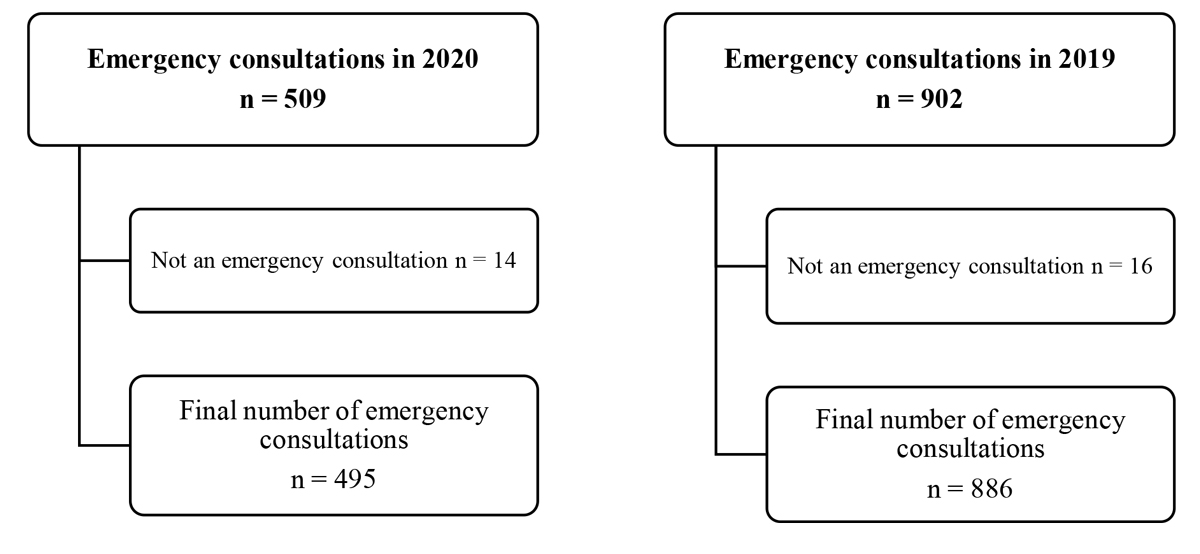
Figure 1 The total number of emergency consultations between 16 March and 26 April, in 2020 and 2019 are shown. Patients were excluded if they had a follow-up visit wrongly labelled as an emergency consultation.
DOI: https://doi.org/10.4414/SMW.2021.w30068
So far, almost 202 million cases and over 4 million deaths have been registered worldwide since the outbreak of the SARS-CoV-2 pandemic [1]. In Switzerland, more than 700,000 people have been tested SARS-CoV-2 positive, which translated into over 10,000 deaths directly linked to the disease [1]. Facing the spread of the pandemic towards western Europe in February 2020, the Swiss government, like most of the neighbouring countries, decided to impose a national lockdown. Thus, along with the call for social distancing, healthcare institutions were requested to postpone all non-urgent consultations, interventions and treatments, in order to spare medical resources (e.g., staff, infrastructure, consumables) [2]. However, besides the reduction of elective consultations and treatments, a marked decrease in emergency visits was observed [3–5]. Possible reasons for this development might be restriction of public life (working from home, closure of schools, ban of public events), but also patients' fear of contact with healthcare providers [2]. The aim of the present study was to investigate the emergency consultations at the largest otorhinolaryngological (ENT) department in Switzerland and to compare the prepandemic (2019) to the pandemic (2020) era. Furthermore, we aimed to assess the effect of postponing non-urgent appointments on disease progression of three particular otorhinolaryngological disease entities, namely chronic rhinosinusitis (CRS), and benign and malignant tumours.
In this monocentric study at a tertiary referral centre we retrospectively reviewed the number of and reason for all consecutive emergency consultations at the Department of Otorhinolaryngology (University Hospital of Zurich, Switzerland) between 16 March 2020 and 26 April 2020 [2]. This period covers the time when healthcare institutions were requested to postpone all non-urgent consultations, interventions and treatments, in order to spare medical resources during lockdown in Switzerland.
Emergency consultations during the same period in 2019 served as a control group. These visits were grouped according to the diagnoses. For instance, consultations due to bacterial infections, acute pain or wound infections of the nasal region were summarised as other rhinological emergencies. The number of inhabitants and therefore the catchment area of our tertiary care hospital stayed largely unchanged over the years, consequently the population at risk of developing an emergency was unchanged. Hence, data between years are directly comparable. All data were retrieved from the clinical information system (KISIM) and systematically ordered in an Excel document. Duplicate data or unavailable medical records were excluded from the analysis. The emergency consultations were assessed for date of consultation, reason for consultation and grouped according to the diagnosis given by two independent examiners. A third examiner was consulted in cases of uncertainty (fig. 1).
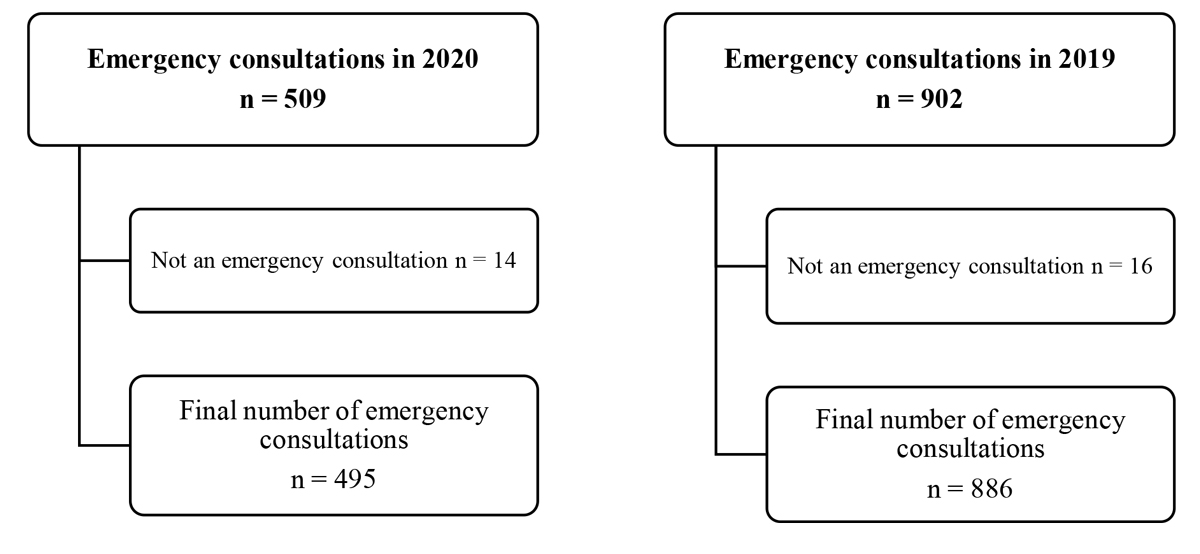
Figure 1 The total number of emergency consultations between 16 March and 26 April, in 2020 and 2019 are shown. Patients were excluded if they had a follow-up visit wrongly labelled as an emergency consultation.
The medical records of the chronic rhinosinusitis patients and patients with a benign or malignant tumours were assessed for date of the cancelled consultation, date of the rescheduled consultation, reason for rescheduling, diagnosis recorded and disease progression by two independent examiners (fig. 2). The study was approved by the Swiss Ethics Committee (ID: KEK 2020-00756). It was conducted in compliance with requirements of the independent ethics commission, the current Helsinki Declaration and Swiss law. All included patients signed the General Consent of the University Hospital Zurich. Patients without a General Consent of the University Hospital Zurich were excluded from the study.
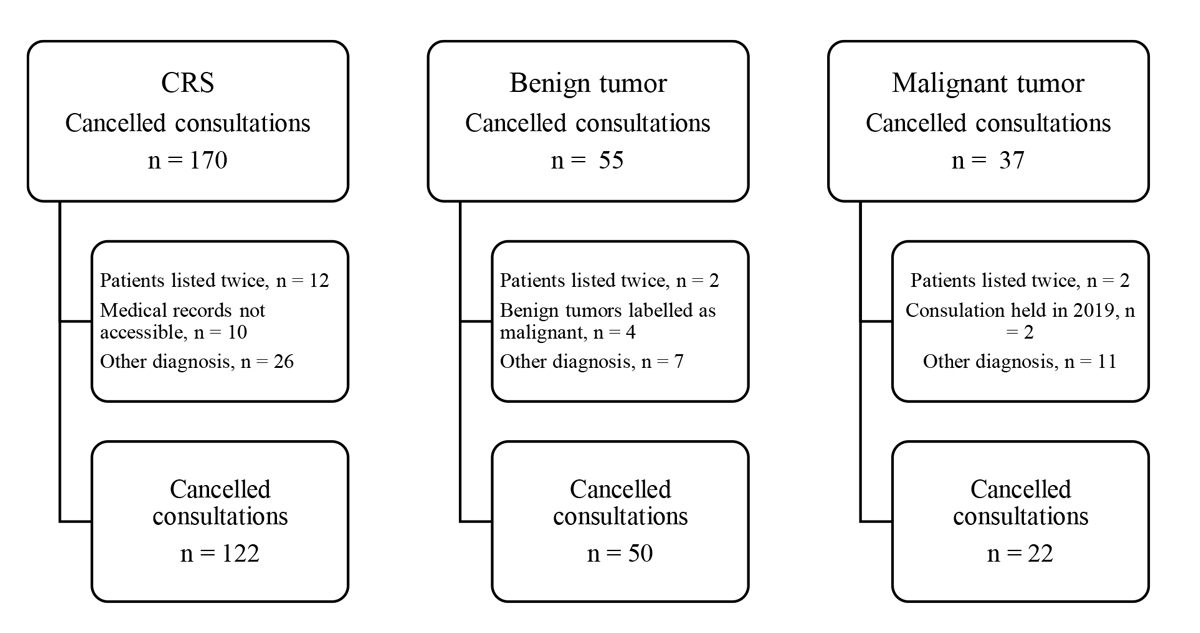
Figure 2 The total number of cancelled consultations between 16 March and 26 April 2020 are shown. Patients were excluded because of duplicate entries, incorrect medical documentation or other diagnosis. CRS = chronic rhinosinusitis.
The effect of postponing appointments on disease progression was examined using the medical records of patients whose consultations were cancelled because of lockdown restrictions. Therefore, the medical history of 122 patients with CRS (chronic rhinosinusitis without nasal polyps and chronic rhinosinusitis with nasal polyps) were studied and all cancelled consultations and their effect on progression of disease were recorded. Disease progression was defined as (1) premature contact by the patient due to an increased level of suffering or additional appointment after the end of lockdown, (2) acute on chronic rhinosinusitis and (3) indication for surgical therapy, systemic steroids or biologicals due to lack of disease control. In chronic rhinosinusitis patients with nasal polyps, an increase of the nasal polyp score (NPS) compared with the last recorded score in the prepandemic era was defined as disease progression. To evaluate the patient’s health-related quality of life, the validated SNOT-20 questionnaire was completed by chronic rhinosinusitis patients up to the end of July 2020 [6]. Assessment of disease progression status was not blinded.
Similarly, the medical records of 50 patients suffering from a benign tumour and 22 patients with the diagnosis of a malignant tumour in the head and neck region, including head and neck carcinoma as well as skin malignancies of the head and neck, were analysed. We recorded whether the cancelled consultations had been rescheduled and whether disease progression was observed. Disease progression was defined as (1) clinical or radiological evidence of an increase in tumour size or (2) recurrence of the tumour. A second follow-up appointment at the clinic, which was scheduled without any lockdown restrictions, was analysed accordingly. Assessment of disease progression status was not blinded.
In order to compare the impact of delaying an appointment owing to lockdown restrictions with regularly scheduled follow-up examinations, all recorded patients with the diagnosis of malignant tumour from 2020 were matched with patients seen at the clinic during the same period of time in 2019. Patients were matched according to the location of the tumour, and the age and gender of the patient. The clinical information system (KISIM) was analysed during the same period of time in 2019 – to reduce seasonal fluctuations – for patients with tumours of the same location, and the same age and gender. Owing to documentations of follow-up visits, it was possible to analyse disease progression, defined as above.
Summing up, primary outcomes were defined as differences in the number of emergency consultations in 2020 versus 2019 and disease progression due to rescheduled consultations in chronic rhinosinusitis patients and patients with benign or malignant tumours. The reasons for emergency consultations for both years, as well as causes of disease progression in chronic rhinosinusitis patients or patients with benign or malignant tumours were analysed as secondary outcomes.
Data are presented as numbers and percentages. The Fisher’s exact test with 2 x 2 contingency tables was used to compare the absolute number of emergency consultations for each clinical presentation between both years, as well as to compare the frequency of disease progression in patients with the diagnosis of a malignant tumour during lockdown with the same period in 2019. In this exploratory analysis, no correction for multiple testing was done. A two-sided p-value of <0.05 was considered significant. The odds ratio (OR) and 95% confidence interval (CI) were calculated for each comparison. Statistical analysis was performed using SPSS software version 26.0 (IBM, Armonk, NY, USA).
Source entry data, study protocol and statistical analysis plan are available on request.
In this monocentric, retrospective study in a tertiary referral centre, a total of 495 emergency consultations were recorded during the lockdown (between 16 March and 26 April) in spring 2020; in comparison, there were 886 emergency consultations during the same period in 2019. This translated into a 44.1% decrease of emergency consultations (a primary outcome; fig. 3). The reasons for the emergency consultations for both years are shown in table 1. The largest decrease in consultation numbers were for otitis media and Eustachian tube dysfunction. Seventeen patients sought emergency assistance for otitis media in 2020, compared with 83 in 2019 (p <0.001, OR 2.906, 95% CI 1.704–4.957). Only 3 patients with Eustachian tube dysfunction were seen in 2020 versus 23 in 2019 (p = 0.007, OR 4.371, 95% CI 1.306–14.631). Furthermore, 29 patients with tonsillitis visited the clinic in 2020 and 80 patients in 2019 (p = 0.038, OR 1.595, 95% CI 1.027–2.476). However, no major increase in visit frequencies due to abscesses could be observed: 28 in 2020 versus 47 in 2019, p = 0.805, OR 0.934, 95% CI 0.577–1.512. Eighty patients presented with epistaxis in 2020, compared with 104 in 2019, p = 0.026, OR 0.690, 95% CI 0.504–0.945.
Figure 3 The number of emergency consultations for each subtype presented as absolute numbers (sorted by organ). * p<0.05, ** p<0.01.
Table 1The number of emergency consultations for each subtype presented as absolute numbers and percentages of the total number of consultations in 2020 and 2019 (sorted by organ).
| Reason for consultation | 2020 (n = 495) | 2019 (n = 886) | p-value | OR | 95% CI |
| Epistaxis* | 80 (16.2%) | 104 (11.7%) | 0.026 | 0.690 | 0.504–0.945 |
| Chronic rhinosinusitis | 5 (1.0%) | 14 (1.6%) | 0.475 | 1.573 | 0.563–4.394 |
| Acute rhinosinusitis | 14 (2.8%) | 27 (3.0%) | 0.870 | 1.080 | 0.561–2.079 |
| Other rhinologic emergencies | 15 (3.0%) | 13 (1.5%) | 0.071 | 0.477 | 0.225–1.010 |
| Acute otitis media** | 17 (3.4%) | 83 (9.4%) | <0.001 | 2.906 | 1.704–4.957 |
| Eustachian tube dysfunction** | 3 (0.6%) | 23 (2.6%) | 0.007 | 4.371 | 1.306–14.631 |
| Otitis externa | 32 (6.5%) | 37 (4.2%) | 0.071 | 0.631 | 0.388–1.026 |
| Tinnitus | 16 (3.2%) | 25 (2.8%) | 0.741 | 0.869 | 0.460–1.644 |
| Cerumen | 18 (3.6%) | 29 (3.3%) | 0.758 | 0.897 | 0.493–1.632 |
| Vertigo | 23 (4.6%) | 41 (4.6%) | >0.999 | 0.996 | 0.590–1.680 |
| Acute hearing loss | 12 (2.4%) | 22 (2.5%) | >0.999 | 1.025 | 0.503–2.089 |
| Other otologic emergencies | 39 (7.9%) | 68 (7.7%) | 0.917 | 0.972 | 0.645–1.465 |
| Chronic dys-/odynophagia of different causes* | 8 (1.6%) | 4 (0.5%) | 0.034 | 0.276 | 0.083–0.921 |
| Acute tonsillitis* | 29 (5.9%) | 80 (9.0%) | 0.038 | 1.595 | 1.027–2.476 |
| Salivary gland problems (inflammatory, obstructive)* | 11 (2.2%) | 7 (0.8%) | 0.044 | 0.350 | 0.135–0.910 |
| Cervical lymphadenopathy | 3 (0.6%) | 17 (1.9%) | 0.060 | 3.208 | 0.936–11.002 |
| Tracheostomy cannula management | 14 (2.8%) | 12 (1.4%) | 0.063 | 0.472 | 0.216–1.028 |
| Temporomandibular joint dysfunction | 10 (2.0%) | 9 (1.0%) | 0.149 | 0.498 | 0.201–1.233 |
| Post-operative haemorrhage | 8 (1.6%) | 6 (0.7%) | 0.158 | 0.415 | 0.143–1.203 |
| Carcinoma | 13 (2.6%) | 15 (1.7%) | 0.239 | 0.639 | 0.301–1.353 |
| Viral respiratory infections | 24 (4.8%) | 56 (6.3%) | 0.282 | 1.324 | 0.810–2.164 |
| Trauma | 22 (4.4%) | 50 (5.6%) | 0.378 | 1.286 | 0.769–2.150 |
| Soft tissue abscesses | 28 (5.7%) | 47 (5.3%) | 0.805 | 0.934 | 0.577–1.512 |
| Foreign body / globus sensation | 7 (1.4%) | 14 (1.6%) | >0.999 | 1.119 | 0.449–2.792 |
| Other head and neck emergencies | 29 (5.9%) | 45 (5.1%) | 0.536 | 0.860 | 0.532–1.390 |
| Phoniatric emergencies | 10 (2.0%) | 16 (1.8%) | 0.837 | 0.892 | 0.402–1.981 |
| Other | 5 (1.0%) | 22 (2.5%) | 0.068 | 2.495 | 0.939–6.631 |
OR: Odds ratio; 95% CI: 95% confidence interval
* p<0.05, ** p<0.01.
Overall, 122 appointments of patients with chronic rhinosinusitis (CRS) were cancelled due to lockdown restrictions in 2020. Of these, 27/122 (22.1%) appointments would have been first consultations at our department after referral from family doctors or private practice ENT specialists. In 36/122 (29.5%) of the cancelled appointments, the cancellation was initiated by the patient. Among all 122 appointments, 102/122 (83.6%) visits were rescheduled after the lockdown. Of the 102 postponed consultations, 90/102 (88.2%) took place within 68 days (standard deviation [SD] 50) after restrictions, and 12/102 (11.8%) patients did not attend the rescheduled appointment. Among all 90 postponed CRS appointments, progression of disease, as defined above, was seen in 40/90 (44.4%) patients. In 5/90 cases (5.6%), patients contacted the clinic earlier, since they experienced an increased level of suffering. In one of these five patients surgery was recommended. One patient (1.1%) presented with an orbital complication of CRS and needed systemic steroids. The patient showed signs of a mucocele originating from the right frontal sinus with compression of the right ocular bulb and was subsequently recommended to undergo surgery. With regard to surgery, an elective surgical procedures was postponed in 3/90 (3.3%) patients. The indication for surgery was established in 12/90 cases (13.3%). Four (4.4%) patients received systemic steroids and one patient (1.1%) biological drugs. Two (2.2%) patients received both pharmaceuticals. Forty-seven of the CRS patients had nasal polyps. In 7/47 cases (14.9%) a higher NPS was seen at the rescheduled appointment. An increased score and a recommendation for a surgical approach was observed in 2/47 cases (4.3%). Two patients (4.3%) presented with an increased score and need for systemic steroids and one patient (2.1%) with a higher NPS and need for biological drugs. In 23/47 cases (48.9%) the NPS remained the same and in 12 (25.5%) patients the score improved.
Fifty-four patients were followed-up for a second time at the clinic. The scheduling of this follow-up was not influenced by lockdown restrictions. Of these 54 patients, 12 (22.2%) presented with disease progression. For five (9.3%) patients surgery was recommended, and three (5.6%) patients received systemic steroids. One (1.9%) patient received both therapies. Twenty-seven of the 54 patients had nasal polyps and in 3/27 cases (11.1%) an increased NPS was observed. The SNOT-20 Questionnaire [6] was sent to all 122 chronic rhinosinusitis patients and 31/122 (25.4%) patients returned the completed form. Of these 31 patients, 4/31 (12.9%) reported no to mild problems, 21/31 (67.7%) moderate problems and 6/31 (19.4%) moderate to severe problems. For none of these patients a SNOT-20 score before the pandemic was available.
Fifty appointments of patients with benign tumours of the head and neck region were cancelled because of the lockdown in spring 2020. The characteristics of these benign tumours can be seen in table 2. Of these, 14/50 (28.0%) patients had requested the cancellation of the consultation themselves. Three (6.0%) patients would have been seen at the clinic for the first time. Of all 50 appointments, 44/50 (88.0%) were rescheduled, 2/50 (4.0%) patients did not require a new appointment, 2/50 (4.0%) appointment proposals were not responded to and 2/50 (4.0%) patients consulted the clinic for a different health issue. Of the 44 rescheduled visits, 37/44 (84.1%) took place with an average delay of 56 days (SD 70.0). Two patients were seen in an emergency consultation before their rescheduled appointment. Seven (15.9%) patients did not attend the rescheduled appointment. In 32/37 (86.5%) postponed visits, no disease progression was seen. In contrast, 5/37 (13.5%) patients showed signs of disease progression (a primary outcome): in 4/37 (10.8%) patients indication for surgery was established and 1/37 patient (2.7%) required a more extensive procedure as a result of postponement of the surgery during the lockdown. However, conversion into a malignant tumour was not found in any of these patients. Fourteen patients had a second follow-up appointment at the clinic, which was not delayed by lockdown restrictions. Of these, only 1 (7.1%) patient was bothered subjectively by the benign tumour and requested surgery.
Table 2The 50 patients with the diagnosis of a benign tumour affected by the lockdown in 2020 are shown. The site of the benign tumour, the number of tumour recurrences and the range in years of the initial diagnosis are summarised (sorted by the number of patients suffering from the tumour).
| Site of the benign tumour | Sinonasal (n = 15) | Thyroid (n = 15) | Pharynx and larynx (n = 7) | Other (n = 7) | Salivary gland (n = 6) |
| Tumour recurrence (n) | 1 | ||||
| Year of initial diagnosis (earliest to latest year) | 2014–2020 | 2015–2020 | 2018–2020 | 2008–2020 | 2018–2020 |
The appointments of 22 patients with the diagnosis of a malignant tumour in the head and neck region were cancelled because of the lockdown restrictions. The characteristics of these malignant tumours can be seen in table 3. Of these, 10/22 (45.5%) patients had requested the cancellation of the consultation themselves. Of these 22 appointments, 20/22 (90.9%) were follow-up visits and 2/22 (9.1%) patients were scheduled to be seen at the clinic for the first time. One of the patients seen for the first time experienced a delay of 15 days due the restrictions. The other patient cancelled the rescheduled appointment himself, resulting in a delay of 49 days.
Of the 22 consultations, 17 (77.3%) appointments were rescheduled. Two (9.1%) patients were followed-up at another department and 3/22 (13.6%) patients did not want to reschedule the visit. Of the 17 rescheduled consultations, 16/17 (94.1%) visits took place with an average delay of 45 days (SD 31.3). One (5.9%) patient did not attend the rescheduled consultation. For the primary outcomes, no disease progression was seen in 13 (81.3%) of the 16 patients, but 3 (18.8%) patients displayed disease progression. One (6.3%) patient required a systemic therapeutic approach and one (6.3%) patient received palliative care. The third (6.3%) patient complained of cervical lymphadenopathy, suspected to be cervical lymph node metastases, but refused physical examination and diagnostics. Since no further information regarding this case could be found, it was labelled as disease progression.
A second follow-up visit, not delayed by lockdown restrictions, was arranged for nine patients and none of them showed signs of tumour progression. For the comparison group, two patients seen in 2020 could not be matched. Patients with a potentially metastasised paraganglioma and a mammary carcinoma that was discovered due to metastasis in the pterygopalatine and the infratemporal fossa could not be matched. Of the 20 patients seen in 2019, 19 (95.0%) were follow-up visits and 1 (5.0%) appointment was an initial consultation. Three (18.8% in 2020 vs 15.0% in 2019, p >0.99, OR = 0.765, CI = 0.132–4.426) patients presented with disease progression, that is to say 3 (15.0%) indications for an operation were established. Compared with 2020 this difference did not proof to be statistically significant.
Table 3The 22 patients with the diagnosis of a malignant tumour affected by the lockdown in 2020. The site of the malignant tumour, the range of the T stage, the number of tumour recurrences and the range in years of the initial diagnosis are summarised (sorted by the number of patients suffering from the tumour).
| Site of the malignant tumour | Head and neck skin cancer (non-melanoma) (n = 13) | Sinonasal (n = 3) | Pharynx and Larynx (n = 3) | Other (n = 3) |
| Range of T stage (lowest to highest T stage) | T1–T4 | T2 | T2–T3 | T3 |
| Tumour recurrence (n) | 6 | 1 | ||
| Year of initial diagnosis (earliest to latest year) | 2010–2019 | 2018–2020 | 2013–2019 | 2014–2020 |
In this retrospective study on consecutive ENT consultations we found a marked decrease in both, elective and emergency appointments, when comparing the lockdown period to the prepandemic era. Interestingly, no increase in complications (for instance peritonsillar abscess) was observed. Although almost 50% of all patients with chronic rhinosinusitis showed a progression of disease during the lockdown period, no negative impact on patients with malignant head and neck tumours was seen.
Our analysis revealed an extensive reduction (44.1%) in emergency patients during the lockdown in 2020, when compared with the same period in 2019. This finding is in line with previous studies [3–5, 7] . Elli et al. reported that the highest reduction of ENT emergencies was due to fewer traumatic injuries (e.g., nose fractures) and attributed this finding to the lockdown restrictions (ban of team sports, restrictions on personal transportation). A reduction in the consultations due to trauma was also observed in this study. However, most likely due to the small sample size, no significance was found.
The largest decrease was observed in consultations for acute otitis media and Eustachian tube dysfunction. Possible explanations for this finding are patient- and lockdown-related. Firstly, patients might have waited longer before consulting a doctor, due to fear of contact with healthcare providers. Secondly, since acute otitis media is often self-limiting, symptom reduction might have been achieved through at-home treatment measures and spontaneous healing [8]. Thirdly, the hygienic precautions implemented by the government to reduce the spread of SARS-CoV-2 could have decreased the incidence of viral and bacterial infections and therefore the number of middle ear infections. Fourthly, the remarkable reduction of air travel during this period could have contributed to the lower occurrence of Eustachian tube dysfunction [9]. Interestingly, in contrast, the frequency of otitis externa was higher in 2020 than in 2019, which strengthens the theory, as it is not a self-limiting disorder [10].
In spring 2020, fewer patients with acute tonsillitis sought assistance at our ENT emergency department, when compared with 2019. However, the number of patients with peritonsillar abscess was not different compared with the prepandemic era. On the one hand, this finding seems to support the theory that acute tonsillitis is often a self-limiting disease and antibiotic treatment might not reduce the number of cases of quinsy [11, 12]. In times of increasing bacterial resistance due to frivolous antibiotic prescription, restrictive usage is an important aspect for future patient care [13]. On the other hand, the pathophysiology of peritonsillar abscess as a result of acute tonsillitis must be reconsidered, as it is not always a complication of acute tonsillitis [14].
Since the population at risk for all emergency visits was the same in both years, the absolute number of patients with epistaxis was reduced in 2020. Reasons for this might have been less exposure to risk factors such as traumatic injury, lockdown restrictions and reduced infections due to hygienic precautions [15]. Furthermore, the introduction of facemasks into everyday life leading to more moistening of the mucosa might have aided in reducing these cases.
More patients with chronic dysphagia or odynophagia of different causes were seen at the clinic in 2020. In the beginning of the lockdown in Switzerland, information about the symptoms of COVID-19 were partly inconsistent. In fear of having contracted the disease, a patient with dysphagia might have been less reluctant to visit an emergency department than patients with symptoms not associated with COVID-19.
During the lockdown, disease progression was seen in almost 50% of chronic rhinosinusitis patients, whereas the analysis of a second follow-up appointment at the clinic, which was not affected by the lockdown restrictions, showed disease progression in only 22.2% of patients. As previous data showed a postoperative polyp recurrence rate of up to 40% within 18 months after functional endoscopic sinus surgery, revision surgery is indicated in about 10% to 20% of all chronic rhinosinusitis patients with nasal polyps within 5 years [16–18]. These findings underline the concept of chronic rhinosinusitis with nasal polyps as a chronic disease. However, regular follow-up appointments might lead to earlier intervention and therefore could reduce the period of suffering in patients with chronic rhinosinusitis.
Overall, 13.5% of all patients with benign tumors in the head and neck region showed disease progression. To reduce the risk of COVID-19 infection, the focus in the management of patients with a benign tumours shifted towards evaluation of patients at risk for significant negative outcomes and recommendations were made to postpone appointments [19]. In this analysis, no conversion into a malignant tumour was observed, implying there was no effect of the delay on the nature of the tumour. On the other hand, nearly one fifth of patients with the diagnosis of a malignant head and neck tumour presented with disease progression during the lockdown period. This progression included an alteration of the therapeutic approach. However, the comparison with the pre-pandemic era (2019) might imply that such disease progressions are inevitable. In 2019, an alteration of the therapeutic approach was also required. In line with this hypothesis, Agrawal et al. previously postulated that survival in patients with head and neck cancer recurrence might relate more to the disease itself than to follow-up surveillance [20]. Similarly, adaption of the therapy of a malignant tumour might be more dependent on the disease itself than on a delayed consultation. Although we could not see a difference in the percentage of tumour patients with disease progression, it does not mean that a delay in therapy could not have happened. Patients who were not referred to our clinic at all were not captured in this study and were also prone to present with higher stage tumours later in the year. Further studies are needed to better understand the impact of the pandemic on cancer care and long-term outcomes of head and neck cancer patients.
The present findings of this analysis should be interpreted within the context of its strengths and limitations. It was an attempt to describe the reduction of otorhinolarnygological consultations due to the COVID-19 lockdown and its impact on disease progression. It was – to the best of our knowledge – the first analysis in this respect in Switzerland. However, to substantiate our findings, larger studies comparing the lockdown period to the prepandemic era in a larger scope are recommended. What remains to be further elaborated is, whether patients with undiagnosed benign and malignant tumours waited longer until seeing a doctor, resulting in advanced tumour stages at the point of initial diagnosis.
Overall, the COVID-19 lockdown led to a marked decrease in ENT emergency consultations. Among others, fewer visits due to acute otitis media and acute tonsillitis were observed. Interestingly, no increase in complications (e.g., peritonsillar abscess) was noted, indicating a different pathophysiological mechanism in some patients. Almost 50% of chronic rhinosinusitis patients showed disease progression, leading to prolonged suffering due to the rescheduling of appointments. The treatment of patients with the diagnosis of a malignant tumour was not affected by the postponement of consultations.
The authors thank Claudia Bierhoff for all her help with data collection.
All authors have completed and submitted the International Committee of Medical Journal Editors form for disclosure of potential conflicts of interest. No potential conflict of interest was disclosed.
This study was not funded.
1. Dong E , Du H , Gardner L . An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020 May;20(5):533–4. https://doi.org/10.1016/S1473-3099(20)30120-1
2. Bundesamt für Gesundheit (BAG) . Verordnung 2 über Massnahmen zur Bekämpfung des Coronavirus (COVID-19) (COVID-19-Verordnung 2). 2020;https://www.bag.admin.ch/bag/de/home/das-bag/aktuell/medienmitteilungen.msg-id-78454.html. Accessed January 18, 2021.
3. Boserup B , McKenney M , Elkbuli A . The impact of the COVID-19 pandemic on emergency department visits and patient safety in the United States. Am J Emerg Med. 2020 Sep;38(9):1732–6. https://doi.org/10.1016/j.ajem.2020.06.007
4. Herranz-Larrañeta J , Klein-Rodríguez A , Menéndez-Riera M , Mejuto-Torreiro L , López-Eiroa A , Vázquez-Barro JC , et al. ENT emergencies during the first wave of COVID-19 pandemic in Spain: our experience. Am J Otolaryngol. 2021 Mar-Apr;42(2):102865. https://doi.org/10.1016/j.amjoto.2020.102865
5. Gelardi M , Iannuzzi L , Trecca EM , Kim B , Quaranta NA , Cassano M . COVID-19: what happened to all of the otolaryngology emergencies? Eur Arch Otorhinolaryngol. 2020 Nov;277(11):3231–2. https://doi.org/10.1007/s00405-020-06046-z
6. Piccirillo JF , Merritt MG Jr , Richards ML . Psychometric and clinimetric validity of the 20-Item Sino-Nasal Outcome Test (SNOT-20). Otolaryngol Head Neck Surg. 2002 Jan;126(1):41–7. https://doi.org/10.1067/mhn.2002.121022
7. Elli F , Turri-Zanoni M , Arosio AD , Karligkiotis A , Battaglia P , Castelnuovo P . Changes in the use of Otorhinolaryngology Emergency Department during the COVID-19 pandemic: report from Lombardy, Italy. Eur Arch Otorhinolaryngol. 2020 Dec;277(12):3525–8. https://doi.org/10.1007/s00405-020-06119-z
8. Rosenfeld RM , Kay D . Natural history of untreated otitis media. Laryngoscope. 2003 Oct;113(10):1645–57. https://doi.org/10.1097/00005537-200310000-00004
9. Bundesamt für Statistik . Sektion Mobilität. Linien- und Charterverkehr. 2020; https://www.bfs.admin.ch/bfs/de/home/statistiken/mobilitaet-verkehr/querschnittsthemen/zivilluftfahrt/linien-charterverkehr.html. Accessed March, 8, 2021.
10. Rosenfeld RM , Schwartz SR , Cannon CR , Roland PS , Simon GR , Kumar KA , et al. Clinical practice guideline: acute otitis externa. Otolaryngol Head Neck Surg. 2014 Feb;150(1 Suppl):S1–24. https://doi.org/10.1177/0194599813514365
11. Spinks A , Glasziou PP , Del Mar CB . Antibiotics for sore throat. Cochrane Database Syst Rev. 2013 Nov;(11):CD000023.
12. Pelucchi C , Grigoryan L , Galeone C , Esposito S , Huovinen P , Little P , et al.; ESCMID Sore Throat Guideline Group . Guideline for the management of acute sore throat. Clin Microbiol Infect. 2012 Apr;18 Suppl 1:1–28. https://doi.org/10.1111/j.1469-0691.2012.03766.x
13. Costelloe C , Metcalfe C , Lovering A , Mant D , Hay AD . Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: systematic review and meta-analysis. BMJ. 2010 May;340(may18 2):c2096. https://doi.org/10.1136/bmj.c2096
14. Sanmark E , Wikstén J , Välimaa H , Aaltonen LM , Ilmarinen T , Blomgren K . Peritonsillar abscess may not always be a complication of acute tonsillitis: A prospective cohort study. PLoS One. 2020 Apr;15(4):e0228122. https://doi.org/10.1371/journal.pone.0228122
15. Kunz SM , Holzmann D , Soyka MB . Association of epistaxis with atherosclerotic cardiovascular disease. Laryngoscope. 2019 Apr;129(4):783–7. https://doi.org/10.1002/lary.27604
16. DeConde AS , Mace JC , Levy JM , Rudmik L , Alt JA , Smith TL . Prevalence of polyp recurrence after endoscopic sinus surgery for chronic rhinosinusitis with nasal polyposis. Laryngoscope. 2017 Mar;127(3):550–5. https://doi.org/10.1002/lary.26391
17. Koskinen A , Salo R , Huhtala H , Myller J , Rautiainen M , Kääriäinen J , et al. Factors affecting revision rate of chronic rhinosinusitis. Laryngoscope Investig Otolaryngol. 2016 Jul;1(4):96–105. https://doi.org/10.1002/lio2.27
18. Hopkins C , Slack R , Lund V , Brown P , Copley L , Browne J . Long-term outcomes from the English national comparative audit of surgery for nasal polyposis and chronic rhinosinusitis. Laryngoscope. 2009 Dec;119(12):2459–65. https://doi.org/10.1002/lary.20653
19. Givi B , Schiff BA , Chinn SB , Clayburgh D , Iyer NG , Jalisi S , et al. Safety Recommendations for Evaluation and Surgery of the Head and Neck During the COVID-19 Pandemic. JAMA Otolaryngol Head Neck Surg. 2020 Jun;146(6):579–84. https://doi.org/10.1001/jamaoto.2020.0780
20. Agrawal A , Hammond TH , Young GS , Avon AL , Ozer E , Schuller DE . Factors affecting long-term survival in patients with recurrent head and neck cancer may help define the role of post-treatment surveillance. Laryngoscope. 2009 Nov;119(11):2135–40. https://doi.org/10.1002/lary.20527