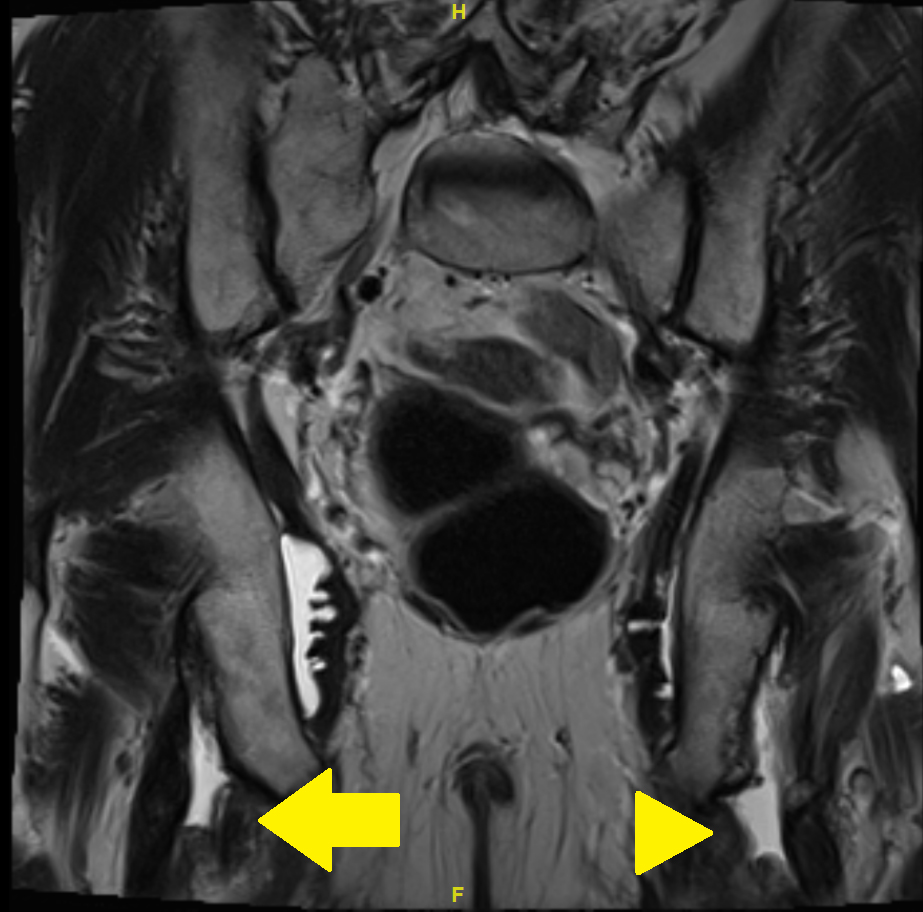
Figure 1 MRI of the pelvis with T2 turbo spin echo (TSE) weighted image: coronary view. Arrow: partial avulsion on the right side; arrowhead: complete avulsion on the left side.
DOI: https://doi.org/10.4414/SMW.2021.w30011
Canadian Research Group of Rheumatology in Immuno-Oncology
fluorine-18-fluorodeoxyglucose
immune checkpoint inhibitor
immune-related adverse event
magnetic resonance imaging
nonsteroidal anti-inflammatory drug
positron emission tomography-computed tomography
turbo spin echo
the United Kingdom Health Improvement Network
United Kingdom
We report a patient treated with immune checkpoint inhibitors and corticosteroids who had a spontaneous bilateral proximal hamstring muscle avulsion. Signs and symptoms were nonspecific and further imaging was necessary for diagnosis. Proximal hamstring muscle or tendon avulsions have been reported almost exclusively in athletes and trauma patients [1—3]. Tendon or muscle ruptures or avulsions are well-known side effects of corticosteroids and quinolone antibiotics [4—7]. Immune checkpoint inhibitors can lead to serious adverse effects including the musculoskeletal disorders [8—11]. We suspected the immune checkpoint inhibitor together with corticosteroids as the possible cause of the spontaneous hamstring muscle avulsion.
A 66-year-old man presented in November 2019 with a 4-week history of bilateral gluteal pain. Pain was mostly present while walking, standing up and in a sitting position, and to a lesser extent in the supine position. The patient had no previous trauma or intensive sports activity. The complaints had started slowly and increased steadily. There were no signs or symptoms of infection. He had previously been treated with the immune checkpoint inhibitors (ICIs) ipilimumab and nivolumab because of metastasising melanoma. Between April and May 2017 he received a total of three doses of ipilimumab and nivolumab, and between August 2017 and October 2018 a total of 29 doses of nivolumab. The therapy induced a lasting remission. Under ICI treatment, he developed various immune-related adverse events (IrAEs), including episodes of hepatitis, vitiligo, cholangitis, rhinosinusitis, serositis and omarthritis, which repeatedly required therapy with corticosteroids. However, there was no episode of tendinitis. He had to start a course of prednisone approximately 2 weeks before beginning of the gluteal pain because of pleural serositis. At the beginning of the pain, he was still on prednisone 20 mg daily. In the past medical history there was an episode of urosepsis 10 months previously. For that, he received the quinolone antibiotic ciprofloxacin for 8 days.
The patient was in a good general condition with a normal weight and afebrile. There was tenderness around the ischial tuberosity, left more than right. Active and passive flexion of the knee led to strong gluteal pain and therefore was limited almost completely on the left and partially on the right side. Blood analysis did not reveal any signs of inflammation. The creatine kinase was normal. Initially, ischial tuberosity bursitis was suspected and nonsteroidal anti-inflammatory drugs (NSAIDs) and physical therapy were prescribed.
Because of a nonresponse to these measures, magnetic resonance imaging (MRI) of the pelvis was carried out. The MRI showed complete bilateral avulsion of the proximal hamstring muscles with the exception of some remaining fibres of the long head of the biceps femoris muscle on the right side (figs 1—4). There were no clear signs of inflammation nor any signs of myxoid degeneration. Also, there were no signs of inflammation in the area of the hamstring tendons in a past positron emission tomography-computed tomography (PET-CT) performed for melanoma follow up 4 months prior to the MRI.
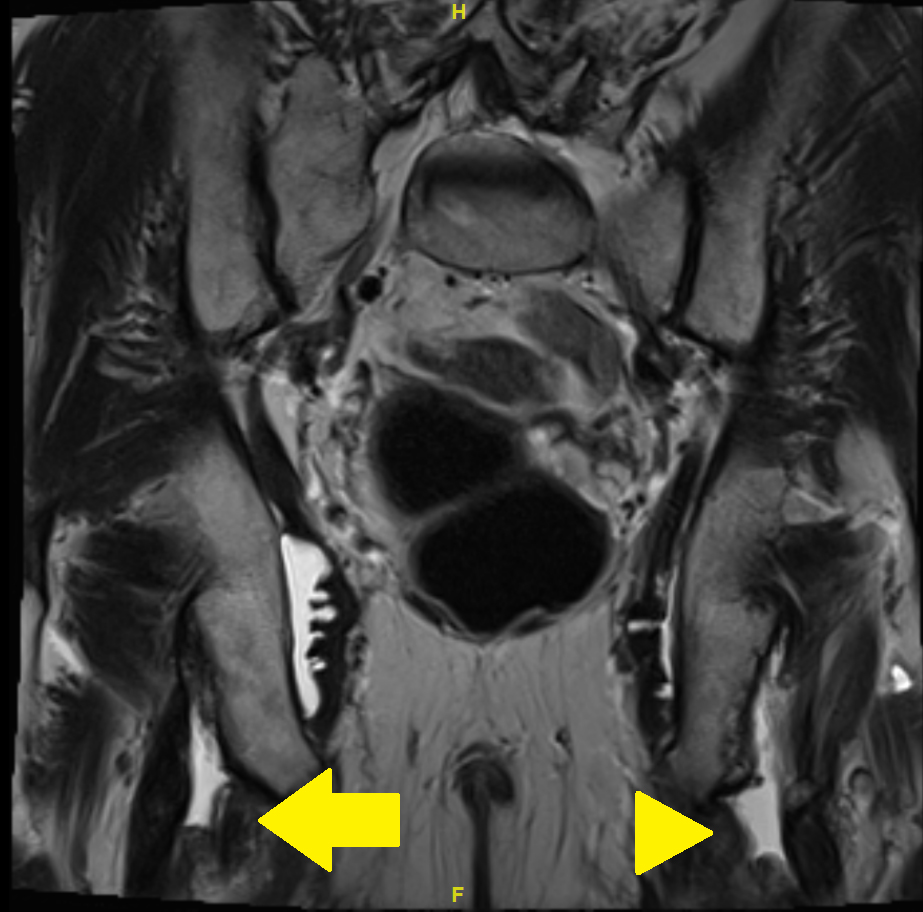
Figure 1 MRI of the pelvis with T2 turbo spin echo (TSE) weighted image: coronary view. Arrow: partial avulsion on the right side; arrowhead: complete avulsion on the left side.
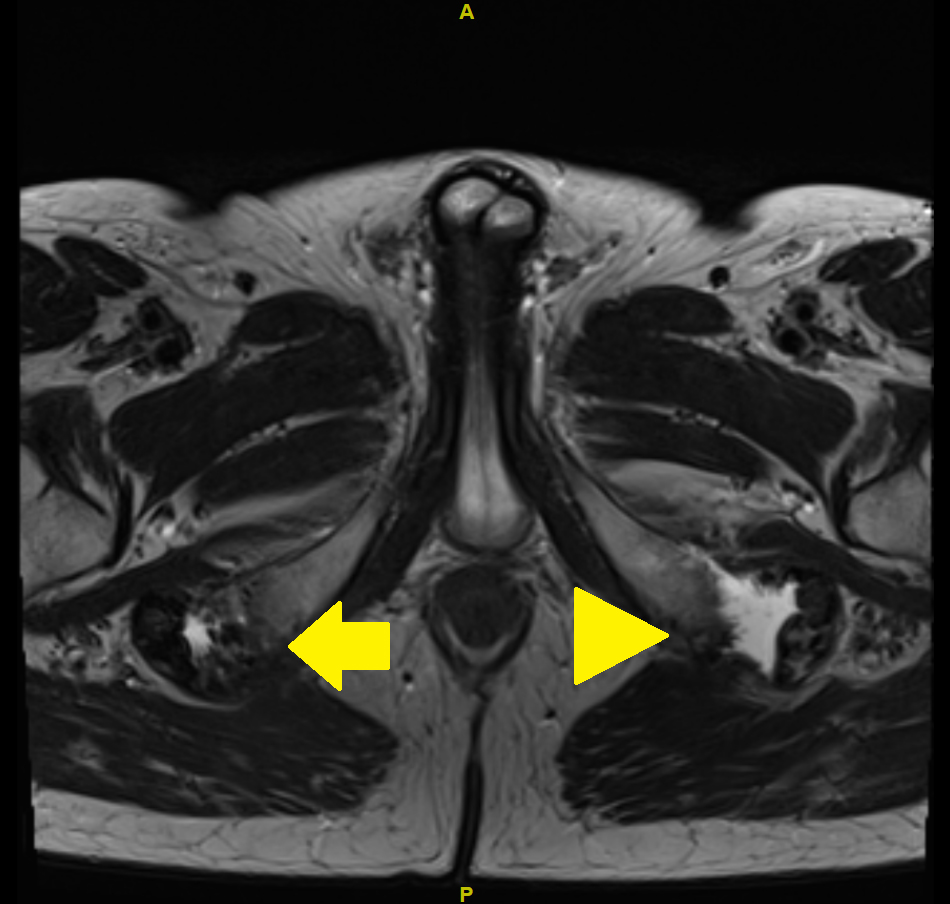
Figure 2 MRI of the pelvis with T2 turbo spin echo (TSE) weighted image: axial view. Arrow: partial avulsion on the right side; arrowhead: complete avulsion on the left side.
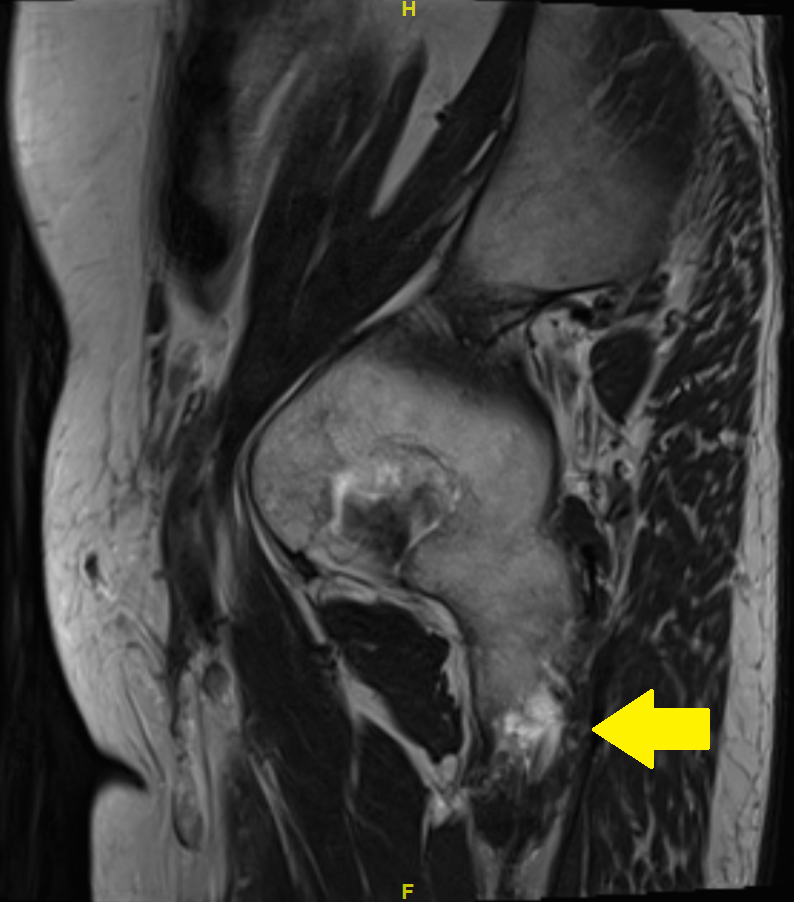
Figure 3 MRI of the pelvis with T2 turbo spin echo (TSE) images: sagittal view. Arrow: partial avulsion on the right side.
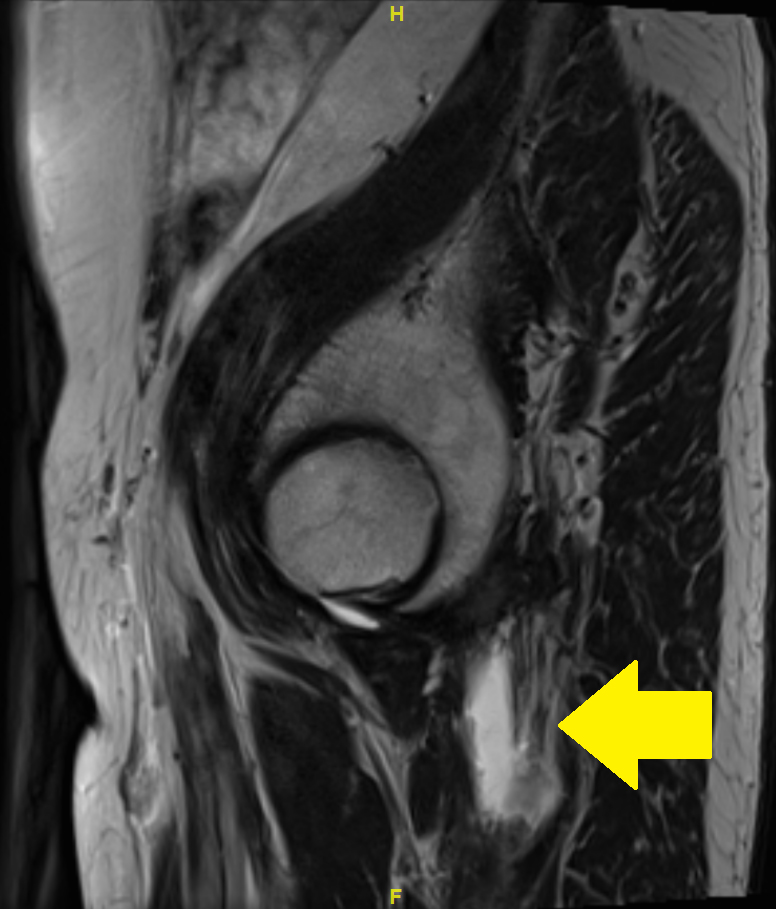
Figure 4 MRI of the pelvis with T2 turbo spin echo (TSE) images: sagittal view. Arrow: complete avulsion on the left side.
Over a period of one month, we observed slow but sustained improvement of the pain and a return to full mobility. PET-CT imaging for the melanoma follow-up 1, 13 and 15 months after the pelvic MRI did not show inflammatory activity in the area of the hamstring tendon insertion (figs 5 and 6). In the area of tendon insertion at the ischial tuberosity, there was a discrete elevation of fluorine-18-fluorodeoxyglucose (FDG) uptake, which could indicate a healing process. However, it also could indicate slightly elevated muscle tone. Because the patient reported no trauma or unusual physical activity, we considered medication as cause.
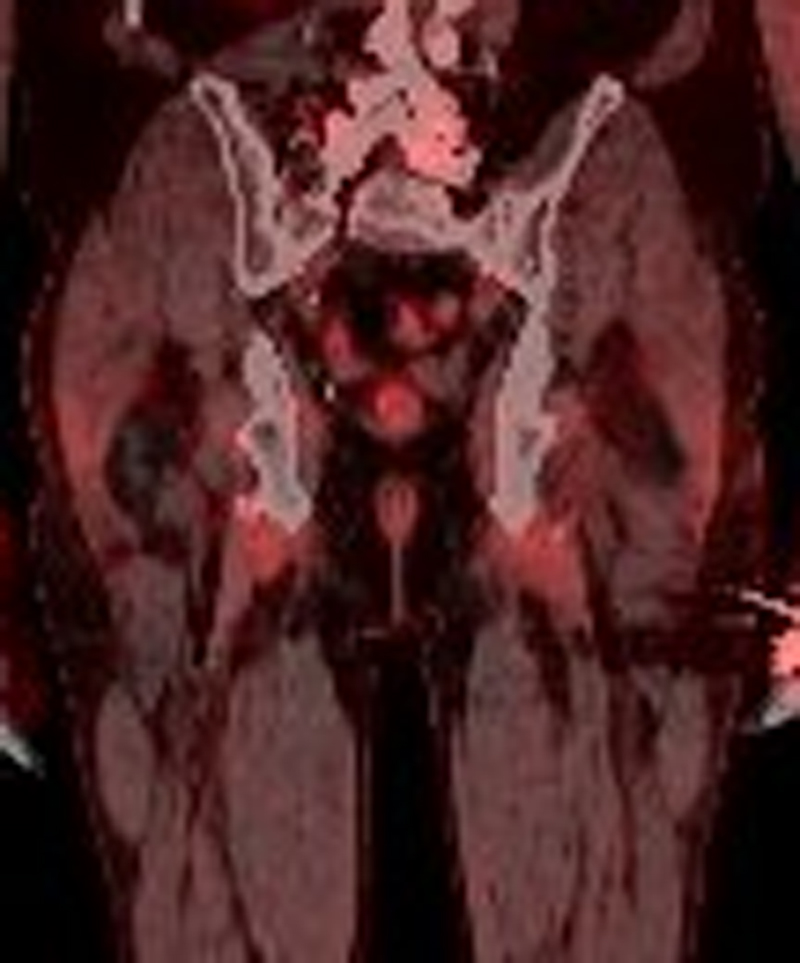
Figure 5 PET-CT of the pelvis 13 month after the rupture: coronary view.
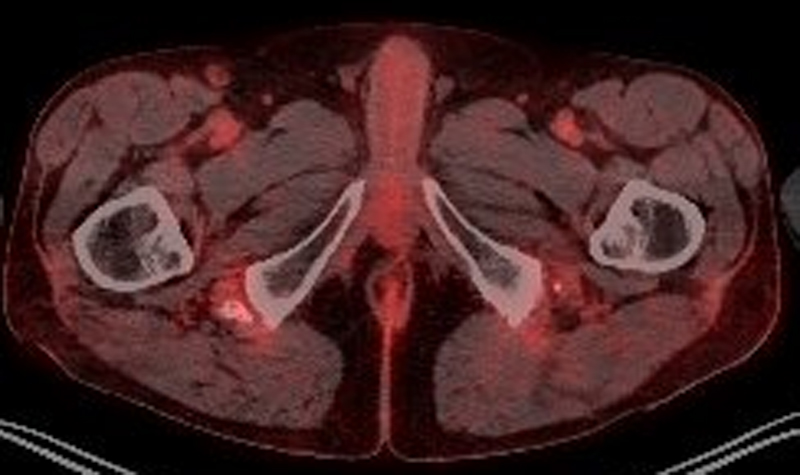
Figure 6 PET-CT of the pelvis 13 month after the rupture: axial view.
The hamstring muscles consist of musculus biceps femoris caput longum, musculus semimembranosus and musculus semitendinosus. They share the proximal origin at the ischial tuberosity. Sudden proximal hamstring avulsion usually leads to severe pain and impaired movement. However, it can sometimes be asymptomatic.
Hamstring strain, avulsion and rupture in athletes are often reported. In an overview of treatment options for hamstring ruptures, patients exclusively were athletes or had suffered trauma [1]. Fast accelerating and decelerating movements were identified as risk factors for acute, and running as risk factor for chronic, proximal hamstring tendinosis or ruptures [2].applewebdata://3E835C25-72CC-4754-B03B-45B55A545731#_msocom_6 In a PubMed and Google® literature search on 16 June 2021applewebdata://3E835C25-72CC-4754-B03B-45B55A545731#_msocom_7 we could find only one case report within the last 20 years with a non-traumatic proximal hamstring muscle avulsion. Kwong et al. published in 2006 a case of a 62-year-old man with sudden onset unilateral buttock pain. MRI of the pelvis demonstrated a complete avulsion of the right proximal hamstring muscle with a large haematoma. There was no past ICI, corticosteroid or quinolone antibiotic use [3]. A retrospective review of MRI of the pelvis of 253 asymptomatic patients, published in 2017, searched for proximal hamstring injuries for any reason. These patients all underwent MRI for purposes not related to possible hamstring lesions and had no known proximal hamstring injury. Four patients had bilateral complete rupture of the proximal hamstring muscles. Ten patients had unilateral a complete tear, four had bilateral complete tears and 81 had uni- or bilateral partial tears. Past or current use of ICIs, corticosteroids or quinolone antibiotics was not documented [12]. A PubMed and Google® literature search for “non traumatic bilateral hamstring avulsion”, “non traumatic bilateral hamstring injury”, “spontaneous bilateral hamstring avulsion”, “spontaneous bilateral hamstring rupture” and “spontaneous bilateral hamstring injury” on 16 June 2021 revealed no hiapplewebdata://3E835C25-72CC-4754-B03B-45B55A545731#_msocom_9t.
Tendons, muscles and entheses are one of the sites of IrAEs of ICIs. A literature review studied 52 out of 1742 publications for the prevalence of musculoskeletal IrAEs in ICI-users. The incidence of arthralgia was between 1% and 43% and of myalgia between 2% and 20%. Three cited studies – two of them were case reports – reported development of myositis. No tendon or muscle rupture or avulsion was mentioned [8]. Inamo et al. conducted a single centre case review of 133 patients with ICI therapy. Three patients had tenosynovitis and enthesitis as IrAEs. Locations were extensor digitorum, flexor digitorum, fibular collateral ligament and quadriceps femoris. No hamstring muscle avulsion or rupture was reported [9]. In June 2020, the Canadian Research Group of Rheumatology in Immuno-Oncology (CanRIO) published a retrospective study on rheumatological IrAEs. They examined 117 patients who developed a total of 136 rheumatological IrAEs after or during ICI therapy. The phenotype was symmetrical polyarthritis in 33.1%, polymyalgia rheumatica-like syndrome in 12.5% and tenosynovitis, tendonitis or enthesitis in 11.8%. No tendon or muscle rupture or avulsion was reported [10]. In a prospective MRI study, 14 patients were reported after ICI treatment with clinical findings suggestive for musculoskeletal IrAE (10.8% of all patients with ICI treatment). In one patient with knee swelling, partial rupture of the quadriceps tendon was found [11].
Tendon or muscle avulsions or ruptures are a well-known side effect of corticosteroids. Persson et al. published a cohort study to assess the absolute rate and the excess risk of tendon ruptures with use of quinolone antibiotics and the effect of corticosteroids. They included 740,926 patients from a British registry between 1990 and 2015 with a total of 3957 non-traumatic tendon ruptures, 31.9% of which were Achilles tendon and 22.0% were biceps brachii tendon ruptures. No single rupture or avulsion of hamstring muscles or tendons was reported. The concomitant use of quinolone antibiotics and corticosteroids elevated the risk for Achilles tendon rupture almost 11-fold. The use of quinolone antibiotics alone elevated the risk only two-fold [4]. A population-based nested case-control study of the United Kingdom (UK) Health Improvement Network (THIN) primary care database investigated the relative and absolute risk of tendon avulsion with use of quinolone antibiotics. Additionally the effects of corticosteroids were examined. This database covers about 6% of the population of the UK. Adults with a prescription for a systemic quinolone antibiotic or amoxicillin /clavulanic acid as a control were compared. The THIN data revealed an adjusted incidence rate ratio of Achilles tendon rupture of 7.78–48.19 with concomitant use of corticosteroids and quinolone antibiotics and 3.43–6.14 with use of corticosteroids alone [5].
Another medication known for elevation of the risk of tendon or muscle rupture or avulsion are quinolone antibiotics. Khaliq et al. conducted a systematic review of 98 case reports of quinolone antibiotic-associated tendon injury. Almost half of the injuries were ruptures. The Achilles tendon was by far the most common site of tendon injury at 89.8%. However, none of the reported cases had hamstring muscle or tendon avulsion or rupture. The mean time between starting quinolone antibiotics and tendon rupture were 25.6 to 42.3 days. The longest interval was 6 months after stopping quinolone use [6]. A systematic review of 16 observational studies of patients taking quinolone antibiotics demonstrated an increased risk for tendon avulsion, especially of the Achilles tendon. A period of 15 days to 18 months between quinolone exposure and tendon avulsion was shown. Mostly, injuries happened within 6 months. Use of corticosteroids seemed to be an additional risk for tendon avulsion [7].
Based on the results of our literature search we considered the short-term quinolone therapy 10 months before diagnosis of spontaneous tendon avulsion as a clearly less probable causal factor than the treatment with ICI and corticosteroids.
Symptomatic proximal hamstring lesions almost always occurs in athletes or after trauma [1—3]. Musculoskeletal problems are emerging IrAEs of ICIs. Mostly they consist of arthritis, myalgia, enthesitis, myositis or tendinitis. Until now, there is no report of hamstring muscle or tendon avulsion or rupture in patients treated with ICIs [8—10]. However, a recent MRI study revealed one patient with a partial rupture of the quadriceps tendon as a potential IrAE [11].applewebdata://3E835C25-72CC-4754-B03B-45B55A545731#_msocom_12 The use of corticosteroids increases the risk for tendon or muscle injury. However, no report of a hamstring lesion in association with these medications has been published so far [4—7].
Although the relative contribution of ICI and corticosteroids cannot be discriminated in our case, ICI, and corticosteroid therapy to control autoimmune manifestations caused by the ICI therapy, were presumably causally related to the occurrence of the avulsions in our patient. This assumption is supported by the fact that the preceding imaging did not show degenerative changes of the tendons or occult ruptures. Recently a partial rupture of the quadriceps tendon after treatment with ICI has been reported [11]. However, in contrast to that report in our case there were no clear signs of inflammation of the tendon or muscle. Therefore a spontaneous rupture unrelated to therapy with ICI and glucocorticoids cannot be ruled out. However, a case of non-traumatic symptomatic bilateral proximal hamstring avulsion or rupture has not been published so far. Our case report suggests that in patients with IrAE during ICI treatment developing hip or gluteal pain, the possibility of spontaneous proximal hamstring avulsion should be considered.applewebdata://3E835C25-72CC-4754-B03B-45B55A545731#_msocom_14
There are no conflicts of interest and there was no external financial assistance or influence.
The patient documented in this case report signed a consent form in which he agrees with the use of his medical record for scientific purpose. We would like to thank the patient for allowing the publication of his case, colleagues of the department of Rheumatology and the department of Oncology and our proofreader.
Author contributions: NF took care of the patient, performed literature research and wrote the manuscript. FC reviewed the radiologic and nuclear medicine imaging. DK took care of the patient, performed literature research, and reviewed the manuscript. All authors approved the final draft.
1 Cohen S , Bradley J . Acute proximal hamstring rupture. J Am Acad Orthop Surg. 2007 Jun;15(6):350–5. https://doi.org/10.5435/00124635-200706000-00004
2 Startzman AN , Fowler O , Carreira D . Proximal Hamstring Tendinosis and Partial Ruptures. Orthopedics. 2017 Jul;40(4):e574–82. https://doi.org/10.3928/01477447-20170208-05
3 Kwong Y , Patel J , Ramanathan EB . Spontaneous complete hamstring avulsion causing posterior thigh compartment syndrome. Br J Sports Med. 2006 Aug;40(8):723–4. https://doi.org/10.1136/bjsm.2005.022749
4 Persson R , Jick S . Clinical implications of the association between fluoroquinolones and tendon rupture: the magnitude of the effect with and without corticosteroids. Br J Clin Pharmacol. 2019 May;85(5):949–59. https://doi.org/10.1111/bcp.13879
5 Morales DR , Slattery J , Pacurariu A , Pinheiro L , McGettigan P , Kurz X . Relative and Absolute Risk of Tendon Rupture with Fluoroquinolone and Concomitant Fluoroquinolone/Corticosteroid Therapy: Population-Based Nested Case-Control Study. Clin Drug Investig. 2019 Feb;39(2):205–13. https://doi.org/10.1007/s40261-018-0729-y
6 Khaliq Y , Zhanel GG . Fluoroquinolone-associated tendinopathy: a critical review of the literature. Clin Infect Dis. 2003 Jun;36(11):1404–10. https://doi.org/10.1086/375078
7 Stephenson AL , Wu W , Cortes D , Rochon PA . Tendon Injury and Fluoroquinolone Use: A Systematic Review. Drug Saf. 2013 Sep;36(9):709–21. https://doi.org/10.1007/s40264-013-0089-8
8 Cappelli LC , Gutierrez AK , Bingham CO 3rd , Shah AA . Rheumatic and musculoskeletal immune-related adverse events due to immune checkpoint inhibitors: A systematic review of the literature. Arthritis Care Res (Hoboken). 2017 Nov;69(11):1751–63. https://doi.org/10.1002/acr.23177
9 Inamo J , Kaneko Y , Takeuchi T . Inflammatory tenosynovitis and enthesitis induced by immune checkpoint inhibitor treatment. Clin Rheumatol. 2018 Apr;37(4):1107–10. https://doi.org/10.1007/s10067-018-4035-0
10 Roberts J , Ennis D , Hudson M , Ye C , Saltman A , Himmel M , et al. Rheumatic immune-related adverse events associated with cancer immunotherapy: A nationwide multi-center cohort. Autoimmun Rev. 2020 Aug;19(8):102595. https://doi.org/10.1016/j.autrev.2020.102595
11 Daoussis D , Kraniotis P , Filippopoulou A , Argiriadi R , Theodoraki S , Makatsoris T , et al. An MRI study of immune checkpoint inhibitor-induced musculoskeletal manifestations myofasciitis is the prominent imaging finding. Rheumatology (Oxford). 2020 May;59(5):1041–50. https://doi.org/10.1093/rheumatology/kez361
12 Thompson SM , Fung S , Wood DG . The prevalence of proximal hamstring pathology on MRI in the asymptomatic population. Knee Surg Sports Traumatol Arthrosc. 2017 Jan;25(1):108–11. https://doi.org/10.1007/s00167-016-4253-4