Appendicitis and cholecystitis during the COVID-19 outbreak: a multicentre experience
DOI: https://doi.org/10.4414/SMW.2021.w30017
Hugo
Teixeira Farinhaa, Jérôme
Gilgiena, Luca
Di Mare b, Pierre
Fournier c, Riadh
Ksontini d, Andrew
Munday e, Cosimo
Scarpaf, Nicolas
Demartines a
aDepartment of Visceral Surgery, Lausanne University Hospital (CHUV), University of Lausanne UNIL, Switzerland
bDepartment of General and Visceral Surgery, Morges Hospital (EHC), Switzerland
cDepartment of General and Visceral Surgery, Nyon Hospital (GHOL), Switzerland
dDepartment of General and Visceral Surgery, Rennaz Hospital (HRC), Switzerland
eDepartment of General and Visceral Surgery, Payerne Hospital (HIB), Switzerland
fDepartment of General and Visceral Surgery, Yverdon Hospital (EHNV), Switzerland
Summary
BACKGROUND: The aim of this study was to assess diagnosis severity, perioperative management and outcomes of two common urgent general surgery situations, appendicitis and cholecystitis, during the COVID-19 outbreak in a region with a high incidence of COVID.
METHODS: Retrospective analysis of all appendicitis and cholecystitis cases in a region of western Switzerland (population 850,000) during the first pandemic peak. Primary endpoints were delay after first symptoms to consultation and delay to surgery. Secondary endpoints were disease severity and postoperative outcome compared with the same period in 2019.
RESULTS: 214 patients were included: 99 during the 2020 pandemic and 115 in 2019. Median time to consultation for appendicitis was 48 hours (interquartile range [IQR] 24–96) in 2020 and 24 hours (12–36) in 2019 (p = 0.004); for cholecystitis, it was 48 hours (24–96) in 2020 and 36 hours (24–72) in 2019 (p = 0.28). Median time to surgery after consultation for appendicitis was 6.5 hours (IQR 4–18) in 2020 and 7.3 hours (5–9) in 2019 (p = 0.68), for cholecystitis 20 hours (12–48) in 2020 and 23 hours (14–39) in 2019 (p = 0.91). More antibiotics were prescribed after appendectomy in 2020 (46 vs 31%, p = 0.026). Significantly more perforations/abscesses related to appendicitis and cholecystitis were observed in 2020 during the COVID-19 outbreak (p = 0.007 and p = 0.044, respectively). No differences were found for postoperative complications and length of stay.
CONCLUSIONS: A delay in patients’ arrival at the emergency room was observed for appendicitis. No delay to surgery during the pandemic was observed. A higher rate of perforations and abscesses associated with appendicitis and cholecystitis was observed during the pandemic period. Morbidity and reoperation rate did not change.
Introduction
The current COVID-19 pandemic had a massive impact on the entire healthcare organisation because of the large flow of sick patients. In addition to the restrictions implemented at a political level [1], every hospital underwent widespread internal reorganisation in order to receive and treat a large number of COVID-19 patients [2, 3]. Thus, centres reorganised their emergency department [2] and increased their intensive care units capacity with some areas, such as some of the operating rooms, dedicated to ventilated COVID-19 patients. Although surgeons were not in the frontline of the pandemic, they had to reduce elective surgeries and adapt their global surgical management by prioritisation of procedures that were urgent and for life-threatening conditions [4, 5].
There were several reasons to adapt surgical strategies within hospitals: to preserve resources, hospital staff, equipment and hospital capacity for COVID-19 patients, when the extent of the outbreak was initially unknown. It was also important to protect patients and surgical staff from the unknown risks of transmission in the hospital and operating rooms, and to avoid whenever possible treatment delay in surgical non-COVID-19 patients [5]. Some hospitals developed a management algorithm for proven or suspected COVID-19 patients needing emergency surgery [6, 7]. The surgical management of oncological patients was widely discussed, in Italy [8, 9] and China, with guidelines on selection of patients who should be operated or not [10].
There are few data on the outcome of basic general surgery during the pandemic. Delayed access to the emergency room by the paediatric population resulting from fear of COVID-19 was observed in northern Italy [11] and in Spain during the pandemic [12]. A similar delay was described in Taiwan during the 2002 SARS outbreak [13]. Moreover, an editorial in Journal de Chirurgie Viscérale suggested that delayed consultation in the ER may have impacted urgent digestive surgery [14]. The only available retrospective data on this specific aspect of delay for general surgery during an epidemic was a paper about the Hong-Kong influenza epidemic in New York in 1969 [15]. Back then, an increased rate of perforated appendicitis was observed. The lack of literature on this topic may be explained by the absence of a similar event, such as the COVID-19 pandemic, during recent decades.
Aim
The current study assessed the perioperative management and outcome of two basic pathologies, acute appendicitis and acute cholecystitis, during the COVID-19 pandemic in a region of western Switzerland with five county and one academic hospital (population area with 850,000 inhabitants).
Materials and methods
This retrospective study aimed to assess all patients in canton Vaud who came through the emergency room with appendicitis or cholecystitis requiring surgery during the peak of the COVID-19 pandemic in spring 2020, and to compare them with similar patients during a similar period in 2019. The Swiss lockdown was decreed by the Government on 15 March 2020. For this reason, the period of 15 March 2020 to 20 April 2020 and the same interval in 2019 (15 March 2019 to 20 April 2019) were selected as study period. The primary endpoints of this study were the time to emergency room consultation after first symptoms and to surgery (access to an operating room after diagnosis) of the patients during and prior to the COVID-19 pandemic.
Secondary endpoints were perioperative outcomes: severity of the findings (perforation, abscess), operation duration, postoperative complications, duration of post-operative antibiotics, length of hospital stay and readmission rate.
The study was approved by local Commission on Ethics in Human Research (CER-VD, protocol number 2019-01265) and was conducted in compliance with the current version of the Declaration of Helsinki.
Study design and methodology
This was a retrospective comparison between the two study groups (during the COVID-19 pandemic or 1 year before) based on the above-mentioned relevant clinicopathological parameters, surgical parameters and outcomes.
Data collected from all participating sites included demographic variables (age, gender, American Society of Anesthesiologists [ASA] score); medical history related to the surgical emergency (consultation delay after first symptoms, radiological workup); surgical findings (intraoperative findings, contamination, intervention duration, intraoperative complications, histopathology); postoperative data (complications, length of stay, antibiotic use). Data were retrospectively collected within each reference centre. These were all standard data, collected on a routine basis and available in the patients’ electronic medical charts and in operating room planning software in all six hospitals.
Inclusion criteria
All consecutive adult patients (>18 years) operated on for appendicitis or cholecystitis who consulted the ER in either of the six participating public hospitals in the canton of Vaud (University Hospital of Lausanne, Hospitals of Morges, Nyon, Yverdon-les-Bains, Payerne, Rennaz). Two periods were assessed, during the COVID-19 peak and 1 year before COVID during the same period in 2019. Paediatric patients (under 18 years) and adults with biliary pancreatitis requiring cholecystectomy were excluded.
Statistics and analysis
Standard statistics were used to compare the two cohorts (2020 and 2019). Continuous variables were presented as mean with standard deviation (SD), or median with range or interquartile range (IQR) for skewed data. Categorical variables were reported as frequencies (%). Categorical data were compared with the use of the chi-square test. Continuous variables were analysed using the Mann-Whitney U- or t-test depending on the normality of the variables and the variances. All statistical tests were two-sided and a level of 0.05 indicated statistical significance. All statistical analyses were performed using SPSS 26 for Mac OS and graphics were drawn using GraphPad software PRISM for MAC version 8.3.0.
Results
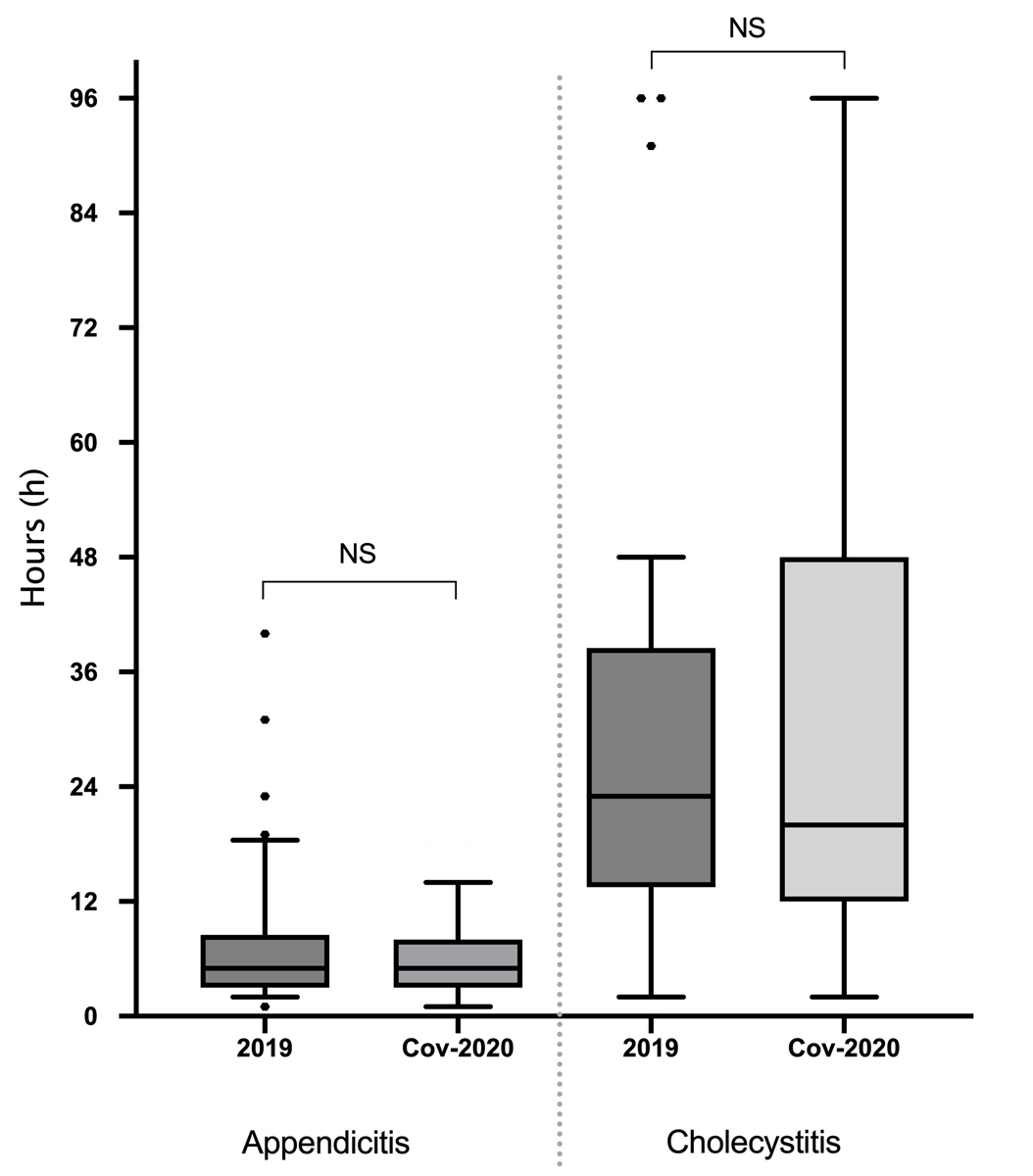
Two hundred and fourteen consecutive patients were included in the analysis: 99 patients during the COVID-19 pandemic in 2020 (68 appendicitis, 31 cholecystitis) and 115 in 2019 for the same period (85 appendicitis, 30 cholecystitis). Median time (IQR)to consultation in the emergency room after first symptoms for appendicitis was 48 hours (24–96) in 2020 and 24 hours (12–36) in 2019 (p = 0.004). For cholecystitis, median time (IQR) to consultation in the emergency room was 48 hours (24–96) in 2020 and 36 hours (24–72) in 2019 (p = 0.28). Median time (IQR) to surgical intervention after consultation in the emergency room for appendicitis was 6.5 hours (4–18) in 2020 and 7.3 hours (5–9) in 2019 (p = 0.68). For cholecystitis, median time to surgery was 20 hours (12–48) in 2020 and 23 hours (14–39) in 2019 (p = 0.91). Primary outcomes are displayed in figures 1 and 2.

Figure 1 Delay (hours) to consultation in the emergency room after first symptoms for appendicitis and cholecystitis: comparison between 2019 and 2020. Appendicitis: p = 0.004, cholecystitis: p = 0.284. Median (interquartile range), NS: non-significant.
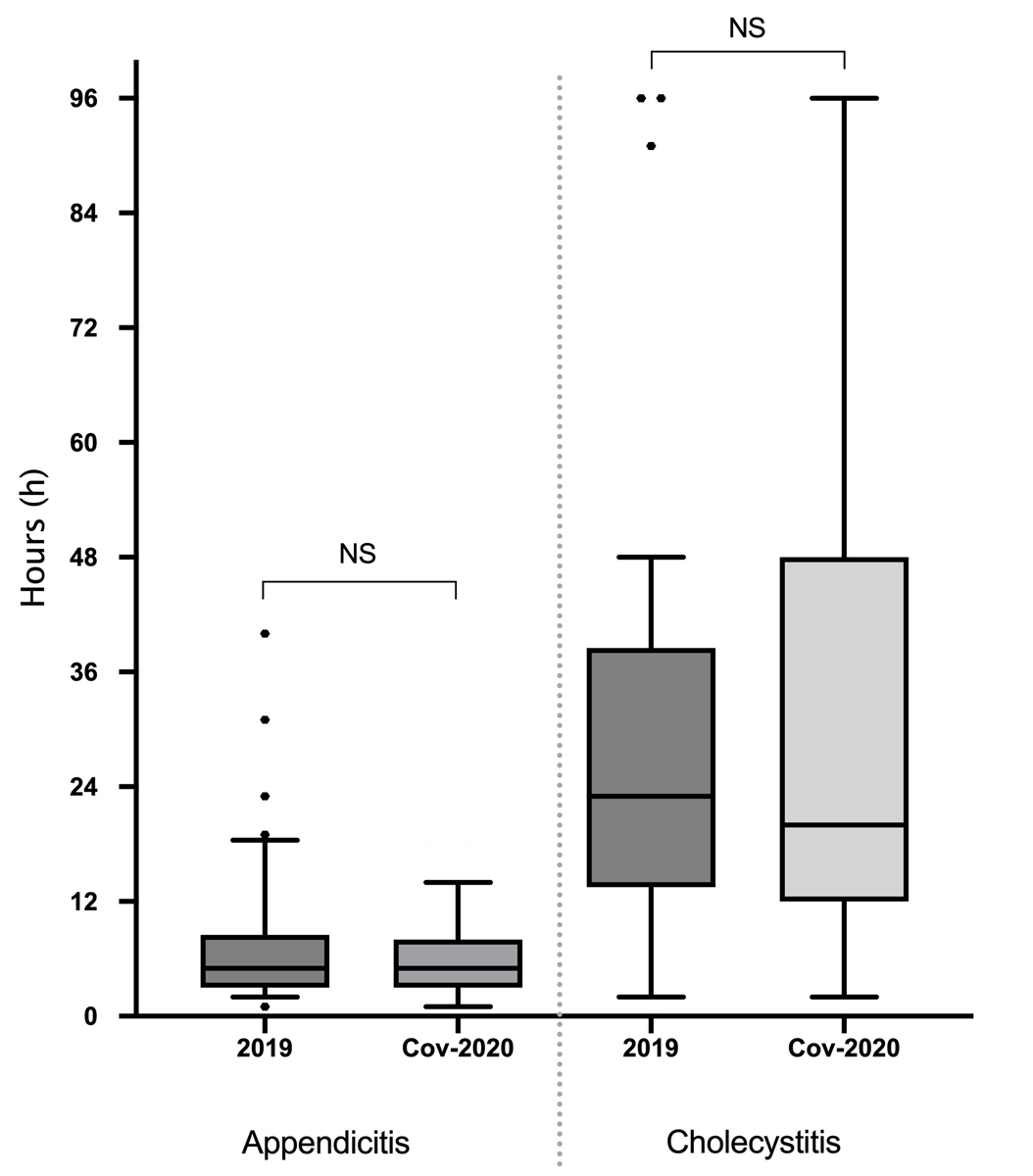
Figure 2 Delay (hours) to surgery after consultation in the emergency room for appendicitis and cholecystitis: comparison between 2019 and 2020. Appendicitis: p = 0.687, cholecystitis: p = 0.914. Median (interquartile range), NS: non-significant.
For both appendicitis and cholecystitis, no significant difference was observed in demography and diagnostic approach between the groups (2020 vs 2019). Significantly more cases of perforated/abscessed appendicitis and abscessed cholecystitis were observed in 2020 during the COVID-19 outbreak (p = 0.007 and p= 0.044, respectively). Significantly more postoperative antibiotics were prescribed after appendectomy (p = 0.026). There were no differences between the 2020 and 2019 groups in operative time (minutes), postoperative complications and length of stay (days). One patient required a reoperation for lavage post-appendectomy in 2019 (1%) and one patient underwent postoperative drainage after appendectomy in 2020 during the COVID-19 outbreak (1.4%). There was no readmission in either group. Secondary outcomes are displayed in table 1 for appendicitis and in table 2 for cholecystitis.
Table 1Baseline demographics, diagnosis, surgical and post-operative details for appendicitis: comparison between 2020 and 2019.
|
|
Appendicitis
2019
(n = 85)
|
Appendicitis
2020
(n = 68)
|
p-value
|
|
Demographics
|
| Gender, n (%) |
Male |
46 (54%) |
40 (59%) |
0.627 |
| Female |
39 (46%) |
28 (41%) |
| Age (years), median (IQR) |
|
29 (21–49) |
36 (26–70) |
0.070 |
| ASA score, n (%) |
I |
38 (45%) |
29 (43%) |
0.948 |
| II |
40 (47%) |
35 (51%) |
| III‒IV |
7 (8%) |
4 (6%) |
|
Diagnosis details
|
| Imaging, n (%) |
Ultrasound |
48 (56%) |
31 (45%) |
0.213 |
| CT-scan |
49 (57%) |
47 (70%) |
|
Surgical details
|
|
|
|
|
| Surgery duration (min), median (IQR) |
|
55 (40–72) |
55 (45–77) |
0.412 |
| Perforated/abscess, n (%) |
|
17 (20%) |
27 (40%) |
0.007
|
| Surgical drain, n (%) |
|
2 (2%) |
6 (9%) |
0.095 |
|
Post-operative details
|
| Post-op. antibiotics, n (%) |
|
24 (28%) |
31 (46 %) |
0.026
|
| Post-op. antibiotics (days), mean (SD) |
|
7 (3.2) |
8 (6.9) |
0.712 |
| 30-day complication (Clavien-Dindo) [21] |
I |
1 (1%) |
2 (3%) |
0.122 |
| II |
4 (5%) |
5 (7%) |
| III |
‒ |
2 (3%) |
| Length of stay (days), mean (SD) |
|
1.5 (1.7) |
2.5 (3.7) |
0.385 |
Table 2Baseline demographics, diagnosis, surgical and post-operative details for Cholecystitis: comparison between 2020 and 2019.
|
|
Cholecystitis 2019 (n = 30)
|
Cholecystitis 2020 (n = 31)
|
p-value
|
|
Demographics
|
| Gender, n (%) |
Male |
10 (33%) |
15 (48%) |
0.231 |
| Female |
20 (66%) |
16 (52%) |
| Age (years), median (IQR) |
|
51 (38–66) |
54 (37–74) |
0.751 |
| ASA score, n (%) |
! |
5 (16%) |
5 (16%) |
0.933 |
| II |
20 (68%) |
21 (68%) |
| III–IV |
5 (16%) |
5 (16%) |
|
Diagnosis details
|
| Imaging, n (%) |
Ultrasound |
21 (70%) |
25 (80%) |
0.313 |
| CT-scan |
11 (37%) |
11 (35%) |
|
Surgical details
|
| Surgery duration (min), median (IQR) |
|
90 (74–116) |
90 (75–114) |
0.722 |
| Perforated/abscess, n (%) |
|
4 (13%) |
11 (35%) |
0.044
|
| Surgical drain, n (%) |
|
3 (10%) |
6 (20%) |
0.301 |
|
Post-operative details
|
| Post-op antibiotics, n (%) |
|
10 (33%) |
14 (45 %) |
0.342 |
| Post-op antibiotics (days), mean (SD) |
|
8 (10.8) |
7 (3.4) |
0.373 |
| 30-day complication (Clavien-Dindo) [21] |
I |
3 (10%) |
2 (6%) |
0.412 |
| II |
1 (3%) |
‒ |
| III |
‒ |
1 (3%) |
| Length of stay (days), mean (SD) |
|
2.5 (3.3) |
2.2 (1.6) |
0.556 |
Discussion
The present study suggests that the COVID-19 pandemic had a negative influence on delay of patients’ arrival at the emergency room. Patients diagnosed with appendicitis waited significantly longer to go to the hospital, with a median of 48 hours (+24 hours compared with 2019, +100%). This was also reported by a Spanish group with consultation delay increasing by 52% during the pandemic for all surgical emergencies in an adult population [12]. The same observation was made in paediatric populations of northern Italy and Australia [11, 16]. In contrast, an Israeli multicentre study carried out between January and April 2020 on 378 patients did not find any delay in emergency room consultation [17]. Fear of viral and nosocomial infection may explain the increased time to consultation [12]. A similar fear was observed in the present study, as mild abdominal pain may have been considered a minor disease, making the patients reluctant to go to the emergency room at the onset of symptoms. Another possible explanation could be that population thought that emergency rooms and hospitals were overwhelmed during the peak of pandemic. Patients therefore tried to avoid hospital. Surprisingly, time to consultation in patients with cholecystitis showed an apparent but non-significant increase by 30% during pandemic. One of the explanations may be the fact that the time to emergency room consultation in cholecystitis for our group was longer during the non-COVID period, as compared with appendicitis. No other paper discussed specifically cholecystitis during the COVID-19 pandemic.
Although consultation delay increased during the pandemic, time to access to the operating room did not change (p = 0.72). Despite the fact that most hospitals underwent widespread internal reorganisation to manage COVID-19 patient flow, availability of emergency operating rooms for general emergency surgery remained unaffected by the pandemic, at least in our region. The reorganisation allowed both hospitalisation of COVID-19 patients and standard emergency surgery and seemed therefore adequate. A similar observation was made by Cano-Valderrama et al. [12].
Some decrease in appendicitis and cholecystitis observed during the peak of the pandemic was described in three publications [12, 17, 18]. This was not the case with cholecystitis in our population (31 vs 30). A decrease in appendicitis (68 vs 85, −20%) was observed, and decreases of −3.3%, −33.4% −40.7% were reported in three studies [12, 17, 18]. These decreases are probably irrelevant, due to the short observation period during the pandemic peak. Moreover, appendicitis treated conservatively was not recorded. In the academic hospital, the only hospital with available data, there was no difference in the number of cases treated conservatively (two patients in 2020 and in 2019).
All patients operated on in 2020 had a COVID-19 screening test before surgery. Two patients with appendicitis were tested positive (3%). Both were operated on according to the institutional recommendations for safety in the operating room. The two operations were uneventful both during and after interventions, with a return to home on the same day for both patients.
No intraoperative complications occurred during the observation periods in 2020 and 2019. However, there were significantly more complicated cases of appendicitis with perforation and abscess in the 2020 group (+20%, p = 0.007). This is probably due to the delay to consultation. An increase in abscesses associated with cholecystitis was observed despite a similar delay between symptom onset and consultation in 2020 and 2019 (+23%, p = 0.004).
Of note, postoperative complications and length of stay remained similar for both study periods, despite the higher rate of complicated appendicitis (p = 0.12). However, significantly more antibiotics were prescribed postoperatively for appendicitis (+20%). Reoperations for lavage (one in 2019) and drainage (one in 2020) were marginal.
Although some differences are significant (e.g., perforated appendicitis), it is not possible to ascertain that these differences are not a coincidence. It would have been necessary to compare several control years to assess the real effect of COVID-19. However, it would have been too difficult to collect all this retrospective data for all centres. The main strength of the present study was that all patients of all six most affected hospitals by COVID-19 were included during the peak of the pandemic. Among COVID-19 patients requiring hospitalisation in the canton Vaud during the study period, 88% were hospitalised in one of the six participating public hospitals. The burden of COVID-19 was equally divided between centres: University Hospital of Lausanne had 31% of the total patients, the hospitals of Morges 11%, Nyon 9%, Yverdon-les-Bains 11%, Payerne 14% and Rennaz 12%. Therefore, downsizing of operative capacity in the participating hospitals was proportional. This covered the western Switzerland region where the epidemic was the most severe [19].
Availability of data and materials
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Author contributions
HTF, JG, LDM, PF, RK, AM, CS and ND meet all the criteria for the definition of authorship and contributed substantially to the manuscript. HTF and ND conceived and designed the study. HTF, JG and ND managed the data and analysed the data. All authors read and approved the final manuscript. ND is the corresponding author.
Prof. Nicolas Demartines, MD
Lausanne University Hospital (CHUV)
Rue du Bugnon 46
CH-1005 Lausanne
Demartines[at]chuv.ch
References
1.
European Centre for Disease Prevention and Control (ECDC)
. Agency of the European Union. Considerations relating to social distancing measures in response to COVID-19 – second update - Stockholm 2020. [Available from: https://www.ecdc.europa.eu/en/publications-data/considerations-relating-social-distancing-measures-response-covid-19-second
2.
Zangrillo A
,
Beretta L
,
Silvani P
,
Colombo S
,
Scandroglio AM
,
Dell’Acqua A
, et al.
Fast reshaping of intensive care unit facilities in a large metropolitan hospital in Milan, Italy: facing the COVID-19 pandemic emergency. Crit Care Resusc. 2020 Apr;22(2):91–4.
3.
Spina S
,
Marrazzo F
,
Migliari M
,
Stucchi R
,
Sforza A
,
Fumagalli R
. The response of Milan’s Emergency Medical System to the COVID-19 outbreak in Italy. Lancet. 2020 Mar;395(10227):e49–50. https://doi.org/10.1016/S0140-6736(20)30493-1
4.
Centers for Disease Control and Prevention (CDC)
. Coronavirus Disease 2019 (COVID-19) 2020. [Available from: https://www.cdc.gov/coronavirus/2019-nCoV/index.html
5.
Vogler SA
,
Lightner AL
. Rethinking how we care for our patients in a time of social distancing during the COVID-19 pandemic. Br J Surg. 2020 Jul;107(8):937–9. https://doi.org/10.1002/bjs.11636
6.
Di Saverio S
,
Khan M
,
Pata F
,
Ietto G
,
De Simone B
,
Zani E
, et al.
Laparoscopy at all costs? Not now during COVID-19 outbreak and not for acute care surgery and emergency colorectal surgery: A practical algorithm from a hub tertiary teaching hospital in Northern Lombardy, Italy. J Trauma Acute Care Surg. 2020 Jun;88(6):715–8. https://doi.org/10.1097/TA.0000000000002727
7.
Liu Z
,
Zhang Y
,
Wang X
,
Zhang D
,
Diao D
,
Chandramohan K
, et al.
Recommendations for Surgery During the Novel Coronavirus (COVID-19) Epidemic. Indian J Surg. 2020 Apr;•••:1–5.
8.
Coccolini F
,
Perrone G
,
Chiarugi M
,
Di Marzo F
,
Ansaloni L
,
Scandroglio I
, et al.
Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020 Apr;15(1):25. https://doi.org/10.1186/s13017-020-00307-2
9.
Lambertini M
,
Toss A
,
Passaro A
,
Criscitiello C
,
Cremolini C
,
Cardone C
, et al.
Cancer care during the spread of coronavirus disease 2019 (COVID-19) in Italy: young oncologists’ perspective. ESMO Open. 2020 Mar;5(2):e000759. https://doi.org/10.1136/esmoopen-2020-000759
10.
Zhen L
,
Lin T
,
Zhao ML
,
Chen H
,
Chen T
,
Guo WH
, et al.
[Management strategy for the resumption of regular diagnosis and treatment in gastrointestinal surgery department during the outbreak of coronavirus disease 2019 (COVID-19)]. Zhonghua Wei Chang Wai Ke Za Zhi. 2020 Apr;23(4):321–6.
11.
Lazzerini M
,
Barbi E
,
Apicella A
,
Marchetti F
,
Cardinale F
,
Trobia G
. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020 May;4(5):e10–1. https://doi.org/10.1016/S2352-4642(20)30108-5
12.
Cano-Valderrama O
,
Morales X
,
Ferrigni CJ
,
Martín-Antona E
,
Turrado V
,
García A
, et al.
Reduction in emergency surgery activity during COVID-19 pandemic in three Spanish hospitals. Br J Surg. 2020 Jul;107(8):e239. https://doi.org/10.1002/bjs.11667
13.
Chang HJ
,
Huang N
,
Lee CH
,
Hsu YJ
,
Hsieh CJ
,
Chou YJ
. The impact of the SARS epidemic on the utilization of medical services: SARS and the fear of SARS. Am J Public Health. 2004 Apr;94(4):562–4. https://doi.org/10.2105/AJPH.94.4.562
14.
Slim K
,
Veziant J
. [Urgent digestive surgery, a collateral victim of the Covid-19 crisis?]. J Chir Visc. 2020 Jun;157(3):S4–5. https://doi.org/10.1016/j.jchirv.2020.04.001
15.
Nealon TF Jr
,
Mackrell J
,
Grossi CE
,
Mitty WF Jr
. Perforated appendix. Influence of outbreak of influenza. N Y State J Med. 1969 Mar;69(5):685–6.
16.
Lee-Archer P
,
Blackall S
,
Campbell H
,
Boyd D
,
Patel B
,
McBride C
. Increased incidence of complicated appendicitis during the COVID-19 pandemic. J Paediatr Child Health. 2020 Aug;56(8):1313–4. https://doi.org/10.1111/jpc.15058
17.
Tankel J
,
Keinan A
,
Blich O
,
Koussa M
,
Helou B
,
Shay S
, et al.
The Decreasing Incidence of Acute Appendicitis During COVID-19: A Retrospective Multi-centre Study. World J Surg. 2020 Aug;44(8):2458–63. https://doi.org/10.1007/s00268-020-05599-8
18.
Guadalajara H
,
Muñoz de Nova JL
,
Fernandez Gonzalez S
,
Yiasemidou M
,
Recarte Rico M
,
Juez LD
, et al.; PIACO Collaboration Group
. Patterns of acute surgical inflammatory processes presentation of in the COVID-19 outbreak (PIACO Study): surgery may be the best treatment option. Br J Surg. 2020 Oct;107(11):e494–5.
19. Office fédéral de la santé publique (OFSP) - Bundesamt für Gesundheit (BAG). Coronavirus: Situation en Suisse. [Available from: https://www.bag.admin.ch/bag/fr/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/situation-schweiz-und-international.html#-1315239417
20.
Rosenbaum L
. The Untold Toll - The Pandemic’s Effects on Patients without Covid-19. N Engl J Med. 2020 Jun;382(24):2368–71. https://doi.org/10.1056/NEJMms2009984