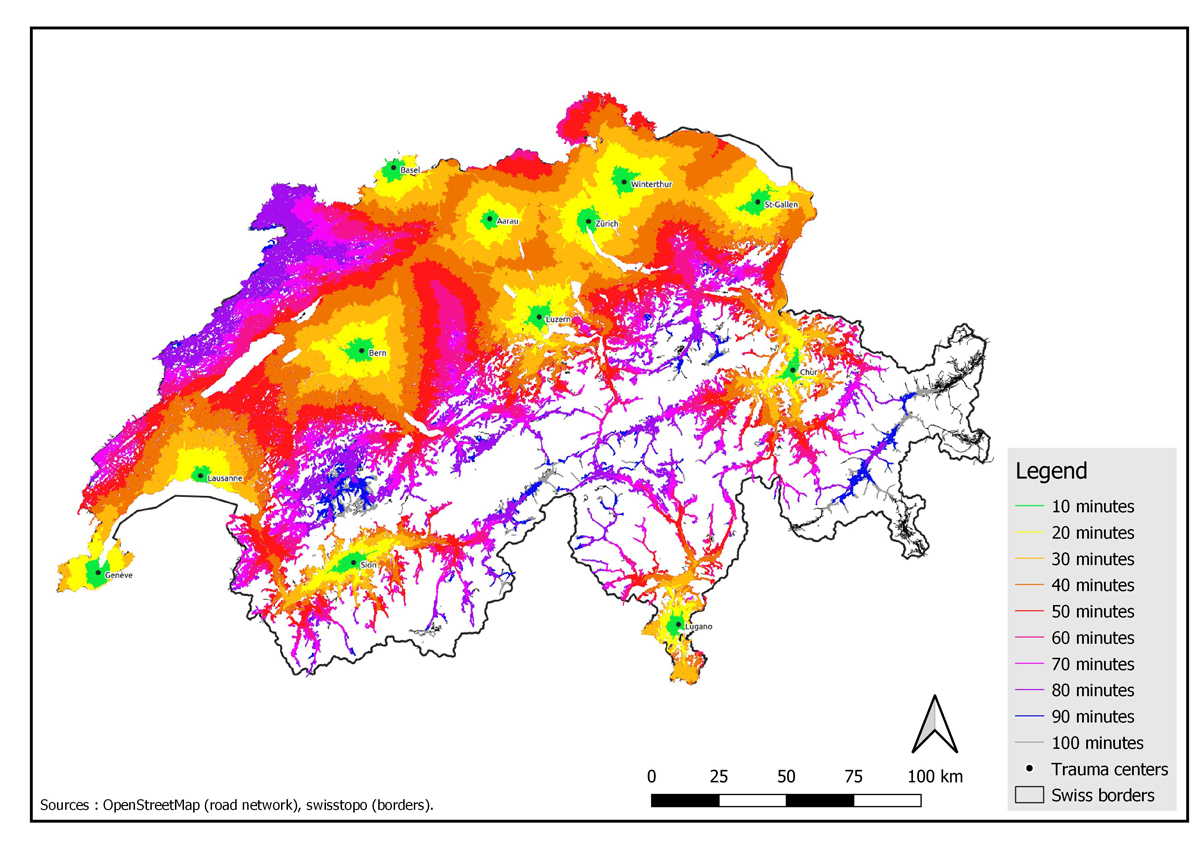
Figure 1 Isochrones of 10 minutes around the trauma centres in Switzerland after validation.
DOI: https://doi.org/10.4414/SMW.2021.w30007
Road accidents were the seventh leading cause of disability-adjusted life-years in 2019 worldwide, and the leading cause in the age group 10 to 24 years [1]. In 2019 in Switzerland, 17,761 road accidents that caused injuries occurred, including 17,641 minor injuries, 3,639 serious injuries and 187 fatalities [2]. Prompt access to a trauma centre can reduce mortality and trauma-related sequelae for those seriously injured in a road accident [3, 4]. This time dependence has been conceptualised as the Golden Hour, which links access time to definitive treatment in a trauma centre within 1 hour of trauma to reduced risk of morbidity and mortality [5]. The Golden Hour spans the time from the call to the emergency dispatch centre to arrival at the nearest trauma centre.
Although the Golden Hour has been questioned [6, 7], an association exists between transport time or distance and mortality, at least for hypotensive patients or those with penetrating wounds [8]. An English study found a 1% increase in mortality for every additional 10 km from the accident site to the trauma centres [9]. In a more recent Canadian study, a calculated access time of more than 30 minutes from the accident site to the trauma centre was associated with an increased risk of mortality for victims of penetrating trauma or road accidents [10]. In Switzerland, the only study that has explored the relationship between accident mortality and travel time showed no difference in survival between patients who arrived at the emergency department in ≤60 minutes and those who arrived in >60 minutes [6]. However, this single-centre study included only 30 deaths and differentiated survivors from non-survivors by 10 critical factors, a number too large to be adequately adjusted for with such a small sample size. To our knowledge, no study has examined the relationship between transport time to the 12 Swiss trauma centres and mortality. This relationship is worth examining, as the geographical distribution of trauma centres in most countries is based on the location of historical hospitals and not on the frequency of accidents or minimisation of transport time. This may be a relevant issue for remote or mountainous regions that combine a high risk of serious accidents, difficult access and long transport time [11].
The aim of our study was therefore to determine whether the current layout of Swiss trauma centres allowed for homogeneous access time within the Golden Hour in the country, or whether overlapping or uncovered areas exist. A secondary aim was to study the relationship between transport time from the accident site to the nearest trauma centre and mortality in Switzerland.
As our study included only anonymous and non-medical data, the cantonal human research ethics commission exempted it from the scope of the federal law on human research (CER-VD 2019-00609).
Switzerland is a country of 41,285 km2, with just over 8 million inhabitants. Since 2011, severe trauma victims, defined by an Injury Severity Score of ≥20 or a traumatic brain injury with an Abbreviated Injury Scale score of ≥3, have been referred to one of the 12 trauma centres that meet the requirements of highly specialised medicine (Aarau, Basel, Bern, Chur, Geneva, Lausanne, Lugano, Lucerne, Sion, St Gallen, Winterthur and Zurich) [12].
Transport time represented the time required for the ambulance to travel from the intervention site to the nearest trauma centre (= return travel time). The mission time was the time required for the entire mission (call to 144, time to and from the site, and time at the site). Transport time around each trauma centre was modelled by using the open source Quantum Geographic Information System (QGIS) software [13]. Isochronous curves corresponding to transportation times of 10 minutes were developed based on the shortest distance between the location of a potential road accident site and the nearest trauma centre, following the Swiss road network (OpenStreetMap), with a transport speed set at the maximum legal speed, according to the category of the roads used. A speed of 50 km/h was assigned to roads of unknown category. The road data were uploaded on August 2 2019. The Swiss border layer of Swisstopo (swissBOUNDARIES3D, revision January 2019) was used.
The geospatial data of fatal road accidents (aggregated fatalities on site and within 30 days) in Switzerland between 2011 and 2017 were obtained from the database of the Federal Roads Office (FEDRO) [14] and used to create a point vector layer. The transport time between the accident site and the nearest trauma centre was modelled with the QNEAT3-QGIS Network Analysis Toolbox extension of QGIS [15], which generates the fastest access time via the road network, taking into account the time required to enter this network when the accident site is not directly on a road, with a default speed of 5 km/h.
The journey times derived from the modelling were tested against a set of real data from priority land missions (with lights and sirens). From 9,579 missions, 1,000 were randomly selected by the random extract function of QGIS, with a median outward journey time of 6.0 minutes (interquartile range [IQR] 3.9—9.6), on-site time of 19.9 minutes (IQR 14.0—27.4), and transportation time to the trauma centre of 12.6 minutes (IQR 7.3—20.1). On GeoDa [16], an alpha factor was calculated for each mission as the ratio between the real mission time and the modelled time. A median alpha for the whole set of modelled transportation times was then calculated and applied as a correction factor to all transport times calculated for accidents in the FEDRO database.
Each accident was characterised by a modelled transport time from the accident site to the nearest trauma centre, as well as by mortality at 30 days. The total number and percentage of accidents were counted for each 10-minute isochrone. As the starting point of the ambulance for each mission was unknown, the data from the validation set were used to estimate the different mission times [15]. The times required to call and prepare for departure was considered negligible. The median time for on-site management was 19.9 minutes (see Validation of the Model section above), leaving 40 minutes for the cumulative time to travel to and from the nearest trauma centre. As the time to the trauma centre was twice as long as the time to the accident site (12.6 minutes vs 6 minutes), a maximum of two thirds of these 40 minutes, i.e., 27 minutes, was used as a cut-off value for compliance with the Golden Hour rule.
The relation between 10-minute intervals and average mortality was fitted using a non-linear regression line, based on a second order polynomial model.
The 10-minute isochrones of simulated return travel are shown in figure 1. Although the travel time to a trauma centre was <30 minutes in the eastern part of the Swiss plateau, it was longer in the Mittelland, the western part of Switzerland, the Alpine valleys and the Jura.
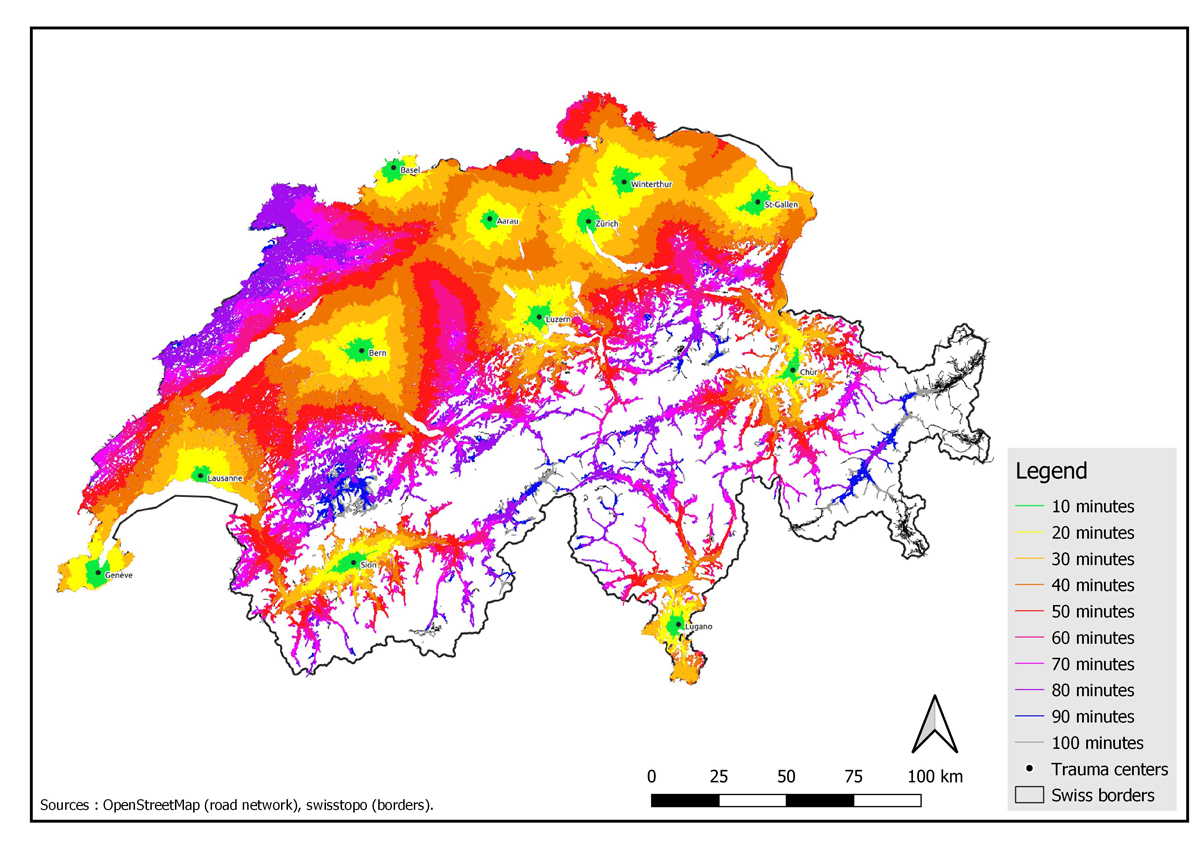
Figure 1 Isochrones of 10 minutes around the trauma centres in Switzerland after validation.
The number and cumulative proportion of fatal accidents per 10-minute isochrone is depicted in figure 2; 45.0% of fatal accidents took less than 27 minutes of transport and 85.8% took less than 54 minutes of transport.
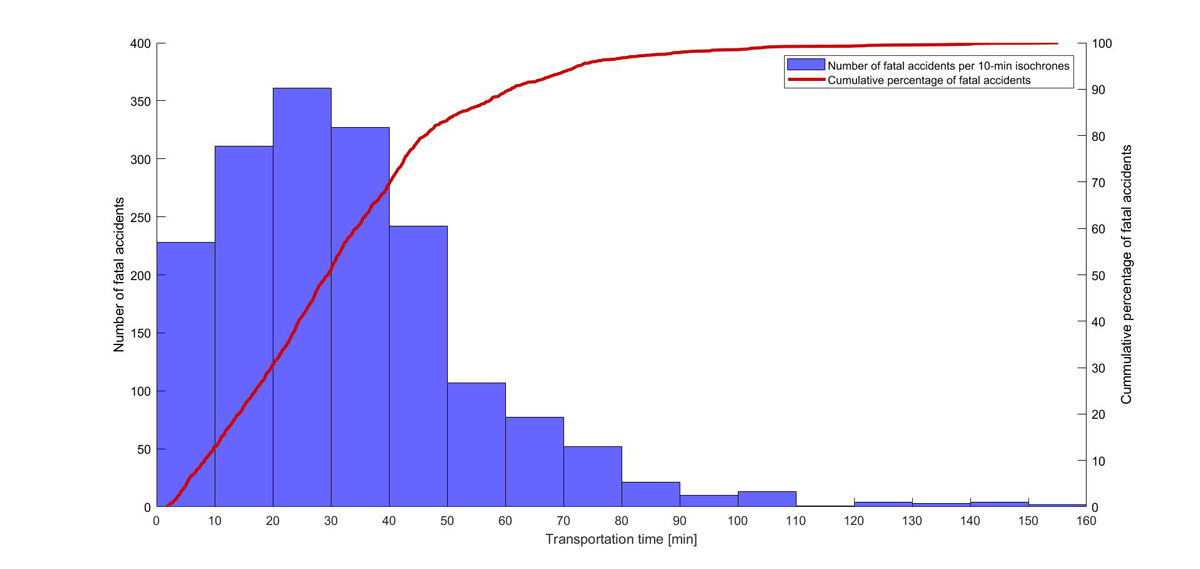
Figure 2 Relationship between the number of fatal accidents and transportation time to the trauma centre (Switzerland 2011—2017).
The average proportion of fatal accidents to the total number of serious accidents was 2.8%, and this increased with longer transport times to the trauma centre (fig. 3). Indeed, there was an association between mortality and transport time, which was notably linear up to 80 minutes, with an average increase in mortality of 0.4% per 10-minute isochrone.
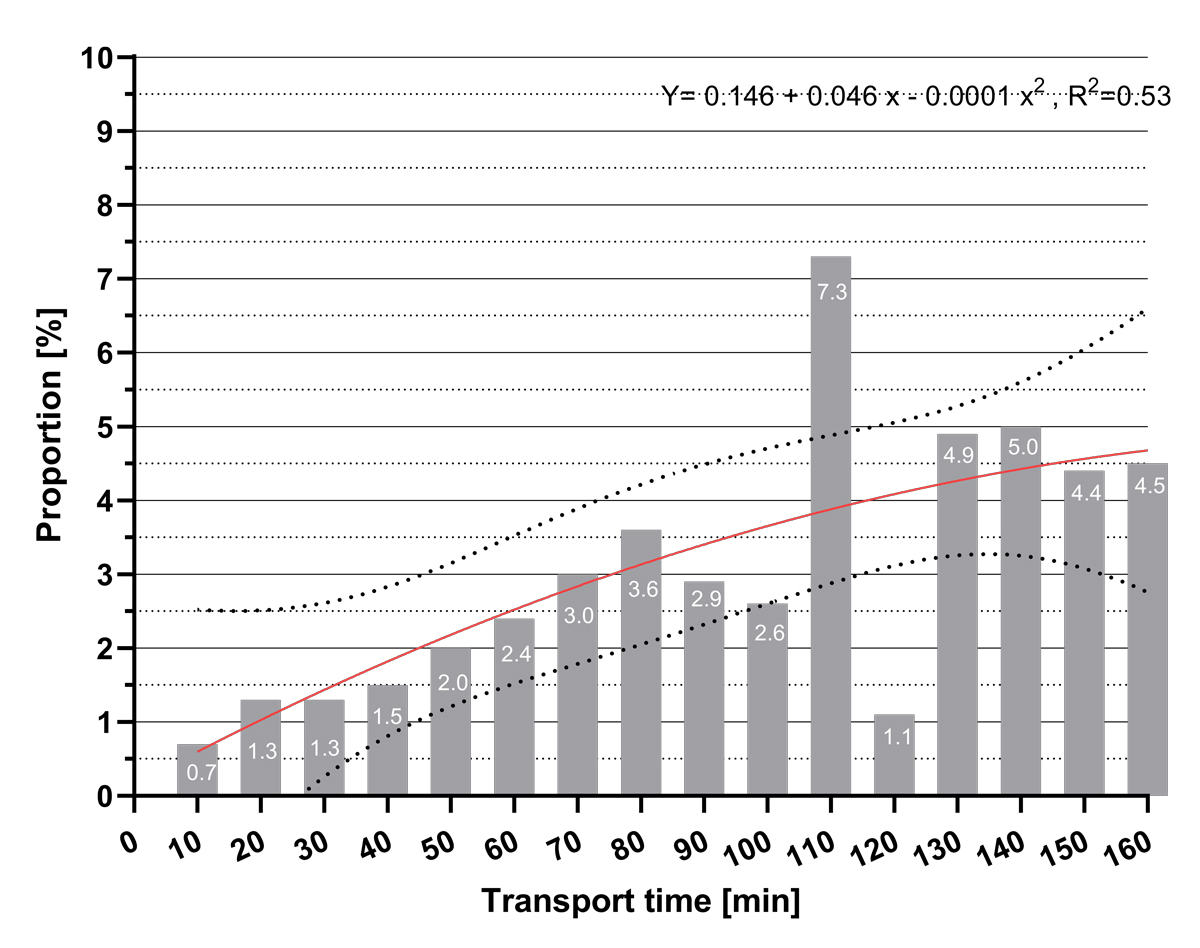
Figure 3 Proportion of fatalities as a function of time for 10-minute isochrones; dashed lines indicate the 95% confidence interval.
The number of fatalities attributed by the modelling to each trauma centre and the proportion of patients admitted after 27 minutes of transportation from the crash site varied widely (table 1). According to our model, Bern was the centre with the most attributed cases. The trauma centres with the highest percentage of fatal accidents admitted in ≥27 minutes were Bern and Chur at nearly 80%, whereas Geneva, at 10%, was the centre with the lowest rate.
Table 1Number of fatal accidents attributed to each trauma center in Switzerland and the number of fatal accidents above the 27-minute cutoff for compliance with the Golden Hour rule.
| Trauma centre | Fatal accidents (n) | Transport time from site to trauma centre ≥27 minutes | |
| n | % (95% CI) | ||
| Geneva | 89 | 9 | 10.1 (4.7—18.3) |
| Zurich | 203 | 65 | 32.0 (25.7–38.9) |
| Winterthur | 108 | 45 | 41.7 (32.3–51.5) |
| Sion | 106 | 48 | 45.3 (35.6–55.2) |
| Basel | 110 | 50 | 45.5 (35.9–55.2) |
| Aarau | 127 | 58 | 45.7 (36.8–54.7) |
| St Gallen | 100 | 47 | 47.0 (36.9–57.2) |
| Lausanne | 187 | 111 | 59.4 (51.9–66.5) |
| Lucerne | 184 | 112 | 60.1 (53.4–68.0) |
| Lugano | 90 | 59 | 65.6 (54.8–75.3) |
| Bern | 325 | 258 | 79.9 (74.6–83.7) |
| Chur | 134 | 108 | 80.6 (72.9–86.9) |
| Total | 1763 | 793 | 45.0 (42.6–47.3) |
95% CI: 95% confidence interval
Finally, only Winterthur and Zurich had overlapping territories with a modelling time of ≤27 minutes, with Winterthur being able to rescue 37 (18.2%) of the accidents attributed to Zurich and Zurich being able to rescue 12 (11%) of those attributed to Winterthur.
This work is the first, to our knowledge, to show that the current distribution of trauma centres allows adequate coverage of the Swiss plateau, with travel times for the transport of road accident victims within the time limits compatible with the Golden hour principle. In addition, our data support a link between return transportation time and mortality.
The location of the trauma centres in Switzerland is adequate, since there is little overlap in their coverages. Our data therefore support the report evaluating the 12 Swiss trauma centres that stated that their distribution was judicious, taking into account geographical peculiarities and favouring optimal access of patients to definitive treatment without long travel, regardless of weather conditions [17].
However, the plateau and large cities were better covered than were the mountainous areas. A new trauma centre in a remote area would, however, have insufficient activity to maintain the required skill level, not to mention the excessive costs. In the United States, a Level I trauma centre must receive at least 1,200 patients per year or have 240 admissions with an Injury Severity Score greater than 15 [18], a requirement that most Swiss trauma centres do not currently meet.
Our work has shown an association between prehospital transport time and the proportion of deaths, with a 0.4% increase in mortality for every 10 minutes. Our results are therefore similar to those of a Canadian study, in which a transport time of more than 30 minutes was associated with a 66% increase in the risk of mortality for road accidents [10]. However, this association disappeared if deaths on site were excluded, which we cannot do with the FEDRO database. This correlation between prehospital time and mortality is, however, debatable. In a recent study, a longer prehospital time was associated with lower mortality [19], as it reflected essential actions for patient survival, such as medication administration, ventilation or patient retrieval. However, the study did not specify whether patients who died during transport were included in their survival calculations. If excluded, this would lead to a biased optimistic estimate of the effect of time, a phenomenon known as "healthy worker survivor bias" [19–21]. The debate between a "scoop and run" vs a "stay and play" strategy is still unresolved. "Scoop and run" may be superior in urban areas with short transport times, whereas “stay and play” would benefit patients in rural areas, allowing for interventions required for stabilisation prior to a longer transport [22]. Outside the field of trauma, out-of-hospital cardiac arrest patients cared for in prehospital systems with a "scoop and run" strategy had a lower probability of survival to hospital discharge [23]. However, the strategy applied by rescuers in our study is unknown.
Our study is an attempt to model the system of care for serious road traffic injuries in Switzerland on the basis of publicly available data. Our modelling suffers from limitations related to the quality of the national data necessary for researchers who are attempting to establish scientifically robust findings. First, although geolocalisation of accidents is accessible, data on patient status and outcomes are lacking. For example, the presence of hypotension and the type of injury (blunt vs penetrating) are not available, but these variables would help to better stratify patients' short-term prognosis. In addition, mortality on site or in the first 30 days is aggregated in the public database. However, deaths — on site, in the hours following the accident or within 30 days — have very different causes, from injuries that are immediately fatal to infections or organ failure in the event of late death [24, 25]. These different causes require different solutions, for which our work cannot provide any insight. A second limitation is the impossibility of obtaining the real timing of the different components of the overall rescue mission, for several reasons. The first is the inability to identify the vehicle type used for transport. The use of a rescue helicopter is frequent in Switzerland, with the REGA Company, the main actor in Switzerland, capable of reaching any point of the territory in 15 minutes at the most from one of its 12 bases. However, it intervened in only 862 road accidents in 2019, a small fraction of the total number [26], but possibly a higher percentage of those with a fatal outcome. Nonetheless, the duration of helicopter transport is not much shorter than that of land ambulance, mainly because of the time required to prepare the helicopter [27]. Other US studies suggest that helicopter transport is slightly shorter, mainly in rural areas [28, 29]. Since distances are much shorter in Switzerland, the impact of helicopter transport on the time between the accident and the arrival at a Swiss trauma centre is unknown. A study in nearby Germany shows an increased mission time by helicopter compared with that of land ambulance because of a greater number of actions performed on site [30]. The third limitation is the inability to know the exact starting point of the ambulance for each mission, since several bases are likely to provide an ambulance for a given accident. Moreover, no official national register exists about their location and whether they operate year-round. Fourth, it is possible that some patients may have been transported to a local hospital before their secondary transfer to a trauma centre. Finally, our model shows a shorter travel time compared with real data. The road data used were from the year 2019. It is therefore possible that road conditions have changed and thus contributed to some inaccuracy. In addition, the traffic conditions at the time of the accident could not be taken into consideration. The use of a correction constant improved the overall accuracy of the modelling, but it remains an approximation.
Management and referral of trauma patients to a trauma centre in a minimal amount of time is a challenge for any healthcare system. In this modelling work, we show that the current layout of trauma centres allows adequate coverage of the Swiss plateau and that a longer transportation time to the nearest trauma centre is potentially associated with a greater probability of death within 30 days. However, our conclusions need to be confirmed by real-world data because of the assumptions required to circumvent the limitations of currently available public data. This work confirms the importance of a nationwide trauma registry, with homogeneous procedures for data collection, in order to improve public health safety. The Swiss trauma registry was created in 2015 (http://www.swisstraumaboard.ch/index.php) and will eventually be an essential tool for benchmarking and improving practices in the care of severe trauma victims in our country.
Olivier Hugli, Raphael Diserens, Stéphane Joost, and Clotilde Marmy designed the study. Clotilde Marmy worked on the geospatial data and developed the model and maps. Mathieu Pasquier provided the anonymised real data. Raphael Diserens collected the data and wrote the first draft of the manuscript. All coauthors critically revised the manuscript.
No financial support and no potential conflict of interest relevant to this article was reported.
The appendix is available in the PDF version of the manuscript.
1. Vos T , Lim SS , Abbafati C , Abbas KM , Abbasi M , Abbasifard M , et al.; GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020 Oct;396(10258):1204–22. https://doi.org/ https://doi.org/10.1016/S0140-6736(20)30925-9
2 Office fédéral de la statistique. Accidents de la route. Accidents de la route 2019. Available from: https://www.bfs.admin.ch/bfs/fr/home/statistiques/mobilite-transports/accidents-impact-environnement/accidents-transports/route.html
3 Jones AP , Bentham G . Emergency medical service accessibility and outcome from road traffic accidents. Public Health. 1995 May;109(3):169–77. https://doi.org/ https://doi.org/10.1016/S0033-3506(05)80049-6
4 Vanderschuren M , McKune D . Emergency care facility access in rural areas within the golden hour? Western Cape case study. Int J Health Geogr. 2015 Jan;14(1):5 https://www.ncbi.nlm.nih.gov/pubmed/25595608https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4305393/pdf/12942_2014_Article_618.pdf https://doi.org/10.1186/1476-072X-14-5
5 Gauss T , Ageron FX , Devaud ML , Debaty G , Travers S , Garrigue D , et al.; French Trauma Research Initiative . Association of prehospital time to in-hospital trauma mortality in a physician-staffed emergency medicine system. JAMA Surg. 2019 Dec;154(12):1117–24 https://www.ncbi.nlm.nih.gov/pubmed/31553431https://jamanetwork.com/journals/jamasurgery/articlepdf/2751937/jamasurgery_gauss_2019_oi_190059.pdf https://doi.org/10.1001/jamasurg.2019.3475
6 Osterwalder JJ . Can the “golden hour of shock” safely be extended in blunt polytrauma patients? Prospective cohort study at a level I hospital in eastern Switzerland. Prehosp Disaster Med. 2002 Apr-Jun;17(2):75–80 https://www.ncbi.nlm.nih.gov/pubmed/12500730 https://doi.org/10.1017/s1049023x00000212 https://doi.org/10.1017/S1049023X00000212
7 Rogers FB , Rittenhouse KJ , Gross BW . The golden hour in trauma: dogma or medical folklore? Injury. 2015 Apr;46(4):525–7 https://www.ncbi.nlm.nih.gov/pubmed/25262329 https://doi.org/10.1016/j.injury.2014.08.043
8 Brown JB , Rosengart MR , Forsythe RM , Reynolds BR , Gestring ML , Hallinan WM , et al. Not all prehospital time is equal: influence of scene time on mortality. J Trauma Acute Care Surg. 2016 Jul;81(1):93–100 https://www.ncbi.nlm.nih.gov/pubmed/26886000https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4915972/pdf/nihms760448.pdf https://doi.org/10.1097/TA.0000000000000999
9 Nicholl J , West J , Goodacre S , Turner J . The relationship between distance to hospital and patient mortality in emergencies: an observational study. Emerg Med J. 2007 Sep;24(9):665–8 https://www.ncbi.nlm.nih.gov/pubmed/17711952https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2464671/pdf/665.pdf https://doi.org/10.1136/emj.2007.047654
10 Tansley G , Schuurman N , Bowes M , Erdogan M , Green R , Asbridge M , et al. Effect of predicted travel time to trauma care on mortality in major trauma patients in Nova Scotia. Can J Surg. 2019 Apr;62(2):123–30 https://www.ncbi.nlm.nih.gov/pubmed/30907993https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6440889/pdf/0620123.pdf https://doi.org/10.1503/cjs.004218
11 Spoerri A , Egger M , von Elm E ; for the Swiss National Cohort Study . Mortality from road traffic accidents in Switzerland: longitudinal and spatial analyses. Accid Anal Prev. 2011 Jan;43(1):40–8 https://www.ncbi.nlm.nih.gov/pubmed/21094295 https://doi.org/10.1016/j.aap.2010.06.009
12 Décision concernant la planification de la médecine hautement spécialisée (MHS) dans le domaine de la prise en charge des blessés graves.(2011). Available from: https://www.gdk-cds.ch/fileadmin/docs/public/gdk/themen/hsm/hsm_spitalliste/Trauma_2011_fr.pdf
13. QGIS Development Team . 2019. QGIS Geographic Information System. Open Source Geospatial Foundation Project. http://qgis.osgeo.org
14 Géoportail fédéral. Available from: https://data.geo.admin.ch/ch.astra.unfaelle-personenschaeden_alle/
15 Spaite DW , Valenzuela TD , Meislin HW , Criss EA , Hinsberg P . Prospective validation of a new model for evaluating emergency medical services systems by in-field observation of specific time intervals in prehospital care. Ann Emerg Med. 1993 Apr;22(4):638–45.https://www.ncbi.nlm.nih.gov/pubmed/8457088 https://doi.org/ https://doi.org/10.1016/S0196-0644(05)81840-2
16 Anselin L , Syabri I , Kho Y . GeoDa: An Introduction to Spatial Data Analysis. Geogr Anal. 2006;38(1):5–22. https://doi.org/10.1111/j.0016-7363.2005.00671.x
17 Conférence suisse des directrices et directeurs cantonaux de la santé. Traitement des blessés graves 2017 [cited 2020 31.12]. Available from: https://www.gdk-cds.ch/fileadmin/docs/public/gdk/themen/hsm/HSM-Bereiche/7_bt_trauma_re1_zuteilung_schlussbericht_publ_20170309_def_f.pdf
18 American College of Surgeons, Committee on Trauma . Resources for optimal care of the injured patient. 2014. Available at: https://www.facs.org/-/media/files/quality-programs/trauma/vrc-resources/resources-for-optimal-care.ashx
19 Clements TW , Vogt K , Hameed SM , Parry N , Kirkpatrick AW , Grondin SC , et al. Does increased prehospital time lead to a “trial of life” effect for patients with blunt trauma? J Surg Res. 2017 Aug;216:103–8 https://www.ncbi.nlm.nih.gov/pubmed/28807193 https://doi.org/10.1016/j.jss.2017.04.027
20. Andersen LW , Grossestreuer AV , Donnino MW . “Resuscitation time bias”-A unique challenge for observational cardiac arrest research. Resuscitation. 2018 Apr;125:79–82 https://www.ncbi.nlm.nih.gov/pubmed/2942597510.1016/j.resuscitation.2018.02.006294259751873-1570 https://doi.org/10.1016/j.resuscitation.2018.02.006
21 Swain SA , Stiff G . Issues and challenges for research in major trauma. Emerg Med J. 2018 Apr;35(4):267–9. https://doi.org/10.1136/emermed-2017-207082https://www.ncbi.nlm.nih.gov/pubmed/29321209 https://doi.org/10.1136/emermed-2017-207082
22 Smith RM , Conn AK . Prehospital care - scoop and run or stay and play? Injury. 2009;40 Suppl 4S23-6. doi: https://dx.doi.org/https://doi.org/10.1016/j.injury.2009.10.033 https://www.ncbi.nlm.nih.gov/pubmed/19895949
23. Grunau B , Kime N , Leroux B , Rea T , Van Belle G , Menegazzi JJ , et al. Association of intra-arrest transport vs continued on-scene resuscitation with survival to hospital discharge among patients with out-of-hospital cardiac arrest. JAMA. 2020 Sep;324(11):1058–67. https://doi.org/10.1001/jama.2020.14185
24 Bardes JM , Inaba K , Schellenberg M , Grabo D , Strumwasser A , Matsushima K , et al. The contemporary timing of trauma deaths. J Trauma Acute Care Surg. 2018 Jun;84(6):893–9 https://www.ncbi.nlm.nih.gov/pubmed/29521807 https://doi.org/10.1097/TA.0000000000001882
25 Gunst M , Ghaemmaghami V , Gruszecki A , Urban J , Frankel H , Shafi S . Changing epidemiology of trauma deaths leads to a bimodal distribution. Proc Bayl Univ Med Cent. 2010 Oct;23(4):349–54 https://www.ncbi.nlm.nih.gov/pubmed/20944754 https://doi.org/10.1080/08998280.2010.11928649
26. Swiss Air-Rescue Rega . Rega 2019 with Annual Report 2019 . Available from: https://www.rega.ch/fileadmin/seiteninhalt/4_Aktuell/2_Publikationen/2_Jahresbericht/Jahresbericht_2019_en.pdf
27 Svenson JE , O’Connor JE , Lindsay MB . Is air transport faster? A comparison of air versus ground transport times for interfacility transfers in a regional referral system. Air Med J. 2006 Jul-Aug;25(4):170–2 https://www.ncbi.nlm.nih.gov/pubmed/16818167 https://doi.org/10.1016/j.amj.2006.04.003
28 Carr BG , Caplan JM , Pryor JP , Branas CC . A meta-analysis of prehospital care times for trauma. Prehosp Emerg Care. 2006 Apr-Jun;10(2):198–206 https://doi.org/10.1080/10903120500541324
29. Zhu TH , Hollister L , Opoku D , Galvagno SM Jr . Improved survival for rural trauma patients transported by helicopter to a verified trauma center: a propensity score analysis. Acad Emerg Med. 2018 Jan;25(1):44–53. https://doi.org/10.1111/acem.13307
30 Andruszkow H , Hildebrand F , Lefering R , Pape HC , Hoffmann R , Schweigkofler U . Ten years of helicopter emergency medical services in Germany: do we still need the helicopter rescue in multiple traumatised patients? Injury. 2014;45 Suppl 3S53-8. doi: https://dx.doi.org/https://doi.org/10.1016/j.injury.2014.08.018 https://www.ncbi.nlm.nih.gov/pubmed/25284235