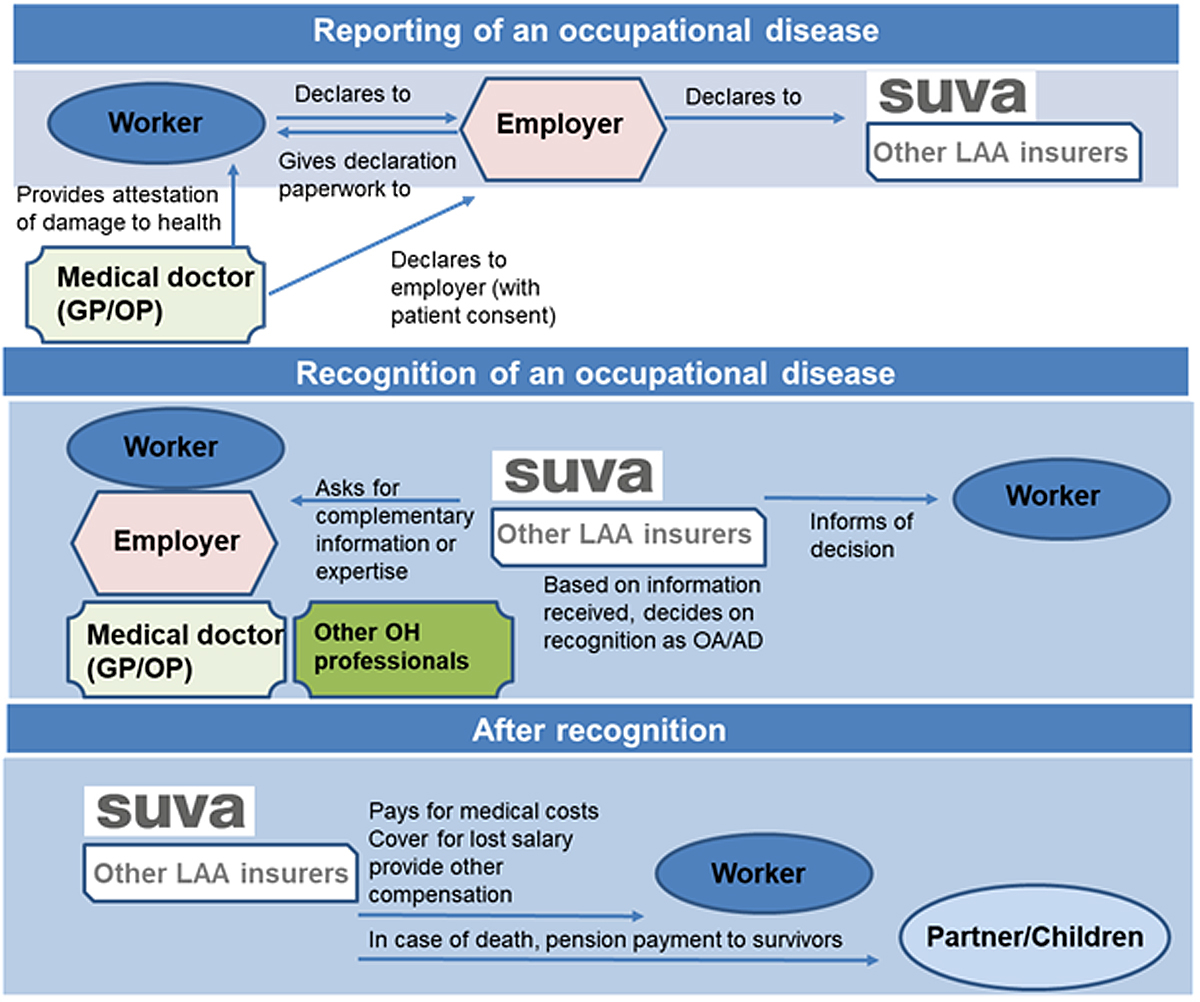
Figure 1 Reporting, recognition and compensation of an occupational disease in Switzerland. GP = general practitioner; OP = occupational physician; OH = occupational health; OA/D = occupational accident/disease.
DOI: https://doi.org/10.4414/smw.2021.20538
Occupational disease lists (ODLs) are essential legal mechanisms for recognising pathologies related to exposure to occupational hazards and assist in settling compensation [1]. There are several definitions of the term “occupational disease”, which may vary regionally and nationally. Nevertheless, the most widely accepted definition comes from the International Labour Organization (ILO) Protocol of 2002 to the Occupational Safety and Health Convention. It states that “the term ‘occupational disease’ covers any disease contracted as a result of an exposure to risk factors arising from work activity” [2]. The ILO further notes that: “Each Member should, under prescribed conditions, report diseases known to arise out of the exposure to substances and dangerous conditions in processes, trades or occupations as occupational diseases.” [3]. Switzerland is a member state of the ILO and therefore participated in the drafting of this convention which was subsequently adopted as an International Labour Standard. Regardless of ratification status, conventions provide a legal framework that is validated through its negotiation in an expert tripartite setting.
The two central elements of an occupational disease thus include: (1) the causal relationship between exposure in a specific working environment or work activity and a particular disease; and (2) the fact that the disease occurs among a group of exposed persons with a frequency above the average morbidity of the rest of the population [4]. In addition, for compensation, monitoring and prevention purposes, a third element appears to be crucial: the inclusion of scientifically defined occupational diseases into a legal framework that recognises them, generally as part of labour or social insurance law.
In 1925, the ILO developed its first official ODL, which included diseases related to exposure to anthrax, lead and mercury. Most importantly, it required ILO member states ratifying the Convention to provide compensation to affected workers [5]. Since then, the list has been regularly revised to reflect changes in working conditions and the evolution of scientific knowledge linking occupational hazards to specific diseases. In 2002, the ILO extended the purpose of the list to include prevention, recording and notification activities [6].
In Europe, the 1957 treaty stipulated that one of the tasks of the European Commission was to develop protective measures regarding occupational accidents and diseases [7]. As part of this objective, the EC produced its first schedule of occupational diseases in 1962 [8]. In 1990, the EC recommended that member states include the ODL in their regulations and introduce workers’ compensation mechanisms for diseases not included in the ODL but which can be proven occupational in nature. In 2003, the EC highlighted the need for further ODL improvements in regards to prevention and the collection of comparable data, and issued an updated ODL [9]. The EC also clarified the need for transparency in the revision process, and recommended the active participation of all stakeholders in the field of occupational health, in particular public authorities and social partners [9]. To fulfil the ODL’s aims of reporting, providing compensation and preventing the recognised occupational diseases, the processes guiding the ODL development or revision must ensure that it reflects the latest development in research and in working conditions. Therefore, the ODL should be reviewed regularly to consider new data and updated state of knowledge [10]. Particularly, the choice of diseases should be evidenced based with solid data from toxicology, exposure science and epidemiology, and guided by clinical medicine [11].
In 2018, the Swiss National Accident Insurance Fund (SUVA) registered 273,675 cases reported as occupational accidents and occupational disease [12]. Ninety-six percent of them were considered for compensation, including 255,716 occupational accidents and 4364 occupational diseases. The Swiss National Accident Insurance statistics are provided in aggregated form, the number of occupational diseases and associated cost were therefore deduced from the number of overall cases and those of occupational accidents. Importantly, while all occupational accidents were recognised as such, only 55% of occupational diseases (n = 2403) were recognised. It is crucial to note that the number of occupational diseases officially recognised likely represents only a small fraction of the overall burden of diseases related to working conditions, and occupational diseases have a significant economic, social and moral impact on working populations and society as a whole. Global burden of disease estimates have shown that the number of deaths due to occupational disease is at least six times higher than those due to occupational accidents [13]. On average, SUVA spends around CHF 140 million yearly for the recognised occupational diseases (estimate over 2014–2018) [12], but the number of occupational diseases has been constantly increasing since 2005, as do the associated costs [14]. However, these figures seem underestimated, as the number of Swiss workers suffering from work-related health problems was estimated to be 1.1 million people and the cost of occupational diseases at least CHF 20 billion per year [15]. There is currently no publicly available centralised database on workers’ exposures to occupational hazards in Switzerland, nor a national register of diseases due to occupational exposures enabling these numbers to be crosschecked [16]. The ODL has existed in Switzerland since 1982; however it has remained unchanged for the last 20 years, and hence it does not explain the increase of occupational disease observed since 2005. Notwithstanding, in 2017, Switzerland initiated the revision of its ODL and solicited stakeholders to review the proposal. This revision represented an important event and was an opportunity to assess the legal status, content and role of Swiss ODL in the reporting and recognition of occupational disease.
In this research, we examined the structure and content of the latest version of Swiss ODL, by comparing it with the official recommendations and ODLs of the ILO and EU. In addition, we addressed the effectiveness of the Swiss ODL from the occupational and public health perspectives, in considering the process of reporting and recognition of occupational disease as a measure for protecting workers’ health.
Because of the unique focus of this investigation, we instituted a mapping study, which enables the review of multifaceted characteristics of a research question [17]. Mapping focuses not only on research findings, but also on qualitative descriptors that reveal relationships and linkages between data and information flow [17]. Our mapping study consisted of iterative, critical reviews of the Swiss ODL with the ILO and EC recommendations, in which we closely and comprehensively examined the history of their development, as well as their structure and content. Furthermore, we compared the detailed content of the Swiss ODL with the latest revision of the EC ODL. We considered this comparison more relevant than that with the ILO’s ODL, as Switzerland has not ratified ILO Convention No.121, which prescribes establishing an official ODL [18]. We also conducted iterative reviews of press and media articles, as well as grey and peer-reviewed literature related to the development and implementation of ODLs.
In addition, stakeholder scoping interviews were used to collect information from relevant experts and took place between December 2018 and January 2020. For the ODL comparison, we solicited a double expertise, namely the expertise of two physicians with a background in occupational medicine and the expertise of two occupational toxicologists with a background in chemistry and occupational hygiene. The former were asked to independently assess the differences between the Swiss and EC ODLs regarding the occupational diseases included, whereas the latter compared the lists regarding occupational hazards and exposures. To evaluate the transparency of the ODL revision process conducted in Switzerland, we consulted official sources responsible for the revision, including SUVA and Swiss Federal Office of Public Health. Finally, we conducted scoping interviews with five experienced occupational physicians employed by university centres of occupational medicine or established on their own account, to evaluate their experience regarding the knowledge and usage of the Swiss ODL in their practice, and the convenience of the procedure of reporting and recognition of occupational disease in Switzerland.
The Swiss ODL is an annex to the Ordinance of Accident Insurance (OLAA) [19]. Under article 9.1 of the Federal Law on Accident Insurance (LAA), occupational diseases listed in annex 1 are recognised as such if they are exclusively or predominantly due to the exercise of professional activity, or exposure to certain harmful work situations. Exclusive or predominant causation means that the disease is caused by working conditions by 50% at least, or that the relative risk is equal or superior to 2. The Swiss ODL has two parts: the first enumerates exposures to specific occupational hazards; the second identifies specific diseases and links them to types of work / work environment (table 1). Article 9.2 of the LAA provides the possibility for diseases not included in the list to be recognised as occupational. However, the causation threshold is higher: such diseases must be proven to be caused exclusively or in a predominantly preponderant way by the exercise of a professional activity. Exclusive or predominantly preponderant causation implies that the disease is caused by working conditions by 75% at least, or that relative risk is equal or superior to 4. Notably, the Swiss ODL does not contain any type of psychological or mental disorder.
Table 1 Comparative assessment of the Swiss, ILO and EC occupational disease lists.
| Place and date of the 1st ODL | Revision dates | Structure and content description |
| Switzerland, 1982 |
1997, 2017 |
Part 1: 127 substances. Part 2: 38 diseases or group of diseases (13 due to physical agents; 25 due to other causes) plus an open clause*
No causative links between substances and diseases explicitly mentioned. |
| ILO, 1925 | 1934, 1964, 1980, 2002, 2010 | Part 1: Diseases caused by exposure to agents arising from work activities (chemical agents: 40 plus catch-all clause†; physical agents: 6 plus catch-all clause; biological agents, infectious or parasitic diseases: 8 plus catch-all clause). Part 2: Diseases by target organ systems (respiratory diseases: 11 plus catch-all clause; skin diseases: 3 plus catch-all clause; musculoskeletal disorders: 7 plus catch-all clause; mental and behavioural disorders: 1 plus catch-all clause). Part 3: Occupational cancers caused by agents (20 plus catch-all clause); Part 4: Other diseases (1 plus catch-all clause). |
| EC, 1962 | 1990, 2003 | Part 1: Diseases caused by chemical agents (54 diseases). Part 2: Skin diseases and skin cancers caused by substances and agents (9 diseases and occupational skin ailments caused by allergenic or irritant substances). Part 3: Diseases caused by the inhalation of substances and agents not included under other headings (19 diseases). Part 4: Infectious and parasitic diseases (7 diseases). Part 5: Diseases caused by physical agents (18 diseases). |
EC = European Commission; ILO = International Labour Organization; ODL = occupational disease list * Open clause or complementary clause: legal regulation allowing for recognition of diseases as or similar to an occupational disease but not included in the list. † Catch-all clause allows for the recognition of occupational disease not contained in the list if a link is established between exposure to risk factors arising from work activities and the disorders contracted by the worker.
The 2010 update of the ILO ODL contains four types of diseases, from those caused by biological chemical and physical agents to musculoskeletal disorders, mental and behavioural disorders, and occupational cancers (table 1). Moreover, all parts contain an open clause, enabling the recognition of the occupational origin of pathologies not explicitly listed, if a presumable link can be established between occupational exposure and resulting health outcome. Four specific criteria are provided for which diseases can be included in the ODL: (1) a causal relationship with a specific agent, exposure or work process; (2) disease occurrence in connection with a specific work environment and/or in specific occupations; (3) disease occurrence among the groups of workers concerned with a frequency that exceeds the average incidence within the rest of the population; and (4) scientific evidence of a clearly defined pattern of disease following exposure and plausibility of cause. All four criteria have to be met for an occupational disease recognition. The ILO ODL was developed in tripartite consultation with workers’ organisations, employers’ organisations and governments, and as such, represents the collective, and agreed upon, viewpoints of stakeholders from the world of work. Its main objective is to serve as a verified international model for the establishment, review and revision of national lists of occupational diseases.
The last version of the EC ODL is divided into five parts and includes infectious and parasitic diseases and diseases caused by physical agents, the latter mostly encompassing musculoskeletal disorders. It emphasises the need for accurate and detailed reporting of epidemiological data of occupational diseases, for reinforcement of preventive measures and for the wide dissemination of documents to assist in the diagnosis of occupational diseases. In 2009, the European Agency for Safety and Health at Work (EU-OSHA) developed the technical report “Information notices on occupational diseases: a guide to diagnosis”, which includes key criteria for diagnosing an occupational diseases for each of the entries of the European Schedule of Occupational Diseases [20]. The diseases are divided in five main sub-headings: (1) diseases caused by chemical agents; (2) skin diseases caused by substances and agents not included under other headings; (3) diseases caused by the inhalation of substances and agents not included under other headings; (4) infectious and parasitic diseases; and (5) diseases caused by physical agents.
Compared with the 2003 EC ODL, the Swiss ODL is not significantly less comprehensive, and there are no major differences between the two instruments. The Swiss ODL contains more individual chemical agents than the EC ODL; however, this is due to the fact that the EC ODL includes entire families of chemicals that encompass the individual agents contained in the Swiss list. When it comes to specific diseases, the majority of the diseases listed in the EC list have equivalent entries in the Swiss list. A few Swiss ODL items have no equivalent in the EC ODL, including blisters, calluses and abrasions; frostbite; sunburn, sunstroke and heatstroke; and illnesses due to ultra- and infrasound. However, there are also instances where the Swiss ODL encompasses a wider range of diseases than the EC ODL, for example all diseases due to non-ionising radiation. Both lists would benefit from the inclusion or expansion of certain diseases, namely chronic obstructive pulmonary disease (COPD) and back pain. The Swiss ODL does not include COPD, and the EC ODL lists COPD exclusively in the context of coal mining. Furthermore, both the EC ODL and Swiss ODL do not mention back pain, even though 26% of back pain cases are attributed to occupational factors [21, 22].
The 2017 revision was welcomed by occupational health stakeholders, but the proposed additions were limited, marking a missed opportunity for a wider discussion on the changes that have affected working lives in Switzerland since the 1997 revision, as well as on the equity of the Swiss occupational disease recognition system. In particular, reflections on how usable the occupational disease list is, and on how the high burden of proof demanded by the LAA may impact recognition rates and consequently the health and life of affected workers were also missing from the process.
As discussed, although the Swiss ODL itself is fairly comprehensive, evidence has shown that a number of occupational diseases, even when they are in the list, are likely not recognised as such, for example musculoskeletal disorders and cancers [23, 24]. Further, clear and transparent information about the revision process of Annex 1 itself is lacking. The federal administration contacted a number of stakeholders for comments regarding the proposed amendments, but they were invited to give their opinion only after the amendments were drafted, and they were not part of the discussions on what the additions to the list should be. This consultation process is well documented and official documents are available for consultation on the Swiss confederation website [25], but publicly accessible information on the process that led to the proposed amendments is not provided. Additionally, although the concerns and suggested amendments sent by some of the stakeholders consulted have been duly documented, there is no information on how the results of the consultation have been taken into account, if at all.
Whatever the disease or health condition assumed to be occupational, the physician, usually a general practitioner (GP) or family doctor, is required to document its link with a specific occupational exposure. This includes reviewing the patient’s occupational history and specifying the occupation, the working conditions (tasks, postures, products handled) that trigger or worsen the symptomatology, their chronology and the latency between the first exposure and the onset of symptoms. In the case of doubt regarding an occupational origin of the disease, the physician can contact the company occupational physician, if available, or a university occupational health centre in order to support the patient and the LAA insurer in the in-depth investigations and occupational disease report. Otherwise, the physician advises the patient directly to make an occupational disease report. The worker must report the occupational disease as soon as possible to his employer. The employer must then report it to his LAA insurer as soon as his employee announces it. Figure 1 summarises the process of the occupational disease reporting, recognition and compensation in Switzerland. An occupational disease report should include the following elements: (1) the disease should be characterised according to the art. 3 of the Federal law on the general part of social insurance law (LPGA); (2) the patient must be insured by the LAA; (3) the company, the insured person, his/her beneficiary or physician must make a report to the LAA insurer; and (4) the causal criteria must be met. Causality is always examined on a case-by-case basis, taking into account the results of medical examinations, symptom chronology, present and past working conditions, exposure levels and duration, latency between exposure and disease, individual factors that could explain the occurrence of the disease, and scientific data, particularly epidemiological evidence concerning the disease. The latter is essential, as it depends on the exhaustiveness of the literature search and the quality of evidence appraisal including a thorough assessment of the risk of bias, particularly in negative epidemiological studies, which is a difficult and time-consuming task. Therefore, the quality of the occupational disease report matters, as its elements could significantly help the LAA insurance physician to deal with the case assessment to decide upon the recognition of an occupational origin of the disease, allowing compensation for the health damage. In the case of refusal of occupational disease recognition, the insured patient may appeal this decision within 30 days.
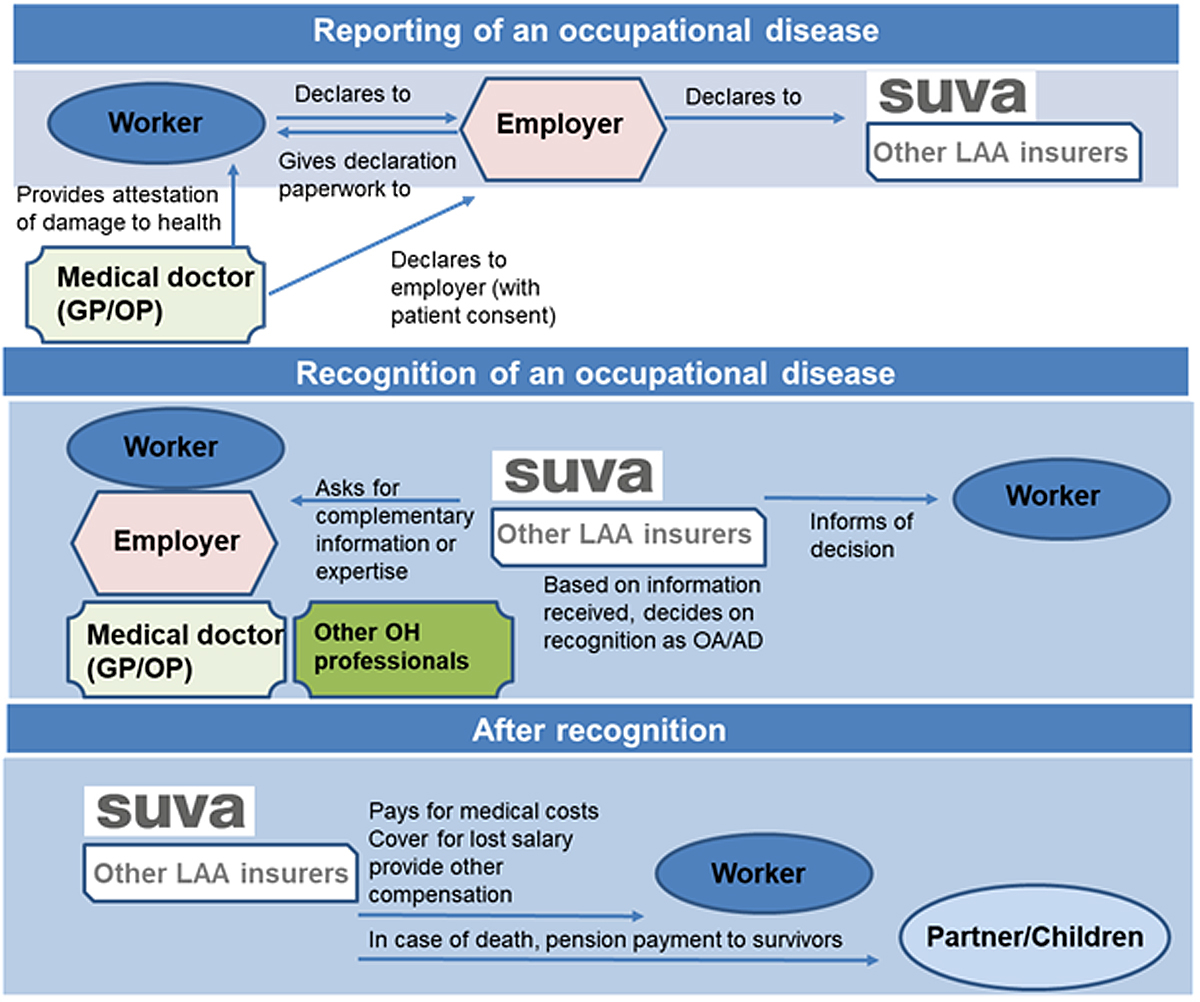
Figure 1 Reporting, recognition and compensation of an occupational disease in Switzerland. GP = general practitioner; OP = occupational physician; OH = occupational health; OA/D = occupational accident/disease.
The interviews with physicians identified several barriers and flows in the current procedure of the occupational disease declaration (table 2). Regarding the ODL itself, they mentioned its complex structure, the fact that the two parts of the Swiss ODL are not complementary and do not match exposures to diseases. This leads to challenges in causative links and limits its usability, notably for physicians not specialised in occupational medicine [11].
Table 2 Challenges pointed out by physicians regarding the occupational disease reporting procedure.
| General lack of training and information on occupational risk factors |
| Lack of knowledge among workers on occupational risk factors and their rights |
| Worker’s fears regarding potential repercussion of occupational disease reporting on his/her employment |
| Complexity of administrative procedure and the absence of clear criteria for occupational disease recognition, discouraging both patients and physicians from make a report |
| Non-recognition of certain multifactorial diseases, in which investigations were stopped on the pretext of individual risk factors |
| Long-latency pathologies, such as cancers, often diagnosed after termination of work when the relationship between the exposure and disease is more difficult to make |
| Insufficient resources for case investigations by occupational physicians, given that the professional path establishment over the entire career, supported with toxicological/occupational hygiene analysis, is time-consuming, costly and not self-financed because of no TarMed pricing in this specialty |
| Limited resources for research on occupational health and surveillance of occupational exposures. These flows can have repercussions in terms of insufficient declaration and recognition of occupational disease, resulting in their underreporting and lack of preventive effort. |
The Swiss ODL shares a great part of its contents with the EC and ILO ODLs, and there does not seem to be any critical disease category missing from it when compared with these two instruments. Despite this, there is a common concern amongst Swiss occupational physicians and other occupational health professionals that the burden of occupational disease is greatly underestimated in Switzerland [24, 26]. This underestimation is not unique to Switzerland and is documented in most European countries [27, 28]. The causes for underreporting are numerous and some are in common with those cited by Swiss physicians (see table 2), including the lack of occupational health training amongst GPs; their difficulties in making the link between certain pathologies, in particular cancers, having multifactorial causes as well as long latencies, and the patient’s profession; dearth of information on occupational health and risks among workers; workers’ fear of losing their job; and complexity and duration of the procedure, with difficulties in providing proof of exposure [28, 29].
However, the scale of underreporting is difficult to evaluate in Switzerland as no comprehensive research has been conducted on this particular topic. Moreover, the annual insurance statistics are usually reported in a very aggregated form, which makes it difficult to disentangle the numbers of specific occupational diseases, such as cancer of a specific location or type from all cancers, or some particular respiratory diseases such as COPD from all respiratory diseases. Even the comprehensive 5-year report is not detailed enough for analysis of the underreporting concern [14, 30]. Nevertheless, some European surveys provide information on the situation in Switzerland [31]. The number of applications for recognition of an occupational disease was 125 per 100,000 insured workers in 2006; by comparison, the rate was 625 for Denmark, 401 in France, and 349 in Sweden. Interestingly, the level of application was lower in Austria (n = 42), Germany (n = 40), Italy (n = 38) and Luxembourg (n = 25) [31]. In the same year, the rate of occupational diseases recognised per 100,000 insured workers was relatively high in Switzerland (n = 103) but considerably lower than France (n = 282), Sweden (n = 267) and Spain (n = 141) [31]. One of the main factors affecting rates of recognition may depend on whether musculoskeletal disorders are more widely recognised; this is true for France, Spain and Sweden [31]. Besides, before 2006 in Switzerland, the rate of recognised occupational diseases may have been overestimated as possible infectious diseases were included in the statistics [31]. In fact, any occupational exposure to an infectious disease followed by prophylactic treatment was declared, recognised and counted as an occupational disease. In 2006, infectious diseases in Switzerland thus accounted for 20% of recognised cases of occupational disease. Since 2006, the method of counting infectious diseases has changed and they are counted in a separate category. The rate for recognised occupational diseases excluding infectious diseases is therefore 40% lower than the rates reported before 2006 [13].
The reason for this low rate is linked to all the reasons previously cited, but particularly to the level of proof that must be demonstrated for each reported case. In Switzerland, the legal requirements for demonstrating the burden of proof or aetiological fraction are particularly strict (i.e., if the disease is included in the list, 50% or relative risk = 2, if outside the list, 75% and relative risk = 4). Moreover, the responsibility of providing proof indicating a causal link is the responsibility of the worker. In this process, the insurance body takes into account all exposure factors and therefore may limit the recognition of the disease for multifactorial causes. The situation is particularly so for diseases with multifactorial origins, such as musculoskeletal disorders and cancers [32, 33].
In 2016, EUROGIP published a study on the recognition of musculoskeletal disorders as occupational diseases in 10 European countries including Switzerland [34]. The content of the list was similar for all countries; the only significant difference was that vertebral and spinal damage are not recognised in Austria, Finland and Switzerland. In Belgium and Denmark, when clinical and exposure criteria were present, the case was generally recognised; in Spain, France and Italy, if there is a presumption of occupational origin, recognition is almost automatically granted.
Regarding reported musculoskeletal disorders, large differences exist between countries: France, Belgium and Denmark had a high ratio of 463, 263 and 257 cases per 100,000 insured workers, respectively, in 2014, whereas Switzerland had the lowest ratio (13 per 100,000 insured workers). When recognised cases of musculoskeletal disorders are considered, many differences remain: France had the highest ratio (322 per 100,000 insured workers), followed by Spain (94), Belgium (82) and Italy (64); and Switzerland had the lowest ratio (6 per 100,000 insured workers). The likely explanation for this very low ratio in Switzerland is two-fold: vertebral and spinal damage are not included in the list of occupational diseases and each case is examined on its own merit with no presumption of causality and a high burden of proof (relative risk = 4) to establish causality.
A cancer is defined as occupational when it results from the worker’s exposure to occupational carcinogens. Occupational carcinogens (chemical, physical or biological) are well documented; the Swiss ODL enumerates them quite exhaustively and does not have any significant omissions. Research studies on the proportion of cancers attributable to occupational carcinogens estimate that between 4% and 8.5% of cancers are of occupational origin; however, the proportions may vary significantly depending on the cancer localisation [22, 35]. For example, recent published data estimated that in France, around 15% of new lung cancers in 2015 can be attributed to occupational exposures [36]. In Switzerland, of 2435 new cases of lung cancer diagnosed in men, only 0.3% (seven cases) were recognised as occupational disease [24], suggesting a significant underestimation of the number of occupational cancers [37]. This underreporting and the rate of recognition of occupational cancers vary from one country to another. However, in 2016, Switzerland had a ratio of recognised occupational cancers of 4.41 per 100,000 insured workers, far behind Germany (15.1) and France (11.39) [38]. In addition, Switzerland recognises very few types of cancer. In 2016, 154 out of 173 recognised cancer cases were pleural mesothelioma and one lung cancer linked to exposure to asbestos (87%) [38]. It is worth highlighting that for several decades, lung cancers were not recognised as occupational in workers with a history of asbestos exposure if they were smokers. This has changed recently, when SUVA updated its recognition criteria in accordance with the Helsinki criteria for diagnosis and attribution of asbestos-related diseases [39, 40]. Even so, the SUVA conditions do not meet the 2014 update of Helsinki criteria [41], recommending the threshold relative risk no greater than 2 for individual attribution of asbestos-related diseases, and do not recognise laryngeal and ovarian cancers as diseases caused by asbestos. This is in contradiction to the Helsinki criteria, which state that their causal evidence is sufficient and that they should viewed as asbestos-related even if the estimated relative risk for laryngeal cancer is 1.6 and that for ovarian cancer is 2.2 [41]. It is remarkable that the Helsinki criteria update has been also criticised for insufficiently diagnosing all asbestos-related diseases, namely non-cancer respiratory diseases, and the resulting underreporting and underrecognition of occupational disease [29, 42]. This information deserves attention and communication among physicians to encourage the reporting of all occupational asbestos-related cancers as such.
The challenges illustrated in the case of the recognition of musculoskeletal disorders and cancer as occupational are more salient in Switzerland, where the recognition decision is based on a relative risk on a population level. Such systems are essentially different from systems based on individual-case recognition, accepting occupational disease cases based on criteria of exposure and of disease, as in Belgium or Spain [43].
In order to more thoroughly address traditional hazards and protect workers from emerging work-related risks, change is needed to improve the legal framework for the protection of workers’ health and safety in Switzerland. However, for change to be substantive and sustainable, it must take on a comprehensive, multi-level approach, spanning from the level of national policy to the physician level.
Several studies have aimed to investigate the success of interventions for enhancing occupational safety and health systems and increasing the reporting of occupational diseases, highlighting the importance of a multifaceted and comprehensive system, specifically designed for the unique characteristics of the county and its workforce [44–47]. Moreover, it has been clearly indicated that multilevel efforts to increase the effective assessment of occupational diseases and compliance in reporting activities enhance the usability of incidence figures for the government, employers and workers alike [48].
Spreeuwers et al. developed quality indicators and criteria to evaluate registries for occupational diseases on their ability to provide appropriate information for preventive policies on a national level [49]. Together, these indicators form a tool, which can be used for quality improvement of occupational disease registries and to continually monitor the situation at the national level, and therefore could be applied in Switzerland. Nevertheless, despite the evidence for improving action at the national and physician level (discussed below), it has been recommended that future studies should investigate the effects of large-scale interventions such as legislation, existing or new disease-specific registries, newly established occupational health services, or specific surveillance systems [45].
At the national level, a more comprehensive policy structure for occupational safety and health is necessary to protect workers across various sectors and industries in Switzerland. First, health information management must be strengthened across the board, including the development of clearly established occupational health indicators. According to the Organization for Economic Cooperation and Development (OECD), Switzerland ranks second to last in terms of availability and use of such indicators [50]. The OECD revealed that there is a lack of connections between different institutions and organisations relating to health research, statistical analysis and monitoring issues: only 14% of datasets are regularly linked for research, statistics and/or monitoring purposes [50].
Except for radiation exposure, there is no centralised database on workers’ exposures to workplace hazards or a national register of chronic effects due to occupational exposures. Conversely, Finland maintains six different registers or databases on exposures for surveillance, hazard control, epidemiology and risk assessment purposes [51]. This paucity of data in Switzerland hampers the design and implementation of epidemiological research on occupational health, and the evaluation of prevention efforts [16]. Even more importantly, inadequate surveillance systems, including lack of a sentinel system for occupational diseases, hinders efforts to foresee and identify emerging risks in the workplace [43]. SUVA is the only institution that can legally recognise the occupational nature of a disease. SUVA simultaneously manages the occupational disease compensation fund, though ILO Convention No. 121 prescribes that these two functions should be independent. (NB: Switzerland has not ratified this convention.)
In addition, it would be useful to follow recent guidance that recommends the national implementation of several different types of sentinel and alert systems, in order to monitor multifaceted aspects of occupational diseases, especially (but not only) for new or emerging diseases [44]. These act as early warning mechanisms to detect new types or combinations of exposure scenarios or health effects at an earlier stage to prevent occupational diseases before they become a burden to workers and society. A comprehensive alert or sentinel system can be seen as a chain of information and communication systems, made up of signal detection, workplace evaluation, signal strengthening and timely alerting of stakeholders, which provides time to respond to and minimise the impact of a potential occupational health threat. In addition to the compensation-related system with an “open list” approach, as is currently in place in Switzerland, a comprehensive and integrated system as described above would allow for a shift towards a much needed preventative approach and at the same time provide useful information to complement official figures on occupational diseases [52].
It is essential to note that national policy measures should include provisions for active surveillance systems that apply a “framework approach” and also extend to the enterprise level, including preventative practical measures for workers on the shop floor. Comprehensive occupational safety and health systems, as outlined in the ILO’s Convention No. 187, highlight that integrated action at the national and enterprise level is essential for developing a preventative safety and health culture [53].
Standardised and reliable data on incidence and prevalence of occupational health effects from a broad range of medical institutions is critical for the development of a comprehensive ODL, as well as broader frameworks for prevention. However, Swiss physicians, including GPs, often do not collect their patients’ occupation or report it in a non-standardised way [54, 55]. Any revision of the ODL must simultaneously promote the strengthening of medical reporting efforts through increased awareness among GPs. Targeted continuing education should focus on occupational health indicators in order to help GPs to better recognise effects from occupational exposures, and to emphasise the importance of referrals to occupational physicians when in doubt. As occupational history is often the most sensitive and specific indicator of occupational exposure in the case report of an occupational disease, it should be taken by an experienced physician and supplemented if necessary by an exposure assessment conducted by an experienced industrial hygienist. The importance of incorporating occupational and environmental health into the primary care curriculum and practice has been recognised in other countries [56] and should be foreseen in Switzerland.
Chiarini et al. showed that awareness of Swiss physicians of occupational exposures varies greatly depending on their specialty [57]. Only 18% of physicians (all specialties combined) have consulted an occupational physician when confronted with a potential occupational pathology and 38% never contacted the employer of a patient whose pathology was mainly due to work. Almost half of the responding physicians (47%) said they have never reported an occupational disease to accident insurance. Among them, only 8% would know how to go about it if that proved necessary [57]. These results demonstrate the need to strengthen the awareness of Swiss doctors on the problem of the occupational disease reporting and recognition, especially during initial and continuing medical training and in the specialties most concerned. Spreeuwers et al. have noted that, in addition to enhanced monitoring and alert systems at the national level, there is an urgent need to improve the education and participation of notifying physicians when it comes to occupational health knowledge and the protocol for diagnosis and reporting of occupational diseases [46]. Furthermore, a sentinel surveillance project that followed a group of 45 occupational physicians for 2 years found that a surveillance group comprising motivated and guided occupational physicians reported a substantially higher incidence of occupational diseases and a lower proportion of incorrect notifications than a national registry [47]. Moreover, Smits et al. reported that relatively simple actions such as an active, multifaceted workshop on occupational disease is effective in increasing the number of physicians reporting occupational diseases. Self-efficacy measures were shown to be a predictive factor for such reporting [58]. Results from these and other studies highlight the importance of enhanced occupational physician training, education and information towards the amelioration of occupational disease reporting systems [47].
In addition to actions specifically at the physician level, it is also important to enhance the training and education of additional occupational safety and health experts such as researchers and hygienists, as well as occupational disease experts working in clinical departments (e.g., respiratory, dermatology, psychology/psychiatry, orthopaedics, oncology, cardiovascular diseases, rehabilitation, etc.). Increased attention is also needed for training and education on the specific differences between recognition of occupational disease (mostly legally based) and work-related diseases.
This investigation provided evidence that the Swiss ODL, revised in 2017, is globally in good compliance with the EC and ILO lists. However, its role as a legal mechanism of workers’ protection is not optimal. Its effectiveness seems to be limited by the conditions for recognising a listed disease as occupational, which are determined by the Swiss federal law and are stricter than in other countries. Moreover, this law confers both the legal recognition of the occupational nature of a disease, and the management of the occupational disease compensation fund on the same institution. This situation is in contradiction with ILO Convention No. 121, which prescribes that the two functions should be independent. Finally, the Swiss list has a complex structure, which makes its use in general medical practice difficult, and hampers case reporting and therefore the recognition of occupational disease. The overall burden of occupational diseases has a significant economic, social and moral impact on working populations, their families and society as a whole. As such, more transparency with respect to the revision of ODL, occupational disease recognition conditions, and data on reported and recognised cases, along with continuous education of physicians, is needed to enhance the effectiveness of the Swiss system of reporting and recognising occupational disease, towards the greater goal of a safer and healthier working population in Switzerland.
The authors would like to thank Drs. Nancy B. Hopf and Jean Jacques Sauvain for their assistance in review of the EU and Swiss ODLs, the five physicians interviewed in this study, and the three institutional physicians who kindly agreed to review this mansucript.
This study was conducted with professorial allocation to Prof. Guseva Canu from the University of Lausanne.
The authors declare no conflict of interest related to this research or manuscript.
1 Kim EA , Kang SK . Historical review of the List of Occupational Diseases recommended by the International Labour organization (ILO). Ann Occup Environ Med. 2013;25(1):14–24. doi:.https://doi.org/10.1186/2052-4374-25-14
2ILO. P155 - Protocol of 2002 to the Occupational Safety and Health Convention, 1981, Art. 1b.
3ILO. R121 - Employment Injury Benefits Recommendation, 1964 (No. 121), Art.6 (1).
4ILO. Identification and recognition of occupational diseases: Criteria for incorporating diseases in the ILO list of occupational diseases. Geneva; 2009.
5ILO. C018 - Workmen's Compensation (Occupational Diseases) Convention 1925 (No. 18).
6ILO. R194 - List of Occupational Diseases Recommendation, 2002 (No. 194), Art. 2.
7EC. Treaty establishing the European Community - Title VIII: Social policy, Education, Vocational training and Youth - Chapter 1: Social Provisions - Article 118. OJ C 224. 1957:P. 0046.
8EC. Commission Recommendation to Member States concerning the adoption of a European List of occupational diseases. OJ 80. 1962: pp. 2188–98.
9EC. Commission Recommendation of 19 September 2003 concerning the European schedule of occupational diseases OJ L 238. 2003: pp. 28–34.
10ILO. R194 - List of Occupational Diseases Recommendation, 2002 (No. 194).
11Driscoll T, Wagstaffe M, Pierce N. Developing a List of Compensable Occupational Diseases: Principles and Issues. The Open Occupational Health and Safety Journal. 2011.
12SUVA. Statistique des accidents LAA 2020. Lucerne: SUVA; 2020. Report No.: 2386.f – 2020.
13Global trends on occupational accidents and diseases [press release]. Geneva; 2015.
14SUVA. Statistique des accidents LAA 2008–2012. Dix-neuvième période quinquennale d’observation de la Suva et cinquième période quinquennale d’observation de tous les assureurs LAA. Lucerne: SUVA; 2014. Report No.: 1946/19.f.
15Laubli T. Les couts de la santé générés par de fortes contraintes au travail. Analyse des données de l’enquête européenne sur les conditions de travail et la santé des travailleurs suisses. Executive Summary. Bern, Switzerland: Secrétariat d’Etat à l’économie SECO; 2014.
16 Guseva Canu I , François M , Graczyk H , Vernez D . Healthy worker, healthy citizen: the place of occupational health within public health research in Switzerland. Int J Public Health. 2020;65(1):111–20. doi:.https://doi.org/10.1007/s00038-019-01245-w
17 Cooper ID . What is a “mapping study?”. J Med Libr Assoc. 2016;104(1):76–8. doi:.https://doi.org/10.3163/1536-5050.104.1.013
18ILO. Employment Injury Benefits Convention, 1964 [Schedule I amended in 1980] (No. 121).
19Conseil fédéral. Ordonnance sur l’assurance-accidents (OLAA), du 20 décembre 1982 (État le 1er avril 2018) (RS 832.202). Portail du gouvernement suisse1982 [updated 2018 April 1]. Available from: https://www.admin.ch/opc/fr/classified-compilation/19820361/index.html.
20EC. Information notices on occupational diseases a guide to diagnosis. Luxembourg: Office for Official Publications of the European Communities: Directorate-General for Employment, Social Affairs and Inclusion (European Commission); 2009.
21 Driscoll T , Jacklyn G , Orchard J , Passmore E , Vos T , Freedman G , et al. The global burden of occupationally related low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(6):975–81. doi:.https://doi.org/10.1136/annrheumdis-2013-204631
22 GBD 2016 Occupational Risk Factors Collaborators. Global and regional burden of disease and injury in 2016 arising from occupational exposures: a systematic analysis for the Global Burden of Disease Study 2016. Occup Environ Med. 2020;77(3):133–41. doi:.https://doi.org/10.1136/oemed-2019-106008
23Danuser B. Comment soigner la santé au travail? REISO Revue d'information sociale. Published online 2014 June 23. https://www.reiso.org/articles/themes/travail/277-comment-soigner-la-sante-au-travail
24 Chouanière D , Praz-Christinaz S-M , Danuser B . Mieux connaître la médecine du travail. Rev Med Suisse. 2009.
25Conseil fédéral. Modification de l’annexe 1 de l’ordonnance sur l’assurance-accidents (OLAA). Adaptation de la liste des maladies professionnelles figurant à l’annexe 1 OLAA aux dernières connaissances scientifiques et techniques sur les substances nocives et les effets mécaniques pour la santé. Portail du Gouvernement suisse. Procédures de consultation terminées. RS 832.202:1.
26Guillemin M. Santé au travail: le déni des politiques publiques. REISO Revue d'information sociale. Published online 2018 August 16. https://www.reiso.org/document/3326.
27EUROGIP. Enquête sur la sous-déclaration des maladies professionnelles en Europe. Paris: EUROGIP; 2002.
28EUROGIP. Reporting of occupational diseases: issues and good practices in five European countries. Paris: EUROGIP; 2015.
29 Baur X , Woitowitz HJ , Budnik LT , Egilman D , Oliver C , Frank A , et al. Asbestos, asbestosis, and cancer: The Helsinki criteria for diagnosis and attribution. Critical need for revision of the 2014 update. Am J Ind Med. 2017;60(5):411–21. doi:.https://doi.org/10.1002/ajim.22709
30Groupe de coordination des statistiques de l’assurance-accidents LAA (CSAA). Statistique des accidents LAA 2019. Lucerne: SUVA; 2019.
31EUROGIP. Les maladies professionnelles en Europe – Statistiques 1990-2006 et actualité juridique. Paris: EUROGIP; 2009.
32 Probst I . La dimension de genre dans la reconnaissance des TMS comme maladies professionnelles [The gender dimension in the recognition of MSDs as occupational diseases]. Pistes. 2009;11(11-2):2. doi:.https://doi.org/10.4000/pistes.2395
33 Probst I , Salerno S . Biais de genre dans la reconnaissance des maladies professionnelles: l’exemple des troubles musculosquelettiques (TMS) en Italie et en Suisse [Gender Bias in the Recognition of Occupational Diseases: The Case of Musculoskeletal Disorders in Italy and Switzerland]. Pistes. 2016;18(18-2):2. doi:.https://doi.org/10.4000/pistes.4889
34EUROGIP. Musculoskeletal disorders: What recognition as occupational diseases? A study on 10 European countries. Paris: EUROGIP; 2016.
35 Marant Micallef C , Shield KD , Baldi I , Charbotel B , Fervers B , Gilg Soit Ilg A , et al. Occupational exposures and cancer: a review of agents and relative risk estimates. Occup Environ Med. 2018;75(8):604–14. doi:.https://doi.org/10.1136/oemed-2017-104858
36 Marant Micallef C , Shield KD , Vignat J , Baldi I , Charbotel B , Fervers B , et al. Cancers in France in 2015 attributable to occupational exposures. Int J Hyg Environ Health. 2019;222(1):22–9. doi:.https://doi.org/10.1016/j.ijheh.2018.07.015
37 Bovio N , Richardson DB , Guseva Canu I . Sex-specific risks and trends in lung cancer mortality across occupations and economic activities in Switzerland (1990-2014). Occup Environ Med. 2020;77(8):540–8. doi:.https://doi.org/10.1136/oemed-2019-106356
38EUROGIP. Incidence and detection of occupational cancers in nine European countries. Paris: EUROGIP; 2018.
39 Tossavainen A . Asbestos, asbestosis, and cancer: the Helsinki criteria for diagnosis and attribution. Scand J Work Environ Health. 1997;23(4):311–6. doi:.https://doi.org/10.5271/sjweh.226
40Jost M, Stöhr S, Pletscher C, Rast H. Maladies professionnelles causées par l’amiante. Factsheet SUVA Division médicale. 2013:1–22.
41 Wolff H , Vehmas T , Oksa P , Rantanen J , Vainio H . Asbestos, asbestosis, and cancer, the Helsinki criteria for diagnosis and attribution 2014: recommendations. Scand J Work Environ Health. 2015;41(1):5–15. doi:.https://doi.org/10.5271/sjweh.3462
42 Collegium Ramazzini. Collegium Ramazzini response to ‘Asbestos, asbestosis, and cancer, the Helsinki criteria for diagnosis and attribution 2014: recommendations’. Scand J Work Environ Health. 2016;42(1):91–4. doi:.https://doi.org/10.5271/sjweh.3535
43 Carder M , Bensefa-Colas L , Mattioli S , Noone P , Stikova E , Valenty M , et al. A review of occupational disease surveillance systems in Modernet countries. Occup Med (Lond). 2015;65(8):615–25. doi:.https://doi.org/10.1093/occmed/kqv081
44EU-OSHA. Methodologies to identify work-related diseases: Review of sentinel and alert approaches. Luxembourg: European Agency for Safety and Health at Work; 2017.
45 Curti S , Sauni R , Spreeuwers D , De Schryver A , Valenty M , Rivière S , et al. Interventions to increase the reporting of occupational diseases by physicians: a Cochrane systematic review. Occup Environ Med. 2016;73(5):353–4. doi:.https://doi.org/10.1136/oemed-2015-103209
46 Spreeuwers D , de Boer AG , Verbeek JH , van Dijk FJ . Evaluation of occupational disease surveillance in six EU countries. Occup Med (Lond). 2010;60(7):509–16. doi:.https://doi.org/10.1093/occmed/kqq133
47 Spreeuwers D , de Boer AG , Verbeek JH , de Wilde NS , Braam I , Willemse Y , et al. Sentinel surveillance of occupational diseases: a quality improvement project. Am J Ind Med. 2008;51(11):834–42. doi:.https://doi.org/10.1002/ajim.20608
48 van der Molen HF , Kuijer PP , Smits PB , Schop A , Moeijes F , Spreeuwers D , et al. Annual incidence of occupational diseases in economic sectors in The Netherlands. Occup Environ Med. 2012;69(7):519–21. doi:.https://doi.org/10.1136/oemed-2011-100326
49 Spreeuwers D , de Boer AG , Verbeek JH , van Dijk FJ . Characteristics of national registries for occupational diseases: international development and validation of an audit tool (ODIT). BMC Health Serv Res. 2009;9(1):194. doi:.https://doi.org/10.1186/1472-6963-9-194
50OECD. Health Data Governance: Privacy, Monitoring and Research. Paris: OECD; 2015.
51 Kauppinen T . Finnish occupational exposure databases. Appl Occup Environ Hyg. 2001;16(2):154–8. doi:.https://doi.org/10.1080/104732201460253
52EU-OSHA. Alert and sentinel approaches for the identification of work-related diseases in the EU. Luxembourg: European Agency for Safety and Health at Work; 2018.
53ILO. Promotional Framework for Occupational Safety and Health Convention 187 (2006).
54 Graczyk H , Hopf NB , Mediouni Z , Guseva-Canu I , Sanvido O , Schmid K , et al. Occupational exposure to plant protection products and health effects in Switzerland: what do we know and what do we need to do? Swiss Med Wkly. 2018;148:w14610. doi:.https://doi.org/10.4414/smw.2018.14610
55 Bovio N , Vienneau D , Canu IG . Inventory of occupational, industrial and population cohorts in Switzerland. Occup Environ Med. 2019;76(Suppl 1):A29.1. doi:.https://doi.org/10.1136/OEM-2019-EPI.77
56 Kass DE , Thier AL , Leighton J , Cone JE , Jeffery NL . Developing a comprehensive pesticide health effects tracking system for an urban setting: New York City’s approach. Environ Health Perspect. 2004;112(14):1419–23. doi:.https://doi.org/10.1289/ehp.7149
57Chiarini B. Projet de sensibilisation des médecins à la santé au travail. Faculté de biologie et de médecine Université de Lausanne UNIL - Bugnon Rue du Bugnon 21 - bureau 4111 CH-1015. Lausanne SUISSE: Université de Lausanne; 2012.
58 Smits PB , de Boer AG , Kuijer PP , Braam I , Spreeuwers D , Lenderink AF , et al. The effectiveness of an educational programme on occupational disease reporting. Occup Med (Lond). 2008;58(5):373–5. doi:.https://doi.org/10.1093/occmed/kqn061