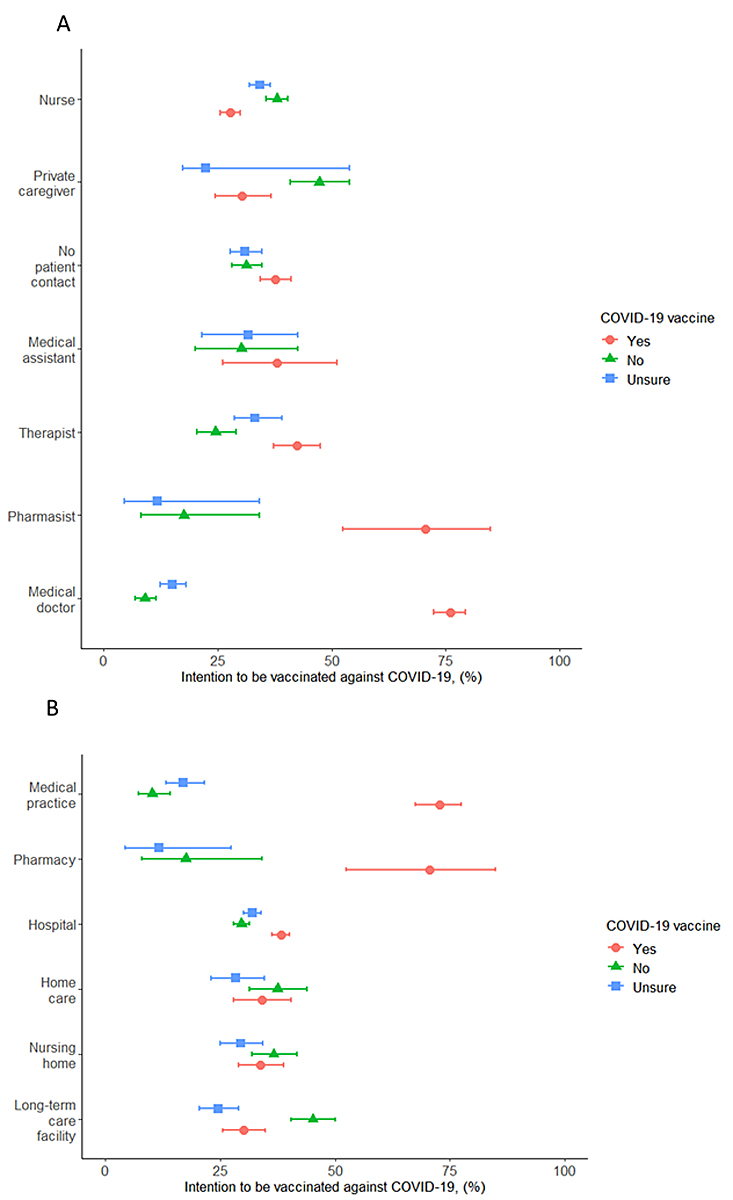
Figure 1 Number of people reporting willingness to be vaccinated against COVID-19 in the Canton of Solothurn, Switzerland by healthcare profession (A) and by workplace (B). Percent with 95% confidence intervals are presented.
DOI: https://doi.org/10.4414/SMW.2021.w30061
The worldwide spread of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections and coronavirus disease 2019 (COVID-19) is a major public health threat [1]. Globally, SARS-CoV-2 infection has been confirmed in over 131,837,512 people and as of 7 April 2021 2,862,664 have died from COVID-19 [2]. In Switzerland, the pandemic has stretched the healthcare system to its limits and burdened the economy with temporary closures of restaurants, stores and large public and private venues [4]. In the absence of effective treatments and a safe and effective vaccine, nonpharmaceutical interventions were implemented to mitigate the pandemic. Measures taken include using personal protective equipment (PPE) such as face masks in public spaces, keeping distance between individuals, and rigorous hand hygiene. Many pharmaceutical companies and research laboratories have been working on vaccines [5–7]. Effective vaccination is key to controlling the COVID-19 pandemic, but global vaccine distribution is challenging [8]. By the end of 2020, several vaccines had demonstrated efficacy in phase III trials [7], and by the beginning of January 2021, two messenger RNA (mRNA) vaccines had been approved by the Swiss Agency for Therapeutic Products (Swissmedic) [9, 10].
The delivery of the COVID-19 vaccines started on 4 January 2021, making it essential to identify and address widespread vaccine uptake barriers. Six months after the start of the national campaign, almost 50% of the total Swiss population have received at least one dose of an mRNA COVID-19 vaccine and about 30% are completely vaccinated. Scepticism about these new vaccines against COVID-19 presents one such challenge to vaccine uptake. Healthcare workers who face an increased risk of infection with SARS-CoV-2 and can transmit the virus among themselves and to highly vulnerable patients [11–15] are an important target group for vaccination. Previous studies have shown that vaccine uptake for vaccine-preventable diseases such as influenza is low among healthcare workers [16, 17]. Given the central role they play in treating COVID-19 and administering vaccinations, healthcare workers are uniquely positioned to influence vaccine uptake. Therefore, understanding the willingness of healthcare workers to be vaccinated against COVID-19, mainly if they are themselves hesitant, will be important in promoting vaccine uptake in the population.
We therefore assessed the willingness of healthcare workers in the Canton of Solothurn, Switzerland, to be vaccinated against influenza and COVID-19, and inquired about reasons for vaccine hesitancy among them.
We conducted a cross-sectional web-based survey among healthcare workers in the Canton of Solothurn, Switzerland. We included adults aged 16 years or older who work in the healthcare system in hospitals, medical practices, retirement and nursing homes, home care, pharmacies and long-term care facilities.
We developed and pilot tested a standardised questionnaire based on the study of Larson et al. [18] and the Vaccine Confidence Project at the London School of Hygiene and Tropical Medicine (www.vaccineconfidence.org/). The electronic questionnaire collected information of three types: (i) demographic details such as sex, age, and profession; (ii) intention to be vaccinated against COVID-19 and reasons for being vaccinated / not being vaccinated or for being unsure, confidence in government, recommendation of the employer, and additional information needed to take a vaccination decision; (iii) history of influenza vaccination for the influenza season 2020/21. We collected the data in mid-December 2020 before the first approval of a COVID-19 vaccine and associated campaigning, using a web-based tool (www.findmind.ch). All fields were mandatory. Free-text fields were restricted to the questions on reasons for not vaccinating, vaccinating or being unsure to vaccinate (“other reasons”; the questionnaire is in the supplementary table S1 in the appendix).
All employees of the cantonal hospital in the Canton of Solothurn were invited to participate. The survey was also sent to the cantonal professional associations of physicians, nursing homes, long-term care facilities and residential care, which invited their members to participate. The survey was distributed via the commonly used channels of communication, such as emails, newsletters and weblinks on the internal hospital website.
The Swiss Federal Office of Public Health (FPOH) defined the following COVID-19 risk groups: persons over the age of 50; those with comorbidities including hypertension, chronic respiratory diseases, diabetes, being immunocompromised, cardiovascular disease, cancer, or obesity (body mass index >30 kg/m2); persons who live in a nursing home or long-term care facility; and those who are pregnant.
The survey participants fell into three groups: persons willing to be vaccinated, those who were not willing to be vaccinated, and those who were hesitant or unsure about being vaccinated. Among those willing to be vaccinated against COVID-19, the reasons for deciding to do so could be characterised as self-protection, individual vaccination as a contribution to pandemic control, and belonging to a risk group for severe COVID-19 disease. Reasons for vaccine hesitancy included opposition to vaccines in general, the perception that COVID-19 is harmless or that PPE is sufficient, concerns about the effectiveness of the vaccine, its safety and side effects, bad experiences with previous vaccinations, fear of needles, and other reasons. People who were unsure about being vaccinated against COVID-19 were hesitant because of perceived inconsistent information, doubt about vaccine effectiveness, doubt about vaccine safety and fear of side effects, doubt about individual vaccination for pandemic control, and uncertainty among colleagues, and lack of information provided by the employer. Supplementary table S1 provides further details.
We used descriptive statistics to characterise the study population by profession and intention to be vaccinated against COVID-19. Differences between groups were assessed using chi‐square, t-test or Wilcoxon rank‐sum tests as appropriate. We calculated the proportions of people intending to be vaccinated against COVID-19 with the corresponding 95% confidence intervals (95% CIs).
We examined factors associated with the healthcare workers’ intention to be vaccinated against COVID-19 in univariate and multivariate logistic regression. Logistic models were adjusted for age group and profession, confidence in government reports, the employer’s recommendation, and influenza vaccine uptake 2020/21. We grouped uncertainty about vaccination and having no intention of being vaccinated against COVID-19. We also performed a sensitivity analysis that combined those who were willing to be vaccinated and those who were not sure about vaccination. Finally, we compared the vaccine refusers and those who were unsure about COVID-19 vaccination. All analyses were performed in Stata (version 15.1, College Station, TX, USA).
Data collection was anonymous. No ethical approval was needed, in line with the Swiss Human Research Act.
A total of 4,244 healthcare workers participated in the survey. Response rates were as follows: ~64% (2679/~4,200) among hospital staff, ~38% (338/~900) among medical practice staff, ~11% (440/~4,000) among nursing home staff, and ~29% (470/~1,600) among long-term care facility staff.
We excluded participants who did not fully complete the survey (n = 421) and those for whom data on sex, age or profession were missing (n = 12). We further excluded participants younger than 16 years (n = 18). The analyses thus included 3,793 healthcare workers (see supplementary fig. S1 in the appendix).
The median age of participanting healthcare workers was 43 years (interquartile range [IQR] 31–53), 2,841 were female (74.9%). Among all healthcare workers, 2,445 (64.5%) worked in hospitals, 398 (10.5%) worked in long-term care facilities, 373 (9.8%) in retirement and nursing homes, 311 (8.2%) in medical practices, 232 (6.1%) in residential care and 34 (0.9%) at pharmacies (table 1 and supplementary table S2 in the appendix). Asked about COVID-19 vaccination, 1,511 healthcare workers (39.8%) reported they planned to have the COVID-19 vaccine, 1,114 (29.4%) said they were unsure and 1,168 (30.8%) said they would not accept vaccination. Willingness to be vaccinated was highest among medical doctors, among whom 467 of 617 (76.1%) were willing to be vaccinated, and it was lowest among nurses at 470 of 1,690 (27.8%) (fig.1A and B shows willingness to be vaccinated by profession and workplace).
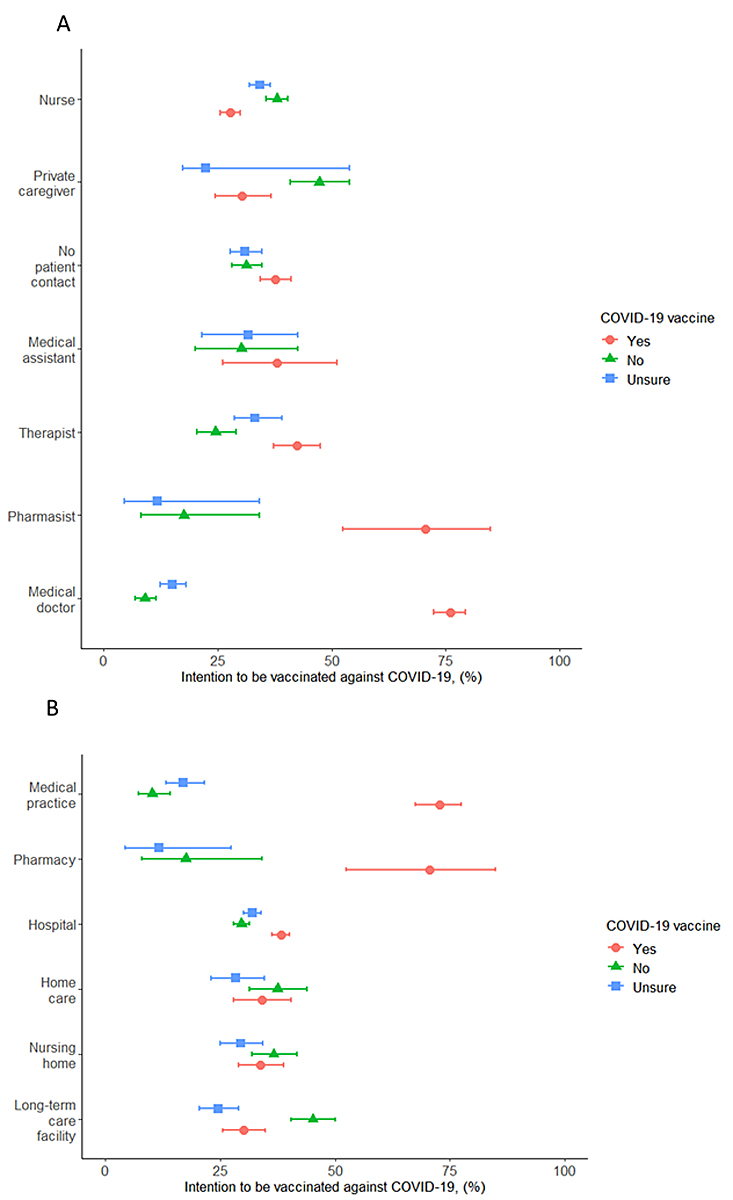
Figure 1 Number of people reporting willingness to be vaccinated against COVID-19 in the Canton of Solothurn, Switzerland by healthcare profession (A) and by workplace (B). Percent with 95% confidence intervals are presented.
The self-reported uptake for seasonal influenza 2020/2021 vaccination was 38.1% (1,446 of 3,793), 118 (3.1%) were unsure whether they had been vaccinated and 2,229 (58.8%) reported they were not vaccinated. The influenza vaccination rate was highest among medical doctors (75.6%) and pharmacists (58.8%). Among the other professions, the vaccination rate ranged from 11.6% to 44.4% (table 1).
Table 1Characteristics of healthcare workers participating in the survey, overall and by profession.
| All HCW (n = 3793) | Nurses (n = 1690) | Medical doctors (n = 614) | Medical assistants (n = 63) | Pharmacist and assistants (n = 34) | Other medical staff* (n = 380) | Private caregivers (n = 224) | Staff without patient contact (n = 788) | |
| Sex | ||||||||
| Male | 952 (25.1) | 202 (12.0) | 358 (58.3) | 1 (1.6) | 10 (29.4) | 57 (15.0) | 77 (34.4) | 247 (31.4) |
| Female | 2,841 (74.9) | 1,488 (88.0) | 256 (41.7) | 62 (98.4) | 24 (70.6) | 323 (85.0) | 147 (65.6) | 541 (68.7) |
| Age in years, median (IQR) | 43 (31–53) | 39 (27–52) | 46 (36–55) | 39 (25–52) | 49 (32–59) | 43 (30.5–53) | 41 (30–55) | 48 (36–55) |
| Workplace | ||||||||
| Hospital | 2,445 (64.5) | 1,122 (66.4) | 372 (60.6) | 0 | 0 | 380 (100) | 0 | 571 (72.5) |
| Medical practice | 311 (8.2) | 6 (0.4) | 240 (39.1) | 58 (92.1) | 0 | 0 | 0 | 7 (0.9) |
| Retirement and nursing home | 373 (9.8) | 287 (17.0) | 0 | 2 (3.2) | 0 | 0 | 0 | 84 (10.7) |
| Residential care | 323 (6.1) | 193 (11.4) | 0 | 2 (3.2) | 0 | 0 | 0 | 37 (4.7) |
| Pharmacy | 34 (0.9) | 0 | 0 | 0 | 34 (100) | 0 | 0 | 0 |
| Long-term care facilities | 398 (10.5) | 82 (4.9) | 2 (0.3) | 1 (1.6) | 0 | 0 | 224 (100) | 89 (11.3) |
| Willingness to get COVID-19 vaccine | ||||||||
| Yes | 1,511 (39.8) | 470 (27.8) | 467 (76.1) | 24 (38.1) | 24 (70.6) | 161 (42.4) | 68 (30.4) | 297 (37.7) |
| No | 1,168 (30.8) | 642 (38.0) | 55 (9.0) | 19 (30.2) | 6 (17.6) | 93 (24.5) | 106 (47.3) | 247 (31.3) |
| Unsure | 1,114 (29.4) | 578 (34.2) | 92 (15.0) | 20 (31.8) | 4 (11.8) | 126 (33.2) | 50 (22.3) | 244 (31.0) |
| Opinion on employer’s recommendation | ||||||||
| No opinion | 893 (23.5) | 452 (26.8) | 107 (17.4) | 16 (25.4) | 8 (23.5) | 80 (21.1) | 40 (17.9) | 190 (24.1) |
| Completely and somewhat disagree | 1066 (28.1) | 598 (35.4) | 75 (12.2) | 17 (27.0) | 3 (8.8) | 86 (22.6) | 95 (42.4) | 192 (24.4) |
| Completely and somewhat agree | 1834 (48.4) | 640 (37.9) | 432 (79.4) | 30 (47.6) | 23 (67.7) | 214 (56.3) | 89 (39.7) | 406 (51.5) |
| Opinion on government reports | ||||||||
| No opinion | 645 (17.0) | 337 (19.9) | 47 (7.7) | 12 (19.1) | 5 (14.7) | 55 (14.5) | 45 (20.1) | 144 (18.3) |
| Completely and somewhat disagree | 868 (22.9) | 489 (28.9) | 48 (7.8) | 18 (28.6) | 6 (17.7) | 57 (15.0) | 71 (31.7) | 179 (22.7) |
| Completely and somewhat agree | 2,280 (60.1) | 864 (51.1) | 519 (84.5) | 33 (52.4) | 23 (67.7) | 268 (70.5) | 108 (48.2) | 465 (59.0) |
| Had influenza vaccine 20/21 | ||||||||
| No | 2,229 (58.8) | 1,101 (65.2) | 113 (18.4) | 34 (54.0) | 11 (32.4) | 217 (57.1) | 193 (86.2) | 560 (71.1) |
| Yes | 1,446 (38.1) | 550 (32.5) | 464 (75.6) | 28 (44.4) | 20 (58.8) | 151 (39.7) | 26 (11.6) | 207 (26.3) |
| Not sure | 118 (3.1) | 39 (2.3) | 37 (6.0) | 1 (1.6) | 3 (8.8) | 12 (3.2) | 5 (2.2 | 21 (2.7) |
| Reasons for vaccine willingness against COVID-19 | 1,511 (100) | 470 (100) | 467 (100) | 24 (100) | 24 (100) | 161 (100) | 68 (100) | 297 (100) |
| Protection | 1,461 (96.7) | 449 (95.5) | 460 (98.5) | 23 (95.8) | 21 (87.5) | 151 (93.8) | 65 (95.6) | 292 (98.3) |
| Vaccine for pandemic control | 1,328 (87.9) | 395 (84.0) | 434 (92.9) | 24 (100) | 21 (87.5) | 143 (88.8) | 55 (80.9) | 256 (86.2) |
| Risk group | 266 (17.6) | 76 (16.2) | 96 (20.6) | 0 | 7 (29.2)) | 20 (12.4) | 14 (20.6) | 53 (17.8) |
| Reasons for vaccine hesitancy against COVID-19 | 1,168 (100) | 642 (100) | 55 (100) | 19 (100) | 6 (100) | 93 (100) | 106 (100) | 247 (100) |
| Vaccine safety and side effects | 1,073 (91.9) | 603 (93.9) | 51 (92.7) | 17 (89.5) | 4 (66.7) | 87 (93.5) | 90 (84.9) | 221 (89.5) |
| PPE is sufficient | 328 (28.1) | 193 (30.1) | 13 (23.6) | 4 (21.1) | 1 (16.7) | 26 (28.0) | 32 (30.2) | 59 (23.9) |
| COVID-19 harmless | 229 (19.6) | 118 (18.4) | 20 (36.4) | 3 (15.8) | 0 | 16 (17.2) | 25 (23.6) | 47 (19.0) |
| Bad experiences | 201 (17.2) | 111 (17.3) | 12 (18.2) | 2 (10.5) | 0 | 11 (11.8) | 20 (18.9) | 45 (18.2) |
| Effectiveness of the vaccine | 128 (11.0) | 85 (13.2) | 6 (10.9) | 1 (5.3) | 0 | 8 (8.6) | 12 (11.3) | 16 (6.5) |
| Opponents of vaccines in general | 39 (3.3) | 20 (3.1) | 0 | 1 (5.3 | 0 | 1 (1.1) | 5 (4.7) | 12 (4.9) |
| Fear of needles | 40 (3.4) | 20 (3.1) | 1 (1.8) | 0 | 1 (16.7) | 4 (4.3) | 4 (3.8) | 10 (4.0) |
| Others | 379 (32.4) | 194 (30.2) | 24 (43.6) | 4 (21.1) | 1 (16.7) | 33 (35.5) | 46 (43.4) | 77 (31.2) |
| Reasons for being unsure of vaccination against COVID-19 | 1,114 (100) | 578 (100) | 92 (100) | 20 (100) | 4 (100) | 126 (100) | 50 (100) | 244 (100) |
| Vaccine safety and side effects | 1,058 (95.0) | 538 (93.1) | 88 (95.7) | 18 (90.0) | 4 (100) | 124 (98.4) | 50 (100) | 236 (96.7) |
| Inconsistent information | 329 (29.5) | 192 (33.2) | 29 (31.5) | 1 (5.0) | 1 (25.0) | 40 (31.7) | 17 (34.0) | 51 (20.9) |
| Effectiveness of the vaccine | 316 (28.4) | 177 (30.6) | 16 (17.4) | 5 (25.0) | 1 (25.0) | 33 (26.2) | 15 (30.0) | 69 (28.3) |
| No education by my employer | 210 (18.9) | 126 (21.8) | 14 (15.2) | 5 (25.0) | 0 | 29 (23.0) | 4 (8.0) | 32 (13.1) |
| Uncertainty by my colleagues | 251 (22.5) | 147 (25.4) | 18 (19.6) | 6 (30.0) | 0 | 31 (24.6) | 10 (20.0) | 39 (16.0) |
| Vaccine for pandemic control | 174 (15.6) | 93 (16.1) | 14 (15.2) | 2 (10.0) | 0 | 17 (13.5) | 10 (20.0) | 38 (15.6) |
| Information needs among unsure HCW | 1,114 (100) | 578 (100) | 92 (100) | 20 (100) | 4 (100) | 126 (100) | 50 (100) | 244 (100) |
| Information about COVID-19 | 116 (10.4) | 68 (11.8) | 8 (8.7) | 1 (5.0) | 0 | 14 (11.1) | 5 (10.0) | 20 (8.2) |
| Information about the vaccine | 1,055 (94.7) | 550 (95.2) | 81 (88.0) | 19 (95.0) | 4 (100) | 121 (96.0) | 47 (94.0) | 233 (95.5) |
| Reports from vaccinated people | 778 (69.8) | 412 (71.3) | 45 (48.9) | 17 (85.0) | 2 (50.0) | 74 (58.7) | 41 (82.0) | 187 (76.6) |
| Opinion of experts | 404 (36.3) | 220 (38.1) | 32 (34.8) | 9 (45.0) | 0 | 56 (44.4) | 15 (30.0) | 72 (29.5) |
HCW = healthcare workers; IQR = interquartile range; PPE = personal protective equipment
Data are n (%) unless otherwise stated.
* “Other medical staff” includes physical therapists, occupational therapists, speech therapists and midwives.
The willingness among healthcare workers to be vaccinated against COVID-19 was lower among females than male participants (odds ratio [OR] 0.33, 95% Cl 0.28–0.38) and increased with age. Willingness was highest among the age group ≥60 years (OR 4.56, 95% Cl 3.50–5.94) compared with the age group <30 years. Healthcare workers reporting having been vaccinated against seasonal influenza 2020/21 were more willing to be vaccinated against COVID-19 (OR 6.30, 95% Cl 5.45–7.23) than the unvaccinated group. Confidence in government reports and employers’ vaccination recommendation were associated with willingness to be immunised against COVID-19: OR 4.12 (95% Cl 3.37–5.03) and OR 14.19 (95% Cl 11.53–17.47), respectively. In contrast, lack of such confidence was negatively associated with willingness to get vaccinated as compared with the group with no opinion (table 2). The willingness to be vaccinated against COVID-19 was higher among pharmacists (OR 6.22, 95% Cl 2.96–13.13) and medical doctors (OR 8.24, 95% Cl 6.66–12.21) than nurses.
In the multivariate analysis, willingness to be vaccinated was positively associated with confidence in government reports on the COVID-19 pandemic (adjusted OR [aOR] 1.41, 95% Cl 1.07–1.85) and negatively with lack of confidence in government (aOR 11.40, 95% Cl 8.87–14.65). Similarly, confidence in employer recommendations was positively associated, whereas lack of confidence was negatively associated. The analysis confirmed that healthcare workers who reported vaccination against seasonal influenza 2020/21 were more likely to be willing to be vaccinated against COVID-19 than those who were not vaccinated (aOR 2.70, 95% Cl 2.20–3.31, table 2). When an interaction term with influenza vaccination and age group was included in the multivariate model, influenza vaccination and age group were interrelated (p-value from the test for an interaction p = 0.03).
In the sensitivity analysis grouping the willing and unsure together (rather than the refusers and unsure), results were similar to the primary analysis (supplementary table S3).
Table 2Characteristics of healthcare workers’ willingness to be vaccinated against COVID-19, vaccine hesitancy and uncertainty about vaccination, and factors associated with willingness to be vaccinated.
| Variables | Total | Willingness to be vaccinated against COVID-19 n (%) | Comparison of persons willing to be vaccinated against COVID-19 with persons with hesitancy/unsure | |||||
| Number of participants | Yes | No | Unsure | UnadjustedOR (95% Cl) | p-value | Adjusted OR(95% Cl)* | p-value | |
| Total | 3,793 | 1,511 | 1,168 | 1,114 | ||||
| Sex | ||||||||
| Male | 952 | 561 (58.9) | 196 (20.6) | 195 (20.5) | 1 | <0.001 | ||
| Female | 2,841 | 950 (33.4) | 972 (34.2) | 919 (32.4) | 0.33 (0.28–0.38) | |||
| Age groups | <0.001 | <0.001 | ||||||
| 29 and younger | 829 | 207 (24.9) | 381 (46.0) | 241 (29.1) | 1 | 1 | ||
| 30 to 39 | 807 | 285 (35.3) | 257 (31.9) | 265 (32.8) | 1.64 (1.33–2.03) | 0.93 (0.68–1.25) | ||
| 40 to 49 | 790 | 335 (42.4) | 215 (27.2) | 240 (30.4) | 2.21 (1.79–2.73) | 1.29 (0.96–1.76) | ||
| 50 to 59 | 1,012 | 470 (46.4) | 254 (25.1) | 288 (28.5) | 2.61 (2.13–3.18) | 1.78 (1.34–2.36) | ||
| 60 and older | 355 | 214 (60.3) | 61 (17.2) | 80 (22.5) | 4.56 (3.50–5.94) | 2.45 (1.68–3.57) | ||
| Profession | <0.001 | <0.001 | ||||||
| Medical doctor | 614 | 467 (76.0) | 55 (9.0) | 92 (15.0) | 8.24 (6.66–12.21) | 4.88 (3.58–6.65) | ||
| Nurse | 1,690 | 470 (27.8) | 642 (38.0) | 578 (34.2) | 1 | 1 | ||
| Medical assistant | 63 | 24 (70.6) | 6 (17.7) | 4 (11.8) | 1.60 (0.95–2.69) | 1.45 (0.68–3.10) | ||
| Pharmacist and pharmacist assistant | 24 | 16 (66.7) | 5 (20.8) | 3 (12.5) | 6.22 (2.96–13.13) | 4.20 (1.53–11.52) | ||
| Other medical staff** | 380 | 161 (42.4) | 93 (24.5) | 126 (33.2) | 1.91 (1.52–2.40) | 1.22 (0.89–1.68) | ||
| Not close patient contact | 788 | 297 (37.7) | 247 (31.3) | 244 (31.9) | 1.57 (1.31–1.88) | 1.15 (0.89–1.48) | ||
| Private caregiver | 224 | 68 (30.4) | 106 (47.3) | 50 (22.3) | 1.13 (0.83–1.53) | 1.51 (0.98–2.33) | ||
| Confidence in the government reports | <0.001 | <0.001 | ||||||
| No opinion | 645 | 150 (23.3) | 238 (36.9) | 257 (39.8) | 1 | 1 | ||
| Completely and somewhat disagree | 868 | 95 (10.9) | 533 (61.4) | 240 (27.7) | 0.41 (0.31–0.54) | 0.58 (0.40–0.84) | ||
| Completely and somewhat agree | 2,280 | 1,266 (55.5) | 397 (17.4) | 617 (27.1) | 4.12 (3.37–5.03) | 1.41 (1.07–1.85) | ||
| Follow employer’s recommendation | <0.001 | <0.001 | ||||||
| No opinion | 893 | 140 (15.7) | 283 (31.7) | 470 (52.6) | 1 | 1 | ||
| Completely and somewhat disagree | 1,066 | 41 (3.9) | 801 (75.1) | 224 (21.0) | 0.22 (0.15–0.31) | 0.30 (0.20–0.44) | ||
| Completely and somewhat agree | 1,834 | 1,330 (72.5) | 84 (4.6) | 420 (22.9) | 14.19 (11.53–17.47) | 11.40 (8.87–14.65) | ||
| Influenza vaccination 20/21 | <0.001 | <0.001 | ||||||
| No | 2,347 | 555 (23.7) | 1019 (43.4) | 773 (32.9) | 1 | 1 | ||
| Yes | 1,556 | 956 (66.1) | 149 (10.3) | 341 (23.6) | 6.30 (5.45–7.23) | 2.70 (2.20–3.31) | ||
| CI = confidence interval; HCW = healthcare worker; OR = odds ratio* Model adjusted for age groups, profession, confidence in the government reports, following employer’s recommendation, and influenza vaccination 20/21.† “Other medical staff” includes physical therapists, occupational therapists, speech therapists, and midwives | ||||||||
CI = confidence interval; HCW = healthcare worker; OR = odds ratio
* Model adjusted for age groups, profession, confidence in the government reports, following employer’s recommendation, and influenza vaccination 20/21.
** “Other medical staff” includes physical therapists, occupational therapists, speech therapists, and midwives
The main reasons for willingness to be vaccinated were personal protection, controlling the pandemic and belonging to a risk group (fig. 2A, table 1). These reasons differed according to profession (p <0.05). The most frequent reasons for vaccine hesitancy among healthcare workers included concerns about vaccine safety and side effects (1,073/1,168, 91.9%), the perception that PPE is sufficient (328/1,168, 28.1%), and that COVID-19 is harmless (231/1,168, 19.8%, fig. 2B and table 1). All reasons for vaccine hesitancy were similar in the different healthcare professions, except for vaccine safety and side effects, which were mentioned more frequently as a reason for vaccine hesitancy by nurses (p = 0.01)
Among the 1,114 healthcare workers who were unsure about a vaccination decision, 1,055 (94.7%) wanted more information on vaccine safety and side effects, 778 (69.6%) awaited reports from already vaccinated people and 404 (36.3%) wanted an opinion from experts. The main reasons can be found in figure 2C and table 1. The reasons for being unsure were similar across the healthcare professions, but pharmacists more frequently wanted information on the vaccine than medical doctors (100% vs 88%, p = 0.01).
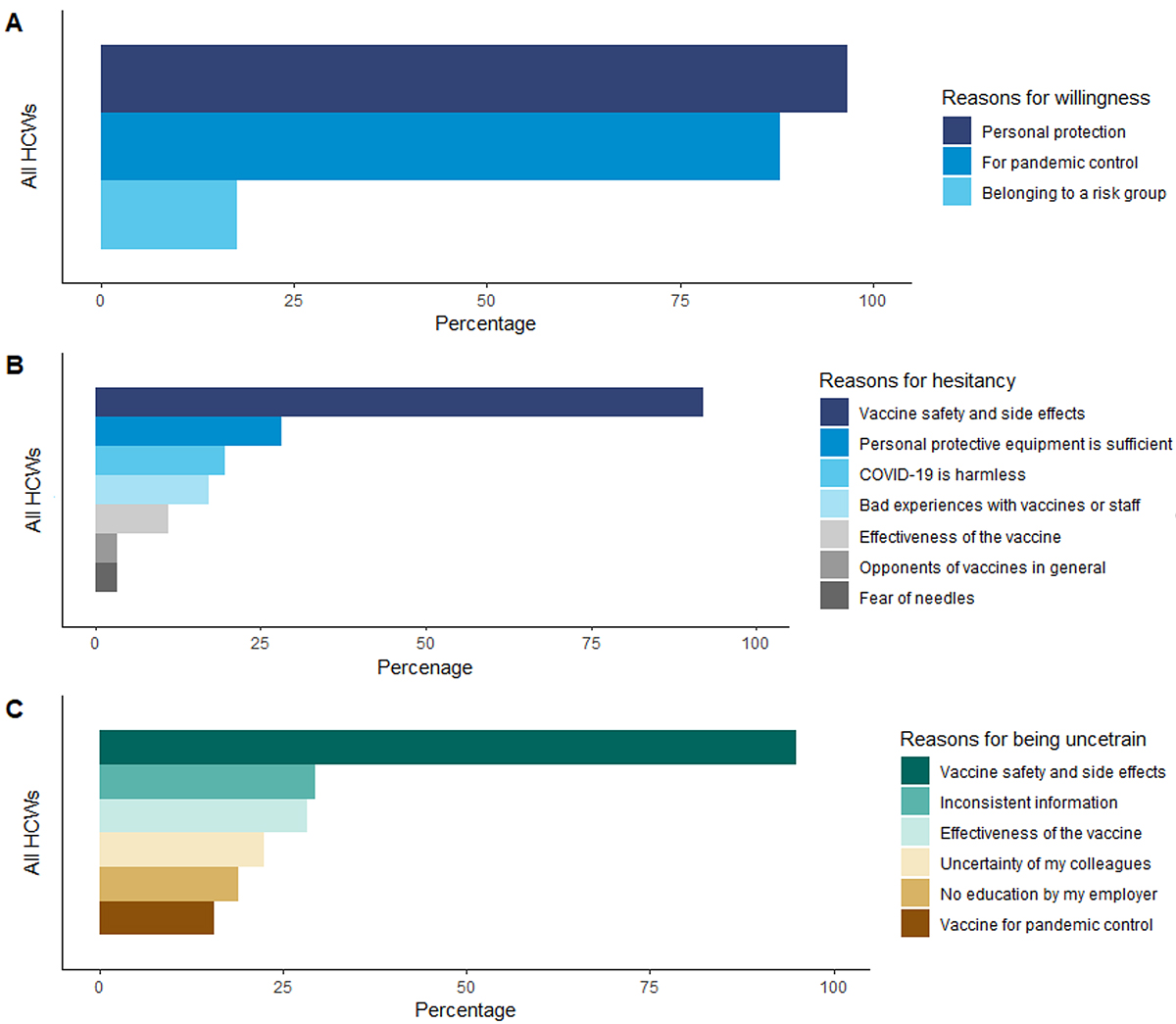
Figure 2 Reasons for vaccine willingness (A), vaccine hesitancy (B) and being uncertain (C) among all healthcare workers. The exact numbers can be found in table 1.
Less than half of participating healthcare workers reported willingness to be vaccinated against COVID-19. The most frequently given reason for vaccine hesitancy was concern about vaccine safety and side effects. Nurses were less likely to be willing to be vaccinated against COVID-19 than medical doctors or pharmacists.
Vaccines are an effective control measure to reduce the burden of infectious disease. Poliomyelitis was eradicated, and we are close to eliminating measles, mumps, and rubella with vaccines [19]. Vaccination will play an important role in the control of the COVID-19 pandemic. Even transient herd immunity in Switzerland will require more than 60% of the population having achieved immunity to SARS-CoV-2 either through infection and recovery or through vaccination, particularly when considering the potential impacts of SARS-CoV-2 variants of concern. However, this proportion varies depending on model assumptions [20].
Willingness to get vaccinated is central to achieving herd immunity. Several cross-sectional studies have assessed the willingness to get vaccinated. In seven countries, a European general population survey found that the willingness to be vaccinated against COVID-19 ranged from 62% to 80% [21]. Similar results were found in the United Kingdom and Ireland, with 69% and 65% acceptance, respectively [22]. In the USA, 37% of healthcare workers reported being willing to get vaccinated against COVID-19 [23]. These results are in line with our results (40%) in the Canton of Solothurn in Switzerland. These numbers cause concern because healthcare workers play an important role in vaccine uptake among the general population. A review on vaccine hesitancy has shown that vaccinated healthcare workers are more likely to recommend vaccination than unvaccinated healthcare workers [24]. Furthermore, a vaccination recommendation given by an healthcare worker is frequently cited as the reason for vaccination acceptance [25]. In contrast, the lack of such a recommendation was the most common reason for not being vaccinated [24, 26].
Some healthcare workers have expressed reservations about the safety and side effects of COVID-19 vaccines. One contributor to such reservations is the perception of undue haste in the development of COVID-19 vaccines compared with previous vaccines. In the twentieth century, it took a decade or longer to get vaccines to the market, for example, in the case of poliomyelitis [27]. Many factors contributed to the comparatively short time it took for COVID-19 vaccines to be granted emergency use authorisations in many countries, with definitive licensing granted on a rolling basis. Researchers have been developing mRNA and viral vector-based vaccines for other diseases for more than a decade [28]. As the pandemic spread, public willingness and even demand led to rapid enrolment in phase I to phase III clinical trials with historically unprecedented speed. Simultaneously, the rapid spread of SARS-CoV-2 allowed endpoint-driven phase III trials to demonstrate vaccine efficacy sooner than was expected at their outset.
We found that confidence in the governmental authorities is associated with willingness to get vaccinated against COVID-19. During a health crisis or a pandemic, trust in the government and risk perception play a key role in vaccine acceptance [29, 30]. A French survey among general practitioners showed they were more likely to recommend vaccines to patients when they trusted official sources of information [31]. A global survey also reported an association between vaccine acceptance and participants’ trust in government [32]. High levels of trust in government was associated with willingness to follow governmental recommendations on preventive behaviours to contain swine flu [33] or compliance with social distancing measures during the Ebola outbreak [34]. In contrast, mistrust and misinformation reduced compliance with social and behavioural measures [35]. A cross-sectional study during the COVID-19 pandemic among UK residents showed that residents who trusted the government to control the pandemic were more likely to follow government recommendations during the lockdown [36].
Strategies to increase vaccine coverage among healthcare workers should draw upon guidance from authorities or persons conceived as such by a target audience (in this case healthcare workers) and specific information about vaccine safety and efficacy. Thus, it is not surprising that many undecided healthcare workers want to have reports from fellow healthcare workers who have been vaccinated before they make up their minds. Peers provide important information that influences decision making, but this source of information is often overlooked. Healthcare workers may be the most effective promotors of vaccination for their fellows.
We observed that healthcare workers who were vaccinated against seasonal influenza are also more likely to willing to be vaccinated against COVID-19. Both diseases are contagious respiratory diseases caused by viruses, and they share some of the same symptoms (fever, cough) and approaches for prevention (hand hygiene, physical distancing, and masks). However, there are important differences. Superspreader events are more common for COVID-19 [37], and mortality rates are higher for COVID-19 than for influenza [38, 39]. A recent study showed that over time, the uptake of the seasonal influenza vaccine in Switzerland had dropped overall, and among older persons (≥65 years) and people with chronic disease [40]. This reduced coverage might be explained by variable and lower seasonal influenza vaccine effectiveness, which can range from 30–60% [41, 42].
The limitations of this study include different response rates among the healthcare professions and potential over-representation of hospital-based healthcare workers. We conducted a web-based cross-sectional online survey in which participation was voluntary but highly supported by the hospital-based personnel. Hospital-based healthcare workers may be over-represented. Healthcare workers interested in the topic are more likely to respond to the questionnaire. This might introduce a bias and lead to an over- or under-estimation of vaccine hesitancy or vaccine acceptance. The survey was conducted only in the Canton of Solothurn and the results cannot be necessarily generalised to the whole of Switzerland. Furthermore, some cantons were more heavily affected by the pandemic than others. This may result in different attitudes towards the COVID-19 vaccine among healthcare workers. Compared with other online surveys, this survey was distributed among specific groups of healthcare workers to cover better this heterogeneous population. Additionally, attitudes towards vaccination against COVID-19 and willingness to get vaccinated change over time. With more people being vaccinated, acceptance increases, and vaccine hesitancy might decrease. Finally, the survey was conducted before the approval of the two COVID-19 vaccines in Switzerland. Perceptions of the safety of the vaccine have changed since the approval of the vaccines and vaccine hesitancy might have decreased in the months after approval. This is true for COVID-19 vaccines, but maybe also be true for any new vaccine introduced in the healthcare sector.
This study’s strength is the inclusion of diverse healthcare institutions and healthcare workers who play quite different roles within them. We included healthcare workers working with varying populations of risk ranging from nursing home residents, hospitalised patients to people living in long-term care facilities. Furthermore, the survey covered the three largest healthcare providers in the canton of Solothurn.
At this early stage of the COVID-19 vaccine campaign, the overall willingness to get vaccinated among healthcare workers is low. Balanced and transparent information on vaccine efficacy, safety and side effects should be provided to healthcare workers and dialogue on vaccine hesitancy initiated.
We would like to thank all healthcare workers who were willing to participate. Further, we would like to thank all the institutions for distributing the survey to their employees. We thank Christopher Ritter for editorial assistance.
There was no specific funding for this project. KZ was supported by grant U01AI069924 from the U.S. National Institutes of Health’s National Institute of Allergy and Infectious Diseases. ME was supported by special project funding (grant 189498) from the Swiss National Science Foundation.
All authors declare that they have no conflict of interest.
1. Zhu N , Zhang D , Wang W , Li X , Yang B , Song J , et al.; China Novel Coronavirus Investigating and Research Team . A Novel Coronavirus from Patients with Pneumonia in China, 2019. N Engl J Med. 2020 Feb;382(8):727–33. https://doi.org/10.1056/NEJMoa2001017
2. World Health Organization . Coronavirus Disease (COVID-19) Dashboard Geneva: World Health Organization; 2021 [cited 2021 13 Reburary]. Available from: https://covid19.who.int/
3. Federal Office of Public Health (FOPH) . Coronavirus: Situation Schweiz Bern Federal Office of Public Health; 2021 [Available from: https://www.bag.admin.ch/bag/de/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/situation-schweiz-und-international.html
4 Nicola M , Alsafi Z , Sohrabi C , Kerwan A , Al-Jabir A , Iosifidis C , et al. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. International journal of surgery (London, England). 2020;78:185-93.
5. Kim JH , Marks F , Clemens JD . Looking beyond COVID-19 vaccine phase 3 trials. Nat Med. 2021 Feb;27(2):205–11. https://doi.org/10.1038/s41591-021-01230-y
6. Parker EP , Shrotri M , Kampmann B . Keeping track of the SARS-CoV-2 vaccine pipeline. Nat Rev Immunol. 2020 Nov;20(11):650. https://doi.org/10.1038/s41577-020-00455-1
7. London School of Hygiene & Tropical Medicine . COVID-19 vaccine tracker London: London School of Hygiene & Tropical Medicine; 2020 [Available from: https://vac-lshtm.shinyapps.io/ncov_vaccine_landscape/
8. So AD , Woo J . Reserving coronavirus disease 2019 vaccines for global access: cross sectional analysis. BMJ. 2020 Dec;371:m4750. https://doi.org/10.1136/bmj.m4750
9. Swissmedic. Swissmedic grants authorisation for the first COVID-19 vaccine in Switzerland Bern: Swissmedic; 2020 [Available from: https://www.swissmedic.ch/swissmedic/en/home/news/coronavirus-covid-19/covid-19-impfstoff_erstzulassung.html
10. Swissmedic. Swissmedic grants authorisation for the COVID-19 vaccine from Moderna: Second COVID-19 vaccine authorised in Switzerland Bern: Swissmedic; 2021 [Available from: https://www.swissmedic.ch/swissmedic/en/home/news/coronavirus-covid-19/zulassung-covid-19-impfstoff-moderna.html
11. Remuzzi A , Remuzzi G . COVID-19 and Italy: what next? Lancet. 2020 Apr;395(10231):1225–8. https://doi.org/10.1016/S0140-6736(20)30627-9
12. International Council of Nurses . International Council of Nurses High proportion of healthcare workers with COVID-19 in Italy is a stark warning to the world: protecting nurses and their colleagues must be the number one priority. 20 March, 2020. Geneva: International Council of Nurses; 2020 [Available from: https://www.icn.ch/news/high-proportion-healthcare-workers-covid-19-italy-stark-warning-world-protecting-nurses-and
13. Garcia-Basteiro AL , Moncunill G , Tortajada M , Vidal M , Guinovart C , Jiménez A , et al. Seroprevalence of antibodies against SARS-CoV-2 among health care workers in a large Spanish reference hospital. Nat Commun. 2020 Jul;11(1):3500. https://doi.org/10.1038/s41467-020-17318-x
14. Folgueira MD , Muñoz-Ruipérez C , Alonso-López MÁ , Delgado R . SARS-CoV-2 infection in Health Care Workers in a large public hospital in Madrid, Spain, during March 2020. medRxiv. 2020:2020.04.07.20055723.
15. Thompson HA , Mousa A , Dighe A , Fu H , Arnedo-Pena A , Barrett P , et al. SARS-CoV-2 setting-specific transmission rates: a systematic review and meta-analysis. Clin Infect Dis. 2021 Aug;73(3):e754–64. https://doi.org/10.1093/cid/ciab100
16. Napolitano F , Bianco A , D’Alessandro A , Papadopoli R , Angelillo IF . Healthcare workers’ knowledge, beliefs, and coverage regarding vaccinations in critical care units in Italy. Vaccine. 2019 Oct;37(46):6900–6. https://doi.org/10.1016/j.vaccine.2019.09.053
17. Harrison N , Brand A , Forstner C , Tobudic S , Burgmann K , Burgmann H . Knowledge, risk perception and attitudes toward vaccination among Austrian health care workers: A cross-sectional study. Hum Vaccin Immunother. 2016 Sep;12(9):2459–63. https://doi.org/10.1080/21645515.2016.1168959
18. Larson HJ , Schulz WS , Tucker JD , Smith DM . Measuring vaccine confidence: introducing a global vaccine confidence index. PLoS Curr. 2015 Feb;7:7. https://doi.org/10.1371/currents.outbreaks.ce0f6177bc97332602a8e3fe7d7f7cc4
19. Andre FE , Booy R , Bock HL , Clemens J , Datta SK , John TJ , et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. 2008 Feb;86(2):140–6. https://doi.org/10.2471/BLT.07.040089
20. Anderson RM , Vegvari C , Truscott J , Collyer BS . Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet. 2020 Nov;396(10263):1614–6. https://doi.org/10.1016/S0140-6736(20)32318-7
21. Neumann-Böhme S , Varghese NE , Sabat I , Barros PP , Brouwer W , van Exel J , et al. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020 Sep;21(7):977–82. https://doi.org/10.1007/s10198-020-01208-6
22. Murphy J , Vallières F , Bentall RP , Shevlin M , McBride O , Hartman TK , et al. Psychological characteristics associated with COVID-19 vaccine hesitancy and resistance in Ireland and the United Kingdom. Nat Commun. 2021 Jan;12(1):29. https://doi.org/10.1038/s41467-020-20226-9
23. Shekhar R , Sheikh AB , Upadhyay S , Singh M , Kottewar S , Mir H , et al. COVID-19 Vaccine Acceptance Among Health Care Workers in the United States. medRxiv. 2021:2021.01.03.21249184.
24. Paterson P , Meurice F , Stanberry LR , Glismann S , Rosenthal SL , Larson HJ . Vaccine hesitancy and healthcare providers. Vaccine. 2016 Dec;34(52):6700–6. https://doi.org/10.1016/j.vaccine.2016.10.042
25. Bianco A , Pileggi C , Iozzo F , Nobile CG , Pavia M . Vaccination against human papilloma virus infection in male adolescents: knowledge, attitudes, and acceptability among parents in Italy. Hum Vaccin Immunother. 2014;10(9):2536–42. https://doi.org/10.4161/21645515.2014.969614
26. Smith LE , Amlôt R , Weinman J , Yiend J , Rubin GJ . A systematic review of factors affecting vaccine uptake in young children. Vaccine. 2017 Oct;35(45):6059–69. https://doi.org/10.1016/j.vaccine.2017.09.046
27. Baicus A . History of polio vaccination. World J Virol. 2012 Aug;1(4):108–14. https://doi.org/10.5501/wjv.v1.i4.108
28. A gamble pays off in 'spectacular success': How the leading coronavirus vaccines made it to the finish line [press release]. Washington, United States The Washington Post2020.
29. Larson HJ , Clarke RM , Jarrett C , Eckersberger E , Levine Z , Schulz WS , et al. Measuring trust in vaccination: A systematic review. Hum Vaccin Immunother. 2018 Jul;14(7):1599–609. https://doi.org/10.1080/21645515.2018.1459252
30. van der Weerd W , Timmermans DR , Beaujean DJ , Oudhoff J , van Steenbergen JE . Monitoring the level of government trust, risk perception and intention of the general public to adopt protective measures during the influenza A (H1N1) pandemic in The Netherlands. BMC Public Health. 2011 Jul;11(1):575. https://doi.org/10.1186/1471-2458-11-575
31. Verger P , Fressard L , Collange F , Gautier A , Jestin C , Launay O , et al. Vaccine Hesitancy Among General Practitioners and Its Determinants During Controversies: A National Cross-sectional Survey in France. EBioMedicine. 2015 Jun;2(8):891–7. https://doi.org/10.1016/j.ebiom.2015.06.018
32. Lazarus JV , Ratzan SC , Palayew A , Gostin LO , Larson HJ , Rabin K , et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2020;1–4.
33 Rubin GJ , Amlôt R , Page L , Wessely S . Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. BMJ. 2009;339(jul02 3):b2651. doi:https://doi.org/https://doi.org/10.1136/bmj.b2651.
34. Blair RA , Morse BS , Tsai LL . Public health and public trust: Survey evidence from the Ebola Virus Disease epidemic in Liberia. Soc Sci Med. 2017 Jan;172:89–97. https://doi.org/10.1016/j.socscimed.2016.11.016
35. Vinck P , Pham PN , Bindu KK , Bedford J , Nilles EJ . Institutional trust and misinformation in the response to the 2018-19 Ebola outbreak in North Kivu, DR Congo: a population-based survey. Lancet Infect Dis. 2019 May;19(5):529–36. https://doi.org/10.1016/S1473-3099(19)30063-5
36. Moxham-Hall V , Strang L . Public opinion and trust in government during a public health crisis London: King's College London; 2020 [Available from: https://www.kcl.ac.uk/news/public-opinion-and-trust-in-government-during-a-public-health-crisis
37. Adam DC , Wu P , Wong JY , Lau EH , Tsang TK , Cauchemez S , et al. Clustering and superspreading potential of SARS-CoV-2 infections in Hong Kong. Nat Med. 2020 Nov;26(11):1714–9. https://doi.org/10.1038/s41591-020-1092-0
38. Piroth L , Cottenet J , Mariet AS , Bonniaud P , Blot M , Tubert-Bitter P , et al. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. Lancet Respir Med. 2020.
39. Petersen E . COVID-19 is not influenza. Lancet Respir Med. 2020.
40. Zürcher K , Zwahlen M , Berlin C , Egger M , Fenner L . Losing ground at the wrong time: trends in self-reported influenza vaccination uptake in Switzerland, Swiss Health Survey 2007-2017. BMJ Open. 2021 Feb;11(2):e041354. https://doi.org/10.1136/bmjopen-2020-041354
41. Sullivan SG , Chilver MB , Carville KS , Deng YM , Grant KA , Higgins G , et al. Low interim influenza vaccine effectiveness, Australia, 1 May to 24 September 2017. Euro surveillance: bulletin Europeen sur les maladies transmissibles = European communicable disease bulletin. 2017;22(43).
42. Sah P , Medlock J , Fitzpatrick MC , Singer BH , Galvani AP . Optimising the impact of low-efficacy influenza vaccines. Proceedings of the National Academy of Sciences of the United States of America. 2018.
Table S1Grouping of the reasons for willingness or hesitancy to be vaccinated against COVID-19 or uncertainty about vaccination.
| Reasons for willingness to be vaccinated | |
| To protect myself from COVID-19 infection. | Protection (myself, patients, and relatives) |
| Because I want to protect my colleagues at work and my patients. | |
| Because I want to protect my family members (parents, siblings, children, etc.). | |
| Because my vaccination is a contribution to the fight against the pandemic. | Vaccine for pandemic control |
| Because this is the only way to stop the pandemic. | |
| Because I belong to the risk groups. | Risk group |
| Other reasons, please specify | Others |
| Reasons for hesitancy to be vaccinated | |
| I think vaccinations are generally unnecessary. | Opponents of vaccination |
| Vaccination against COVID-19 is not necessary. | COVID-19 is harmless |
| I don't think COVID-19 is dangerous for my health. | |
| COVID-19 is no worse than the flu. | |
| I don't think the vaccine is effective. | Effectiveness of the vaccine |
| I think the COVID-19 vaccine may not be safe. | |
| I am concerned that the vaccine was approved too quickly and has not been tested enough | Vaccine safety and side effects |
| I am afraid of possible side effects. | |
| I have had a bad experience or reaction to a previous vaccination | Bad experiences with vaccines |
| I had a bad experience with vaccinations at a previous physician or health clinic. | |
| I am afraid of needles. | Fear of needles |
| I am already protected because I comply with protective measures (masks, hand hygiene). | Personal protective equipment is sufficient |
| I protect my environment because I follow the protective measures, therefore vaccination is unnecessary. | |
| Because some colleagues do not want to be vaccinated either. | Other |
| Because the experts' opinions are inconsistent | |
| The best way is to let nature take its course. | |
| Religious reasons. | |
| Other reasons, please specify | Others |
| Reasons for being unsure about being vaccinated | |
| The information is inconsistent | Inconsistent information |
| The vaccines were too fast/quickly approved Swissmedic | Vaccine safety and side effects |
| I fear possible side effects. | |
| I don't know if the vaccination will provide protection for me and/or others. | Effectiveness of the vaccine |
| I don't know if my vaccination will help contain the pandemic (herd immunity). | Vaccine for pandemic control |
| My colleagues are also unsure or against vaccination. | Uncertainty of my colleagues |
| I have not yet been educated by my employer. | Education by employer |
| Other | Others |
| Information needed to take a decision | |
| General information about the disease COVID-19. | Information about COVID-19 |
| Information on the safety of the vaccination. | Information's about vaccine (safety, effectiveness, side effects) |
| Information about possible side effects of the vaccination. | |
| Information about the effectiveness of the vaccination (does it protect me?) | |
| Information about the vaccination procedure (e.g. how often vaccination is necessary). | |
| Experiences and reports from people who have already been vaccinated. | Reported experiences from vaccinated people |
| A statement from experts | Opinion by experts |
| Other | Others |
Table S2Participant characteristics by workplace.
| Total | Hospital | Medical practice | Nursing home | Home care organisation | Pharmacy | Long-term care facilities | |
| Total | 3,975 | 2,445 | 311 | 373 | 232 | 34 | 398 |
| Sex | |||||||
| Male | 952 (25.1) | 576 (23.6 | 164 (52.7) | 59 (15.8) | 15 (6.5) | 10 (29.4) | 128 (6.5) |
| Female | 2,841 (74.9) | 1,869 (76.4) | 147 (47.3) | 314 (84.2) | 217 (93.5) | 24 (70.6) | 270 (67.8) |
| Age in years, median (IQR) | 43 (31–53) | 40 (30–52) | 52 (44–60) | 46 (30–55) | 49.5 (38.5–57) | 49 (32–59) | 44 (31–55) |
| Profession | |||||||
| Medical doctor | 614 (16.2) | 372 (15.2) | 240 (77.2) | 0 | 0 | 0 | 2 (0.5) |
| Nurse | 1,690 (44.6) | 1,122 (45.9) | 6 (1.9) | 287 (76.9) | 193 (83.2) | 0 | 82 (20.6) |
| Medical assistant | 63 (1.7) | 0 | 58 (18.7) | 2 (0.5) | 2 (0.9) | 0 | 1 (0.3) |
| Other medical staff* | 380 (10.0) | 380 (15.5) | 0 | 0 | 0 | 0 | 0 |
| Pharmacist | 34 (0.9) | 0 | 0 | 0 | 0 | 24 (70.6) | 0 |
| Not close patient contact | 788 (20.8) | 571 (23.4) | 7 (2.3) | 84 (22.5) | 37 (16.0) | 0 | 89 (22.4) |
| Willingness to get COVID-19 vaccine | |||||||
| Yes | 1,511 (39.8) | 936 (38.3) | 226 (72.7) | 126 (33.8) | 79 (34.0) | 24 (70.6) | 120 (30.2) |
| No | 1,168 (30.8) | 726 (29.7) | 32 (10.3) | 137 (36.7) | 87 (37.5) | 6 (17.6) | 180 (45.2) |
| Unsure | 1,114 (29.4) | 783 (32.0) | 53 (17.0) | 110 (29.5) | 66 (28.5) | 4 (11.8) | 98 (24.6) |
| Follow my employer’s recommendation | |||||||
| Completely disagree | 443 (11.7) | 237 (9.7) | 15 (4.8) | 64 (17.2) | 44 (19.0) | 3 (8.8) | 80 (20.1) |
| Somewhat disagree | 623 (16.4) | 403 (16.5) | 32 (10.3) | 61 (16.4) | 47 (20.3) | 0 | 80 (20.1) |
| No opinion | 893 (23.5) | 584 (23.9) | 74 (23.8) | 101 (27.1) | 49 (21.1) | 8 (23.5) | 77 (19.4) |
| Somewhat agree | 742 (19.6) | 528 (21.6) | 41 (13.2) | 54 (14.5) | 43 (18.5) | 6 (17.7) | 70 (17.6) |
| Completely agree | 1,092 (28.8) | 693 (28.3) | 149 (47.9) | 93 (24.9) | 49 (21.1) | 17 (50.0) | 91 (22.9) |
| Confidence in the government reports | |||||||
| Completely disagree | 230 (6.1) | 129 (5.3) | 7 (2.3) | 37 (9.9) | 14 (6.0) | 0 | 43 (10.8) |
| Somewhat disagree | 638 (16.8) | 388 (15.9) | 33 (10.6) | 74 (19.8) | 48 (20.7) | 6 (17.7) | 89 (22.4) |
| No opinion | 645 (17.0) | 409 (16.7) | 31 (10.0) | 76 (20.4) | 47 (20.3) | 5 (14.7) | 77 (19.4) |
| Somewhat agree | 955 (25.2) | 645 (26.4) | 71 (22.8) | 74 (19.8) | 70 (30.2) | 11 (32.4) | 84 (21.1) |
| Completely agree | 1325 (34.9) | 874 (35.8) | 169 (54.3) | 112 (30.0) | 53 (22.8) | 12 (35.3) | 105 (26.4) |
| Influenza vaccine 20/21 | |||||||
| No | 2,229 (58.8) | 1364 (55.8) | 78 (25.1) | 262 (70.2) | 171 (73.7) | 11 (32.4) | 343 (86.2) |
| Yes | 1,446 (38.1) | 995 (40.7) | 222 (71.4) | 102 (27.4) | 58 (25.0) | 20 (58.8) | 49 (12.3) |
| Unsure | 118 (3.1) | 86 (3.5) | 11 (3.5) | 9 (2.4) | 1 (0.6) | 3 (2.4) | 6 (1.5) |
IQR = interquartile range
Data are n (%) unless otherwise stated.
* “Other medical staff” includes physical therapists, occupational therapists, speech therapists, and midwives.
Table S3Sensitivity analysis: Determinants for the willingness to be vaccinated against COVID-19 (yes/unsure) among healthcare workers compared with healthcare workers with hesitancy.
| Variables | Total num ber of participants | Willingness to be vaccinated against COVID–19: n (%) | Comparison of willingness to be vaccinated against COVID–19 (yes/unsure) with persons with hesitancy | ||||
| Yes | No | Unadjusted OR (95% Cl) | p–value | Adjusted OR (95% Cl)* | p–value | ||
| Total | 3,793 | 2,625 | 1,168 | ||||
| Sex | <0.001 | ||||||
| Male | 952 | 756 (79.4) | 196 (20.6) | 1 | |||
| Female | 2,841 | 1869 (65.8) | 972 (34.2) | 0.50 (0.42–0.59) | |||
| Age groups | <0.001 | <0.001 | |||||
| 29 and younger | 829 | 448 (54.0) | 381 (46.0) | 1 | 1 | ||
| 30 to 39 | 807 | 550 (68.2) | 257 (31.9) | 1.64 (1.33–2.03) | 1.48 (1.12–1.97) | ||
| 40 to 49 | 790 | 575 (72.8) | 215 (27.2) | 2.21 (1.79–2.73) | 1.70 (1.23–2.29) | ||
| 50 to 59 | 1012 | 758 (74.9) | 254 (25.1) | 2.61 (2.13–3.18) | 2.08 (1.58–2.73) | ||
| 60 and older | 355 | 294 (82.8) | 61 (17.2) | 4.56 (3.50–5.94) | 2.72 (1.79–4.13) | ||
| Profession | <0.001 | <0.001 | |||||
| Medical doctor | 614 | 559 (91.0) | 55 (9.0) | 6.22 (4.64–8.35) | 1.93 (1.31–2.84) | ||
| Nurse | 1,690 | 1,048 (62.0) | 642 (40.0) | 1 | 1 | ||
| Medical assistant | 63 | 44 (69.4) | 19 (30.2) | 1.42 (0.82–2.45) | 1.20 (0.56–2.57) | ||
| Pharmacist and pharmacist assistant | 34 | 28 (82.4) | 6 (17.6) | 2.86 (1.18–6.94) | 0.85 (0.26–2,79) | ||
| Other medical staff† | 380 | 287 (75.5) | 93 (24.5) | 1.89 (1.47–2.44) | 1.04 (0.73–1.47) | ||
| No close patient contact | 788 | 541 (68.6) | 246 (31.4) | 1.34 (1.12–1.61) | 0.62 (0.41–0.94) | ||
| Private caregiver | 224 | 118 (52.7) | 106 (47.3) | 0.68 (0.52–0.90) | 0.80 (0.62–1.04) | ||
| Confidence in the government reports | <0.001 | <0.001 | |||||
| No opinion | 645 | 407 (63.1) | 238 (36.9) | 1 | 1 | ||
| Completely and somewhat disagree | 868 | 335 (38.6) | 533 (61.4) | 0.37 (0.30–0.45) | 0.82 (0.62–1.09) | ||
| Completely and somewhat agree | 2,280 | 1,883 (82.6) | 397 (17.4) | 2.77 (2.29–3.36) | 1.59 (1.23–2.06) | ||
| Follow employer’s recommendation | <0.001 | <0.001 | |||||
| No opinion | 893 | 610 (68.3) | 283 (31.7) | 1 | 1 | ||
| Completely and somewhat disagree | 1,066 | 265 (24.9) | 801 (75.1) | 0.15 (0.13–0.19) | 0.17 (0.13–0.21) | ||
| Completely and somewhat agree | 1,834 | 1,750 (95.4) | 84 (4.6) | 9.67 (7.45–12.54) | 6.58 (4.94–8.76) | ||
| Influenza vaccination 20/21 | <0.001 | <0.001 | |||||
| No | 2,347 | 1,328 (56.7) | 1,019 (43.4) | 1 | 1 | ||
| Yes | 1,556 | 1,297 (89.7) | 149 (10.3) | 6.68 (5.53–8.06) | 2.48 (1.94–3.17) | ||
CI = confidence interval; OR = odds ratio
* Model adjusted for age groups, profession, confidence in the government reports, following employer's recommendation, and influenza vaccination 20/21.
† “Other medical staff” includes physical therapists, occupational therapists, speech therapists, and midwives.
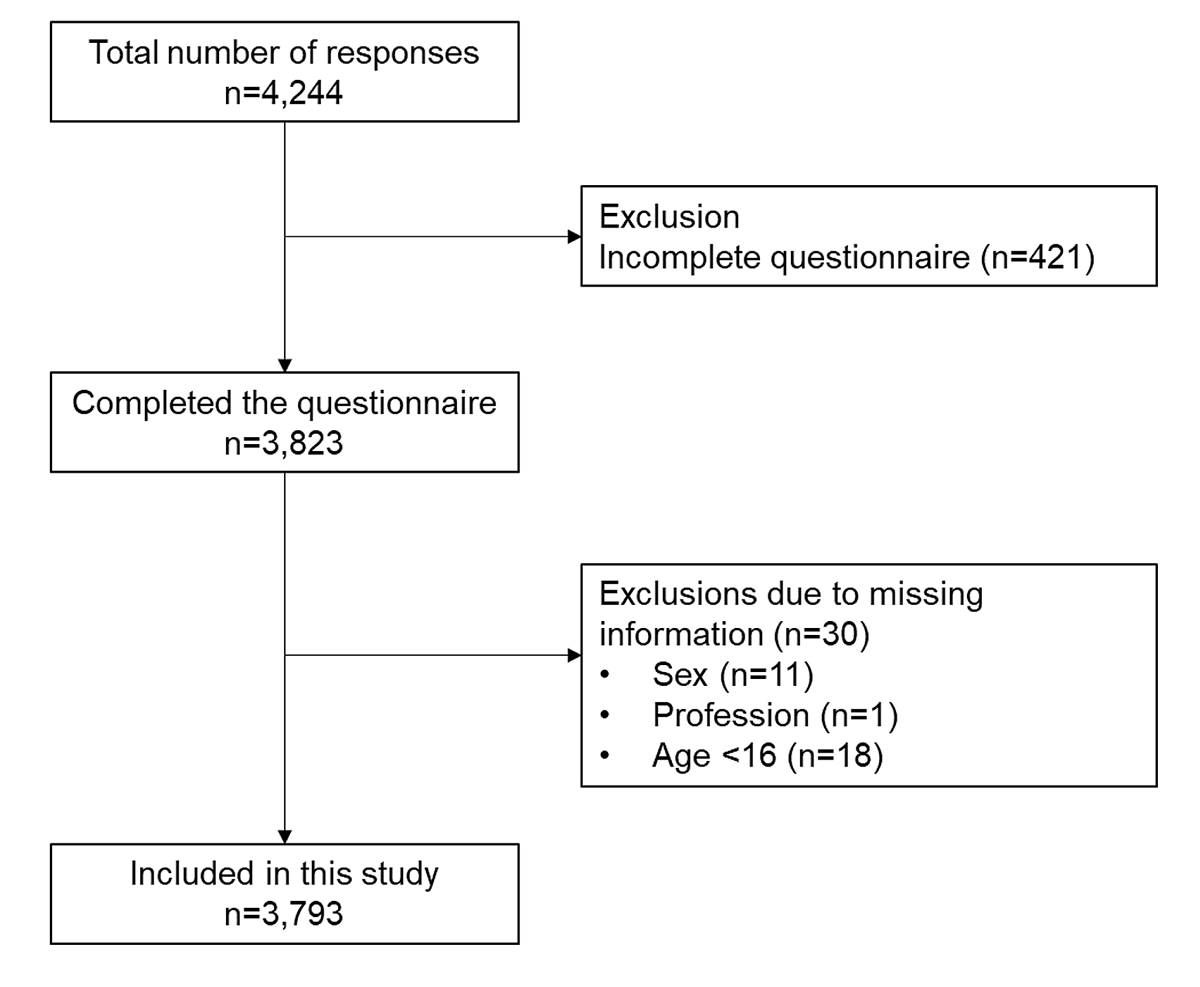
Figure S1 Study flow chart.