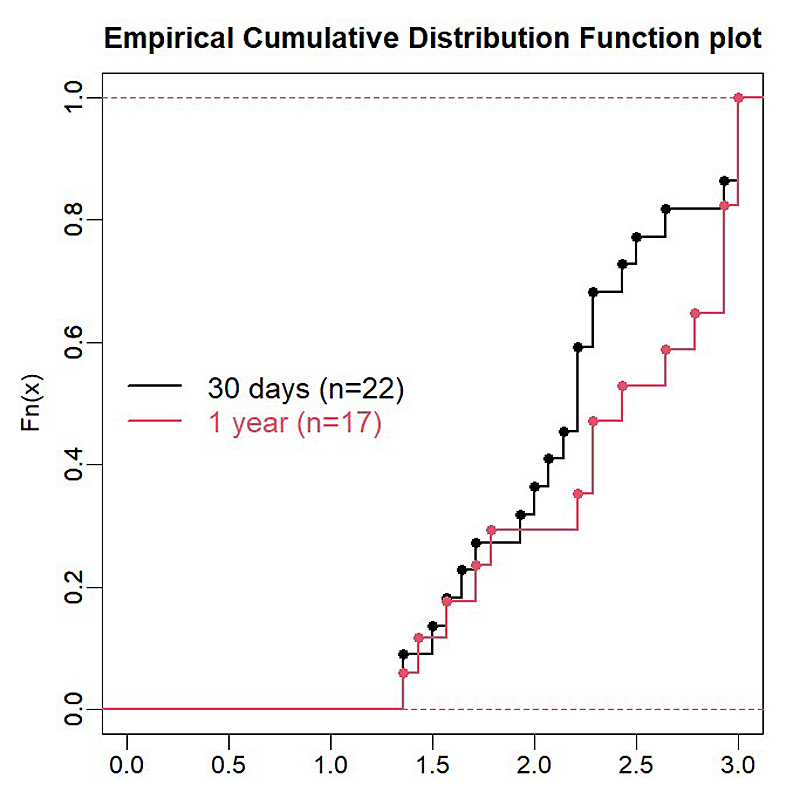
Figure 3 HeartQoL scores in CVD patients at 1 month and 1 year after discharge following an acute COVID-19 episode.
Scores on the Heart QoL (the higher is HeartQoL score, the better is the quality of life) among patients with CVD, at 1 month and 1 year follow up after discharge. Heart QoL scores ranged from 1.4 to 3, with a median score of 2.2 (IQR 1.8–2.5) at 1 month (22 patients) and of 2.4 (IQR 1.8;–2.9) at 1-year follow up (17 patients).
We report long-term symptoms and quality of life after discharge for COVID-19 patients hospitalised at the Geneva University Hospitals. In our follow-up study, persistent symptoms in patients after acute COVID-19 were predominantly fatigue and dyspnoea, which are in line with previous reports.
Although dyspnoea strongly decreased over time in our study, it was still present in 28% and 14% of cases, at one month and one-year follow up, respectively. Persistent, exertional dyspnoea has already been described in patients after acute COVID-19, particularly in patients who required ICU admission and presented premorbid lung problems, higher age, higher BMI, and were Black Asian and Minority Ethnic [20].
According to some studies, it seems that persistent symptoms are independent of the severity of the initial infection [21, 22]. Persistent fatigue, lasting up to 6 months, has been already observed after other viral and bacterial infections [23], but the mechanisms underlying this symptom are still not explained. Possibly, these could be due to alterations in the activity of the immune system, which have shown to be associated with potential post-viral fatigue [24].
We also found that 17% of patients reported neurological problems such as memory loss, concentration problems, dizziness or sleep disorders, up to one year after discharge. This is in line with another study finding, that patients surviving COVID-19 are at higher risk for developing subsequent central and peripheral neurological diseases [25]. Finally, some authors emphasised the need for long-term psychological support of post-COVID-19 patients, in particular for those with neurological and psychological impairment in the sub-acute phase [26].
Considering the emotional assessment in our study, scores were generally low suggesting a low impact of COVID-19 hospital admission on emotional post-discharge well-being at one month and one year. It is worth stating that patients who accepted the follow-up had several differences compared to those who did not accept to be followed up, which may limit the generalisability of these findings. However, patients included in our follow-up study were more frequently admitted to the ICU or IMCU which would be expected to overestimate the impact of hospital stay on their post-discharge well-being.
Health-related quality-of-life estimates, are important tools to monitor multi-dimensional clinical outcomes after an acute event and have been gaining increasing interest to quantify emotional and long-term social impact related to the pandemic [27, 28].
The EQ-5D-5L is a validated tool to measure QoL, introduced by the Euro Qol group in 2009, considering five dimensions (mobility, self-care, usual activities, pain/discomfort and anxiety/depression) [16]. In our study, the most reported issue at one year follow up was anxiety/depression suggesting that interventions at different levels should be offered in fragile and selected patients after discharged for COVID-19.
In CVD patients, the mean Heart QoL score at one month and one year post discharge was similar to the mean score observed in European CVD patients [29].
Finally, older patients hospitalized for COVID-19 seem to be more susceptible to report a negative change in health related QoL, with one out of three reporting a persistent impaired mobility and ability to carry out activities of daily living [30].
A comprehensive multi-dimensional follow-up approach for COVID-19 patients deserves particular attention. Early interventions, as well as regular follow up, have to be considered to promote recovery in patients post COVID-19 hospitalisation.
To our knowledge, this study provides the first implementation of the HeartQoL questionnaire for the follow up of CVD patients after a severe COVID-19 episode. Unfortunately, the low number of CVD patients makes it difficult to draw any conclusion.
The rate of participation in our study was low and coupled with a selection bias, resulting in a limitation to a significant degree of the generalisability of our findings. However, the rate of participation was in the usual range for studies recruiting patients based on postal mail invitation. Especially, in the context of this pandemic, many patients could have been over-solicited and overwhelmed by a wide range of follow-up studies. Still, patients who agreed to participate in the follow-up, were younger, more likely to be male, and had more favourable outcomes at discharge (shorter length of stay and fewer MACE) and yet were more frequently admitted to the ICU or IMCU, compared with those who did not accept the follow up.
Our findings suggest that after recovery from acute manifestations of COVID-19 requiring hospitalisation, the main persistent complaints are fatigue, dyspnoea and neurological disorders up to 1 year , with little impact on emotional status and quality of life. Owing to the large spectrum of symptoms, we believe a comprehensive multi-dimensional follow-up approach is needed for COVID-19 patients.
Special thanks to Philippe Sigaud, Sandrine Brader, Anne Bevand, Aurélie Schneider-Paccot for data collection and for database management. Special gratitude is expressed to Aliki Buhayer (Prism Scientific Sàrl; www.prismscientific.ch) for medical writing support.
Authors’ contribution: all authors contributed equally in writing the manuscript
No financial support was reported.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed
1. www.worldometers.info/coronavirus/?zarsrc=130. Worldometer. COVID-19 Coronavirus Pandemic 2020.
2. Liu C , Ye L , Xia R , Zheng X , Yuan C , Wang Z , et al. Chest Computed Tomography and Clinical Follow-Up of Discharged Patients with COVID-19 in Wenzhou City, Zhejiang, China. Ann Am Thorac Soc. 2020 Oct;17(10):1231–7. https://doi.org/10.1513/AnnalsATS.202004-324OC
3. El Keshky ME , Basyouni SS , Al Sabban AM . Getting Through COVID-19: The Pandemic’s Impact on the Psychology of Sustainability, Quality of Life, and the Global Economy - A Systematic Review. Front Psychol. 2020 Nov;11:585897. https://doi.org/10.3389/fpsyg.2020.585897
4. Mo X , Jian W , Su Z , Chen M , Peng H , Peng P , et al. Abnormal pulmonary function in COVID-19 patients at time of hospital discharge. Eur Respir J. 2020 Jun;55(6):2001217. https://doi.org/10.1183/13993003.01217-2020
5. Xiong TY , Redwood S , Prendergast B , Chen M . Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J. 2020 May;41(19):1798–800. https://doi.org/10.1093/eurheartj/ehaa231
6. Chen KY , Li T , Gong FH , Zhang JS , Li XK . Predictors of Health-Related Quality of Life and Influencing Factors for COVID-19 Patients, a Follow-Up at One Month. Front Psychiatry. 2020 Jul;11:668. https://doi.org/10.3389/fpsyt.2020.00668
7. The Lancet . Facing up to long COVID. Lancet. 2020 Dec;396(10266):1861. https://doi.org/10.1016/S0140-6736(20)32662-3
8. https://www.who.int/publications/i/item/clinical-management-of-covid-19. WHO Guideline Development Group for Clinical Management of COVID-19. Clinical management of COVID-19. Interim guidance.
9. Ponikowski P , Voors AA , Anker SD , Bueno H , Cleland JG , Coats AJ , et al.; ESC Scientific Document Group . 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016 Jul;37(27):2129–200. https://doi.org/10.1093/eurheartj/ehw128
10. Thygesen K , Alpert JS , Jaffe AS , Chaitman BR , Bax JJ , Morrow DA , et al.; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction . Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol. 2018 Oct;72(18):2231–64. https://doi.org/10.1016/j.jacc.2018.08.1038
11. https://www.escardio.org/Education/Practice-Tools/CVD-prevention-toolbox/HeartQoL
12. Oldridge N , Höfer S , McGee H , Conroy R , Doyle F , Saner H ; for the HeartQoL Project Investigators . The HeartQoL: part I. Development of a new core health-related quality of life questionnaire for patients with ischemic heart disease. Eur J Prev Cardiol. 2014 Jan;21(1):90–7. https://doi.org/10.1177/2047487312450544
13. Oldridge N , Höfer S , McGee H , Conroy R , Doyle F , Saner H ; for the HeartQoL Project Investigators . The HeartQoL: part II. Validation of a new core health-related quality of life questionnaire for patients with ischemic heart disease. Eur J Prev Cardiol. 2014 Jan;21(1):98–106. https://doi.org/10.1177/2047487312450545
14. Kristensen MS , Zwisler AD , Berg SK , Zangger G , Grønset CN , Risom SS , et al. Validating the HeartQoL questionnaire in patients with atrial fibrillation. Eur J Prev Cardiol. 2016 Sep;23(14):1496–503. https://doi.org/10.1177/2047487316638485
15. Grønset CN , Thygesen LC , Berg SK , Zangger G , Kristensen MS , Sibilitz KL , et al. Measuring HRQoL following heart valve surgery: the HeartQoL questionnaire is a valid and reliable core heart disease instrument. Qual Life Res. 2019 May;28(5):1245–53. https://doi.org/10.1007/s11136-018-02098-1
16. https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/
17. EuroQol Group . EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990 Dec;16(3):199–208. https://doi.org/10.1016/0168-8510(90)90421-9
18. Brooks R . EuroQol: the current state of play. Health Policy. 1996 Jul;37(1):53–72. https://doi.org/10.1016/0168-8510(96)00822-6
19. Janssen MF , Pickard AS , Golicki D , Gudex C , Niewada M , Scalone L , et al. Measurement properties of the EQ-5D-5L compared to the EQ-5D-3L across eight patient groups: a multi-country study. Qual Life Res. 2013 Sep;22(7):1717–27. https://doi.org/10.1007/s11136-012-0322-4
20. Halpin SJ , McIvor C , Whyatt G , Adams A , Harvey O , McLean L , et al. Postdischarge symptoms and rehabilitation needs in survivors of COVID-19 infection: A cross-sectional evaluation. J Med Virol. 2021 Feb;93(2):1013–22. https://doi.org/10.1002/jmv.26368
21. Carfì A , Bernabei R , Landi F ; Gemelli Against COVID-19 Post-Acute Care Study Group . Persistent Symptoms in Patients After Acute COVID-19. JAMA. 2020 Aug;324(6):603–5. https://doi.org/10.1001/jama.2020.12603
22. Townsend L , Dyer AH , Jones K , Dunne J , Mooney A , Gaffney F , et al. Persistent fatigue following SARS-CoV-2 infection is common and independent of severity of initial infection. PLoS One. 2020 Nov;15(11):e0240784. https://doi.org/10.1371/journal.pone.0240784
23. Bansal AS , Bradley AS , Bishop KN , Kiani-Alikhan S , Ford B . Chronic fatigue syndrome, the immune system and viral infection. Brain Behav Immun. 2012 Jan;26(1):24–31. https://doi.org/10.1016/j.bbi.2011.06.016
24. Natelson BH , Haghighi MH , Ponzio NM . Evidence for the presence of immune dysfunction in chronic fatigue syndrome. Clin Diagn Lab Immunol. 2002 Jul;9(4):747–52.
25. Heneka MT , Golenbock D , Latz E , Morgan D , Brown R . Immediate and long-term consequences of COVID-19 infections for the development of neurological disease. Alzheimers Res Ther. 2020 Jun;12(1):69. https://doi.org/10.1186/s13195-020-00640-3
26. Alemanno F , Houdayer E , Parma A , Spina A , Del Forno A , Scatolini A , et al. COVID-19 cognitive deficits after respiratory assistance in the subacute phase: A COVID-rehabilitation unit experience. PLoS One. 2021 Feb;16(2):e0246590. https://doi.org/10.1371/journal.pone.0246590
27. Cao W , Zhang Y , Qian P . Corrrection: The Effect of Innovation-Driven Strategy on Green Economic Development in China-An Empirical Study of Smart Cities. Int. J. Environ. Res. Public Health 2019, 16(9), 1520. Int J Environ Res Public Health. 2020 May;17(10):E3380. https://doi.org/10.3390/ijerph17103380
28. Garrigues E , Janvier P , Kherabi Y , Le Bot A , Hamon A , Gouze H , et al. Post-discharge persistent symptoms and health-related quality of life after hospitalization for COVID-19. J Infect. 2020 Dec;81(6):e4–6. https://doi.org/10.1016/j.jinf.2020.08.029
29. De Smedt D , Clays E , Höfer S , Oldridge N , Kotseva K , Maggioni AP , et al. The use of HeartQoL in patients with coronary heart disease: association with risk factors and European reference values. The EUROASPIRE IV study of the European Society of Cardiology. Eur J Prev Cardiol. 2016 Jul;23(11):1174–86. https://doi.org/10.1177/2047487316631400
30. Walle-Hansen MM , Ranhoff AH , Mellingsæter M , Wang-Hansen MS , Myrstad M . Health-related quality of life, functional decline, and long-term mortality in older patients following hospitalisation due to COVID-19. BMC Geriatr. 2021 Mar;21(1):199. https://doi.org/10.1186/s12877-021-02140-x