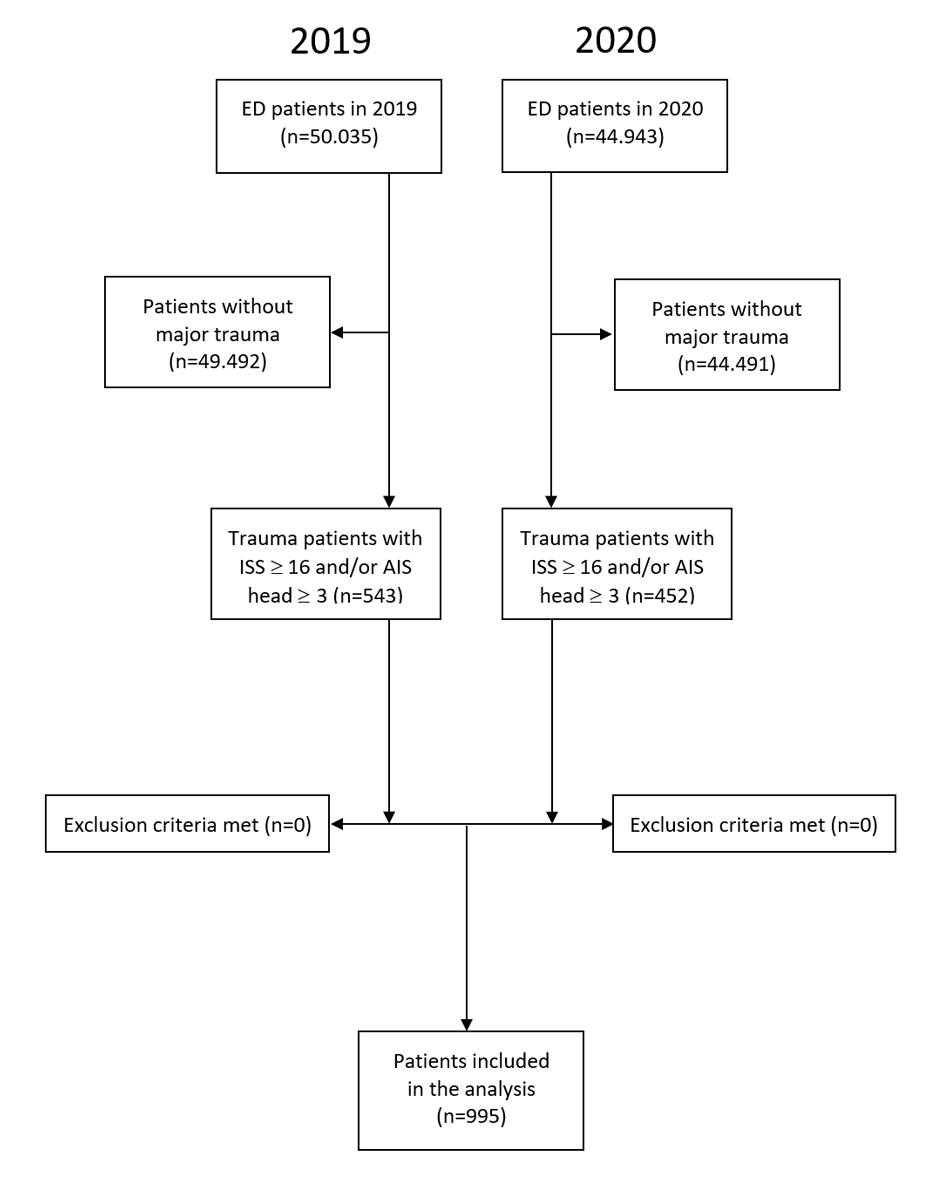
Figure 1 Study flow chart. AIS: Abbreviated Injury Score; ED = emergency department; ISS = Injury Severity Score
DOI: https://doi.org/10.4414/SMW.2021.w30010
The first cases of coronavirus disease 2019 (COVID-19) were described in Wuhan, China, in December 2019 [1]. Since then, the virus has spread throughout the world and was declared a pandemic in March 2020 by the World Health Organization (WHO) [2].
In Switzerland, the first case of COVID-19 was confirmed on 25 February 2020 [3]. A few days later, the Swiss federal council prohibited large events. In March, schools and all non-essential businesses and services closed and private and public events were prohibited. Most of these restrictions were eased by the end of April 2020 [4].
The second rise in incidence in Switzerland started in August – with the peak in November 2020 [3]. In line with the renewed increase in the number of cases, the restrictions were tightened. The Swiss population was advised to travel less; home working was introduced and working hours were reduced. Stay-at-home orders and physical distancing were widely implemented [4]. It can be assumed that these official restrictions have decreased mobility and the associated accidents. However, it is also conceivable that people in Switzerland might have changed their behaviour, and spend more time pursuing other activities than before the pandemic, and this might have modified the patterns of accident and trauma. In Switzerland, restrictions to outdoor activities (e.g., skiing) were largely avoided [5].
Most severe injuries at our emergency department (ED) are the result of road traffic accidents and falls. During the pandemic and stay-at-home orders, EDs worldwide and in Europe reported a decrease in total numbers and changes in the composition of patients [6–8].
This led to our hypothesis that during the pandemic in 2020 total numbers of severely injured patients decreased relative to 2019 and that this was associated with a change in injury pattern. Therefore, the aim of this study was to provide an overview of the impact of the first and second peaks in incidence of COVID-19 and the subsequent restrictions on the number of admissions and trauma patterns of patients with major trauma at a level 1 trauma centre in 2020 compared with 2019 as control period.
We conducted a retrospective, single-centre, cohort study in a level 1 trauma centre. Our ED is one of the largest in Switzerland, treating about 50,000 patients per year. As a level 1 trauma centre, we admit around 500 patients with major trauma per year (fig. 1).
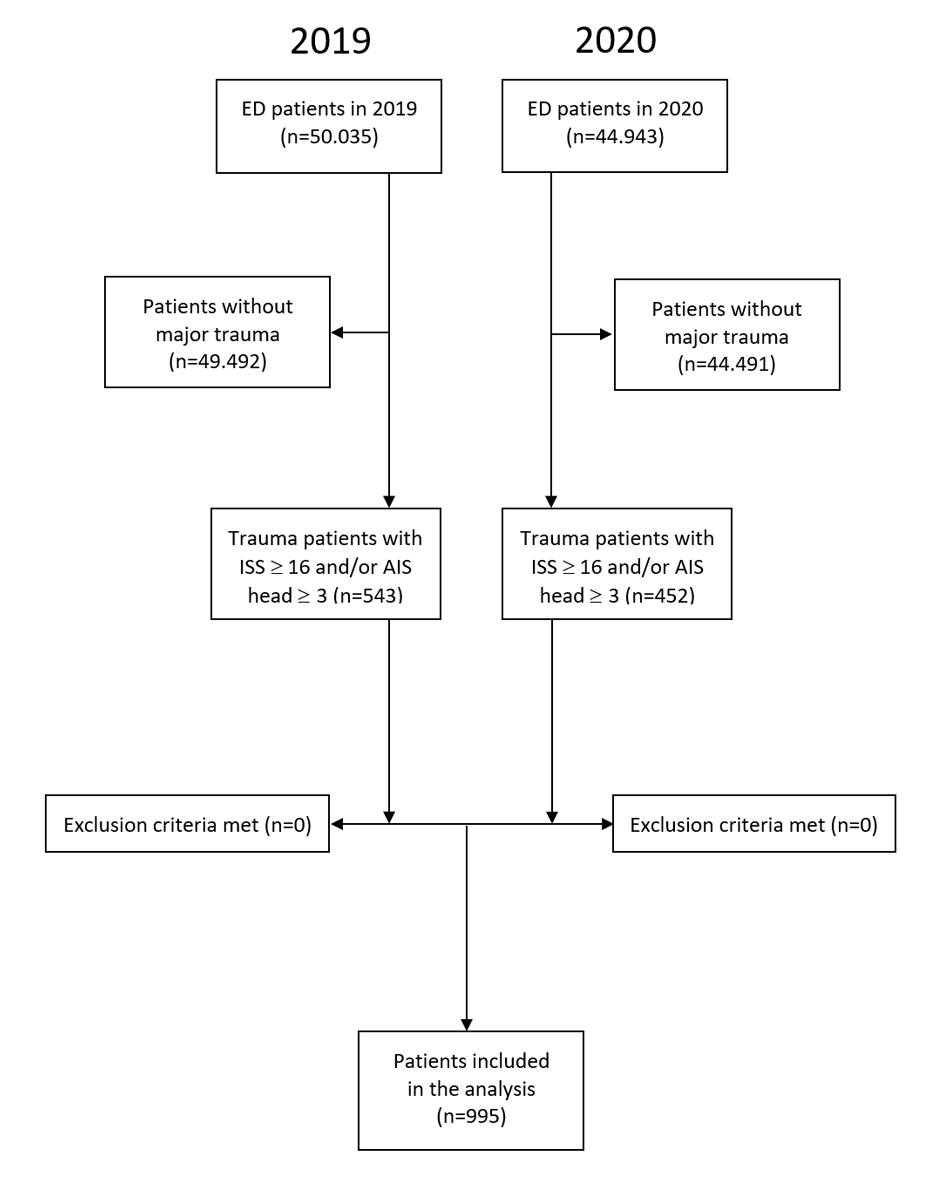
Figure 1 Study flow chart. AIS: Abbreviated Injury Score; ED = emergency department; ISS = Injury Severity Score
The severity of the patient's trauma is assessed with the Injury Severity Score (ISS) [9]. The body is divided into six ISS body regions. Each body region is then classified using the Abbreviated Injury Scale (AIS), from 1 (minor) to 6 (unsurvivable). To calculate the ISS, the square of the AISs from the three worst affected body regions are summed. In addition, patients with an AIS of 6 receive an ISS of 75. An ISS ≥16 or a head AIS ≥3 defines a major trauma [10].
All major trauma patients admitted in 2019 and 2020 with an ISS of ≥16 and/or a head AIS of ≥3 were included in the analysis. Exclusion criteria were age under 16 years and no major trauma – defined as ISS <16 and head AIS <3. All consecutive patients were included; no patient was lost. To minimise a potential observer bias, all data were assessed by one specially trained consultant. He calculated the AIS and ISS based on the radiological imaging conducted on the patients and the information in our hospital electronic patient records. Quality control was ensured through regular controls and audits. In all major trauma patients, the following parameters are assessed in accordance with Swiss law and society recommendations [11, 12]: ISS, date and time of admission, age at date of admission, type of injury, involved ISS body region, admission to an intensive care unit (ICU) and death within 30 days of admission.
The primary outcome of this study was the change in total number of patients with major trauma admitted to our institution.
Before analysis, the data were anonymised. The total number of patients admitted per year was compared between 2019 and 2020. The chi-square test was used to compare observed frequencies of parameters (e.g., cause of trauma) between 2019 and 2020. Non-normally distributed data were assessed using the Wilcoxon rank sum-test and displayed as medians, with interquartile range (IQR) in parentheses.
The 30-day mortality was further assessed using a multivariable logistic regression analysis including the following potential confounders: ISS, age, gender and type of injury. The statistical analysis was performed withSTATA® 16.1 (StataCorp, The College Station, Texas, USA).
The Cantonal Ethics Committee judged the study as a quality evaluation study (Study- Nbr: Req-2020-01429). The study was performed in accordance with the Declaration of Helsinki and the Guidelines for Good Clinical Practice.
In 2020, 454 patients with major trauma were admitted to our institution; this was 17% fewer than in 2019 with 543 patients (see fig. 1) and also than the average number of the previous 5 years (545.4 patients/year). The median ISS was higher in 2020 than in 2019 (25, IQR 17–26.5 vs 22, IQR 16–26, p = 0.04, table 1).
In comparison to 2019, the total number of patients per month dropped in February to April, August/September and December 2020 (fig. 2).
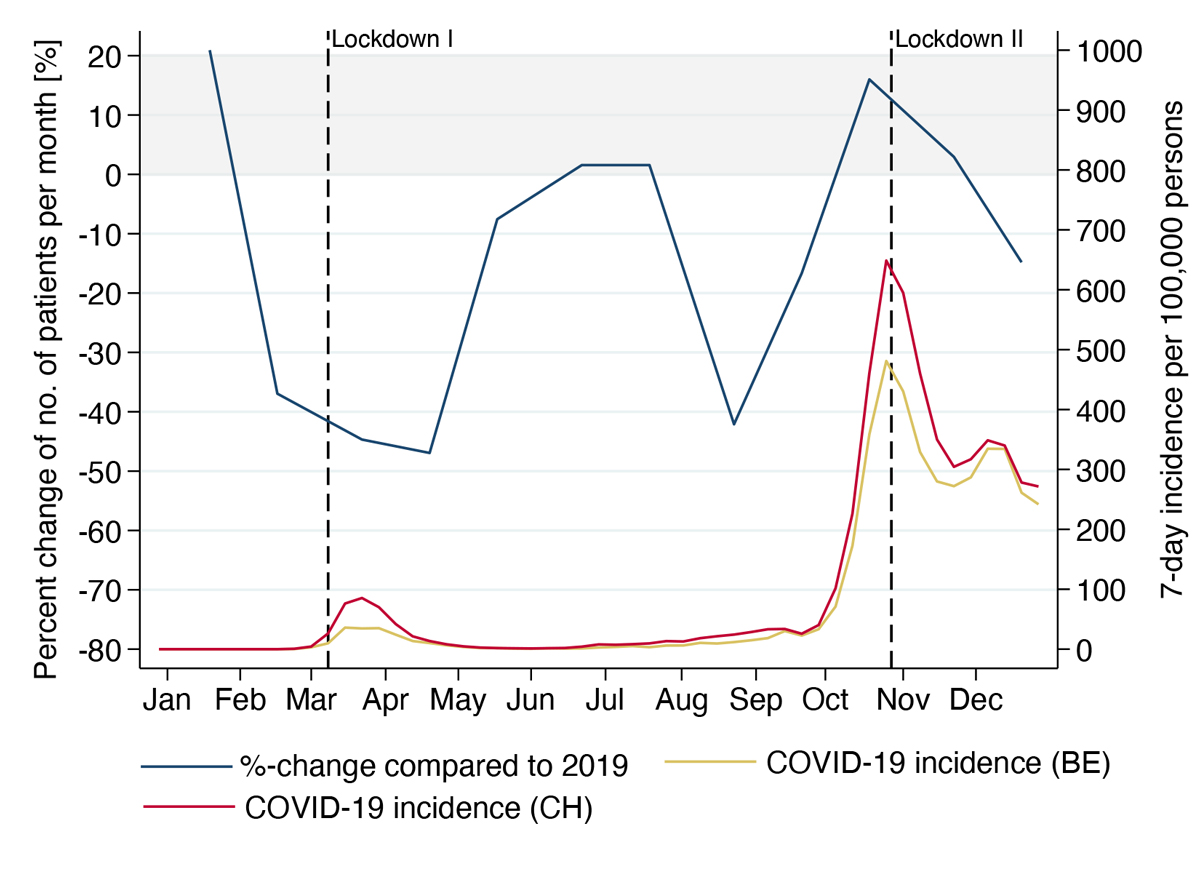
Figure 2 The relative change (%) in the number of major trauma patients in 2020 compared to the baseline year 2019 (left axis and blue curve). The red curve (right axis) shows the 7-day incidence per 100,000 persons in 2020 in Switzerland. The two “lockdown” dates are marked with a dashed line. The weekly COVID-19 incidence in 2020 in Switzerland is published by the Federal Office of Public Health [13].
In the remaining 6 months, the total number of patients remained similar to 2019 or was slightly higher. The decreases in the number of patients overlapped the rise in COVID-19 incidence in both the first and second peaks in incidence.
The secondary outcomes were change in the type of injury and involved body regions, and follow up including admission to an ICU and 30-day mortality.
The type of injury did not differ significantly between 2019 and 2020. The distribution of the traffic accidents changed, with significantly fewer accidents as pedestrians: 4.2% (5 of 118 traffic accident patients) in 2020 versus 11.4% (17 of 149 patients) in 2019; p = 0.034). The percentage increase in bicycle accidents did not reach significance: 55.9% (66 of 118 patients) in 2020 versus 44.3 % (66 of 149 patients) in 2019; p = 0.059 (table 1). In 2020, 42% of the patients (n = 189) were admitted during working hours, defined as 08:00 to 18:00 Monday to Friday. This percentage was unchanged from 2019 (p = 0.858). There was no significant difference in median age of patients and in the involved ISS body regions (table 1).
Table 1Characteristics of major trauma in 2020 compared with 2019.
| Parameter | 2020 | 2019 | Change | p-value* |
| Number of patients (n) | 452 | 543 | -17% | |
| ISS, median (IQR) | 25 (17–26.5) | 22 (16–26) | +3 | 0.039 |
| ISS >19, n (%) | 294 (65.0) | 315 (58.0) | –7% | 0.042 |
| ISS 16-19, n (%) | 105 (23.2) | 139 (25.6) | –24% | |
| ISS <16, head AIS ≥ 3, n (%) | 53 (11.7) | 89 (16.4) | –40% | |
| Age (years), median (IQR) | 67 (51–79) | 64 (45–79) | +3 | 0.109 |
| Body region | ||||
| Head and neck, n (%) | 381 (84.3) | 446 (82.1) | –15% | 0.366 |
| Face, n (%) | 63 (13.9) | 93 (17.1) | –32% | 0.168 |
| Chest, n (%) | 163 (36.1) | 181 (33.3) | –10% | 0.368 |
| Abdomen or pelvic contents, n (%) | 92 (20.4) | 113 (20.8) | –19% | 0.859 |
| Extremities and pelvic girdle, n (%) | 133 (29.4) | 191 (35.2) | –30% | 0.054 |
| Type of trauma, n (%) | 0.269 | |||
| Traffic accidents total | 118 (26.1) | 149 (27.4) | –21% | |
| Car accidents | 21 (5) | 28 (5) | –25% | |
| Motorcycle accidents | 19 (4.2) | 30 (5.5) | –37% | |
| Bike accidents | 66 (14.6) | 66 (12.2) | 0 | |
| Pedestrian accidents | 5 (1.1) | 17 (3.3) | –71% | |
| Other traffic accidents | 7 (1.6) | 8 (1.5) | –12% | |
| Falls total | 297 (65.7) | 331 (61.0) | –10% | |
| Falls under 3 metres | 167 (37.0) | 235 (43.3) | –29% | |
| Falls over 3 metres | 52 (11.5) | 43 (7.9) | –17% | |
| Falls of unknown height | 78 (17.3) | 53 (9.8) | +32% | |
| Other/unknown | 37 (8.0) | 63 (11.6) | –40% | |
| Time of admission, n (%) | 0.858 | |||
| Working hours | 189 (41.8) | 224 (41.3) | –16% | |
| Weekend and nights | 263 (58.2) | 319 (58.7) | –18% | |
| Admission to ICU, n (%) | 391 (86.5) | 422 (77.7) | –7% | <0.001 |
| Death within 30 days, n (%) | 40 (8.8) | 27 (5.0) | +48% | 0.015 |
“Working hours” are defined as the time frame from 08:00-18:00 from Monday to Friday. “Weekend and nights” are defined as the time frame outside working hours.
ICU: intensive care unit; IQR: interquartile range; ISS: Injury Severity Score.
* Wilcoxon rank sum-test or chi-square test, as appropriate
In 2020, 86.5% of the patients with major trauma were admitted to an ICU, and 8.8% died within 30 days of arrival in hospital. These numbers were increased compared with 2019, when 77.7% of the patients were admitted to an ICU (p <0.001) and 5.0% died within 30 days of arrival in hospital (p = 0.015).
The odds ratio for admission to ICU in 2020 was 2.0 (95% confidence interval [CI] 1.4–3.0; p <0.001) compared with 2019. The odds ratio for death within 30 days in 2020 was 1.7 (95% CI 1.0–2.9; p = 0.039). After adjusting for the following potential confounders – ISS, age, gender, type of injury and working hour admission – the odds ratio for admission to ICU in 2020 was 2.0 (95% CI 1.3–3.1; p = 0.001) and the odds ratio for death within 30 days in 2020 was 1.8 (95% CI 1.03.1; p = 0.036).
The retrospective, single centre data analysis identified a decrease in the total numbers of patients with major trauma treated at our ED during the year of the COVID-19 pandemic in 2020 compared with the previous year, which proceeded with and overlapped both COVID-19 peaks in incidence. This observation is in line with other studies from EDs around the world, which also reported a general decrease in patient admissions during the pandemic [7, 8, 14]. The number of trauma patients decreased in most institutions by between 30% and 60% [15–17], and even reached 89% during a strict lockdown [18].
The reduction in major trauma cases correlates with the regulations issued by the authorities [4]. February to April 2020 corresponds to the timeframe of the first peak in incidence of the pandemic in Switzerland, when restrictions were implemented. In August 2020, the second rise in incidence began, but in the peak in November 2020 the number of patients admitted was similar to 2019 and the effect seen during the first peak in incidence was less marked. This might have been the effect of campaigns to encourage patients to seek safe treatment in hospitals and EDs in countries that observed a decline in ED consultations during the first peak in incidence [19], although severely injured patients were presumably less influenced than critically ill patients.
There have been reports that workplace accidents and road traffic accidents decreased during the pandemic (by up to 80.5%) [16, 20]. In our study population, the type of injury did not change significantly, but there was a trend to a lower percentage of pedestrian accidents. The number of bicycle accidents stayed at the same level, and all other types of traffic accidents decreased. Higher rates of bicycle accidents during the pandemic have been reported in UK and Australian studies [21, 22].
However, although the total number of patients with major trauma decreased, the severity of injuries increased. This is reflected by a higher median ISS as well as a higher rate of ICU admission. Thirty-day mortality was significantly higher in 2020. This could not be explained only by the severity of trauma. After adjusting for potential confounders (ISS, age, gender, type of injury) in a multivariable logistic regression analysis, the 30-day mortality was still higher in 2020. The number of ICU beds at our institution was increased in 2020 as a reaction to COVID-19. Fewer patients were admitted to the ICU, but they stayed longer leading to a similar bed occupancy in 2019 and 2020. However, we cannot exclude an increased mortality due to limited human resources. Elective surgeries were postponed during the peaks in incidence. Urgent surgeries including the treatment of patients with major trauma were conducted with no delay. Hence, postponed surgical treatment is unlikely to be the cause of the increased mortality.
Other trauma centres reported a stable or slightly lower mortality due to major trauma [22]. This effect was also seen in non-traumatic emergency admissions in our ED [23].
Limitations: This was a retrospective study, subsequently information and selection bias cannot be excluded. However, the data were systematically registered by one specially trained physician. As we only included patients with major trauma in our study, these findings cannot be generalised to all trauma patients. However, further studies at our institution assessing the change in patients with minor trauma are planned. Further, we did not have information on how many of our patients suffered from COVID-19, so no connection between changes in treatment and outcome of trauma patients with COVID-19 can be made.
In conclusion, it can be stated that in the first year of the COVID-19 pandemic, 17% fewer patients with major trauma were admitted to our institution than in the previous year. However, the patients were more severely injured, as reflected by a higher median ISS, a higher rate of ICU admission and a higher 30-day mortality rate.
Understanding the differences in injury patterns and admissions in major trauma patients under special conditions — such as a pandemic — could help us to allocate rare resources adequately.
However, a decrease in pure case load does not reflect the resource needs in EDs, as a variety of other aspects (e.g., severity of injuries/illness, special hygiene measures, sick leave) are major factors in ensuring adequate emergency care.
The authors report no conflict of interest.
1 Huang C . Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. 2020;395:10.
2 World Health Organization . WHO announces COVID-19 outbreak a pandemic [Internet]. 2020 [cited 2021 April 19]. Available at: http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic
3 Bundesamt für Gesundheit BAG . Epidemiologische Zwischenbilanz zum neuen Coronavirus in der Schweiz und im Fürstentum Liechtenstein [Internet]. 2020 [cited 2021 April 19]. Available at: https://www.bag.admin.ch/dam/bag/de/dokumente/mt/k-und-i/aktuelle-ausbrueche-pandemien/2019-nCoV/covid-19-zwischenbilanz-mai-2020.pdf.download.pdf/BAG_Epidemiologische_Zwischenbilanz_zum_neuen_Coronavirus.pdf
4 Bundesamt für Gesundheit BAG. Coronavirus: Massnahmen und Verordnungen [Internet]. 2021. Available at: https://www.bag.admin.ch/bag/de/home/krankheiten/ausbrueche-epidemien-pandemien/aktuelle-ausbrueche-epidemien/novel-cov/massnahmen-des-bundes.html#1570431754
5 Schweizer Tourismus-Verband. Coronavirus: Chronik mit Bezug zum Schweizer Tourismus [Internet]. Available at: https://www.stv-fst.ch/de/chronik-coronavirus
6 Cano-Valderrama O , Morales X , Ferrigni CJ , Martín-Antona E , Turrado V , García A , et al. Acute Care Surgery during the COVID-19 pandemic in Spain: changes in volume, causes and complications. A multicentre retrospective cohort study. Int J Surg. 2020 Aug;80:157–61. https://doi.org/10.1016/j.ijsu.2020.07.002
7 Westgard BC , Morgan MW , Vazquez-Benitez G , Erickson LO , Zwank MD . An Analysis of Changes in Emergency Department Visits After a State Declaration During the Time of COVID-19. Ann Emerg Med. 2020 Nov;76(5):595–601. https://doi.org/10.1016/j.annemergmed.2020.06.019
8 Slagman A , Behringer W , Greiner F , Klein M , Weismann D , Erdmann B , et al. Medizinische Notfälle während der COVID-19-Pandemie [Medical Emergencies During the COVID-19 Pandemic]. Dtsch Arztebl. 2020;117(33-34):545–52.
9 Baker SP , O’Neill B , Haddon WJr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma Acute Care Surg [Internet]. 1974;14(3). Available at: https://journals.lww.com/jtrauma/Fulltext/1974/03000/the_injury_severity_score__a_method_for_describing.1.aspx
10 Copes WS , Champion HR , Sacco WJ , Lawnick MM , Keast SL , Bain LW . The Injury Severity Score Revisited. J Trauma Acute Care Surg [Internet]. 1988;28(1). Available at: https://journals.lww.com/jtrauma/Fulltext/1988/01000/The_Injury_Severity_Score_Revisited.10.aspx
11 Bless N , Jakob M . Traumazentren in der Schweiz. Swiss Knife. 2012;4:10–1.
12 Interkantonale Vereinbarung über die hochspezialisierte Medizin. Entscheid zur Planung der hochspezialisierten Medizin (HSM) im Bereich der Behandlung von Schwerverletzten [Internet]. 2011. Available at: https://www.fedlex.admin.ch/eli/fga/2011/744/de
13 Bundesamt für Gesundheit BAG . Covid-19 Schweiz [Internet]. Available at: https://www.covid19.admin.ch/de/epidemiologic/case
14 Kuitunen I , Ponkilainen VT , Launonen AP , Reito A , Hevonkorpi TP , Paloneva J , et al. The effect of national lockdown due to COVID-19 on emergency department visits. Scand J Trauma Resusc Emerg Med. 2020 Dec;28(1):114. https://doi.org/10.1186/s13049-020-00810-0
15 Sherman WF , Khadra HS , Kale NN , Wu VJ , Gladden PB , Lee OC . How Did the Number and Type of Injuries in Patients Presenting to a Regional Level I Trauma Center Change During the COVID-19 Pandemic with a Stay-at-home Order? Clin Orthop Relat Res. 2021 Feb;479(2):266–75. https://doi.org/10.1097/CORR.0000000000001484
16 Kamine T , Rembisz A , Barron R , Baldwin C , Kromer M . Decrease in Trauma Admissions with COVID-19 Pandemic. West J Emerg Med [Internet]. 22. May 2020 [cited 2021 April 14];21(4): 819–22. Available at: https://escholarship.org/uc/item/05n535hg
17 Harris D , Ellis DY , Gorman D , Foo N , Haustead D . Impact of COVID-19 social restrictions on trauma presentations in South Australia. Emerg Med Australas. 2021 Feb;33(1):152–4. https://doi.org/10.1111/1742-6723.13680
18 Pintado JF , Gibaja W , Vallejos RA , Rosas W , Guerra-Farfan E , Nuñez JH . How COVID-19 has affected emergent visits to a Latin-American trauma department: Experience at a Peruvian national trauma referral center. 2020;51(12):2834–9.
19 Wong LE , Hawkins JE , Langness S , Iris P , Sammann A . Where Are All the Patients? Addressing Covid-19 Fear to Encourage Sick Patients to Seek Emergency Care. NEJM Catalyst. 2020 May 14. Available at: https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0193
20 Venter A , Lewis CM, Saffy P, Chadinha LP. Locked down: Impact of COVID-19 restrictions on trauma presentations to the emergency department. S Afr Med J.2020;111(1):52–6. 10.7196/SAMJ.2021.v111i1.15289.
21 Probert AC , Sivakumar BS , An V , Nicholls SL , Shatrov JG , Symes MJ , et al. Impact of COVID-19-related social restrictions on orthopaedic trauma in a level 1 trauma centre in Sydney: the first wave. ANZ J Surg. 2021 Jan;91(1-2):68–72. https://doi.org/10.1111/ans.16375
22 Rajput K , Sud A , Rees M , Rutka O . Epidemiology of trauma presentations to a major trauma centre in the North West of England during the COVID-19 level 4 lockdown. Eur J Trauma Emerg Surg [Internet]. 2021;47:631–6. [cited 2021 April 14]. Available at: http://link.springer.com/10.1007/s00068-020-01507-w
23 Hautz WE , Sauter TC , Exadakytlos AK , Krummrey G , Schauber S , Müller M . Barriers to seeking emergency care during the COVID-19 pandemic may lead to higher morbidity and mortality – a retrospective study from a Swiss university hospital. Swiss Med Wkly. 2020;150:w20331. https://doi.org/10.4414/smw.2020.20331