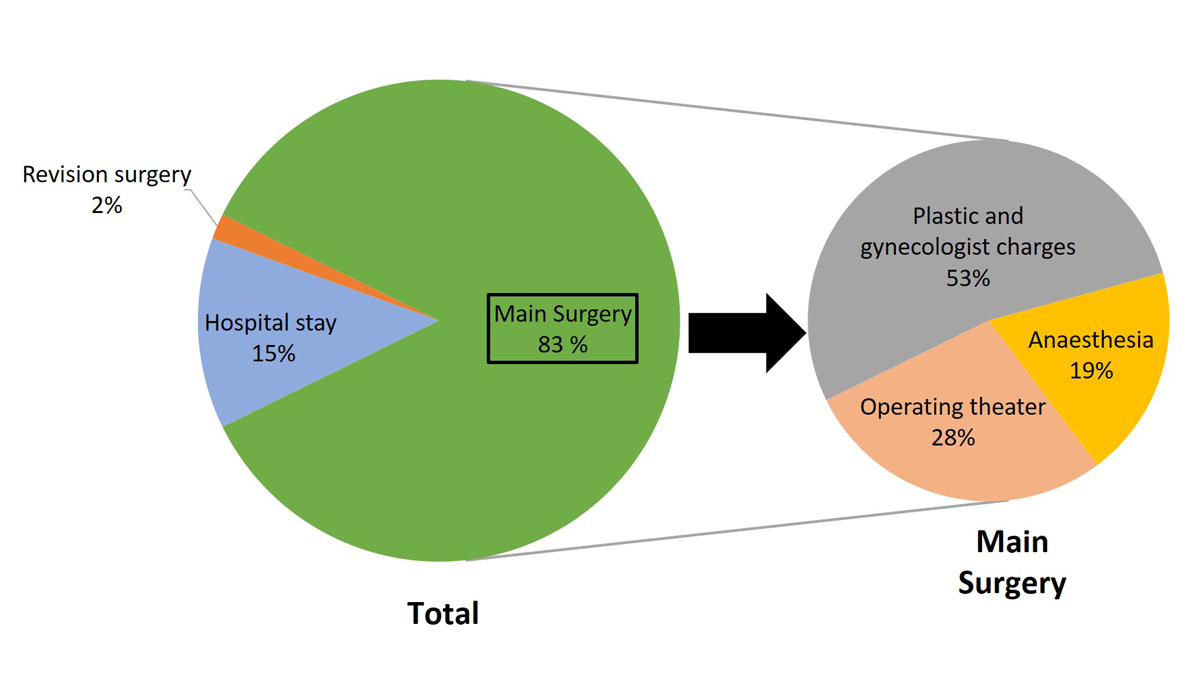
Figure 1 Distribution of “real cost” estimated for each component (% of total cost).
DOI: https://doi.org/10.4414/smw.2021.20530
Breast cancer is the most common malignancy in women worldwide, with a mean incidence of 5750 new cases each year in Switzerland [1]. Despite a trend toward more conservative approaches, mastectomy still maintains an essential role in oncological therapy. This procedure offers high survival rates, but involves an important body mutilation resulting in low self-image and self-esteem [2]. Therefore, different breast reconstruction techniques have been developed and several studies have demonstrated their beneficial effect on the socio-psychological health of patients. Implant-based breast reconstructions are the most common procedures, despite some disadvantages such as higher infection rates, unnatural feeling, implant rupture, or peri-prosthetic capsular contracture risks, which may require additional procedures such as fat grafting, or implant exchange or removal [3]. In the last decade, autologous free-flap reconstructions such as the deep inferior epigastric perforator flap (DIEP), first used in 1994, became a popular alternative to prosthesis reconstruction [3]. Autologous tissue-based reconstructions seem to offer higher satisfaction rates and better long-term outcomes with lower complication rates, requiring fewer secondary procedures than implant-based reconstructions [4].
However, DIEP free-flap breast reconstruction is complex, and requires higher expertise and a longer operation time than other breast reconstruction procedures. So it is to be expected that the DIEP procedure is more costly, and its cost-coverage is currently questionable. To answer this question, the real costs of the procedure and hospital stay for immediate DIEP free-flap breast reconstruction after unilateral mastectomy were estimated and compared with healthcare reimbursement.
In Switzerland, since 2012 the reimbursement of all the medical and surgical cases requiring a hospital stay is billed according to a specific diagnosis-related group (DRG) system. This attribution to a DRG code depends on the main diagnosis, secondary diagnosis, treatments and complications occurring during the stay, as well as the patient’s age and comorbidities. Each DRG code has its own basic cost weight, which can be affected by the length of hospital stay. A mean range of hospital stay is presupposed for each DRG. The final fee for a hospital stay results from the cost weight of the case multiplied by the annual base rate decided between the caregiver on a cantonal basis and the insurance providers. This model is expected to offer a similar charge for all patients classified in the same DRG group and to cover the mean total costs generated by patients consuming different resources.
The medical charts of all consecutive patients who underwent unilateral immediate DIEP free flap-based breast reconstruction after unilateral mastectomy for breast cancer between January 2012 and September 2017 in our Plastic, Reconstructive and Aesthetic Surgery Department were reviewed. Of the 27 patients reviewed, one was excluded because of incomplete invoice data, one patient had an intra-operative flap failure that led to expander placement and was not coded for billing as a DIEP procedure. Five patients who had private insurance coverage were not included, as the billing system differs and could lead to confounding factors. Therefore, 20 consecutive patients fulfilling the study criteria were included.
The real cost generated by each patient during her hospitalisation was estimated. This estimation was based on an algorithm including operating theatre occupation time, anaesthesia and surgeons’ fees (e.g., plastic surgeons and gynaecologists), length of hospital stay, administration fees and the cost of revision surgery during the main hospital stay if needed. All rates used in the algorithm were based on mean real costs calculated by our financial department including costs related to medical and paramedical staff salary, consumables, medications and amortisation. In this study, as the inflation rate was insignificant in Switzerland between 2012 and 2017 (<1% according to the Federal Office of Statistics), for all patients operated on during this period, we based our estimation on the mean real cost of treatments provided in 2017 (table 1).
Table 1 Cost estimation algorithm calculation.
| Cost = (α + 60 min)*(cost per minute of the operating theatre + cost per minute anaesthesia) + α * β * cost per minute plastic surgeon + 120 * γ * cost per minute gynaecologist + δ * (cost per day of hospitalisation + cost per day of nursing care) + administration fee + ε | |
| α = surgery duration, β = number of plastic surgeons, γ = number of gynaecologists, δ = length of stay, ε = cost of revision surgery, calculated with the same algorithm as the main surgery | |
| Rates: | “cost per minute of the operating theatre” including nurses and paramedical salary, consumables and amortisation: CHF 12.17 / min |
| “cost per minute anaesthesia” including anaesthetists and nurses salary, consumables, medications: CHF 8.29 / min | |
| “cost per minute per surgeon”: CHF 4.42 / min | |
| “cost per day of hospitalisation” including hotel cost and medical charges out of surgery room: CHF 408 / day | |
| “cost per day of nursing care” including paramedical staff charges, consumables and medications used out of the surgery room: CHF 102 / day | |
| administration fee: 107 CHF / patient | |
| Because the duration of the mastectomy procedure was not specified in the medical records, a mean time of 120 minutes for the gynaecologist was assumed. | |
To assess if the real cost of the procedure and hospital stay was covered by the healthcare system, the total sum of the estimated costs was calculated for each patient and compared with the total amount billed according to the DRG system. This amount was reimbursed 45% by the patient’s insurance company and 55% was covered by the canton. The total DRG amount was obtained by the multiplication of the case cost weight by the annual base rate (table 2).
Table 2 Value of each DRG code used and real cost estimated for each patient.
| Year | DRG code | Cost weight | Annual base rate | DRG price in CHF | Estimated cost in CHF | Variation |
|---|---|---|---|---|---|---|
| 2012 | J14B | 1.758*† | 10,950 | 19,250.‒ | 32,626.‒ | −13,376.‒ |
| 2013 | J08B J14B J26Z |
2.131 1.460 3.083 |
10,900 | 23,228.‒ 15,914.‒ 33,610.‒ |
39,912.‒ 36,805.‒ 34,721.‒ |
−16,684.‒ −20,891.‒ −1111.‒ |
| 2014 | J02A J02B J02B J02B |
4.740*‡
2.180 2.180 2.180 |
10,500 | 49,791.‒ 22,890.‒ 22,890.‒ 22,890.‒ |
34,032.‒ 44,952.‒ 44,974.‒ 27,414.‒ |
+15,759.‒ −22,062.‒ −22,084.‒ −4524.‒ |
| 2015 | J02A J02B J02B J02B J02B J02B |
4.628*‡
2.128 2.128 2.128 2.128 2.128 |
10,400 | 48,131.‒ 22,131.‒ 22,131.‒ 22,131.‒ 22,131.‒ 22,131.‒ |
26,479.‒ 47,036.‒ 22,131.‒ 36,588.‒ 26,394.‒ 22,648.‒ |
+21,652.‒ −24,905.‒ 0.‒ −14,457.‒ −4263.‒ −517.‒ |
| 2016 | J01Z J01Z J01Z |
3.017 3.017 3.017 |
10,650 | 32,131.‒ 32,131.‒ 32,131.‒ |
43,240.‒ 35,039.‒ 29,799.‒ |
−11,109.‒ −2908.‒ +2332.‒ |
| 2017 | J01B J01B J02A |
2.867 2.867 6.079 |
10,650 | 30,534.‒ 30,534.‒ 64,741.‒ |
29,869.‒ 20,633.‒ 33,028.‒ |
+665.‒ +9901.‒ +31,713.‒ |
*outliers/ † longer stay / ‡shorter stay.
To facilitate the analysis of the results, all the costs are presented as whole numbers in Swiss francs (CHF).
The mean age of patients was 49 years (38–66) at the time of surgery, with a mean body mass index (BMI) of 26.69 kg/m2 (18.8–40). Four were smokers (two active smokers at the time of surgery) and three patients suffered from diabetes.
For 18 patients (90%), it was a primary tumour: two of them had had neo-adjuvant chemotherapy, and one had a lumpectomy 4 months before the mastectomy, but with unsatisfactory margins. She did not receive any other treatment in the interval. The two remaining patients presented recurrent neoplasia 9 and 11 years after a lumpectomy and radiotherapy. No patient underwent prophylactic mastectomy in this study.
Sixteen patients (80%) underwent a skin-sparing mastectomy, three (15%) had a nipple-sparing mastectomy and one (5%) a standard mastectomy. Three (15%) benefited from axillary lymph node dissection during the reconstruction procedure.
The mean surgery time was 581 minutes (345–840). The mean duration of hospitalisation was 9.7 days (7–15).
Three patients (15%) needed revision surgery during the immediate postoperative period: one free-flap pedicle revision for arterial insufficiency suspicion not requiring microsurgical intervention, one microsurgical revision of the pedicle for venous thrombosis, and one breast hematoma drainage. Four (20%) patients presented with significant postoperative complications: one pulmonary embolism, one ulnar nerve paresis due to positioning during the surgery, one skin necrosis on the mastectomy flap managed with hyperbaric oxygen therapy and one partial necrosis of the mastectomy skin margin (post-radiotherapy) treated with conservative management.
The mean total real cost estimated for each hospitalisation stay was CHF 33,416 (CHF 20,633–47,036). Patients without complication generated lower costs (mean real cost of CHF 30,313; CHF 20,633–43,240) than those with complications or requiring surgical revision (mean CHF 40,656; CHF 33,028–47,036). The revision surgery alone had a mean cost of CHF 3626(CHF 2238–4597). Patients with revision surgery had an increased duration of hospital stay with a mean of 12 days (9–15) versus 9 days (7–14) for the patients without revision surgery.
The mastectomy and immediate reconstructive surgery time represented 83% of the total estimated cost of hospitalisation: surgeons’ (gynaecologists’ and plastic surgeons’) fees represented 44% of the total cost, anaesthesia 18% and operating theatre 23% (e.g., ward nurses, consumables) (fig. 1)
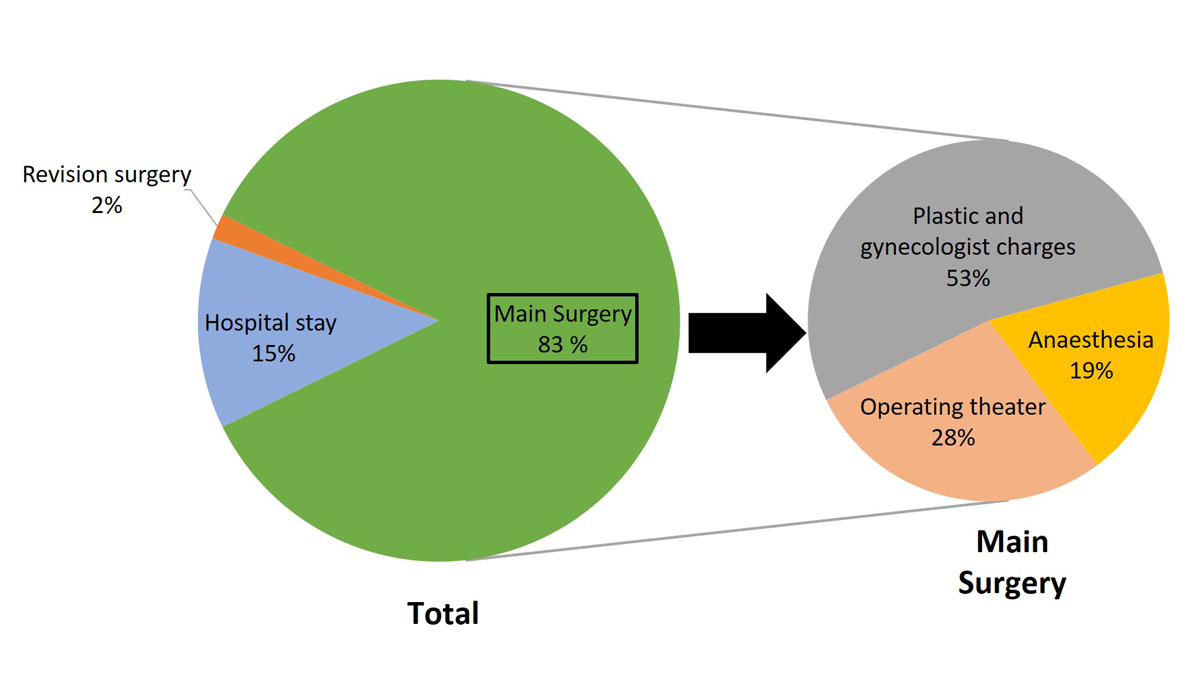
Figure 1 Distribution of “real cost” estimated for each component (% of total cost).
Through 2012 to 2017, seven different DRG codes were used (table 3). The mean price according to the DRG pricing system was CHF 29,573 (CHF 19,256–64,741).
Table 3 Swiss-DRG codes definitions adapted from https://www.swissdrg.org, consulted on 19 September 2019.
| DRG |
DRG definition
in bold = original French text |
Year: Inliers cost weight | Comments |
|---|---|---|---|
| J01B |
Transplantation de tissu avec anastomose microvasculaire lors d'affections de la peau, du tissu sous-cutané et de la glande mammaire, pour néoformation maligne.
Tissue transplantation with microvascular anastomosis used for skin, subcutaneous or breast tissue disease, for malignant neoplasm. |
2017: 2867 2019: 2772 |
DRG created in 2017, replaces J01Z. Offers a more precise definition, distinguishing unilateral (J01B) from bilateral procedure (J01A). It is the most specific code for DIEP reconstruction to date, and it offers a good cost coverage. |
| J01Z |
Transplantation de tissu avec anastomose microvasculaire lors d'affections de la peau, du tissu sous-cutané et de la glande mammaire, pour néoformation maligne.
Tissue transplantation with microvascular anastomosis used for skin, subcutaneous or breast tissue disease, for malignant neoplasm. |
2016: 3017 | Appeared since the 1st DRG Version in 2013 until the 6th DRG Version in 2017, where it is replaced by J01A and J01B. Only used to code DIEP in 2016, where it replaced J02B. |
| J02A |
Transplantation de peau, plastie par lambeaux, lymphadénectomie étendue, transplantation de tissu avec anastomose microvasculaire avec traitement sous vide complexe ou CC extrêmement sévères.
Skin transplantation, flap approach, extensive lymphadenectomy, tissue transplantation with microvascular anastomosis with complex negative pressure therapy or extremely severe complications or comorbidity level. |
2014: 7014 2015: 5840 2017: 6079 2019: 4882 |
Appeared in 2014 and keeps the same definition in 2017. Still used in 2017 for procedures using a lot of resources. |
| J02B |
Transplantation de peau ou plastie par lambeaux, lymphadénectomie étendue, transplantation de tissu avec anastomose microvasculaire, sans traitement sous vide complexe, sans CC extrêmement sévère.
Skin transplantation, flap approach, extensive lymphadenectomy, tissue transplantation with microvascular anastomosis without complex negative pressure therapy, without extremely severe complications or comorbidity level. |
2014: 2180 2015: 2128 |
Appeared in 2014 and was used for DIEP until 2015. Was replaced by J01Z in 2016. |
| J08B |
Autre transplantation de peau ou débridement avec diagnostic complexe, avec intervention supplémentaire au niveau de la tête et de la gorge, sans procédure complexe, avec CC extrêmement sévères.
Other skin transplant or debridement with complex diagnosis, with supplemental surgery on the head and throat with extremely severe complications or comorbidity level, without a complex procedure. |
2013: 2131 | Appeared in the 1st DRG Version in 2013 until the 5th DRG version in 2016, where the definition will be slightly changed. Used in the first years, because no specific DRG existed for DIEP or free flaps. The attribution between J08B, J14B and J26Z was dependent on patient’s past medical story and the number of resources used during the hospital stay. |
| J14B |
Plastie reconstructive de la glande mammaire pour néoformation maligne sans reconstruction coûteuse.
Reconstructive plasty of the breast tissue for a malignant neoplasm without costly reconstruction. |
2012: 1568 2013: 1460 |
Appeared in the 1st DRG Version in 2013 and still present in the 6th DRG Version in 2017. Used in the first years, because no specific DRG existed for DIEP or free flaps. The attribution between J08B, J14B and J26Z was dependent on patient’s past medical story and the number of resources used during the hospital stay. |
| J26Z |
Plastie reconstructive de la glande mammaire avec transplantation complexe de peau, ou grandes interventions sur la glande mammaire pour néoformation maligne avec intervention complexe
Reconstructive plasty of the breast tissue with complex skin transplant, or extensive surgery of the breast tissue for a malignant neoplasm with complex procedures. |
2013: 3083 | Appeared in the 1st DRG Version in 2013 and still present uo to 2018. Used in the first years, because no specific DRG existed for DIEP or free flaps. The attribution between J08B, J14B and J26Z was dependent on patient’s past medical story and the number of resources used during the hospital stay. |
All patients except three stayed in the hospital for a duration corresponding to the range set by their DRG and were therefore invoiced according to the basic cost weight of the DRG (inliers). The three other patients were considered outliers because of shorter or longer stays (table 2).
From 2012 to 2016, the DRG rate was lower than the real estimated cost except for four cases. (table 3). In 2017, this trend inverted with a new DRG code (J01B) defined specifically for unilateral breast reconstruction with the DIEP procedure. The price of this code has a cost weight of 2867, corresponding to a value of CHF 30,534 in our hospital, approaching the mean real cost (CHF 30,313).
This study demonstrates that in our public university hospital, the mean real cost estimated for unilateral immediate DIEP breast reconstruction is CHF 33,416 CHF. The mean DRG price of CHF 29,573 offer a good approximation of the real cost of the procedure and we can conclude that it covers the charges of such surgery. This result might not be extrapolated to the whole institutions of Switzerland, as cost differs among university, non-university, public or private hospitals and even between the cantons. However, the base-rate variation seen between the different institutions is supposed to flatten those differences to offer a fair reimbursement of the procedure. In 2017, the base-rate of our institution had a value of CHF 10,650. Compared with other Swiss institutions it has a high value; for comparison the mean base-rate in public hospitals in 2016 was CHF 9911 [5].
The mean real cost of DIEP breast reconstruction was higher than reported in other countries. Neyt et al. estimated a mean cost of EUR 4486 (CHF 4935 on the basis of EUR 1 = CHF 1.1) for one-stage DIEP flap breast reconstruction after mastectomy in Belgium [6]. In the UK, Paget et al. reported a mean cost of GBP 7628 (CHF 9916 on the basis of GBP 1 = CHF 1.3) for delayed DIEP breast reconstructions. Because of the secondary nature of the reconstruction in that study, the added expenses of a concomitant mastectomy were not included [7]. According to European statistics, hospital treatments costs generally 146% more in Switzerland than the European Union average [8]. These differences can be explained by higher staffing costs, higher per-capita volume of healthcare services and pricier medical equipment in Switzerland, linked to higher salaries and cost of living. According to Eurostat in 2018, the mean consumer price level for food was 43% higher in Switzerland compared with Belgium and 76% higher than in the UK [9].
The “tariff data cost estimation method” used in this study is like the one that Paget et al. have already validated as an accurate cost-estimation design. In a prospective study they compared two methods of cost estimation for the DIEP procedure. On one hand, a “micro-costing method” was used: all consumables, staffing cost and static fees generated by each patient were individually calculated. On the other hand, as performed in our study, the “tariff data cost method” was applied: based on cost generated by all patients, a mean cost of each procedure was calculated and multiplied by duration of anaesthesia, operating theatre occupation and length of hospital stay for each patient. They found no statistical difference between these two methods. Despite being validated, this method remains the main limitation of our study because it does not include the cost of non-surgical therapies needed for some patients presenting complications, such as hyperbaric oxygen therapy or thromboembolic event management. It can be assumed that for patients who with subsequent complications, the total cost will be slightly underestimated because those therapies are not included in our algorithm. This effect is partially compensated by an increased length of hospital stay.
Each year, to obtain a DRG codification corresponding as much as possible to the real cost of each procedure and following medical evolution, the whole DRG billing framework is updated. At the time of the first version of the DRG codification in 2012, the DIEP breast reconstruction was not well known; consequentially it did not receive his own DRG code. Therefore, between 2012 and 2015, the procedure was billed according to unspecific DRG codes (e.g., J14B, J08B, J26Z, J02A, J02B) corresponding mainly to “non-complex reconstruction”. As a result, in the earliest versions of DRG, the rates tended to undercompensate the real cost (table 3). However, outliers with extreme values and some patients coded as more complex procedures allowed smoothing of this slight difference. Since 2017, the DRG definitions became more precise and a new DRG code (J01B) has been created specifically for “Tissue transplantation with microvascular anastomosis for skin, subcutaneous or breast tissue disease, for malignant neoplasm”. This offers the closest real cost coverage for this procedure. For patients undergoing DIEP-based breast reconstruction but needing more resources than usual, a specific code (J02A) with a higher cost weight is attributed. This code has been applied for three cases corresponding to three extreme fees found in this study and allowed the mean DRG price to be raised closer to the mean real cost estimated. These patients required more intensive and heavier treatments because of their past medical history (e.g., radiotherapy, diabetes) or occurrence of complications (e.g., mastectomy skin necrosis requiring hyperbaric oxygen therapy). Other patients who needed revision surgery or presented complications were not considered significant enough to be coded in the DRG J02A.
Currently in 2020, the DIEP reconstructions are still codified with the J01B code group, but the inlier cost weight is lower than the one of 2017 (2.821 vs 2.867). However, in our institution the reimbursement according to DRG still offers a good approximation of the real cost because the difference does not seem significant (CHF 29,677 vs CHF 30,313).
An alternative to flap-based techniques for breast reconstruction is an implant. This technique, developed in the 1960s, is still the most used method worldwide. Using breast prosthesis, the surgery is less complex, shorter and believed to generate less expenses than free flap reconstructions. In 2020, according to the Swiss DRG rates, skin-sparing mastectomy with unilateral immediate implant-based breast reconstruction is billed CHF 18,063 (DRG code J06Z). Obviously, this cost is significantly lower than a DIEP procedure. But, it has been widely reported that implant-based reconstruction requires significantly more revision procedures because of specific complications related to the implant, such as peri-prosthetic capsulitis, late infections or implant breakage [10–12]. Because of this need, implant-based reconstruction seems to have the same total costs over 2 years and is even more costly in the long term [13]. Furthermore, Durry et al. showed that long-term patient satisfaction is significantly higher with free flap reconstructions than implant-based reconstruction [14]. Moreover, Toyserkani et al. demonstrated recently in a meta-analysis the superiority of autologous breast reconstruction compared with implant-based reconstruction regarding psychosocial and sexual well-being, and breast and general outcome satisfaction [15].
Therefore, cost-effectiveness of these methods should be based on long-term costs and patient satisfaction. Multiple cost-effectiveness studies have been conducted, suggesting that the DIEP flap is a cost-effective solution compared with implant-based reconstructions [16–18]. A Dutch study reported that in the short term (<6 weeks), the DIEP procedure was more expensive than a two-stage expander-implant or one stage implant reconstruction, but in the long term (>6 weeks) costs did not statistically differ [19]. In Spain, it was also found that in the long term the DIEP procedure for breast reconstruction compared with expander-prosthesis reconstruction did not show a statistical difference in long-term costs [20]. American study groups found that free flaps generate less or similar costs in the long term than implant-based reconstruction due to potential implant failures, since free flaps need fewer revision surgeries [13, 21]. However, as Khajuria et al. underlined in their meta-analysis, those results arise from studies with different cost-effectiveness evaluations, which limits comparison between them [22]. Furthermore, as depicted above, the high healthcare costs in Switzerland might influence the difference between DIEP and implant-based reconstruction costs. All those factors explain why the DIEP procedure became for selected patients the gold-standard breast reconstruction technique.
Since 2017, a specific DRG code has been defined for “Tissue transplantation with microvascular anastomosis for breast malignant neoplasm”. This new codification seems to offer a good cost coverage of the procedure in our public university hospital. As DIEP-based breast reconstruction offer high patient satisfaction, this technique should be offered to elective patients requiring a breast reconstruction.
No financial support and no potential conflict of interest relevant to this article was reported.
1National Institute for Cancer Epidemiology and Registration. Switzerland | NICER [Internet]. [cited 2020 Feb 6]. Available from: https://www.nicer.org/en/
2 Koçan S , Gürsoy A . Body Image of Women with Breast Cancer After Mastectomy: A Qualitative Research. J Breast Health. 2016;12(4):145–50. doi:.https://doi.org/10.5152/tjbh.2016.2913
3 Homsy A , Rüegg E , Montandon D , Vlastos G , Modarressi A , Pittet B . Breast Reconstruction: A Century of Controversies and Progress. Ann Plast Surg. 2018;80(4):457–63. doi:.https://doi.org/10.1097/SAP.0000000000001312
4 Howard-McNatt MM . Patients opting for breast reconstruction following mastectomy: an analysis of uptake rates and benefit. Breast Cancer (Dove Med Press). 2013;5:9–15. doi:.https://doi.org/10.2147/BCTT.S29142
5Felder DS, Merian-Weg P. Différences de tarif et de financement entre les hôpitaux publics et les cliniques privées. Faculty of Economics, University of Basel; 2016. Final report.
6 Neyt MJ , Blondeel PN , Morrison CM , Albrecht JA . Comparing the cost of delayed and immediate autologous breast reconstruction in Belgium. Br J Plast Surg. 2005;58(4):493–7. doi:.https://doi.org/10.1016/j.bjps.2004.12.002
7 Paget JT , Young KC , Wilson SM . Accurately costing unilateral delayed DIEP flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2013;66(7):926–30. doi:.https://doi.org/10.1016/j.bjps.2013.03.032
8Koechlin F, Konijn P, Lorenzoni L, Schreyer P. Comparing Hospital and Health Prices and Volumes Internationally: Results of a Eurostat/OECD Project. 2014 Aug 26 [cited 2020 Feb 6]; Available from: https://www.oecd-ilibrary.org/social-issues-migration-health/comparing-hospital-and-health-prices-and-volumes-internationally_5jxznwrj32mp-en
9Eurostat: Consumer price levels [Internet]. [cited 2020 Feb 6]. Available from: //ec.europa.eu/eurostat/cache/infographs/pricelevels/pricelevels_2018/index.html
10 Pool SMW , Wolthuizen R , Mouës-Vink CM . Silicone breast prostheses: A cohort study of complaints, complications, and explantations between 2003 and 2015. J Plast Reconstr Aesthet Surg. 2018;71(11):1563–9. doi:.https://doi.org/10.1016/j.bjps.2018.07.010
11 Lam TC , Hsieh F , Salinas J , Boyages J . Immediate and Long-term Complications of Direct-to-implant Breast Reconstruction after Nipple- or Skin-sparing Mastectomy. Plast Reconstr Surg Glob Open. 2018;6(11):e1977. doi:.https://doi.org/10.1097/GOX.0000000000001977
12 Collier W , Scheefer Van Boerum M , Kim J , Kwok AC . Are 30-Day Outcomes Enough? Late Infectious Readmissions following Prosthetic-Based Breast Reconstruction. Plast Reconstr Surg. 2019;144(3):360e–8e. doi:.https://doi.org/10.1097/PRS.0000000000005903
13 Lemaine V , Schilz SR , Van Houten HK , Zhu L , Habermann EB , Boughey JC . Autologous Breast Reconstruction versus Implant-Based Reconstruction: How Do Long-Term Costs and Health Care Use Compare? Plast Reconstr Surg. 2020;145(2):303–11. doi:.https://doi.org/10.1097/PRS.0000000000006422
14 Durry A , Baratte A , Mathelin C , Bruant-Rodier C , Bodin F . Satisfaction des patientes après reconstruction mammaire immédiate : comparaison entre cinq techniques chirurgicales [Patients’ satisfaction after immediate breast reconstruction: Comparison between five surgical techniques]. Ann Chir Plast Esthet. 2019;64(3):217–23. Article in French. doi:.https://doi.org/10.1016/j.anplas.2018.12.002
15 Toyserkani NM , Jørgensen MG , Tabatabaeifar S , Damsgaard T , Sørensen JA . Autologous versus implant-based breast reconstruction: A systematic review and meta-analysis of Breast-Q patient-reported outcomes. J Plast Reconstr Aesthet Surg. 2020;73(2):278–85. doi:.https://doi.org/10.1016/j.bjps.2019.09.040
16 Matros E , Albornoz CR , Razdan SN , Mehrara BJ , Macadam SA , Ro T , et al. Cost-effectiveness analysis of implants versus autologous perforator flaps using the BREAST-Q. Plast Reconstr Surg. 2015;135(4):937–46. doi:.https://doi.org/10.1097/PRS.0000000000001134
17 Thoma A , Veltri K , Khuthaila D , Rockwell G , Duku E . Comparison of the deep inferior epigastric perforator flap and free transverse rectus abdominis myocutaneous flap in postmastectomy reconstruction: a cost-effectiveness analysis. Plast Reconstr Surg. 2004;113(6):1650–61. doi:.https://doi.org/10.1097/01.PRS.0000117196.61020.FD
18 Grover R , Padula WV , Van Vliet M , Ridgway EB . Comparing five alternative methods of breast reconstruction surgery: a cost-effectiveness analysis. Plast Reconstr Surg. 2013;132(5):709e–23e. doi:.https://doi.org/10.1097/PRS.0b013e3182a48b10
19 Damen THC , Wei W , Mureau MA , Tjong-Joe-Wai R , Hofer SO , Essink-Bot ML , et al. Medium-term cost analysis of breast reconstructions in a single Dutch centre: a comparison of implants, implants preceded by tissue expansion, LD transpositions and DIEP flaps. J Plast Reconstr Aesthet Surg. 2011;64(8):1043–53. doi:.https://doi.org/10.1016/j.bjps.2010.12.028
20 Lagares-Borrego A , Gacto-Sanchez P , Infante-Cossio P , Barrera-Pulido F , Sicilia-Castro D , Gomez-Cia T . A comparison of long-term cost and clinical outcomes between the two-stage sequence expander/prosthesis and autologous deep inferior epigastric flap methods for breast reconstruction in a public hospital. J Plast Reconstr Aesthet Surg. 2016;69(2):196–205. doi:.https://doi.org/10.1016/j.bjps.2015.11.027
21 Fischer JP , Wes AM , Nelson JA , Basta M , Rohrbach JI , Wu LC , et al. Propensity-matched, longitudinal outcomes analysis of complications and cost: comparing abdominal free flaps and implant-based breast reconstruction. J Am Coll Surg. 2014;219(2):303–12. doi:.https://doi.org/10.1016/j.jamcollsurg.2014.02.028
22 Khajuria A , Prokopenko M , Greenfield M , Smith O , Pusic AL , Mosahebi A . A Meta-analysis of Clinical, Patient-Reported Outcomes and Cost of DIEP versus Implant-based Breast Reconstruction. Plast Reconstr Surg Glob Open. 2019;7(10):e2486. doi:.https://doi.org/10.1097/GOX.0000000000002486
No financial support and no potential conflict of interest relevant to this article was reported.