Figure 1 Screenshot from the guidance on the management of acute severe peripheral arterial disease.
DOI: https://doi.org/10.4414/SMW.2021.w30045
Diabetic foot syndromes (DFS) are a heterogenous group of frequent and serious problems of the diabetic foot encompassing ischaemia, infection, Charcot foot deformities and other complications [1, 2]. They are usually difficult to treat and associated with substantial morbidity, treatment failure, and high psychological burden and financial costs [1–10]. Common reasons for treatment failure include inappropriate pressure off-loading, underestimated peripheral arterial disease, missed infection and a delay in referral to specialized centers [1–10] (if they exist). Twenty years ago, approximately 175 million people were suffering from diabetes mellitus worldwide. By 2030, the number could rise to 360 million [1, 2]. Switzerland is no exception. Despite the presence of an efficient health system in Switzerland, the annual incidence of diabetic foot ulcers and amputations remains high. Krzywicki et al. showed in 2012 that diabetic foot ulcers, their recurrence and the consequent amputations increased in Switzerland during the previous decade [3]. In 2016, the Swiss Federal Statistic Office and the INFRAS Institute reported an annual number of 1600 amputations in Switzerland, a country with roughly 8 million inhabitants [11], translating into an estimated annual increase of 5% in Switzerland since 2012. In the same year, Schimke et al. estimated a 20% prevalence of foot ulcers in the Swiss diabetic population [8], resulting in a conservatively estimated attributable annual cost of 96 million Swiss Francs per year [11].
There are internationally accepted guidelines, for example,from the Infectious Diseases Society of America (IDSA) [1] or the International Working Group on the Diabetic Foot (IWGDF) [5, 6]. While these documents offer helpful give guidance on management of diabetic foot syndromes, they do not provide information on how to conduct surveillance or how care is provided or to actively set up networks to deal with these problems.They “only” give guidance, but do not survey care or actively set up networks. They also are usually not country-specific or mostly target one specific aspect of DFS – infection – although DFS usually reflect more than one concomitant problem; and the rapidity to professional care is an issue. The nationwide lack of a comprehensive definition of diagnosis, therapy and a structured itinerary (nationwide clinical pathway) motivated the Swiss Society of Endocrinology and Diabetology (SSED), in close collaboration with QualiCCare [7], to develop a nationwide interdisciplinary short guideline based on "good practices", and also to implement these practices and make them operational on a sustained basis. As the Swiss health system differs from one region to another, this guidance will help to unify the management of DFS patients. This manuscript only presents our quality of care project. The scientific aspects behind the individual strata of DFS are addressed in prior publications [2, 6, 8, 9].
QualiCCare is an interprofessional, multi-stakeholder association that adapts international best practices and guidelines for Switzerland and performs pilot projects for their implementation (www.qualiccare.ch). In late 2017, QualiCCare and the SSED invited 12 Swiss healthcare societies to delegate an expert in the field of DFS. All societies agreed and proposed 8 women and 12 men, representing the German- and French-speaking parts of Switzerland. The experts worked in subgroups of six to eight persons on specific topics according to their expertise. Chaired by the first author (BPR), the working group of QualiCCareheaded these subgroups. In a second step, the work of these subgroups was discussed and validated by the entire group. The group also defined three levels of DFS care for Switzerland, based on severity of DFS, and decided to pilot the project in three regions. This project may also provide data for academic purposes.
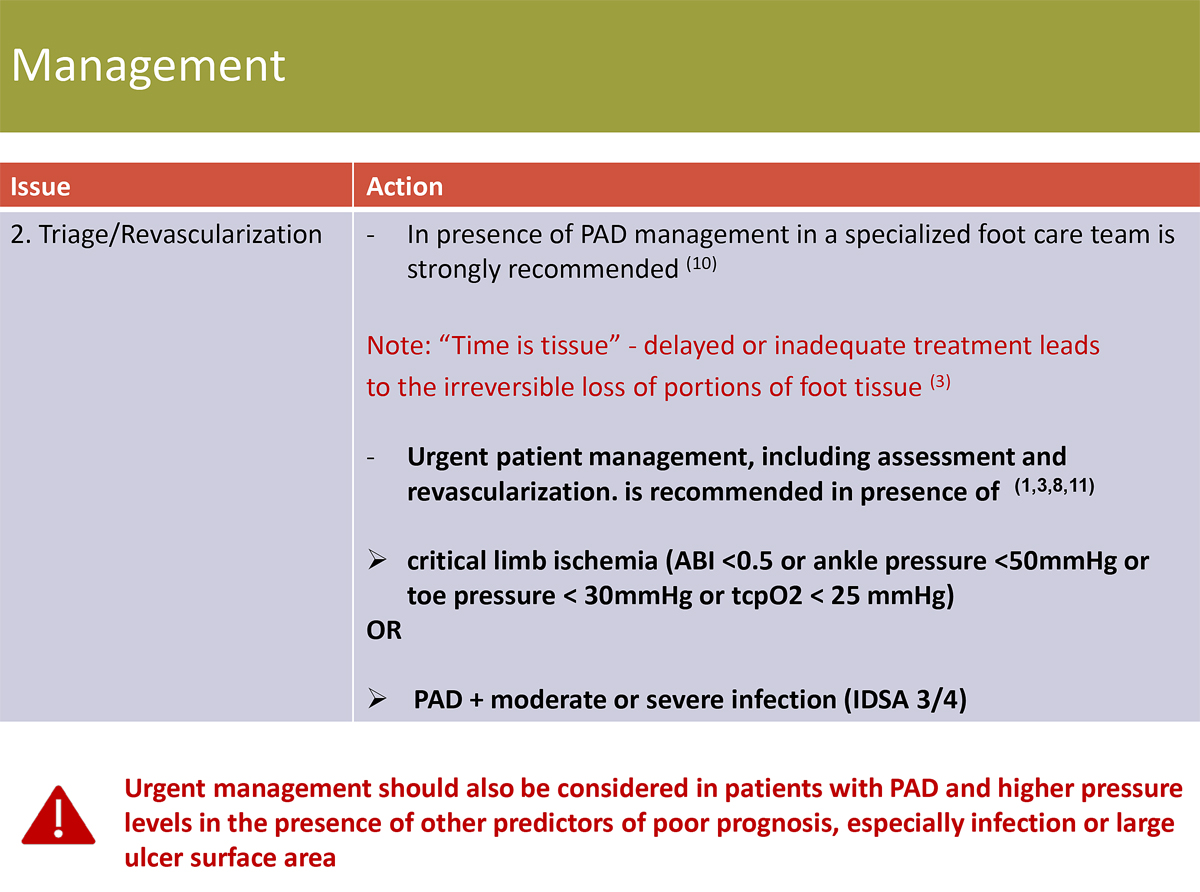
The following Swiss societies participated: endocrinology and diabetology, orthopaedic surgery, infectiology, angiology, interventional radiology, vascular surgery, wound nurses and general internal medicine. Further professions include a diabetology nurse specialised in wound care, a pharmacist, orthopaedic shoemakers, a representative of a health insurer, and podiatrists. After four plenary meetings in Bern, and six individual subgroup sessions between March 2018 and January 2020, we issued four short protocols (keyword-style, with "red flags", take-home messages, 8–10 pages long). The protocols are laid out as brochures and are freely accessible at the website www.qualiccare.ch and on the homepages of the individual societies. They are currently in English and German or French, but will be translated into Italian after the pilot evaluation. We have not provided printed booklets. Figure 1 gives an example of a short protocol page regarding the fast-track approach to acute ischaemia.
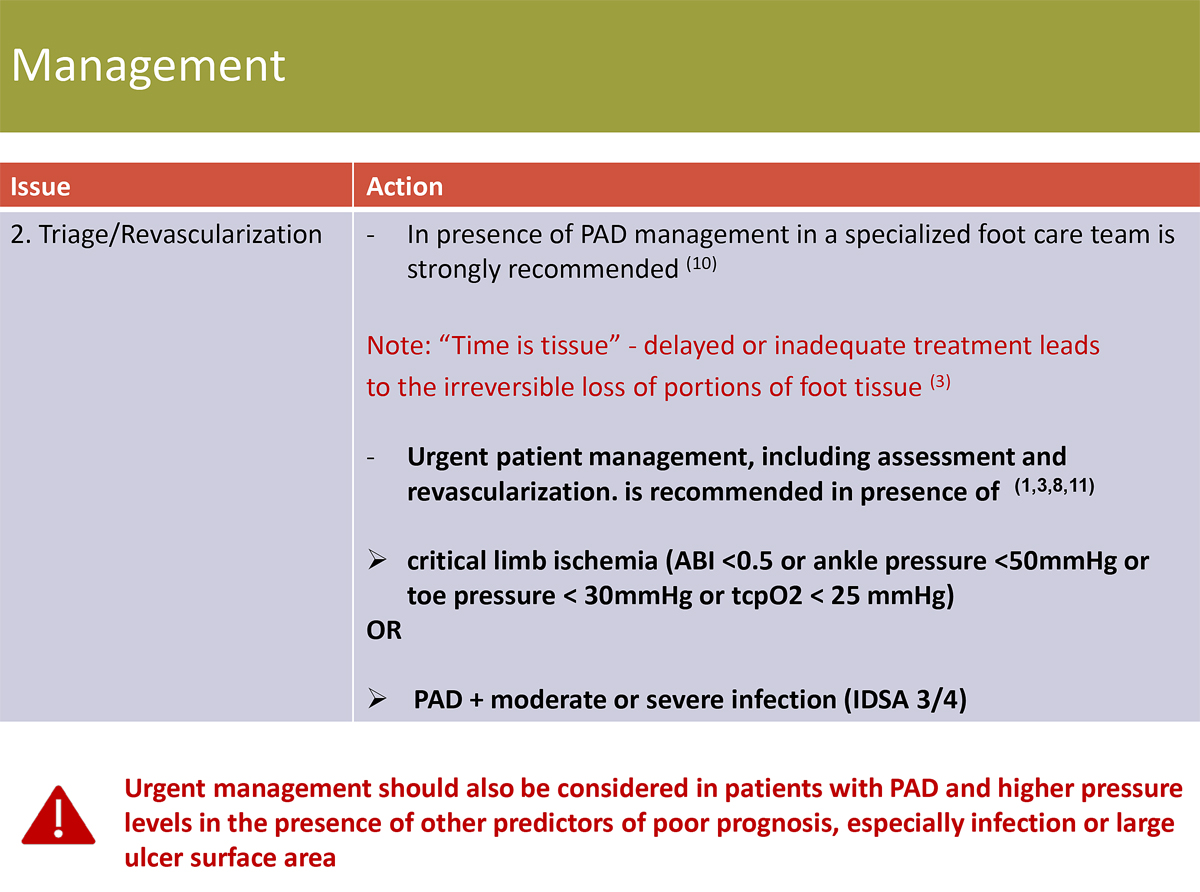
Figure 1 Screenshot from the guidance on the management of acute severe peripheral arterial disease.
Figure 2 represents the protocol for suspected Charcot arthropathy. The appendix provides a full example for infections. Both figures and the appendix were edited by QualiCCare (AZ) and approved for publication in this manuscript.
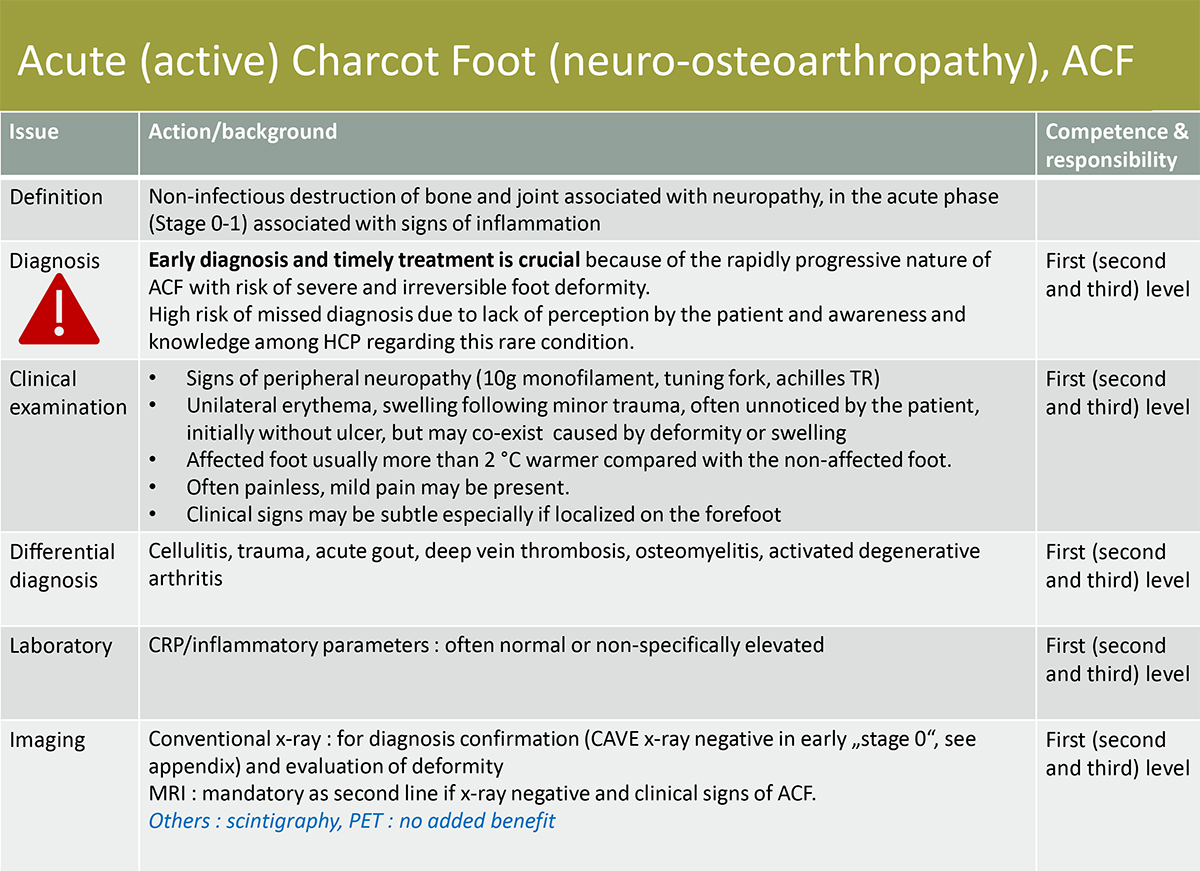
Figure 2 Example of the guidance for awareness in suspected acute Charcot arthropathy.
Table 1 summarises the key messages targeting acute ischaemia [10], infections [1–6], Charcot arthropathy [12, 13], off-loading [4, 5, 14] and the triage and treatment of DFS in primary care. We further identified three levels of care settings/networks, according to the severity (and the urgency) of DFS and propose to implement such specialised care structures across Switzerland (Table 2). On the first level, the patient is treated by a primary care provider, who can be a general practitioner, a pharmacist, a specialised nurse, or a podiatrist. These first-level, single-discipline settings should have expertise in DFS, meaning that they should see DFS patients regularly and know the triage requirements. Additional experts are non-urgent and involved when needed. The second level consists of a network of experienced clinicians who are able to correctly diagnose the underlying problem and to refer the patient to specific care without delay. This requires a pre-established network, which does not necessarily have to be on-site. The third level requires the immediate accessibility of all specialists, who are required for each individual case, including the possibility to perform invasive interventions (in-house or in a neighbouring hospital). Usually, this third level is a hospital, but it does not need to be. Provided that the expertise is available at any moment, level III can also be composed of experienced clinicians with secondary rapid access to invasive interventions. QualiCCare and the project leaders will identify these third level centres and ensure their financing in the coming years.
Table 1 Examples of information in the proposed Swiss guidance on diabetic foot syndrome (DFS)- stratified by the most important key messages.
| Main identified problem | Proposed solution | Difficulties for implementation | |
| Peripheral arterial disease | Loosing time before revascularisation. Time is tissue. | Rapid access to vascular evaluation and eventual intervention. Practical guidance for every clinician. Red flags. | Necessity for transfer to a secondary or tertiary specialised centre and hospitalisation. |
| Charcot arthropathy | Missed recognition and missed early treatment. | Awareness, knowledge, magnetic resonance imaging with experienced radiologists, further consultation without losing time. | Recognition of the medical emergency of acute Charcot arthropathy, mimicking infection. Correct and consequent off-loading. |
| Infectious diseases | Excess of iterative antibiotic prescription with adverse events and lack of clinical benefit. | Antibiotic stewardship in the field of DFS. Streamlining of therapies. Surgery, off-loading, debridement. | Lack of experience in antibiotic stewardship in low-volume centres. Desperate situations with easy solution of antibiotic prescription for preventive reasons. |
| Off-loading | Compliance, adherence of the patient. | Education, specialised technicians and centres. Choosing the off-loading strategy with patient considering the individual situation to achieve highest possible adherence. | Adherence, secondary ulceration, close clinical controls by specialised healthcare workers. Eventually thrombosis prophylaxis. Off-loading is an interim solution, not the final answer. |
Table 2Proposed requirements for specialised diabetic foot syndrome (DFS) centres in Switzerland.
| Level of centre | Requirements | Composition | Difficulties |
| I General practitioner; podiatrist; specialised nurses | Expertise of the individual clinician or nurse / podiatrist in the field of DFS, either by long-term experience, scientific output or participation in professional networks specialised in DFS. | Single expert or two. Mostly the general practitioner or the diabetologist, but identifiable as an expert in DFS. | Limited to DFS of mild or moderate severity. Definition of "expert in DFS" is a flaw, as there are no official titles in Switzerland. Few accessible for emergencies. |
| II Local network | Several medical and nursing experts in close collaboration, able to treat and follow-up all DFS in an outpatient setting, including debridement, antibiotic therapy, and radiological and angiology work-ups. | Diabetologist, specialized nurse / podiatrist. Availability of a specialised infectious diseases physician, radiologist or angiologist within 2–3 days. | Difficult accessibility during night shifts and/or week-ends. Depends on the individual expertise of the specialised healthcare workers. Invasive interventions performed by a third party, who must agree with the request and recommendations. |
| III Regional diabetic foot centre or network | All expertise and all invasive procedures available within 24 hours, including during night shifts and week-ends. Easily accessible emergency line 24/7. | All medical and nursing disciplines available, including surgeons. All interventions needed accessible without major delay or transfer, with replacements during holidays. | Costly to maintain, if organised as an outpatient network system of specialists. On guard accessibility during night shifts. |
We are piloting the implementation of our project in three regions of Switzerland: Lucerne, Sion/Valais, and Burgdorf/Emmental. The practical pilot will lastfor approximatively 12 months (with possible extension to 18 months because of the COVID-19 pandemic) to obtain a representative number of DFS patients and to give valid feedback on the practicality and benefit for both healthcare providers and patients. We expect higher efficiency and better coordination of DFS care. First interim results should be available by mid-2022.
DFSs are frequent, in Switzerland and worldwide, and mostly concern multimorbid, frail patients with long-standing diabetic mellitus and probably (secondary) poor compliance [1, 3]. Our daily experience suggests that we regularly lose time and resources with DFS episodes for various reasons: late referral, non-compliance, inadequate off-loading, resignation, delays in treatment for infection or revascularisation, immobile patients, unprofessional debridement and rudimentary experience in DFS. Due to the high prevalence of DFS, it is imperative that its management must be better recognised and standardised at the national level. The experts or centres treating this pathology must be easily identifiable, allowing healthcare professionals to quickly identify the problem and to know when and where they should refer a patient. Therefore, our project does not primarily aim to spread knowledge, but rather to facilitate nation-wide access to specialised care in a timely manner. We chose a freely accessible website with short information available at a glance. Of note, our protocols do not replace already existing recommendations in Switzerland, such as those on antibiotic therapy for diabetic foot infections [15]. We intend to complement these and to make them operational. The recommendations are open for discussion and can be updated upon feedback from the medical and nursing community of Switzerland and abroad.
Our project is congruent with the majority of international guidance. For example, the latest IDSA guidelines on diabetic foot infections [1] propose multidisciplinary rapid-response teams, and encouragement by medical institutions, insurance companies and other healthcare systems. Also, the IDSA encourages diabetic foot centres of excellence to audit regularly various aspects of processes and outcomes [1].
Despite being a nationwide quality of care project, we see two potential shortcomings.
First, we have no guaranteed public support besides our societies, putting the sustainability in question. However, QualiCCare has experience in implementing and sustaining quality projects [7] and has some political support. Furthermore, DFS are very probably gaining prominence among decision makers. One of the best signs of this is that the podiatrists are in the process of being reimbursed by insurance (should be effective in 2022), which will be a great step towards better management/prevention of foot ulcers in our diabetic patients [11, 16]. Second, our method of national consensus finding was different from those used in the devlopement of international guidelines. For example, in the IWGDF guidelines [5] for diabetic foot infections, the expert panels followed the GRADE methodology, structuring it around clinical questions in the PICO (Patient, Intervention, Comparison, Outcome) format, followed by recommendations and the rationale for them [5]. They judged a recommendation to be "strong", "moderate" or "weak" [5]. In contrast, we did not interpret data in terms of scientific evidence, but focused on practical aspects from the start. We did not need to use established paths designed for synthesising judgements for a broader audience, such as the Delphi, the Nominal Group Technique, or the Consensus Development Conference techniques [17].
Our interprofessional group of experts in DFS proposes a nationwide guidance and the implementation of rapidly accessible recommendations in Switzerland for all aspects of DFS. We also provide evidence-based tools for all primary care providers and specialists in the management of DFS. We define criteria for referral to interprofessional foot-care centres and increase the accessibility of all patients to specialised highly professional care. This project is currently in the pilot phase and should be developed further. We therefore need to exchange of experiences and encourage all colleagues who regularly treat DFS patients to support this nationwide project.
Interdisciplinary Expert Group for the Diabetic Foot of Swiss Society of Endocrinology and Diabetology: Bettina Peter-Riesch, Astrid Czock, Ulf Benecke, Thomas Böni, Bernard Chappuis, Angela Cottier, Emanuel Christ, Marc Egli, Sandro Fraternali, Christian Frei, Isabelle Hagon-Traub, Axel Haine, Mario Malgaroli, Dieter Mayer, Salah Qanadli, Christina Ruob, Katrin Schimke, Claude Schoenenweid, Ilker Uçkay, and Véronique Urbaniak.
This project and guidance are endorsed by the following professional societies. The corresponding endorsements principally address the specialty of the Society.
Swiss Society of Endocrinology and Diabetology www.sgedssed.ch
Swiss Diabetic Nursing Society www.sidb-gicid.ch
Swiss Orthopaedics www.swissorthopaedics.ch
The Union of Vascular Societies of Switzerland UVSS www.uvs.ch
Swiss Society for Wound Care www.safw.ch
Swiss Society for Angiology www.angioweb.ch
Swiss Society for Infectious Diseases www.sginf.ch
Swiss Society of Pharmacists www.pharmasuisse.org
Swiss Society of Radiology www.sgr-ssr.ch
Swiss Surgeons www.sgc-ssc.ch
QualiCCare www.qualiccare.ch
Swiss Society of Family Doctors www.hausaerzteschweiz.ch
Association Pied et Chaussure www.fussundschuh.ch
SWİCA Insurance www.swica.ch
Swiss Organization of Podiatry, www.ops.ch
We thank all representatives of the involved professional societies for their valuable contribution to this project and to Prof. Benjamin A. Lipsky for assistance in medical English language. We are indebted to QualiCCare under the lead of Hans Stöckli, member of the Swiss Council of States.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
AC is an employee of QualiCCare. The elaboration of the best practice recommendations by the working group was financed by QualiCCare. Funding for the practice implementation of the best practices is requested with different foundations and organisations. To date, funding is confirmed by the following: Swiss Diabetes Foundation, Swiss Organisation of Podiatrists, Research Fund for Diabetology of Lucerne Cantonal Hospital, Berner Hilfswerk. Further requests are under way.
1. Lipsky BA , Berendt AR , Cornia PB , Pile JC , Peters EJ , Armstrong DG , et al. 2012 Infectious Diseases Society of America (IDSA) clinical practice guideline for the diagnosis and treatment of diabetic foot infections. Clin Infect Dis. 2012;54(12):132–73. https://doi.org/10.1093/cid/cis346
2. Uçkay I , Jornayvaz FR , Lebowitz D , Gastaldi G , Gariani K , Lipsky BA . An Overview on Diabetic Foot Infections, including Issues Related to Associated Pain, Hyperglycemia and Limb Ischemia. Curr Pharm Des. 2018;24(12):1243–54. https://doi.org/10.2174/1381612824666180302145754
3. Krzywicki CP , Wasserfallen JB . [Hospitalizations due to diabetic foot in Switzerland]. Rev Med Suisse. 2012 Jun;8(344):1215–6.
4. Peter-Riesch B . The diabetic foot: the never-ending challenge. Endocr Dev. 2016;31:108–34. https://doi.org/10.1159/000439409
5. Lipsky BA , Senneville E , Abbas ZG , Aragón-Sánchez J , Diggle M , Embil JM , et al. IWGDF guideline on the diagnosis and treatment of foot infection in people with diabetes. Diabetes Metab Res Rev. 2020;36:3280.
6. Ertuğrul B , Uçkay I , Schöni M , Peter-Riesch B , Lipsky BA . Management of diabetic foot infections in the light of recent literature and new international guidelines. Expert Rev Anti Infect Ther. 2020 Apr;18(4):293–305. https://doi.org/10.1080/14787210.2020.1730177
7. Valeri F , Hatz C , Jordan D , Leuthold C , Czock A , Lang P . Immunisation coverage of adults: a vaccination counselling campaign in the pharmacies in Switzerland. Swiss Med Wkly. 2014 Apr;144:w13955. https://doi.org/10.4414/smw.2014.13955
8. Schimke K , Chappuis B , Egli M , Hagon-Traub I , Malacarne S , Schönenweid C , et al. Prévention et prise en charge des problèmes de pieds chez les patients diabétiques. Swiss Medical Forum-Forum Médical Suisse. 2016;16(2829):578–83. https://doi.org/10.4414/fms.2016.02695
9. Malacarne S , Chappuis B , Egli M , Hagon-Traub I , Schimke K , Schönenweid C , et al. [Preventive measures of diabetic foot complications]. Rev Med Suisse. 2016 Jun;12(521):1092–6.
10. Hinchliffe RJ , Brownrigg JR , Andros G , Apelqvist J , Boyko EJ , Fitridge R , et al.; International Working Group on the Diabetic Foot . Effectiveness of revascularization of the ulcerated foot in patients with diabetes and peripheral artery disease: a systematic review. Diabetes Metab Res Rev. 2016 Jan;32 Suppl 1:136–44. https://doi.org/10.1002/dmrr.2705
11. Vettori A , von Stokar T , Angst V , Diem P. INFRAS. Auswirkungen der Aufnahme von Podologinnen und Podologen als Leistungserbringer zulasten der obligatorischen Krankenpflegevrrsicherung (OKP). INFRAS: 30 November 2018.
12. Rosskopf AB , Loupatatzis C , Pfirrmann CW , Böni T , Berli MC . The Charcot foot: a pictorial review. Insights Imaging. 2019 Aug;10(1):77. https://doi.org/10.1186/s13244-019-0768-9
13. Chantelau EA , Richter A . The acute diabetic Charcot foot managed on the basis of magnetic resonance imaging—a review of 71 cases. Swiss Med Wkly. 2013 Jul;143:w13831. https://doi.org/10.4414/smw.2013.13831
14. Lewis J , Lipp A . Pressure-relieving interventions for treating diabetic foot ulcers. Cochrane Database Syst Rev. 2013 Jan;1(1):CD002302. https://doi.org/10.1002/14651858.CD002302.pub2
15. Swiss Society for Infectious Diseases . DIGEST-Guideline 2019: Infections du pied diabétique. https://ssi.guidelines.ch/guideline/3056 (last assessed on 4 July 2021). French-language version; also available as a German-language version.
16. Bundesamt für Gesundheit. Änderung der Verordnung über die Krankenversicherung und der Krankenpflege-Leistungsverordnung. Zulassung der Podologinnen und Podologen als Leistungserbringer im Rahmen der obligatorischen Krankenpflegeversicherung (OKP). https://www.bag.admin.ch/bag/de/home/versicherungen/krankenversicherung/krankenversicherung-revisionsprojekte/aenderungen-zulassung-podologen-als-leistungserbringer.html
17. Black N , Murphy M , Lamping D , McKee M , Sanderson C , Askham J , et al. Consensus development methods: a review of best practice in creating clinical guidelines. J Health Serv Res Policy. 1999 Oct;4(4):236–48. https://doi.org/10.1177/135581969900400410
The appendix is available as separate PDF file for download. It was edited by QualiCCare (AZ) and approved for publication with this manuscript.