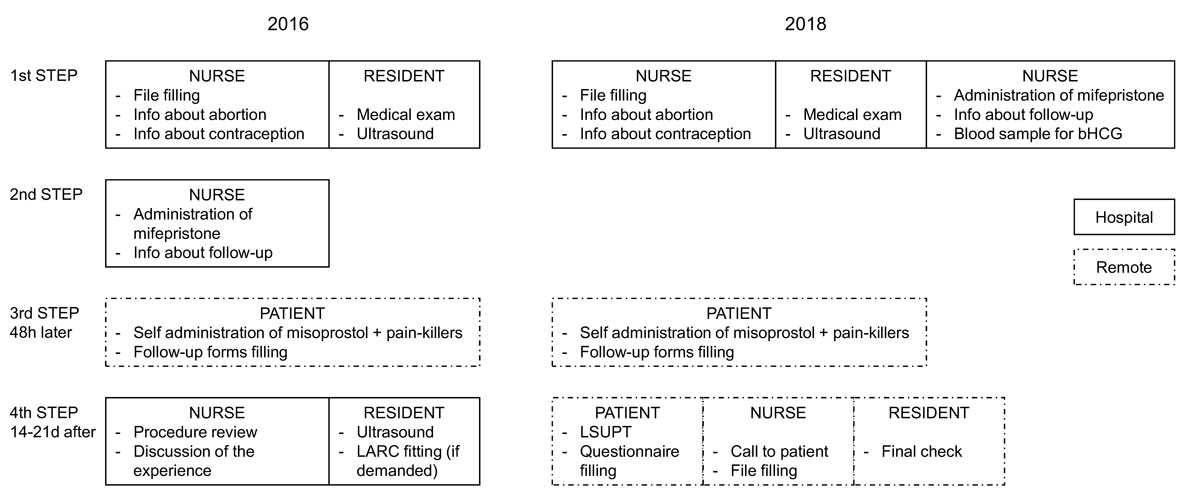
Figure 1 Comparison between IMAD2016 and IMAD2018. LSUPT = low-sensitivity urine pregnancy test (detection limit 1000 IU beta-human chorionic gonadotrophin
DOI: https://doi.org/10.4414/smw.2021.20531
During the last decade, efforts have been made to respond to women’s rising demand to have a more active role in medical termination of pregnancy (mTOP) with the mifepristone-misoprostol regimen, enabling more privacy and fewer time-consuming visits to the hospital [1–7]. Recent evidence shows that mTOP has the same efficacy (up to 98%) regardless of whether it is carried out at home or at the hospital, with the patient’s choice and physician’s assessment taken into consideration [8, 9]. Several strategies for the assessment of procedure success have been proposed [10] and two recent meta-analyses [11, 12] showed that a remote follow-up based on self-assessment and a telephone call by a healthcare provider have the same effectiveness, safety and acceptability as a routine clinical follow-up.
This remote patient-centred policy in mTOP reduces costs and overtreatment in terms of unnecessary consultations (including ultrasound examinations) and supplementary treatments or surgery, while responding to women’s wishes [13, 14]. Nevertheless, failure of mTOP, defined as ongoing viable pregnancy, can occur in 0.5–1% of cases, and women should be appropriately warned [2, 15]. Counselling and prescription of post-abortion contraception, as a fundamental part of the pregnancy termination procedure, should be approached during the first in-presence consultation, enabling a quick post-abortion initiation, including in cases where women do not adhere to follow-up [1, 16, 17].
In Switzerland, as in most European countries, many changes in abortion care took place in the last decade with the aim of meeting women’s demands and offering better cost-effective options. Voluntary termination of pregnancy is allowed up to 12 weeks of gestation; however, mTOP is reserved for pregnancies up to 9 weeks. According to the Swiss National Statistics, the rate of termination of pregnancy in Switzerland has been stable (about 7/1000 women) for almost 10 years and decreased to 6.4/1000 women in 2018, of which 72% were mTOP [18]. In 2018, the Geneva University Hospitals (HUG) alone managed about 10% of all terminations up to 12 weeks of pregnancy in Switzerland (1027/10457). Despite the national trend, the rate of mTOP at HUG was 26% in 2016 and only 6.3% were home-based mTOP. In 2018, a protocol based on remote self-assessment follow-up was introduced for home-based mTOP.
The aim of this study was to evaluate the compliance with and acceptability of this protocol, as well as adherence to contraception. We have also explored its impact in cost reduction.
The study was conducted in the family planning clinic of HUG, where pregnancy termination can be achieved by three methods: (1) aspiration under general anaesthesia after 7 weeks of gestation, (2) ambulatory mTOP (administration of misoprostol at the hospital under surveillance) for pregnancies up to 9 weeks of gestation, and (3) home-based mTOP (with home self-administration of misoprostol). A retrospective comparative analysis was made between two different procedures of home-based mTOP, named IMAD (“interruption médicamenteuse de grossesse à domicile”) adopted respectively in 2016 and 2018 (hereafter named IMAD2016 and IMAD2018).
IMAD2016 was limited to pregnancies up to 7 weeks of gestation; IMAD2018 was extended up to 9 weeks of gestation. Data from patients undergoing pregnancy termination between 01January 2016 and 31 December 2016 and between 01 January 2018 and 31 December 2018 were analysed. Data from 2017 were not included due to the adoption of an intermediary procedure. Women were eligible if they were pregnant, >18 years old, French or English speakers and if they freely chose the IMAD procedure. The exclusion criteria were diagnosis of extra-uterine pregnancy or missed abortion, gestational age >7 weeks in 2016 and >9 weeks in 2018 or choice for surgical termination of pregnancy. The ethics committee of Geneva approved the study (CCER 2019-01713) and, given that only anonymised data were collected, the need for informed consent from patients was waived.
The IMAD procedures in 2016 and 2018 are reported in figure 1. Both adopted the same treatment: oral mifepristone 200 mg followed 48 hours later by two doses of oral misoprostol 400 μg each (at a 3-hour interval). The use of mifepristone for pregnancy termination up to 9 weeks is based on international scientific evidence [1], despite being considered off-label by Swissmedic. In IMAD2016, patients had a standard of three hospital-based consultations, whereas in IMAD2018 they had just one. The main changes were the taking of a blood sample for beta-human chorionic gonadotropin (b-HCG) measurement during the first consultation and modification of the fourth step into a remote self-assessed follow-up. This comprised an autonomous low-sensitivity urine pregnancy test (LSUPT, detection 1000bHCG, CheckToP®) and completion of a two-section questionnaire evaluating procedure success and compliance with contraception. A separate satisfaction questionnaire was administered to evaluate remote follow-up. A telephone call with a nurse was scheduled, and a resident performed a double check of the final medical file. In both third steps, patients were asked to fill in a pictorial assessment chart for assessing bleeding and a visual analogue scale for evaluation of pain during the first 24 hours after the procedure. Patients were advised to contact the emergency service if pain persisted despite analgesic medication, or the bleeding score was ≥9/h or more (normal <9/h according to the pictorial chart), or if they had minimal or absent bleeding. IMAD failure was defined as the persistence of an intrauterine gestational sac. In such a case, an aspiration was performed. Other cases of retained products of conception (RPOC) could require additional treatments or expectant management. In IMAD2016, the diagnosis of ongoing pregnancy or RPOC was based on sonographic criteria: visualisation of intrauterine gestational sac for the first case, endometrium thicker than 15 mm or positive Doppler flow for the second case. Management depended on the patient’s symptoms and physician’s choice (i.e., ultrasound evaluation following menses or second administration of misoprostol with a follow-up 14 days later). In IMAD2018, RPOC was suspected in the case of a positive low-sensitivity urine pregnancy test (LSUPT) or presence of at least two of the following criteria: persistence of two pregnancy symptoms, impression of no expulsion, and minimal bleeding. In this case, patients were asked to come to the clinic for b-HCG level testing and ultrasound to rule out ongoing pregnancy. If the b-HCG level was <20% of the first measurement and the ultrasound did not show a persistent gestational sac, patients were asked to come back for serial b-HCG testing until levels were negative. It is worth mentioning that this prolonged follow-up of b-HCG level decrease is not essential to determine the success of the procedure, but has been adopted in order to avoid unattended complications. In patients with associated bleeding or pain, aspiration was carried out.
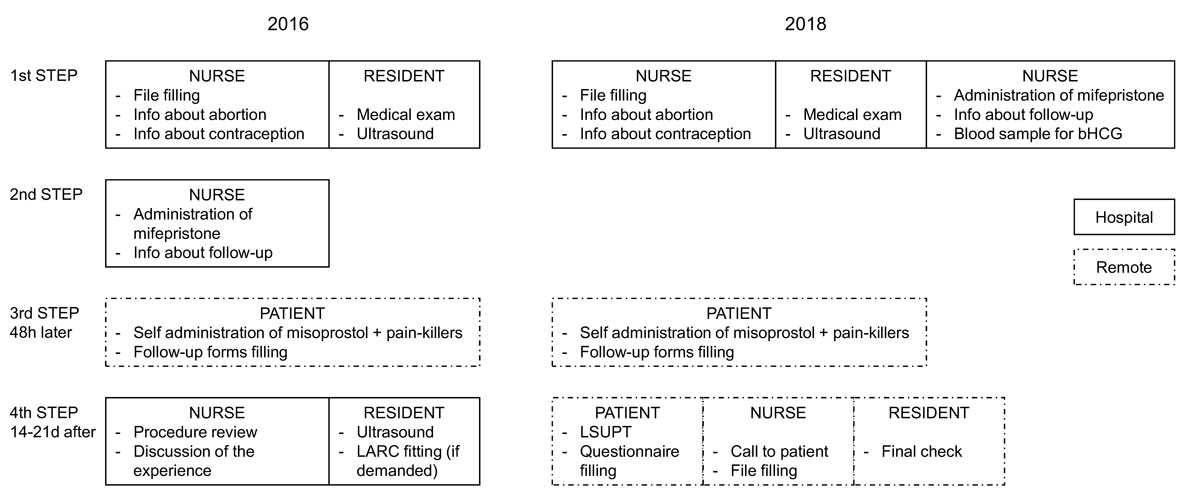
Figure 1 Comparison between IMAD2016 and IMAD2018. LSUPT = low-sensitivity urine pregnancy test (detection limit 1000 IU beta-human chorionic gonadotrophin
In IMAD2016, contraception was started immediately after the fourth step. In IMAD2018: combined oral contraceptive pills were started at the third step, implants were inserted at the second step; intrauterine devices were fitted in a supplementary visit.
The primary outcome was the total number of outpatient consultations for each procedure and the associated costs. The number of supplementary consultations was calculated for every patient starting from the fourth step of IMAD up to 2 months after the procedure, including all visits related to mTOP. Scheduled consultations for long-acting reversible contraceptive (LARC) insertion were not included. Secondary outcomes were acceptability of and adherence to the remote follow-up method, type of contraception chosen, number of RPOC diagnoses, loss to follow-up and LSUPT accuracy.
Health costs in Switzerland are regulated by a national tariff system. Table 1 shows the costs of all visits related to mTOP provided by the accounting division of HUG and converted into USD with an exchange rate of 1 USD = 1 Swiss franc (1 December 2019). According to article 30 of the Swiss Federal Law on Health Insurance (LAMal) and article 119 of the Swiss Penal Code, terminations of pregnancy are covered by basic health insurance after deductible and co-payment (10% of the costs), regardless of the method selected.
Table 1 Cost of all visits related to medical termination of pregnancy (in USD).
| Step | Procedure | 2016 | 2018 |
|---|---|---|---|
| Cost for standard procedure (total) | 704.3 | 552.65 | |
| 1st step | Nurse consultation (30 min) | 21.60 | 21.60 |
| Resident consultation (20 min) | 59.65 | 59.65 | |
| Gynaecological examination | 87.35 | 87.35 | |
| Ultrasound | 142.00 | 142.00 | |
| Discussion on contraception (10 min) | 34.10 | 34.10 | |
| Care in absence of the patient (10 min) | 34.10 | 34.10 | |
| 2nd step | Nurse consultation (30 min) | 21.60 | 21.60 |
| Mifepristone | 46.55 | 46.55 | |
| b-HCG blood sample | – | 19.50 | |
| 3rd step | Check-top LSUPT | 18.00 | |
| 4th step | Nurse consultation (30 min) | 21.60 | – |
| Resident consultation (20 min) | 59.65 | – | |
| Ultrasound | 142.00 | – | |
| Care in absence of the patient (10 min) | 34.10 | 68.2 | |
| Cost for supplementary appointments (total) | 201.65 | 60.2 (202.2)* | |
| Extra | Resident consultation (20 min) | 59.65 | – |
| Ultrasound | 142.00 | (142.00)* | |
| b-HCG blood sample and nurse services | – | 26.10 | |
| Care in absence of the patient | – | 34.10 | |
b-HCG = beta-human chorionic gonadotrophin; LSUPT = low-sensitivity urine pregnancy test * Cost for first supplementary appointment including ultrasound examination
The total cost of a termination of pregnancy ranges from USD 700 to 3000. The average cost of a hospital-based medical termination is USD 1400 and a surgical termination comes to USD 2100.
Statistical analysis was performed using the Stata program version 13 (StataCorp LP: College Station, TX, USA); the significance level for all tests was p <0.05.
Among the 892 women who requested termination of pregnancy in 2016, 56 (6.3%) opted for IMAD and were included in the study; gestational age was <7 weeks for all of them. In 2018, 1027 patients requested termination of pregnancy and 145 (14.1%) opted for IMAD. Among them, 97 (9.4%) were <7 weeks and 48 (4.7%) were between 7 and 9 weeks of gestation (fig. 2). Overall, IMAD demand increased by 7.8% between 2016 and 2018 (p <0.01). When only pregnancies <7 weeks of gestation are considered, IMAD uptake increased by 3.1% (p <0.01). Loss to follow-up was similar in both groups, with three missed patients in 2016 (5.3%) and eight in 2018 (5.5%) (p = 0.234).

Figure 2 Distribution of pregnancy termination methods at the HUG family planning clinic in 2016 and 2018. IMAD = interruption médicamenteuse de grossesse à domicile; TOP = termination of pregnancy
Table 2 summarises participants’ characteristics (n = 201). The median age was 31 years (interquartile range [IQR] 27–35). About half (52.7%) of the women were nulliparous and 40.3% had a previous history of pregnancy termination. There was a statistically significant difference in the distribution of gestational weeks between the groups, because in 2018 pregnancies between 7 and 9 weeks of gestation were also eligible for IMAD.
Table 2 Demographic characteristics.
| Variable | 2016 | 2018 | Total | p-value |
| n (%) | n (%) | n (%) | ||
| Total | 56 (27.9) | 145 (72.1) | 201 (100) | |
| Age (years), median (IQR) | 31.5 (28–36) | 30 (26–35) | 31 (27–35) | 0.215 |
| Parity | 0.509 | |||
| – 0 | 29 (51.8) | 77 (53.1) | 106 (52.7) | |
| – 1 | 10 (17.9) | 34 (23.5) | 44 (21.9) | |
| – ≥2 | 17 (30.4) | 34 (23.5) | 51 (25.4) | |
| Previous caesarean section | 3 (5.4) | 15 (10.3) | 18 (9.0) | 0.267 |
| Previous TOP | 26 (46.4) | 55 (37.9) | 81 (40.3) | 0.271 |
| Weeks of gestation | <0.001 | |||
| – ≤6 weeks | 32 (57.1) | 39 (26.9) | 71 (35.3) | |
| – ≤7 weeks | 24 (42.9) | 58 (40.0) | 82 (40.8) | |
| – ≤8 weeks | 0 | 28 (19.3) | 29 (13.9) | |
| – ≤9 weeks | 0 | 20 (13.8) | 20 (10.0) |
IQR = interquartile range; TOP = termination of pregnancy
Table 3 Follow-up after medical termination of pregnancy (n = 201).
| Variable | 2016 | 2018 | Total | p-value |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | ||
| Total | 56 (27.9) | 145 (72.1) | 201 (100) | |
| Need for supplementary appointments | 0.389 | |||
| – No | 37 (69.8) | 110 (75.9) | 106 (52.7) | |
| – Yes | 16 (30.2) | 35 (24.1) | 44 (21.9) | |
| Number of follow-up appointments (mean ± SD) | 1.47 ± 0.85 | 0.41 ± 0.88 | 0.70 ± 0.99 | <0.001 |
| Suspicion of RPOC | 16 (30.2) | 21 (15.3) | 37 (19.5) | 0.021 |
| Supplementary treatment | 0.686 | |||
| – Surgery (curettage/ hysteroscopy) | 2 (3.8) | 8 (5.5) | 10 (5.1) | |
| – Second misoprostol administration | 4 (7.5) | 7 (4.8) | 11 (5.6) | |
| Method of contraception chosen | 0.039 | |||
| – LARCs (including the implant, hormonal and copper IUD) | 21 (42.0) | 74 (56.9) | 95 (52.8) | |
| – SARCs (including the pill, patch and vaginal ring) | 28 (56.0) | 47 (36.2) | 75 (41.7) | |
| Other (condom, vasectomy) | 1 (2.0) | 9 (6.9) | 10 (5.5) | |
| – Pain score (VAS), median (IQR) | 1 (0–1) | 4 (3–6) | 3 (1–5) | <0.001 |
LARC = long-acting reversible contraception; IQR = interquartile range; IUD = intrauterine device; RPOC = retained products of conception; SARC = short-acting reversible contraception; SD = standard deviation; VAS = visual analogue scale
In 2016, a total of 78 follow-up consultations were needed compared with 60 in 2018; this resulted in an average number of consultations per patient of 1.47 in 2016 vs 0.41 in 2018, leading to a reduction of 1.06 consultations per patient (p <0.001). In 2016, 16 (30.2%) women needed supplementary appointments because of suspicion of RPOC. In 2018, 35 (24.1%) women needed an in-clinic consultation either for suspicion of RPOC (21, 60%), bleeding (5, 14.3%) or for other causes such as anxiety (9, 25.7%).
The cost analysis is represented in table 1. The overall cost of the IMAD2018 standard procedure was reduced by about 27% compared with IMAD2016 (USD 704.30 vs 552.65). When supplementary appointments for follow-up were considered, the overall cost of the IMAD2018 was reduced by about 39% (USD 985.17 vs 611.84).
Regarding contraception, 56.9% of women opted for LARCs in 2018 compared with 42.0% in 2016 (p = 0.039). The percentage of patients who did not start contraception was similar: 10.7% (n = 6) in 2016 and 10.3% (n = 15) in 2018 (p = 0.939).
No case of on-going pregnancy was detected by IMAD2016, whereas two cases were detected by IMAD2018 (1.4%), both with a pregnancy of less than 7 weeks gestation: one patient had a positive LSUPT, one patient came before the fourth step assessment because of minimal bleeding. Both pregnancies were identified before 12 weeks of gestation and patients underwent surgical termination of pregnancy. No ongoing pregnancies were missed with the IMAD2018 protocol.
The rate of RPOC diagnosis was double with the IMAD2016 protocol (n = 16, 30.2%) compared with IMAD2018 (n = 21, 15.3%) (p = 0.021). In 2016, 11/16 of the suspected RPOC cases were based on sonographic criteria (two had thicker endometrium, eight had positive Doppler, and one had both) and 5/16 on physician’s impression. All patients were asymptomatic. In 2018, 15/21 cases had positive or doubtful LSUPT, and 6/21 had other criteria suspicious for retention. One LSUPT was found to be a false positive after evaluation of blood b-HCG levels.
The questionnaire about satisfaction was filled in by 71.4% of patients in 2016 and by 84.8% in 2018. IMAD2018 had a higher level of satisfaction (95.1% vs 55.0%, p <0.001), with only 3% of patients left unsatisfied (vs 15%). Questions concerning satisfaction about remote follow-up added in the IMAD2018 protocol were answered by 84.8% of patients, showing excellent rates of acceptability (97.5% of respondents claimed to have received thorough information on the procedure and follow-up, and 99.1% confirmed that they had no need to call the emergency unit). Adherence to the procedure was recorded only in 2018 when active participation of patients in follow-up was evaluated. Overall, 91 pictorial charts (62.7%) for pain and bleeding were completed and submitted.
This study shows that a remote follow-up based on self-assessment for mTOP of less than 9 weeks is an acceptable alternative to hospital-based follow-up, is associated with fewer supplementary appointments, and eventually reduces the costs borne by the healthcare system. Moreover, all procedure failures were identified, showing a good efficacy of the remote procedure.
Thus far, the few studies that have assessed the cost-effectiveness of mTOP management always compared it with surgical management and most of them examined the treatment in cases of early pregnancy loss rather than termination of pregnancy, with contradictory results. Some studies showed an economic advantage of medical treatment over surgery [19, 20], but direct comparisons were inadequate because of diversity of management strategies, outcome measures and costs. For some analyses, the lower cost of medical treatment did not always translate into higher efficacy [19–21]. In a sample of 33,846 women, medical abortion showed excellent efficacy of 96.7% in pregnancies up to 9 weeks of gestation [21]; two other studies showed that surgical aspiration was the least costly and most effective option, especially when performed in an ambulatory outpatient setting; nonetheless, medical management was more efficient for incomplete abortion [21, 22]. Besides this contradictory evidence, an individual’s self-determined choice could ultimately result in higher satisfaction with and success of the procedure, thereby playing an essential role [7].
Studies analysing the influence on costs of the follow-up procedure are also lacking. In our analysis, we noticed that by simply eliminating the post-procedure ultrasound examination we could significantly reduce costs. Moreover, replacement of the physician by an experienced nurse at follow-up was an additional element that further reduced costs [23–26]. At the family planning clinics of HUG, residents are under rotation every 6 months; thus, they do not gain sufficient experience and expertise in termination of pregnancy management, diagnosis of RPOC by ultrasound and contraceptive counselling. This may have contributed to overestimation of retention (8.9%) in 2016, as physicians did not feel comfortable in interrupting follow-up when they were uncertain about the success of the method, leading to multiple visits and implying consequent stress and discomfort for patients choosing mTOP. Note that ultrasound diagnosis of RPOC can be ineffective even if carried out by experienced physicians, hence follow-up with a pregnancy test should be chosen [27].
Several authors [27, 28] have suggested that by offering a unique method based on objective criteria (LSUPT and serum b-HCG testing), unnecessary consultations can be eliminated while ensuring the same level of efficacy as documented for ultrasound screening. Our results support this evidence, showing a statistically significant reduction in RPOC diagnosis and number of total consultations per patient, while maintaining good efficacy and satisfaction.
After the introduction of the IMAD2018 protocol, the more experienced members of the mTOP team managed the procedure, leading to more skilful execution of the follow-up coupled with more efficient contraceptive counselling. This might explain the statistically significant increase in demand for LARCs in 2018, since it has been shown that TOP providers play a key role in the choice of contraception, especially in pursuing LARCs [29]. Women who chose LARCs were particularly adherent in attending their scheduled appointments; hence we did not notice a reduction of attendance due to elimination of in-presence follow-up.
Rates of loss to follow-up with IMAD2018 were comparable to those with IMAD2016 and only rarely patients completely skipped the follow-up appointments. These results, together with high adherence rate, are in line with literature analysing the clinical impact of a remote follow-up [30] and confirm that a patient-centred approach to pregnancy termination, where women can choose the treatment and the follow-up, is a suitable and affordable option for eligible patients seeking mTOP in Switzerland [31].
The introduction of the IMAD2018 protocol and the extension of gestational age eligible for IMAD resulted in a 158% rise in demand for the procedure (computed as percentage increase).
To the best of the authors’ knowledge, this study is the first to analyse the influence in terms of costs of the follow-up procedure for home-based mTOP. The main limitations of the study are the small sample size and the retrospective nature of the analysis. Although the number of patients in 2018 was three times higher than in 2016, the two samples were similar in terms of sociodemographic characteristics. Another limitation relates to the satisfaction questionnaires that were administered only at the first follow-up appointment and, therefore, not considering evaluations by patients undergoing prolonged follow-up assessments. Information provided by women in the first questionnaire following the abortion may differ from that gathered several weeks after the procedure.
Remote follow-up based on self-assessment for home-based mTOP is a suitable and efficient alternative to hospital-based follow-up and is associated with fewer follow-up consultations and reduced costs. Patients are globally satisfied with this method, which places them in the centre of care, leading to lower risk of overtreatment with higher satisfaction. The results of our study may help assist private gynaecologists and clinics to implement guidelines for remote follow-up and hospitals to also include this option for hospital-based mTOP. A cost-effectiveness analysis as well as the acceptability of these strategies would be useful. Long-term acceptability of these procedures should also be assessed in the form of questionnaires that could be administered some months later.
The authors kindly acknowledge Mrs. Chantal Dunand for her support in the realisation of this study.
No financial support and no other potential conflict related to this article was reported.
1World Health Organization. Safe abortion: technical and policy guidance for health systems. 2nd ed. Geneva: WHO; 2012.
2 Kulier R , Kapp N , Gülmezoglu AM , Hofmeyr GJ , Cheng L , Campana A . Medical methods for first trimester abortion. Cochrane Database Syst Rev. 2011;11(11):CD002855.
3 Ngo TD , Park MH , Shakur H , Free C . Comparative effectiveness, safety and acceptability of medical abortion at home and in a clinic: a systematic review. Bull World Health Organ. 2011;89(5):360–70. doi:.https://doi.org/10.2471/BLT.10.084046
4 Fiala C , Winikoff B , Helström L , Hellborg M , Gemzell-Danielsson K . Acceptability of home-use of misoprostol in medical abortion. Contraception. 2004;70(5):387–92. doi:.https://doi.org/10.1016/j.contraception.2004.06.005
5 Purcell C , Cameron S , Lawton J , Glasier A , Harden J . Self-management of first trimester medical termination of pregnancy: a qualitative study of women’s experiences. BJOG. 2017;124(13):2001–8. doi:.https://doi.org/10.1111/1471-0528.14690
6 Cameron S , Glasier A , Dewart H , Johnstone A . Women’s experiences of the final stage of early medical abortion at home: results of a pilot survey. J Fam Plann Reprod Health Care. 2010;36(4):213–6. doi:.https://doi.org/10.1783/147118910793048719
7 Kopp Kallner H , Fiala C , Gemzell-Danielsson K . Assessment of significant factors affecting acceptability of home administration of misoprostol for medical abortion. Contraception. 2012;85(4):394–7. doi:.https://doi.org/10.1016/j.contraception.2011.08.009
8World Health Organization. Health worker roles in providing safe abortion care and post-abortion contraception. Geneva: WHO; 2015.
9 Gambir K , Kim C , Necastro KA , Ganatra B , Ngo TD . Self-administered versus provider-administered medical abortion. Cochrane Database Syst Rev. 2020;3(3):CD013181.
10National Guideline Alliance (UK). Abortion care. London: National Institute for Health and Care Excellence (UK); 2019 Sep. https://www.nice.org.uk/guidance/ng140.
11 Baiju N , Acharya G , D’Antonio F , Berg RC . Effectiveness, safety and acceptability of self-assessment of the outcome of first-trimester medical abortion: a systematic review and meta-analysis. BJOG. 2019;126(13):1536–44. doi:.https://doi.org/10.1111/1471-0528.15922
12 Schmidt-Hansen M , Cameron S , Lohr PA , Hasler E . Follow-up strategies to confirm the success of medical abortion of pregnancies up to 10 weeks’ gestation: a systematic review with meta-analyses. Am J Obstet Gynecol. 2020;222(6):551–563.e13. doi:.https://doi.org/10.1016/j.ajog.2019.11.1244
13 Clark WH , Gold M , Grossman D , Winikoff B . Can mifepristone medical abortion be simplified? A review of the evidence and questions for future research. Contraception. 2007;75(4):245–50. doi:.https://doi.org/10.1016/j.contraception.2006.11.011
14 Grossman D , Ellertson C , Grimes DA , Walker D . Routine follow-up visits after first-trimester induced abortion. Obstet Gynecol. 2004;103(4):738–45. doi:.https://doi.org/10.1097/01.AOG.0000115511.14004.19
15 Fiala C , Cameron S , Bombas T , Parachini M , Agostini A , Lertxundi R , et al. Outcome of first trimester medical termination of pregnancy: definitions and management. Eur J Contracept Reprod Health Care. 2018;23(6):451–7. doi:.https://doi.org/10.1080/13625187.2018.1535058
16Haute Autorité de Santé. Contraception chez la femme après une interruption volontaire de grossesse (IVG). Saint-Denis La Plaine: HAS; 2019.
17Royal College of Obstetricians and Gynaecologists. Best practice in comprehensive abortion care. Best Practice Paper n.2. London: RCOG; 2015.
18Office fédéral de la statistique. Interruption de grossesse. Neuchâtel: OFS; 2019.
19 Petrou S , Trinder J , Brocklehurst P , Smith L . Economic evaluation of alternative management methods of first-trimester miscarriage based on results from the MIST trial. BJOG. 2006;113(8):879–89. doi:.https://doi.org/10.1111/j.1471-0528.2006.00998.x
20 Graziosi GC , Bruinse HW , Reuwer PJ , van Kessel PH , Westerweel PE , Mol BW . Misoprostol versus curettage in women with early pregnancy failure: impact on women’s health-related quality of life. A randomized controlled trial. Hum Reprod. 2005;20(8):2340–7. doi:.https://doi.org/10.1093/humrep/dei019
21 Hu D , Grossman D , Levin C , Blanchard K , Goldie SJ . Cost-effectiveness analysis of alternative first-trimester pregnancy termination strategies in Mexico City. BJOG. 2009;116(6):768–79. doi:.https://doi.org/10.1111/j.1471-0528.2009.02142.x
22 Rausch M , Lorch S , Chung K , Frederick M , Zhang J , Barnhart K . A cost-effectiveness analysis of surgical versus medical management of early pregnancy loss. Fertil Steril. 2012;97(2):355–60.e1. doi:.https://doi.org/10.1016/j.fertnstert.2011.11.044
23 Sjöström S , Kopp Kallner H , Simeonova E , Madestam A , Gemzell-Danielsson K . Medical Abortion Provided by Nurse-Midwives or Physicians in a High Resource Setting: A Cost-Effectiveness Analysis. PLoS One. 2016;11(6):e0158645. doi:.https://doi.org/10.1371/journal.pone.0158645
24 Sjöström S , Dragoman M , Fønhus MS , Ganatra B , Gemzell-Danielsson K . Effectiveness, safety, and acceptability of first-trimester medical termination of pregnancy performed by non-doctor providers: a systematic review. BJOG. 2017;124(13):1928–40. doi:.https://doi.org/10.1111/1471-0528.14712
25 Kopp Kallner H , Gomperts R , Salomonsson E , Johansson M , Marions L , Gemzell-Danielsson K . The efficacy, safety and acceptability of medical termination of pregnancy provided by standard care by doctors or by nurse-midwives: a randomised controlled equivalence trial. BJOG. 2015;122(4):510–7. doi:.https://doi.org/10.1111/1471-0528.12982
26 Barnard S , Kim C , Park MH , Ngo TD . Doctors or mid-level providers for abortion. Cochrane Database Syst Rev. 2015;(7):CD011242. doi:.https://doi.org/10.1002/14651858
27 Fiala C , Safar P , Bygdeman M , Gemzell-Danielsson K . Verifying the effectiveness of medical abortion; ultrasound versus hCG testing. Eur J Obstet Gynecol Reprod Biol. 2003;109(2):190–5. doi:.https://doi.org/10.1016/S0301-2115(03)00012-5
28 Michie L , Cameron ST . Simplified follow-up after early medical abortion: 12-month experience of a telephone call and self-performed low-sensitivity urine pregnancy test. Contraception. 2014;89(5):440–5. doi:.https://doi.org/10.1016/j.contraception.2014.01.010
29 Maxwell L , Voetagbe G , Paul M , Mark A . Does the type of abortion provider influence contraceptive uptake after abortion? An analysis of longitudinal data from 64 health facilities in Ghana. BMC Public Health. 2015;15(1):586. doi:.https://doi.org/10.1186/s12889-015-1875-2
30 Chen MJ , Rounds KM , Creinin MD , Cansino C , Hou MY . Comparing office and telephone follow-up after medical abortion. Contraception. 2016;94(2):122–6. doi:.https://doi.org/10.1016/j.contraception.2016.04.007
31 Seidenberg A , Fiala C . One stop MToP. Swiss Medical Forum 2015;15(34):745–8. doi:https://doi.org/10.4414/smf.2015.02375
No financial support and no other potential conflict related to this article was reported.