Physician anaesthesia providers in Switzerland today and tomorrow: results of the National Anaesthesia Workforce Study (NAWOS)
DOI: https://doi.org/10.4414/SMW.2021.w30003
Guy
Hallerab, Christoph
Heimc, Kaspar
Meierd, Nicola
Clericie, Christophe
Combescuref, Michael T.
Ganterg, Jürg
Schliessbach h, Christoph
Kindleri, Urs
Eichenbergerj, Christian
Kernk
a Department of Acute Care Medicine, Division of Anaesthesiology, Geneva University Hospitals, Switzerland
b Department of Epidemiology and Preventive Medicine, Health Services Management and Research Unit, Monash University, Melbourne Victoria, Australia
c Division of Anaesthesiology, Kantonsspital Münsterlingen, Thurgau, Switzerland
d Division of Anaesthesiology, Regionalspital Surselva, Ilanz, Graubunden, Switzerland
e Servizio di anestesiologia, Ospedale Regionale di Locarno, Ticino, Switzerland
f Department of Health and Community Medicine, Division of Clinical Epidemiology, University Hospitals of Geneva and Faculty of Medicine, University of Geneva, Switzerland
g Institute of Anaesthesiology, Kantonsspital Winterthur, Switzerland
h Institute of Anaesthesiology, Zurich University Hospital, University of Zurich, Switzerland
i Anesthesia Klinik, Kantonsspital Aarau, Switzerland
j Department of Anaesthesiology, Intensive Care and Pain Medicine Balgrist University Hospital, University of Zurich, Switzerland
k Division of Anaesthesiology-Centre Hospitalier Universitaire Vaudois-CHUV, Lausanne, Switzerland
Summary
AIMS OF THE STUDY: The Swiss healthcare system is highly ranked, given its unrestricted access to specialised care and short waiting lists for surgery. However, the need for anaesthetic and surgical care is escalating owing to the increasing size and ageing of the Swiss population. In addition, to address the persistent and recurrent SARS-CoV-2 pandemic crisis, the speciality of anaesthesia is under tremendous pressure to maintain an effective workforce in order to address population needs. The current number, characteristics and future evolution of the physician anaesthesia workforce in Switzerland are currently unknown. The purpose of this study was to assess the size and professional and sociodemographic characteristics of the current anaesthesia workforce in Switzerland and to forecast its development up to 2034.
METHODS: We performed a cross-sectional study using a 150-item questionnaire prepared by the National Anaesthesia Workforce Study Group (NAWOS). We included all physicians (trainees and certified) practising anaesthesia in Switzerland. We collected demographic and professional information, such as the current position, hospital characteristics, workload, number of shifts and future life plans. We built a computer-based Markov model with Monte Carlo simulations to project both supply and demand for physician anaesthesia provider positions.
RESULTS: Of the 2661 distributed questionnaires, 1985 (74.2%) were completed and returned. We found that the average age of anaesthesiologists practising in Switzerland was 45.2 years, with 44.3% of them being women and 76.9% holding a Swiss specialist title. Only 59.6% of respondents worked full time. The forecasting model showed a steady increase in the number of anaesthesiologists retiring by 2034, with 27% of full-time equivalent jobs being lost in the next 8 years. Even if existing full-time equivalent training positions are all filled, a gradual deficit of anaesthesiologists is to be expected after 2022, and the deficit should culminate in 2034 with a deficit ratio of 0.87.
CONCLUSIONS: Due to the upcoming high retirement rate of anaesthesiologists, Switzerland is likely to face a shortage of anaesthesiologists in the near future. To compensate for the shortage, the country will likely increase its reliance on medical staff trained abroad. Southern and eastern cantons of Switzerland are particularly at risk, given that they already heavily rely on foreign anaesthesia workforce. This reliance should be considered a national priority because anaesthesiologists are heavily involved in both the treatment of patients with respiratory complications of SARS-CoV2 infection and the care of surgical patients, the number of which is expected to rise steadily in upcoming years.
Introduction
The Swiss healthcare system ranks third in the world classification of healthcare systems based on the access dimension of care [1, 2]. There are several reasons for this ranking [3]. One is the implementation of a universal and compulsory insurance coverage system that guarantees fair access to a wide range of treatments. Another is the high density of hospitals and private healthcare organisations with nearly unrestricted access for patients to all types of specialists. Furthermore, the waiting list for any type of surgical or medical treatment is typically relatively short. Finally, there is a high density of both general practitioners and specialists available for the population, including perioperative care specialists, such as surgeons or anaesthesiologists [4]. However, the sustainability of this optimistic picture is at risk, particularly access to anaesthesia care, for several reasons.
First, the speciality of anaesthesia is currently under tremendous pressure. Following the recent SARS-CoV-2 pandemic, a large number of both specialists and trainees in anaesthesia have been transferred to intensive care units (ICUs) and high-dependency units (HDUs) to care for patients affected by COVID-19. Due to their specific skills for acute care procedures and mechanical ventilation techniques, anaesthesiologists have become an indispensable part of the frontline workforce during both the first and second waves of the SARS-CoV-2 pandemic. A recent short survey of the Swiss Society for Anaesthesiology and Resuscitation (SSAR) showed that almost half of trainees and staff anaesthesiologists of public hospitals in the western part of Switzerland were sent to ICUs/HDUs to care for patients with COVID-19 disease [report of the past SSAR president Prof. C Kern]. During the same period, largely due to a lack of anaesthetic staff, many operating theatres were shut down across Switzerland. In many hospitals, only emergency or oncological surgery was performed [5]. This has resulted in a progressive increase in the size of the waiting list for surgery, whereas care for patients with COVID-19 disease is still needed.
Second, pressure on the anaesthesia workforce will also continue to grow in the future as a result of both the ongoing growth (17% over the past 20 years) and ageing of the Swiss population [6]. The number of residents aged 65 and over will increase from 18% to 27% in 2030. This will result in an increased need for surgical care and anaesthesia care [7].
In anticipation of a likely shortage of physicians, not only in anaesthesia but also in many other specialities, Swiss universities have increased the number of new medical students from 10.4/100,000 inhabitants in 2010 to 12.1/100,000 inhabitants in 2018 [8]. However, this increase has mostly benefited general internal medicine rather than anaesthesiology, with comparative increases of 30% and 13%, respectively [9, 10]. In addition, newly opened Master Programmes for medical training in four Swiss universities (Fribourg, St Gallen, Lucerne, Lugano) are mainly aimed at increasing the size of the general practitioner workforce. It is therefore unknown, in the context of a current and upcoming high demand for anaesthesiologists, whether the number of physician anaesthesia providers available in Switzerland is adequate and will be maintained in the near future.
The purpose of this study was to assess the current number of physician anaesthesia providers in Switzerland, identify their professional characteristics and career plans, and model the evolution of the size of the anaesthesia workforce in the country over the next 14 years.
Material and methods
Study design and setting
The Cantonal Commission for Ethics in Research (CCER) provided a waiver for the study (Req-2018-00738), given that it did not fall within the scope of the Swiss law on research on human beings (LRH). We performed the study between December 2018 and April 2019 in all 26 cantons (member states) of Switzerland using a cross-sectional design. All anaesthesiologists (in training or board-certified) practising anaesthesia in all categories of hospitals (teaching, nonteaching; public, private) and in office-based anaesthesia institutions (ambulatory setting) were included in the study. We also included physicians who were training in emergency medicine or intensive care and performing a 1- or 2-year rotation in anaesthesia. We excluded anaesthesiologists working full time as intensive care physicians.
Participants
The SSAR runs a national quality improvement programme named A-QUACH (Anaesthesia QUAlity in Switzerland) to which all institutions are affiliated (https://sgar-ssar.ch/a-qua/). In 2019, 188 Swiss institutions were listed in the database. In each of them, a local study coordinator was recruited and asked to disclose the number of anaesthesiologists practising in his or her institution. Anaesthesiologists working on their own were also identified and approached. We used this methodological approach given that the list of physicians of the Swiss Medical Association (FMH) does not include physicians from foreign countries working temporarily in Switzerland or those doing an anaesthesia rotation or full training. As a result, a total of 2667 potential participants were identified.
Measurement tool and variables
We used a 150-item questionnaire prepared by the NAWOS (National Anaesthesia Workforce Study) working group. The questionnaire included questions on demographic and personal information (i.e., gender, age, family status, professional training) and questions on professional activity (i.e., type of institution, position, workload, number of shifts, days and nights calls, professional and personal life plans). We also assessed general health, personal motivators for choosing the profession of anaesthesiologist, satisfaction, and the levels of stress and burnout using validated subforms. [11—13]. These subforms were not analysed for this study. The questionnaire was prepared in three of the four Swiss national languages (German, French, Italian). Validated translations from English were used for the SF-36 and Maslach questionnaires. All questionnaires were pretested for readability and acceptability within the SSAR Study Steering Committee composed of 15 trilingual professional anaesthesiologists.
Each anaesthesiologist identified by local coordinators was given a unique identifying number (ID) that included his or her institution SSAR code and a random number generated by the study coordination office. Questionnaires were then distributed individually by local coordinators to each anaesthesiologist working in their institutions. Completed questionnaires could then be sent by post mail (paper format) or answers were directly recorded on the study website https://survey.dcs.ch/sgar-ssar/it/de/fr developed by Data Conversion SA, Geneva. Both paper and electronic questionnaires were provided to maximise the response rate.
The central study office could subsequently forwarded reminders to local coordinators of institutions where not all questionnaires had been answered. Up to three reminders were sent. More than 50 regional study collaborators were involved in the whole data collection process.
Data management
The Data Manager of Data Conversion SA created an electronic file that included answers from handwritten questionnaires and those directly recorded on the website system. A double data entry approach was used to minimise the risk of recording errors when paper-based questionnaires were transformed to an electronic format. Two investigators (GH, CH) participated in the data preparation process and the interpretation of ambiguous or hard-to-decipher answers. Data were then prepared and analysed by an epidemiologist (GH) and a statistician (CC) of the Geneva University Hospitals Centre for Clinical Research (HUG_CRC).
Statistical analysis
Sample size precision calculation and descriptive analysis
With a population of 2661 physicians (specialists, in training, in temporary employment) practising anaesthesia in Switzerland, a response rate of 70% (95% confidence interval [CI] 69–71%) was planned for the survey. This represents 1862 questionnaires. With this sample size, for any of the variable assessed, the expected 95% CI of the estimated standard proportion of 0.50 would be 0.47–0.52, or ±0.023.
Sociodemographic characteristics, professional- and personal-related variables were described using frequencies and proportions. Continuous variables, such as age and working hours, were transformed into separate and mutually exclusive categories.
We used means and standard deviations for other continuous variables (retirement age). Densities were calculated with proportions using data from local investigator registries and demographic information (i.e., population by canton) from the databases of the Federal Statistical Office. Data from satisfaction and burnout questionnaires were not analysed for this study.
Modelling
For the projection model, we used a forecasting model based on supply and demand projection. These models estimate the amount of workforce needed to maintain current standards and the volume of services per capita [14]. These models are the most commonly used methods to forecast the needs of physicians [15]. We included the following variables in the model: gender, age, type of professional training and diploma, country of origin, professional activity and position, type of institution, professional life plan, desired retirement age and full- or part-time work. The latter was defined according to the number of days of professional activity per week with full-time being five days per week.
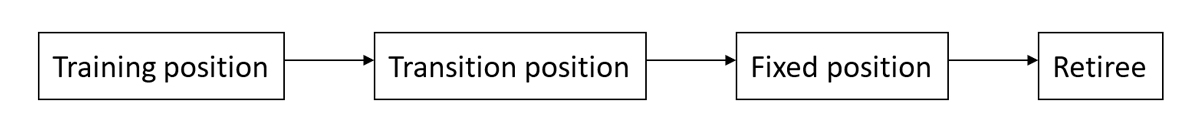
We developed a computer-based Markov model to project both supply and demand for anaesthesia positions until 2034. These models allow the analysis of several different factors affecting the workforce and are commonly used in workforce projection studies [16, 17]. In our model, we considered that factors affecting demand were official and desired retirement age (when expressed), gender, demographic distribution of existing workforce, number of long-term positions available (consultant in a private or public hospital, leading positions in public hospitals, office-based anaesthesia) and age of diploma. The supply-side assumptions of the model were that a fixed quota of trainees would enter the anaesthesia workforce each year and that the number of foreign trained physicians working in anaesthesia care would remain constant. In the model,we defined the training position as all positions filled by a noncertified anaesthesiologist (internship). Transition positions were all those that were filled by certified anaesthesiologists (advanced residency positions named in Switzerland “chef de Clinique”; “Oberarzt”; “capo di clinica”). We defined fixed positions as those that were filled by certified anaesthesiologists working as consultants in private hospitals or staff anaesthesiologists in a public hospital or those performing office-based anaesthesia. The transition probability among the training position (internship), transition positions and fixed positions was determined by the number of individuals in training, the duration of training, favoured retirement age, gender and the number of part/full-time positions available. The model’s assumption was that fixed positions would constantly be filled by the existing pool of anaesthesiologists in transition positions.
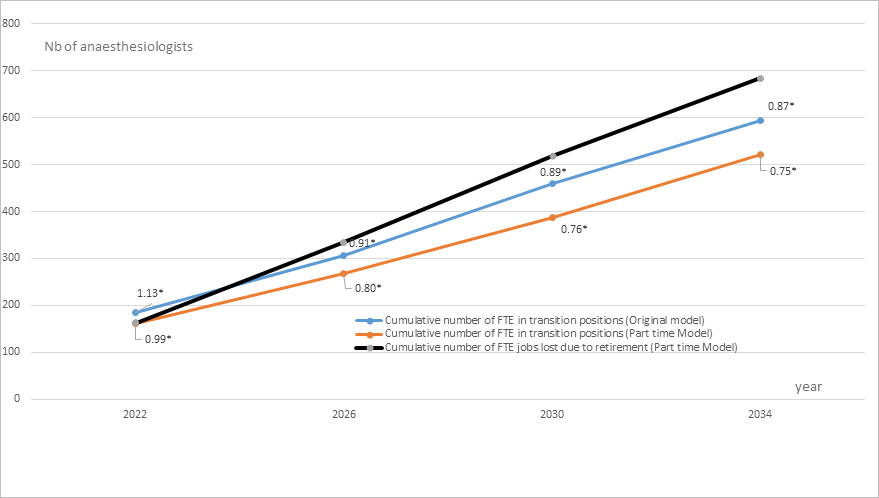
The model developed is illustrated in figure 1. Monte Carlo methods were used to assess the number of anaesthesiologists in each state of the model and their transition probability to the next state. The resultsare reported as absolute numbers with 95% CIs.
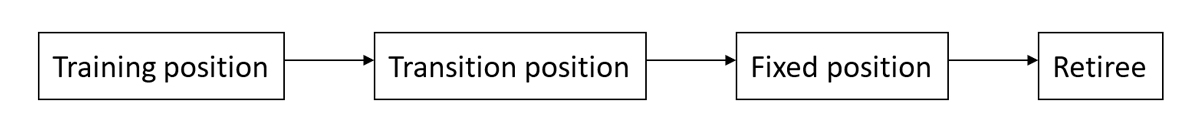
Figure 1 Diagram of the four-state Markov model used to predict the distribution of anaesthesiologists.
The four states of the model represent the different possible positions of anaesthesiologists during their careers in Switzerland. Training includes the period between graduation from medical school and speciality completion (internship). Transition position (advanced residency positions named in Switzerland “chef de Clinique”; “Oberarzt”; “capo di clinica”) represents the period between speciality completion and nomination to a senior position in a hospital or as an independent practitioner in a private setting. These are named fixed positions. The final state of the diagram is retirement. All transitions probabilities in this Markov model are calculated through Monte-Carlo simulations. To model the evolution of physician anaesthesia workforce in Switzerland based on a defined quota of interns starting training in anaesthesia that fills all available training positions.
Sensitivity analysis
To the original model, two additional scenarios were added. One was the likely increase of Switzerland's population by 2034. The other was the likely augmentation of part-time work among anaesthesiologists working in Swiss hospitals, due to the rising number of women entering the profession as well as the aspiration of younger anaesthesiologists for an improved work life balance [18, 19].
For the increased population scenario, we used calculations of the Swiss Federal Office of Statistics projecting a population of 9,347,230 residents in Switzerland by 2034 [7]. Based on the assumption that there would be an increase in the number of surgical procedures proportional to the population growth, we calculated an increase in the number of surgical procedures from 1,071,054 in 2019 to 1,171,733 procedures in 2034. This corresponds to an overall 9.4% increase. Based on the hypothesis that increased workload would mainly affect anaesthesiologists in fixed positions (since the number of transition positions are determined in our model by gender, duration of training, part/full time work), a needed increase of up to 88 full-time equivalents (FTEs) by 2034 was calculated in order to guarantee the same anaesthesiologist/patient ratio. Distributed over the whole time period of our model, this represents an incremental number of 22 FTE positions needed every 4 years in fixed positions. These figures were integrated into the original model to calculate the overall number of fixed positions missing as a result of retirement and increased workload. (sensitivity analysis 1).
For the augmentation of part-time work scenario (sensitivity analysis 2) we made the following assumptions based on the finding that in our current survey, 23% of anaesthesiologists in transition position were working part time. Assuming that part-time work = 0.50 FTE, this proportion represents in terms of FTE positions: N × (0.23 × 0.50 + 0.77 × 1) = N x 0.885 FTE. Based on a comparison of the figures of the current survey with a previous demographic survey performed in 2009 [20], we assumed that, by 2034, women would represent 61% of the overall workforce. Applying the FTE calculation formula to the current proportion of women/men working part time, the overall proportion of anaesthesiologists in transition positions working part time in 2034 would be 45%. In terms of FTEs this would represent: N × (0.45 × 0.50 + 0.55 × 1) = N × 0.775 FTE. As a result, the new number of FTE positions with 45% of anaesthesiologists in transition positions working part time would be: current FTE × 0.775 / 0.885 or new FTE = current FTE × 0.876. These calculations were integrated into the original model to project the additional number of anaesthesiologists in transition positions missing due to part-time work (sensitivity analysis 2).
Statistical analyses were performed with Stata/IC 12.0 (Stata-Corp, College station, TX) and S-Plus 8.0 for Windows (Insightful Corp., Seattle, WA).
Results
Participation rate and density of anaesthesiologists
Following the initial round and two additional reminders, 74.2% (n = 1985) of identified participants returned a completed questionnaire. The highest participation rates were recorded in the cantons of Obwalden, Uri and Zug, where a 100% response rate was achieved. Since our participation rate was larger than the initially planned 70%, the precision of our results is even better than the projected ±0.023.
Through the initial list of the SSAR, we identified 2667 physician anaesthesia providers in Switzerland. This represents 1/3194 inhabitants or 31.3/100,000 inhabitants. The highest density was found in the canton of Basel City (81.4/100,000), Zurich (40.5/100,000), the canton of Schaffhausen (39/100,000) and Bern (34.6/100,000). The lowest density of anaesthesiologists was in the cantons of Fribourg (16/100,000), Jura (13.6/100,000) and Uri (11/100,000). Details are provided in table 1.
Table 1Density of anaesthesiologists by cantons in Switzerland.
|
Canton
|
Absolute number of anaesthesiologists*
|
Number of anaesthesiologists per 100,000 inhabitants
†
|
| Aargau |
202 |
29.9 |
| Appenzell Inner-Rhode |
11 |
68.2 |
| Appenzell Outer-Rhode |
13 |
23.5 |
| Bern |
359 |
34.6 |
| Basel-Country |
72 |
25.0 |
| Basel-City |
159 |
81.4 |
| Fribourg |
51 |
16.0 |
| Geneva |
168 |
33.6 |
| Glarus |
11 |
27.2 |
| Graubunden |
59 |
29.7 |
| Jura |
10 |
13.6 |
| Lucerne |
124 |
30.2 |
| Neuchâtel |
30 |
17.0 |
| Nidwalden |
14 |
32.5 |
| Obwalden |
5 |
21.1 |
| St Gallen |
150 |
29.5 |
| Schaffhausen |
32 |
39.0 |
| Solothurn |
83 |
30.3 |
| Schwyz |
26 |
16.4 |
| Thurgau |
55 |
19.8 |
| Ticino |
96 |
27.2 |
| Uri |
4 |
11.0 |
| Vaud |
219 |
27.3 |
| Valais |
67 |
19.5 |
| Zug |
30 |
23.7 |
| Zurich |
617 |
40.5 |
|
Total
|
2667
|
31.3
|
Personal characteristics of anaesthesiologists
The majority of anaesthesiologists (55%) were between 35 and 55 years old, with an average age of 45.2 years (SD 10.7). The proportion of women was 44.3%, and more than 85% of anaesthesiologists lived with a partner. Among those living alone, approximately two thirds (62.1%) were women. Approximately 58.3% of anaesthesiologists had a child with 12.1% of them having three or more children.
The majority of anaesthesiologists (68.1%) were of Swiss origin. European nationals represented 30.8% of the total workforce, and only 1.1% were from non-European countries (mainly Africa and South America). Among Europeans, anaesthesiologists from Germany (71.7%), Italy (12.2%) and France (8.9%) represented the majority of anaesthesiologists. Details are provided in table 2.
Table 2Demographic characteristics of participants.
|
Variables
|
Numbers (%)
n = 1985
|
| Gender |
Female |
853 (44.3%) |
| Male |
1071 (55.7%) |
| Age |
<35 years |
453 (23.6%) |
| 35–55 years |
1054 (55.0%) |
| >55 years |
410 (21.4%) |
| Mean (SD) |
45.2 (10.7) |
| Single |
Yes, |
285 (15.0%) |
| — Female |
177 (62.1%) |
| — Male |
108 (37.9%) |
| No |
1621 (85.0%) |
| Number of minor dependent children in the family |
0 |
614 (41.7%) |
| 1 |
279 (19.0%) |
| 2 |
399 (27.1%) |
| 3 |
146 (9.9%) |
| 4 |
27 (1.8%) |
| 5 |
5 (0.3%) |
| 6 |
1 (0.1%) |
| Nationality |
Swiss |
1311 (68.1%) |
| European |
594 (30.8%) |
| — German |
426 (71.7 %)* |
| — Italian |
73 (12.2 %)* |
| — French |
53 (8.9%)* |
| Other European countries |
42 (7.2)* |
| Other countries |
24 (1.1%) |
Professional characteristics and future life plan
The majority of anaesthesiologists (76.9%) were trained in the speciality and had a Swiss specialist title diploma. Only 59.6% of anaesthesiologists worked full time, and the others (40.4%) worked between 10% and 95%. The average working time was 50.8 hours/week (SD 18.5). The majority of anaesthesiologists (59.2%) worked 50 hours or less per week (median of the distribution). However, approximately one third of them (31.9%) worked between 51 and 69 hours per week. In total, 8.9% of anaesthesiologists exceeded 70 hours per week (table 3). Anaesthesiologists of Swiss origin represented 80.3% of the workforce in private hospitals, whereas anaesthesiologists of European origin worked in all types of hospitals and more often in office-based anaesthesia (38.6%). Non-European anaesthesiologists worked mainly in regional hospitals. Although the legal age for retirement in Switzerland is 64 years for women and 65 years for men, 443 (26.3%) anaesthesiologists wished to retire earlier, on average at 63.4 years of age (SD 2.1) for men and 60.0 years (SD 2.8) for women. The majority of trainees (60.6%) were in their third to sixth year of training. Details are provided in table 3.
Table 3 Professional characteristics and life plans of anaesthesiologists in Switzerland.
|
Characteristic
|
n (%)
|
| Type of hospital |
Public hospital |
1496 (77.3%) |
| Private hospital |
368 (19.0%) |
| Office-based |
71 (3.7%) |
| Full/part time |
Full-time |
1122 (59.6%) |
| Part-time |
762 (40.4%) |
| Working hours |
≤50 hours |
1120 (59.2%) |
| 51–69 hours |
603 (31.9%) |
| ≥70 hours |
169 (8.9%) |
| Overall, mean (SD) |
50.8 (18.5) |
| Wished retirement age (years) |
Males, mean (SD) |
63.4 (2.1) |
| Females, mean (SD) |
60.0 (2.8) |
| Total number of anaesthesiologists wishing changes |
443 (26.3%) |
| SIWF (FMH) title* |
No |
442 (23.1%) |
| Yes |
1470 (76.9%) |
| Training years |
≤2 years |
49 (13.7%) |
| 3 to 4 years |
108 (30.3%) |
| 5 to 6 years |
108 (30.3%) |
| 7 to 8 years |
60 (16.8%) |
| 9 +years |
32 (9%) |
| Type of professional activity |
All types of anaesthesia |
1317 (71.1%) |
| All types with specialisation |
392 (21.2%) |
| Only specialised anaesthesia |
144 (7.8%) |
| Job position |
| All anaesthesiologists |
Fixed |
940 (52%) |
| Transition |
507 (28.1%) |
| Training |
359 (19.9%) |
| European and extra-European |
Fixed |
31 (41%) |
| Transition |
20 (27%) |
| Training |
24 (32%) |
| Type of hospital by nationality |
| Swiss |
University hospital |
499 (68.8%) |
| Regional hospital |
282 (61.0%) |
| Private hospital |
290 (80.3%) |
| Office-based |
42 (60.0%) |
| European |
University hospital |
220 (30.3%) |
| Regional hospital |
172 (37.2%) |
| Private hospital |
68 (18.8%) |
| Office-based |
27 (38.6%) |
| Extra-European |
University hospital |
6 (0.8%) |
| Regional hospital |
8 (1.7%) |
| Private hospital |
3 (0.8%) |
| Office-based |
1 (1.4%) |
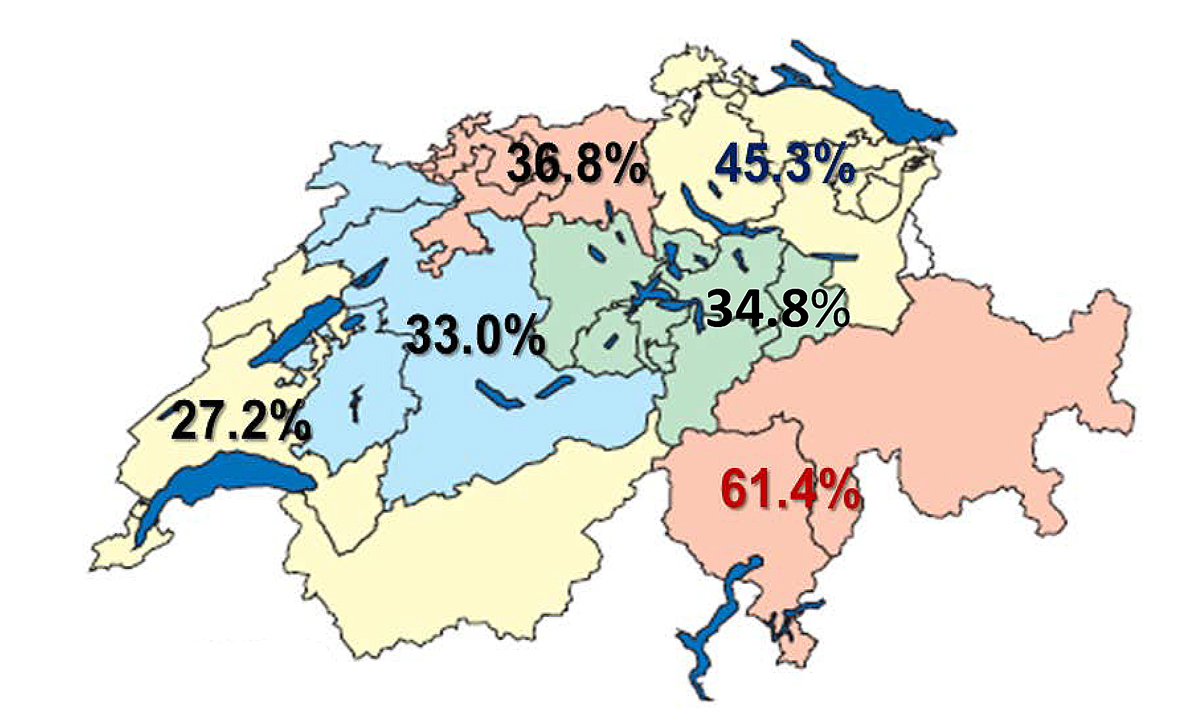
The proportion of anaesthesiologists with a non-Swiss medical degree varied widely between the different areas of Switzerland. The highest proportion (61.4%) was found in the southern parts (region 6 of the Swiss Federal Office of Public Health, FOPH: GR = Graubunden and TI = Ticino) and the eastern parts (45.3%) of the country (region 5: AI = Appenzell Inner-Rhodes; AR = Appenzell Outer-Rhodes; GL= Glarus; SG = St Gallen; SH = Schaffhousen; TU = Thurgau; ZH= Zurich) (fig. 2).
When the level of seniority of trainees was analysed, we found that the cantons of Bern, Fribourg and Jura (region 2 FOPH that includes BE; FR; JU) had the largest proportion of advanced trainees in contrast with Graubunden and Ticino (region 6 FOPH that includes GR and TI) that had the highest number of trainees at the early beginning of their training period. Details are provided in table 4.
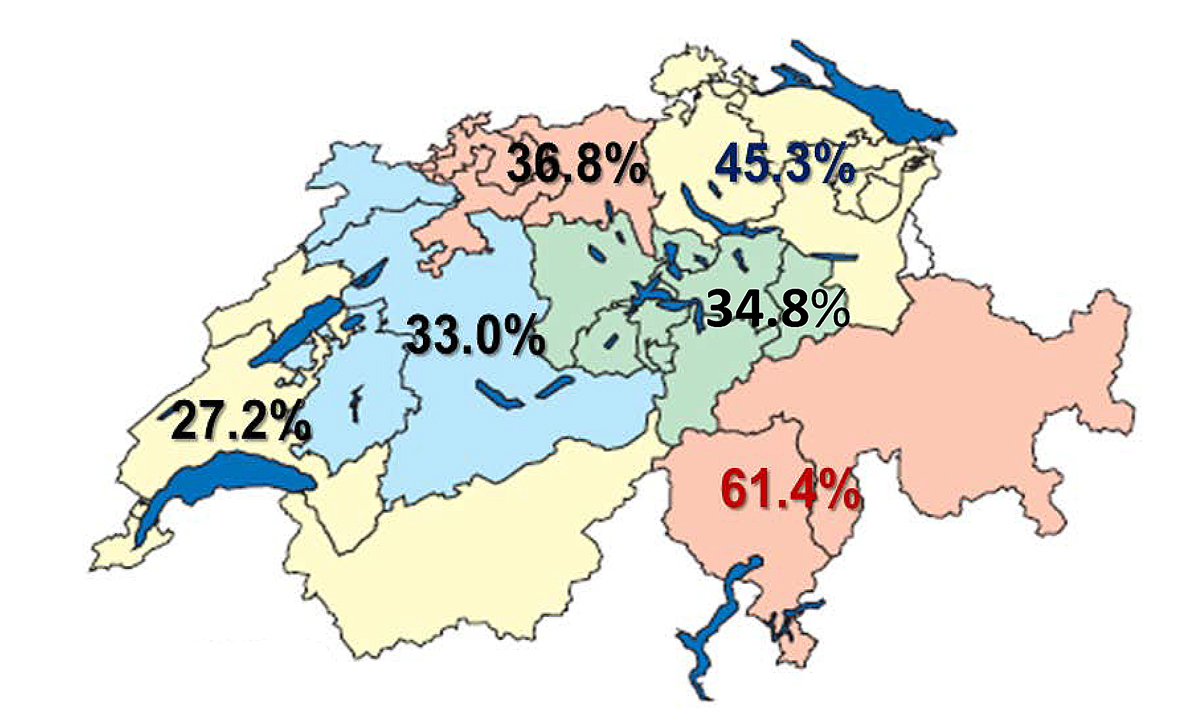
Figure 2 Distribution of anaesthesiologists with a non-Swiss medical degree (N = 872).
Table 4Number of trainees according to the different areas of Switzerland in 2019.
|
Training years
|
Region 1 (GE, NE, VD, VS)
|
Region 2 (BE, FR, JU)
|
Region 3 (AG, BL, BS, SO)
|
Region 4 (LU, NW, OW, SZ, UR, ZG)
|
Region 5 (AI, AR, GL, SG, SH, TG, ZH)
|
Region 6 (GR, TI)
|
| ≤2 years |
4 |
2 |
13 |
3 |
25 |
2 |
| 3 to 4 years |
29 |
10 |
24 |
11 |
29 |
5 |
| 5 to 6 years |
21 |
24 |
20 |
15 |
26 |
2 |
| 7 to 8 years |
15 |
6 |
12 |
2 |
24 |
1 |
| 9 and + years |
7 |
2 |
13 |
1 |
8 |
1 |
|
Total
|
76
|
44
|
82
|
32
|
112
|
11
|
Projection over upcoming years
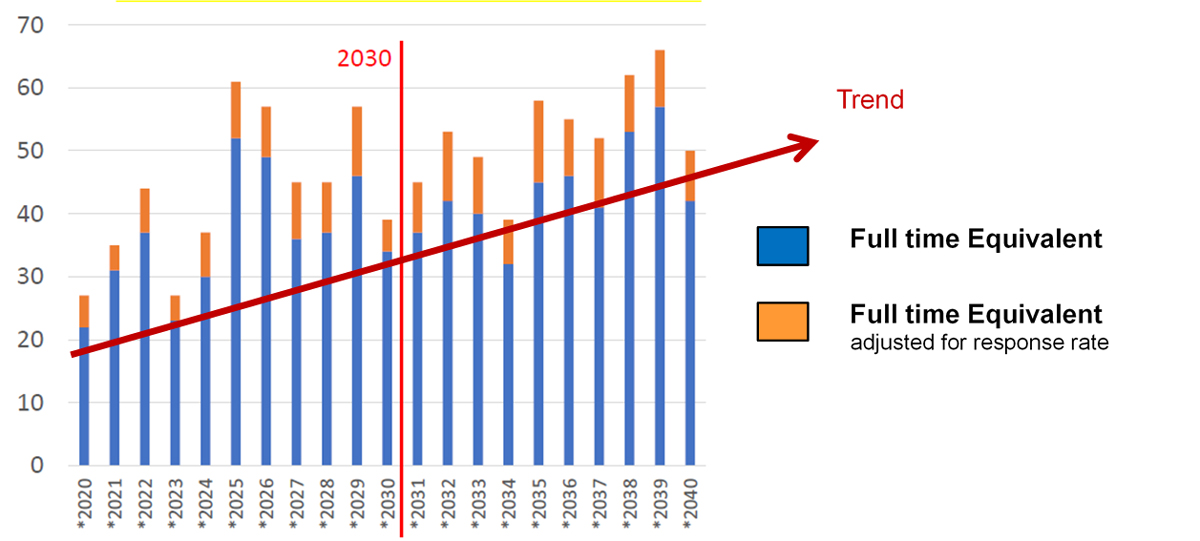
The model shows a steady increase in the number of anaesthesiologists retiring by 2030 with an average of 30 to 40 FTEs (95% CI 20–55) being lost each year (fig. 3). In addition, to keep the overall number of trainees steady, an average of 51.7 to 56.3 new FTE trainee positions must be filled each year up to 2022, and 31.3 to 44.7 during the five following years. The eastern (region 5: AI/AR/GL/SG/SH/TG/ZH) and northern parts of Switzerland (region 3: AG; BL; BS, SO) are the areas that should recruit the largest number of new interns in anaesthesia. In these areas, retirement will occur at a fast pace, and fixed positions will be quickly filled by physicians in transition positions. This will leave a significant number of advanced training positions empty.
From 2024 onward, a slight decrease in the number of FTE positions lost will occur, allowing the recruitment of a lower number of trainees to maintain a steady state in training positions with a range of between 31.3 and 48.2 FTE trainee positions. However, this finding implies that commitments must be made beforehand to maintain a constant number of trainees until 2024. Details are provided in table 5.
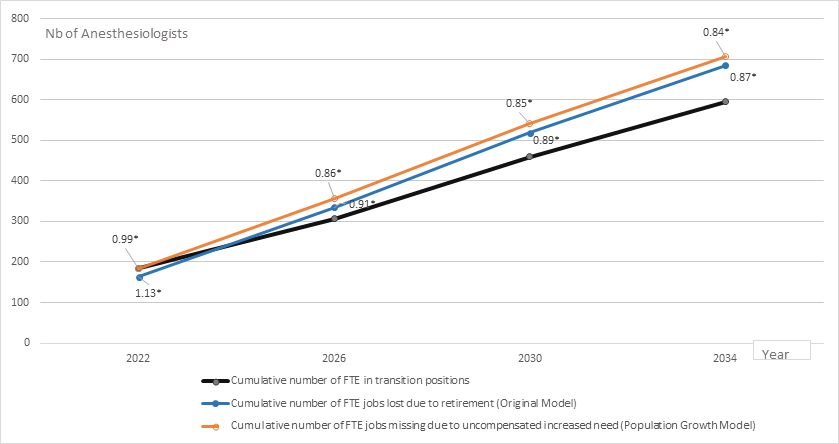
Table 6 shows data of the full forecasting supply model starting in 2019 and stratified by 4-year periods up to 2034. The model details the number of anaesthesiologists (FTE) reaching transition positions, those retiring and the ratio between the two. A ratio greater than 1 indicates that anaesthesiologists in transition will compensate for FTE positions lost due to retirement, whereas a ratio of less than 1 indicates a deficit. The model shows that even if new trainees are actively recruited each year to fill in all empty training positions (table 5), they will not be able to compensate for transition positions left empty by a major shift of the workforce towards fixed positions in a timely manner. A deficit of anaesthesiologists in transition positions is to be expected at a national level after 2023 due to retirement of the baby boomer generation. This phenomenon will worsen over the years with a deficit ratio of 0.87 by 2034 at the national level. This deficit will be particularly significant in southern parts, region 6 (GR; TI), central parts (region 4: LU; NI; OB;SZ; UR; ZU) and northwestern parts (region 2: BE; FR; JU) of Switzerland. In contrast, regions 1 (GE; NE; VD; VS) and 3 (AG; BL; BS; SO) will be spared and seem to be heading towards a positive ratio.
Table 5Average number new trainees (FTE) to be recruited annually to maintain a constant number of trainees.
|
Year
|
Switzerland
|
Region 1 (GE, NE, VD, VS)
|
Region 2 (BE, FR, JU)
|
Region 3 (AG, BL, BS, SO)
|
Region 4 (LU, NW, OW, SZ, UR, ZG)
|
Region 5 (AI, AR, GL, SG, SH, TG, ZH)
|
Region 6 (GR, TI)
|
| 2019 |
55.6 |
12.0 |
7.8 |
13.5 |
3.6 |
16.5 |
1.1 |
| 2020 |
55.4 |
12.7 |
9.4 |
11.5 |
5.0 |
15.4 |
1.4 |
| 2021 |
56.3 |
13.0 |
8.0 |
12.2 |
5.7 |
15.7 |
1.7 |
| 2022 |
51.7 |
12.2 |
6.8 |
11.0 |
5.3 |
14.8 |
1.6 |
| 2023 |
44.7 |
9.6 |
4.6 |
10.1 |
4.5 |
14.1 |
1.5 |
| 2024 |
34.5 |
6.7 |
3.0 |
8.0 |
3.2 |
12.0 |
1.2 |
| 2025 |
31.3 |
5.7 |
3.0 |
7.6 |
2.6 |
11.2 |
1.2 |
| 2026 |
33.6 |
6.2 |
3.8 |
8.6 |
2.6 |
11.0 |
1.0 |
| 2027 |
40.7 |
8.4 |
5.5 |
9.4 |
3.3 |
12.8 |
1.2 |
| 2028 |
44.8 |
9.8 |
6.3 |
9.9 |
4.0 |
13.4 |
1.3 |
| 2029 |
48.2 |
10.7 |
6.6 |
10.6 |
4.5 |
14.2 |
1.4 |
| 2030 |
47.2 |
10.4 |
6.1 |
10.4 |
4.5 |
14.2 |
1.4 |
| 2031 |
43.3 |
9.3 |
5.1 |
9.7 |
4.1 |
13.5 |
1.4 |
| 2032 |
39.7 |
8.2 |
4.5 |
9.1 |
3.7 |
12.7 |
1.3 |
| 2033 |
38.1 |
7.7 |
4.3 |
8.9 |
3.4 |
12.4 |
1.2 |
| 2034 |
38.3 |
7.8 |
4.5 |
8.9 |
3.3 |
12.3 |
1.2 |
Table 6Ratio between anaesthesiologists in transition position filled in by residents having completed their speciality training and anaesthesiologists lost because of retirement.
|
Switzerland
|
Region 1 (GE, NE, VD, VS)
|
Region 2(BE, FR, JU)
|
Region 3 (AG, BL, BS, SO)
|
Region 4 (LU, NW, OW, SZ, UR, ZG)
|
Region 5 (AI, AR, GL, SG, SH, TG, ZH)
|
Region 6(GR, TI)
|
|
Cumulative number of new FTE jobs in transition positions
|
| Over next 4 years (2022) |
184.9 |
42 |
27.1 |
39.5 |
16.4 |
53.8 |
4.5 |
| Over next 8 years (2026) |
306.3 |
66.2 |
39.2 |
67.5 |
27.3 |
94.9 |
8 |
| Over next 12 years (2030) |
459.7 |
99.6 |
60 |
101.8 |
41.1 |
141 |
12.4 |
| Over next 16 years (2034) |
594.8 |
127.6 |
75.6 |
132.8 |
53.4 |
184.2 |
17.3 |
|
Cumulative number of FTE jobs lost due to retirement (transition+fixed positions)
|
| Over next 4 years (2022) |
163 |
27.5 |
26.5 |
24 |
16 |
52 |
13 |
| Over next 8 years (2026) |
335 |
52.5 |
55.5 |
48.5 |
37.5 |
106 |
30 |
| Over next 12 years (2030) |
518.5 |
77.5 |
82.5 |
78 |
56 |
170.5 |
48 |
| Over next 16 years (2034) |
684.5 |
103 |
105.5 |
115 |
72 |
219.5 |
63.5 |
|
Cumulative ratio of FTE new transition positions / retirements
|
| Over next 4 years (2022) |
1.13 |
1.53 |
1.02 |
1.65 |
1.03 |
1.03 |
0.35 |
| Over next 8 years (2026) |
0.91 |
1.26 |
0.71 |
1.39 |
0.73 |
0.90 |
0.27 |
| Over next 12 years (2030) |
0.89 |
1.29 |
0.73 |
1.31 |
0.73 |
0.83 |
0.26 |
| Over next 16 years (2034) |
0.87 |
1.24 |
0.72 |
1.15 |
0.74 |
0.84 |
0.27 |
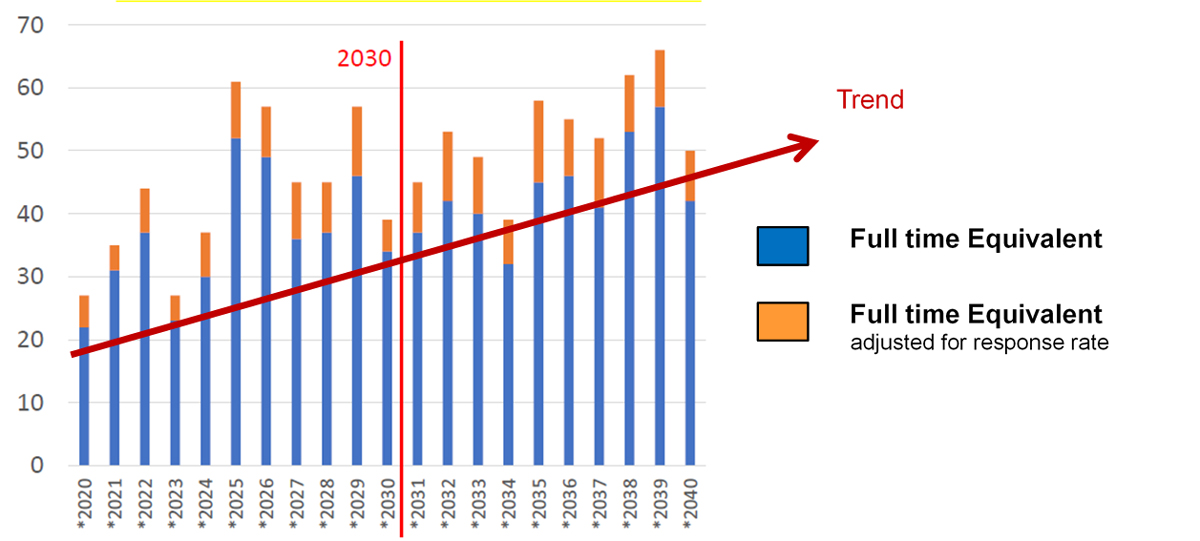
Figure 3 Bar chart of full-time equivalent (FTE) anaesthesiologist positions lost due to retirement over the years.
Sensitivity analysis
We projected an increase of 9.4% in the overall number of surgical procedures by 2034. This would represent 88 FTE fixed positions lacking over the time period. This would result in an increased imbalance between anaesthesiologists in transition and those in fixed positions. In 2022 this imbalance would increase from a ratio of 1.13 to 0.99 and in 2034 from 0.87 to 0.84 resulting in more anaesthesiologists needing to be trained to compensate for the lack (fig. 4).
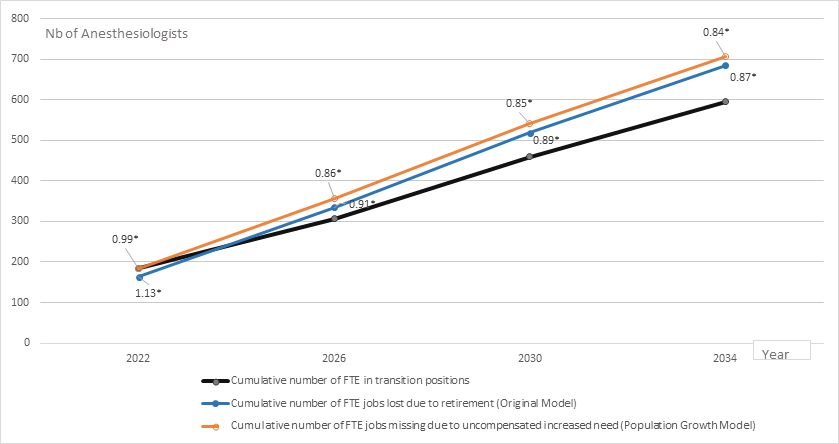
Figure 4 Cumulative change over time in the number of full-time equivalent (FTE) fixed positions according to original and increased population scenarios.
* Ratio of FTE transition positions / FTE jobs lost due to retirement or missing due to uncompensated increased need following population growth [stability =1].
When modelling part-time work we also found that an increasing number of anaesthesiologists in transition positions would be lacking in the future, from 22.9 in 2022 to 73.8 FTE in 2034. This would result in an imbalance between anaesthesiologists in transition and those in fixed positions, from a ratio of 0.99 in 2022 to 0.75 in 2034 (fig. 5).
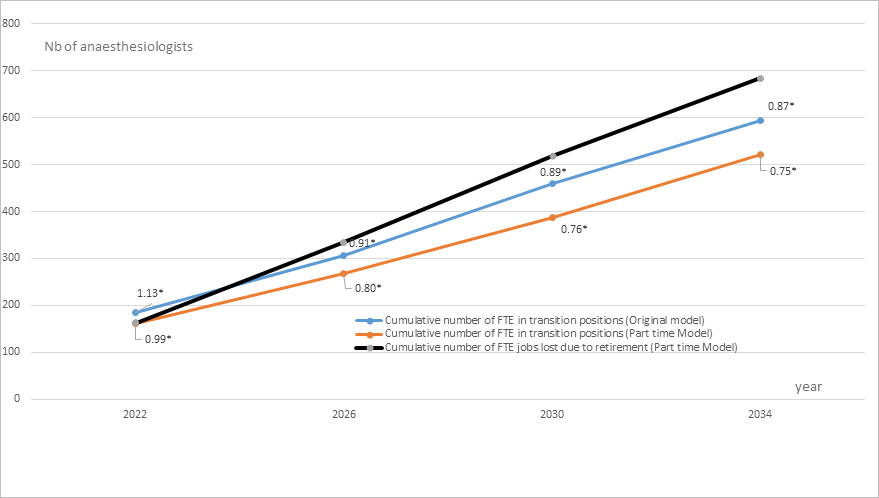
Figure 5 Cumulative change over time in the number of full-time equivalent (FTE) transition positions according to original and increased part-time scenarios.
* Ratio of FTE transition positions / FTE jobs lost due to retirement (stability = 1).
Discussion
We found a density of 31.3 anaesthesiologists for 100,000 inhabitants in Switzerland. This density was greater than most countries in the world except Austria, which has 39.3 anaesthesiologists for 100,000 inhabitants [21]. The international comparisons of such data should, however, be made with caution. Some countries (Australia, New Zealand, UK) consider only certified physicians to be full anaesthesia providers, whereas others, such as the United States, include anaesthesia nurses (43,570 nurse anaesthesia providers in 2019) in their calculation [22, 23]. This difference makes it difficult to make reliable comparisons between countries. In our study, we did not include anaesthesia nurses, but we also calculated the density of anaesthesiologists by canton. As a result, we found significant variations between the different areas of the country. In some cantons, such as Basel-City, the value reached 81.4 per 100,000 inhabitants. However, in the cantons of Neuchatel or Jura, with 17 and 13.6 anaesthesiologists per 100,000 inhabitants, respectively, the density of anaesthesiologists was lower than that in many countries, including Ireland, Poland and the UK.
This phenomenon is likely explained by the increasing concentration of advanced surgical care in university-affiliated hospitals in large cities of Switzerland. This results in a higher number of procedures being performed in these categories of institution [4, 24]. These hospitals also have a larger number of training positions available. This automatically increases the size of the anaesthesia workforce in specific areas of the country.
In our study, we also found that following retirement of a high number of anaesthesiologists over the next 8 upcoming years, an average of 30 to 40 FTE positions (95% CI 20–55) will be lost yearly. These departures should be compensated for if the rate of new interns starting their training in anaesthesia is maintained at the current rate, but only up to 2022 and not in the cantons of Graubunden and Ticino. These two cantons will see a significant number of anaesthesiologists retiring in the following 4 years and do not have sufficient trainees to fill positions left empty, particularly advanced residency positions (transition jobs). In the next 8 years, the model shows that other regions of Switzerland are progressively going to lack anaesthesiologists. This is the case for central parts (region 4: LU; NI; OB; SZ; UR; ZU) and northwestern parts (region 2: BE; FR; JU) of Switzerland. To a lesser extent, by 2026, the eastern part of the country (region 5: AI; AR; GL; SG; SH; TG; ZH) will also start to lack anaesthesiologists. For the latter and the cantons of Graubunden and Ticino (region 6), the situation may become particularly critical, given that these regions require a high number of new trainees to compensate for retirements. Furthermore, in contrast to the western region of Switzerland, which includes three universities (Geneva, Lausanne, Bern), these regions largely rely on the University of Zurich and the recently founded “Università della Svizzera italiana” to provide a supply of new trainees likely to join the speciality. Although a large proportion of the Swiss population (2.6 million) commutes to work in another canton on a daily basis, moving to live in another part of the country is not common (1.7%) [25]. Intercantonal mobility is therefore unlikely to compensate for these shortages in areas of the country that are not easily and quickly reachable on a daily basis (i.e., Appenzell, Ticino, Graubunden). Another issue is the large number of hospitals in Graubunden, which disperses the overall workforce in several different institutions. Training positions in these areas are therefore quite unlikely to become occupied by graduates from Swiss universities. The sensitivity analysis performed to model the additional impact of a likely increase in the size of the Swiss population and of part-time work in the future shows that the lack of anaesthesiologists could already start at a National level in 2022 and could become very serious by 2034, particularly in the increased part-time work model.
A common mechanism to compensate for this type of staff shortage is to hire anaesthesiologists (trained or in training) from abroad. However, this strategy should be considered only as a temporary buffer. The proportion of foreign anaesthesiologists in Switzerland is already high, particularly in the eastern and southern parts of Switzerland at 45.3% and 61.4%, respectively.
Should policies from neighbouring European countries become more restrictive for physician mobility, particularly in the current context of the SARS-CoV-2 pandemic, these parts of Switzerland would experience a severe and uncontrollable shortage of physician anaesthesia providers. Furthermore, attracting physicians trained abroad is likely to further increase the brain drain in neighbouring countries [26, 27]. Western OECD countries, particularly Switzerland, are the primary destinations for medical migrants, resulting in a shortage of physicians, particularly in east European countries [28]. The brain drain has serious negative consequences on the overall functioning of healthcare systems of countries with a negative immigration balance and should be considered unethical [29, 30].
To compensate for the upcoming shortage of anaesthesiologists in Switzerland, a number of alternative strategies could also be considered. One strategy is the active promotion of the speciality of anaesthesia among medical students. This speciality is little known, and few formal training tracks exist at the undergraduate level. Another strategy could be to retain the existing workforce by increasing retirement age and working hours. However, these strategies are quite unlikely to work. More than one quarter (26.3%) of anaesthesiologists interviewed wanted to retire earlier. Our study also showed that the average working time was already 50.8 hours per week and was even higher for anaesthesiologists in fixed positions with additional management or academic commitments. Anaesthesiologists had working hours often exceeding 70 hours a week. It is therefore unlikely that working hours can be augmented much further, given that working hours for physicians in public hospitals are limited to 50 hours a week [31, 32]. Another option could be the implementation of independent anaesthesia nurse practitioners. In Switzerland, nurse anaesthetists represent a significant part of the anaesthesia workforce. Nurse anaesthetists can perform a large number of procedures, including tracheal intubation, drug administration and anaesthesia surveillance. However, these procedures can only be performed under the strict supervision of a certified anaesthesiologist, and there is significant controversy as to whether this approach would be detrimental or beneficial to the overall quality of anaesthesia care provided [33, 34]. Furthermore, the recruitment of nurses can be quite difficult, and many countries, including Switzerland, suffer from nurse workforce shortages [35]. Another alternative is to increase productivity through financial incentives (i.e., fee-for-service payments), technological innovation and the development of day-care surgery [36]. Some of these policies to increase productivity are already ongoing. For instance, an increasing number of surgical procedures in Switzerland are performed on a day-care basis. This increases productivity through enhanced patient turnover in hospitals. Replacing cost reimbursement by activity-based payments is another method to enhance productivity, given that it rewards efficiency [37]. However, this strategy has limitations. If patient turnover is escalated excessively, the overall quality of the service provided can be jeopardised. In contrast to the manufacturing industry, healthcare productivity cannot be increased perpetually given that a minimum staff/patient ratio needs to be achieved to minimise the risk of adverse outcomes [38, 39]. This notion is especially true in anaesthesia, a high-risk speciality [40—42]. Nevertheless, to respond to the upcoming likely physician anaesthesia workforce shortage, all these options should be explored, and their combination is likely to produce the best expected results.
There are a number of limitations to this study that should be mentioned. First, we used a cross-sectional study design, which can only provide a snapshot of the workforce status from which extrapolations are performed. These cannot be considered as definite conclusions. Second, in our supply statistical model, we assumed that, over the years, a predefined quota of new trainees would enter the workforce and that a constant number of European and extra-European trainees and senior residents would join the workforce. The model does not take into account more restrictive policies that limit the migration of foreign physicians to Switzerland. Our model is therefore only one of several possible scenarios that may occur in the near future. Third, information on anaesthesiologists working in intensive care units was lacking. A number of these anaesthesiologists also worked part time in operating theatres and reinforced the anaesthesia workforce. Our model may therefore have undercounted the true size of the anaesthesia workforce. However, the current workforce shift from anaesthesia to the ICU to care for COVID-19 patients shows that it is unlikely that ICU units will be able to compensate for a future shortage of anaesthesiologists. Finally, to build our model, we used both legal and desired retirement age. Due to social desirability and temporary excess workload, some anaesthesiologists may have shortened or increased the real duration of their working careers, potentially causing some measurement errors.
Despite these limitations, the current study provides an interesting overview of the current and future development of physician anaesthesia workforces in Switzerland in a large sample of anaesthesiologists in all 26 cantons of the country. Future studies should explore this problem in other specialities, particularly given that the COVID-19 pandemic is challenging the future of the workforce across all medical disciplines.
Conclusions
Due to the progressive ageing of the Swiss population and an increasing demand for surgical and acute care, particularly in the case of recurring SARS-CoV-2 epidemics, there will be an increasing demand for anaesthesiologists. Due to retirement and a lack of medical graduates from Swiss universities who will likely not compensate for the loss of anaesthesiologists, it is quite possible that this demand will not be fulfilled. Reliance on European and extra-European workforces to compensate for this shortage is likely to increase, whereas the availability of these workforces is not guaranteed. Emerging solutions include an active strategy to recruit more interns, enhance intercantonal mobility and implementation of innovative solutions to provide appropriate care in the context of workforce shortages.
Acknowledgments
The study authors would like to thank Ms Suzanne Reuss and Mr Adrian Koenig for their kind and efficient help in the coordination of the study and management of questionnaires.
Guy Haller MD, MSc, PhD
Département de Médecine Aigue-Service d’Anesthésiologie
Hôpitaux Universitaires de Genève
4 rue Perret-Gentil
1211 Genève 14-Switzerland
guy.haller[at]hcuge.ch
References
1.
GBD 2015 Healthcare Access and Quality Collaborators. Electronic address: cjlm@uw.edu
GBD 2015 Healthcare Access and Quality Collaborators
. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990-2015: a novel analysis from the Global Burden of Disease Study 2015. Lancet. 2017 Jul;390(10091):231–66. https://doi.org/10.1016/S0140-6736(17)30818-8
2.
Björnberg A
,
Yung Phang A
. Euro Health Consumer Index 2018. Available at https://healthpowerhouse.com/publications/#200118 Accessed 2 February 2020).
3.
Agency for Healthcare Research and Quality R
. MD. Elements of Access to Health Care 2018 [cited December 2019]. Available from: https://www.ahrq.gov/research/findings/nhqrdr/chartbooks/access/elements.html
4.
De Pietro C
,
Camenzind P
,
Sturny I
,
Crivelli L
,
Edwards-Garavoglia S
,
Spranger A
, et al.
Switzerland: Health System Review. Health Syst Transit. 2015;17(4):1-288, xix. Epub 2016/01/15. PubMed PMID: 26766626
5.
Hübner M
,
Zingg T
,
Martin D
,
Eckert P
,
Demartines N
. Surgery for non-Covid-19 patients during the pandemic. PLoS One. 2020 Oct;15(10):e0241331. https://doi.org/10.1371/journal.pone.0241331
6. Office fédéral de la statistique. Bilan de la population résidante permanente, 1861-2018. Available at https://www.bfs.admin.ch/bfs/fr/home/statistiques/population/effectifevolution.assetdetail.9486047.html Accessed 12 February 2020
7. Office fédéral de la statistique. Les scénarios de l’évolution de la population de la Suisse 2015–2045. Available at https://www.bfs.admin.ch/bfs/fr/home/statistiques/catalogues-banques-donnees/publications.assetdetail.350327.html Accessed 12 February 2020
8.
Hänsgen K.-D.
,
Spicher B.
Numerus clausus: le «test d’aptitudes pour les études de médecine» (AMS) permet-il de trouver les personnes les plus aptes? Bulletin des médecins suisses 2002;83: Nr 47
9. Fédération des médecins suisse.Statistique Médicale de la FMH.Enquête sur la démographie médicale dans les établissements de formation IFSM. Mai 2018. Available at https://www.fmh.ch/fr/prestations/statistique/indicateurs.cfm Accessed 5 January 2020
10. Fédération des médecins suisse.Statistique Médicale de la FMH. Outil de recherche interactif. Available at https://aerztestatistik.myfmh2.fmh.ch/ Accessed 5 January 2020
11.
Kerr EA
,
Hays RD
,
Mittman BS
,
Siu AL
,
Leake B
,
Brook RH
. Primary care physicians’ satisfaction with quality of care in California capitated medical groups. JAMA. 1997 Jul;278(4):308–12. https://doi.org/10.1001/jama.1997.03550040064039
12.
Maslach C
,
Jackson SE
. The Measurement of Experienced Burnout. J Occup Behav. 1981;2(2):99-113. http://doi: DOI https://doi.org/10.1002/job.4030020205
13.
McMurray JE
,
Williams E
,
Schwartz MD
,
Douglas J
,
Van Kirk J
,
Konrad TR
, et al.; SGIM Career Satisfaction Study Group
. Physician job satisfaction : developing a model using qualitative data. J Gen Intern Med. 1997 Nov;12(11):711–4. https://doi.org/10.1046/j.1525-1497.1997.07145.x
14.
Roberfroid D
,
Leonard C
,
Stordeur S
. Physician supply forecast: better than peering in a crystal ball? Hum Resour Health. 2009;7:10. Epub 2009/02/17. http://doi: https://doi.org/1478-4491-7-10 [pii]https://doi.org/10.1186/1478-4491-7-10
15.
European Commission
. EU level Collaboration on Forecasting Health Workforce Needs, Workforce Planning and Health Workforce Trends – A Feasibility Study. http://ec.europa.eu/health/workforce/key_documents/study_2012/index_en.htm
16.
Deal CL
,
Hooker R
,
Harrington T
,
Birnbaum N
,
Hogan P
,
Bouchery E
, et al.
The United States rheumatology workforce: supply and demand, 2005-2025. Arthritis Rheum. 2007 Mar;56(3):722–9. https://doi.org/10.1002/art.22437
17.
Lagarde M
,
Cairns J
. Modelling human resources policies with Markov models: an illustration with the South African nursing labour market. Health Care Manage Sci. 2012 Sep;15(3):270–82. https://doi.org/10.1007/s10729-011-9184-5
18.
Jovic E
,
Wallace JE
,
Lemaire J
. The generation and gender shifts in medicine: an exploratory survey of internal medicine physicians. BMC Health Serv Res. 2006 May;6(1):55. https://doi.org/10.1186/1472-6963-6-55
19.
Sheahan P
. Generation Y: thriving and surviving with Generation Y at work Grant H, editor. Prahran, Victoria: Hardy Grant; 2005. 274 p.
20.
Mamie C
,
Clergue F
,
Zocatelli D
,
Haller G
. Swiss healthcare cost containment policies and their impact on anaesthetists’ density and satisfaction. Swiss Med Wkly. 2011 Oct;141:w13251. https://doi.org/10.4414/smw.2011.13251
21.
Kempthorne P
,
Morriss WW
,
Mellin-Olsen J
,
Gore-Booth J
. The WFSA Global Anesthesia Workforce Survey. Anesth Analg. 2017 Sep;125(3):981–90. https://doi.org/10.1213/ANE.0000000000002258
22. US bureau of labor statistics. Nurse anaesthetists, nurse midwives, and nurse practitionners. Available at https://www.bls.gov/ooh/healthcare/nurse-anesthetists-nurse-midwives-and-nurse-practitioners.htm. Accessed 20 February 2021.
23.
Meeusen V
,
van Zundert A
,
Hoekman J
,
Kumar C
,
Rawal N
,
Knape H
. Composition of the anaesthesia team: a European survey. Eur J Anaesthesiol. 2010 Sep;27(9):773–9. https://doi.org/10.1097/EJA.0b013e32833d925b
24.
Vonlanthen R
,
Lodge P
,
Barkun JS
,
Farges O
,
Rogiers X
,
Soreide K
, et al.
Toward a Consensus on Centralization in Surgery. Ann Surg. 2018 Nov;268(5):712–24. https://doi.org/10.1097/SLA.0000000000002965
25.
Cheneval F
,
Ferrin M.
Switzerland: A Future Model for the EuropeanUnion? Similarities and Differences. 2017. Brussel.European commission https://doi.org/https://doi.org/10.5167/uzh-136069
26.
Mullan F
. The metrics of the physician brain drain. N Engl J Med.2005;353(17):1810-8. Epub 2005/10/28.http://doi: https://doi.org/353/17/1810 [pii]https://doi.org/10.1056/NEJMsa050004. PubMed PMID: 16251537.
27.
International Organization for Migration
. Managing Labour Mobility in the Evolving Global Economy.Geneva; 2008
28.
Buchan J
. How can the migration of health professionals be managed so as to reduce any negative effects on supply.Policy Brief Series World Health Organization 2008 and World Health Organization, on behalf of the European Observatory on Health Systems and Policies 2008 Available at https://www.euro.who.int/data/assets/pdf_file/0006/75453/E93414.pdf
29.
Kirigia JM
,
Gbary AR
,
Muthuri LK
,
Nyoni J
,
Seddoh A
. The cost of health professionals' brain drain in Kenya. BMC Health Serv Res. 2006;6:89. Epub 2006/07/19. http://doi: https://doi.org/1472-6963-6-89 [pii]https://doi.org/10.1186/1472-6963-6-89
30.
Mills EJ
,
Kanters S
,
Hagopian A
,
Bansback N
,
Nachega J
,
Alberton M
, et al.
The financial cost of doctors emigrating from sub-Saharan Africa: human capital analysis. BMJ. 2011 Nov;343 nov23 3:d7031. https://doi.org/10.1136/bmj.d7031
31.
Cohen JJ
. Our compact with tomorrow’s doctors. Acad Med. 2002 Jun;77(6):475–80. https://doi.org/10.1097/00001888-200206000-00002
32.
Waurick R
,
Weber T
,
Bröking K
,
Van Aken H
. The European Working Time Directive: effect on education and clinical care. Curr Opin Anaesthesiol. 2007 Dec;20(6):576–9. https://doi.org/10.1097/ACO.0b013e3282f0ef6100001503-200712000-00016 https://doi.org/10.1097/ACO.0b013e3282f0ef61
33.
Clergue F
. Time to consider nonphysician anaesthesia providers in Europe? Eur J Anaesthesiol. 2010 Sep;27(9):761–2. https://doi.org/10.1097/EJA.0b013e32833c1bb3
34.
Lange M
,
Prien T
,
Brussel T
,
Van Aken H
. The anaesthetist makes a difference: the bottom line matters! Eur J Anaesthesiol. 2011;28(4):306; author reply -7. Epub 2010/11/23.http://doi: https://doi.org/10.1097/EJA.0b013e3283414cd2.
35. World Health Organization on behalf of the European Observatory on Health Systems and Policies. Health Professional Mobility and Health Systems.Evidence from 17 European countries Edited by Wismar M, Maier C, Glinos I, Dussault G, Figueras J. Copenhagen: WHO 2011. https://www.euro.who.int/__data/assets/pdf_file/0017/152324/Health-Professional-Mobility-Health-Systems.pdf
36.
Bloor K
,
Maynard A
. The productivity of health care. Health Econ. 2006 Dec;15(12):1257–9. https://doi.org/10.1002/hec.1183
37.
Organisation for Economic Co-Operation and Development
. OECD Health Data 2017. Available at http://www.oecd-ilibrary.org/. Accessed 5 January 2020
38.
Goodman DC
,
Fisher ES
,
Little GA
,
Stukel TA
,
Chang CH
. Are neonatal intensive care resources located according to need? Regional variation in neonatologists, beds, and low birth weight newborns. Pediatrics. 2001 Aug;108(2):426–31. https://doi.org/10.1542/peds.108.2.426
39.
Needleman J
,
Buerhaus P
,
Mattke S
,
Stewart M
,
Zelevinsky K
. Nurse-staffing levels and the quality of care in hospitals [pii]. N Engl J Med. 2002 May;346(22):1715–22. https://doi.org/10.1056/NEJMsa012247346/22/1715 https://doi.org/10.1056/NEJMsa012247
40.
Bixenstine PJ
,
Shore AD
,
Mehtsun WT
,
Ibrahim AM
,
Freischlag JA
,
Makary MA
. Catastrophic medical malpractice payouts in the United States. J Healthc Qual. 2014 Jul-Aug;36(4):43–53. https://doi.org/10.1111/jhq.12011
41.
Campbell G
,
Rollin AM
,
Smith AF
. Cases relating to anaesthetists handled by the UK General Medical Council in 2009: methodological approach and patterns of referral. Anaesthesia. 2013 May;68(5):453–60. https://doi.org/10.1111/anae.12117
42.
Staender S
,
Schaer H
,
Clergue F
,
Gerber H
,
Pasch T
,
Skarvan K
, et al.
A Swiss anaesthesiology closed claims analysis: report of events in the years 1987-2008. Eur J Anaesthesiol. 2011 Feb;28(2):85–91. https://doi.org/10.1097/EJA.0b013e3283414fea