Evolution of disability pension after renal transplantation: methods and results of a database linkage study of the Swiss Transplant Cohort Study and Swiss Disability Insurance
DOI: https://doi.org/10.4414/SMW.2021.w30027
Sanda
Branca-Draganab, Michael T.
Kollerab, Brigitta
Danuserc, Regina
Kunzade, Jürg
Steigerabe, Balthasar L.
Hugafg, for the Swiss Transplant Cohort Study
aBasel University, Switzerland
bSwiss Transplant Cohort Study Team
cDépartement Santé, Travail, Environnement de l’Unisanté, UNIL, Lausanne, Switzerland
dSwiss National Accident Insurance Fund (SUVA), Lucerne, Switzerland
eBasel University Hospital, Switzerland
fLuzerner Kantonsspital, Lucerne, Switzerland
gLucerne University, Switzerland
* Shared first authorship
Summary
AIMS: In Switzerland, certain patients with disabilities and reduced working ability are entitled to a disability pension granted by the Swiss Federal Social Insurance Office (FSIO). The aim was to assess the evolution of disability pension and work capacity after kidney transplantation and thereby pilot the procedures linking FSIO data with Swiss Transplant Cohort Study (STCS) data.
METHODS: The current study pilot tested the record linkage of FSIO data with data from the STCS in a single-centre, observational setting. Patients were requested to consent to the use of their Swiss social security number (SSSN) for the purpose of record linkage. A privacy preserving trust centre approach was implemented with blinded statistical analysis.
RESULTS: Between May 2008 and December 2015, 282 working-age renal transplant recipients of the University Hospital of Basel transplant centre were eligible for inclusion and 136 (48%, median age 48 years) consented to the use of their social security number and record linkage. The FSIO datasets of all patients were successfully retrieved and linked to STCS data in the trust centre and were numerically analysable. Yearly FSIO allowance data were available for the entire study duration. Fifty-five patients (40%) were registered as disability insurance recipients (DIR). In the entire population, the proportion of working patients slightly decreased from 76% to 72% between the pre-transplant and the post-transplant period. This was due to the lower proportion of patients working after transplantation in DIR compared with non-recipients (non-DIR) (DIR: 60% before vs 44% after; non-DIR: 83% before vs 88% after). In the DIR group, the proportion of patients not working increased from 36% to 49%, whereas in non-DIR the proportion changed only marginally (14% to 12%). The average disability insurance allowance was CHF 1172 per month. It changed from CHF 1135 before transplantation to CHF 1209 after transplantation (p = 0.59).
CONCLUSIONS: In the Swiss healthcare and social insurance system, record linkage studies combining clinical datasets with data from FSIO are feasible but associated with great efforts and resource needs. The lack of changes in disability allowances after kidney transplantation should be further investigated in the nationwide setting.
ClinicalTrials.gov Number: NCT01204944
Abbreviations:
- DI
-
disability insurance (German: IV)
- DIR
-
disability insurance recipient
- EQ-5D VAS
-
European Quality of Life 5 Dimension Visual Analogue Scale
- FSIO
-
Federal Social Insurance Office (German: BSV)
- PSQ
-
psychosocial questionnaire
- SSSN
-
Swiss social security number (German: AHV)
- STCS
-
Swiss Transplant Cohort Study
Background
End-stage renal disease is common in the general population and is accompanied by a high prevalence of disability, morbidity and mortality [1]. A survey performed by Slakey et al. [2] showed that 81% of patients on dialysis feel disabled and 63% of kidney transplant recipients perceive themselves as disabled. It is one of the goals of transplantation to enable individuals with chronic kidney disease to return to work and to improve social participation. Research identified various factors that predict employment after transplantation, such as being employed before transplantation, higher education, a stable family environment, receiving a living donor transplant or pre-emptive transplantation.
In Switzerland, patients with disability and therefore limited capacity to work are entitled to a disability pension. The Swiss disability insurance is hosted at the Federal Social Insurance Office (FSIO). The DI aims to use rehabilitation measures or financial support to ensure the livelihoods of persons who suffer from disabilities [3]. The Swiss disability insurance evaluates the entitlement and the amount of a pension and re-evaluates these benefits at regular intervals. (As a note, throughout the manuscript pension and allowance are used as synonyms, but allowance refers to the amount of the pension.) In the setting of kidney transplantation, it is of particular interest that patients improve upon their degree of disability in the post-transplant period. This issue has already been studied in Switzerland by Eppenberger et al. [4–6], who found that living donor transplantation, pre-emptive transplantation, dialysis duration of less than a year, higher education and preserved employment before transplantation had a positive impact on post-transplantation employment, whereas dialysis with a duration of over one year and age over 50 had a negative impact.
The current work adds a record linkage study combining disability pension data from the FSIO with psychosocial and outcome data from the Swiss Transplant Cohort Study (STCS). Such record linkage is a procedure of general interest for Switzerland. It is important to note that in Switzerland there is no system for national patient identification in human research. The national unique patient identifier is the Swiss social security Number (SSSN - AHV number), but its use for research is not provided by law unless patients specifically consent. Record linkage therefore represents a challenging task.
The STCS is a nationwide prospective open multicentre cohort of all solid organ transplant recipients transplanted in Switzerland since May 2008 [7, 8]. The STCS is the national infrastructure for transplantation outcome research in Switzerland. The STCS has gained international recognition because of the high granularity of its data and high-quality long-term follow-up. The rationale and design of the STCS are detailed elsewhere [7].
Materials and methods
Aims
Our study had two major aims. The first was to assess the feasibility of record linkage of the Swiss disability insurance data from the FSIO with data from the STCS on the individual patient level. The feasibility focused on (1) investigating the willingness of patients to consent to the use of their SSSN and to further use disability pension data for research, (2) developing a privacy-preserving and secure method for the use of the SSSN in conformity with the Swiss data protection regulations and (3) assessing whether Swiss disability insurance data from the FSIO are suitable for data analysis and research. The second aim was to perform a “proof of concept” observational data analysis using the two linked datasets to assess pre- versus post-transplant evolution of disability allowances and work capacity after transplantation.
Study design and participants
We performed a single centre observational study nested within the STCS. To provide the proof of concept for our record linkage approach and to test the analysability of the linked data, we designed our project a priori as a “pilot study” restricted to the transplant centre of the University Hospital of Basel. Eligible patients were renal allograft recipients aged between 20 and 60 years from the University Hospital of Basel transplanted between May 2008 and the end of 2015 with each patient having at least 2 years of prospective follow up. Data from FSIO were provided from 2005 to the end of 2014 and are shown for the entire reporting period.
Record linkage and blinded data analysis
All consenting patients agreed to have their SSSN retrieved from the hospital information system. The key principle of our record linkage approach was to preserve patient privacy throughout all data processing steps. That meant proper encoding of health related personal data was maintained during record linkage and only authorised employees were allowed to see and manage SSSNs of enrolled patients. Figure 1 (below) displays the method. The study protocol defined the inclusion criteria. The STCS data centre derived a list of patients who fulfilled the criteria and solely transferred the STCS-specific unique patient identifiers to the University Hospital of Basel transplant centre. Since employees at the University Hospital of Basel are involved in patient care directly, they are authorised to access the SSSN and, with consent of the patient, to create the mapping file linking the SSSNs with the STCS-specific patient identifier. The mapping file containing only identifiers was securely transferred to FSIO. They retrieved the sensitive disability insurance data, removed the SSSN and sent the data to the CTU Basel. It acted as “trust centre” and merged the FSIO data with the STCS data based on the STCS-specific identifier. All data analyses were done in a blinded way within the Clinical Trial Unit Basel trust centre. The analyses were programmed by the STCS data centre and executed by the trust centre only. Both the STCS and the FSIO signed a legal agreement on patient privacy, data security and the exclusive use of data for research and quality control.
Description of data sources
The two sources of data were the STCS database and the FSIO database. The STCS data comprised gender, age, donor type, previous transplantations, underlying end stage renal disease, allograft function and patient survival, as well as data from the patient-reported STCS psychosocial questionnaire (PSQ) [9] containing information on marital status, education, income, primary occupation, work capacity, self-reported health status, self-care and mobility [7]. The FSIO provided the data per patient for the month of December of each year (from 2005 until 2015) [10]. The data originated from the local social security office and contained the following information: marital status, canton of residence and disability and/or helplessness allowance. For disability pensions, the following information was included: pension type, pension part (100%, 75%, 50%, 25%), new pensions, additional pension for spouses, additional pension for children, supplementary pensions, disorder accounting for disability insurance pension, and functional deficit code (see table 3). If not stated otherwise, we always reported the first payment in a row of several yearly December payments reports. Of note, the amount of a full disability insurance pension in Switzerland varies between CHF 1185 and CHF 2370.
Outcome measures
Feasibility: proportion of eligible patients consenting to record linkage using the SSSN and the further use of FSIO data for research; narrative description of work load and challenges.
Proof of concept for record linkage and evaluation of the data: Pre- and post-transplant disability pensions and monthly payments reported per annum; patient self-reported pre- and-post-transplant work capacity and health related quality of life as evaluated by the STCS PSQ. We used the closest assessment before transplantation and the 24-month time-point for STCS post-transplant evaluations; the 24-month PSQ data were missing in some cases and the 12-month evaluation (five patients, 9%) or 6-month evaluation (one patient, 1.8%) was used instead.
Statistical analysis
To comply with our privacy preserving approach, all analysis scripts were developed in R (statistical computing software) on mock data with identical variable names. The code was then transferred to the trust centre (CTU Basel) for execution and the aggregated results were sent back to the study team (see fig. 1). All feasibility aspects of our study are reported in a descriptive or narrative way. For the quantitative aspects of this study, we used primarily descriptive analysis methods, tables with summary statistics of STCS data (baseline characteristics) and FSIO data with frequencies, medians and interquartile ranges (IQRs) and counts of missing data. The analysis also included graphical representation to show the pre- to post-transplant development and longitudinal analysis of disability pension data. A paired t-test was used for the comparison of pre- and post-transplantation DIR pension means. Because of the descriptive nature of the project, no other inferential statistical methods were used.
Ethics approval
For the STCS in general, patients provide consent in writing to participation, collection and further use of STCS data for research (EKNZ BASEC 2018-02394). The responsible ethics committees of all the transplant centres approved the STCS. All regulatory documents and processes are in accordance with the Swiss Human Research Act. For the current study, eithics committee approval was sought from the Ethics Committee of Northwestern Switzerland (EKNZ BASEC 2016-00846). All analysed patients consented in writing to this study and in particular to the use of the SSSN for record linkage. The consent of patients who died during the study period was waived by the above mentioned ethics committee on grounds of the general STCS consent provided by these patients.
Results
Record linkage as shown in figure 1 was feasible; however, it took approximately 2 years to obtain all ethics and legal approvals.

Figure 1 Privacy preserving approach for record linkage and blinded analysis in 136 consenting STCS renal transplant recipients from the transplant centre Basel.
All participating institutions are shown with their respective available data. The blue boxes show which data were exchanged at the patient individual level. The red boxes show the exchange of the analysis script or the analysis report. Data were exchanged in an encrypted way. CTU Basel provided the necessary infrastructure and instructions for further data transmissions. At CTU Basel, data were stored locally only in encrypted form. Any access to data is regulated and documented individually.
SSSN: Swiss social security number (AHV number: Alters- und Hinterbliebenen Versicherung Nummer); CTU: clinical trial unit; ID: identity; STCS: Swiss Transplantation Cohort Study; FSIO: Federal Social Insurance Office (ref); USB: University Hospital Basel
Out of 3309 patients transplanted nationwide between May 2008 and December 2015 who consented to participate in the STCS, 282 working-age renal transplant recipients of the Basel transplant centre were eligible for inclusion and were contacted in writing for study participation (fig. 2). Seven patients explicitly refused consent and informed consent could not be obtained from 139 recipients: 107 did not respond, 15 moved away and in 17 patients various reasons (no signature, language/comprehension/health problems, birthdate entry error, one non-Swiss citizen without an SSSN) led to absence of consent. Hence, a total of 136 patients out of 282 (48%) were included in our study. Written informed consent was provided by 128 patients and in 8 deceased patients the data could be re-used according to the exception clause of the Federal Human Research Act (waiver by ethics committee review board, see above).

Figure 2 Candidate patient population (n = 282) divided by study participants (disability insurance recipients and non-recipients) and non-participants (consent not obtained or refused).
According to the data available from FSIO for payments made between 2005 and 2014, 55 out of 136 patients (40.4%) were registered as disability insurance recipients (DIR) and received at least one type of payment (fig. 2). Fifty-four patients had at least one disability pension, four patients had at least one helplessness allowance and three patients had both types of pension.
The baseline patient characteristics are shown in table 1. The median age was 48 years at the time of the study. Compared with transplanted patients who did not receive DI allowances, those who did were proportionally more female (48.1% vs 33.3%), more often not married (71.6% vs 54.5%), had more often undergone more than one transplantation (36.4% vs. 11.1%), more often had received deceased donor transplants (69.1% vs 23.5%) and less often a living donor organ (30.9% vs 76.6%).
Table 1Baseline and clinical characteristics from the Swiss Transplant Cohort Study stratified by disability insurance recipients (DIR) and non-recipients (non-DIR).
|
DIR (n = 55)
|
Non-DIR (n = 81)
|
| Recipient age (years), median (IQR) |
|
48 (41–57) |
48 (37–54) |
| Gender, n (%) |
Female |
23 (41.8%) |
27 (33.3%) |
| Donor type, n (%) |
Deceased |
38 (69.1%) |
19 (23.5%) |
| Living |
17 (30.9%) |
62 (76.5%) |
| Previous transplantation, n (%) |
Yes |
20 (36.4%) |
9 (11.1%) |
| Underlying kidney disease, n (%) |
Congenital |
2 (3.6%) |
1 (1.2%) |
| Diabetes mellitus nephropathy |
12 (21.8%) |
3 (3.7%) |
| Glomerulonephritis |
19 (34.5%) |
28 (34.6%) |
| Hereditary non-polycystic kidney disease |
1 (1.8%) |
2 (2.5%) |
| Interstitial nephritis |
3 (5.5%) |
5 (6.2%) |
| Nephrosclerosis |
3 (5.5%) |
7 (8.6%) |
| Polycystic kidney disease |
5 (9.1%) |
18 (22.2%) |
| Previous graft failure |
2 (3.6%) |
2 (2.5%) |
| Reflux/pyelonephritis |
4 (7.3%) |
9 (11.1%) |
| Other |
3 (5.5%) |
3 (3.7%) |
| Missing |
1 (1.8%) |
3 (3.7%) |
The underlying kidney diseases were similar for patients who received DI allowances and those who did not, except for diabetic nephropathy, which was more prevalent (21.8% vs 3.7%) and polycystic kidney disease, which was less prevalent (9.1% vs 22.2%, see table 1).
Overall, the patient self-reported working capacity (table 2) indicated that the proportion of working patients in the pre-transplant period (76%) decreased to 72% in the post-transplant period. This was due to the lower proportion working after transplantation in DIR compared with non-DIR (DIR: 60% before vs 44% after; non-DIR: 83% before vs 88% after). More patients had part-time occupations (≤50% employment) in the DIR group than in the non-DIR group and this proportion decreased in both groups after transplantation (DIR: 42% vs. 22%; non-DIR: 30% vs 12%). In the DIR group, the proportion of patients not working increased from 36% to 49% whereas in the non-DIR this proportion decreased from 14% to 12%. The median health related quality of life score (health status EQ-5D VAS) pre-transplantation in the DIR group was 60 compared with 70 in the non-DIR group. After -transplantation the median health status was 74.5 for DIR compared with 90 for non-DIR.
Table 2Psychosocial characteristics from Swiss Transplant Cohort Study psychosocial questionnaire evaluations stratified by disability insurance recipients (DIR) and non-recipients (non-DIR).
|
DIR (n = 55)
|
Non-DIR (n = 81)
|
|
|
Pre-TX
|
Post-TX
|
Pre-TX
|
Post-TX
|
| Work capacity (in %), n (%) |
> 80% |
4 (7.3%) |
7 (12.7%) |
34 (42%) |
51 (63%) |
| 51–80% |
6 (10.9%) |
5 (9.1%) |
9 (11.1%) |
10 (12.3%) |
| 21–50% |
22 (40%) |
9 (16.4%) |
19 (23.5%) |
7 (8.6%) |
| 1–20% |
1 (1.8%) |
3 (5.5%) |
5 (6.2%) |
3 (3.7%) |
| 0% |
20 (36.4%) |
27 (49.1%) |
11 (13.6%) |
10 (12.3%) |
| Refused |
0 (0%) |
1 (1.8%) |
0 (0%) |
0 (0%) |
| Missing |
2 (3.6%) |
3 (5.5%) |
3 (3.7%) |
0 (0%) |
| EQ-VAS heath status |
Median (IQR) |
60 (50–71) |
74.5 (60–80) |
70 (50–80) |
90 (80–95) |
| Missing, n (%) |
4 (7.3%) |
5 (9.1%) |
2 (2.5%) |
2 (2.5%) |
| Self-care, n (%) |
No problems |
50 (90.9%) |
47 (85.5%) |
78 (96.3%) |
80 (98.8%) |
| Some problems |
4 (7.3%) |
4 (7.3%) |
2 (2.5%) |
1 (1.2%) |
| Missing |
1 (1.8%) |
4 (7.3%) |
1 (1.2%) |
0 (0%) |
| Mobility, n (%) |
No problems |
35 (63.6%) |
28 (50.9%) |
67 (82.7%) |
74 (91.4%) |
| Some problems |
19 (34.5%) |
23 (41.8%) |
12 (14.8%) |
7 (8.6%) |
| Missing |
1 (1.8%) |
4 (7.3%) |
2 (2.5%) |
0 (0%) |
| Primary occupation, n (%) |
Apprentice |
0 (0%) |
|
1 (1.2%) |
|
| Employee |
18 (32.7%) |
|
35 (43.2%) |
|
| Family business |
2 (3.6%) |
|
1 (1.2%) |
|
| Housewife/man |
10 (18.2%) |
|
10 (12.3%) |
|
| Invalidity pensioner |
3 (5.5%) |
|
0 (0%) |
|
| Lower management |
5 (9.1%) |
|
9 (11.1%) |
|
| Management |
0 (0%) |
|
5 (6.2%) |
|
| Self-employed |
4 (7.3%) |
|
11 (13.6%) |
|
| Student, scholar |
1 (1.8%) |
|
1 (1.2%) |
|
| Other |
8 (14.5%) |
|
7 (8.6%) |
|
| Missing |
4 (7.3%) |
|
1 (1.2%) |
|
| Marital status, n (%) |
Married |
30 (54.5%) |
|
58 (71.6%) |
|
| Other |
24 (43.6%) |
|
22 (27.2%) |
|
| Missing |
1 (1.8%) |
|
1 (1.2%) |
|
Table 3 provides a summary of the data provided by the FSIO. Out of 54 patients who received an allowance, the majority (92.6%) had an ordinary allowance and 61.1% had a full allowance. Disorders accounting for the pension were mostly kidney and urinary tract disorders (70.4%). The aetiology of the functional deficit was split between impairment of general condition (44.4%), disorders of kidney function (31.5%) and other deficits (24.1%). Thirty-five (64.8%) patients received a new allowance during the observation period. The median disability allowance was CHF 1253 (IQR 884.5–1833.5). Only 18.5% of patients received an additional allowance for spouses and 25.9% an additional pension for children. The median helplessness allowance received by four patients was CHF 449.
Table 3Summary of data from the Federal Social Insurance Office for the study period of 2005 to 2015.
| Disability insurance (DI) pension only |
n = 54 |
| Pension type, n (%) |
Ordinary pension |
50 (92.6%) |
| Extraordinary pension |
4 (7.4%) |
| Pension part, n (%) |
Half pension |
17 (31.5%) |
| Full pension |
33 (61.1%) |
| Other |
4 (7.4%) |
| Disorder accounting for DI pension, n (%) |
Kidney and urinary tract disorders |
38 (70.4%) |
| Diabetes mellitus |
5 (9.3%) |
| Other |
11 (20.4%) |
| Type of functional deficit, n (%) |
Impairment of the general condition |
24 (44.4%) |
| Disorders of the kidney functions |
17 (31.5%) |
| Othera
|
13 (24.1%) |
| New pension during study period, n (%) |
Yes |
35 (64.8%) |
| Disability pension amount (CHF) |
Median (IQR) |
1253 (884.5–1833.5) |
| Additional pension for spouses, n (%) |
Yes |
10 (18.5%) |
| Additional pension for children, n (%) |
Yes |
14 (25.9%) |
| Disability and child pensions (CHF) |
Median (IQR) |
1453 (907.2–2092) |
| Disability and supplementary pensions (CHF) |
Median (IQR) |
1483.5 (946.8–2092) |
| Helplessness allowance pension recipientsb
|
|
4 |
| Helplessness allowance pension amount (CHF) |
Median (IQR) |
449 (439–459) |
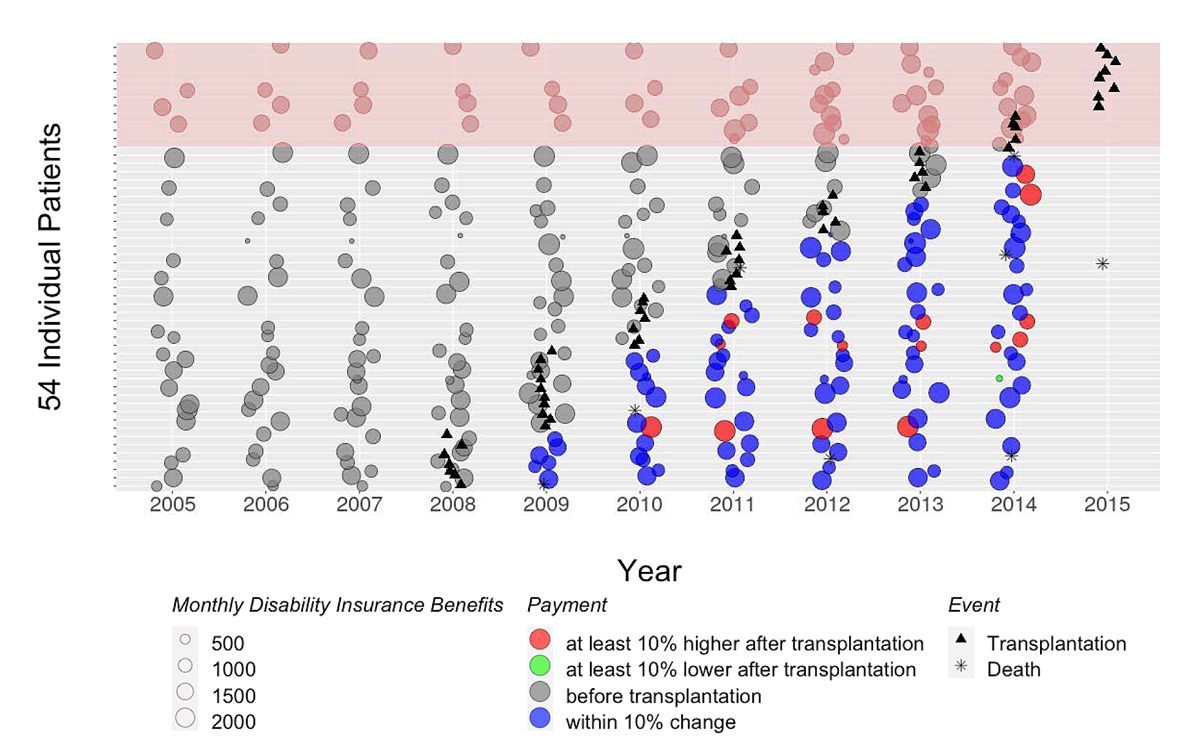
Figure 3 shows the longitudinal graphical representation of the monthly disability insurance allowance by calendar year. Only 39 of 54 patients had both pre- and post-transplant data available. In 15 patients, the payments were stopped during the observation period (in 7 patients, payments were stopped because of death). Eleven patients had no pre-transplant payments but received payments after transplantation. Only one patient had a decrease of more than 10% in payments after transplantation (fig. 3, green), whereas six patients had at least one payment 10% higher after transplantation (fig. 3, red). Two patients died within 1 year after transplantation. In summary, the overall average disability insurance allowance was CHF 1172 per month. The monthly disability insurance allowance was CHF 1135 before and CHF 1209 after transplantation (p = 0.59 from paired t-test).
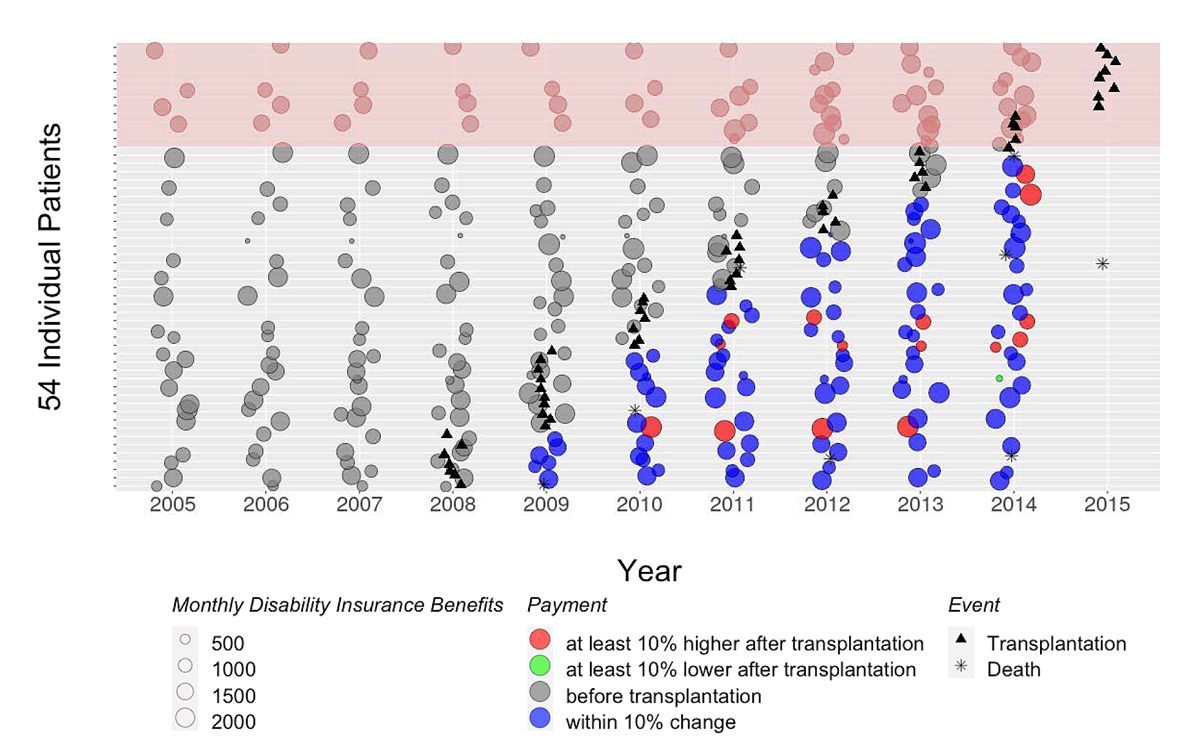
Figure 3 Disability insurance benefits for all 54 recipients as reported by FISO (2005 to 2014). Each white horizontal line belongs to one patient, the bubbles represent the monthly disability allowance (pension), the triangles show the year of transplantation of a given patient and the asterisk the year of death if applicable. The size of the bubble represents the amount of the monthly pension. Each payment after transplantation was compared to the last payment before transplantation and color coded. Blue: less than 10% change of the monthly allowance post-transplant. Red: increase of the allowance of more than 10%. Green: decrease of the allowance by more than 10% after transplantation. The lines highlighted on top in pink emphasise those 13 patients transplanted in 2015 for whom FSIO data is not available after transplantation.
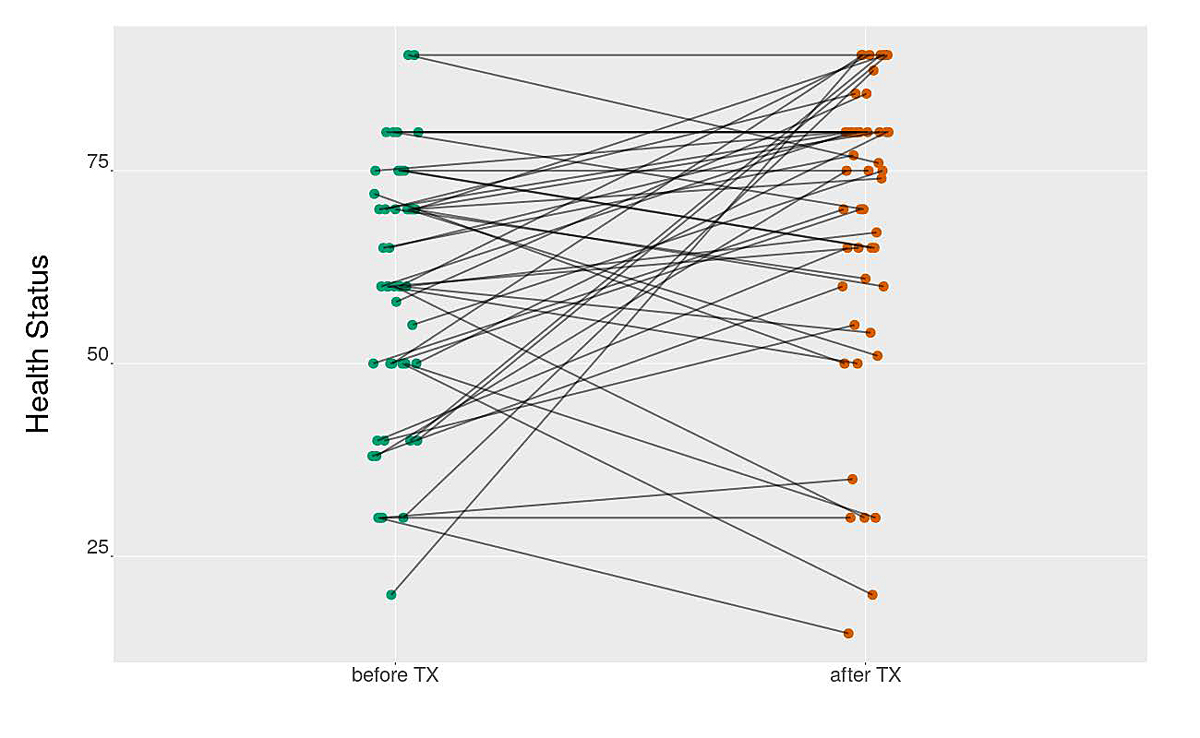
Figure 4 shows the pre- to post-transplant evolution of the health-related quality of life (EQ-5D VAS). Only 47 out of 55 DIR had both a pre- and post-transplant health status, 57% reported an increase in health-related quality of life, 30% a decrease in quality of life and 13% reported no change.
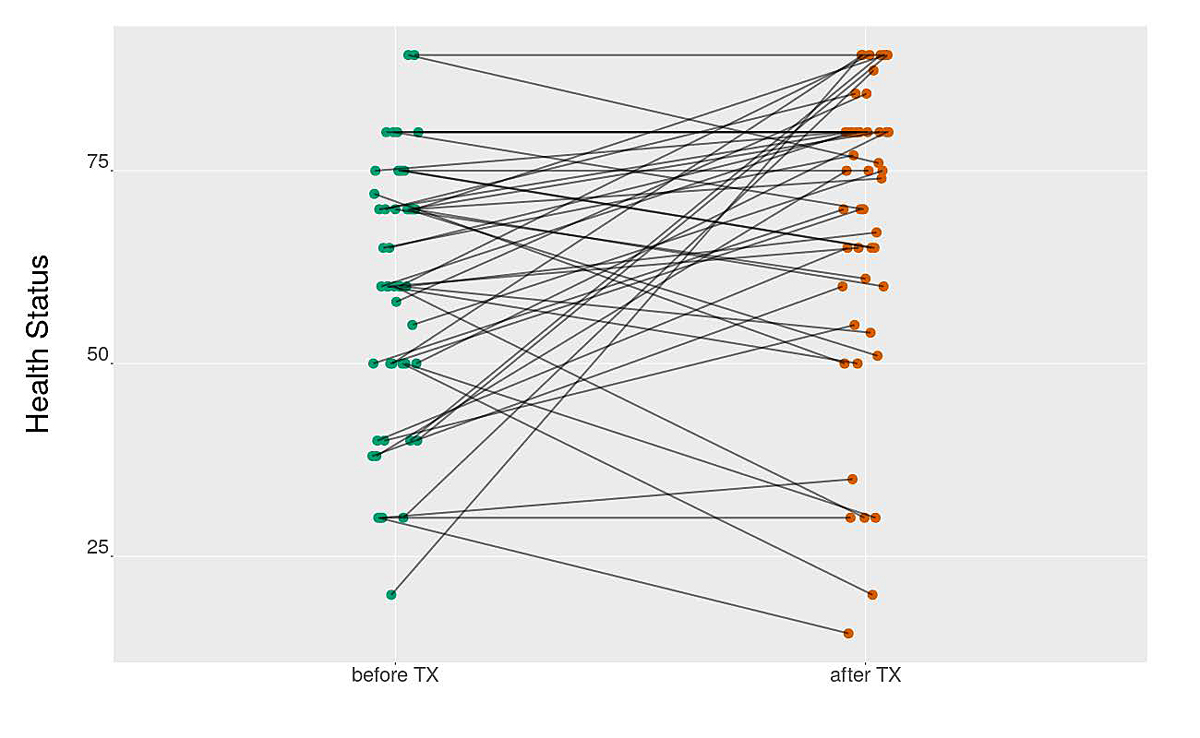
Figure 4 Self-reported health-related quality of life (EQ-5D VAS) before and 24 months after transplantation (n = 47).
Discussion
Our study shows that record linkage from the two fully independent institutions (STCS and FSIO) is feasible and that the merged datasets can be used for quantitative scientific analyses in the context of health service and potentially different social insurance research. Hence, similar projects on the national level and beyond transplantation medicine are possible. However, the efforts are substantial. They are primarily bound to the patient consent procedure, to the challenging privacy-preserving database linkage approach and to the blinded analysis developed on mock data and performed in collaboration with a trust centre. Nevertheless, the important finding was that around half of all patients were willing to provide their SSSN and agreed to the re-use of sensitive data on disability pensions for research, given the rigorous privacy protection measures implemented in our study.
The main challenge for this study were the ethics and legal requirements needed, next to patient data protection for pulling the data, transfer and linkage of the two databases. These preparations, meetings and documentation took more than 2 years of working as a highly efficient team. Results like the ones presented here in this pilot study are badly needed on a national level in order to evaluate psycho-social and economic consequences of organ transplantation. Thus, faster and more efficient ways are needed to facilitate such analyses while preserving patient data protection. In order to speed up the current bureaucratic procedures we suggest the following. (1) We not only got the ethics committee approval but had to get a legal contract for linking the databases. We suggest a lean process with one encompassing ethics approval only. (2) All patients included in the STCS signed an approval that their data may be used for research. Patients have a possibility to decline at this point. The ethics procedures asked us to contact all patients once more on a personal basis to get a second approval. We suggest working with one patient approval only, making this process lean and efficient. (3) Reaction times, above all in the legal field, were prolonged. Additionally to point (1,) we suggest fixing a mandatory return time between researchers and legal teams for requests so as not to prolong any processes.
The results of the pilot study using the linked datasets provides some first evidence that transplantation has not yet been able to achieve the expected positive effects on work ability and reduction of disability insurance allowances. This is not surprising given the complex dependency on numerous factors: pre-transplant employment, sociodemographic characteristics, clinical conditions and comorbidities, operative technique (invasive or not), type of transplant (living donor or cadaver), pre-transplant dialysis, psychosocial support, educational level and participation in education programmes [11]. In the DIR population, a decrease in working ability was observed in the post-transplant observation period, whereas in the non-DIR subset, working ability and capacity was increased or remained similar after transplantation. Here one could argue that the non-DIR subset of patients must have a positive selection bias regarding working ability due to the factors discussed above and the fact that they did not need any pension in the first place. However, our study was designed as a pilot study and further evidence on a larger and more representative population is needed to draw in depth conclusions about this important topic.
A recent study from Austria confirmed that self-assessed mental health,work ability and quality of life were significantly associated with employment after renal transplantation [12]. Earlier studies revealed that about 60% of patients perceive themselves to be able to work full- or part-time after renal transplantation but only 30–40% will do so [13]. Therefore, identification of the disability pension situation and transplantation characteristics that favour post-transplant employment is an important area for research. A survey by Eng et al. (2012) showed that among patients <65 years of age, 56% were employed after renal transplantation [14]. Furthermore, early referral (age <50 years, <2 years of dialysis or pre-dialysis) as well as pre-transplant employment are favourable predictors for employment after transplantation [5, 14]. Race, marital status, previous transplantation and complicated postoperative course do not seem to influence post-transplant employment [5, 14]. These studies were conducted abroad, above all in the USA with regard to local insurance services such as Medicare and Medicaid. Similar to our results, STCS pre- and post-transplant analyses from Danuser et al. and by Eppenberger et al. showed that being older and having no professional education plus symptoms of depression from patients’ perceived health status were significantly correlated with not working before transplantation [4, 5]. Severity of the disease was statistically significant in explaining the pre-transplant working status in kidney patients only. The longer the patient was on dialysis, the higher the risk of not returning to gainful employment [5, 6]. Hence, physical disability and work incapacity are decisive components that impact on the social and economic welfare of patients with renal insufficiency. Financial security may also play a role. For example, a dialysis patient with 100% work incapacity and full disability insurance pension, after transplantation with better health and lower disability insurance pension, but still without work, is financially worse off than during the dialysis period due to the new and expensive immunosuppressants.
Our study has several limitations. First, due to its feasibility nature, the time frame to observe changes in pension allowances and work capacity after transplantation was limited to a relatively short period. Second, in line with the feasibility nature of the study and around 50% consent rate, the sample was rather small and our findings need urgent validation in a larger sample and broader domain of transplantation medicine or other fields of complex care. However, it is important to say that also big data return to work studies always represent a proportionally small number of individuals owing to missing data or exclusion of a large number of records (problem also discussed in Danuser et al. 2017 [5]). Although a rigorous data safety concept was applied, a low consent rate was observed, which may indicate patients` scepticism about this type of study. Moreover, the small study sample may limit the representativeness of our results. Third, in depth evaluations on the availability and analysability of disability assessment data or on the decision-making processes for when and why changes to the allowances were made would be of great interest. For example, in the current project it was unknown whether the fact of transplantation was considered in the re-evaluation of the future pension need and amount of pension allowances. Information on the current employment status for partially disabled persons was not available from FSIO and would need to be clarified. Moreover, to fully guarantee data privacy of included patients in the situation of a small dataset, the blinded analyst should be a completely independent third party without access to the primary research dataset.
Conclusions
Database linkage studies combining clinical data with data from the Swiss disability insurance are feasible for research and quality of care control, but require some important hurdles to be overcome. Also, our blinded analysis approach in collaboration with the trust centre was successful but used substantial resources. These findings need to be considered when planning a nationwide study in this subject area. The participation rate after a one-time participation request was below 50% but may potentially be improved with appropriate reminders.
Acknowledgements
This study was conducted in the framework of the Swiss Transplant Cohort Study (STCS). The STCS is funded by the Swiss National Science Foundation (SNSF) Grant 33CS30_177522, Unimedsuisse and the transplant centres.
We thank the members of FSIO for their collaboration in the study.
We thank Juliane Rick for supporting the data management. We thank Thomas Fabbro and Thomas Zumbrunn for the data merging concept and to act as trust center.
Author contributions: BLH and SBD wrote the manuscript, performed research and participated in the study design, SBD performed the statistical analyses, BLH and MK reviewed and critically revised the manuscript and contributed to the study design. All co-authors provided critical feedback and have given final approval of the manuscript.
Prof. Balthasar L. Hug, MBA, MPH
Head of Division of Internal Medicine
Spitalstrasse
CH-6000 Lucerne
balthasar.hug[at]luks.ch
References
1.
Levey AS
,
Coresh J
. Chronic kidney disease. Lancet. 2012 Jan;379(9811):165–80. https://doi.org/10.1016/S0140-6736(11)60178-5
2.
Slakey DP
,
Rosner M
. Disability following kidney transplantation: the link to medication coverage. Clin Transplant. 2007 Mar-Apr;21(2):224–8. https://doi.org/10.1111/j.1399-0012.2006.00629.x
3.
https://www.ahv-iv.ch/en/Social-insurances/Disability-insurance-DI
4.
Eppenberger L
,
Hirt-Minkowski P
,
Dickenmann M
. Back to work? Socioeconomic status after kidney transplantation. Swiss Med Wkly. 2015 Jul;145:w14169. https://doi.org/10.4414/smw.2015.14169
5.
Danuser B
,
Simcox A
,
Studer R
,
Koller M
,
Wild P
; Psychosocial Interest Group, Swiss Transplant Cohort Study
. Employment 12 months after kidney transplantation: an in-depth bio-psycho-social analysis of the Swiss Transplant Cohort. PLoS One. 2017 Apr;12(4):e0175161. https://doi.org/10.1371/journal.pone.0175161
6.
Vieux L
,
Simcox AA
,
Mediouni Z
,
Wild P
,
Koller M
,
Studer RK
, et al.; Swiss Transplant Cohort Study
. Predictors of Return to Work 12 Months After Solid Organ Transplantation: Results from the Swiss Transplant Cohort Study. J Occup Rehabil. 2019 Jun;29(2):462–71. https://doi.org/10.1007/s10926-018-9804-8
7.
Koller MT
,
van Delden C
,
Müller NJ
,
Baumann P
,
Lovis C
,
Marti HP
, et al.
Design and methodology of the Swiss Transplant Cohort Study (STCS): a comprehensive prospective nationwide long-term follow-up cohort. Eur J Epidemiol. 2013 Apr;28(4):347–55. https://doi.org/10.1007/s10654-012-9754-y
8.
Branca-Dragan S
,
Koller M
,
Stampf S
,
Rick J
,
Mellac K
,
Rossi S
, et al.
Steiger J; on behalf of all members of the STCS. Swiss Transplant Cohort Study report. Swiss Transplant Cohort Study. http://www.stcs.ch/research/publications. Published 2019. Updated 1 June2020. Accessed 2020 June 1.
9.
De Geest S
,
Burkhalter H
,
Berben L
,
Bogert LJ
,
Denhaerynck K
,
Glass TR
, et al.; Psychosocial Interest Group, Swiss Transplant Cohort Study
. The Swiss Transplant Cohort Study’s framework for assessing lifelong psychosocial factors in solid-organ transplants. Prog Transplant. 2013 Sep;23(3):235–46. https://doi.org/10.7182/pit2013250
10.
https://sozialversicherungen.admin.ch/de/d/6411/download?version=1
11.
D’Egidio V
,
Mannocci A
,
Ciaccio D
,
Sestili C
,
Cocchiara RA
,
Del Cimmuto A
, et al.
Return to work after kidney transplant: a systematic review. Occup Med (Lond). 2019 Oct;69(6):412–8. https://doi.org/10.1093/occmed/kqz095
12.
Jordakieva G
,
Grabovac I
,
Steiner M
,
Winnicki W
,
Zitta S
,
Stefanac S
, et al.
Employment Status and Associations with Workability, Quality of Life and Mental Health after Kidney Transplantation in Austria. Int J Environ Res Public Health. 2020 Feb;17(4):E1254. https://doi.org/10.3390/ijerph17041254
13.
McGee J
,
Jackson NR
,
Slakey DP
. Disability and kidney transplantation in the United States. Clin Transplant. 2012 May-Jun;26(3):377–81. https://doi.org/10.1111/j.1399-0012.2012.01612.x
14.
Eng M
,
Zhang J
,
Cambon A
,
Marvin MR
,
Gleason J
. Employment outcomes following successful renal transplantation. Clin Transplant. 2012 Mar-Apr;26(2):242–6. https://doi.org/10.1111/j.1399-0012.2011.01441.x