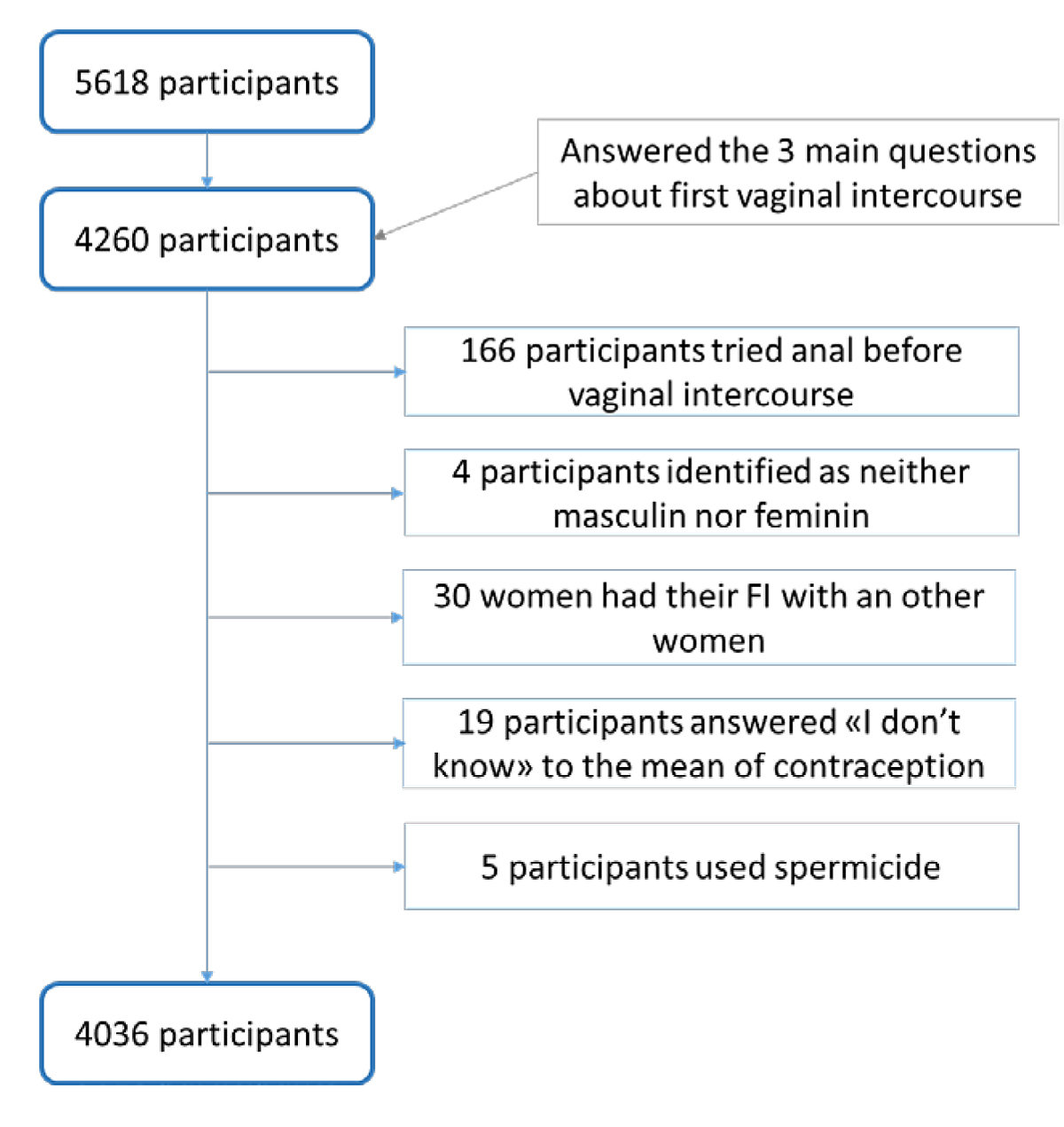
Figure 1 Study flow diagram. FI = first intercourse
DOI: https://doi.org/10.4414/smw.2021.20509
According to the World Health Organization [1], adolescence is a crucial and transitional period of the human life and an important period to learn about dealing with emotions and relationships. This phase is particularly delicate as the youth is confronted with the adult world while still developing biological and psychosocial maturity. Sexuality plays an important role in an individual’s life, and especially in adolescents’, as most begin their sexual activity at that period. Furthermore, encouraging young people to practice safe sex is a major public health challenge. The study of adolescent behaviour, especially in the sexuality field, is relevant as it can have consequences not only during this period but also over the life course [1].
In most western countries, the median age at first intercourse is 17 years [2]. Nevertheless, we observe divergences between countries in the abortion and delivery rates, suggesting differences in the use of contraception [2], cultural context and health policies. Good practice and knowledge of contraception at first intercourse may lead the adolescent to a safer sexual life. When talking about contraception, one should distinguish its two different effects, the contraception part, preventing unwanted pregnancies, and the protection part preventing sexually transmitted infections (STIs) provided only by condom use. Most studies [3–6] investigating the context of first intercourse are primarily interested in the use of a reliable contraceptive (condom, copper intrauterine device [IUD] and hormonal contraception [pill, implant, IUD or injection]). Even though studies may vary in terms of population type, age range and contraception type, the percentages of contraception use at first intercourse vary from one country to another. These rates fluctuate between 28.6% among Vietnamese youths [7] to almost 90.5% among Scandinavian women [3, 8–10]. A previous study in Switzerland, conducted in 1996 found a rate of contraception use of 86% among youths [11]. Studies investigating first intercourse context have found some factors that decrease the use of contraception: a younger age at coitarche [3, 10–15], an older partner for girls [3, 11–13], being in a casual relationship rather than a steady one [11, 13], smoking initiation before first intercourse [3, 12] and a lower educational level [10, 12–16]. The context in which the adolescent grew up was also found to have an influence: a lower socioeconomic family status decreases the odds of using contraception [10], whereas having a two-parent household increases it [13]. Further, access to sex education and knowledge of contraceptive methods is known to increase the use of contraception [8, 13, 14, 16–19].
To date, studies have mainly focused on women when investigating contraception use [3, 8, 10, 12, 13, 17, 18], or studied only condom use when addressing both genders [7, 15]. We found few articles that included both genders and all the main means of contraception [11, 14, 19], and none were published in the last 10 years. Furthermore, studies usually addressed the age at first intercourse and only a few variables influencing contraception use. The aim of this study is to determine the rate of contraception use at first intercourse and to identify its associated variables among youths living in Switzerland. The present study adds to the current knowledge by offering a more in depth overview of youth use of contraception at first intercourse. This was achieved through a large selection of variables, the fact that we address both males and females and that we have considered a wide range of contraceptive means.
Data were collected in 2017 as part of a Swiss national study on sexual health and behaviours [20]. This study provided self-reported information about sexual and reproductive health among young adults aged 24–26 years on the 30 September 2016. This age range was selected in order to ensure that the majority of the participants would be sexually active and, at the same time, sufficiently young to be able to recall accurately the beginning of their sexual life. The Federal Statistical Office provided the initial sample that was representative of the Swiss resident population in terms of sex, language (French, Italian or German) and canton of residence. We obtained their postal addresses, and an invitation letter was sent with a unique randomly created code to enter the online survey. The response rate was 15.1%. The final sample included 7142 participants (mean age 26.3 when completing the survey). To correct a slight overrepresentation of females from the French speaking part of Switzerland, analyses were weighted by gender and canton of residence. Data were collected using a life history calendar approach, a method that facilitates recall of past events [21, 22]. In the life history calendar, participants were asked to identify the occurrence of different key events in their life such as moving to a new residence or finishing school. Therefore, other personal events could be placed in time by referencing it to milestones in their life. Ethics clearance in agreement with Swiss law was given by the ethics committee in research of the canton of Vaud. A detailed description of the survey methodology can be found elsewhere [20].
A total of 4260 participants answered the three following questions and were included in our study “Have you ever experienced vaginal intercourse?”, “At what age did you experience vaginal intercourse for the first time” and “Which contraception and/or protection did you and/or your partner use during your first intercourse?” (fig. 1).
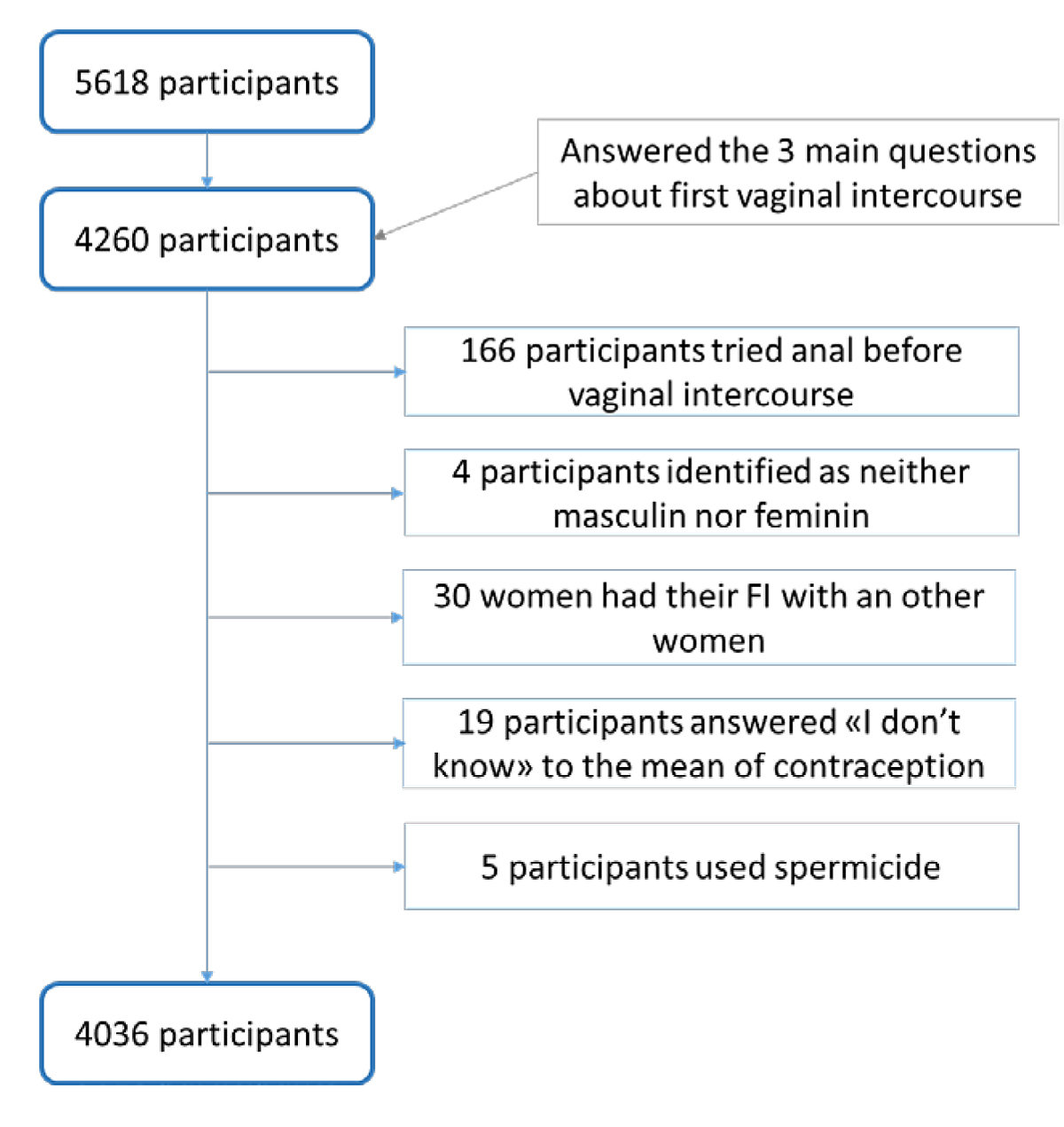
Figure 1 Study flow diagram. FI = first intercourse
The means of contraception was sought through a question with multiple possible answers including: nothing, male condom, female condom, contraceptive pill, hormonal vaginal ring, contraceptive patch, hormonal implant or injection, hormonal or copper intrauterine device, spermicides, withdrawal, natural methods (temperature, calendar), other (with free text option) and I don’t know. The contraceptive methods were then assorted into three categories. The first one, “Condom”, consisted of barrier methods (female and male condom), the second one, “Contraceptive”, included the highly effective contraceptives (pill, vaginal ring, IUD, implant and injection), the third category, “Non-Use”, consisted of non-use and low effective methods (withdrawal, natural methods) [2]. We decided to focus on first heterosexual vaginal intercourse owing to differences in terms of contraception needs in anal or same sex intercourse. Because of the structure of the survey, the question about which means of contraception was used during first intercourse was not directly linked with the questions on either vaginal or anal first intercourse. Therefore, we could not assume if participants thought it concerned their first vaginal or anal experience. In order to eliminate this bias, we decided to analyse only participants who had experienced vaginal intercourse before anal intercourse, excluding 166 persons. Those 166 individuals were similar to the included participants in terms of age (mean age at time of survey 26.31 ± 0.007 years), but differed in terms of gender (83.6% males).We decided to remove 4 individuals who identified themselves as neither masculine nor feminine and 30 women who had their first vaginal intercourse with another woman. The 19 participants who answered, “I don’t know” to the question on means of contraception were removed from the analysis. We also decided to remove 5 persons who used spermicide because it could not be considered as a highly effective contraceptive but also could not be included in the Non-Use category [2]. All free text answers were recoded into the previous categories. We decided to assimilate the 1445 (36.5%) participants who had used a condom and a contraceptive method at the same time in the Condom group as all were protected against sexually transmitted infections (STIs) and unwanted pregnancies. Nevertheless, we compared both groups (Condom Only and Condom and Contraceptive) and there were no differences regarding gender, age, age at first intercourse, socioeconomic status or living in a Catholic canton. However, those in the condom only group were less likely to live in the German-speaking part of Switzerland or in a rural area (data not shown). The final sample consisted of 4036 participants (mean age at the time of the survey 26.35 ± 0.01 years; 48% males) who were divided into the three groups: Condom (n=3488; 86.4%), Contraceptive (n=334; 8.3%) and Non-Use (n=214; 5.3%).
Participants were able to choose the answer “I don’t know” in various questions, these were then removed from the analysis. Sociodemographic characteristics included: gender, birth place of participant (Switzerland/other) and parents (at least one born in Switzerland/other), place of residence (urban/rural), attained education level (tertiary/below), family structure (parents together / not together), perceived family socioeconomic status at the age of 15 (dichotomised into average or above versus below average, 1.35% answered “I don’t know”) [23] and perceived puberty onset (advanced / on time / delayed) [24]. As society norms and religious practice may have an impact on contraception use and knowledge [25], we distinguished Swiss cantons that are historically Catholic from the other cantons (Protestant or bi-confessional) [26]. The main resource of sex education was grouped into school versus other resources [27], as it is the main resource in Switzerland and the most frequently studied worldwide. The episodes of alcohol drunkenness, and the consumption of tobacco, cannabis and other drugs before the age of first intercourse were analysed.
Characteristics and context related to the first vaginal intercourse were inquired by the following questions: age at first vaginal sex, context of the relationship (steady/casual), age of the partner (younger or same age vs older), and if it was the first sexual experience of the partner (yes/no, 2.47% answered “I don’t know”). We also inquired if the first intercourse happened while the participant was “under the influence of alcohol or drugs”. We asked participants to report their reaction to their first vaginal experience in terms of later regrets and possible answers were: “I should not have done it”, “I should have waited longer”, “I should not have waited so long” and “It was the right moment”, dichotomised into right moment versus all the others, 9.35% answered “I don’t know”. We also obtained their perception of their first intercourse, dichotomised into unpleasant or other (pleasant and neutral, 2.75% answered “I don’t know”).
All exclusions made from the initial sample mentioned above were pre-specified.
First we ran a bivariate analysis comparing the three groups. We used chi-square tests for categorical variables and analysis of variance (ANOVA) for continuous ones. Then, statistically significant variables were entered into a multinomial regression analysis using the Condom group as the reference category. Results are given as relative risk ratios (RRRs) with 95% confidence intervals.
We used STATA 14.0 (StataCorp, College Station, TX, USA) for all the analyses, with a significance level of p <0.05.
Participants had their first intercourse at a mean age of 17.62 (± 0.05) years. Overall, 3490 (86.4%) participants used a condom with or without contraceptive, 334 (8.3%) used a contraceptive method only and 214 (5.3%) did not use any contraception.
Table 1 Bivariate analysis of sociodemographic and personal characteristics according to contraception used at first intercourse
| Variables |
Condom (%)
n = 3488 (86.4%) |
Contraceptive (%)
n =334 (9.6%) |
Non-Use (%)
n = 214 (5.3%) |
p-Value |
|---|---|---|---|---|
| Sociodemographic and personal | ||||
| Mean age at study time (years) ± SD | 26.35 ± 0.02 | 26.35 ± 0.05 | 26.38 ± 0.06 | 0.627 |
| Gender (male) | 47.65 | 45.49 | 52.42 | 0.3033 |
| Family SES (below average) | 14.87 | 9.33 | 23.33 | <0.01 |
| Birth place (foreign) | 10.75 | 10.65 | 17.07 | <0.05 |
| Parents birth place (2 parents foreign born) | 15.82 | 13.67 | 21.93 | <0.05 |
| Parents situation (together) | 64.66 | 74.64 | 59.00 | <0.01 |
| Residence (urban) | 54.14 | 52.56 | 54.35 | 0.8634 |
| Canton of residence (Catholic) | 22.65 | 17.10 | 24.68 | <0.05 |
| Education level (tertiary) | 52.87 | 54.87 | 51.23 | 0.703 |
| Main sex-education resource (school) | 16.78 | 17.65 | 21.04 | 0.2894 |
| Perceived timing of puberty | ||||
| – Advanced | 27.14 | 25.13 | 29.69 | 0.8173 |
| – On time | 44.18 | 44.58 | 43.64 | |
| – Delayed | 28.66 | 30.29 | 26.67 | |
| Substance consumption before first intercourse | ||||
| Smoking | 27.45 | 30.43 | 29.11 | 0.4925 |
| Drunkenness episode | 72.86 | 73.96 | 65.09 | <0.05 |
| Cannabis use | 38.19 | 40.22 | 40.67 | 0.6308 |
| Other drugs use | 2.56 | 2.83 | 2.62 | 0.9599 |
| Factors directly linked to first intercourse | ||||
| Mean age at first intercourse (years) ± SD | 17.56 ± 0.05 | 17.44 ± 0.18 | 17.35 ± 0.25 | 0.176 |
| Type of relationship with partner (steady) | 69.60 | 79.98 | 57.36 | <0.01 |
| Age of partner (older) | 37.37 | 31.97 | 41.73 | 0.0587 |
| Partner experience (first time too) | 40.98 | 41.04 | 34.51 | 0.2058 |
| Under the influence of alcohol or drugs (yes) | 2.55 | 2.27 | 8.31 | <0.01 |
| Type of experience (unpleasant) | 18.84 | 14.11 | 17.22 | 0.0886 |
| Perceived timing (not good) | 22.80 | 20.87 | 39.11 | <0.01 |
SES = socioeconomic status
We found that family socioeconomic status, being born in Switzerland, having at least one parent born in Switzerland, having parents who are together and living in a Catholic canton had a significant association with the contraception choice at first intercourse. The Non-Use group was associated with characteristics often considered as an indicator of vulnerability. The only substance that had an association with the contraception choice at first intercourse was alcohol misuse. No gender differences were found among the groups
The mean age at first intercourse was 17.6 years for Condom, 18.4 years for Contraceptive and 17.4 years for Non-Use. The type of relationship with partner, being under the influence of drugs or alcohol during first intercourse and deeming that first intercourse happened at the right time all had a significant association with the choice of contraception at first intercourse. A trend (p = 0.0587) towards contraception non-use was found when the partner was older.
Table 2 Multivariate analysis of sociodemographic and personal characteristics by contraception used at first intercourse.
| Variables |
Contraceptive
RRR (95% CI) |
Non-Use
RRR (95% CI) |
|---|---|---|
| Gender (male) | 0.95 (0.74–1.24) | 1.38 (0.96–1.86) |
| Mean age | 0.99 (0.86–1.15) | 0.98 (0.81–1.19) |
| Family SES (below average) | 0.59* (0.39–0.90) | 1.35 (0.90–2.04) |
| Birth place (foreign) | 1.41 (0.82–2.42) | 1.21 (0.65–2.27) |
| Parents birth place (2 parents foreign born) | 0.71 (0.44–1.15) | 1.31 (0.75–2.27) |
| Parents situation (together) | 1.52** (1.14–2.02) | 0.88 (0.62–1.25) |
| Canton of residence (Catholic) | 0.71* (0.52–0.97) | 1.45* (1.01–2.08) |
| First drunkenness episode before age of first intercourse (yes) | 1.06 (0.80–1.42) | 0.61** (0.42–0.88) |
| Mean age at first intercourse | 1.08** (1.03–1.13) | 0.98 (0.91–1.05) |
| Type of relationship with partner (casual) | 0.54** (0.38–0.77) | 1.60* (1.10–2.33) |
| First intercourse under the influence of alcohol or drugs (yes) | 0.77 (0.23–2.57) | 2.94** (1.49–5.81) |
| Perceived timing of first intercourse (not good) | 1.09 (0.79–1.51) | 1.80** (1.26–2.55) |
CI = confidence interval; RRR = relative risk ratio; SD = standard deviation; SES = socioeconomic status * p <0.05, ** p <0.01
Compared with participants in the Condom group, those in the Contraceptive group were less likely to belong to a below average socioeconomic status family (RRR 0.59) and to live in a Catholic canton (RRR 0.71) and more likely to have parents living together (RRR 1.52). They were also more likely to be older (RRR 1.08) and their first intercourse was less likely to have taken place in the context of a casual relationship (RRR 0.64).
Compared with participants in the Condom group, those in the Non-Use group were significantly more likely to live in a Catholic canton (RRR 1.45), and less likely to have ever had a drunkenness experience before their first intercourse (RRR 0.61). They were more likely to have had their first intercourse in the context of a casual relationship (RRR 1.60), to have been under the influence of alcohol or drugs during first intercourse (RRR 2.94) and more likely to judge their first intercourse as not having occurred at the right time (RRR 1.80). We found a trend for males to be overrepresented in this group (p = 0.056).
Our main outcome is that 94.7% of the young adults living in Switzerland used some type of contraception for their first intercourse. Out of this rate, 86.4% used the best possible protection by adopting a condom with or without another contraceptive, thus being protected both against STI and unwanted pregnancy. Only 5.3% of participants did not use any form of contraception. These rates are better than those reported in 1996 in Switzerland, where non-users were 13% [11] and in other countries where non-use ranged from 9.5% among Danish women to 71% among Vietnam youths [3, 7–10].
On the downside, characteristics associated with population vulnerability are still linked to non-use of contraception. In our study, individuals from low income families, who were foreign-born, who had two foreign-born parents or parents not together anymore were more at risk of not using any contraception during first intercourse. In contrast, we found no influence of the level of education, although the literature suggests that women with a higher level of education [3, 10] are more likely to use contraception. We found no data in the literature for males.
Regarding factors related to the context, participants in the CONTRACEPTIVE group were older and more likely to be in a steady relationship at first intercourse. These findings are certainly linked, as participants may have waited to be in a steady relationship to have their first intercourse, and had more time to plan long-term contraception. We hypothesise that a steady relationship leads to knowing and trusting the partner better. In this context, participants may think that there is no need for STI prevention, thus privileging pregnancy prevention only. On the other side, we note an increase of non-use of contraception among individuals engaged in casual relationships. This is a more concerning outcome, because of the risks these individuals have of contracting infectious diseases. Studies looking at first intercourse [13] or adolescent sexuality in general [28], found similar results that linked a casual relationship with non-use of a condom. We can assume that in the context of a casual relationship it is more difficult to discuss contraception with the partner, because of the immediacy of the situation. A study looking at relationship context [13] suggested that individuals in a closer relationship were more aware that their relationship may become sexual, and might be more prepared for a sexual encounter. Women can take the pill or another contraceptive means on their own, whereas they might need to negotiate with their male partner in order to use a condom [29, 30], and to do so they need to have time and space to discuss it with him, which might not be the case in a casual setting. Furthermore, women might suffer from the fear of getting a promiscuous reputation for carrying a condom or requiring condom use, as reported by participants in a New Zealand qualitative study [31]. On the subject of decision making on contraceptive use, a study looking at 33 countries [32] showed that higher gender equality in societies leads to a higher rate of contraception use, by enabling women to take a more active role in the contraception decision-making process.
We found a difference between Catholic and other cantons. In Catholic cantons participants were more likely to not use any contraception and less likely to use a contraceptive only. This might be explained by differences in cultural background and sexual education, which might be more conservative in Catholic regions, as Catholicism is one of the strictest religions in terms of contraception use [33]. This cultural difference may lead to a general disapproval of adolescent sexual activity and a lack of sex education causing adolescents to not plan their first intercourse. A study looking at European countries [25], found that the highest rates of contraceptive use among 15-yearolds were in the non-Catholic countries.
We found that participants who were under the influence of drugs or alcohol during their first intercourse were largely less likely to have used any type of contraception. This may be due to impaired autonomy or decision making due to the drug taken. We might also imagine that individuals from Catholic cantons, who may not be proud of having had their first intercourse because of the cultural context, try to justify it by saying they were intoxicated and, in consequence, not responsible. Regarding the influence of alcohol misuse before the age of the first intercourse, we found that participants who had non-use of contraception at first intercourse had a higher chance of never having had any episode of drunkenness before the age of their first intercourse, which might seem counterintuitive. We did not find any study linking alcohol consumption before first intercourse to contraception use. A study looking at adolescent sexual intercourse in general [25] found that drunkenness episodes were linked with non-use of a condom. The reason why our results diverge might be explained by the fact that most (72.5%) of our participants had an episode of drunkenness before the age of first intercourse. Such a rate makes drunkenness episodes normative and therefore might no longer be an indicator of risk behaviour. We can also suppose that this result is linked to the overrepresentation of residents from Catholic cantons in the NON-USE group who are less inclined to alcohol drunkenness because of their Catholic beliefs and norms [34].
We found a non-significant relationship in the non-use of contraception when the partner was older than the subject in both genders. Other studies have noted a link between non-use of contraception and the age of a woman’s partner [3, 12], assuming that an older male partner could have more influence on contraception use because of the woman’s inexperience, thus choosing not to use contraception [12]. No studies were found on the influence of an older partner in men’s choice of contraception, but here it seems that they might as well be influenced by it.
Among all groups, a large majority of participants felt that their first intercourse happened at the right time and this was linked with an increased rate of contraception use. Again, this result may be explained by the fact that youths who had planned and thought about that step in their life before its occurrence would be more likely to use contraception and not regret their choice.
The strength of this study is the sample size. Even though the response rate was low (15.1%) for the overall study, it is still a very large representative sample of young adults living in Switzerland. Moreover, data were weighted by gender and canton of residence to ensure the representativeness of this population. Secondly, unlike most studies we considered both genders and all types of contraception.
However, some limitations need to be put forward. First, the response rate was low, even though this rate is similar to the 20% rate reported in a Danish survey using almost exactly the same methodology [35]. The fact that sexual health and behaviour is a sensitive theme and that potential participants may not be at ease answering through the web (even if it was secured) could be an explanation, as surveys using other data collection techniques such as face-to-face interviews [36] or paper-based questionnaires, web questionnaires or phone interviews [3] reached much higher response rates (73% and 60%, respectively). Moreover, as the Federal Statistical Office collects only postal addresses in its population register, we could only contact participants though postal mail and having to connect to the website and introduce a code might have reduced the likelihood to answer compared to having received the invitation electronically. Additionally, the survey was launched just before the Swiss summer holidays, which might also have reduced the response rate. For these reasons, we decided to start with a very large sample so that the final one would be large enough for statistical purposes. Second, we asked participants with a mean age of 26.3 years to remember their first intercourse. It is possible that we have faced some recall bias, although asking the question at the age of 26 gives them an important temporal perspective. As explained in the methods, we tried to minimise the recall bias by using the life history calendar approach [21, 22]. Third, this was a cross sectional study and no causation can be inferred. Nevertheless, although it was cross-sectional, these retrospective data allowed us to identify events that happened before or after first intercourse, and to explore its context. Fourth, it may be that respondents were individuals more interested in responding to a sexual behaviour survey, and we cannot exclude a response bias.
We found that most of the Swiss resident youths used contraception at their first intercourse. This result is good news for the health of young people living in Switzerland. Moreover, this confirms the importance and the success of campaigns on safe sex, and the need to perpetuate them and continue the efforts in terms of communication, demystification and knowledge on contraception use. Nevertheless, we should still be attentive to paying special attention to people from the most vulnerable strata of the population who are at risk of lower use. It may be necessary to address a particular message to youth, advising them to think ahead about their contraception choice in order to be prepared, as it may happen more quickly than they think. For this, continuous sex education from early age is a great opportunity. We hope that this will help increasing the rate of contraception use in the setting of casual relationships and for intercourse while intoxicated.
This study was funded by the Swiss National Science Foundation [grant 162538].
The authors declare that they have no conflict of interest.
1World Health Organization (WHO). Adolescent development. Available from : https://www.who.int/maternal_child_adolescent/topics/adolescence/development/en/ [cited 2019 Nov 18].
2 Apter D . Contraception options: Aspects unique to adolescent and young adult. Best Pract Res Clin Obstet Gynaecol. 2018;48:115–27. doi:.https://doi.org/10.1016/j.bpobgyn.2017.09.010
3 Guleria S Juul KE Munk C Hansen BT Arnheim-Dahlström L Liaw KL Contraceptive non-use and emergency contraceptive use at first sexual intercourse among nearly 12 000 Scandinavian women. Acta Obstet Gynecol Scand. 2017;96(3):286–94. doi:.https://doi.org/10.1111/aogs.13088
4 Guleria S Thomsen LT Munk C Nygård M Hansen BT Elfström KM Contraceptive use at first intercourse is associated with subsequent sexual behaviors. Contraception. 2019;99(4):217–21. doi:.https://doi.org/10.1016/j.contraception.2018.12.006
5 Wang MY Temmerman M Zhang WH Fan Y Mu Y Mo SP Contraceptive and reproductive health practices of unmarried women globally, 1999 to 2018: Systematic review and meta-analysis. Medicine (Baltimore). 2020;99(49):e23368. doi:.https://doi.org/10.1097/MD.0000000000023368
6 Palmer MJ Clarke L Ploubidis GB Wellings K . Prevalence and correlates of ‘sexual competence’ at first heterosexual intercourse among young people in Britain. BMJ Sex Reprod Health. 2019;45(2):127–37. doi:.https://doi.org/10.1136/bmjsrh-2018-200160
7 Do TH Le LC Burgess JA Bui DS . Determinants of condom use at sexual debut among young Vietnamese. Int J Adolesc Med Health. 2014;26(3):403–10. doi:.https://doi.org/10.1515/ijamh-2013-0322
8 Hersh AR Saavedra-Avendaño B Schiavon R Darney BG . Sexuality Education During Adolescence and Use of Modern Contraception at First Sexual Intercourse Among Mexican Women. J Adolesc Health. 2019;65(5):667–73. doi:.https://doi.org/10.1016/j.jadohealth.2019.05.028
9 Moreira LR Dumith SC Paludo SDS . Uso de preservativos na última relação sexual entre universitários: quantos usam e quem são? [Condom use in last sexual intercourse among undergraduate students: how many are using them and who are they?] Cien Saude Colet. 2018;23(4):1255–66. doi:.https://doi.org/10.1590/1413-81232018234.16492016
10 Lee J Berenson AB Patel PR . Characteristics of Females Who Use Contraception at Coitarche: An Analysis of the National Survey of Family Growth 2006-2010 Database. J Womens Health (Larchmt). 2015;24(12):972–7. doi:.https://doi.org/10.1089/jwh.2015.5219
11 Narring F Wydler H Michaud PA . First sexual intercourse and contraception: a cross-sectional survey on the sexuality of 16-20-year-olds in Switzerland. Schweiz Med Wochenschr. 2000;130(40):1389–98.
12 Svare EI Kjaer SK Thomsen BL Bock JE . Determinants for non-use of contraception at first intercourse; a study of 10841 young Danish women from the general population. Contraception. 2002;66(5):345–50. doi:.https://doi.org/10.1016/S0010-7824(02)00333-5
13 Manning WD Longmore MA Giordano PC . The relationship context of contraceptive use at first intercourse. Fam Plann Perspect. 2000;32(3):104–10. doi:.https://doi.org/10.2307/2648158
14 Wellings K Nanchahal K Macdowall W McManus S Erens B Mercer CH Sexual behaviour in Britain: early heterosexual experience. Lancet. 2001;358(9296):1843–50. doi:.https://doi.org/10.1016/S0140-6736(01)06885-4
15 Paiva V Calazans G Venturi G Dias R Grupo de Estudos em População, Sexualidade e Aids . Idade e uso de preservativo na iniciação sexual de adolescentes brasileiros [Age and condom use at first sexual intercourse of Brazilian adolescents]. Rev Saude Publica. 2008;42(Suppl 1):45–53. Article in Portugese. doi:.https://doi.org/10.1590/S0034-89102008000800007
16 Klavs I Rodrigues LC Wellings K Weiss HA Hayes R . Increased condom use at sexual debut in the general population of Slovenia and association with subsequent condom use. AIDS. 2005;19(11):1215–23. doi:.https://doi.org/10.1097/01.aids.0000176223.78979.26
17 Isley MM Edelman A Kaneshiro B Peters D Nichols MD Jensen JT . Sex education and contraceptive use at coital debut in the United States: results from Cycle 6 of the National Survey of Family Growth. Contraception. 2010;82(3):236–42. doi:.https://doi.org/10.1016/j.contraception.2010.03.019
18 Mauldon J Luker K . The effects of contraceptive education on method use at first intercourse. Fam Plann Perspect. 1996;28(1):19–24. doi:.https://doi.org/10.2307/2135958
19 Mueller TE Gavin LE Kulkarni A . The association between sex education and youth’s engagement in sexual intercourse, age at first intercourse, and birth control use at first sex. J Adolesc Health. 2008;42(1):89–96. doi:.https://doi.org/10.1016/j.jadohealth.2007.08.002
20Barrense-Dias Y, Akré C, Berchtold A, Leeners B, Morselli D, Surís JC. Sexual health and behavior of young people in Switzerland (Raison de santé 291). Lausanne: Institut universitaire de médecine sociale et préventive; 2018.
21 Martyn KK Saftner MA Darling-Fisher CS Schell MC . Sexual risk assessment using event history calendars with male and female adolescents. J Pediatr Health Care. 2013;27(6):460–9. doi:.https://doi.org/10.1016/j.pedhc.2012.05.002
22 Morselli D Berchtold A Suris Granell JC Berchtold A . On-line life history calendar and sensitive topics: A pilot study. Comput Human Behav. 2016;58:141–9. doi:.https://doi.org/10.1016/j.chb.2015.12.068
23Hibell B, Guttormsson U, Ahlstrom S, Balakireva O, Bjarnason T, Kokkevi A, et al. The 2007 ESPAD report: substance use among students in 35 European countries. Stockholm: The Swedish Council for Information on Alcohol and Other Drugs (CAN). 2009.
24 Berg-Kelly K Erdes L . Self-assessment of sexual maturity by mid-adolescents based on a global question. Acta Paediatr. 1997;86(1):10–7. doi:.https://doi.org/10.1111/j.1651-2227.1997.tb08822.x
25 Lazarus JV Moghaddassi M Godeau E Ross J Vignes C Ostergren PO A multilevel analysis of condom use among adolescents in the European Union. Public Health. 2009;123(2):138–44. doi:.https://doi.org/10.1016/j.puhe.2008.10.014
26Office fédéral de la statistique (OFSP) Confédération Suisse. Population résidante permanente âgée de 15 ans ou plus selon l'appartenance religieuse par canton et ville, 2010-2017. 15.11.19]; Available from: https://www.bfs.admin.ch/bfs/fr/home/statistiques/population/langues-religions/religions.assetdetail.7226716.html.
27 Barrense-Dias Y Akre C Surís JC Berchtold A Morselli D Jacot-Descombes C Does the Primary Resource of Sex Education Matter? A Swiss National Study. J Sex Res. 2020;57(2):166–76. doi:.https://doi.org/10.1080/00224499.2019.1626331
28 Chernick LS Chun TH Richards R Bromberg JR Ahmad FA McAninch B Pediatric Emergency Care Applied Research Network (PECARN) . Sex Without Contraceptives in a Multicenter Study of Adolescent Emergency Department Patients. Acad Emerg Med. 2020;27(4):283–90. doi:.https://doi.org/10.1111/acem.13867
29 Williams RL Fortenberry JD . Dual use of long-acting reversible contraceptives and condoms among adolescents. J Adolesc Health. 2013;52(4, Suppl):S29–34. doi:.https://doi.org/10.1016/j.jadohealth.2013.02.002
30 Fennell JL . Men Bring Condoms, Women Take Pills. Gend Soc. 2011;25(4):496–521. doi:.https://doi.org/10.1177/0891243211416113
31 Abel G Fitzgerald L . ‘When you come to it you feel like a dork asking a guy to put a condom on’: is sex education addressing young people’s understandings of risk? Sex Educ. 2006;6(2):105–19. doi:.https://doi.org/10.1080/14681810600578750
32 de Looze M Madkour AS Huijts T Moreau N Currie C . Country-Level Gender Equality and Adolescents’ Contraceptive Use in Europe, Canada and Israel: Findings from 33 Countries. Perspect Sex Reprod Health. 2019;51(1):43–53. doi:.https://doi.org/10.1363/psrh.12090
33 Pinter B Hakim M Seidman DS Kubba A Kishen M Di Carlo C . Religion and family planning. Eur J Contracept Reprod Health Care. 2016;21(6):486–95. doi:.https://doi.org/10.1080/13625187.2016.1237631
34 Charro Baena B Meneses C Caperos JM Prieto M Uroz J . The Role of Religion and Religiosity in Alcohol Consumption in Adolescents in Spain. J Relig Health. 2019;58(5):1477–87. doi:.https://doi.org/10.1007/s10943-018-0694-z
35 Jørgensen MJ Maindal HT Christensen KS Olesen F Andersen B . Sexual behaviour among young Danes aged 15-29 years: a cross-sectional study of core indicators. Sex Transm Infect. 2015;91(3):171–7. doi:.https://doi.org/10.1136/sextrans-2014-051814
36 Copen CE Chandra A Febo-Vazquez I . Sexual Behavior, Sexual Attraction, and Sexual Orientation Among Adults Aged 18-44 in the United States: Data From the 2011-2013 National Survey of Family Growth. Natl Health Stat Rep. 2016;(88):1–14.
This study was funded by the Swiss National Science Foundation [grant 162538].
The authors declare that they have no conflict of interest.