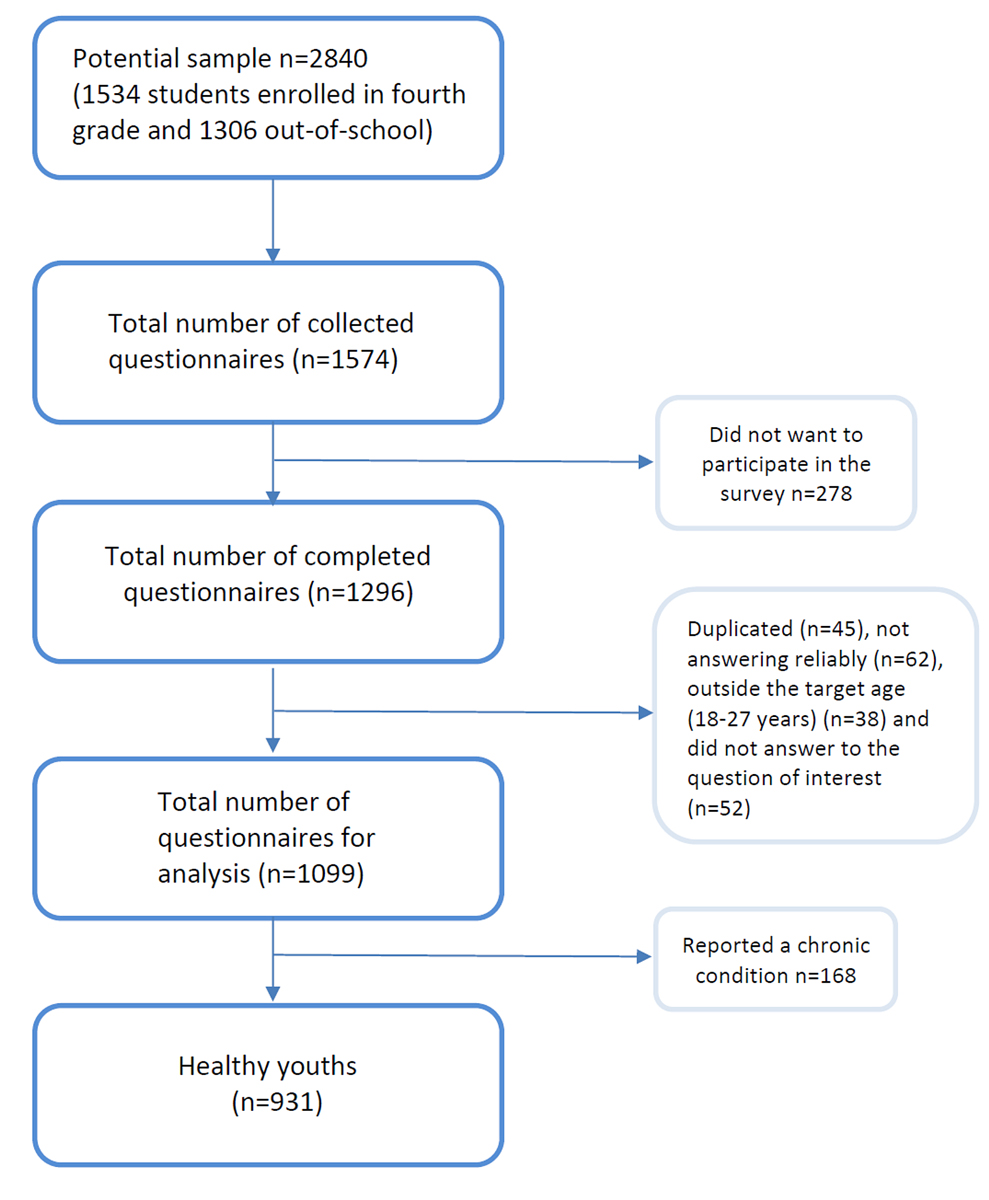
Figure 1 Flowchart showing the sampling technique.
DOI: https://doi.org/10.4414/SMW.2021.w30019
Transition is defined as the purposeful, planned movement for adolescents and young adults with chronic physical and medical conditions from a child-centered to an adult-oriented health system [1]. Thus, most transition studies have been performed among youths with chronic conditions. However, all adolescents have to go through a transition process to adult health care at some point [2].
Adolescence is a critical period of development and the aim of a planned transition is to maximise lifelong functioning and well-being for all young people, regardless of whether they have a chronic condition or not [3]. Since many diseases and poor lifestyle habits begin during adolescence, it is important to identify and address these health-related issues early to reduce their prevalence in adulthood [4].
Transition from paediatric to adult care among healthy youths is little studied [5], and most of the studies have been conducted in the United States [6–9], with a healthcare system very different from the Swiss one.
In a national survey in the United States, Lebrun-Harris et al. [7] found that 17% of youths with chronic conditions and 14% of healthy ones had made an overall transition. According to this study, youths with chronic conditions were more likely to receive personalised information on transition planning than their healthy peers. These authors also established that having a private insurance was associated with a higher rate of complete transition, and that healthy youths whose parents had lower levels of education were associated with a higher rate of discussion about transition to adult care. In contrast, Wisk et al. [9] demonstrated that the lapse between the last visit to a paediatrician and the first visit to an adult healthcare provider was longer for young people living in low-income areas.
Emerging adulthood is a vulnerable period in which youths seem to withdraw from the healthcare system because they do not feel concerned about their health. Furthermore, a French study showed that 27% of young adults forego the healthcare system, especially for financial reasons [10]. In addition, a study [11] conducted in the United States reported that young people are overrepresented in emergency departments for problems that do not require emergency care and could be treated with outpatient procedures. A planned transition could avoid unnecessary visits in these departments.
A review article [12] revealed that there is a limited consensus on how and at what age healthy adolescents should approach transition. In fact, transition policies are unfamiliar to most health professionals and also to young patients and their families. Many are not even aware of its existence [5], whereas a coordinated and timely transfer from paediatric to adult care has been shown to be an important marker of quality of care for all young people [9].
The purpose of our study was to compare the characteristics of healthy youths who had discussed transition with those who did not or did not remember, and whether they differed in their sociodemographic characteristics, the perception of their health and their use of the health system. We hypothesised that youths who had not discussed transition were more likely to withdraw from the mainstream system of care.
We used the fourth wave (2018–2019) of the GenerationFRee study, a web-based survey on the lifestyle of youths carried out in the 11 post-mandatory schools (five high schools and six vocational schools) of the canton of Fribourg. In Switzerland, after mandatory education (age ~15 years ), about one third of young people attend high school and two thirds vocational schools. All students in the fourth year of post-mandatory education (high school or vocational school) were invited to answer an anonymous questionnaire online in the computer classroom of their school (n = 1534). However, as most vocational programmes last 2 or 3 years, we asked former students to also answer the survey using contact details collected during the previous waves (n = 1306). In addition, as some students were doing an internship during that period, we asked their teachers to send them an email with the link to the online survey so that they could participate in the study. Out of 1574 collected questionnaires (response rate: 55.4%), 1099 were considered for analysis. After eliminating those with a chronic condition, the final sample included 931 healthy youths (refer to the flowchart, fig. 1).
The Cantonal Ethics Committee of Vaud approved the study protocol.
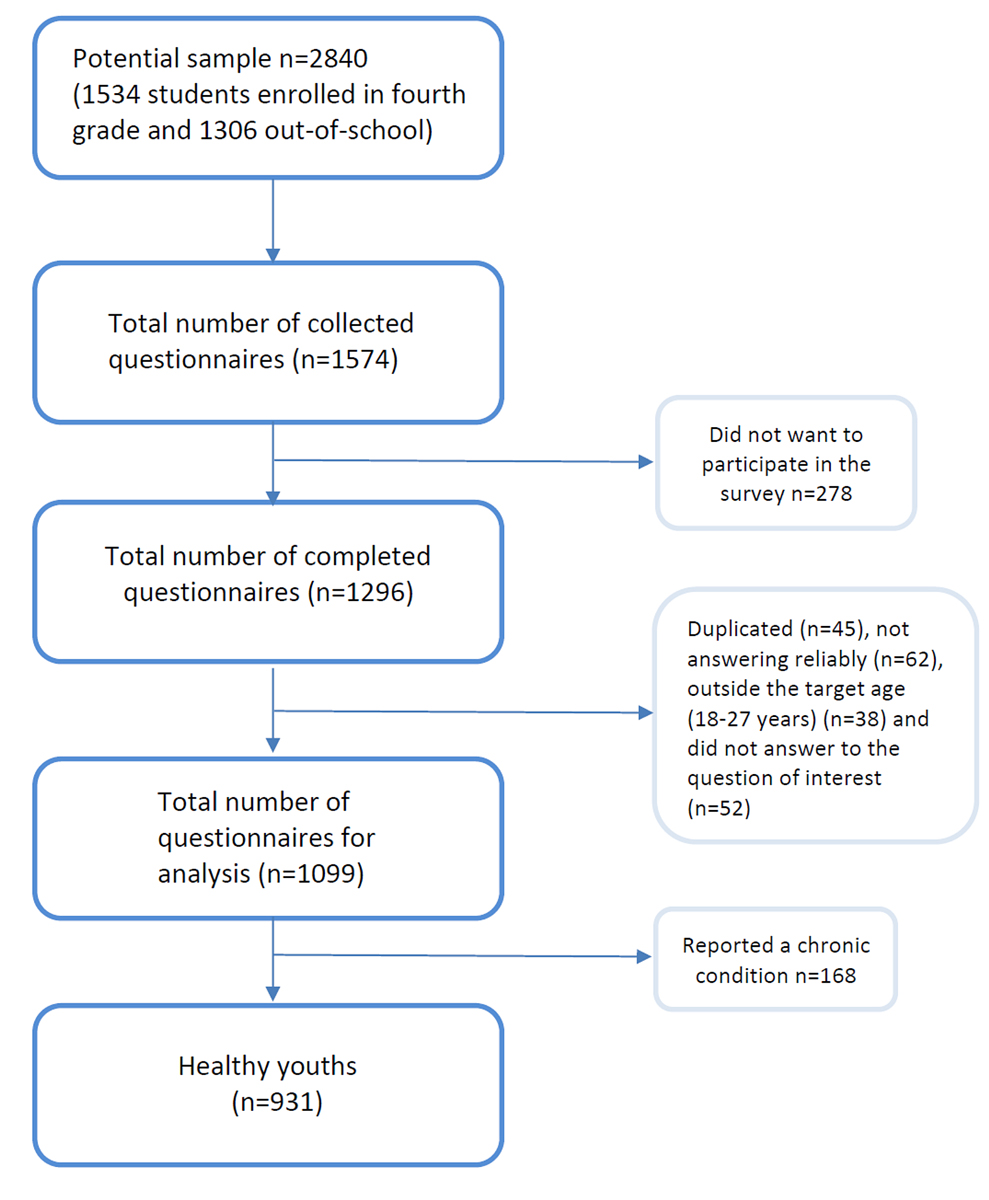
Figure 1 Flowchart showing the sampling technique.
To categorise youths based on having discussed transition, we used the following question: “Had/has your paediatrician discussed with you how to continue your medical care when you will be too old to go to the paediatrician? (transition to adult care)” and divided them into three groups according to the answer: (1) Yes, the paediatrician had talked about transition (Yes, n = 176; 52.3% girls); (2) No, the paediatrician had not discussed transition (No, n = 286; 44.7% girls); and (3) I don't know / don’t remember (Don’t know, n = 469; 49.3% girls)
Sociodemographic variables were used to describe each group. These variables included age (range: 18 to 27 years), gender, birthplace (Switzerland/other), parents’ birthplace (At least one born in Switzerland / both abroad), area of residence (urban/rural), housing type (with parents / other), family structure (parents living together / other) and academic track (student/apprentice).
We included two socioeconomic variables based on the perception of their family socioeconomic status and their involvement with health insurance payment. The socioeconomic status was evaluated using the European School Project on Alcohol and other Drugs question [13]: "Compared to the financial situation of other families in Switzerland, would you say that your family is...'' with seven possible answers ranging from "very much below average" to "very much above average” dichotomised into below average or average and above. We also asked them who paid for their health insurance, trichotomised into: I pay all/most of it; Partly me and partly my parents; My parents pay most of if / I don’t have this expense / I don’t know.
Health-related variables included perceived health status, emotional wellbeing and perceived onset of puberty. The question used to measure perceived health status comprised five possible responses that were dichotomised into Good (excellent, very good, good) and Poor (fair, poor). Emotional wellbeing was assessed using the WHO-5 index [14]. This index includes five statements related to the last 2 weeks (e.g., "I felt good and in a good mood") rated on a scale ranging from 0 (at no time) to 5 (all the time). By adding the different answers, the total score ranges from 0 to 25. A score below 13/25 is considered as a poor emotional wellbeing. For perceived onset of puberty we asked them if they thought their pubertal timing was advanced, on time, or delayed compared with their peers [15].
We also assessed the effect of transition on healthcare use with four variables: Having a primary care provider (dichotomised into Yes [family doctor, general practitioner, internist, specialist, or other] and No). Among those responding positively to the question (82% of boys and 91% of girls), we asked how they had met their current doctor (recommended by their paediatrician or by a friend, family member's doctor, found on the Internet, did not know, other). We further asked the average frequency of consultations with the primary care provider (Never/Rarely, About once every two years, About once a year, Several times a year) and whom they consult in first place when they have a medical concern (primary care provider, family, Internet, phone service, emergency department, friends, do not know, other).
Even though we were interested in the transition among healthy youths, we also compared it with those suffering from a chronic condition (n = 168; 56% girls). The chronic condition variable was assessed with the following question: “Do you have a chronic condition (i.e., a condition that has lasted for more than a year and requires regular care, such as asthma, diabetes, scoliosis, etc) or a physical disability (i.e., a lesion that affects the integrity of your body and limits its functioning not allowing you to do the same activities as other people your age)?”. Participants answering affirmatively were then included in the sample (n = 168).
Statistical analyses were performed using STATA 14.2. To compare the three groups, we first ran a bivariate analysis using the chi-square test for categorical variables and analysis of variance (ANOVA) for continuous ones. The threshold for statistical significance was set at p <0.05. Secondly, we made post-hoc two-by-two comparison tests between the three groups using a Bonferroni-type fit, with a statistical threshold set at p <0.017.
We then compared the rates of transition discussion between healthy adolescents and those with chronic conditions using the chi-square test.
All analyses were done separately by gender as they differ in the use of the healthcare system [16].
Overall, one fifth of girls and 17.5% of boys reported having discussed transition to adult care with their paediatrician. For both genders, about half of them (51.2% of girls, 49.6% of boys) responded that they did not know or did not remember discussing transition with their paediatrician. Over one quarter of girls (28%) and a third of boys (33%) stated that they had not discussed transition.
Girls who reported having discussed transition were more likely to perceive their socioeconomic status as below average and reported significantly more often having a primary care provider, although it was not associated with the frequency of visits. Their current doctor had been recommended by their paediatrician significantly more often than in the other two groups. Nonetheless, results showed that the first resource regarding health concerns was predominantly the family in all groups. Although girls who had discussed transition were more likely to consult a healthcare professional for health concerns, no significant difference was found between the three groups for perceived health status and emotional wellbeing. However, we found a trend among girls who discussed transition to reporting feeling better (perceived good health = 99.3%; good emotional wellbeing = 80.6%) than girls who did not discuss transition (perceived good health = 94.6%; good emotional wellbeing = 69.3%). Girls who reported not having discussed transition were more likely to have two foreign-born parents. In most cases, all three groups had met their current doctor because s/he was the primary care provider of other family members.
Table 1Comparison of characteristics according to the transition discussion among girls (n = 451).
| Talked about transition with paediatrician | Yes (n = 92) | No (n = 128) | Do not know / remember (n = 231) | p-value |
| Mean age (years ± SE) | 19.3 ± 0.19 | 19.4 ± 0.13 | 19.4 ± 0.11 | 0.58 |
| Academic track (student) | 43.9% | 59.1% | 49.3% | 0.50 |
| Birthplace (Switzerland) | 80.0% | 83.7% | 89.8% | 0.44 |
| Parents' birthplace (at least one in Switzerland) | 86.1% | 72.0%c | 86.5%c | 0.02 |
| Residence (urban) | 23.2% | 25.3% | 29.0% | 0.65 |
| Housing type (living with parents) | 77.9% | 91.4% | 92.0% | 0.14 |
| Family structure (parents living together) | 65.7% | 67.8% | 73.1% | 0.59 |
| Perceived socioeconomic status (below average) | 29.7%b | 8.5% | 7.4%b | <0.01 |
| Health insurance: | 0.99 | |||
| – I pay all or most of it | 16.2% | 15.5% | 13.5% | |
| – Me partly and my parents partly | 5.5% | 6.0% | 6.6% | |
| – My parents mostly / I don't have this expense / I don't know | 78.3% | 78.5% | 79.9% | |
| Perceived health status (good) | 99.3% | 94.6% | 95.4% | 0.20 |
| Emotional wellbeing (good) | 80.6% | 69.3% | 77.9% | 0.25 |
| Perceived pubertal timing | 0.06 | |||
| – Advanced | 39.8% | 40.3% | 21.1% | |
| – On time | 49.1% | 47.5% | 56.3% | |
| – Delayed | 11.1% | 12.2% | 22.6% | |
| Having a primary care provider (Yes) | 98.7%a | 89.7%*c | 96.5%c | <0.01 |
| Frequency of consultations: | 0.83 | |||
| – Never / Rarely | 30.6% | 27.2% | 24.5% | |
| – About once every two years | 19.6% | 12.8% | 21.0% | |
| – About once a year | 34.7% | 37.1% | 31.6% | |
| – Several times a year | 15.1% | 22.9% | 22.9% | |
| How the current primary care provider was met (n = 410): 8.3%† 82.3%† | <0.01 | |||
| – Recommended by paediatrician | 8.3%b | 0%c | 0.2%b,c | |
| – Primary care provider of parents / family members | 82.3%b | 76.1%c | 75.1%b,c | |
| – Recommended by friend | 5.2%b | 6.7%c | 5.6%b,c | |
| – Internet | 0%b | 5.0%c | 1.9%b,c | |
| – Do not know | 3.0%b | 5.0%c | 15.9%b,c | |
| – Others | 1.2%b | 7.2%c | 1.3%b,c | |
| First resource for health concern: | 0.31 | |||
| – Family | 38.9% | 54.3% | 59.5% | |
| – Primary care provider | 37.7% | 24.8% | 26.7% | |
| – Internet | 21.0% | 13.1% | 9.9% | |
| – A friend | 1.8% | 1.8% | 0.9% | |
| – Telephone service | 0.6% | 4.0% | 2.0% | |
| – Emergency department | 0% | 1.0% | 0.3% | |
| – Others | 0% | 1.0% | 0.7% | |
a indicates statistical significance following post hoc test (Bonferroni correction; p <0.017) between Yes and No
b indicates statistical significance following post hoc test (Bonferroni correction; p <0.017) between Yes and Don’t know/remember
c indicates statistical significance following post hoc test (Bonferroni correction; p <0.017) between No andDon’t know/remember
Boys who had discussed transition were more likely to report a perceived advanced puberty onset than those in the two other groups. Having a primary care provider was reported less often by boys who had not discussed transition. Still, those who had discussed transition were more likely to have met their current provider by referral from their paediatrician. However, in most cases, they met him/her because s/he was the primary care provider for other family members. In all groups, family was the first resource for health issues, but boys who had discussed transition with their paediatrician were more likely to seek information from a health professional.
We noted that 91.2% of boys who discussed transition reported a good emotional wellbeing compared with 81.2% of those who did not discuss it. The perceived health status was very similar among the three groups, and there was no difference in the frequency of consultations.
Table 2Comparison of characteristics according to the transition discussion among boys (n = 480).
| Talked about transition with paediatrician | Yes (n = 84) | No (n = 158) | Do not know / remember (n = 238) | p-value |
| Mean age (years ± SE) | 19.4 ± 0.16 | 19.4 ± 0.11 | 19.3 ± 0.08 | 0.58 |
| Academic track (student) | 23.3% | 30.2% | 30.3% | 0.40 |
| Birthplace (Switzerland) | 93.4% | 91.4% | 91.0% | 0.79 |
| Parents' birthplace (at least one in Switzerland) | 85.2% | 79.4% | 82.6% | 0.51 |
| Residence (urban) | 32.0% | 30.9% | 31.2% | 0.98 |
| Housing type (living with parents) | 92.4% | 90.3% | 95.6% | 0.11 |
| Family structure (parents living together) | 69.5% | 73.0% | 67.4% | 0.50 |
| Perceived socioeconomic status (below average) | 10.6% | 7.5% | 10.7% | 0.55 |
| Health insurance: | 0.94 | |||
| – I pay all or most of it | 14.8% | 16.9% | 14.8% | |
| – Me partly and my parents partly | 8.0% | 7.3% | 9.4% | |
| – My parents mostly / I don't have this expense / I don't know | 77.2% | 75.8% | 75.8% | |
| Perceived health status (good) | 97.2% | 98.4% | 97.8% | 0.82 |
| Emotional wellbeing (good) | 91.2% | 81.2% | 87.1% | 0.08 |
| Perceived pubertal timing | 0.04 | |||
| – Advanced | 26.4%a | 19.8% | 12.3%a | |
| – On time | 58.6%a | 61.3% | 68.9%a | |
| – Delayed | 15.0%a | 18.9% | 18.8%a | |
| Having a primary care provider (yes) | 89.5% | 78.4%b | 87.7%b | 0.02 |
| Frequency of consultations (n = 406): | 0.15 | |||
| – Never/rarely | 31.0% | 25.9% | 34.3% | |
| – About once every two years | 23.6% | 26.3% | 24.8% | |
| – About once a year | 34.9% | 28.3% | 32.0% | |
| – Several times a year | 10.5% | 19.5% | 8.9% | |
| How the current primary care provider was met (n = 395): | 0.01 | |||
| – Recommended by paediatrician | 7.0%a | 1.7% | 1.5%a | |
| – Primary care provider of parents / family members | 68.8%a | 82.1% | 73.0%a | |
| – Recommended by friend | 6.0%a | 0.9% | 1.8%a | |
| – Internet | 2.6%a | 0.9% | 0.7%a | |
| – Do not know | 11.5%a | 10.6% | 20.6%a | |
| – Others | 4.1%a | 3.8% | 2.4%a | |
| First resource for health concern: | 0.73 | |||
| – Family | 44.8% | 52.6% | 50.9% | |
| – Primary care provider | 38.5% | 28.7% | 30.6% | |
| – Internet | 10.1% | 12.2% | 12.3% | |
| – A friend | 0.8% | 3.2% | 1.0% | |
| – Telephone service | 1.4% | 1.4% | 2.0% | |
| – Emergency department | 0.9% | 0.7% | 1.4% | |
| – Others | 3.5% | 1.2% | 1.8% | |
a indicates statistical significance following post hoc test (Bonferroni correction; p <0.017) betweenYes and Do not know/remember
b indicates statistical significance following post hoc test (Bonferroni correction; p <0.017) between No and Don’t know/remember
The prevalence of discussion about transition to adult care among girls with a chronic condition did not differ significantly from their healthy peers (30.3% vs. 20.4%).
In contrast, boys with a chronic condition reported having discussed about transition significantly more frequently than their healthy peers (30.4% vs. 17.5%).
Table 3Comparison between youths with and without chronic conditions regarding discussions about transition, by gender (n = 1099).
| Girls (n = 545) | p-value | Boys (n = 554) | p-value | |||||
| Talked about transition with paediatrician | Yes (n = 120) | No (n = 150) | Do not know/ remember (n = 275) | Yes (n = 106) | No (n = 179) | Do not know / remember (n = 269) | ||
| Chronic condition (Yes) | 30.3% | 23.0% | 46.7% | 0.24 | 30.4% | 28.0% | 41.6% | 0.04 |
| Chronic condition (No) | 20.4% | 28.5% | 51.1% | 17.4% | 32.9% | 49.7% | ||
The main purpose of this study was to compare the characteristics of healthy youths enrolled in post-mandatory education depending on whether or not they had had a discussion about transitioning from paediatric to adult care with their pediatrician.
Findings show that, in the vast majority of cases, healthy youths (both girls and boys) did not remember whether they had discussed transition with their paediatrician. We can assume that healthy youths are therefore quite uninformed about this process and its usefulness. In their study among youths with chronic conditions, Rutishauser et al. [17] suggested that the lack of information about transition was a significant barrier to this process. Moreover, another study conducted in Hong Kong [18] among chronically ill youths showed that only a small proportion of adolescents and parents received information about transition from their doctor.
In addition, our results show that having discussed transition is closely related to having a primary care provider for adults. It would seem that when the paediatrician has discussed transition, healthy youths are more likely to benefit from continuity of care as they enter adulthood, hence potentially reducing the incidence of health problems. Indeed, Toulany et al. [19] reported that access to transition, and thus to continuity of primary care to adult care, enabled young people with severe mental illness to improve their health outcomes in early adulthood. Nonetheless, we found that having discussed transition was not associated with the frequency of visits. These results confirm partially our hypothesis in the sense that discussing transition is related to having a primary health provider in young adulthood, but makes no difference to the frequency of consultations.
We also found that girls reported that they had discussed transition more often than boys. We can assume a major potential role for another health specialist: the gynaecologist. Indeed, gynaecologists have the opportunity to interact with the female population for primary prevention, whereas young boys do not have an equivalent [20]. This could be an additional key in the long-term follow-up of this population. In addition, the need to consult a professional on a regular basis is emphasised by the GAPS (AMA Guidelines for Adolescent Preventive Services), which state that for prevention to be effective, young people should see their doctor once a year [21].
In the present study, both girls and boys who had previously discussed transition with their paediatrician reported having met their current doctor through their paediatrician significantly more often. However, the majority of participants in all groups, regardless of gender, claimed to have met their current doctor because s/he was the family doctor. In this sense, transition seems to have little effect. However, this choice could have an effect on the care of these youths because, if followed by the same doctor as their parents, it could lead to embarrassment and fear because of confidentiality issues [22]. These concerns could potentially cause a discontinuity of care.
In line with Ackard et al. [23], in all groups, the first resource used by youths for health concerns was their family. Nevertheless, we observed that youths who had discussed transition seemed to be more likely to contact their doctor if they had a health problem. Our results seem to indicate that the transition process encourages youths to seek professional advice. Moreover, although we expected to find emergency departments as the first resource for youths [24], these were mentioned very rarely by either gender.
Among girls, we found that a below average socioeconomic status was associated with a higher rate of discussion about transition. As a low socioeconomic status is associated with poorer health [25], as reported by Lebrun-Harris et al. [7], we hypothesised that paediatricians are aware of the risk of loss to follow-up which these youths are exposed to. Therefore, they are particularly careful to support them to avoid discontinuity of care. Additionally, girls were more likely to have discussed transition if they had at least one Swiss-born parent. We can assume that these parents better knew better the Swiss healthcare system and how to use it. Corscadden et al. [26] detailed the barriers limiting access to health care at an international level and concluded that people who were foreign-born were more likely to face multiple barriers.
Regardless of gender, youths having discussed transition reported a better emotional wellbeing, and girls appeared to perceive themselves as healthier, although these results were not significant. Additionally, perceived pubertal onset appeared to be a marker associated with transition among boys. It could be hypothesised that having an advanced puberty facilitates the transition process. Paediatricians may transfer more easily these young people because they are physically developed enough to be treated by an adult care provider or because they do not feel at ease dealing with adolescents. This hypothesis could be linked to the results observed by Ishiazaki et al. [27], who showed that psychosocial maturity was a factor involved in transition.
In terms of discussion on transition, we found fewer differences than expected between healthy youths and those with a chronic condition, even though chronically ill youths were more likely to have discussed the topic than healthy ones [6]. However, in line with Lebrun-Harris et al. [7], transition rates remain low, even among those with chronic conditions.
This study adds to the literature on transition among healthy young adults. Furthermore, we also took into consideration youths who did not know or remember as a separate group, which allowed us to highlight the current lack of knowledge regarding transition to adult care among young people. Nevertheless, some limitations need to be considered. First, the cross-sectional design of the study does not allow conclusions about causality to be drawn. Second, because the data were self-reported, we cannot exclude the presence of possible response or social desirability biases. However anonymous questionnaires are known to reduce this effect [28]. Third, the number of youths who discussed transition was relatively low (92 girls and 84 boys), reducing the statistical power of the study. Finally, although we asked whether transition had been discussed, we lack information both on its content and on the time when the discussion took place.
In conclusion, health professionals should systematically address transition among healthy youths and provide their patients with the necessary information to achieve an optimal passage to adult care, as this seems to allow young adults to remain integrated in healthcare, to be followed by a healthcare provider and to be more involved in their health. In general, the entire population should be made aware of transition to adult care and its importance. From an economic point of view, it is difficult to be pro-active in a system that practices fee-for-service, as is the case in Switzerland. This highlights the limitations of setting up a campaign promoting transition for all young people because doctors are paid on a fee-for-service basis. Our study warrants further specific research on the long-term health status of healthy youths depending on whether they went through the transition process or not.mailto:Joan-carles.suris@unisante.ch
The authors declare that they have no conflict of interest.
The GenerationFRee study was funded by theProgramme Intercantonal de Lutte contre la Dépendance au Jeu(PILDJ) and the Canton of Fribourg.
1. Blum RW , Garell D , Hodgman CH , Jorissen TW , Okinow NA , Orr DP , et al. Transition from child-centered to adult health-care systems for adolescents with chronic conditions. A position paper of the Society for Adolescent Medicine. J Adolesc Health. 1993 Nov;14(7):570–6. https://doi.org/10.1016/1054-139X(93)90143-D
2. Rosen DS . Transition of young people with respiratory diseases to adult health care. Paediatr Respir Rev. 2004 Jun;5(2):124–31. https://doi.org/10.1016/j.prrv.2004.01.008
3. Cooley WC , Sagerman PJ American Academy of Pediatrics American Academy of Family Physicians American College of Physicians; Transitions Clinical Report Authoring Group . Supporting the health care transition from adolescence to adulthood in the medical home. Pediatrics. 2011 Jul;128(1):182–200. https://doi.org/10.1542/peds.2011-0969
4. Nair M , Baltag V , Bose K , Boschi-Pinto C , Lambrechts T , Mathai M . Improving the Quality of Health Care Services for Adolescents, Globally: A Standards-Driven Approach. J Adolesc Health. 2015 Sep;57(3):288–98. https://doi.org/10.1016/j.jadohealth.2015.05.011
5. Leung S , Walgrave M , Mennito S . Improving Transitions of Care for Healthy Adolescents and Young Adults. South Med J. 2019 Oct;112(10):501–11. https://doi.org/10.14423/SMJ.0000000000001021
6. Eaton CK , Davis MF , Gutierrez-Colina AM , LaMotte J , Blount RL , Suveg C . Different Demands, Same Goal: Promoting Transition Readiness in Adolescents and Young Adults With and Without Medical Conditions. J Adolesc Health. 2017 Jun;60(6):727–33. https://doi.org/10.1016/j.jadohealth.2017.01.002
7. Lebrun-Harris LA , McManus MA , Ilango SM , Cyr M , McLellan SB , Mann MY , et al. Transition Planning Among US Youth With and Without Special Health Care Needs. Pediatrics. 2018 Oct;142(4):e20180194. https://doi.org/10.1542/peds.2018-0194
8. Schuiteman S , Chua KP , Plegue MA , Ilyas O , Chang T . Self-Management of Health Care Among Youth: Implications for Policies on Transitions of Care. J Adolesc Health. 2020 May;66(5):616–22. https://doi.org/10.1016/j.jadohealth.2020.01.009
9. Wisk LE , Finkelstein JA , Sawicki GS , Lakoma M , Toomey SL , Schuster MA , et al. Predictors of timing of transfer from pediatric- to adult-focused primary care. JAMA Pediatr. 2015 Jun;169(6):e150951. https://doi.org/10.1001/jamapediatrics.2015.0951
10. Baggio S , Iglesias K , Fernex A . Healthcare renunciation among young adults in French higher education: A population-based study. Prev Med. 2017 Jun;99:37–42. https://doi.org/10.1016/j.ypmed.2017.02.002
11. Ziv A , Boulet JR , Slap GB . Emergency department utilization by adolescents in the United States. Pediatrics. 1998 Jun;101(6):987–94. https://doi.org/10.1542/peds.101.6.987
12. Lotstein DS , McPherson M , Strickland B , Newacheck PW . Transition planning for youth with special health care needs: results from the National Survey of Children with Special Health Care Needs. Pediatrics. 2005 Jun;115(6):1562–8. https://doi.org/10.1542/peds.2004-1262
13. Hibell B , Andersson B , Bjarnason T , Ahlström S , Balakireva O , Kokkevi A , et al. The ESPAD report 2003: Alcohol and Other Drugs Use Among Students in 35 European Countries. The Swedish Council for Information on Alcohol and Other Drugs; 2003.
14. Allgaier AK , Pietsch K , Frühe B , Prast E , Sigl-Glöckner J , Schulte-Körne G . Depression in pediatric care: is the WHO-Five Well-Being Index a valid screening instrument for children and adolescents? Gen Hosp Psychiatry. 2012 May-Jun;34(3):234–41. https://doi.org/10.1016/j.genhosppsych.2012.01.007
15. Berg-Kelly K , Erdes L . Self-assessment of sexual maturity by mid-adolescents based on a global question. Acta Paediatr. 1997 Jan;86(1):10–7. https://doi.org/10.1111/j.1651-2227.1997.tb08822.x
16. Bertakis KD , Azari R , Helms LJ , Callahan EJ , Robbins JA . Gender differences in the utilization of health care services. J Fam Pract. 2000 Feb;49(2):147–52.
17. Rutishauser C , Sawyer SM , Ambresin AE . Transition of young people with chronic conditions: a cross-sectional study of patient perceptions before and after transfer from pediatric to adult health care. Eur J Pediatr. 2014 Aug;173(8):1067–74. https://doi.org/10.1007/s00431-014-2291-9
18. Wong LH , Chan FW , Wong FY , Wong EL , Huen KF , Yeoh EK , et al. Transition care for adolescents and families with chronic illnesses. J Adolesc Health. 2010 Dec;47(6):540–6. https://doi.org/10.1016/j.jadohealth.2010.04.002
19. Toulany A , Stukel TA , Kurdyak P , Fu L , Guttmann A . Association of Primary Care Continuity With Outcomes Following Transition to Adult Care for Adolescents With Severe Mental Illness. JAMA Netw Open. 2019 Aug;2(8):e198415. https://doi.org/10.1001/jamanetworkopen.2019.8415
20. Delisi K , Gold MA . The initial adolescent preventive care visit. Clin Obstet Gynecol. 2008 Jun;51(2):190–204. https://doi.org/10.1097/GRF.0b013e31816d1fd6
21. Knishkowy B , Palti H . GAPS (AMA Guidelines for Adolescent Preventive Services). Where are the gaps? Arch Pediatr Adolesc Med. 1997 Feb;151(2):123–8. https://doi.org/10.1001/archpedi.1997.02170390013002
22. Pérez-Cárceles MD , Pereñiguez JE , Osuna E , Luna A . Balancing confidentiality and the information provided to families of patients in primary care. J Med Ethics. 2005 Sep;31(9):531–5. https://doi.org/10.1136/jme.2004.010157
23. Ackard DM , Neumark-Sztainer D . Health care information sources for adolescents: age and gender differences on use, concerns, and needs. J Adolesc Health. 2001 Sep;29(3):170–6. https://doi.org/10.1016/S1054-139X(01)00253-1
24. Knowlton AR , Weir B , Fields J , Cochran G , McWilliams J , Wissow L , et al. Pediatric Use of Emergency Medical Services: The Role of Chronic Illnesses and Behavioral Health Problems. Prehosp Emerg Care. 2016 May-Jun;20(3):362–8. https://doi.org/10.3109/10903127.2015.1115928
25. Hanson MD , Chen E . Socioeconomic status and health behaviors in adolescence: a review of the literature. J Behav Med. 2007 Jun;30(3):263–85. https://doi.org/10.1007/s10865-007-9098-3
26. Corscadden L , Levesque JF , Lewis V , Strumpf E , Breton M , Russell G . Factors associated with multiple barriers to access to primary care: an international analysis. Int J Equity Health. 2018 Feb;17(1):28. https://doi.org/10.1186/s12939-018-0740-1
27. Ishizaki Y , Maru M , Higashino H , Katsumoto S , Egawa K , Yanagimoto Y , et al. The transition of adult patients with childhood-onset chronic diseases from pediatric to adult healthcare systems: a survey of the perceptions of Japanese pediatricians and child health nurses. Biopsychosoc Med. 2012 Mar;6(1):8. https://doi.org/10.1186/1751-0759-6-8
28. Brener ND , Billy JO , Grady WR . Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. J Adolesc Health. 2003 Dec;33(6):436–57. https://doi.org/10.1016/S1054-139X(03)00052-1