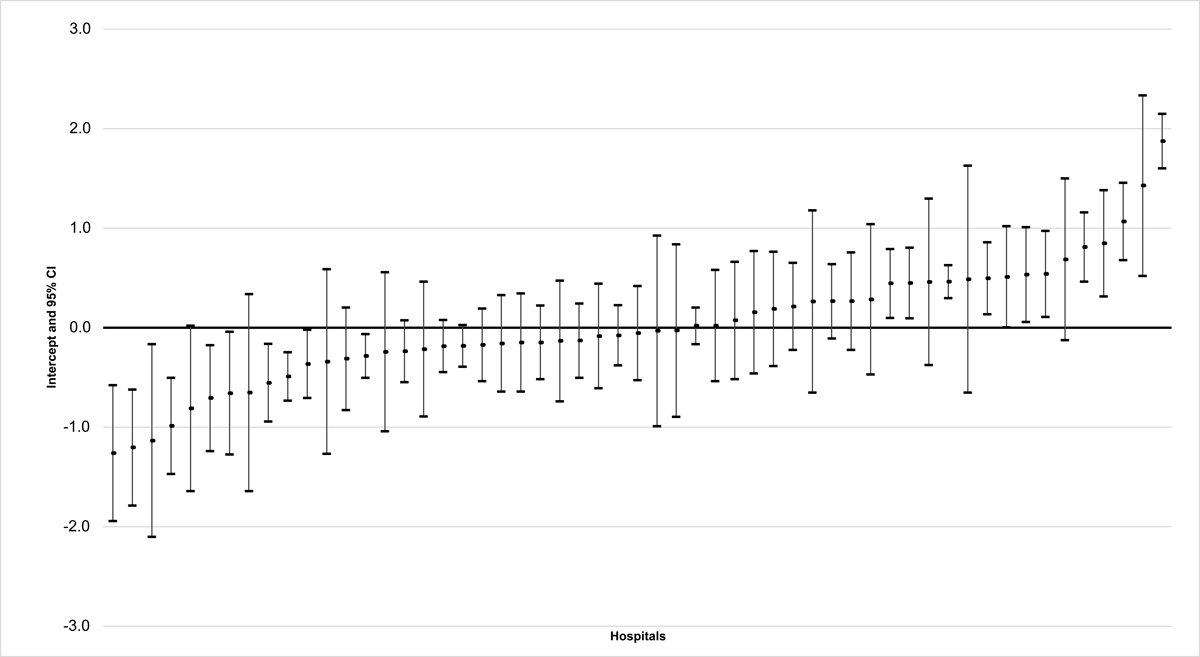
Figure 1 Risk-adjusted restraint use hospital comparison (residuals and 95% confidence interval [CI]).
DOI: https://doi.org/10.4414/SMW.2021.w30043
Restraints have been used in health care settings for centuries. In mental health care, there is an increasing awareness of the negative consequences of restraints, and therefore, restraint use is more and more regulated. For example, it has been an important quality indicator for inpatient psychiatry for many years [1–3]. This restrictive practice is increasingly also viewed critically in nursing home settings. In Australia, for example, stricter regulations regarding restraint use in residential care settings were introduced in 2019 [4]. In Switzerland, interventions restricting movement in nursing homes have been monitored at the national level since 2019 [5]. However, most countries lack clear regulations for somatic acute care hospitals (subsequently referred to as "hospitals"), and often only recommendations exist. In Canada, for example, recommendations from the Canadian Agency for Drugs and Technologies in Health (CADTH) are available [6]. In Switzerland, medical ethics guidelines regarding coercive measures in medicine exist, including recommendations for restraint use in general [7].
Restraints are used frequently in hospitals. Internationally, prevalence rates range from 0% to 100% [e.g., 8–10]. These large differences may primarily be influenced by different definitions of restraint use, the setting (e.g., intensive care units or general wards), the legal situation in a particular country, or the availability of equipment (e.g., belts for mechanical fixation) in the institution or on the ward [11–14]. In hospitals, restraints are frequently used to prevent adverse events such as falls or therapy interruption [10, 15–18]. However, the effectiveness of restraints for these purposes is increasingly being questioned. Various studies have reported that restraints have no effect on fall prevention or self-extubation [18–22]. In contrast, there is evidence that restraints in hospitals are associated with negative consequences for patients' physical and mental health [23–25], and also with moral distress among health professionals [18, 26]. Thus, based on the available evidence, it is not certain that in the hospital setting the benefits of restraint use exceed the harms, which is a basic ethical requirement for restraint use. Therefore, it is recommended to reduce restraint use as much as possible [6, 27].
Different measures for restraint reduction have been examined in various healthcare settings. Many studies have concluded that individual measures such as education of health professionals can be beneficial. However, national approaches might have an even greater impact [28, 29]. Local or national measurement and quality improvement initiatives are known in the nursing home and mental health care settings [3, 30–32]. However, national approaches to restraint reduction might also be relevant for hospitals. Apart from the considerable differences in prevalence rates described above, there is increasing evidence that restraint use in hospitals also depends on patient-independent factors such as routine, local habits, organisational attitudes, and hospital structures and policies [11–14, 33–35]. When such factors are recognised by hospital management and staff as being relevant to the reduction of restraint use, efforts can be made to change them.
Often, a key aspect of national programmes is the measurement and benchmarking of certain indicators of clinical performance [36]. Benchmarking can allow critical reflection upon the restraint practice within the ward or institution and the identification of potential for improvement. However, such quality measurements are only meaningful if risk-adjusted differences between hospitals (that take into account the different patient mixes) are identified, because it is these that can reveal potential for quality improvement [36].
Therefore, the aim of this study was to reanalyse existing data on restraint use in Swiss hospitals in order to assess the potential of restraint use as a national quality indicator for the hospital setting.
Using a cross-sectional, multicentre design, the data used for the secondary analysis were collected as part of the ANQ"s (Swiss National Association for Quality Development in Hospitals and Clinics) "falls and pressure ulcers" national prevalence measurement in Switzerland [37]. The annual measurement of falls and pressure ulcers is mandatory for all hospitals in Switzerland. In addition to these two indicators, hospitals can measure restraint use on a voluntary basis. For the present study, data from hospitals measuring restraint use at the following three measurement points were included: 08 November 2016, 14 November 2017 and 13 November 2018.
The sample consisted of patients aged 18 and older who were hospitalised on one of the reference dates when the measurement took place and who (or whose legal representative) gave informed oral consent for their participation in the overall quality measurement. The documentation of oral consent was the responsibility of the hospitals. It was recommended that consent be recorded in a central document or in the patient documentation. All medical specialties (ward types) were included, except for maternity units, emergency departments and post-anaesthesia care units. Patients who were not available on the ward during the measurement (e.g., those undergoing surgery) were excluded. We did not apply any other exclusion criteria for this secondary analysis.
Data were collected utilising the LPZ 2.0 (Landelijke Prevalentiemeting Zorgkwaliteit) instrument (version 2016), which was developed by an international consortium led by Maastricht University in the Netherlands ([38], www.lpz-um.eu). This instrument assesses general and care indicator specific information at the institutional, ward and patient levels. In this study, we conducted a secondary data analysis using variables relating to restraint use at all three levels (see supplementary table S1 in the appendix). Restraints were defined as "interventions that may infringe [on] a person's human rights and freedom of movement, including observation, seclusion, manual restraint, mechanical restraint and rapid tranquillisation" [39]. This definition largely corresponds to that of the Swiss Academy of Medical Sciences (SAMS), from which the national language translation for the LPZ 2.0 measurement is derived [7].
The LPZ 2.0 instrument utilises standardised data collection procedures. The entire procedure (e.g., recruitment of and obtaining information from patients and preparation of data for collection, including documentation of restraint use 30 days prior to data collection) and all questions and answer options are the same across the participating LPZ consortium nations and are described in a manual. Data are collected via an online tool that guarantees completion of the questionnaire. To ensure uniform execution of the measurement across participating hospitals, data collectors were trained prior to the measurement. Utilising the train-the-trainer concept, the national coordinator trained a responsible person within each hospital (the institutional coordinator). The institutional coordinator subsequently trained the data collectors (registered nurses) on the wards. Additionally, the measurement manual containing all the relevant information was readily available (within the data entry programme) to the data collectors.
The data from the different measurement points from 2016 to 2018 were pooled. Descriptive statistics (numbers, percentages, 95% confidence intervals [CIs], medians and interquartile ranges [IQRs]) were used to describe the sample.
For the benchmarking, a multilevel modelling approach was used. This approach allows for the adjustment of "... patient-level risk factors that are outside the control of providers" [36]. In other words, the different patient mixes, and thus the risk of using more or fewer restraint, which depend on the complexity of the patient situations in each hospital, were considered in the benchmarking. A very similar approach is used for the ANQ's "falls and pressure ulcers" national prevalence measurement [37]. The model was built as follows: restraint use was defined as the dependent variable; hospitals were considered as a random effect; and the institutional and ward level variables, as well as the general patient-level information, were considered as fixed effects (see table S1 in the appendix). The ward level could not be included as a third level in the model (i.e., a three-level model could not be built), as restraint use was assessed over a period of 30 days at the hospital level and not at the ward level. Since patient transfers from one ward to another are frequent, there was a risk of misclassification, and thus bias, when including the ward level.
Given the insufficient theoretical database available on restraint use in the hospital setting (with the partial exception of for mechanical restraint use in the intensive care setting), it was not possible to determine which of all possible fixed effects to include or exclude in a purely theory-driven manner. Since including all possible fixed effects might have led to an overadjustment, we decided on a data-driven model. For the data-driven modelling, we considered several variable selection procedures for logistic multilevel models. However, the very few software implementations available were not applicable to our problem. Therefore, we used the Akaike information criterion (AIC) [40] backwards procedure, implemented in the R package "MASS" [41]. Consequently, the hospital random effect had to be treated as a fixed effect for variable selection. In addition, the AIC procedure was employed in such a way that the hospital variable could not be unselected, as comparing between hospitals is an explicit part of this study. To reduce the number of noisy variables selected due to the large sample size and thus enhance the stability of the variable selection, we used a split-half approach, in which the data were randomly divided into two subsets and the AIC procedure was applied to each subset. For the final multilevel model, we used only the variables included in both selections. Afterwards, a generalised linear mixed model, fit by maximum likelihood (Laplace approximation), was built using the R package "Ime4" [42]. To assess the relevance of the random effect, the intraclass correlation coefficient (ICC) was estimated, and a log-likelihood ratio test was performed. Afterwards, a caterpillar plot was built with all hospitals on the x-axis and their residuals and 95% CIs on the y-axis.
The ICD-10 diagnosis groups [43] "pregnancy, childbirth and the puerperium"; "congenital malformations, deformations and chromosomal abnormalities"; and "certain conditions originating in the perinatal period", as well as the answer option unknown/no diagnosis, had to be excluded, as they were present in less than 1% of the patients. The inclusion of these variables would have led to convergence problems in the variable selection. In addition, the variables "age in years" and "number of days since admission to hospital" had to be centred for similar reasons. Multicollinearity was tested using the variance inflation factor (VIF). There were no missing data, as the online data entry program only allowed the survey to be finished if all the questions were answered.
The statistical analysis was conducted using R version 4.0.1 [44] and the R packages "compareGroups" [45], "Hmisc" [46], "Ime4" [42], "jtools" [47], „MASS" [41], "MuMIn" [48], "sjPlot" [49] and "tidyverse" [50].
The Ethics Committee of the Canton of Bern declared that the present study was not subject to the Swiss Human Research Act (April 2019, BASEC-Nr: Req-2019-00259). Therefore, ethical approval was not required. All patients, or their legal representatives, received written information about the measurement and gave their oral informed consent. Data were collected pseudonymously, so that no conclusions could be made regarding the individual patients. Participation was voluntary.
The sample consisted of 18,938 patients who were hospitalised in 55 hospitals (table 1). The participation rate was 76.6% (n = 18,938/24,736) across all three years. The 30-day prevalence rate of patients with at least one restraint was 10.2% (n = 1933/18,938). Detailed information regarding restraint type used (e.g., mechanical, pharmacological or electronic), reason for restraint use (e.g., fall prevention or aggression) and the processes surrounding restraint use (e.g., documentation or evaluation), as well as the distribution of the sample across different hospital and ward types, are available in the appendix.
For 68.7% (n = 13,016/18,938) of the patients there were institutional level guidelines regarding restraint use in the respective hospital and for 34.3% (n = 6503/18,938) a multi-disciplinary expert committee on restraints was available. At the ward level, 66.7% (n = 12,635/18,938) of the patients surveyed were hospitalised in wards where regular audits were carried out to ensure compliance with the guidelines regarding restraints. Nursing staff had attended a refresher course on restraint use in 10.5% (n = 1980/18,938) of all patient situations.
Table 1Sample description.
| Characteristics | Total (n = 18,938) | |
| Institutional level | n | % (95% CI) |
| Availability of guidelines regarding restraints (yes) | 13,016 | 68.7 (68.1–69.4) |
| Availability of a multi-disciplinary expert committee on restraints (yes) | 6503 | 34.3 (33.7–35.0) |
| Ward level | ||
| Performance of regular audits to ensure compliance with the guidelines regarding restraints (yes) | 12,635 | 66.7 (66.0–67.4) |
| Refresher course on restraints in the last two years for at least 80% of the ward's nursing staff (yes) | 1980 | 10.5 (10.0–10.9) |
| Patient level | median | IQR |
| Age in years | 70 | 24 |
| Number of days since admission to hospital | 5 | 9 |
| Care dependency scale (sum score)a | 70 | 15 |
| n | % (95% CI) | |
| Female gender | 9031 | 47.7 (47.0–48.4) |
| Surgical intervention in the two weeks prior to data collection (yes) | 7667 | 40.5 (39.8–41.2) |
| Three most frequent ICD-10 diagnosis groups (multiple responses) | ||
| Diseases of the circulatory system | 10,757 | 56.8 (56.1–57.5) |
| Diseases of the musculoskeletal system and connective tissue | 6829 | 36.1 (35.4–36.7) |
| Endocrine, nutritional and metabolic diseases | 6432 | 34.0 (33.3–34.6) |
| Restraint use (yes) | 1933 | 10.2 (9.8–10.6) |
IQR = interquartile range; 95% CI = 95% confidence interval; ICD-10 = International Statistical Classification of Diseases and Related Health Problems 10th Revision [43].
a Care dependency assessed using the care dependency scale (CDS) [54]. In the CDS, 15 items (e.g., eating and drinking or mobility) are rated on a Likert scale from 1 (completely dependent) to 5 (completely independent). It results in a sum score of 15–75 (higher score indicating higher care independency), which is divided into five categories (15–24 completely dependent, 25–44 dependent to a great extent, 45–59 partially dependent, 60–69 independent to a great extent, 70–75 completely independent).
Several factors associated with restraint use were found in the multilevel regression analysis (table 2). Patients' care dependency showed the strongest association with restraint use (odds ratio [OR] 52.65, 95% CI 41.71–66.48 for completely dependent patients compared to completely independent patients). Furthermore, a strong association between mental and behavioural disorders and restraint use was found (OR 2.22, 95% CI 1.97–2.49). No organisational factors were selected for the model.
Table 2Multilevel logistic regression model.
| Model: AIC 9025.02; marginal R2 = 0.35; conditional R2 = 0.43; ICC = 0.12 | |
| Random effect | Variance (SD) |
| Hospital (intercept) | 0.45 (0.67) |
| Fixed effects | OR (95% CI) |
| (Intercept) | 0.02 (0.01–0.02)* |
| Age in years | 1.01 (1.01–1.02)* |
| Female gender | 0.71 (0.64–0.79)* |
| Number of days since admission to hospital | 1.01 (1.01–1.01)* |
| Care dependency scale (CDS) | |
| – ≥70 completely independent | Reference |
| – 60–69 independent to a great extent | 3.37 (2.80–4.07)* |
| – 45–59 partially dependent | 9.74 (8.11–11.71)* |
| – 25–44 dependent to a great extent | 27.42 (22.50–33.42)* |
| – ≤24 completely dependent | 52.65 (41.71–66.48)* |
| ICD-10 diagnosis group: mental and behavioural disorders | 2.22 (1.97–2.49)* |
| ICD-10 diagnosis group: factors influencing health status and contact with health services | 1.33 (1.12–1.58)* |
* Statistically significant based on the 95% CI
AIC = Akaike information criterion; ICC = intraclass correlation coefficient; SD = standard deviation; OR = odds ratio; 95% CI = 95% confidence interval; ICD-10 = International Statistical Classification of Diseases and Related Health Problems 10th Revision
In total, 35% of the variation in restraint use could be explained by fixed effects (selected patient characteristics; marginal R2 = 0.35). The full model, including the random effect (hospital, as a cluster variable), explained 43% of the variation in restraint use (conditional R2 = 0.43). Based on the ICC (0.12) and the log-likelihood ratio test (p-value <0.000), there was relevant and significant between-hospital variability, underlining the relevance of hospital as a random effect and thus indicating the great potential for benchmarking the use of restraints across hospitals.
The risk-adjusted hospital comparison (fig. 1) showed that hospitals in Switzerland differ significantly in their use of restraints, even when adjusting for patient characteristics. Figure 1 shows how 10 hospitals differed positively (in a clinical sense, i.e. they had lower restraint rates compared to other institutions) and 12 hospitals differed negatively (i.e., they had higher restraint rates) from the average.
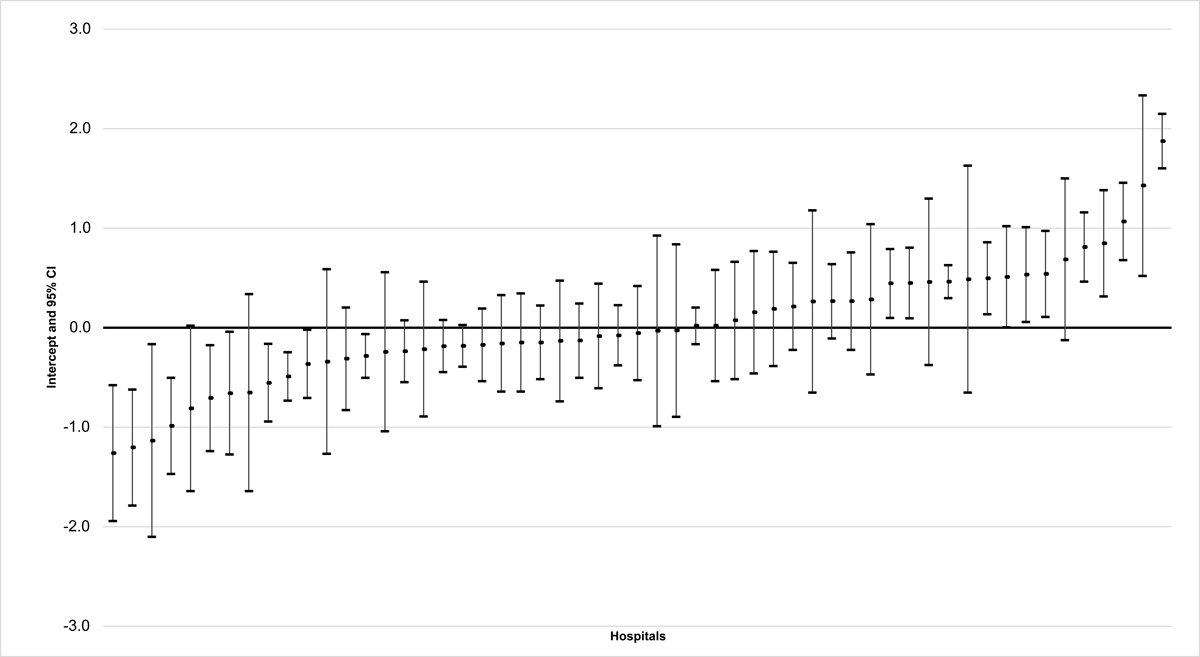
Figure 1 Risk-adjusted restraint use hospital comparison (residuals and 95% confidence interval [CI]).
In this secondary data analysis of cross-sectional data on restraint use in Swiss hospitals, we found a prevalence of restraint use of 10.2%. We detected a strong association of restraint use with the care dependency of patients, as well as with patients with mental and behavioural disorders. Furthermore, Swiss hospitals differed significantly regarding their restraint use, even after the adjustment for risk (taking into account the different patient mixes, and thus the different risk of hospitals for using restraints). Overall, 22 out of 55 hospitals differed significantly, either positively or negatively, from the average.
The 55 participating hospitals make up about one quarter of all hospitals in Switzerland. The characteristics of the patients included are comparable to those in the mandatory fall and pressure ulcer measurements, carried out using the same methodology [37]. Consequently, it can be assumed that the sample is likely to be representative for Swiss hospitals. The prevalence of restraint use of 10.2% includes electronic measures such as sensor mats or video surveillance, whereas most other studies in the hospital setting only examined mechanical restraint with belts. Therefore, comparisons of prevalence rates are not possible. However, as reported by Thomann et al. [10], mechanical restraint with belts constitutes only 9.7% of all mechanical restraints used in Swiss hospitals.
Based on the multilevel regression analysis, a very vulnerable patient group, namely older, more care-dependent patients and those with mental and behavioural disorders, seemed to be most affected by restraint use. This result is ethically highly relevant, as restraint use affects a group of patients who are often unable to defend their own rights. Therefore, it seems even more important that any use of restraints is critically analysed from both an ethical and a legal point of view. In this context, it is important to note that restraint use often violates a basic ethical principle: the expected positive health effects must exceed the harm. The positive effects of restraints in the hospital setting have not yet been proven [14, 18, 22].
Based on the risk-adjusted benchmarking, we found that restraint use differs significantly in Swiss hospitals. The caterpillar plot shows that 40% of all hospitals differ significantly, either positively or negatively, from the average. In comparison to other quality indicators, this is a very high value. For example, the same data collection method and a very similar statistical method were utilised for the ANQ"s "falls and pressure ulcers" national prevalence measurement. The number of outliers in past measurements of these quality indicators has been between 0% and 8% [37]. In other words, care quality regarding falls and pressure ulcers differs only slightly between Swiss hospitals. In contrast, there are relevant differences in restraint use. Such differences indicate potential for improvement [51]. Based on the results of this study, it remains unclear how the differences can be explained, especially as none of the included structural characteristics (guidelines, expert committees, audits, refresher courses) were selected for the model. Thus, it remains unclear which quality improvement measures could be effective in reducing restraint use.
Nevertheless, as mentioned above, factors that are difficult to measure, such as routine, institutional culture or attitudes, may have an influence on the results. Since restraint use is associated not only with quality of care, but also with human rights, it seems legally and ethically problematic if decision-making is based on (individual) opinions, attitudes or culture. Clearer and binding regulations and the promotion of critical scrutiny of hospitals' internal restraint practices could help to address the dilemma of legal certainty versus practical challenges (e.g., in patients with cognitive impairments) [26]. Thus, there seems to be a lot of potential for restraint use as a quality indicator for hospitals.
Restraint use is a very sensitive issue, and clear, binding legal regulations for hospitals are lacking [10]. Therefore, a national approach to quality measurement and development seems necessary. Firstly, such an approach would encourage discussion of the issue among policymakers, professional organisations and society. This would result in the establishment of the necessary structures at a macro level, which is an important element of quality development [36]. Secondly, a national approach consisting of monitoring and benchmarking would stimulate critical interprofessional discussions, both at different management levels within institutions and in direct patient care. Such interprofessional discussions across the different organisational levels of a hospital are needed to reflect on and address its institutional culture and routine, which seem to play an important role in the use of restraints [14, 52]. Thirdly, a national approach could also contribute to improving the current lack of data and evidence on restraint use in hospitals [53]. This would then enable the development and implementation of a (national) quality improvement program. Interprofessional decision-making based on evidence would then be promoted, instead of decision-making being based on personal opinions, the intuition or the institutional culture. An adequate database would also allow examination of the extent to which concepts for better restraint prevention and management from long-term care or mental health settings could be adapted for the hospital setting.
Although restraint use potentially violates human rights, there are no clear and binding legal regulations regarding restraint use in hospitals, despite it being well known that they are frequently used in this setting. This study highlights large risk-adjusted differences between Swiss hospitals regarding their restraint use. These differences seem questionable from a professional, ethical and legal point of view. Therefore, monitoring and benchmarking of restraint use in hospitals through a national quality indicator seems necessary. This would help ensure that restraint use is in alignment with professional values, as well as ethical and legal requirements. Additionally, it would stimulate quality improvement in this area and guarantee high-quality care in Swiss hospitals.
One limitation is the definition of restraints used. As can be expected, not all restraint types restrict freedom and human rights to the same extent, so it would be worth examining whether different restraint types should be analysed separately. Nevertheless, even measures such as sensor mats are restrictive interventions whose effectiveness has not yet been proven [7, 22]. On the contrary, it is currently a topic of discussion as to whether the risk of undesirable events increases when such electronic measures are used without reflection, thereby causing „alarm fatigue" [22]. Furthermore, the Swiss Academy of Medical Sciences guidelines also include electronic restraints, emphasising the need for critical reflection regarding their use and, therefore, the need to measure them along with all other restraint types [7]. We were not able to comprehensively cover the diversity of restraint measures. Different restraint measures have different impacts on the affected patients, both objectively and subjectively. However, it is unclear whether, for example, the impact felt from mechanical restraints is subjectively worse than that from pharmacological interventions. Much more sophisticated research is needed to gain more insight on this matter.
A second limitation with this measurement is that a potentially very vulnerable patient group, one that is heavily affected by restraint use (older patients, more care-dependent patients and/or patients with cognitive impairments), may have been excluded, as they were not able to give informed consent. Therefore, a selection bias may exist. A third limitation is the possibility of a recall or documentation bias, as restraint use was assessed within the institution over a period of 30 days. It is known that the use of restraints is often not well documented; therefore, some undocumented restraint use may not have been assessed within this measurement [10, 18]. Consequently, the use of restraints may have been underestimated. The assessment of restraint use over a 30-day period at the hospital level also meant the ward level could not be included in the multilevel modelling (i.e., a three-level model could not be built; see the Materials and methods section). Since restraint use may differ depending on ward type, future studies should assess restraint use at the ward level, as this could provide important information regarding intra-hospital variation.
Some limitations must also be expected due to the cross-sectional design and the instrument used. The cross-sectional design favours detecting variation within the population assessed, and the detection of causal associations and/or the direction of any associations is not possible. For example, care dependency could be the reason for, but also a consequence of restraint use. The instrument utilised included only certain organisational factors, and these were not selected for the model. In order to stimulate quality improvement, it would be worth examining which organisational factors are associated with restraint use. Due to the limited evidence available, some patient characteristics that are relevant for the risk adjustment might also be missing. A more in-depth investigation of risk factors to ensure adequate risk adjustment is necessary.
In addition, the hospital type was not considered in this analysis. However, we assumed that care dependency acted as a kind of proxy variable in this context, as the complexity of the patient cases and, consequently, the extent of (medical) care needed is relevant for the differences between hospital types. Also, due to hospital mergers, there is a risk of inadequate classification, as the hospital group's classification may not be accurate for all hospital sites within that hospital group.
Apart from these limitations, the results are likely to be generalisable for Swiss hospitals, as the large sample studied is comparable with the population assessed in the ANQ"s „falls and pressure ulcers" national prevalence measurement in Swiss hospitals [37]. In addition, the data collection method is well-established in Swiss hospitals and is expected to have a positive impact on data quality.
The data that support the findings of this study are available from the Swiss National Association for Quality Development in Hospitals and Clinics. However, restrictions apply to the availability of these data, which were used under licence for the current study and so are not publicly available.
We would like to thank the Swiss National Association for Quality Development in Hospitals and Clinics (ANQ) for their support with the data collection in Switzerland, Dr Reto Bürgin for sharing his experience in multilevel modelling, and all the hospitals and patients for their participation in the quality measurement.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
The data collection was funded as part of the "falls and pressure ulcers" national quality measurement by the Swiss National Association for Quality Development in Hospitals and Clinics (ANQ). Funding for data analysis was obtained through the Academic Practice Partnership of Bern University of Applied Sciences and University Hospital Bern (Insel Group).
Detailed information regarding variables (table S1), hospital and ward types (table S2), restraint types (table S3), reasons for restraint use (table S4) and the processes surrounding restraint use (table S5). A discussion of restraint types, reasons for restraint use and the processes surrounding restraint use can be found in Thomann et al. [10].
Table S1Variables.
| Level and variable | Details |
| Institutional level | |
| Availability of a protocol/guidelines regarding restraints (based on national/international guidelines) within the institution | Yes/no |
| Availability of a multi-disciplinary expert committee on restraints within the institution | Yes/no |
| Ward level | |
| Performance of regular audits to ensure compliance with the protocol/guidelines regarding restraints | Yes/no |
| Assessment regarding whether at least 80% of the ward"s nursing staff had attended a refresher course on restraints in the last two years | Yes/no |
| Patient level | |
| Age in years | Continuous |
| Sex | Female, male |
| Surgical intervention in the two weeks prior to data collection | Yes/no |
| Number of days since admission to hospital | Continuous |
| Medical diagnosis groups according to ICD-10 (International Statistical Classification of Diseases and Related Health Problems 10th Revision) [43] | Yes/no for each diagnosis group |
| Care dependency assessed using the care dependency scale (CDS) [54]. In the CDS, 15 items (e.g., eating and drinking or mobility) are rated on a Likert scale from 1 (completely dependent) to 5 (completely independent). It results in a sum score of 15–75 (higher score indicating higher care independency), which is divided into five categories (15–24 completely dependent, 25–44 dependent to a great extent, 45–59 partially dependent, 60–69 independent to a great extent, 70–75 completely independent). | Continuous or ordinal |
| Restraint use within the institution retrospectively over a maximum period of 30 days | Yes/no |
Table S2Sample description – hospital and ward type.
| Characteristics | Total (n = 18,938) | |
| Hospital type a | n | % (95% CI) |
| Centre care hospital | 8642 | 45.6 (44.9–46.3) |
| University hospital | 7384 | 39.0 (38.3–39.7) |
| Primary care hospital | 2537 | 13.4 (12.9–13.9) |
| Specialised hospital | 375 | 2.0 (1.8–2.2) |
| Ward type | ||
| Surgical | 8576 | 45.3 (44.6–46.0) |
| Non-surgical (medical) | 7154 | 37.8 (37.1–38.5) |
| Acute geriatrics | 950 | 5.0 (4.7–5.3) |
| Intensive care | 784 | 4.1 (3.9–4.4) |
| High dependency care | 411 | 2.2 (2.0–2.4) |
| Gynaecology | 409 | 2.2 (2.0–2.4) |
| Other | 401 | 2.1 (1.9–2.3) |
| Short stay | 147 | 0.8 (0.7–0.9) |
| Palliative care | 106 | 0.6 (0.5–0.7) |
a hospital type (specialisation) according to the Swiss Federal Office of Public Health [55]
Table S3Restraint type.
| Patients with restraint (n) | 1933 | |
| Restraint type (multiple responses) | n | % (95% CI) |
| Mechanical restraints | 1125 | 58.2 (56.0–60.4) |
| Type of mechanical restraint (multiple responses, only available for 2018) | ||
| n participants in 2018 | 6344 | |
| n mechanical restraints (yes) in 2018 | 454 | |
| Bed rails | 397 | 87.4 (84.0–90.4) |
| Other mechanical restraints | 85 | 18.7 (15.2–22.6) |
| Belt fixation | 43 | 9.5 (6.9–12.5) |
| Tabletop / chair table | 43 | 9.5 (6.9–12.5) |
| Electronic restraints | 694 | 35.9 (33.8–38.1) |
| Pharmacological restraints | 504 | 26.1 (24.1–28.1) |
| Other | 281 | 14.5 (13.0–16.2) |
| One-to-one supervisiona | 202 | 10.5 (9.1–11.9) |
| Physical restraint (keeping someone restrained with human physical force) | 67 | 3.5 (2.7–4.4) |
| Locked ward or building | 57 | 2.9 (2.2–3.8) |
95% CI = 95% confidence interval
a This answer option was only available for 2017 and 2018 (n participants = 12,560).
Table S4Reasons for restraint use.
| Patients with restraint (n) | 1933 | |
| Main reason for restraint use (single response) | n | % (95% CI) |
| (Preventing) falls | 935 | 48.4 (46.1–50.6) |
| Confusion or delirious behaviour | 419 | 21.7 (19.9–23.6) |
| Other motive | 190 | 9.8 (8.5–11.2) |
| Agitation | 106 | 5.5 (4.5–6.6) |
| At request of the patient and/or their family | 99 | 5.1 (4.2–6.2) |
| Non-compliance with treatment | 68 | 3.5 (2.7–4.4) |
| (Preventing) wandering around | 37 | 1.9 (1.4–2.6) |
| Unknown | 18 | 0.9 (0.6–1.5) |
| (Preventing) aggressive behaviour | 15 | 0.8 (0.4–1.3) |
95% CI = 95% confidence interval
Table S5Processes surrounding restraint use.
| Patients with restraint (n) | 1933 | |
| Process indicators (multiple responses) | n | % (95% CI) |
| The restraining was documented in the patient file. | 1270 | 65.7 (63.5–67.8) |
| The patient and/or their legal representatives were informed about the entire process surrounding the use of restraints. | 985 | 51.0 (48.7–53.2) |
| In each shift a person/nurse was appointed to monitor the patient undergoing restraint regularly, according to the defined prescription. | 858 | 44.4 (42.2–46.6) |
| The use of restraints was evaluated by all persons involved (including the patient). | 836 | 43.2 (41.0–45.5) |
| Primarily alternatives were used to minimise the use of restraints. | 724 | 37.5 (35.3–39.7) |
| None | 208 | 10.8 (9.4–12.2) |
95% CI = 95% confidence interval
1. Cusack P , Cusack FP , McAndrew S , McKeown M , Duxbury J . An integrative review exploring the physical and psychological harm inherent in using restraint in mental health inpatient settings. Int J Ment Health Nurs. 2018 Jun;27(3):1162–76. https://doi.org/10.1111/inm.12432
2. Richter D . Qualitätsindikatoren für die psychiatrische Versorgung - Eine Übersicht über Kriterien, Methoden und Probleme. Krankenhauspsychiatrie. 2004;15(03):104–13. https://doi.org/10.1055/s-2004-830051
3. Swiss National Association for Quality Development in Hospitals and Clinics (ANQ) . Erwachsenenpsychiatrie. 2020. [cited 2020 September 09]. Available from: https://www.anq.ch/de/fachbereiche/psychiatrie/messinformation-psychiatrie/erwachsenenpsychiatrie/
4. Australian Government Aged Care Quality and Safety Commission . Minimising the use of restraints. 2020. [cited 2020 September 09]. Available from: https://www.agedcarequality.gov.au/providers/assessment-processes/minimising-restraints
5. Bundesamt für Statistik . Alters- und Pflegeheime. 2020. [cited 2020 December 04]. Available from: https://www.bfs.admin.ch/bfs/de/home/statistiken/gesundheit/gesundheitswesen/alters-pflegeheime.html
6. Lachance, C. and M.-D. Wright Avoidance of Physical Restraint Use among Hospitalized Older Adults: A Review of Clinical Effectiveness and Guidelines. 2019.
7. Swiss Academy of Medical Sciences . Coercive measures in medicine. Medical-ethical guidelines. 2015, Swiss Academy of Medical Sciences: Bern.
8. Benbenbishty J , Adam S , Endacott R . Physical restraint use in intensive care units across Europe: the PRICE study. Intensive Crit Care Nurs. 2010 Oct;26(5):241–5. https://doi.org/10.1016/j.iccn.2010.08.003
9. Krüger C , Mayer H , Haastert B , Meyer G . Use of physical restraints in acute hospitals in Germany: a multi-centre cross-sectional study. Int J Nurs Stud. 2013 Dec;50(12):1599–606. https://doi.org/10.1016/j.ijnurstu.2013.05.005
10. Thomann S , Zwakhalen S , Richter D , Bauer S , Hahn S . Restraint use in the acute-care hospital setting: A cross-sectional multi-centre study. Int J Nurs Stud. 2021 Feb;114:103807. https://doi.org/10.1016/j.ijnurstu.2020.103807
11. De Bellis A , Mosel K , Curren D , Prendergast J , Harrington A , Muir-Cochrane E . Education on physical restraint reduction in dementia care: a review of the literature. Dementia. 2013 Jan;12(1):93–110. https://doi.org/10.1177/1471301211421858
12. Goethals S , Dierckx de Casterlé B , Gastmans C . Nurses’ decision-making process in cases of physical restraint in acute elderly care: a qualitative study. Int J Nurs Stud. 2013 May;50(5):603–12. https://doi.org/10.1016/j.ijnurstu.2012.10.006
13. Hignett S , Sands G , Fray M , Xanthopoulou P , Healey F , Griffiths P . Which bed designs and patient characteristics increase bed rail use? Age Ageing. 2013 Jul;42(4):531–5. https://doi.org/10.1093/ageing/aft040
14. Lach HW , Leach KM , Butcher HK . Evidence-based practice guideline: changing the practice of physical restraint use in acute care. J Gerontol Nurs. 2016 Feb;42(2):17–26. https://doi.org/10.3928/00989134-20160113-04
15. Fariña-López E , Estévez-Guerra GJ , Gandoy-Crego M , Polo-Luque LM , Gómez-Cantorna C , Capezuti EA . Perception of spanish nursing staff on the use of physical restraints. J Nurs Scholarsh. 2014 Sep;46(5):322–30. https://doi.org/10.1111/jnu.12087
16. Freeman S , Hallett C , McHugh G . Physical restraint: experiences, attitudes and opinions of adult intensive care unit nurses. Nurs Crit Care. 2016 Mar;21(2):78–87. https://doi.org/10.1111/nicc.12197
17. Gu T , Wang X , Deng N , Weng W . Investigating influencing factors of physical restraint use in China intensive care units: A prospective, cross-sectional, observational study. Aust Crit Care. 2019 May;32(3):193–8. https://doi.org/10.1016/j.aucc.2018.05.002
18. Perez D , Peters K , Wilkes L , Murphy G . Physical restraints in intensive care-An integrative review. Aust Crit Care. 2019 Mar;32(2):165–74. https://doi.org/10.1016/j.aucc.2017.12.089
19. Kiekkas P , Aretha D , Panteli E , Baltopoulos GI , Filos KS . Unplanned extubation in critically ill adults: clinical review. Nurs Crit Care. 2013 May;18(3):123–34. https://doi.org/10.1111/j.1478-5153.2012.00542.x
20. Sze TW , Leng CY , Lin SK . The effectiveness of physical restraints in reducing falls among adults in acute care hospitals and nursing homes: a systematic review. JBI Library Syst Rev. 2012;10(5):307–51. https://doi.org/10.11124/jbisrir-2012-4
21. Ai ZP , Gao XL , Zhao XL . Factors associated with unplanned extubation in the Intensive Care Unit for adult patients: A systematic review and meta-analysis. Intensive Crit Care Nurs. 2018 Aug;47:62–8. https://doi.org/10.1016/j.iccn.2018.03.008
22. LeLaurin JH , Shorr RI . Preventing falls in hospitalized patients: state of the science. Clin Geriatr Med. 2019 May;35(2):273–83. https://doi.org/10.1016/j.cger.2019.01.007
23. Hofmann H , Hahn S . Characteristics of nursing home residents and physical restraint: a systematic literature review. J Clin Nurs. 2014 Nov;23(21-22):3012–24. https://doi.org/10.1111/jocn.12384
24. Möhler R , Nürnberger C , Abraham J , Köpke S , Meyer G . Interventions for preventing and reducing the use of physical restraints of older people in general hospital settings. Cochrane Libr. 2016;(12): https://doi.org/10.1002/14651858.CD012476
25. Said AA , Kautz DD . Reducing restraint use for older adults in acute care. Nursing. 2013 Dec;43(12):59–61. https://doi.org/10.1097/01.NURSE.0000437484.75992.ca
26. Salehi Z , Najafi Ghezeljeh T , Hajibabaee F , Joolaee S . Factors behind ethical dilemmas regarding physical restraint for critical care nurses. Nurs Ethics. 2020 Mar;27(2):598–608. https://doi.org/10.1177/0969733019858711
27. Registered Nurses’ Association of Ontario Promoting Safety : Alternative Approaches to the Use of Restraints. 2012.
28. Pivodic L , Smets T , Gambassi G , Kylänen M , Pasman HR , Payne S , et al.; PACE . Physical restraining of nursing home residents in the last week of life: an epidemiological study in six European countries. Int J Nurs Stud. 2020 Apr;104:103511. https://doi.org/10.1016/j.ijnurstu.2019.103511
29. Abraham J , Kupfer R , Behncke A , Berger-Höger B , Icks A , Haastert B , et al. Implementation of a multicomponent intervention to prevent physical restraints in nursing homes (IMPRINT): A pragmatic cluster randomized controlled trial. Int J Nurs Stud. 2019 Aug;96:27–34. https://doi.org/10.1016/j.ijnurstu.2019.03.017
30. Australian Government Department of Health . Minimising inappropriate use of restraint in aged care. 2020. [cited 2020 September 09]. Available from: https://www.health.gov.au/initiatives-and-programs/minimising-inappropriate-use-of-restraint-in-aged-care
31. Australian Government National Mental Health Commission . Reducing Restrictive Practices. 2020. [cited 2020 September 09]. Available from: https://www.mentalhealthcommission.gov.au/Mental-health-Reform/Reducing-restrictive-practices
32. Lombardo C , Van Bortel T , Wagner AP , Kaminskiy E , Wilson C , Krishnamoorthy T , et al. PROGRESS: the PROMISE governance framework to decrease coercion in mental healthcare. BMJ Open Qual. 2018 Jul;7(3):e000332. https://doi.org/10.1136/bmjoq-2018-000332
33. Perren A , Corbella D , Iapichino E , Di Bernardo V , Leonardi A , Di Nicolantonio R , et al. Physical restraint in the ICU: does it prevent device removal? Minerva Anestesiol. 2015 Oct;81(10):1086–95.
34. Möhler R , Meyer G . Attitudes of nurses towards the use of physical restraints in geriatric care: a systematic review of qualitative and quantitative studies. Int J Nurs Stud. 2014 Feb;51(2):274–88. https://doi.org/10.1016/j.ijnurstu.2013.10.004
35. Teece A , Baker J , Smith H . Identifying determinants for the application of physical or chemical restraint in the management of psychomotor agitation on the critical care unit. J Clin Nurs. 2020 Jan;29(1-2):5–19. https://doi.org/10.1111/jocn.15052
36. Busse R , et al., editors . Improving healthcare quality in Europe. Characteristics, effectiveness and implementation of different strategies. Health Policy Series. 2019, World Health Organization (WHO), Organisation for Economic Co-operation and Development (OECD): United Kingdom.
37. Thomann S , et al. Sturz und Dekubitus Akutsomatik Erwachsene. Nationaler Vergleichsbericht 2019. 2020, Nationaler Verein für Qualitätsentwicklung in Spitälern und Kliniken (ANQ), Berner Fachhochschule, Angewandte Forschung und Entwicklung Pflege: Bern.
38. van Nie-Visser NC , Schols JM , Meesterberends E , Lohrmann C , Meijers JM , Halfens RJ . An international prevalence measurement of care problems: study protocol. J Adv Nurs. 2013 Sep;69(9):e18–29. https://doi.org/10.1111/jan.12190
39. National Institute for Health and Care Excellence . Violence and aggression: short-term management in mental health, health and community settings. 2015, NICE.
40. Akaike H . A new look at the statistical model identification. IEEE Trans Automat Contr. 1974;19(6):716–23. https://doi.org/10.1109/TAC.1974.1100705
41. Venables WN , Ripley BD . Modern Applied Statistics with S. 4 ed. 2002, New York: Springer.
42. Bates D , Mächler M , Bolker B , Walker S . Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;67(1):1–48. https://doi.org/10.18637/jss.v067.i01
43. World Health Organization . International Statistical Classification of Diseases and Related Health Problems 10th Revision. 2016. [cited 2019 November 01]. Available from: https://icd.who.int/browse10/2016/en#/XIII
44. R Core Team . R: A language and environment for statistical computing. 2020, R Foundation for Statistical Computing: Vienna, Austria.
45. Subirana I , Sanz H , Vila J . Building Bivariate Tables: The compareGroups Package for R. J Stat Softw. 2014;57(12):1–16. https://doi.org/10.18637/jss.v057.i12
46. Harrell, F.E. and C. Dupont , Hmisc: Harrell Miscellaneous. R package version 4.4-1. 2020.
47. Long, J.A. , _jtools: Analysis and Presentation of Social Scientific Data_. R package version 2.0.1. 2019.
48. Bartoń, K. , MuMIn: Multi-Model Inference. R package version 1.43.17. 2020.
49. Lüdecke, D. , _sjPlot: Data Visualization for Statistics in Social Science_. R package version 2.8.4. 2020.
50. Wickham H , Averick M , Bryan J , Chang W , McGowan L , François R , et al. Welcome to the tidyverse. J Open Source Softw. 2019;4(43):1686. https://doi.org/10.21105/joss.01686
51. van der Kooi AW , Peelen LM , Raijmakers RJ , Vroegop RL , Bakker DF , Tekatli H , et al. Use of physical restraints in Dutch intensive care units: a prospective multicenter study. Am J Crit Care. 2015 Nov;24(6):488–95. https://doi.org/10.4037/ajcc2015348
52. Kong EH , Choi H , Evans LK . Staff perceptions of barriers to physical restraint-reduction in long-term care: a meta-synthesis. J Clin Nurs. 2017 Jan;26(1-2):49–60. https://doi.org/10.1111/jocn.13418
53. Xyrichis A , Hext G , Clark LL . Beyond restraint: raising awareness of restrictive practices in acute care settings. Int J Nurs Stud. 2018 Oct;86:A1–2. https://doi.org/10.1016/j.ijnurstu.2018.06.006
54. Dijkstra A , Yönt GH , Korhan EA , Muszalik M , Kędziora-Kornatowska K , Suzuki M . The care dependency scale for measuring basic human needs: an international comparison. J Adv Nurs. 2012 Oct;68(10):2341–8. https://doi.org/10.1111/j.1365-2648.2011.05939.x
55. Federal Office of Public Health . Facts & figures on hospitals. 2018. [cited 2021 June 28]. Available from: https://www.bag.admin.ch/bag/en/home/zahlen-und-statistiken/zahlen-fakten-zu-spitaelern.html