Are we fit to teach? A survey in physicians of the in- and outpatient departments of internal medicine at a Swiss university hospital
DOI: https://doi.org/10.4414/smw.2021.20505
Andrea
Meienberga, Michael
Mayra, Stefano
Bassettib, Eliska
Potlukovab
a Outpatient Medical Department, University Hospital Basel and University of Basel, Switzerland
b Division of Internal Medicine, University Hospital Basel and University of Basel, Switzerland
Summary
AIM OF THE STUDY
Teaching is one of the three pillars of medical-academic activity, alongside patient care and research. The aim of our study was to assess current teaching practice in the medical departments of the University Hospital Basel, Switzerland, in order to organise a faculty development programme tailored to local needs.
METHODS
We performed a cross-sectional online survey among the teaching faculty and the residents. For both groups, we assessed their estimation of the general importance and perceived frequency of various teaching formats in everyday practice. Additionally, we asked the senior physicians to evaluate their teaching competencies and the residents to state their opinion on factors promoting a positive learning experience.
RESULTS
Twenty-eight of 34 senior physicians (82%) and 48 of 90 residents (53%) participated in the study. Both groups broadly agreed on the importance of various teaching formats for the professional development of physicians, placing particular importance on bedside teaching, providing feedback, teaching during case discussions, and observation and modeling. However, the residents perceived that they obtained less teaching, feedback and support than the senior physicians perceived they were giving. Overall, teaching during case discussions represented the format most often applied, and it was also the one in which the senior physicians felt most competent. Residents claimed “time” to be the most important factor promoting a positive learning experience, followed by a positive attitude und the personal characteristics of the supervisor.
CONCLUSION
Our study shows that, despite being an integral part of everyday work at a university clinic, many aspects of current teaching practice allow discussion on possibilities of adaptations and improvement. Evaluation of current teaching practice provides the basis for designing a faculty development programme tailored to specific needs.
Introduction
The duties and requirements of the medical faculties in hospitals are multifaceted and demanding. The core competencies of patient care, research and teaching diversify the daily business and highly depend on one another. However, they entail miscellaneous competencies beyond medical expert knowledge. According to the training programme for internal medicine specialists of the Swiss Institute for Advanced Medical Training and Education (SIWF, Schweizerisches Institut für ärztliche Weiter- und Fortbildung), teaching, with leadership, research, and continuing education, are integral parts of a physician’s duties [1]. The various competing demands and conflicting priorities in daily clinical routine may hinder clinical teaching. Furthermore, education and continuing education of physicians currently mainly focuses on fostering medical expert knowledge and technical skills, and the development of the didactic skills of clinical teachers is frequently neglected [2]. Thus, the teaching faculty may remain in their own comfort zone as clinicians and not embrace their dual role as clinicians and teachers [3].
Theoretically, various faculty development interventions have been reported to enhance teaching in clinical settings. Evidence indicates that faculty development programmes (a) improve attitudes towards teaching, (b) improve the quality of teaching and didactic skills, and (c) increase perception of the changes in teaching skills by learners [4].
Currently, different faculty development interventions are offered in Switzerland. Examples are didactic programmes of the universities as a prerequisite for an academic career, faculty development courses organised by the SIWF (in collaboration with the Royal College of Physicians of London), regular workshops offered yearly during the Swiss Society of General Internal Medicine (SGAIM) meetings about teaching skills, a master programme on medical education in Bern (MME), or a certificate of advanced studies (CAS) in medical education at the University of Geneva. Additionally, various other local individual courses, such as a faculty development programme for junior clinical faculty in Geneva, Switzerland, are available [5]. However, a systematic and comprehensive training for the teaching faculties of any specialisation or for internal medicine specialists – a representative of the largest specialist training programme – is lacking, raising the question of whether clinical teachers are well prepared for this duty.
The aim of our study was to assess current clinical teaching practice, focusing on unstructured teaching in the clinical setting of the medical departments of the University Hospital Basel, Switzerland, as well as the self-estimated teaching competence of the senior physicians. We also aimed to assess residents’ perceptions of factors promoting a positive learning experience.
Results of this study will be used to define the content of a new faculty development programme on clinical teaching at our hospital and may act as a model for other hospitals and medical schools that wish to introduce new teaching concepts.
Materials and methods
Participants and setting
In April 2019, we invited all physicians of the Inpatient and Outpatient Medical Departments of the University Hospital Basel to participate in this cross-sectional study. The medical staff of the two departments includes 90 residents and 34 senior physicians (6 senior consultants, 26 consultants and both heads of the departments).
The University Hospital Basel is one of the five university hospitals in Switzerland and is affiliated with the University of Basel. From the total of 700 hospital beds, 204 are at the disposal of the Division of Internal Medicine, with approximately 6700 inpatients treated per year. The Outpatient Medical Department accounts for approximately 25,000 visits per year.
Measurement and procedure
Using the program SurveyMonkey (SurveyMonkey Inc.) [6], we developed an online survey directed at assessing current teaching practice in the clinical setting. Specifically, we assessed and compared the estimation of general importance and perceived frequency of various teaching formats from the perspective of the residents and of the senior physicians.
The survey was divided into two parts with adaptations to the target participants, i.e., the residents and the senior physicians (table 1). The first part of the survey was identical for all physicians. If needed, the wording was adapted according to its function in the context of the question. In the second part of the survey, the senior physicians answered questions on self-estimation of their teaching competencies, and their need of and interest in further medical education training. The residents answered an open question on strategies promoting a positive learning experience using free text.
Table 1 Overview of the content of the survey.
|
Part 1 (identical for residents and senior physicians)
|
| Sociodemographic characteristics, i.e., sex, current workplace and work experience in years |
| Evaluation of the importance of different teaching formats for the professional development of physicians in general, including learning through observation, bedside teaching, case discussions, peer teaching, internal rounds and skill evaluation (mini-CEX and DOPS) |
| Evaluation of the actual teaching practice by assessing the frequency of different teaching units in everyday work |
| Evaluation of different teaching strategies beneficial to support and empowerment of the learner (e.g., time management, involvement in case discussions, encouragement to work independently, stimulation of self-directed learning, evidence-based clinical reasoning, bring up problems and difficulties) |
|
Part 2 (different for residents and senior physicians)
|
| Senior physicians: Self-estimation of their teaching competencies and their need and interest in further medical education training |
| Residents: Strategies promoting a positive learning experience |
To launch the survey, we sent an e-mail to all participants explaining the purpose of the survey, followed by an e-mail with the link. We asked the participants to fill in the survey within 2 weeks after obtaining the link, and we sent a reminder e-mail 3 days before closure of the survey.
In order to assess qualitative data from the survey, we used a five-point Likert scale [7]. Depending on the question, the Likert scale assessed either the consent of the participant, ranging from 1 to 5 (1 = does not apply at all, 2 = rather does not apply, 3 = indifferent, 4 = rather does apply, 5 = does apply strongly, 0 = not applicable), or the frequency of a specific event (e.g., teaching unit), ranging from 1 to 5 ( 1= never, 2 = seldom, 3 = occasionally, 4 = frequently, 5 = very frequently, 0 = not applicable).
Moreover, we used a qualitative approach with an inductive content analysis method to analyse residents’ perceptions of factors promoting a positive learning experience. The purpose of this method is to frame categories aiming to describe and understand a phenomenon [8]. Therefore, we read the residents’ answers and labeled meaningful statements with a code. As residents had the opportunity to indicate multiple factors promoting a positive learning experience, several codes per answer were possible.
Statistics
We conducted the statistical analysis using the program GraphPad Prism version 5.0 for Windows, GraphPad Software, La Jolla. Continuous variables were expressed as mean ± standard deviation (SD) unless otherwise stated, and a t-test or Mann-Whitney test was used for comparison between groups. For correlations, we used Spearman correlation. A p-value of <0.05 was considered statistically significant.
To visualise the different codes emerging from the content analysis, we used the statistical program R, version 4.0.0 (Arbor Day). In order to identify meaningful themes referring to the central research question, we grouped similar codes into categories. Finally, we completed the analysis by a quantitative description of the different categories.
Ethical considerations
Participant confidentiality was protected by complete anonymity of the data collection. The protocol was approved by the local ethics committee (EKNZ Req-2019-01006).
Results
Participants
Twenty-eight of 34 (82%) senior physicians and 48 of 90 (53%) residents participated in the study. The baseline characteristics of the participants are shown in table 2.
Table 2 Characteristics of participating physicians.
|
Characteristics
|
Senior physicians
|
Residents
|
| n |
28 |
48 |
|
Gender*
|
|
|
| Male |
15 (56) |
20 (42) |
| Female |
12 (44) |
28 (58) |
|
Workplace*
|
|
|
| Inpatient Medical Department |
18 (66) |
37 (77) |
| Outpatient Medical Department |
9 (33) |
11 (23) |
|
Time since state examination, FTE years
|
13.25 (6–27) |
4 (1–8) |
|
Work experience as a senior physician, FTE years
|
5.6 (0-18) |
|
|
Participation at a faculty development course
|
|
|
| Yes |
16 (57) |
|
| – Higher education didactic programmes†
|
7 (44) |
|
| – Other didactic training‡
|
9 (56) |
|
| No |
12 (43) |
|
Sixteen of 28 (57%) senior physicians had attended some kind of faculty development course in the past. Of these, 7 (7/16; 44%) senior physicians had attended a higher education didactic programme such as faculty courses organised by the University as a prerequisite for their academic career; one holds a master’s degree in medical education (MME). Nine senior physicians (9/16; 56%) participated in “train the trainers” workshops offered by various providers, namely 1- or 2-day faculty training courses offered by the SIWF and Royal College of Physicians (four participants), 1-day didactic training for tutors offered by the Swiss Ultrasound Association (two participants), and various short monothematic courses from different providers (three participants).
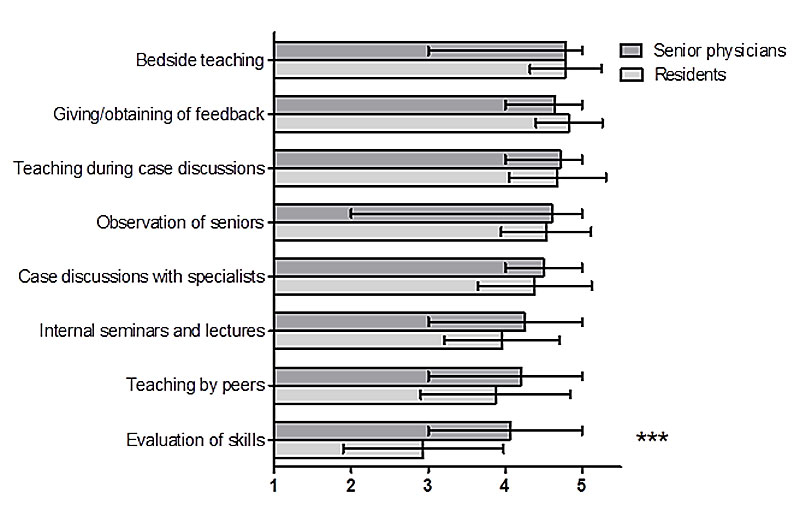
Importance of different teaching and learning formats for professional development
The assessments of the importance of different teaching and learning formats for professional development are shown in figure 1. Both residents and senior physicians paid particular attention to informal teaching such as bedside teaching, giving feedback, case discussions with the supervising senior physicians and specialists in dedicated rounds and in one-on-one discussions, as well as learning from observation of more experienced physicians. Both groups rated formal teaching units, such as seminars and lectures, as less important than various informal teaching situations. Overall, the ratings showed a broad agreement between residents and senior physicians; a significant difference was seen only with regard to the assessment of the importance of skills evaluation. This teaching format was seen as less important by the residents than by the senior physicians.
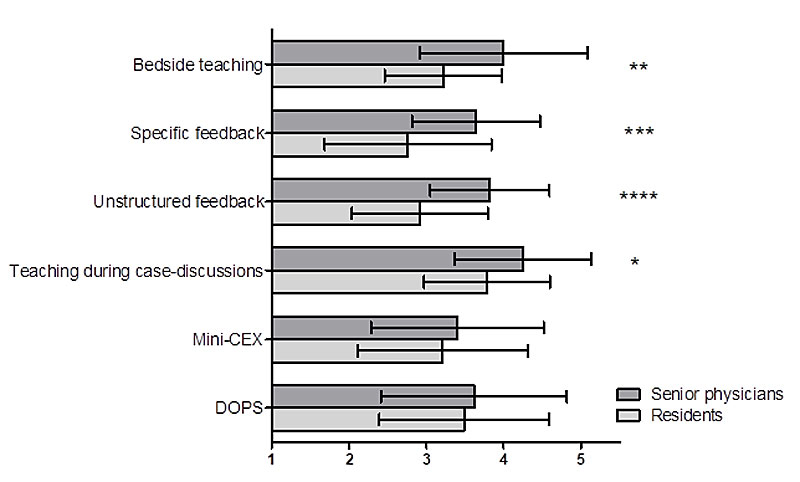
Frequency of different teaching and learning units applied in everyday work
The assessments of the frequency of various teaching and learning units carried out during daily clinical work are shown in figure 2. Informal teaching during case discussions with the supervisor in the ward and accompanying consultations were rated as the most common teaching format by both residents and senior physicians. However, there was a significant difference between the two groups in the perception of the frequency of different teaching units: the residents perceived the frequencies of the various teaching units as lower than the senior physicians, especially regarding case discussions, providing feedback (specific and unspecific) and bedside teaching.
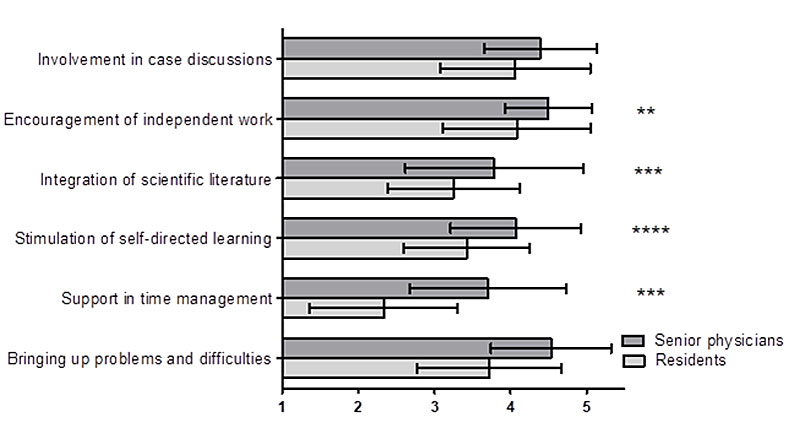
Support of residents in clinical work
The assessment of the frequency of various strategies for supporting and promoting residents on the job is shown in figure 3. Both groups found encouraging independent work and active involvement in case discussions to be the most commonly implemented support strategy. As compared with the senior physicians, residents perceived some of the implemented strategies as much less frequently performed, namely encouragement of independent work, integrating scientific literature, encouraging self-directed learning and support in time management. The residents rated support in time management as by far the least frequently implemented support strategy.
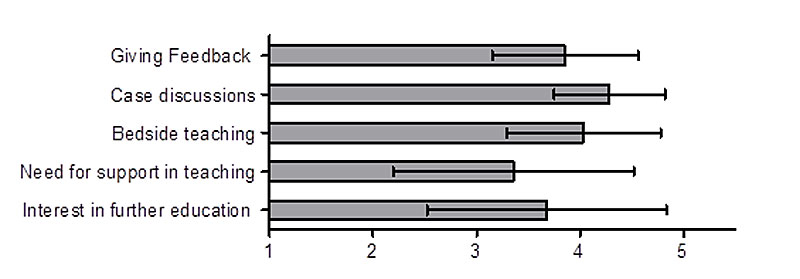
Self-estimated teaching competencies of the senior physicians
Self-estimated teaching competencies of the senior physicians and their need for support in clinical teaching and interest in further knowledge of the principles of medical education are summarised in figure 4. Senior physicians see their main teaching competencies in case discussions, bedside teaching and providing feedback. They expressed interest in obtaining further knowledge on principles of medical education, as well as a need for support in clinical teaching.
Impact of the length of working experience on the need for didactic support and interest in didactic education
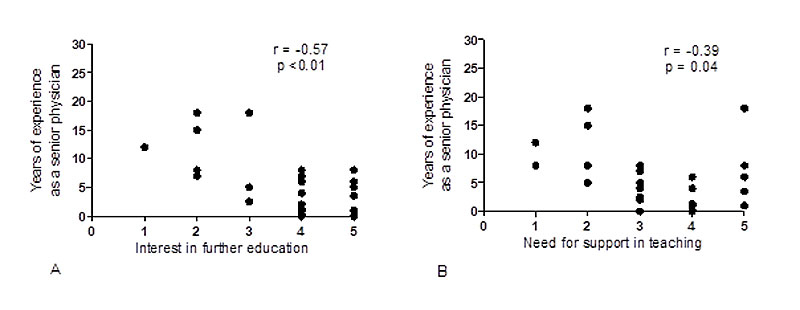
The length of professional experience in the position of a senior physician correlated negatively with the need for support in teaching and interest in further education (figure 5). We saw a similar correlation between total years of working experience and interest in further education (r = −0.6; p <0.001). The correlation was not significant in the case of total years of working experience and the need for support in teaching (data not shown).
Factors promoting a positive learning experience
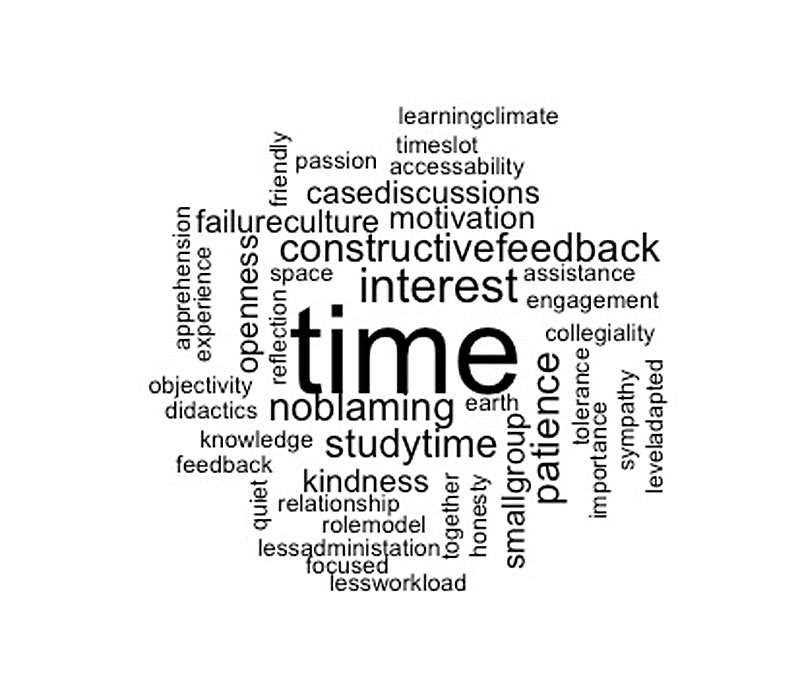
Twenty-nine of 48 (60.4%) residents answered the question on factors promoting a positive learning atmosphere. Content analysis brought up 51 different codes representing factors promoting a positive learning experience. Codes are visualised in figure 6, where the size of each word represents the number of mentions. Using an inductive process looking for similarities among the different codes, we finally identified 11 different categories. Table 3 gives an overview of the different categories, including the subsumed codes, as well as the weight of each category, representing the number of times each category was mentioned by the participants. The factor time and a positive attitude of the teacher were the most quoted factors promoting a positive learning environment. Furthermore, the motivation of the teacher, specific didactical method and setting (teaching in small groups, one-on-one teaching, quiet environment, smaller offices) were seen as important factors.
Table 3 Overview and weighting of factors that promote a positive learning atmosphere.
|
Categories and including codes of factors promoting a positive learning atmosphere
|
Weight*
|
Time
Protected time for teaching, defined timeslots, less workload, less administration |
18 |
Characteristics of a positive attitude of the teacher
Kindness, patience, reflection, objectivity, honesty, down-to-earthess, tolerance, friendliness, openness for questions and understanding of residents |
13 |
Motivation of the teacher
Motivation, engagement and passion of the supervisor; general interest in teaching; acknowledgment of the importance of teaching despite of workload |
8 |
Didactical method and setting
Teaching in small groups, 1:1 teaching, active participation, targeted learning, case discussions, need for self-directed learning, quiet environment, smaller offices |
8 |
No-blame culture
Open culture to cope with failure, no-blame culture, good learning climate |
6 |
Knowledge
Teachers as medical experts with didactic knowledge and experience in their field of work, readiness of mind |
5 |
Relationship
Collegiality, connectedness, good relationship with the supervisor |
4 |
Feedback
Constructive feedback |
4 |
| Self-directed learning |
3 |
Teaching adapted to the learners’ level
Teaching should be aligned to residents' knowledge and level of training |
2 |
| Role model |
1 |
Discussion
In our study, we present an overview of current teaching practice at the medical departments of the University Hospital Basel, Switzerland. We focused on the question of how physicians value different teaching formats for the professional development of medical expertise; we explored the self-estimated teaching competencies of the teaching faculty, and we analysed the residents’ view on factors promoting a positive learning environment.
Importance of different teaching forms for professional development of a medical expert
Both residents and senior physicians mostly agreed in their views on the benefits of different teaching formats for the professional development of medical experts. In general, they rated unstructured teaching initiatives (bedside teaching and teaching during case discussions) higher than structured teaching units (internal seminars, lectures, etc.). This is of particular interest, as the Swiss specialists training programmes governed by the SIWF explicitly request 4 hours of designated structured training per week in all accredited clinics, without defining the number of unstructured training units required [9].
It was evident that peer teaching was not seen as an essential teaching strategy by either group. This is in contrast to previous findings of Ramani and Ten Cate, who showed that peer teaching via residents plays a key role in the clinical education of peers and junior learners [10, 11]. One possible explanation of this discrepancy could be the current culture of peer teaching at our hospital. Junior physicians might perceive a lack of peer teaching as a results of senior physicians’ constant presence on the wards and close supervisory back-up for outpatient consultations. Nevertheless, peer teaching takes place in our daily routine, for example, in the form of the introduction of new colleagues on the wards and in the outpatient department. Moreover, junior physicians prepare structured teaching sessions such as journal clubs and case seminars.
Both groups of physicians rated providing feedback as highly important. However, unlike the senior physicians, residents rated evaluation of skills as the least important teaching strategy. As described by Watling et al., direct observation is fundamental to both trustworthy assessment and credible feedback [12]. For learners, being observed typically feels like being assessed [13]. We can assume that although the residents appreciate feedback, they dismiss evaluation of skills because they feel uncomfortable in an official evaluation setting. Another possibility is that our current practice of skills evaluation needs to improve. In both our internal medicine departments, we evaluate skills using mini-CEXs (mini-clinical evaluation exercises) and DOPS (direct observation of procedural skills) only to the extent required in the Swiss training programme for internal medicine. Therefore, we probably do not utilise the full potential of these tools as assessment instruments: we should use them more often, in a wide variety of clinical situations and skills, and by different supervisors.
Overall, our findings are in line with a systematic review on the diverse learner needs forming a basis of faculty development initiatives [4].
Frequency of different forms of clinical teaching
Residents had a perception of the frequency of applied teaching units in everyday work different from that of the senior physicians. This phenomenon has been described previously [14]. The everyday clinical work shapes the focus of teaching, even if it is not always apparent for the learner, and the boundaries between clinical work and teaching are often blurred. Thus, a gap in perceptions of teaching between teacher and learner may appear [15].
According to both residents and the senior physicians, teaching during case discussions seems to be the teaching form most often applied. This may be best explained by the fact that senior physicians stick to the teaching strategy they feel most competent in and prefer not to leave their comfort zone. Furthermore, a general shift in the setting of clinical teaching – away from the bedside towards the office in front of a computer – is apparent. In this setting, the teacher feels more in control and has prompt access to the results of diagnostic procedures [16].
Although receiving feedback is important to the residents, they reported obtaining it just occasionally, and our data showed a wide perception gap between the residents and senior physicians with regard to giving and receiving feedback. This is of particular interest given the utmost importance of effective feedback for the training of residents [17]. According to Archer et al. [18], feedback must be considered as a supportive, sequential process rather than a series of unrelated events. Therefore, repetitive and coordinated strategies on how to improve the quality, timing and perception of feedback must be established in the clinics.
Additionally, monitoring of activities of the learners are key elements in the professional development of medical experts. Noticing the sporadic performance of workplace-based assessments, i.e., mini-CEXs and DOPS in our clinics (mirrored by the perceived low importance by the residents), a well-structured feedback and assessment programme would address this deficit.
Another approach would be the implementation of Entrusted Professional Activities (EPAs) in the training of residents, a movement in medical education currently taking place at the national and international level in undergraduate and postgraduate settings [19–21]. In this context, a working group of SIWF is currently addressing questions arising during implemention of EPAs in the Swiss curriculum [22]. However, the introduction of EPAs alone will not counteract the lack of effective and regular feedback. Therefore, the faculty should be trained in their role as evaluators and in giving effective feedback.
Self-evaluation
Just under 60% of the faculty had attended some type of faculty development training, although supervision and instruction of residents and students is one of the primary responsibilities of the senior physicians. Self-estimated confidence in one’s own teaching competencies was highest for case discussions and lowest for giving feedback. However, the accuracy of self-assessment is known to be relatively weak. Additionally, we know from the literature that being a good clinician does not necessarily mean being a good teacher [23]. We did not explore why many faculty members had not yet had any teach-the-teacher training. Therefore, it is not easy to interpret these results.
Nevertheless, participants expressed their need for support in clinical teaching and a fundamental interest in medical education knowledge. This was particularly true for junior faculty members, but it was also evident for several very experienced faculty members. This is of particular interest as our observations are not in line with previous findings that novices tend to overestimate themselves [24].
Factors promoting a positive learning experience
Excellence in clinical teaching goes beyond medical expert knowledge; specifically, non-cognitive factors such as enthusiasm, communication skills and a positive teacher-learner relationship play an important role [23]. The results of our study are in line with these findings, and they even go beyond them. The time factor turned out to be by far the most frequently mentioned factor important for a positive learning environment, as a lack of time stands in the way of clinical lessons [19]. Clinical teaching is largely spontaneous and born out of opportunity [15, 25], and a variety of short effective strategies for clinical teaching in inpatient and outpatient settings is available [26, 27]. Faculty development programmes should address the time aspect by covering clinical teaching models, promoting teaching strategies in a busy working life [28] and improving clinical teaching skills [29].
There are several limitations of our study. Firstly, our data rely on self-assessment, which is prone to bias such as the social desirability bias. Secondly, although we assessed previous attendance by senior physicians at any faculty training programmes, we did not evaluate the influence on their teaching competencies. Thirdly, the evaluation of the frequency of teaching units was only a subjective assessment, which may bias the time estimate.
Despite these limitations, we present a unique overview of current teaching practice in the setting of a university hospital in Switzerland, based on the responses of a representative sample of residents and senior physicians. Our data lay the basis for designing future faculty development programmes at our institution. Based on our results, we will emphasise the benefits of peer teaching, assessment and feedback, focusing on workplace-based assessments. We will design the programme as a series of faculty development lunches at noon, easily accessible to all faculty members. Our approach may thus become a model for educators planning to introduce new educational concepts.
In conclusion, our study shows that many aspects of current teaching practice, although an integral part of the daily work at a university clinic, require a discussion of opportunities for adaptation and improvement. The assessment of current teaching practice forms the basis for designing a faculty development programme tailored to specific local needs.
Acknowledgments
The authors thank Dr Annina Vischer for creating the word-cloud in R.
References
1SIWF. Lernzielkatalog Allgemeine Lernziele für die Weiterbildungsprogramme. Available from: https://www.siwf.ch/files/pdf17/allg_lz_d.pdf [cited 2020 April 30].
2
Staff
YS
. Development for medical teachers. Clin Teach. 2005;2(2).
3
Audétat
MC
,
Dory
V
,
Nendaz
M
,
Vanpee
D
,
Pestiaux
D
,
Junod Perron
N
, et al.
What is so difficult about managing clinical reasoning difficulties?
Med Educ. 2012;46(2):216–27. doi:.https://doi.org/10.1111/j.1365-2923.2011.04151.x
4
Steinert
Y
,
Mann
K
,
Centeno
A
,
Dolmans
D
,
Spencer
J
,
Gelula
M
, et al.
A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 2006;28(6):497–526. doi:.https://doi.org/10.1080/01421590600902976
5
Bajwa
NM
,
De Grasset
J
,
Audétat
MC
,
Jastrow
N
,
Richard-Lepouriel
H
,
Dominicé Dao
M
, et al.
Training junior faculty to become clinical teachers: The value of personalized coaching. Med Teach. 2020;42(6):663–72. doi:.https://doi.org/10.1080/0142159X.2020.1732316
6
SurveyMonkey. Available from: https://www.surveymonkey.de/?cmpid=&cvosrc=&keyword=%2Bsurveymonkey&matchtype=b&network=g&mobile=0&searchntwk=1&creative=269466776838&adposition=1t1&campaign=60_Shared_Google_WW_German_Search_Brand_Beta&cvo_campaign=60_Shared_Google_WW_German_Search_Brand_Beta&cvo_adgroup=&dkilp=&cvo_creative=&utm_source=adwords&utm_medium=ppc&utm_content=269466776838&utm_adgroup=55623815952&utm_term=%2Bsurveymonkey&utm_bu=Core&utm_network=g&utm_campaign=1403489965&&gclid=EAIaIQobChMIl6nD8pHA4QIVTqqaCh3t9A-GEAAYASAAEgIdOvD_BwE.
7
Carifio
J
,
Perla
RJ
. Ten Common Misunderstandings, Misconceptions, Persistent Myths and Urban Legends about Likert Scales and Likert Response Formats and their Antidotes. J Soc Sci. 2007;3(3):106. doi:.https://doi.org/10.3844/jssp.2007.106.116
8
Elo
S
,
Kyngäs
H
. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–15. doi:.https://doi.org/10.1111/j.1365-2648.2007.04569.x
9FMH. Weiterbildungsprogram Facharzt für Allgemeine Innere Medizin [last revision 20 December 2018; cited 2019 April 7]. Available from: https://www.fmh.ch/files/pdf21/aim_version_internet_d.pdf.
10
Ramani
S
,
Mann
K
,
Taylor
D
,
Thampy
H
. Residents as teachers: Near peer learning in clinical work settings: AMEE Guide No. 106. Med Teach. 2016;38(7):642–55. doi:.https://doi.org/10.3109/0142159X.2016.1147540
11
Ten Cate
O
,
Durning
S
. Peer teaching in medical education: twelve reasons to move from theory to practice. Med Teach. 2007;29(6):591–9. doi:.https://doi.org/10.1080/01421590701606799
12
Watling
CJ
,
Ginsburg
S
. Assessment, feedback and the alchemy of learning. Med Educ. 2019;53(1):76–85. doi:.https://doi.org/10.1111/medu.13645
13
LaDonna
KA
,
Hatala
R
,
Lingard
L
,
Voyer
S
,
Watling
C
. Staging a performance: learners’ perceptions about direct observation during residency. Med Educ. 2017;51(5):498–510. doi:.https://doi.org/10.1111/medu.13232
14
Ramani
S
,
Krackov
SK
. Twelve tips for giving feedback effectively in the clinical environment. Med Teach. 2012;34(10):787–91. doi:.https://doi.org/10.3109/0142159X.2012.684916
15
Steinert
Y
,
Basi
M
,
Nugus
P
. How physicians teach in the clinical setting: The embedded roles of teaching and clinical care. Med Teach. 2017;39(12):1238–44. doi:.https://doi.org/10.1080/0142159X.2017.1360473
16
Peters
M
,
Ten Cate
O
. Bedside teaching in medical education: a literature review. Perspect Med Educ. 2014;3(2):76–88. doi:.https://doi.org/10.1007/s40037-013-0083-y
17
LaDonna
KA
,
Watling
C
. In search of meaningful feedback conversations. Med Educ. 2018;52(3):250–1. doi:.https://doi.org/10.1111/medu.13518
18
Archer
JC
. State of the science in health professional education: effective feedback. Med Educ. 2010;44(1):101–8. doi:.https://doi.org/10.1111/j.1365-2923.2009.03546.x
19
Michaud
PA
,
Jucker-Kupper
P
; The Profiles Working Group. The “Profiles” document: a modern revision of the objectives of undergraduate medical studies in Switzerland. Swiss Med Wkly. 2016;146:w14270. doi:.https://doi.org/10.4414/smw.2016.14270
20
Sohrmann
M
,
Berendonk
C
,
Nendaz
M
,
Bonvin
R
; Swiss Working Group For Profiles Implementation. Nationwide introduction of a new competency framework for undergraduate medical curricula: a collaborative approach. Swiss Med Wkly. 2020;150:w20201.
21Training Requirements for the Specialty of Internal Medicine: European Standards of Postgraduate Medical Specialist Training. Available from: https://www.uems.eu/__data/assets/pdf_file/0017/44450/UEMS-2016.13-European-Training-Requirements-Internal-Medicine.pdf2016 [cited 2021 March 17].
22
https://www.siwf.ch/siwf-projekte/epa.cfm [
23
Sutkin
G
,
Wagner
E
,
Harris
I
,
Schiffer
R
. What makes a good clinical teacher in medicine? A review of the literature. Acad Med. 2008;83(5):452–66. doi:.https://doi.org/10.1097/ACM.0b013e31816bee61
24
Cleary
TJ
,
Konopasky
A
,
La Rochelle
JS
,
Neubauer
BE
,
Durning
SJ
,
Artino
AR, Jr
. First-year medical students’ calibration bias and accuracy across clinical reasoning activities. Adv Health Sci Educ Theory Pract. 2019;24(4):767–81. doi:.https://doi.org/10.1007/s10459-019-09897-2
25
Williams
KN
,
Ramani
S
,
Fraser
B
,
Orlander
JD
. Improving bedside teaching: findings from a focus group study of learners. Acad Med. 2008;83(3):257–64. doi:.https://doi.org/10.1097/ACM.0b013e3181637f3e
26
Neher
JO
,
Gordon
KC
,
Meyer
B
,
Stevens
N
. A five-step “microskills” model of clinical teaching. J Am Board Fam Pract. 1992;5(4):419–24.
27
Wolpaw
TM
,
Wolpaw
DR
,
Papp
KK
. SNAPPS: a learner-centered model for outpatient education. Acad Med. 2003;78(9):893–8. doi:.https://doi.org/10.1097/00001888-200309000-00010
28
Chinai
SA
,
Guth
T
,
Lovell
E
,
Epter
M
. Taking Advantage of the Teachable Moment: A Review of Learner-Centered Clinical Teaching Models. West J Emerg Med. 2018;19(1):28–34. doi:.https://doi.org/10.5811/westjem.2017.8.35277
29
Ramani
S
. Twelve tips to improve bedside teaching. Med Teach. 2003;25(2):112–5. doi:.https://doi.org/10.1080/0142159031000092463