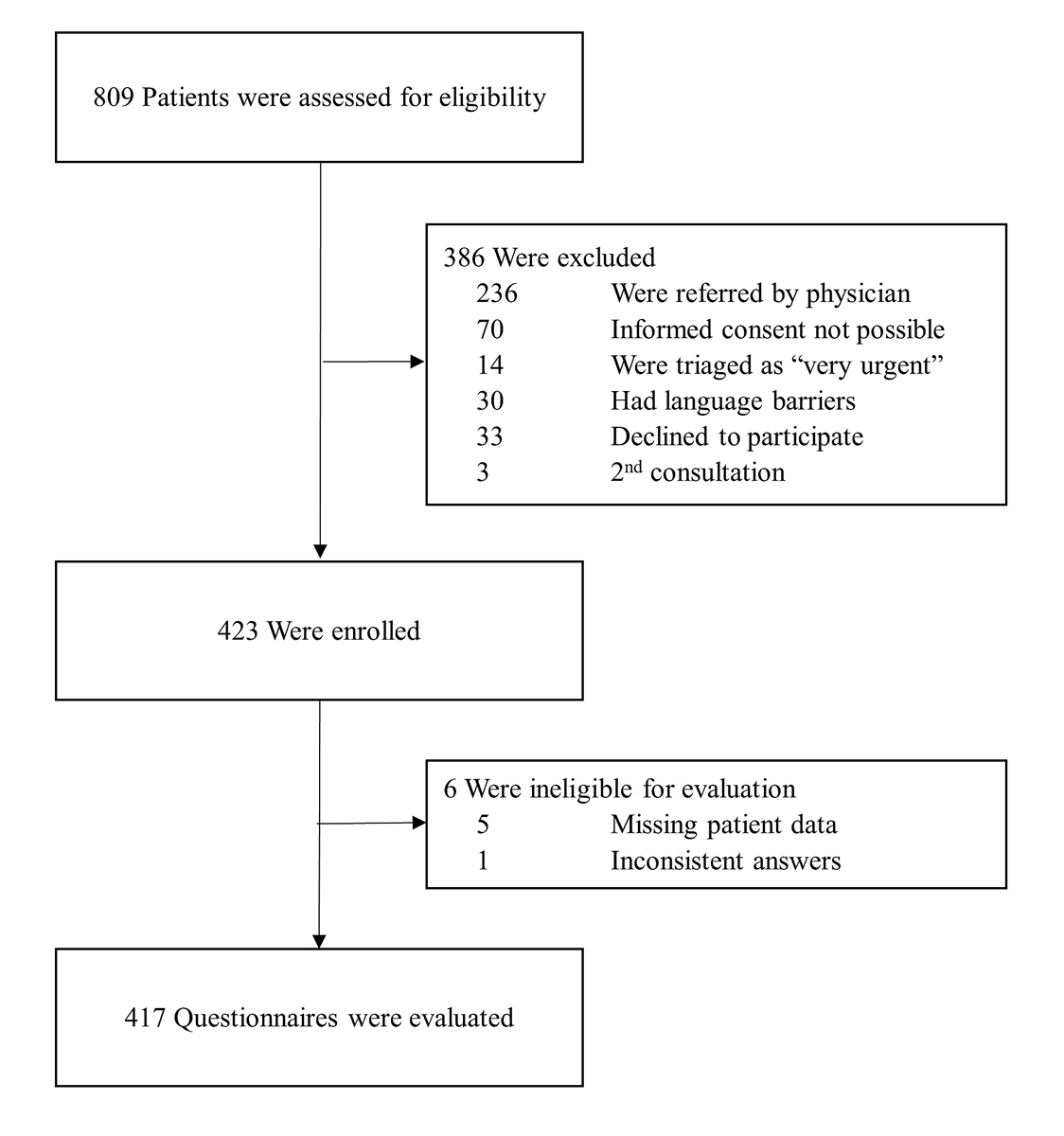
Figure 1 Flowchart of the study.
DOI: https://doi.org/10.4414/smw.2021.20543
Telehealth is defined by the US National Institutes of Health (NIH) as medical care provided at a distance. It can include communication technologies, phone or video calls, smartphone applications and the use of internet resources for self-care [1]. The use of telehealth resources for health issues in general and emergency situations in particular has become widespread among patients [2–4].
In 2018, more than 65% of the Swiss reported having used the internet in the previous 3 months to obtain information on health issues [5]. Various studies reported that 65–80% of patients who use telehealth or inform themselves online about their symptoms before an emergency consultation do not communicate this to their attending emergency physician, and consequently do not give the emergency team the opportunity to adequately respond to this prior information and the resulting needs of the patients [4, 6–9].
As a result of the increasing number of emergency patients and the decreasing willingness of young general practitioners to provide emergency services, and exacerbated by the coronavirus pandemic, there is currently a debate in Switzerland as to whether telehealth could provide support in this regard [10].
According to the literature, the use and acceptance of digital tools [11], and telehealth specifically, depend on age [12], gender [13, 14] and level of education [14]. In order to optimise the use of emergency telehealth in the future, reliable data are needed on both the current use and the users of telehealth, the outcomes of its use and the willingness of patients to use telehealth in emergency situations.
With this exploratory study, we aimed to (i) explore whether patients use telehealth (defined as phone calls, internet use and use of applications) before presenting to the emergency department (ED), (ii) compare patients with and without telehealth use, (iii) investigate outcomes of telehealth use (adherence to the recommendation, confidence and satisfaction), and (iv) explore the attitudes towards telehealth use of non-users.
Around 50,000 patients are treated at Bern University Hospital (Inselspital) ED per year [15]. In accordance with the objective of this exploratory study, a consecutive convenience sample was obtained during 10 early shifts (7:15–14:30), 10 late shifts (14:30–22:30) and 10 night shifts (22:30–07:15) within the study period from 23 October to 15 December 2019, including weekend days and weekdays in the ratio 2:5.
Inclusion criteria were age >17 years, primary presentation and consent to participate in the survey. We excluded patients who had not taken the decision to consult the ED themselves (referral for a planned specialist follow-up or referral by family physicians or police) and patients who were categorised as “very urgent” according to the Swiss emergency triage scale (STS) [16]. Severe language barriers with the study team (who spoke fluent German, French and English) were also a reason for exclusion, as well as failure to obtain informed consent or patient discharge before the survey was conducted.
The study was conducted as a cross-sectional study with prospective data collection among the adult walk-in population of a tertiary care ED in Switzerland. Patients were enrolled and screened consecutively for eligibility. Informed consent was obtained in the waiting room area.
In order to assure the safety of patient data and avoid missing data and misunderstanding of the questions, the survey was conducted as a paper-based survey and completed by the study team together with the patients in the waiting area. The study team involved in the patient survey consisted of two medical students, who were instructed and closely supervised by the senior researchers (AM, TCS). Treatment was not delayed for the patient to complete the questionnaire; if the questionnaire was not completed during the waiting time, this was finalised after the consultation.
The survey consisted of 19 questions (see appendix 1). Our survey questions covered three main areas in accordance with the study aims: (i) the use of telehealth before presenting to the ED and characteristics of telehealth use, (ii) telehealth outcomes, and (iii) readiness for future use of telehealth. We tested the questionnaire before the start of our survey with medical doctors working in the ED and with a convenience sample of patients.
Patient and consultation characteristics were extracted from the electronic patient records. Triage at ED presentation is made by trained nurses according to the Swiss Emergency Triage Scale [16].
The present investigation was registered with the Ethics Committee of Canton Bern, Switzerland under the number 2019-00635.
Data analysis was performed in Stata® MP 16 (StataCorp, The College Station, Texas, USA). For descriptive analysis, categorical variables were presented as absolute numbers and percentages. The distribution of the continuous variable “age” was described as median and interquartile range (IQR), as the variable was not normally distributed. All other variables were categorical variables and were compared using the chi-square test or Wilcoxon rank-sum tests, as appropriate. A p-value <0.05 was considered significant.
The present investigation was registered with the Ethics Committee of Canton Bern, Switzerland under the number 2019-00635. Consent was obtained from each patient. No treatment was delayed or otherwise influenced.
During the shifts included within the study period (23October to 15 December 2019), 809 walk-in patients who visited our ED were screened for eligibility. A breakdown of the reasons for exclusion (n = 392) is presented in the study flowchart (fig. 1). A total of 423 patients were finally included in our study, and 417 complete questionnaires were evaluated. Baseline characteristics of all survey participants are presented in table 1.
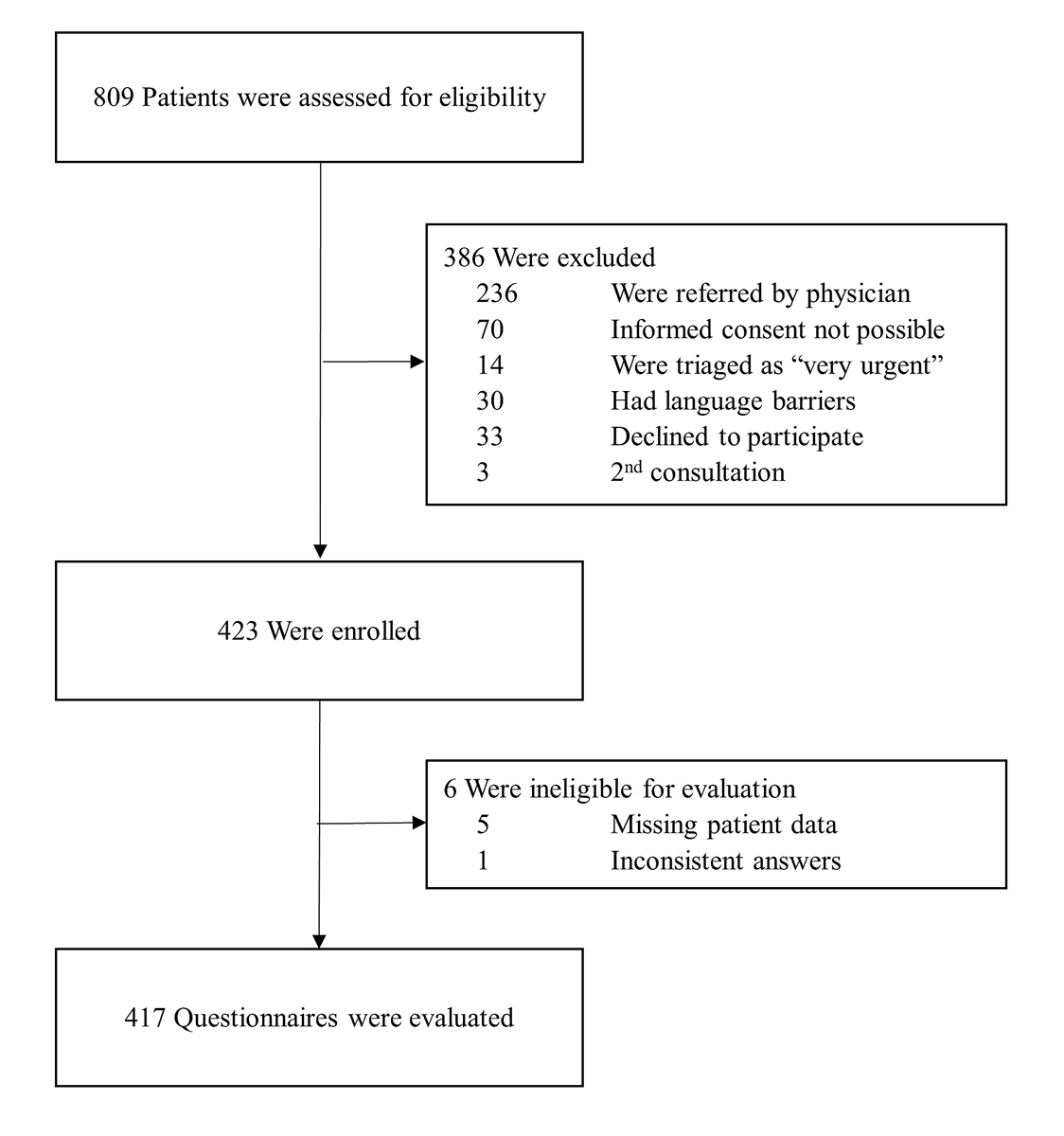
Figure 1 Flowchart of the study.
Table 1 Baseline characteristics of survey participants.
| All patients (n = 417) | |
|---|---|
| Demographic data | |
| Age (years), median (IQR) | 42 (29–59) |
| Gender, female, n (%) | 231 (55.4) |
| Education, n (%) | |
| Tertiary | 116 (27.8) |
| Secondary | 221 (53.0) |
| Obligatory | 68 (16.3) |
| No formal education | 12 (2.9) |
| Language, n (%) | |
| German | 339 (81.3) |
| French | 16 (3.8) |
| Italian | 7 (1.7) |
| English | 18 (4.3) |
| Other | 37 (8.9) |
| Nationality, n (%) | |
| Swiss | 275 (66.0) |
| Other | 142 (34.1) |
| Triage urgency, n (%) | |
| Urgent conditions | 76 (18.2) |
| Semi-urgent | 310 (74.3) |
| Non urgent | 31 (7.4) |
| Hours of presentation, n (%) | |
| 7:15–14:30 | 182 (43.7) |
| 14:30–22:30 | 163 (39.1) |
| 22:30–7:15 | 72 (17.3) |
| Presentation on weekend days, n (%) | 157 (37.7) |
IQR = interquartile range
Fewer than half of our patients (43.9%, n = 183) used telehealth resources before presenting to the ED. Table 2 compares the patients who used or did not use telehealth. The use of telehealth did not depend on age (p = 0.355). The proportion of females in the telehealth user group was lower than for non-users (46.5%, n = 85 vs 62.4%, n = 146; p = 0.001). There was a significant association between education and telehealth use (p = 0.009). In our sample, 34.4% (n = 63) of telehealth users had received tertiary education compared with 22.7% (n = 53) of non-users (see table 2). Patients who had previously successfully solved a medical problem using telehealth were more likely to be in the telehealth group at presentation (34.4%, n = 63 vs 20.5%, n = 48; p = 0.001). Patients consulting because of trauma used telehealth significantly less often than patients with medical emergencies (15.9%, n = 29 vs 84.15%, n = 154; p <0.001). Patients who were admitted to the hospital after ED evaluation used telehealth less frequently than patients treated on an outpatient basis (18.6%, n = 34 vs 81.4%, n = 149; p = 0.022).
Table 2 Comparison of patients with and without telehealth use.
| All patients | Telehealth used | Telehealth not used | p-value | |
|---|---|---|---|---|
| Total, n (%) | 417 (100) | 183 (43.9) | 234 (56.1) | |
| Demographic data | ||||
| Age (years), median (IQR) | 42 (29–59) | 39 (29–60) | 43.5 (30–58) | 0.355 |
| Gender, female, n (%) | 231 (55.4) | 85 (46.5) | 146 (62.4) | 0.001 |
| Education, n (%) | 0.009 | |||
| Tertiary | 116 (27.8) | 63 (34.4) | 53 (22.7) | |
| Secondary | 221 (53.0) | 96 (52.5) | 125 (53.4) | |
| Obligatory | 68 (16.3) | 21 (11.5) | 47 (20.1) | |
| No formal education | 12 (2.9) | 3 (1.6) | 9 (3.9) | |
| Previous telehealth use, n (%) | 111 (26.6) | 63 (34.4) | 48 (20.5) | 0.001 |
| Trauma, n (%) | 101 (24.2) | 29 (15.9) | 72 (30.8) | <0.001 |
| Hospital admission, n (%) | 59 (14.2) | 34 (18.6) | 25 (10.7) | 0.022 |
Table 3 summarises the characteristics and outcomes of telehealth use by age group. Telephone calls were the most common modality of telehealth used by patients before presenting to the ED (72%, n = 133). Most phone calls were made to healthcare professionals (81.2%, n = 108); 16.5% (n = 22) called a friend or colleague and 3.3% (n = 3) of the patients did not specify whom they had called.
Table 3 Characteristics and outcomes of telehealth use by age group.
| All patients | 18–24 | 25–44 | 45–64 | >64 | p-value | |
|---|---|---|---|---|---|---|
| Telehealth service used, n (%) | ||||||
| Phone call | 133 (72.7) | 23 (74.2) | 50 (65.9) | 22 (67.7) | 38 (90.5) | |
| Internet resources | 49 (26.8) | 7 (22.6) | 27 (35.1) | 11 (33.3) | 4 (9.5) | |
| Phone application | 1 (0.5) | 1 (3.2) | 0 | 0 | 0 | 0.021 |
| Outcome regarding recommendation, n (%) | ||||||
| Adherence | 131 (77.9) | 25 (83.3) | 54 (76.1) | 20 (69.0) | 32 (84.2) | 0.410 |
| Satisfaction | 140 (83.8) | 23 (76.7) | 55 (79.7) | 27 (90.0) | 35 (92.1) | 0.190 |
| Confidence | 50 (74.6) | 11 (78.6) | 21 (70.0) | 10 (76.9) | 8 (80.0) | 0.877 |
Service used n = 183, adherence n = 168, satisfaction n = 167, confidence n = 67
There was a significant association between the modalities used and the age groups of users (see table 3). Most patients (77.9%, n = 131) adhered to the recommendation given, 83.8% (n = 140) were satisfied with the telehealth service used and 78.6% (n = 50) were confident in the recommendation given (see table 3). Only 14 patients (7.7%) stated that they were obliged to use telehealth provided by their insurance before consultation at the ED.
Most patients (71.4%, n = 130) were recommended by telehealth to visit the ED (table 4). No patient who was triaged as “urgent” (STS 2) at ED admission received the lowest telehealth triage for location – “recommendation to self-care or go to the pharmacy”. The lowest telehealth triage for urgency was “consultation within days” and was recommended to three patients who were triaged as “urgent” at ED admission (see table 4).
Table 4 Comparison of telehealth recommendations and ED triage score.
| All patients (n = 182) | Triage “urgent” | Triage “semi-urgent” | Triage “non-urgent” | |
|---|---|---|---|---|
| Location of treatment, n (%) | ||||
| Emergency department | 130 (71.4) | 22 (75.9) | 101 (72.1) | 7 (53.9) |
| Family doctor | 25 (13.7) | 4 (13.8) | 17 (12.1) | 4 (30.8) |
| Self-care or pharmacy | 8 (4.4) | 0 (0) | 7 (5.0) | 1 (7.7) |
| Other | 19 (10.4) | 3 (10.3) | 15 (11.7) | 1 (7.7) |
| Urgency of treatment, n (%) | ||||
| Immediately | 59 (32.4) | 11 (37.9) | 47 (33.6) | 1 (7.7) |
| Same day | 43 (23.6) | 7 (24.1) | 34 (24.3) | 2 (15.4) |
| Within days | 32 (17.6) | 3 (10.3) | 25 (17.9) | 4 (30.8) |
| No suggestion | 48 (26.4) | 8 (27.6) | 34 (24.3) | 6 (46.2) |
STS triage consist of four categories. Patients categorised as “very urgent” were excluded.
Most patients who did not employ telehealth stated that they considered that telehealth was not important (62%, n = 145, table 5). There was a significant association between the patient’s age and reasons not to use telehealth (p=0.015). “Difficulties using internet” were mostly mentioned by patients >64 years, see table 5. Readiness to use telehealth was significantly (p <0.001) associated with age.
Table 5 Attitude towards telehealth in non-users by age group.
| All patients | 18–24 | 25–44 | 45–64 | >64 | p-value | |
|---|---|---|---|---|---|---|
| Reason not to use telehealth, n (%) | 234 (100) | 0.015 | ||||
| Did not know about telehealth possibilities | 12 (5.1) | 1 (3.2) | 6 (6.5) | 2 (2.7) | 3 (7.9) | |
| Was not interested | 16 (6.8) | 1 (3.2) | 7 (7.6) | 5 (6.9) | 3 (7.9) | |
| Deemed not important | 145 (62.0) | 23 (74.2) | 57 (62.0) | 45 (62.0) | 20 (52.6) | |
| Difficulties with internet | 6 (2.6) | 0 | 1 (1.1) | 0 | 5 (13.1) | |
| Insurance model | 2 (0.9) | 0 | 0 | 2 (3%) | 0 | |
| Other | 53 (22.7) | 6 (19.4) | 21 (22.8) | 19 (26.0) | 7 (18.4) | |
| Readiness to use telehealth, n (%) | 417 (100) | |||||
| Ready to use | 216 (51.8) | 31 (50.0) | 112 (66.3) | 50 (47.2) | 23 (28.8) | <0.001 |
Number of patients questioned: “reasons not to use telehealth” n = 234, readiness to use telehealth n = 417
Forty-four percent (44%) of our patients used telehealth before attending the ED. Telehealth was predominantly used by well-educated male patients for semi-urgent, non-traumatic diseases that did not lead to hospitalisation. The telephone was by far the most commonly used telehealth modality – especially in elderly people – and internet services or apps played only a minor role. The main reason for not using telehealth was the lack of knowledge about its importance. Most patients, especially younger ones, are ready to use telehealth for future consultations.
In our population, more male than female patients used telehealth. Gender differences in telehealth use are known and may have an impact on the acceptance of digital healthcare services [13]. Differences can depend on factors such as technical skills and interest in health topics and social media [17, 18]. In previous studies, telehealth phone services were more often used by women [12, 19, 20].
Poorly educated people are also at risk of being left behind in the process of digitalisation [21, 22], as was confirmed in our study. Older people using internet tools have been found to have higher socioeconomic status and higher levels of education [23]. A recent study from Switzerland investigated the accessibility and practicality of an online triage tool during the COVID-19 pandemic and confirmed that elderly people in Switzerland are ready to use online tools, but may require specific instruction [24, 25]. Older patients may be inhibited in using digital tools by lack of technical knowledge, needs and cost [26]. This is reflected in our population, as some elderly patients reported that technical problems may have prevented them from using telehealth. Although age was not significantly different in the two main groups in our study, age differences were found in the service used. Further research is warranted on barriers and drivers of use in specific patient populations and ways to overcome potential challenges [27]. This could include qualitative research.
Phone calls to the family doctor were the most popular telehealth service before presentation. Few older patients used internet resources and nearly none used other forms of telehealth. This might be connected to the popularity and promotion of family doctors, especially in older patients in Switzerland. In the course of 2017, 68.5% of all men and 72.9% of all women in Switzerland consulted a general practitioner [28]. Furthermore, some Swiss health insurance models require patients to contact a telehealth provider before consulting a doctor, although this was the case for only a few of our patients.
Another reason for this predominant use of telephone contact could be the trust in known institutions – which can influence adherence, satisfaction and outcome – and which may play a major role in the doctor-patient relationship in the digital age [27, 29]. In our population, all age groups expressed satisfaction with telehealth, trusted the recommendations and adhered to them. As the quality of the information available in digital sources can vary greatly, future research projects should include a detailed evaluation of the different internet sources or applications. A study [30] from a Swiss telehealth centre confirmed that more than 80% of patients adhere to the recommendation given.
In our sample, 18.1% (n = 33) of patients who received the recommendation “treatment at the pharmacy or at the GP” still presented at the ED. It is striking that four of these non-adherent patients then received an “urgent” triage in our ED. Further research is needed about the patient's reasons for not adhering to the telehealth recommendation, as well as the predictors and outcomes of non-adherence.
When telehealth triage recommendations were compared with ED triage, we found three patients who reported that they received non-urgent triage from telehealth – with the recommendation to consult within days – but were judged as “urgent” at ED triage.
Our data are solely based on information provided by the patient. Therefore, it remains unclear whether this discrepancy occurred because of a misunderstanding, incorrect information, or a real telemedicine under-triage. Nevertheless, the risk of over- or under-triage exists and may put the patient at risk, especially patients with high-risk symptoms [20, 33].
With the increasing shortage of primary care physicians in Switzerland and the decrease in the willingness of primary care physicians to be available 24/7, the role of alternative solutions will become more important. Telehealth can be an opportunity in this context [10]. A Cochrane review [31] found that at least 50% of telephone consultations could be handled through telephonic advice alone. A recent study [32] of telephone triage in western Switzerland found that telephone triage reduced the intention to visit the ED. As in our study, the patients were highly satisfied and adhered to the recommendations.
The most important reason for not using telehealth mentioned in our investigation is that the patient considered that telehealth was not important. This might be influenced by the fact that health services are widely available in Switzerland, due to good coverage, short distances and obligatory health insurance. In contrast to this, within the COVID–19 pandemic, 55% of the older adults in the USA experienced disruption in care [34]. Barriers to accessing the emergency system have also been demonstrated in Switzerland [35]. The use of telehealth has increased substantially around the world and is advocated as an important part of medical care, especially in the context of the pandemic [25, 36, 37]. The COVID-19 pandemic has stimulated digitalisation and telehealth. Future research must examine whether this effect will extend beyond the pandemic. Thus, our findings could serve as a basis for investigations of the impact of the coronavirus pandemic on telehealth use in Switzerland.
One strength of this study is that the study team filled out the questionnaires together with the patients. This led to a low number of dropouts or insufficiently answered questionnaires. On the other hand, this could also be a potential source of bias if patients want to provide convenient or desired responses for the investigator, especially in the self-reported telehealth triage category section. The study team was specifically trained to avoid influencing patients in their responses as much as possible and to deal with anxiety or misunderstanding in the emergency setting with the necessary empathy.
The multiple-choice character of the questions leads to missing information that deserves further qualitative research, for example, exploring the reasons for non-use of telehealth. It is important to keep in mind that we included patients who presented to an ED. Therefore, patients who consulted a telehealth service and found adequate treatment for their complaints were not represented. However, the aim of our study was to provide emergency physicians with an overview of telehealth use in the ED population. In addition to this, our study included only walk-in patients, thus leading to a selection bias. The median age of our population was similar to walk-in patients elsewhere [38].
Many patients used telehealth before ED presentation, with the telephone being the most commonly used telehealth modality, especially among elderly patients. Lack of knowledge about telehealth opportunities, especially those extending beyond phone calls, and technical barriers should be addressed to include all population groups and to realise the full potential of telehealth`s technical capabilities, and should build on the momentum generated by the coronavirus pandemic.
Julian Berger contributed to data acquisition. We thank him for this valuable contribution. Emergency telemedicine at the University of Berne, Switzerland, is supported by the Touring Club Switzerland (TCS) through an endowed professorship.
No funding.
All authors declare that there is no conflict of interest for the present manuscript. TCS holds the endowed professorship for emergency telemedicine at the University of Berne, Switzerland. The founders (Touring Club Switzerland) have no influence on the general direction of telemedicine research. In particular, there is no influence on the content of the current publication or the decision to conduct or publish the present study.
1Telehealth. National Institutes of Health. https://www.nibib.nih.gov/science-education/science-topics/telehealth (2020).
2 McCartney M . How do we know whether medical apps work? BMJ. 2013;346(mar20 1):f1811–1811. doi:.https://doi.org/10.1136/bmj.f1811
3 Millenson ML , Baldwin JL , Zipperer L , Singh H . Beyond Dr. Google: the evidence on consumer-facing digital tools for diagnosis. Diagnosis (Berl). 2018;5(3):95–105. doi:.https://doi.org/10.1515/dx-2018-0009
4Schwenk U. Wer suchet, der findet – Patienten mit Dr. Google zufrieden. Bertelsmann Stiftung Carl-Bertelsmann-Str. 256 33311 Gütersloh www.bertelsmann- stiftung.de, 2018.
5Bundesamt für Statistik (Federal Office of Statistics). Suche nach Gesundheitsinformationen im Internet, internationaler Vergleich - 2018-2019 | Diagramm. Bundesamt für Statistik/content/bfs/de/home/statistiken/kultur-medien-informationsgesellschaft-sport/informationsgesellschaft/gesamtindikatoren/gesundheit-gesundheitssystem/digitale-medizinische-daten.assetdetail.11307965.html (2019).
6 Masters K . Preparing medical students for the e-patient. Med Teach. 2017;39(7):681–5. doi:.https://doi.org/10.1080/0142159X.2017.1324142
7 Silver MP . Patient perspectives on online health information and communication with doctors: a qualitative study of patients 50 years old and over. J Med Internet Res. 2015;17(1):e19. doi:.https://doi.org/10.2196/jmir.3588
8 Diaz JA , Sciamanna CN , Evangelou E , Stamp MJ , Ferguson T . Brief report: What types of Internet guidance do patients want from their physicians? J Gen Intern Med. 2005;20(8):683–5. doi:.https://doi.org/10.1111/j.1525-1497.2005.0115.x
9 Klinar I , Balažin A , Barsić B , Tiljak H . Identification of general characteristics, motivation, and satisfaction of internet-based medical consultation service users in Croatia. Croat Med J. 2011;52(4):557–65. doi:.https://doi.org/10.3325/cmj.2011.52.557
10 Sauter TC , Hautz WE , Lehmann B , Exadaktylos AK . eNotfallmedizin: Notfallversorgung der Zukunft. Schweiz Arzteztg. 2019. doi:.https://doi.org/10.4414/saez.2019.18198
11 Renggli JF , Eken C , Siegrist V , Ortega RN , Nickel C , Rosin C , et al. Usability of a Web-based Software Tool for History Taking in the Emergency Department. Acute Med. 2020;19(3):131–7. doi:.https://doi.org/10.52964/AMJA.0816
12 Dahlgren K , Holzmann MJ , Carlsson AC , Wändell P , Hasselström J , Ruge T . The use of a Swedish telephone medical advice service by the elderly - a population-based study. Scand J Prim Health Care. 2017;35(1):98–104. doi:.https://doi.org/10.1080/02813432.2017.1288816
13 Haluza D , Wernhart A . Does gender matter? Exploring perceptions regarding health technologies among employees and students at a medical university. Int J Med Inform. 2019;130:103948. doi:.https://doi.org/10.1016/j.ijmedinf.2019.08.008
14 Haluza D , Wernhart A . Does gender matter? Exploring perceptions regarding health technologies among employees and students at a medical university. Int J Med Inform. 2019;130:103948. doi:.https://doi.org/10.1016/j.ijmedinf.2019.08.008
15Bern IGA. 3010. Zahlen und Fakten. http://www.notfallzentrum.insel.ch/de/ueber-uns/ueber-die-klinik/zahlen-und-fakten/.
16 Rutschmann OT , et al. Reliability of the revised Swiss Emergency Triage Scale: a computer simulation study. Eur J Emerg Med. 2018;25(4):264–9. doi:.https://doi.org/10.1097/MEJ.0000000000000449
17 Escoffery C . Gender Similarities and Differences for e-Health Behaviors Among U.S. Adults. Telemed J E Health. 2018;24(5):335–43. doi:.https://doi.org/10.1089/tmj.2017.0136
18 Zhang X , Guo X , Lai KH , Guo F , Li C . Understanding gender differences in m-health adoption: a modified theory of reasoned action model. Telemed J E Health. 2014;20(1):39–46. doi:.https://doi.org/10.1089/tmj.2013.0092
19 McAteer A , Hannaford PC , Heaney D , Ritchie LD , Elliott AM . Investigating the public’s use of Scotland’s primary care telephone advice service (NHS 24): a population-based cross-sectional study. Br J Gen Pract. 2016;66(646):e337–46. doi:.https://doi.org/10.3399/bjgp16X684409
20 Huibers L , Smits M , Renaud V , Giesen P , Wensing M . Safety of telephone triage in out-of-hours care: a systematic review. Scand J Prim Health Care. 2011;29(4):198–209. doi:.https://doi.org/10.3109/02813432.2011.629150
21Zelenzny-Green R, Vosloo S, Conole G. Digital inclusion for low-skilled and low-literate people: a landscape review. https://unesdoc.unesco.org/ark:/48223/pf0000261791 (2018).
22 Buccoliero L , Bellio E , Mazzola M , Solinas E . A marketing perspective to “delight” the “patient 2.0”: new and challenging expectations for the healthcare provider. BMC Health Serv Res. 2015;16(1):47. doi:.https://doi.org/10.1186/s12913-016-1285-x
23 Luger TM , Houston TK , Suls J . Older adult experience of online diagnosis: results from a scenario-based think-aloud protocol. J Med Internet Res. 2014;16(1):e16. doi:.https://doi.org/10.2196/jmir.2924
24Michel J. Effects and utility of an online forward triage tool during the SARS-CoV-2 pandemic: patient perspectives (Preprint). http://preprints.jmir.org/preprint/26553 (2020) doi:10.2196/preprints.26553.
25 Hautz WE , Exadaktylos A , Sauter TC . Online forward triage during the COVID-19 outbreak. Emerg Med J. 2020;38(2):106–8. doi:.https://doi.org/10.1136/emermed-2020-209792
26 Kruse C , Fohn J , Wilson N , Nunez Patlan E , Zipp S , Mileski M . Utilization Barriers and Medical Outcomes Commensurate With the Use of Telehealth Among Older Adults: Systematic Review. JMIR Med Inform. 2020;8(8):e20359. doi:.https://doi.org/10.2196/20359
27 Michel J , Hautz WE , Sauter TC . Telemedicine and Online Platforms as an Opportunity to Optimise Qualitative Data Collection, Explore and Understand Disease Pathways in a Novel Pandemic Like COVID-19. J Int Soc Telemed eHealth. 2020. doi:.https://doi.org/10.29086/JISfTeH.8:e9
28Andreani T, Marquis JF; Bundesamt für Statistik. Gesundheitsstatistik 2019. Available from: https://www.bfs.admin.ch/bfs/de/home/aktuell/neue-veroeffentlichungen.gnpdetail.2019-0201.html
29 Birkhäuer J , Gaab J , Kossowsky J , Hasler S , Krummenacher P , Werner C , et al. Trust in the health care professional and health outcome: A meta-analysis. PLoS One. 2017;12(2):e0170988. doi:.https://doi.org/10.1371/journal.pone.0170988
30 Rimner T , Blozik E , Begley C , Grandchamp C , von Overbeck J . Patient adherence to recommendations after teleconsultation: survey of patients from a telemedicine centre in Switzerland. J Telemed Telecare. 2011;17(5):235–9. doi:.https://doi.org/10.1258/jtt.2011.101013
31 Bunn F , Byrne G , Kendall S . Telephone consultation and triage systems: effects on health care use and patient satisfaction. Cochrane Database Syst Rev. 2003;CD004180. doi:.https://doi.org/10.1002/14651858.CD004180
32 Thierrin C , Augsburger A , Dami F , Monney C , Staeger P , Clair C . Impact of a telephone triage service for non-critical emergencies in Switzerland: A cross-sectional study. PLoS One. 2021;16(4):e0249287. doi:.https://doi.org/10.1371/journal.pone.0249287
33 Gamst-Jensen H , Lippert FK , Egerod I . Under-triage in telephone consultation is related to non-normative symptom description and interpersonal communication: a mixed methods study. Scand J Trauma Resusc Emerg Med. 2017;25(1):52. doi:.https://doi.org/10.1186/s13049-017-0390-0
34 More Than Half Of Older Adults In The U.S. Have Experienced Disruptions In Care Due To Coronavirus. NORC https://www.norc.org/NewsEventsPublications/PressReleases/Pages/more-than-half-of-older-adults-in-the-us-have-experienced-disruptions-in-care-due-to-coronavirus.aspx (2020).
35 Hautz WE , Sauter TC , Exadakytlos AK , Krummrey G , Schauber S , Müller M . Barriers to seeking emergency care during the COVID-19 pandemic may lead to higher morbidity and mortality - a retrospective study from a Swiss university hospital. Swiss Med Wkly. 2020;150:w20331. doi:.https://doi.org/10.4414/smw.2020.20331
36 Keesara S , Jonas A , Schulman K . Covid-19 and Health Care’s Digital Revolution. N Engl J Med. 2020;382(23):e82. doi:.https://doi.org/10.1056/NEJMp2005835
37 Hollander JE , Carr BG . Virtually Perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382(18):1679–81. doi:.https://doi.org/10.1056/NEJMp2003539
38 Hysenbegasi M , Hubloue I , Vanobberghen R , Kartounian J , Devroey D . Evolution over 11 years of the characteristics of walk-in patients at the emergency department of a university hospital in Brussels. J Med Life. 2019;12(1):34–42. doi:.https://doi.org/10.25122/jml-2018-0053
No funding.
All authors declare that there is no conflict of interest for the present manuscript. TCS holds the endowed professorship for emergency telemedicine at the University of Berne, Switzerland. The founders (Touring Club Switzerland) have no influence on the general direction of telemedicine research. In particular, there is no influence on the content of the current publication or the decision to conduct or publish the present study.