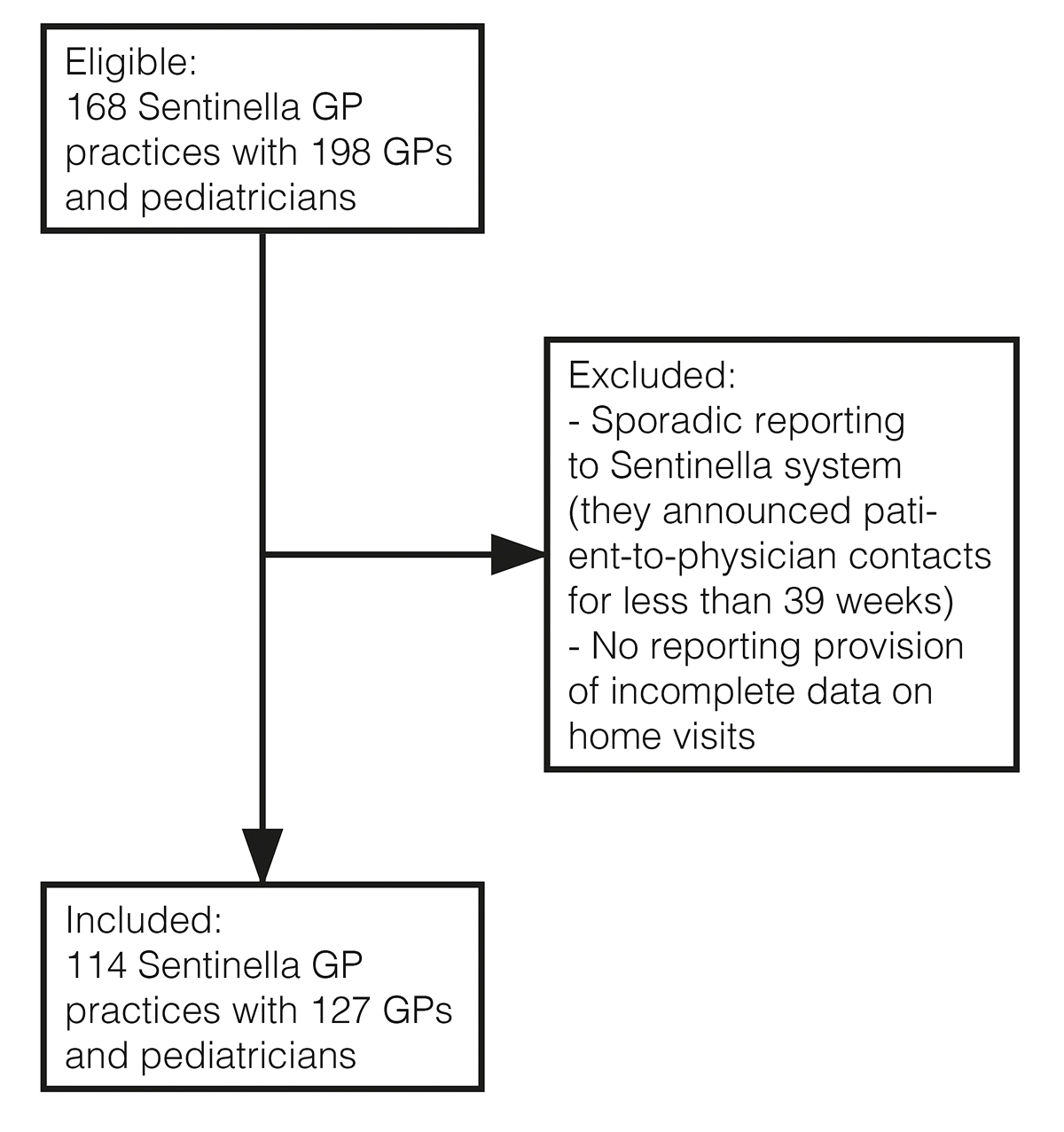
Figure 1 Flow chart of GPs invited to participate.
DOI: https://doi.org/10.4414/SMW.2021.w30062
Home visits are an important part of primary care, which are traditionally provided by general practitioners (GPs). In Switzerland, a home visit is characterised as a GP’s visit to patient’s home in order to examine, diagnose and treat the patient. Home visits are typically performed during office hours, and infrequently out of hours, for instance, in the context of medical emergencies [1]. Especially elderly, multimorbid patients with reduced mobility receive visits [14]. As this part of the population is growing, the workload due to home visits is likely to increase [5]. However, there is an increasing shortage of GPs and the number of home visits is declining in many western countries [2,6]. This has also been observed in Switzerland, where the number of home visits decreased by about 40% between 2006 and 2015 [1]. In some countries, GPs are now being supported by nurse practitioners. These nurses with an extended training can take over some of the home visits [7]. In Switzerland, this possibility is only being tested in pilot studies [8].
Home visits need planning and decision making. They can be performed on a routine basis or requested by the patient at short notice if needed. When considering a visit, the practice team must decide whether a home visit is necessary or if another patient pathway is preferable, such as contacting the hospital emergency department [4]. Another study in primary care showed that the reception of the request is especially crucial for correct triage [9]. As another part of the pre-visit triage, it must be decided whether the patient’s complaint leading to the request for a home visit fits the scope of practice of a nurse practitioner or if a GP is required [10]. Our assumption is that the suspected health problem (based on pre-visit assessment) is important to take these decisions. The accuracy of the pre-visit assessment would then affect the quality of care. If the home visit is performed, it uncovers the actual health problem (based on a post-visit assessment).
There are some studies on the accuracy of assessments, but they were performed in a different setting as they determined the accuracy of pre-hospital diagnoses in the emergency setting [11, 13]. Depending on the study, accuracy varied between 50 and 90%, making it an issue for further evaluations. Patients with comorbidities and at high age were red flags for inaccuracy [12, 13]. To our knowledge, our study is the first to address this topic in the setting of home visits.
We aimed to evaluate the agreement between suspected and actual health problems from pre-visit and post-visit assessments, respectively, when conducting home visits and to determine red flags for disagreement.
Data were collected as part of the Swiss Sentinel Surveillance System (Sentinella) [14]. Sentinella is a nationwide system to collect surveillance data in primary health care. The Swiss Federal Office of Public Health (FOPH) runs the administrative part of the system and ensures that GPs are included as representatives of all GPs working in Switzerland [15]. Overall, 127 GPs and paediatricians practising in 114 different GP practices participate throughout the country (fig. 1). This corresponds to 64% of all registered Sentinella doctors and 68% of all registered Sentinella GP practices. Their participation is voluntary and includes a small annual reimbursement for collecting the data. The current study (Req-2020-01088) was approved by the ethics committees of Bern (KEK) and central and northwestern Switzerland (EKNZ). Patient consent was not required as all data were collected anonymously.
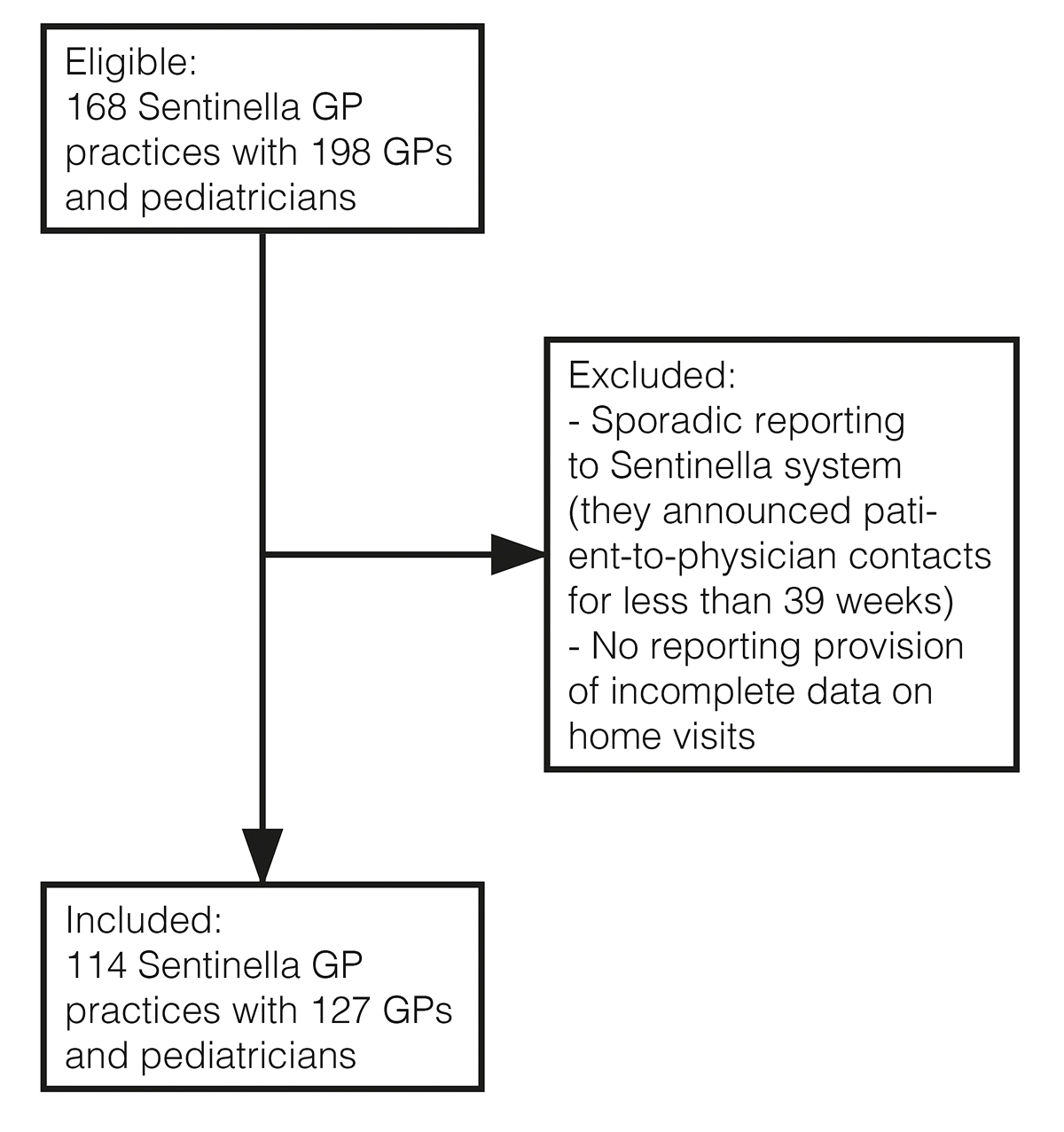
Figure 1 Flow chart of GPs invited to participate.
A digital questionnaire in French or German was filled in by participating Sentinella physicians (see separate appendix file available for download). Data collection took place between January and December 2019. Up to 20 consecutive home visits had to be documented by each physician. The limit of 20 was a trade-off between generating enough data and restricting individual GPs’ workload and influence. To avoid seasonal bias, the physicians were randomly assigned a date throughout the year on which data collection had to be started.
Physicians were asked to document suspected and actual health problems, based on pre-visit and post-visit assessments, respectively, for each visit. The suspected health problem was defined as the description of the health problem as it was relayed to the physician before the visit. Typically, the patient or a caregiver informed either the GP or the practice assistant about the problem by telephone. If the practice assistant was informed, he or she informed the GP. The actual health problem was defined as the result of the GP’s home visit, based on history, clinical examination and on-site applicable diagnostic methods such as blood pressure or blood glucose measurement.
To code the health problems, we used the main chapter headings of the International Classification of Primary Care (ICPC)-2 [16]. The nine most commonly encountered chapters of health problems in primary care were offered as individual options ("general and unspecified“, "respiratory“, "musculoskeletal“, "neurological“, "digestive“, "circulatory“, "psychological“, "social“ and "endocrine, metabolic or nutritional“) [17, 18]. The remaining chapters were summarised as "other area“. Two options were added ("no actual problem“ and “unclear”). Up to three possible health problems, pre-visit and post-visit, could be documented for each visit.
In addition, the questionnaire contained the patients’ year of birth, gender, number of chronic conditions, place of home visit, the urgency level of the visit, the time of patient contact and information on repeated visits. In order to determine the number of chronic conditions, a list of pre-specified chronic diseases to choose from was handed out with the questionnaire. This list had already been used in prior Sentinella studies on multimorbidity [15] and was initially developed by N’Goran et al. [19]. To describe the place of home visit, we differentiated between a private home and an institution. To describe the urgency level of the home visit, we applied the three urgency levels that are used to get reimbursed for the service ("regular“, "urgent“, "emergency“) [20]. For the variable on the time of patient contact, we distinguished patient contacts during office hours and out-of-hours. Lastly, the visit was classified as a repeat visit to the same patient or a first visit to a patient within the survey period of a total of 20 consecutive home visits per GP.
We excluded routine home visits in nursing homes (ward rounds) and home visits made while on public emergency duty. The latter were excluded because the visited patients were unknown to the GP and thus pre-visit assessments would be very susceptible to error. Visits with missing information on the results of pre- or post-visit assessments were also excluded.
The suspected and actual health problems from pre- and post-visit assessments were analysed for agreement as co-primary outcome measures. Each suspected health problem from pre-visit assessments was classified as confirmed (same health problem from post-visit assessment) or unconfirmed (no such health problem from post-visit assessment). Each actual health problem from post-visit assessments was classified as foreseen (same health problem as the pre-visit assessment) or unforeseen (no such health problem from pre-visit assessment; Figure 2). For example, patient A was suspected to have a respiratory and a psychological health problem before the home visit. During the home visit, the GP detected a respiratory and a digestive health problem. The suspected respiratory health problem was confirmed correctly during the home visit, but the psychological health problem remained unconfirmed. The actual respiratory health problem was correctly foreseen, but the digestive health problem was unforeseen, i.e., only discovered during the home visit.
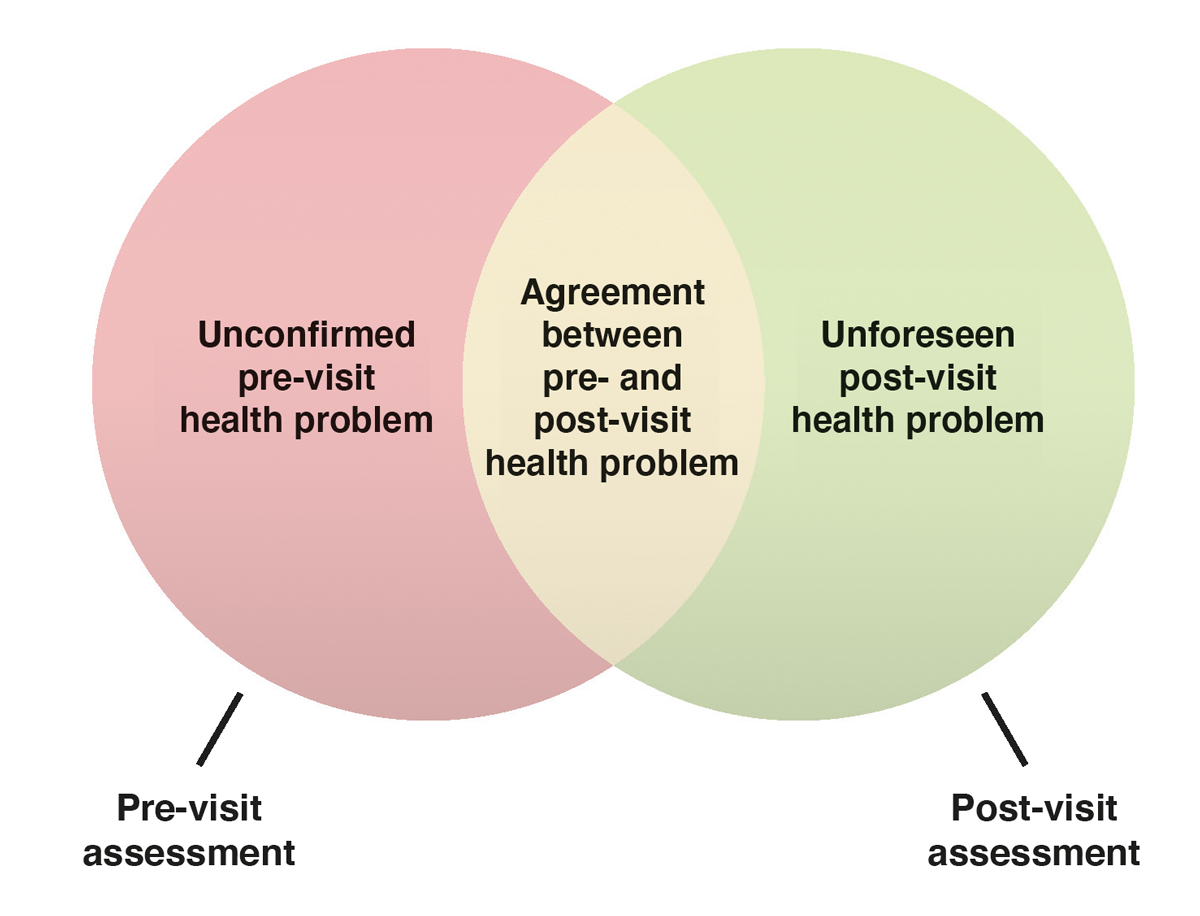
Figure 2 Intersection diagram. Definition of pre-visit and post-visit assessments.
We calculated proportions for each variable to characterise the home visits and health problems. The health problems were broken down into confirmed and unconfirmed suspected health problems from pre-visit assessments, and foreseen and unforeseen actual health problems from post-visit assessments. We used multilevel mixed-effects logistic regressions to determine factors associated with inaccuracy on the level of health problems while accounting for clustering on the GP level. The outcomes were defined as the suspected and actual health problems from pre-visit and post-visit assessment, respectively. In each case, we present both the univariable and multivariable models. All regression models accounted for clustering at the GP level as well as the level of the home visit (since multiple visits per patient were possible). We did a complete case analysis. The independent variables included in the multivariable model were patients’ age, gender, number of chronic conditions, place of home visit, urgency level of the visit, time of patient contact and suspected or actual health problems.
We carried out several sensitivity analyses to test the robustness of our data. First, we restricted the data to include only first home visits. Second, we stratified the analyses according to place of home visit (private home and institution). Third, we redid the analyses on the level of visits instead of health problems. To do so, all health problems (up to three) had to be combined for each visit. To count as accurate, all suspected health problems had to be confirmed and all actual health problems had to be foreseen.
Data analysis was performed with STATA 15.1 (StataCorp, College Station, TX, USA). Statistical significance was determined by using two-sided tests with alpha ≤0.05.
Overall, 114 GP practices participated. A total of 1560 home visits were registered, of which 64 were excluded owing to data that were incomplete or visits that were not made. This led to a sample of 1496 visits that were included in the analysis, with a total of 1789 suspected health problems from pre-visit assessments and 1762 actual health problems from post-visit assessments.
Characteristics of the visits are summarised in table 1. Out of all home visits, 72% were for patients older than 81 years and 65% for female patients. Patients had at least two chronic conditions in 91% of all visits. Two thirds of the home visits were during consultation hours and 70% were classified as non-urgent. Emergency visits accounted for 6%. In both pre-visit and post-visit assessments, musculoskeletal (17%) and circulatory health problems (14%) were the most common chapters.
Table 1Characteristics of the home visits.
| Variables | n (patients) | % | |
| Age (in years) | 0–20 | 15 | 1% |
| 21–40 | 23 | 2% | |
| 41–60 | 73 | 5% | |
| 61–80 | 303 | 20% | |
| ≥81 | 1082 | 72% | |
| Gender | Female | 966 | 65% |
| Male | 530 | 35% | |
| Chronic conditions | 0 | 31 | 2% |
| 1 | 89 | 6% | |
| 2–4 | 784 | 54% | |
| 5–10 | 495 | 34% | |
| >10 | 38 | 3% | |
| Unknown | 17 | 1% | |
| Place of home visit | Private home | 746 | 50% |
| Institution | 743 | 50% | |
| Urgency level | Regular (non-urgent) | 1045 | 70% |
| Urgent | 357 | 24% | |
| Emergency | 87 | 6% | |
| Time of patient contact | During office hours | 906 | 62% |
| Out-of-hours | 567 | 38% | |
| Repeated visit | Yes | 801 | 54% |
| No | 684 | 46% | |
| Variables | n (health problems) | % | |
| Pre-visit assessment | General and unspecified | 174 | 10% |
| Respiratory | 178 | 10% | |
| Musculoskeletal | 312 | 17% | |
| Neurological | 160 | 9% | |
| Digestive | 82 | 5% | |
| Circulatory | 255 | 14% | |
| Psychological | 155 | 9% | |
| Social problems | 47 | 3% | |
| Endocrine, metabolic, nutritional | 45 | 3% | |
| Other diagnostic area | 220 | 12% | |
| No problem | 126 | 7% | |
| Unclear | 35 | 2% | |
| Post-visit assessment | General and unspecified | 151 | 9% |
| Respiratory | 175 | 10% | |
| Musculoskeletal | 305 | 17% | |
| Neurological | 156 | 9% | |
| Digestive | 84 | 5% | |
| Circulatory | 249 | 14% | |
| Psychological | 164 | 9% | |
| Social problems | 44 | 2% | |
| Endocrine, metabolic, nutritional | 50 | 3% | |
| Other diagnostic area | 218 | 12% | |
| No problem | 130 | 7% | |
| Unclear | 36 | 2% | |
Overall, the suspected health problems from pre-visit assessments were confirmed in 85%. Accuracy was highest in respiratory and psychological (90%) and lowest in general and unspecified complaints at 74%. Overall, the actual health problems from post-visit assessments were foreseen in 87% of the cases. The most frequent unforeseen health problems were of endocrine/metabolic and digestive nature, of which 20% were unforeseen. In contrast to this, respiratory and musculoskeletal complaints were unforeseen in only 9% (table S1).
Older age (odds ratio [OR] 1.1 by 10-year increase; 95% confidence interval [95% CI] 1.0–1.3) and an increased urgency level of visits (OR 1.7 compared with regular visits; 95% CI 1.1–2.6) showed a trend for more unforeseen health problems. They should thus be red flags for GPs who have to schedule home visits (table 2). When the different types of health problems were compared, respiratory (OR 0.3; 95% CI 0.20.7), musculoskeletal (OR 0.4; 95% CI 0.-0.7), circulatory (OR 0.5; 95% CI 0.20.9) and psychological (OR 0.3; 95% CI 0.10.7) problems were less likely to be unconfirmed than general/unspecified problems. The results of the univariable model were similar to those of the multivariable model. For both of our outcomes, we found evidence for clustering at the GP level (i.e., confirmed/unconfirmed outcome: intraclass correlation coefficient [ICC] 0.20; foreseen/unforeseen outcome: ICC 0.18).
Table 2Associations of possible red flags with unconfirmed and unforeseen health problems.
| Unconfirmed health problem from pre-visit assessment | Unforeseen health problem from post-visit assessment | |||||||
| Univariable model 1 | Multivariable model 2 | Univariable model 1 | Multivariable model 2 | |||||
| Odds ratio | 95% CI | Odds ratio | 95% CI | Odds ratio | 95% CI | Odds ratio | 95% CI | |
| Age (in ten years steps) | 1.1 | 0.9–1.2 | 1.1 | 0.9–1.2 | 1.1 | 1.0–1.3 | 1.1 | 1.0–1.3 |
| Female (reference: male) | 0.8 | 0.6–1.1 | 0.8 | 0.6–1.1 | 0.8 | 0.6–1.1 | 0.7 | 0.5–1.1 |
| Number of chronic conditions3 | 1.1 | 0.9–1.5 | 1.1 | 0.8–1.4 | 1.1 | 0.8–1.5 | 1.1 | 0.8–1.5 |
| Urgent/emergency level (reference: regular) | 1.2 | 0.9–1.7 | 1.4 | 0.9–2.0 | 1.4 | 1.0–2.1 | 1.7 | 1.1–2.6 |
| Institution (reference: private home) | 0.8 | 0.6–1.2 | 0.8 | 0.5–1.2 | 0.8 | 0.6–1.2 | 0.7 | 0.5–1.2 |
| Out-of-hours (reference: during office hours) | 1.1 | 0.7–1.6 | 0.9 | 0.6–1.4 | 1.2 | 0.8–1.8 | 1.0 | 0.6–1.6 |
| Health problem (reference: general/unspecified) | ||||||||
| Respiratory | 0.4 | 0.2–0.7 | 0.3 | 0.2–0.7 | 0.6 | 0.3–1.4 | 0.6 | 0.2–1.4 |
| Musculoskeletal | 0.4 | 0.2–0.7 | 0.4 | 0.2–0.7 | 0.6 | 0.3–1.2 | 0.6 | 0.3–1.2 |
| Neurological | 0.5 | 0.3–1.1 | 0.5 | 0.2–1.0 | 0.8 | 0.3–1.9 | 0.9 | 0.4–2.2 |
| Digestive | 0.7 | 0.3–1.4 | 0.6 | 0.3–1.4 | 1.5 | 0.6–3.7 | 1.5 | 0.6–4.0 |
| Circulatory | 0.5 | 0.3–0.9 | 0.5 | 0.2–0.9 | 0.8 | 0.4–1.7 | 0.7 | 0.3–1.7 |
| Psychological | 0.3 | 0.2–0.7 | 0.3 | 0.1–0.7 | 1.2 | 0.5–2.6 | 1.4 | 0.6–3.2 |
| Social problems | 0.8 | 0.3–2.1 | 0.8 | 0.3–2.1 | 1.6 | 0.5–5.2 | 1.9 | 0.6–6.5 |
| Endocrine, metabolic, nutritional | 0.3 | 0.1–1.0 | 0.4 | 0.1–1.2 | 1.6 | 0.5–4.6 | 1.7 | 0.6–5.3 |
| Other diagnostic area | 0.6 | 0.3–1.1 | 0.6 | 0.3–1.2 | 1.2 | 0.6–2.6 | 1.4 | 0.6–3.0 |
| No problem | 0.9 | 0.5–1.8 | 0.9 | 0.4–1.9 | 2.7 | 1.2–6.5 | 3.9 | 1.5–9.8 |
| Not clear | 5.1 | 1.4–18.6 | 4.8 | 1.1–20.5 | 20.4 | 4.2–98.8 | 17.2 | 2.9–101.2 |
CI: confidence interval. 1 Adjusted for clustering on the levels of GPs and visits only; 2 adjusted for clustering on the levels of GPs and visits, and each other variable; 3 continuous variable, assuming a linear trend.
In the sensitivity analyses, we found a trend towards statistical significance showing that more chronic conditions were a possible red flag when only first visits were included or when the analysis was redone on the level of visits instead of health problems (tables S2 and S4). The stratified analysis by place of the visit did not result in significant differences when comparing patients in their private homes or in institutions (table S3).
Our study shows that when GPs made a home visit about one out of seven health problems from pre-visit and post-visit assessments were unconfirmed and unforeseen, respectively. This means that GPs arrive on site and are exposed to a problem different from that anticipated. The level of agreement varied depending on patients’ health problems. Increasing age and rising urgency level showed a trend for inaccuracy especially in cases of unforeseen diagnoses.
To our knowledge, our study is the first to address the accuracy of suspected health problems when GPs decide to make a home visit. Some studies on this topic have been done in the setting of emergency medicine and showed surprisingly similar results despite the different setting. Heuer et al. [12] and Ramadanov et al. [11] compared the pre-hospital diagnosis of emergency physicians with the hospital discharge diagnosis. They found a match in 90% and 76%, respectively. Our data show a similar accuracy for pre-visit assessments. Also similarly, Heuer et al. detected a higher failure rate with increasing patient age and comorbidity. Heuer suspected a connection between the difficulty in taking a complete medical history in the elderly and the reduced diagnostic accuracy. Although our setting included GPs who potentially knew the history of their elderly patients already, we were still able to detect the same trends. In contrast, Ramadanov did not detect a correlation between age, gender or medication and the accuracy of the pre-hospital diagnosis [11]. In another study, Eames et al. [13] compared the emergency discharge with the hospital discharge diagnosis. In this study, the physician had more time and diagnostic tools to decide on a diagnosis but the diagnoses matched in only 47%. It remains unclear why more time and equipment did not lead to better accuracy, or how the GPs in our study were affected by little time and no tools in the absence of the patient.
Other hospital studies on accuracy focused on specific subgroups of patient complaints. In the subgroup of neurological complaints, Sporer et al. [21] analysed the accuracy of diagnoses made within 20 minutes when patients presented with an acutely altered mental state. Depending on the aetiology, the accuracy varied greatly between 93% and 0%. In our study, the accuracy of the pre-visit neurological diagnoses was 87%. Al-Huthail et al. [22] explored the accuracy of initial psychiatric diagnoses of primary medical providers and compared them with those of a requested psychiatric specialist in an in-patient setting. The accuracy of psychiatric diagnoses ranged from 60% (cognitive disorders) to 0% (psychosis). In our study, GPs predicted psychiatric complaints with an accuracy rate of 90%. We assume that the rather high accuracy in our study can be explained by the broad ICPC-2 chapters, which are less detailed than the diagnostic groups that were used in the other studies.
In our study, unspecific complaints were reported in about 12% of all diagnoses and showed the highest disagreement rate between pre- and post-visit assessments (27%). This might be unproblematic, as visits potentially clarify the problems. However, the Basel Non-Specific Complaints Study (BANC) showed that patients with unspecific complaints presenting to the emergency department are at high risk of unfavourable outcomes [23]. This indicates that special care should be taken in the triage of patients with unspecific problems, which might be equally true in the setting of home visits.
Many previous studies on diagnostic accuracy cannot be directly compared with our study. In their narrative review on missed diagnoses, Singh et al. [24] named infections, cardiovascular disease and cancer as the most significant categories of harmful diagnostic errors in the ambulatory setting. As most of the data of the reviewed studies were collected from malpractice claims, the reported numbers do not represent the actual frequency of missed diagnoses.
We suppose that a mismatch between pre- and post-visit assessments carries the risk of delayed proper medical care and might lead to poorer patient outcomes. A negative impact on outcomes could result from the GP being less well prepared on arrival or even lacking materials needed to start treatment. According to our literature search, outcomes have never been studied in the setting of home visits, but were analysed in the study of Eames et al. [13] in the emergency setting. They found an increase in patients’ morbidity and mortality rates when the emergency discharge diagnosis was wrong.
Correct patient triage helps to determine who should make the home visit, if home visits could also be carried out by medical professionals other than GPs, such as nurse practitioners. Our study findings suggest that patient complaints, which are to be expected in home visits, potentially fit nurse practitioners’ scope of practice. In a study performed in an out-of-hours primary care setting, GPs were substituted by nurse practitioners who were capable of taking over most patient groups [25]. Only patients younger than 1 year, with psychiatric complaints, abdominal or chest pain, neck ailments, headache or dizziness were excluded from the nurses’ scope of practice owing to their level of training [25]. Van der Biezen et al. found that 77% of patients who consult a doctor outside office hours suffer from health problems that fall within the remit of nurse practitioners. Our ICPC-2 categories indicate that a relevant number of the patients visited by GPs would fall within such a scope of practice of nurse practitioners. As an indication that studies on out-of-hours services and home visits are comparable, Chmiel et al. found that patients asked for home visits in 63% of out-of-hours requests for medical help in Switzerland [26].
Nevertheless, it will be important to avoid deploying nurse practitioners to home visits when the health problems that they encounter could surprise them, i.e., to reduce unforeseen health problems. This is especially important for older and multimorbid patients who show a trend for more unforeseen health problems when GPs conducted the home visits in our study. Nurse practitioners encounter many of those patients [27], who have also been described as the main target group when nurse practitioners start performing home visits in Switzerland [28]. Therefore, the triage process involving nurse practitioners has to be conducted very carefully. The entire practice team, including the practice assistant, must be aware of these vulnerable patient groups and the GPs’ and nurses’ scope of practice.
Sentinella is an established research network including physicians who are experienced in data collection for the purpose of studies. The network accurately represents the geographic distribution of physicians in Switzerland, supporting the generalisability of our results. In addition, we carried out several sensitivity analyses to better understand the influence of important variables. Our study is the first on unconfirmed and unforeseen health problems when making home visits and raises many important questions for future research.
Data were acquired by self-reporting of the physicians. There is a potential for selection as well as recall bias regarding the documentation of the pre- and post-visit assessments, as there might have been a time-gap between the home visit itself and its documentation. Moreover, there is no verification of assessments by another independent physician. In addition, our study did not consider how the suspected health problem from pre-visit assessments was arrived at. This may well be a source of error, since the triage process depends largely on the triage person (GP versus practice assistant) and his or her experience and judgement.
Furthermore, physicians were able to document up to three health problems from pre-visit and post-visit assessments for each visit, but no distinction was made between the different problems, so that the main problem cannot be isolated. Additionally, the health problems were surveyed with the help of the ICPC-2 main chapters, which do not allow any conclusions about the exact diagnosis, neither can we determine the disease severity.
In further studies on home visits, a breakdown by detailed diagnoses should be included. To distinguish secondary from main complaints, a severity rating would be of additional help. More precise data collection would also help to define the future task field of GPs and nurse practitioners.
It remains unclear how the setting, content and speed of the process that leads to a suspected diagnosis affect accuracy for home visits and comparisons with hospital-based accuracy studies. It is also unclear how important pre-visit assessments are for the decision whether, by whom and when a home visit is carried out. Qualitative studies could illuminate those issues.
With quality improvement circles or intervention studies, it might be possible to improve the rate of correct pre-visit assessments. For example, telemedicine might have a positive impact on accuracy. To improve the triage and information flow in the team, it could be worthwhile to develop a checklist for primary care practices. Last, it will be important to measure patient outcomes associated with the accuracy of assessments when conducting home visits, such as morbidity and risk of hospitalisation.
When home visits were conducted, about one out of seven health problems from pre-visit and post-visit assessments were unconfirmed and unforeseen. Particularly when patients were older or visits were urgent, there were higher odds of unconfirmed and unforeseen assessments. These results should be considered when triaging the patients.
The data were collected as part of the Swiss Sentinel Surveillance System and made available to the Centre of Primary and Community Care for scientific publications.
We wish to thank all participating Sentinella physicians for their contribution to this study. We further thank Lars Fischer for his editorial support.
Author contributions
Data acquisition: CM and SE; conceptualisation, analysis and interpretation of data: NM, KTJ, SS and SE; drafting - original preparation NM and SE; drafting - review and editing: NM, KTJ, CM, SS and SE; supervision: SE. All authors approved the final version of the manuscript.
1. Mueller Y , David S , Cohidon C , Locatelli I , Senn N . Home visits made by general practitioners in the canton of Vaud between 2006 and 2015. Swiss Med Wkly. 2019 Mar;149(11-12):w20037. https://doi.org/10.4414/smw.2019.20037
2. van den Berg MJ , Cardol M , Bongers FJ , de Bakker DH . Changing patterns of home visiting in general practice: an analysis of electronic medical records. BMC Fam Pract. 2006 Oct;7(1):58. https://doi.org/10.1186/1471-2296-7-58
3. Kaneko M , Van Boven K , Takayanagi H , Kusaba T , Yamada T , Matsushima M . Multicentre descriptive cross-sectional study of Japanese home visit patients: reasons for encounter, health problems and multimorbidity. Fam Pract. 2020 Mar;37(2):227–33. https://doi.org/10.1093/fampra/cmz056
4. Theile G , Kruschinski C , Buck M , Müller CA , Hummers-Pradier E . Home visits - central to primary care, tradition or an obligation? A qualitative study. BMC Fam Pract. 2011 Apr;12(April):24. https://doi.org/10.1186/1471-2296-12-24
5. Pochert M , Voigt K , Bortz M , Sattler A , Schübel J , Bergmann A . The workload for home visits by German family practitioners: an analysis of regional variation in a cross-sectional study. BMC Fam Pract. 2019 Jan;20(1):3. https://doi.org/10.1186/s12875-018-0891-6
6. Joyce C , Piterman L . Trends in GP home visits. Aust Fam Physician. 2008 Dec;37(12):1039–42. Available from: https://www.racgp.org.au/afpbackissues/2008/200812/200812joyce.pdf
7. Norful AA , de Jacq K , Carlino R , Poghosyan L . Nurse practitioner–physician comanagement: A theoretical model to alleviate primary care strain. Ann Fam Med. 2018 May;16(3):250–6. https://doi.org/10.1370/afm.2230
8. Gysin S , Sottas B , Odermatt M , Essig S . Advanced practice nurses’ and general practitioners’ first experiences with introducing the advanced practice nurse role to Swiss primary care: a qualitative study. BMC Fam Pract. 2019 Nov;20(1):163. https://doi.org/10.1186/s12875-019-1055-z
9. Mellor RM , Sheppard JP , Bates E , Bouliotis G , Jones J , Singh S , et al. Receptionist rECognition and rEferral of Patients with Stroke (RECEPTS): unannounced simulated patient telephone call study in primary care. Br J Gen Pract. 2015 Jul;65(636):e421–7. https://doi.org/10.3399/bjgp15X685621
10. Maier CB , Barnes H , Aiken LH , Busse R . Descriptive, cross-country analysis of the nurse practitioner workforce in six countries: size, growth, physician substitution potential. BMJ Open. 2016 Sep;6(9):e011901. https://doi.org/10.1136/bmjopen-2016-011901
11. Ramadanov N , Klein R , Aguilar Valdez AD , Behringer W . Influence of patient-specific factors on the diagnosis by the prehospital emergency physician. Notf Rettmed. 2020;23(4):282–8. https://doi.org/10.1007/s10049-019-00633-2
12. Heuer JF , Gruschka D , Crozier TA , Bleckmann A , Plock E , Moerer O , et al. Accuracy of prehospital diagnoses by emergency physicians: comparison with discharge diagnosis. Eur J Emerg Med. 2012 Oct;19(5):292–6. https://doi.org/10.1097/MEJ.0b013e32834ce104
13. Eames J , Eisenman A , Schuster RJ . Disagreement between emergency department admission diagnosis and hospital discharge diagnosis: mortality and morbidity. Diagnosis (Berl). 2016 Mar;3(1):23–30. https://doi.org/10.1515/dx-2015-0028
14. Sentinella Meldesystem . http://sentinella.ch/de/info. Accessed December 1, 2020.
15. Excoffier S , Herzig L , N’Goran AA , Déruaz-Luyet A , Haller DM . Prevalence of multimorbidity in general practice: a cross-sectional study within the Swiss Sentinel Surveillance System (Sentinella). BMJ Open. 2018 Mar;8(3):e019616. https://doi.org/10.1136/bmjopen-2017-019616
16. WONCA International Classification Committee . International Classification of Primary Care ICPC-2-R, Revised second edition. Oxford Univ Press 2005.
17. Voigt K , Liebnitzky J , Riemenschneider H , et al. Beratungsanlässe bei allgemeinärztlichen hausbesuchen: erste ergebnisse der SESAM-3-studie. Z Allgemeinmed. 2011;87(2):65–71. https://doi.org/10.3238/zfa.2011.065
18. Tandjung R , Hanhart A , Bärtschi F , Keller R , Steinhauer A , Rosemann T , et al. Referral rates in Swiss primary care with a special emphasis on reasons for encounter. Swiss Med Wkly. 2015 Dec;145:w14244. https://doi.org/10.4414/smw.2015.14244
19. N’Goran AA , Blaser J , Deruaz-Luyet A , Senn N , Frey P , Haller DM , et al. From chronic conditions to relevance in multimorbidity: a four-step study in family medicine. Fam Pract. 2016 Aug;33(4):439–44. https://doi.org/10.1093/fampra/cmw030
20. Tarifsystem TA . https://www.bag.admin.ch/bag/de/home/versicherungen/krankenversicherung/krankenversicherung-leistungen-tarife/Aerztliche-Leistungen-in-der-Krankenversicherung/Tarifsystem-Tarmed.html. Accessed December 1, 2020.
21. Sporer KA , Solares M , Durant EJ , Wang W , Wu AH , Rodriguez RM . Accuracy of the initial diagnosis among patients with an acutely altered mental status. Emerg Med J. 2013 Mar;30(3):243–6. https://doi.org/10.1136/emermed-2011-200452
22. Al-Huthail YR . Accuracy of referring psychiatric diagnosis. Int J Health Sci (Qassim). 2008 Jan;2(1):35–8. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3068718/pdf/ijhs-2-1-0035.pdf
23. Nemec M , Koller MT , Nickel CH , Maile S , Winterhalder C , Karrer C , et al. Patients presenting to the emergency department with non-specific complaints: the Basel Non-specific Complaints (BANC) study. Acad Emerg Med. 2010 Mar;17(3):284–92. https://doi.org/10.1111/j.1553-2712.2009.00658.x
24. Singh H , Schiff GD , Graber ML , Onakpoya I , Thompson MJ . The global burden of diagnostic errors in primary care. BMJ Qual Saf. 2017 Jun;26(6):484–94. https://doi.org/10.1136/bmjqs-2016-005401
25. van der Biezen M , Schoonhoven L , Wijers N , van der Burgt R , Wensing M , Laurant M . Substitution of general practitioners by nurse practitioners in out-of-hours primary care: a quasi-experimental study. J Adv Nurs. 2016 Aug;72(8):1813–24. https://doi.org/10.1111/jan.12954
26. Chmiel C , Huber CA , Rosemann T , Zoller M , Eichler K , Sidler P , et al. Walk-ins seeking treatment at an emergency department or general practitioner out-of-hours service: a cross-sectional comparison. BMC Health Serv Res. 2011 May;11(1):94. https://doi.org/10.1186/1472-6963-11-94
27. Osakwe ZT , Aliyu S , Sosina OA , Poghosyan L . The outcomes of nurse practitioner (NP)-Provided home visits: A systematic review. Geriatr Nurs. 2020 Nov - Dec;41(6):962–9. https://doi.org/10.1016/j.gerinurse.2020.07.001
28. Gysin S , Bischofberger I , Meier R , van Vught A , Merlo C , Essig S . Nurse Practitioners in Swiss Family Practices as Potentially Autonomous Providers of Home Visits: An Exploratory Study of Two Cases. Home Heal Care Manag Pract. 2021. doi:https://doi.org/10.1177/1084822320946289
Tables S1-S4 are available as appendix in the PDF version of this article.