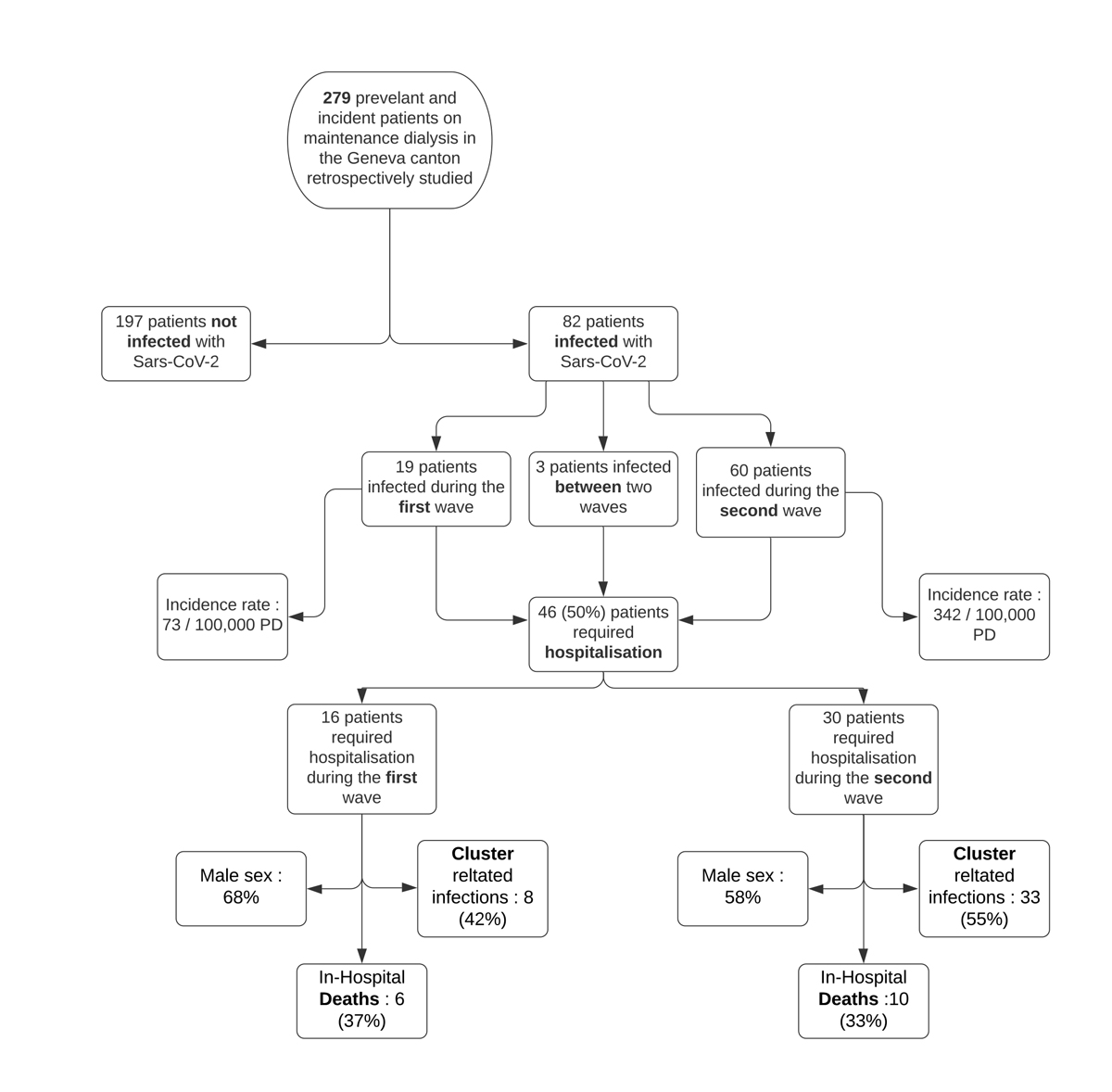
Figure 1 Flow chart for study population and COVID-19 related outcomes. PD: patient days.
DOI: https://doi.org/10.4414/SMW.2021.w30006
The coronavirus-related disease (COVID-19) outbreak, caused by the novel coronavirus named SARS-CoV-2, was declared a pandemic by the World Health Organization (WHO) on 12 March 2020 [1]. Since the diagnosis of four cases of pneumonia in Wuhan, China in late December 2019, SARS-CoV-2 infection has spread with an unparalleled transmission rate, resulting in more than 177 million confirmed cases, responsible for over 3.8 million deaths worldwide [2].
In the effort to reduce the viral transmission rate and relieve overwhelmed healthcare systems, jurisdictions worldwide adopted containment strategies, such as travel restrictions, social distancing, quarantine for suspected cases and isolation for confirmed cases [2—4]. At the individual level, the WHO is recommending hygiene measures, such as frequent hand washing and use of personal protective equipment [5].
Patients with end-stage kidney disease on maintenance dialysis have a high prevalence of cardiovascular disease, diabetes, hypertension and old age [6], all of which put them at high risk for a severe COVID-19 infection and death [4, 7, 8]. Whereas most outpatient activities for patients with chronic conditions could be temporarily held, in-centre haemodialysis sessions require the physical presence of the patients. Moreover, not all dialysis facilities can guarantee adequate distance between patients because of space restrictions. In addition, patients are required to travel several times per week to the dialysis units, often using public transportation, thus exposing themselves to the risk of community transmitted infection. Infected patients would expose other patients and medical staff to SARS-CoV-2 with the risk of creating clusters within dialysis units, which might result in catastrophic outcomes for this extremely vulnerable population [9].
Since the beginning of the COVID-19 outbreak in Switzerland, the Geneva region has had the highest burden of infections in the country and during the second wave our region suffered from the highest infection incidence rate in Europe. Our objectives for this study were to present an overview of local experience with dialysis unit management and reorganisation, local epidemiology and short-term outcomes of the COVID-19 outbreak in Geneva, Switzerland during the first and second outbreak waves.
All confirmed SARS-CoV-2 infections were reported to cantonal health authorities who provided daily updated data on local epidemiology.
From the beginning of the local epidemic, patients were asked to call ahead to their dialysis unit before coming for their session if they had fever and upper respiratory symptoms. Their body temperature was systematically measured upon arrival. If any symptoms were present or if the patient was febrile (>37.5°C), a screening nasopharyngeal swab was taken in a dedicated room. While awaiting the results, the patient was dialysed keeping a distance of at least 2 metres from other patients or in a separate room if the latter were available. All patients had to wear a surgical mask upon arrival and during the whole dialysis session. In addition, the dialysis units provided two masks to patients who used public transportation; patients were asked to wear them on their way home as well as on their way to the unit for the next session. Hospitalised patients were screened in their respective wards if suspect symptoms were present. If the test was positive for SARS-CoV-2 infection, patients were transferred to a dedicated ward.
The same preventive measures were applied in the three affiliated outpatient dialysis facilities, except that face masks were not systematically provided to patients. In addition, visits were not allowed during dialysis and the waiting rooms were reorganised to guarantee a two-meters distance between chairs. Only one patient at a time was allowed in the locker room.
For patients treated by peritoneal dialysis, regular monthly visits in outpatient clinics were replaced by phone calls. Should an emergency condition require an in-hospital evaluation, the same preventive measures as described above were applied.
All SARS-CoV-2-positive outpatients on maintenance dialysis from affiliated units were transferred to the Geneva University Hospitals dialysis unit in order to avoid creation of new clusters of transmission. Within this unit, confirmed or suspected COVID-19 outpatients were separated from non-infected patients in two distinct parts of the unit. In addition, a third shift was added to accommodate patients with COVID-19 and enforce the recommended two metres distance between patients during sessions. Between shifts, standard disinfection procedures for dialysis machines were applied. For patients who were dependent on public transportation, private transport was organised in order to decrease risk of community transmission.
At work, all staff had to wear surgical face masks and keep two metres distance from patients when possible. Nurses who worked in proximity with confirmed cases wore an N95 respirator, goggles, gloves and a long-sleeved impervious gown. Any staff member with fever (>37.5 °C) or upper respiratory symptoms was systematically screened. Staff with a positive test had to self-isolate at home for at least 10 days and were allowed to resume their activity after day 10 if they had no symptoms for at least 48 hours, or after day 14.
Staff of each unit approached patients during their dialysis sessions from the beginning of the local epidemic in order to share information about the outbreak, explain the importance of and rationale for containment measures, organisational and staff changes, give advice on individual prevention methods and answer patients’ questions. Patients received an information letter and frequent updates were provided to patients through a dedicated website.
Acute patient care at Geneva University Hospitals is provided in the medical (or surgical) wards, the intermediate care unit (IMCU; offering monitoring and noninvasive positive pressure ventilation) or the intensive care unit (ICU), as needed. Criteria for admission to the COVID-19 medical wards followed institutional protocols that were mostly based on oxygen needs and patients’ comorbidities. Admission to the IMCU or the ICU was restricted in accordance with the consensus criteria drafted by the Swiss Academy for Medical Sciences [10]. The following exclusion criteria applied: patients with unwitnessed or recurrent cardiac arrest, cardiac arrest without return of spontaneous circulation, vasopressor-resistant circulatory failure, any disease with life expectancy <12 months, end-stage neurodegenerative disease or severe dementia, severe and irreversible neurological event-condition, New York Heart Association class IV heart failure, chronic obstructive pulmonary disease (GOLD stage 4D), or liver cirrhosis (Child-Pugh score >8).
Our institution developed management protocols for patients admitted with SARS CoV-2 infection based on published evidence. Treatment with hydroxychloroquine (single dose of 800 mg) and/or lopinavir/ritonavir (200/50 mg twice daily for 5 days) during the first wave and remdesivir (200 mg on the first day followed by 4 days of 100 mg daily) during the second wave could be prescribed at the discretion of the attending physician. Remdesivir was contraindicated for patients with creatinine clearance <30 ml/min, including those on maintenance dialysis. Dexamethasone 6 mg once a day for 7 to 10 days was administered to most hospitalised patients during the second wave. High-flow nasal cannulae were also readily used for severe cases.
All prevalent and incident patients on maintenance dialysis treated in the canton of Geneva between25 February to 31 December 2020, were retrospectively included in the study (fig. 1).
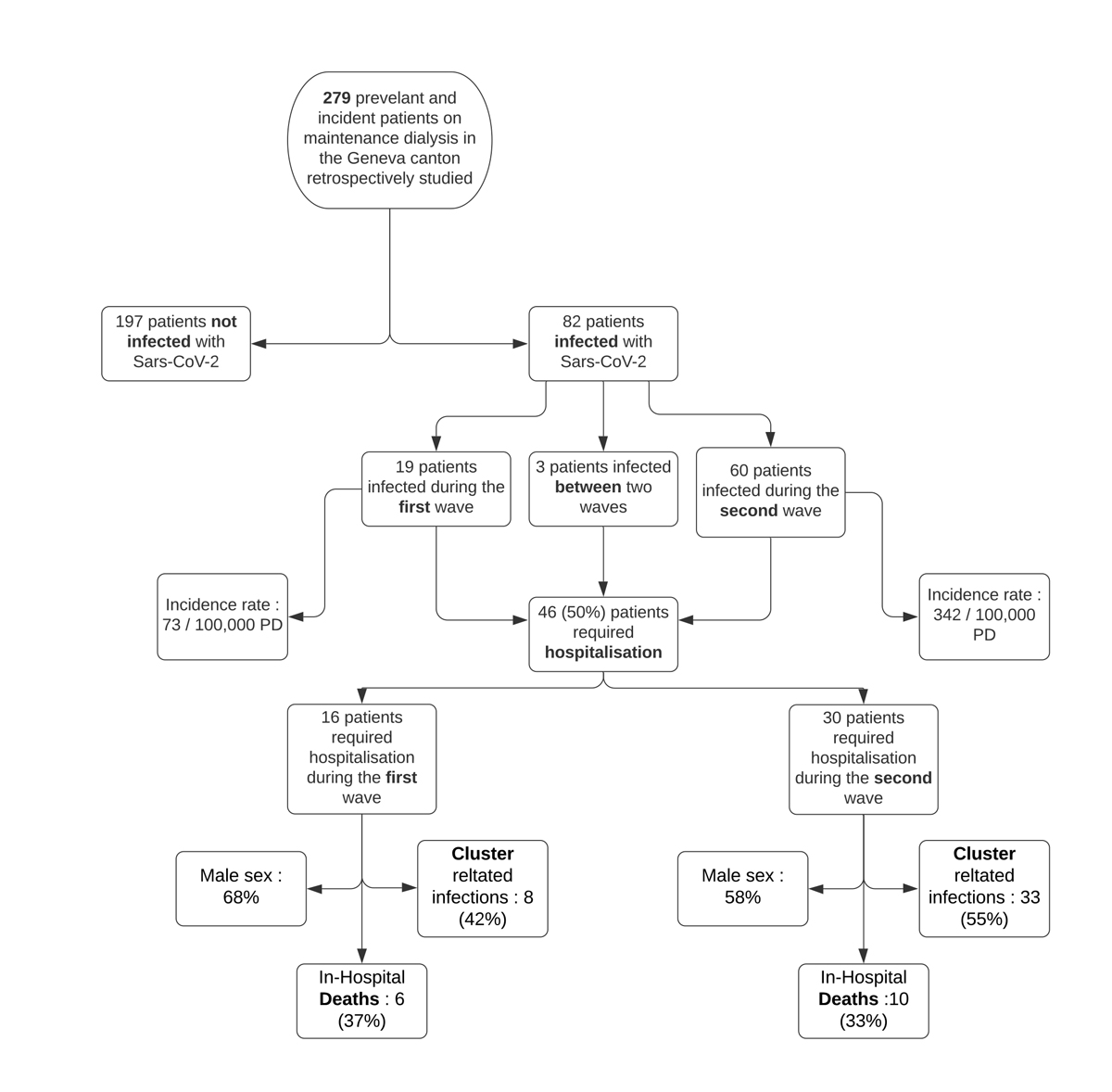
Figure 1 Flow chart for study population and COVID-19 related outcomes. PD: patient days.
In Switzerland, all patients on maintenance dialysis are listed in a national registry and have provided informed written consent for their pseudo-anonymised data to be used for quality control or clinical research purposes. The study was approved by the research ethics committee of the canton of Geneva (ID 2020-01281). Data on demographic characteristics, baseline comorbidities, COVID-19 status, related symptoms or laboratory findings, and outcomes were retrospectively collected both from the registry and from patients’ electronic medical records. For this study, the modified Charlson comorbidity index was used [11]. Data for the COVID-19 incidence, related hospitalisation and deaths were obtained from public federal databases and institutional unpublished data.
All patients have provided written informed consent for their anonymised data to be used for quality control or clinical research purposes. The study was approved by the research ethics committee of the canton of Geneva “Commission cantonale d'éthique de la recherche” (CCER Genève, ID 2020-01281).
The primary outcome for this study was the cumulative incidence of COVID-19 infections among patients on maintenance dialysis in the Geneva regional district (canton). Secondary outcomes were COVID-19-related death and hospitalisation rates in patients on maintenance dialysis.
Results are presented as mean ± standard deviation (SD), median with interquartile range (IQR), or number (percentage). Groups were compared with the unpaired t-test, the chi-square or the Mann-Whitney test, as appropriate. The incidence rates were estimated using the stptime function in Stata (the number of cases per time period was in the numerator and the patient-days variable in the denominator; data were declared to be survival data using the stset function). IBM SPSS Statistics (version 24.0, Armonk, NY) and Stata SE (version 17, College Station, TX) was used.
The first SARS-CoV-2 infection in Switzerland was confirmed on 24 February 2020 and the first case in the canton of Geneva on 27 February 2020. On 31 December 2020, the canton of Geneva had a cumulative total of 40,952 confirmed cases of SARS-CoV-2 infection (fig. 2), an overall incidence rate of 29.9 cases per 100,000 person-days. Fifty-five percent of infected patients were women. During the same time period, 657 COVID-19-related deaths were reported (both within and outside hospital settings), representing a mortality rate of 1.6% [12]. Among patients who died, 55% were men and 90% were over 70 years old. Most cases occurred in two distinct waves: in the first wave, between 25 February and 14 June, the incidence rate was 10.8 cases per 100,000 patient-days; in the second wave, between 1 October and 31 December, the incidence rate increased eight-fold to reach 86.3 cases per 100,000 patient-days.
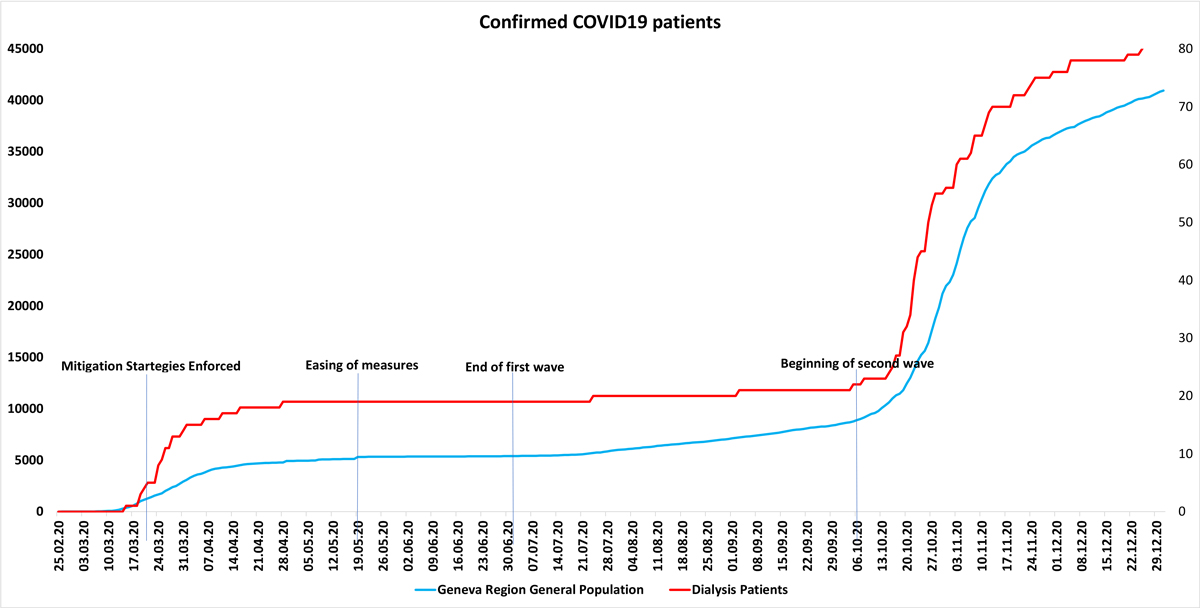
Figure 2 Cumulative frequency of SARS CoV-2 in the general population and in patients on maintenance dialysis.
In-hospital outcomes for the general population are summarised in table 3 (below). In total, 3852 patients accounted for a total of 4403 hospitalisations, of which 1372 (31%) were in the IMCU or ICU. The mortality rate of hospitalised patients was 13% with a total of 514 COVID-19-related deaths.
In the canton of Geneva, four dialysis units treated a total of 279 prevalent and incident maintenance dialysis patients during the study period. Two of them provided in-centre dialysis for outpatients, whereas those at University of Geneva Hospitals and at Hospital de la Tour provided in-centre dialysis for both outpatients and inpatients. Under normal circumstances, all units have two daily dialysis shifts from Monday to Saturday. No patient was lost to follow-up during our study period and there were no missing variables in the patient data collected.
From 24 February to 31 December a total of 82 (29.4%) patients on maintenance dialysis tested positive for SARS-CoV-2. Nineteen of the cases occurred during the first wave, three sporadic cases occurred between the end of June and early October and 60 cases during the second wave (see fig. 1 above). Baseline characteristics of patients by infection status are shown in table 1. As compared with non-infected patients, patients who tested positive for SARS-CoV-2 had a significantly higher body mass index (BMI; 27 ± 6 vs 25 ± 5 kg/m2, p = 0.05, table 1), longer dialysis duration (41 [19–74] vs 30 [17–57] months, p = 0.047, table 1), longer in-hospital stay from any cause (39 ± 61 vs 16 ± 31 days, p = 0.001, table 1) and a higher death rate (19.5% vs 10%, p = 0.037, table 1). Among infected patients, 66 patients (80%) required hospitalisation, of which 46 (69%) were COVID-19 related.
Table 1Baseline characteristics of patients on maintenance dialysis by infection status (Geneva area March–December 2020).
| Characteristics | Not infected by SARS CoV-2 (n = 197) | Infected by SARS CoV-2 (n = 82) | p-value |
| Mean age (years) | 67 ± 15 | 67 ± 17 | 0.83 |
| Male gender, n (%) | 128 (65) | 51 (62) | 0.29 |
| BMI (kg/m2) | 25 ± 5 | 27 ± 6 | 0.005 |
| Diabetes, n (%) | 65 (33) | 36 (44) | 0.08 |
| Modified* CCI | 7.6 ± 3.1 | 7.3 ± 2.7 | 0.45 |
| Dialysis duration (months) | 30 (17–57) | 41 (19–74) | 0.047 |
| Patients on HD, n (%) | 165 (84) | 77 (94) | 0.023 |
| Transplanted, n (%) | 8 (4) | 0 (0) | |
| Hospitalised, n (%) | 116 (59) | 66 (80) | 0.001 |
| – COVID-related, n (%) | NA | 46 (56) | 0.001 |
| Hospital days (mean + SD) | 16 ± 31 | 39 ± 61 | 0.001 |
| – COVID-related | NA | 22 ± 44 | |
| Death, n (%) | 20 (10) | 16 (19.5) | 0.037 |
BMI: body mass index; CCI: Charlson comorbidity index; HD: haemodialysis; NA = not applicable. Data are presented as mean ± standard deviation (SD), median (interquartile range) or n (%). * 1 point per decade over 40 years.
Characteristics of hospitalised patients are summarised in table 2. Among hospitalised patients, 16 died (34%) from COVID-19-related complications. Deceased patients were older (77 ± 6 vs 70 ± 11 years, p = 0.02, table 2) and had a significantly lower BMI (25 ± 6 vs 29 ± 5 kg/m2, p = 0.01, table 2). On presentation, the most common symptoms were fever (82%), cough (60%) and fatigue (64%).
Table 2Characteristics of hospitalised patients on maintenance dialysis with SARS CoV-2 pneumonia by outcome (Geneva area March–December 2020).
| Characteristics | Survived (n = 30) | Died (n = 16) | p-value |
| Mean age (years) | 70 ± 11 | 80 ± 6 | 0.002 |
| Male gender, n (%) | 14 (48) | 12 (75) | 0.08 |
| Diabetes, n (%) | 19 (66) | 6 (38) | 0.07 |
| BMI (kg/m2) | 29 ± 5 | 25 ± 5 | 0.01 |
| Modified CCI | 8.1 ± 2.3 | 9.1 ± 1.4 | 0.15 |
| Dialysis duration (months) | 41 (15–85) | 46 (24–75) | 0.67 |
| Patients on HD, n (%) | 28 (97) | 14 (88) | 0.28 |
| Clinical presentation on diagnosis | |||
| Fever, n (%) | 26 (87) | 12 (75) | 0.42 |
| Cough, n (%) | 20 (67) | 8 (50) | 0.35 |
| Dyspnoea, n (%) | 16 (53) | 13 (81) | 0.11 |
| Fatigue, n (%) | 19(64) | 12 (75) | 0.52 |
| Myalgia, n (%) | 6 (20) | 1 (6) | 039 |
| Diarrhoea, n (%) | 5 (17) | 2 (13) | 1.00 |
| Laboratory tests on diagnosis | |||
| WBC (x 1000/μl) | 7.8 ± 4.4 | 8.9 ± 4.3 | 0.43 |
| Neutrophils (%) | 79 ± 8 | 75 ± 22 | 0.40 |
| Lymphocytes (%) | 12 ± 7 | 10 ± 5 | 0.43 |
| Peak C-reactive protein (mg/l) | 110 ± 96 | 146 (92) | 0.25 |
| Chest x-ray | |||
| Multifocal opacities, n/n (%) | 23/29 (79) | 13/14 (93) | 0.40 |
| Outcomes | |||
| Optiflow, n (%) | 8 (27) | 4 (25) | 1.00 |
| Dexamethasone, n (%) | 13 (43) | 7 (44) | 0.94 |
| ICU-IMCU, n (%) | 10 (35) | 4 (25) | 1.00 |
| Intubation required, n (%) | 3 (10) | 0 | |
| Hospital days to discharge or death | 74 ± 81 | 39 ± 40 | 0.11 |
| ICU- IMCU days to discharge or death | 4.2 ± 9.2 | 1.4 ± 2.6 | 0.26 |
BMI: body mass index; CCI: Charlson comorbidity index; HD: haemodialysis; WBC: white blood cell count; ICU: intensive care unit; IMCU: intermediate care unit. Data are presented as mean ± standard deviation (SD), median (interquartile range) or n (%).
Outcomes among dialysis patients in each wave of the local SARS-CoV-2 epidemic are summarised in table 3.
Table 3Comparison of hospitalised patients on maintenance dialysis with SARS-CoV-2 pneumonia during each wave of the local epidemic.
| Characteristics | First wave | Second wave | ||
| Dialysis | General population | Dialysis | General population | |
| Total number of patients hospitalised owing to a SARS-CoV-2 infection | 16 | 1074 | 30 | 2778 |
| Male sex % | 68% | NA | 58% | NA |
| Cluster-related infections, n (%) * | 8 (42%) | NA | 33 (55%) | NA |
| Incidence rate per 100,000 patient-days | 73 | 11 | 342 | 86 |
| In-hospital deaths, n (%) | 6 (37%) | 160 (15%) | 10 (33%) | 354 (13%) |
IMCU_ intermediate care unit; ICU: intensive care unit; NA: not available
* Out of all infected patients
From 25 February to 14 June 2020, a total of 19 patients (8%) from all dialysis units tested positive for SARS-CoV-2, representing an incidence rate of 73 cases per 100,000 person-days (27 cases per 100 patient-years). Thirteen patients (68%) were men and six women (32%). All infections were detected during the second epidemiological phase after 13 March 2020 but most of them (12/19) were identified in the first 2 weeks following initiation of mitigation strategies (see fig. 2 above). Eight of these infections were hospital-acquired (patients initially admitted to non-COVID wards). Of note, the only SARS-CoV-2 positive patient on peritoneal dialysis was hospitalised prior to testing positive.
Within this 17-week time period, nine patients died, six of whom were positive for SARS-CoV-2 (31%). Five deaths were COVID-19-related and one death was due to dialysis withdrawal at the patient’s request. During the same period, 1074 patients from the general population of the Geneva canton were hospitalised because of a SARS-CoV-2 infection, of whom 160 (15%) died.
Mitigation measures were highly effective at the cantonal level, with infection rates, death rates, hospitalisations and ICU admissions dropping considerably, which allowed gradual easing of the measures from 27 April 2020. By 15 June 15 2020 the first SARS-CoV-2 wave in Switzerland was officially declared over with European border restrictions lifted.
From 5 October to 31 December 2020, 60 dialysis patients were diagnosed with a SARS-CoV-2 infection, representing 342 cases per 100,000 patient-days (or 125 cases per 100 patient-years).
Thirty patients required hospitalisation (50%). Six infections (12%) were nosocomial, and the rest occurred in the outpatient setting. A total of 33 infections (55%) were traced to one dialysis centre, where an infectious cluster was discovered. Thirty-five patients were men (58%) and twenty-five patients were women (42%). Eleven patients died (18%). Ten deaths were COVID-19 related (91%).
During the same period, 2778 patients from the Geneva canton were hospitalised because of a SARS-CoV-2 infection, of whom 354 (13%) died.
During the same period, a total of seven staff members, six nurses and one physician, tested positive for SARS-CoV-2.
To our knowledge, this is the first report describing the COVID-19 epidemic in an administrative region including all patients on maintenance dialysis during two waves of the local viral spread. This is also the first report that provides insights into in-hospital mortality rates of dialysis patients as compared with the regional general population. We show several important findings: first, the incidence of SARS-CoV-2 infection may be higher in patients on maintenance haemodialysis and confers a high mortality risk, stressing the extreme vulnerability of patients on haemodialysis to in-centre viral transmission; second, most cases during both waves were related to clusters, demonstrating that social distancing and other preventive measures were successful in slowing down infection spread in this population.
The incidence rate of SARS-CoV-2 infection appears to be higher among patients on maintenance dialysis than in the general population. However, the real incidence of SARS-CoV-2 infection in the general population remains to be determined, as testing was not systematic, especially at the beginning of the epidemic, and it is likely that many mild cases were undetected. On the other hand, the threshold for testing was very low in patients on maintenance dialysis.
During the first wave, 12 patients were infected in the first 2 weeks after mitigation enforcement and 8 patients were infected in the hospital. On the basis of the incubation time of SARS-CoV-2 [13], the majority of infections were acquired before the beginning of mitigation strategies. Therefore, infection control measures for patients on maintenance dialysis should be part of a wider strategy and established as early as possible in an outbreak’s timeline in order to be efficient.
Similarly, during the second wave, more than half of the infections were traced to one dialysis centre cluster, stressing the vulnerability of dialysis patients, the importance of cluster prevention and the efficacy of preventive measures to reduce transmission rate. This was of particular importance in our region given the high local prevalence during this period, which was probably the highest in the continent.
Overall mortality rates of patients on maintenance dialysis decreased during the second wave (33% vs 18%). This is most probably a result of less severe disease among infected patients, as manifested by lower hospitalisation rates during the second as compared with the first wave (84% vs 50%). However, COVID-19-related mortality among hospitalised patients on maintenance dialysis remained similar during the second wave as compared with the first wave (37% vs 33%) despite the widespread use of promising and proven treatment strategies, including dexamethasone and high-flow nasal cannulae [14, 15].
Several recently published reports have focused on dialysis units' ongoing experience during the COVID-19 outbreak. They provide epidemiological data on infection and mortality rates in their dialysis population [16-20]. However, these reports provide data over significantly shorter periods and lack a comparison of in-hospital outcomes.
Of importance, in our cohort, death rates from COVID-19 among hospitalised patients on maintenance dialysis remained higher than those of the general population during both waves. Deceased patients had lower BMIs than those who survived a SARS-CoV-2 infection. Although these results differ from those recently published by Hsu et al. [21], there is some evidence that a higher BMI results in lower all-cause mortality among haemodialysis patients [22]. It is also likely that among those who survived, there were fewer cachectic/malnourished patients.
During the current outbreak, national authorities and infection control experts drafted specific guidance for dialysis centres. For example, the American Centers for Disease Control and Prevention (CDC) and the British National Institute for Healthcare and Excellence (NICE) provided such guidance [23,24]. Moreover, several calls for action were made, signalling the urgent need for vigilance and proposing measures to deal with the current outbreak within dialysis units [25–28]. Containment measures are more effective when they are taken as early as possible and should be part of a clear nationwide strategy and response plan [29, 30]. In addition, vaccination of this very vulnerable patient group may save lives and these patients should be prioritised, in our opinion, to promptly receive one of the available vaccines.
Moreover, the current health crisis required an important reorganisation and restructuring of health institutions worldwide. In our institution, medical outpatient activity was significantly decreased and non-urgent or elective surgeries were cancelled or postponed. Medical and surgical wards, along with their staff, were converted to admit COVID-19 patients and new dedicated wards were created to deal with the large influx of patients. Physicians and nurses from the University Hospital haemodialysis unit were also recruited to the wards or the ICU. The reduced medical staff resources created yet another challenge for the treatment of haemodialysis patients during the outbreak. Of note, in several jurisdictions SARS-COV-2 infected patients on maintenance dialysis were treated in their dialysis centre of origin, whereas our cantonal authorities decided to group all COVID-1-infected patients on maintenance dialysis in the Geneva University Hospital dialysis centre. This was done in order to avoid creation of community-based clusters and to allow optimal care based on regional resources and geography.
Patients on maintenance dialysis in Switzerland might not be offered admission to the ICU in the event of severe disease, due to comorbidities and older age [10]. In our institution, several dialysis patients who died from COVID-19 would not have been candidates for ICU admission according to local rationing criteria. None of the dialysis patients who died from COVID-19 was intubated, a finding not reported in other jurisdictions. This finding stresses the importance of infection prevention and highlights the importance of timely discussion with patients and their families about their goals of care and their values.
Our study has several limitations. The number of patients is relatively small and the whole effect of the pandemic may have not been captured as more infections may occur. In addition, we may have missed asymptomatic or pauci-symptomatic infections as we were able to preventively test during the second wave only 60% of the dialysis patients in only two dialysis centres (MVsanté and the Geneva University Hospital). However, inclusion of all patients on maintenance dialysis at the cantonal level during both waves with no losses to follow-up represent important strengths of this report.
In conclusion, the COVID-19 outbreak represents an unprecedented challenge for dialysis facilities worldwide, with high infection and case fatality rates. Early and strict mitigation measures enforced at Geneva University Hospitals in Switzerland seemed to be effective in controlling the spread of infection among patients on maintenance dialysis. Large-scale multicentre epidemiological studies are eagerly awaited to assess the efficacy of preventive measures in decreasing infection and mortality rates within the dialysis population and to increase readiness for future outbreaks.
Data were retrieved from the Swiss Dialysis Registry and are summarised in tables 1 and 2.
Anonymous raw data could be provided for specific reasons upon request.
No potential conflict of interest relevant to this article was reported.
Dr Mavrakanas has received salary support from the Department of Medicine at McGill University and is currently supported by the FRQS Junior 1 Clinician Scholar program.
Acknowledgements to our nursing staff and all our patients who had to comply with these new procedures.
Author contributions: IZ – Drafted the manuscript, participated in literature review and data collection; TAM – Critically revised the manuscript, participated in literature review and data analysis; TE, NH, BP, VB, MZ, NM, FR, RW, AI – Critically revised the manuscript, participated in data collection; PYM, SC – Critically revised the manuscript, participated in data interpretation; PS – Supervised the study, critically revised the manuscript, participated in literature review, responsible for data collection and analysis.
1 WHO. WHO announces COVID-19 outbreak a pandemic. 2020.
2 WHO . (2021, March 18). WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int
3 Fisher D , Heymann D . Q&A: the novel coronavirus outbreak causing COVID-19. BMC Med. 2020 Feb;18(1):57. https://doi.org/10.1186/s12916-020-01533-w
4 Wu Z , McGoogan JM . Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239. https://doi.org/10.1001/jama.2020.2648
5 Sohrabi C , Alsafi Z , O’Neill N , Khan M , Kerwan A , Al-Jabir A , et al. World Health Organization Declares Global Emergency: A Review of the 2019 Novel Coronavirus (COVID-19). Int J Surg. 2020;76:71-76. 10.1016/j.ijsu.2020.02.034.
6 do Sameiro-Faria M , Ribeiro S , Costa E , Mendonça D , Teixeira L , Rocha-Pereira P , et al. Risk factors for mortality in hemodialysis patients: two-year follow-up study. Dis Markers. 2013;35(6):791–8. https://doi.org/10.1155/2013/518945
7 Jordan RE , Adab P , Cheng KK. Covid-19: risk factors for severe disease and death. BMJ.2020;368:m1198. 10.1136/bmj.m1198.
8 @robinlayfield: Global Covid-19 Case Fatality Rates - CEBM. 2020.
9 Weiner DE , Watnick, SG. Hemodialysis and COVID-19: An Achilles’ Heel in the Pandemic Healthcare Response in the United States. Kidney Med. 2020;2(3):227-30. doi: 10.1016/j.xkme.2020.03.004.
10 The Swiss Academy for Medical Sciences : Intensive care medicine: triage in case of bottlenecks. & Privacy Policy, 2020.
11. Beddhu S , Bruns FJ , Saul M , Seddon P , Zeidel ML . A simple comorbidity scale predicts clinical outcomes and costs in dialysis patients. Am J Med. 2000 Jun;108(8):609–13. https://doi.org/10.1016/S0002-9343(00)00371-5
12 Federal Office of Public Health : New coronavirus: Current situation – Switzerland and international. 2020.
13 Lauer SA , Grantz KH , Bi Q , Jones FK , Zheng Q , Meredith HR , et al. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: estimation and Application. Ann Intern Med. 2020 May;172(9):577–82. https://doi.org/10.7326/M20-0504
14 RECOVERY Collaborative Group , Horby P, Lim WS, et al. Dexamethasone in Hospitalized Patients with Covid-19 - Preliminary Report [published online ahead of print, 2020 Jul 17]. N Engl J Med. 2021;384(8):693–704.https://doi.org/10.1056/NEJMoa2021436.
15 Chandel A , Patolia S , Brown AW , et al. High-flow nasal cannula in COVID-19: Outcomes of application and examination of the ROX index to predict success [published online ahead of print, 2020 Dec 16]. Respir Care. 2021;66(6):909–19. doi:https://doi.org/10.4187/respcare.08631
16 Meijers B , Messa P , Ronco C . Safeguarding the Maintenance Hemodialysis Patient Population during the Coronavirus Disease 19 Pandemic. Blood Purif. 2020;49(3):259–64. https://doi.org/10.1159/000507537
17 Alberici F , Delbarba E , Manenti C , Econimo L , Valerio F , Pola A , et al. Management Of Patients On Dialysis And With Kidney Transplant During SARS-COV-2 (COVID-19) Pandemic In Brescia, Italy. Kidney Int Rep. 2020;5(5):580–5. 10.1016/j.ekir.2020.04.001
18 Alberici, F , Delbarba, E , Manenti, C , Econimo, L , Valerio, F , Pola, A , et al. : A report from the Brescia Renal COVID Task Force on the clinical characteristics and short-term outcome of hemodialysis patients with SARS-CoV-2 infection. Kidney Int. 2020 Jul;98(1):20–6. 10.1016/j.kint.2020.04.030
19 Goicoechea M, Cámara LAS, Marañón, Muñoz de Morales A , González Rojas a , Bascuñana A, et al. COVID-19: Clinical course and outcomes of 36 maintenance hemodialysis patients from a single center in Spain. Kidney Int. 2020;8(1):27–34.10.1016/j.kint.2020.04.031<br>.
20 De Meester J , De Bacquer D , Naesens M , Meijers B , Couttenye MM , De Vriese AS ; NBVN Kidney Registry Group . Incidence, Characteristics, and Outcome of COVID-19 in Adults on Kidney Replacement Therapy: A Regionwide Registry Study. J Am Soc Nephrol. 2021 Feb;32(2):385–96. https://doi.org/10.1681/ASN.2020060875
21 Hsu CM , Weiner DE , Aweh G , et al. COVID-19 Infection Among US Dialysis Patients: Risk Factors and Outcomes From a National Dialysis Provider [published online ahead of print, 2021 Jan 16]. Am J Kidney Dis. 2021;S0272-6386(21)00025-1. doi:https://doi.org/10.1053/j.ajkd.2021.01.003
22 Jialin W , Yi Z , Weijie Y . Relationship between body mass index and mortality in hemodialysis patients: a meta-analysis. Nephron Clin Pract. 2012;121(3-4):c102–11. https://doi.org/10.1159/000345159
23 @CDCgov: Considerations for Providing Hemodialysis to Patients with Suspected or Confirmed COVID-19 in Acute Care Settings | CDC. 2020.
24 NICE : Overview | COVID-19 rapid guideline: dialysis service delivery | Guidance | NICE. 2020.
25 Kliger, AS , Silberzweig, J : Mitigating Risk of COVID-19 in Dialysis Facilities. 2020.
26 Watnick S , McNamara E. Keeping Patients on Long-Term Dialysis Safe. Clin J Am Soc Nephrol. 2020 May 7;15(5):710–13. 10.2215/CJN.03540320<br><br>.
27 Mokrzycki MH , Coco M Management of hemodialysis patients with suspected or confirmed COVID-19 infection: perspective of two nephrologists in the United States. Kidney360. 2020;1(4):273–8. 10.34067/KID.0001452020.
28 Ikizler TA . COVID-19 and Dialysis Units: What Do We Know Now and What Should We Do? Am J Kidney Dis. 2020 Jul;76(1):1–3. https://doi.org/10.1053/j.ajkd.2020.03.008
29 Li C , Romagnani P , von Brunn A , Anders HJ . SARS-CoV-2 and Europe: timing of containment measures for outbreak control. Infection. 2020;48(3):483–6. 10.1007/s15010-020-01420-9
30 @CDCgov: Evaluation of the Effectiveness of Surveillance and Containment Measures for the First 100 Patients with COVID-19 in Singapore — January 2–February 29, 2020 | MMWR. 2020.