Figure 1 Sites of the SwissNOS panellists.
DOI: https://doi.org/10.4414/smw.2021.20501
In Switzerland, as in many European countries, there is no specific standard procedure for assessing “fitness-to-drive” of brain tumour patients. Brain tumour patients do not have to be reported to a Swiss Road Traffic Office (Strassenverkehrsamt, STVA) unless a physician considers them to be medically “unfit-to-drive” and not adhering to the advice to abstain from driving, or in the event of a traffic accident reported to the STVA. According to the Swiss Road Traffic Act (Strassenverkehrsgesetz, SVG, Loi fédérale sur la circulation routière, Legge federale sulla circolazione stradale) article 15, there is an explicit reporting right of the treating physician. Furthermore, the Swiss Road Traffic Act, articles 26 and 31, requires each road user to take personal responsibility.
The task of determining medical “fitness-to-drive” in patients with deficits caused by brain tumours falls primarily on the treating physician, although few have been formally trained in this area. Swiss guidelines exist for patients with seizures [1], which is an immediate reason for driving cessation. There are Swiss guidelines for other conditions that increase the risk for traffic accidents, such as visual impairments (minimum requirements are defined in the Verkehrszulassungsverordnung, VZV) [2] and daytime sleepiness [3], among others. Updated guidelines can be found on the following websites: https://www.uzh.ch/cmsssl/irm/de/downloads/vm/richtlinien.html
https://www.sgrm.ch/de/verkehrsmedizin/arbeitsgruppen/qm-verkehrsmedizin/
Cognitive requirements are mentioned in various parts of the Road Traffic Act (SVG), the Traffic Regulation (Verkehrsregelverordnung, VRV) and the Traffic Licensing Ordinance (Verkehrszulassungsverordnung, VZV), which describe minimum medical requirements for safe driving. However, they define the issue of neurocognition rather vaguely.
The Traffic Licensing Ordinance (VZV) lists 10 minimum medical requirements for “fitness-to-drive”, which are divided by areas of function (vision, psyche, cognition), and disease (neurological, cardiovascular and metabolic diseases, diseases of the respiratory and abdominal organs, diseases of the spinal column and the musculoskeletal system). A further requirement relates to centrally acting substances (recreational drugs, medicines). Hearing performance is no longer a criterion for “fitness-to-drive”.
Brain tumours may cause, among others, visual changes, motor and sensory deficits, headaches, malfunctioning of neurocognitive domains including delayed reaction time, attention deficits and seizures – all of which can impair a patient’s ability to drive safely. In daily practice, there is a paucity of published data on which to provide comprehensive evidence-based recommendations on when and how to intervene when patients with a brain tumour wish to resume driving.
To address this situation, 22 members of the interdisciplinary Swiss Neuro-Oncology Society (SwissNOS), one traffic physician and representative of the Swiss Society of Legal Medicine with Level 4 qualification (Institute of Legal Medicine, Zurich) and an electrocencephalogram (EEG) specialist were invited to participate in a modified Delphi process in April and in August 2020. The aim was to shed light on procedures used in daily practice and to agree on minimum requirements to determine “fitness-to-drive” for brain tumour patients in Switzerland. Glioblastoma, the most common and aggressive brain tumour, was selected in a first step as an appropriate candidate tumour that allows to study a relatively homogeneous brain tumour subtype with standardized intial care, a relatively uniform prognosis and a lower incidence of seizures than lower grade gliomas [4, 5]. Standard treatment of newly diagnosed glioblastoma consists of maximum safe resection, followed by chemo-radiotherapy for 3–6 weeks (depending on the age of the patient) and maintenance chemotherapy for 6 months [6, 7]. Median survival with current treatment is expected to be between 15 and 24 months, with deviations in both directions depending on molecular characteristics of the tumour [8]. Hereafter we refer to driving a car or motorcycle for personal purposes and exclude professional driving of, for example, trucks, buses or taxis.
At several meetings in 2019 and 2020, Swiss neuro-oncologists discussed common practices on how to advise patients with a stable (non-progressive) glioblastoma, who wish to resume driving after initial standard tumour treatment.
In a first step, a questionnaire with three inaugural questions and seven statements pertaining to “fitness-to-drive” for glioblastoma patients was distributed to 22 Swiss neuro-oncologists from all parts of Switzerland (fig. 1) and from different disciplines, encompassing neurologists (n = 10), neurosurgeons (n = 7), radiation oncologists (n = 2), medical oncologists (n = 3) and one traffic physician. Two neuropsychologists experienced in assessing “fitness-to-drive” proposed a standardised test battery covering the following domains: basic processing speed, attention, visuo-spatial perception, attention and executive functions. Furthermore, semi-standardised questions aimed at assessing driving experience, as well as possible behavioural and personality-related aspects (impulsiveness, risk behaviour, etc.). One EEG specialist was specifically questioned about the value of EEG to predict “fitness-to-drive”. Members of the Swiss Society for Legal Medicine (SGRM) were invited to comment on the procedures.
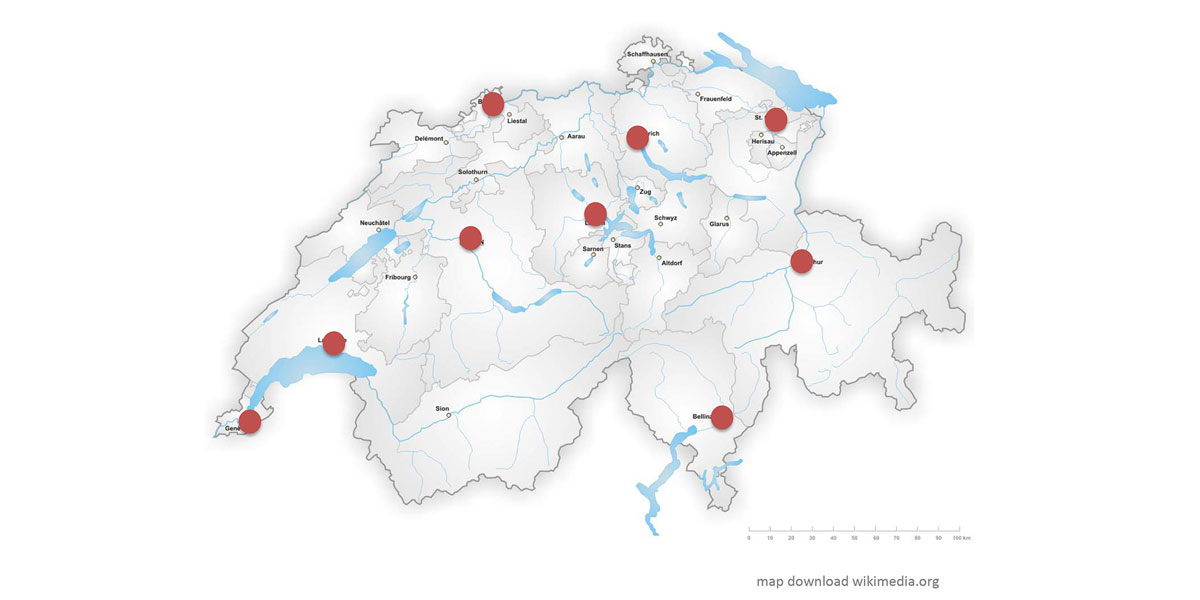
Figure 1 Sites of the SwissNOS panellists.
The following assessments considered to be useful to assess “fitness-to-drive“ were proposed in the survey, grouped into four main categories: (1) cranial magnetic resonance imaging (cMRI) at baseline (T0) and in the follow-up period; (2) clinical neurological examination, including a thorough history and an EEG at baseline, i.e., once prior to resuming driving (T0); (3) vision and (4) neuropsychological assessments focussing on driving capacities, both at baseline.
The seven statements of the modified Delphi survey read as follows:
In a further step, statements were compiled to frame a tentative Swiss guideline for glioblastoma patients, who wish to resume driving after completion of the initial standard treatment. In a last step, responses were compared with national and international recommendations for the respective items.
The first question of the survey on whether the treating physician would even consider “fitness-to-drive” assessments in a brain tumour patient was uniformly answered with yes. The question of an upper age limit or restrictions to certain type of roads was mainly denied (fig. 2).
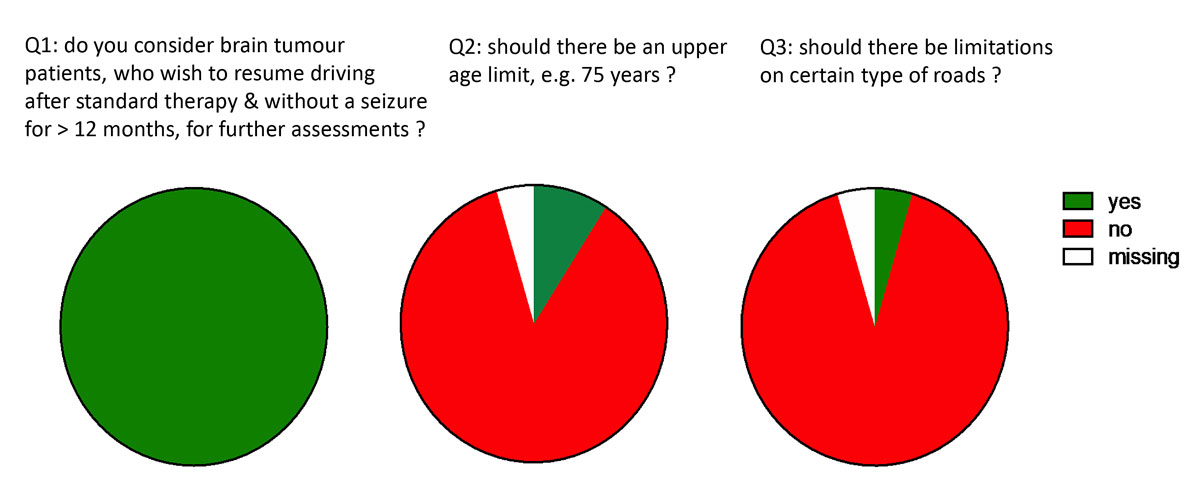
Figure 2 Inaugural questions. Proportion of agreement, panellists n = 23.
Tools that were considered necessary to assess “fitness-to-drive” after standard treatment of a glioblastoma are compiled in table 1. Consensus could be reached for a thorough history and neurological examinations at baseline and at each follow-up visit.
Table 1 Tools proposed to assess “fitness-to-drive”.
| Tools | Panellists (n = 23) |
|---|---|
| Thorough history and neurological examination at T0 and in follow-up | 23 yes, 0 no |
| EEG at T0 | 17 yes, 7* no |
| Cranial MRI at T0 | 22 yes, 1 no |
| Cranial MRI every 3 months during follow-up | 23 yes, 0 no |
| Visual fields and visual acuity at T0 | 16 yes, 7 no† |
| Neuropsychology at T0‡ | 14 yes, 9 no |
EEG = electrocencephalogram; MRI = magnetic resonance imaging; T0 = baseline, i.e., prior to resuming driving. *An EEG specialist was consulted for the EEG-specific question, therefore 24 panellists answered this question. † Panellists who voted “no” declared this assessment to be part of a thorough neurological examination without the need of a specialist. ‡ Neuropsychological tests with focus on “fitness-to-drive” as proposed by the two neuropsychologists
A baseline EEG without any history or clinical evidence of epilepsy was supported by two thirds of the respondents. There was consensus on baseline and regular follow-up imaging. Visual field examinations were considered by one third of the panellists as part of a thorough neurological examination and not in need of a specialist (i.e., an ophthalmologist). The same holds true for a neuropsychological assessment (table 1).
Criteria incompatible with driving for glioblastoma patients were discussed inconsistently among the panellists and are presented in table 2. Consensus could be reached for neurological deficits incompatible with driving, such as non-compensated palsies, neglect, altered consciousness and any visual field deficits. Epilepsy-specific potentials on EEG were considered as a contraindication to drive by 18 out of 24 panellists. The ones who voted against this statement asked for a more nuanced evaluation. Unreliability of a patient in terms of not adhering to the physician’s advice such as taking antiepileptic drugs, was considered by only 18 out of 23 panellists as incompatible with “fitness-to-drive”
Table 2 Criteria considered incompatible with driving.
| Criteria | Panellists ( n = 23) |
|---|---|
| Palsies, sensory disorders affecting driving, neglect, etc. | 23 yes |
| Epilepsy-specific potentials | 19 yes, 5* no |
| Cranial MRI; progressive disease (RANO) | 23 yes |
| Vision: any anopsy | 23 yes |
| Neuropsychology: attention deficits, neglect, etc. according to reccomendations of neuropsychologist | 21 yes, 2 no |
| Unreliability of patient | 18 yes, 5 no |
EEG = electrocencephalogram; MRI = magnetic resonance imaging. RANO = Response Assessment in Neuro-Oncology. *An EEG specialist was consulted for the EEG-specific question, therefore 24 panellists answered to this question.
There were some comments from the panellists outside the Delphi questionnaire, mainly dealing with medication such as opioids and adherence to antiepileptic drug treatment.
It was a strong wish of most panellists to harmonise the procedure for “fitness-to- drive” in Switzerland for all brain tumour patients and for patients with brain metastases.
It was well accepted that, following the investigations deemed necessary, a lead physician, usually a neurologist, who coordinates the tests, has to communicate the results to the patient and decisions on “fitness-to-drive” have to be documented in the patient’s file. Whether the patient has to sign a document remains controversial. The proposed follow-up examinations every 3 months in glioblastoma patients were unanimously accepted by the panellists.
Swiss guidelines exist for epilepsy and driving: “Fahreignung mit Epilepsie” [1] issued by the Verkehrskommission der Schweizerischen Liga gegen Epilepsie (Ligue Suisse contre l’Epilepsie, Lega Svizzera contro l’Epilessia., SLE). These guidelines also apply to brain tumour patients experiencing seizures. Repeat EEG recordings are clearly indicated in glioblastoma patients with a first symptomatic seizure, but this is not the case in seizure-free patients. Since these patients do not suffer from epilepsy according to the current ILAE (International League Against Epilepsy) diagnostic criteria (www.ilae.org/files/ilaeGuideline/Definition2014.pdf) the recommendations of the SLE do not apply and should not be applied. When an EEG is recorded in these patients, there is the possibility that it will show epileptiform discharges in the absence of clinical signs of epilepsy. At this point, neuro-oncologists have to decide whether they would declare the patient with a glioblastoma “fit -to-drive” despite the EEG abnormalities. This question is not answered by scientific evidence.
Requirements regarding vision and driving are regulated by law (Strassenverkehrsgesetz, SVG, Verordnung über die Zulassung von Personen und Fahrzeugen zum Strassenverkehr “Verkehrszulassungsverordnung”, VZV, Bundesamt für Strassen, ASTRA).
In contrast, there are no specific guidelines for brain tumour patients and driving in Switzerland. Internationally, there are a few guidelines for brain tumour patients and their treating physicians to guide “fitness-to-drive”.
In the UK, for instance, patients are not allowed to drive for 1 year after treatment of a World Health Organization (WHO) grade 1 or 2 glioma. The situation is usually reassessed after 1 year. The patients get their licence back as long as they are not having seizures or any disability that affects their ability to drive https://www.cancerresearchuk.org/about-cancer/brain-tumours/living-with/driving. However, in the UK, a patient with a WHO grade 3 glioma or a glioblastoma (WHO grade 4) is not allowed to drive for 2 years after initial treatment. This usually means 2 years after 9 months of initial standard therapy. Most glioblastoma patients in the UK, therefore, will never have the chance to resume driving. It is common for the Driver and Vehicle Licensing Agency (DVLA) to ask people with a brain tumour to surrender their licence. The return of this document is not by default, but the treating specialist is contacted, and decisions are made on an individual basis. If patients get their licence back, it may only be valid for a short period and the doctor's consent will be necessary for renewal.
German colleagues are guided by the “Begutachtungsleitlinien zur Kraftfahreignung”, a document regularly updated, revised and published online after approval by the Federal Ministry for Transport and Digital Infrastructure (www.bast.de). The German guidelines are a compilation of physical and/or mental handicaps that make people unable to drive or limit their driving ability. These guidelines are intended to ease the case-by-case evaluation of “fitness-to-drive” and serve as a reference tool for evaluators who have to judge driving licence applicants or holders with regard to their ability to drive. However, the 57-page document has no chapter devoted specifically to brain tumour patients.
Recently, Valencia-Sanchez et al. from the Mayo Clinic, Phoenix AZ, published their clinical evaluation of “fitness-to-drive” in patients with brain metastases [10]. The authors prospectively evaluated the concordance between neurology assessments in 41 individuals with brain metastases. The evaluation included an interview and neurological examination. Participants subsequently underwent an “occupational therapy driving assessment” during which a battery of objective measures of visual, cognitive, and motor skills related to driving was administered. There was poor association between the assessment by neurologists and the outcome of the test battery. The authors concluded that subtle deficits, which might impair the ability to drive safely, may not be evident on neurological examination alone and strongly recommend objective measures.
In order to obtain more evidence on whether and which assessments are complementary to increase road safety for brain tumour patients, we are currently conducting a prospective observational study with a cohort of glioblastoma patients who wish to resume driving after initial standard treatment (GLIODRIVE project design, fig. 3). First and foremost, it is worthwhile to plan the order of assessments according to minimum medical requirements and exclusion criteria, and to avoid unnecessary cost and burden for the patient. Four main test categories will be studied at baseline and compared with each other: (1) imaging (cMRI); (2) neurological examination, including a thorough history and an EEG; (3) examination of visual fields and acuity; and (4) neuropsychological evaluation focussing on safe driving. The research aims to confirm the feasibility of the proposed tools in daily practice and to compare outcome of the respective instruments in predicting “fitness-to-drive”, as well as matching results with events obtained from the Road Traffic Registry (Strassenverkehrsamt). An additional question of the study will be whether the patient's self-assessment correlates with events on the street.
Figure 3 GLIODRIVE Project (BASEC ID 2020-00365).
Provided that the study results prove useful, the concept can be expanded to other types of brain tumours and patients with brain metastases, preferably again in the context of an observational study.
In anticipation of study results, we propose tentative assessments that are currently agreed on by the SwissNOS panellists, in red with a consensus, in blue considered optional (fig. 4).
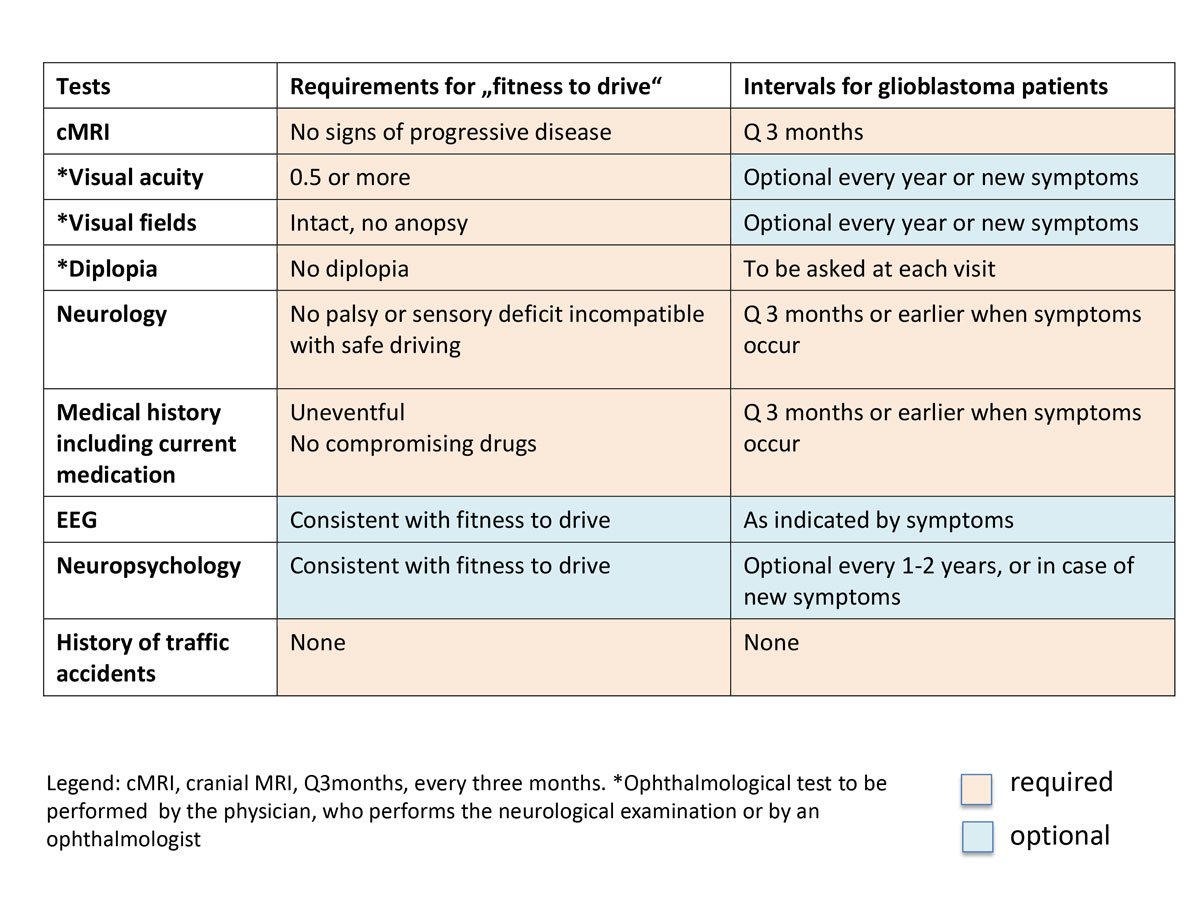
Figure 4 Proposed assessments for “fitness-to-drive” for glioblastoma patients.
There are no funding sources for this initiative. The authors declare that there are no conflicts of interest regarding the content of this paper.
Conception of the two Delphi surveys: HS
SwissNOS members participating in the Delphi surveys: HS, IL, RU, HG, HT, HC, LRE, VF, CD, NM, HA, MD, BB, LH, GD, RM, PGF, SP, WT, WHG, WF, RP, WM and Karl F. Kothbauer, Lucerne (deceased)
Swiss Society for Legal Medicine: KK
Conception and design of the GLIODRIVE Project: HS, LD, FI, RU, EN, PT
1 Arnold P , Bonetti C , Mathis J , Meyer K , Seeck M , Seeger R , et al. Fahreignung mit Epilepsie. Swiss Med Forum. 2019;19(4546):737–40. doi:.https://doi.org/10.4414/smf.2019.08402
2 Mérour A , Favrat B , Borruat F-X , Pasche C . [Requirements on vision for driving: to see more clearly]. Rev Med Suisse. 2014;10(452):2252–4, 2256–7. [Article in French.]
3 Mathis J , Kohler M , Hemmeter UM , Seeger R . Verkehrskommission Schweizerische Gesellschaft für Schlafforschung, Schlafmedizin und Chronobiologie (SGSSC). Fahreignung bei Schläfrigkei. Swiss Med Forum. 2017;17(20):442–7. doi:.
4 van Breemen MSM , Wilms EB , Vecht CJ . Epilepsy in patients with brain tumours: epidemiology, mechanisms, and management. Lancet Neurol. 2007;6(5):421–30. doi:.https://doi.org/10.1016/S1474-4422(07)70103-5
5 Skardelly M , Brendle E , Noell S , Behling F , Wuttke TV , Schittenhelm J , et al. Predictors of preoperative and early postoperative seizures in patients with intra-axial primary and metastatic brain tumors: A retrospective observational single center study. Ann Neurol. 2015;78(6):917–28. doi:.https://doi.org/10.1002/ana.24522
6 Weller M , van den Bent M , Preusser M , Le Rhun E , Tonn JC , Minniti G , et al. EANO guidelines on the diagnosis and treatment of diffuse gliomas of adulthood. Nat Rev Clin Oncol. 2021;18(3):170–86. doi:.https://doi.org/10.1038/s41571-020-00447-z
7 Roth P , Hottinger AF , Hundsberger T , Läubli H , Schucht P , Reinert M , et al. A contemporary perspective on the diagnosis and treatment of diffuse gliomas in adults. Swiss Med Wkly. 2020;150:w20256 .https://doi.org/10.4414/smw.2020.20256
8 Gramatzki D , Roth P , Rushing EJ , Weller J , Andratschke N , Hofer S , et al. Bevacizumab may improve quality of life, but not overall survival in glioblastoma: an epidemiological study. Ann Oncol. 2018;29(6):1431–6. doi:.https://doi.org/10.1093/annonc/mdy106
9 Wen PY , Macdonald DR , Reardon DA , Cloughesy TF , Sorensen AG , Galanis E , et al. Updated response assessment criteria for high-grade gliomas: response assessment in neuro-oncology working group. J Clin Oncol. 2010;28(11):1963–72. doi:.https://doi.org/10.1200/JCO.2009.26.3541
10 Valencia-Sanchez C , Gorelkin VC , Mrugala MM , Sharma A , Vora SA , Ashman JB , et al. Clinical evaluation of fitness to drive in patients with brain metastases. Neurooncol Pract. 2019;6(6):484–9. doi:.https://doi.org/10.1093/nop/npz027
There are no funding sources for this initiative. The authors declare that there are no conflicts of interest regarding the content of this paper.