Trapeziometacarpal osteoarthritis – a stepwise therapeutic approach
DOI: https://doi.org/10.4414/smw.2021.20465
Nils C.
Nuessle, Esther
Vögelin, Stefanie
Hirsiger
Department of Hand and Peripheral Nerve Surgery, Inselspital University Hospital Bern, Switzerland
Summary
Osteoarthritis of the trapeziometarcarpal joint, also called rhizarthrosis, is a common finding in the second half of life. It has a higher prevalence in females and is of growing importance in ageing societies. A variety of conservative and surgical treatment options are known, including conservative treatment up to joint replacement. Without treatment, rhizarthrosis can lead to disabling pain and loss of hand function. The goal of this overview of treatment options is to present a stepwise approach that can be initiated by any physician.
Treatment of trapeziometacarpal osteoarthritis should be started early with conservative measures such as splinting and physical therapy, which can be supplemented by oral and topical analgesics and local infiltrations subsequently. If all of these interventions do not provide sufficient relief, referral to a hand surgeon should be considered.
Surgical strategies vary from arthroscopic debridement over trapeziectomy, with or without tendon interposition and ligament reconstruction, to interposition implants and total joint replacements. The planned intervention should be based on clinical and subjective functional limitations and associated degenerative changes, as well as the patient’s expectations and needs.
The goal of this paper is to develop a treatment algorithm, leading to higher levels of patient functionality and satisfaction. Below we discuss the current literature and point out key treatment options used in our department.
Introduction
Osteoarthritis of the trapeziometarcarpal joint (TMO) is a common disease, especially in postmenopausal women [1, 2]. Radiological prevalence ranges from 13.4% above 70 years of age up to 35.8% above 55 years [3]. However, radiographic findings do not always correlate with clinical symptoms [4]. The prevalence of symptomatic TMO is notably lower than radiological changes, which are often incidental [5]. Symptomatic TMO has been found to peak at 5.3% in women aged 70–74 and at 1.7% in men aged 80–84 [6]. On the other hand, there is often no or little evidence of TMO on conventional radiographs in early stages, whereas functional limitations and pain can be very prominent [5]. Symptoms of TMO usually include pain in the trapeziometarcarpal (TMC) joint, reduced hand strength and decreased mobility of the thumb [7]. Pain can vary from episodic to pain related to a specific activity, sometimes accompanied by a background ache [7, 8]. Grasping and pinching is often limited [9]. As the thumb is needed for countless daily activities and represents approximately 40% of overall hand function, limitation of its function can be very disabling [9–11]. Known risk factors include obesity [5], heavy manual labour [12], female gender and hormonal changes, such as menopause [1]. Trauma, rheumatoid arthritis and hyperlaxity diseases (Marfan/Ehlers-Danlos) are risk factors for secondary osteoarthritis of the TMC joint [13, 14]. Because of our ageing societies, TMO is a growing medical challenge and economic burden [15]. Patients who are referred to our hand surgical consultation are mostly aware of their diagnosis, but have not yet received the full array of conservative treatments and often hesitate to consider surgical treatment. This review aims to give an overview of current and evidence-based treatment options and to formulate a stepwise approach for optimal patient care.
Imaging and classification
Conventional radiographs
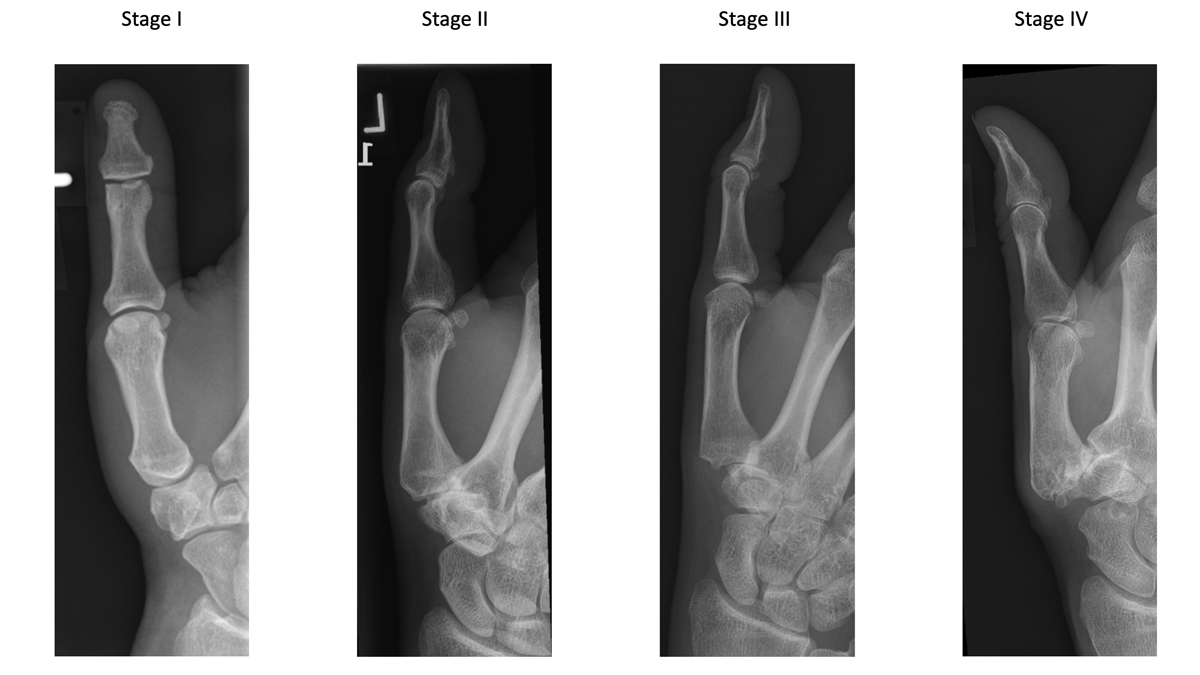
In 1987, Eaton and Littler proposed a radiological classification of trapeziometacarpal osteoarthritis, which is still the most widely used for staging. This classification system consists of four different stages (fig. 1) [16, 17]. Even though other imaging techniques and classification systems exist, X-rays of the thumb in two planes remain the gold standard and should be ordered early in suspected TMO [16, 17]. It is, however, important to evaluate the neighbouring joints such as the scaphotrapezial and scaphotrapezoidal (STT) joints for treatment.
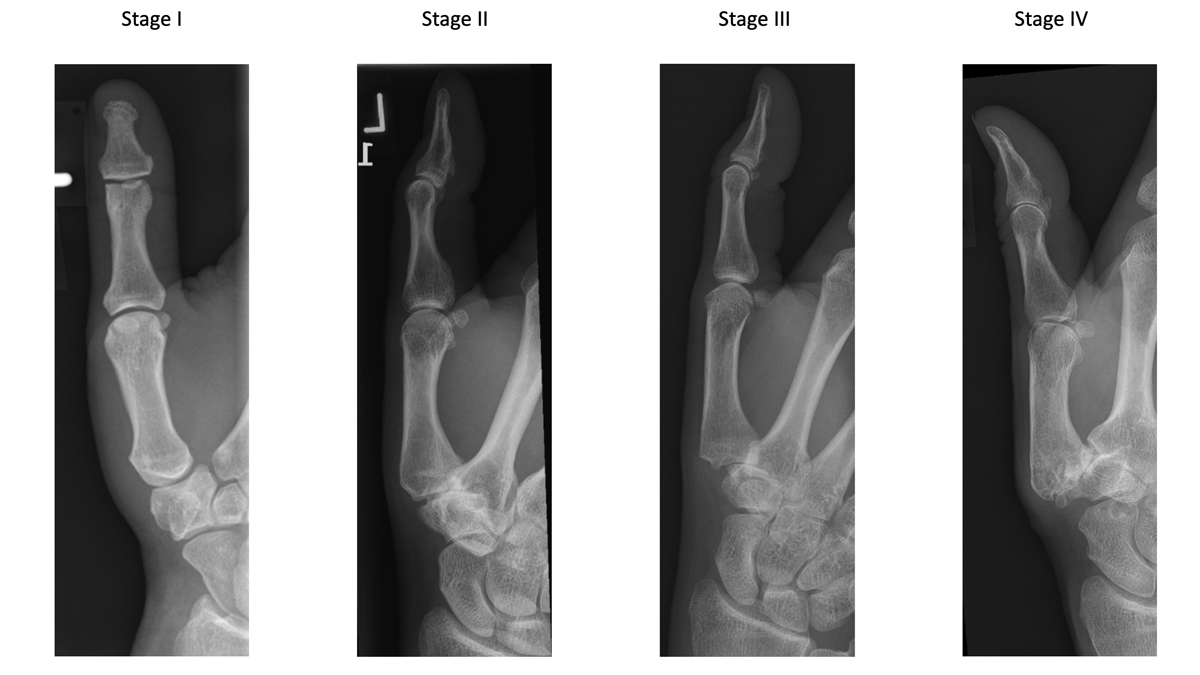
Figure 1 Eaton/Littler classification of trapeziometacarpal osteoarthritis.
Stage I: slight widening of the joint space and normal contours.
Stage II: slight narrowing of the TMC and sclerosis, osteophytes <2mm, up to 1/3 subluxation of the joint
Stage III: marked joint space narrowing, osteophytes >2mm, >1/3 subluxation
Stage IV: Pantrapezial arthritis, major subluxation, cystic and sclerotic subchondral bone changes, significant erosion of the scaphotrapezial joint.
Additional imaging
Multilayer imaging can help to evaluate the trapeziometacarpal joint and the neighbouring joints in more detail. To evaluate bone stock and cartilage surfaces, and especially if planning prosthetic implants, computed tomography (CT) enhanced by intra-articular contrast injection can be useful [18]. Magnetic resonance imaging (MRI) allows ligament and soft tissue evaluation. Recent developments of specific sequences can quantitatively analyse cartilage or define alterations in its composition [19]. Single-photon emission computed tomography combined with conventional CT (SPECT/CT) can be used to discriminate between pain arising from the TMC or the STT joint [20]. In patients with persistent postoperative pain SPECT is a good adjunct, as other forms of imaging can be difficult to evaluate owing to residual changes from the intervention [21]. Arthroscopic evaluation may allow earlier and more detailed evaluation of degenerative changes [22].
The treatment ladder
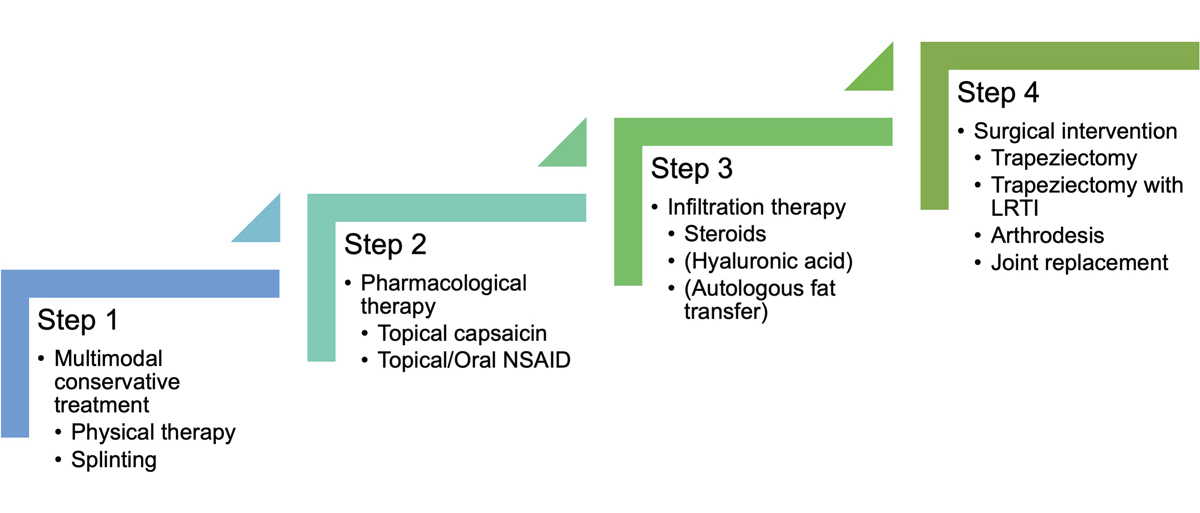
Treatment of TMO should not only be based on the radiological classification, but also focus on the patient’s symptoms, subjective loss of function and the evolution over time. Conservative options are at the bottom and ultimately surgery is the last step of the treatment ladder (fig. 2). The treatment ladder is based on current literature, as well as experience in our centre.
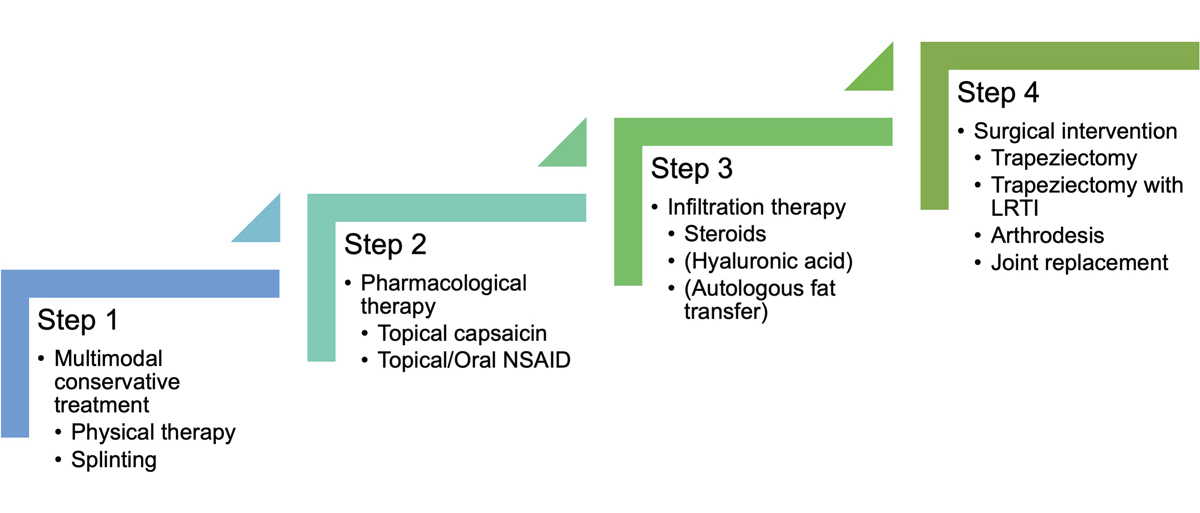
Figure 2 Treatment ladder for basal thumb osteoarthritis. A structured approach for all caregivers recommended by the department of hand surgery at Inselspital Bern, Switzerland. Different steps should be combined to ensure optimal treatment. If results are unsatisfactory for the patient, the treatment can be escalated to the next step.
Step I: Multimodal conservative treatment
In every stage of TMO, conservative treatment is the first step of the treatment ladder. All therapeutic modalities described below should be used in combination to optimise the treatment effect.
Splinting
In a recent meta-analysis, splinting caused a moderate to large reduction in pain in the medium term (3–12 months) and an improvement of function, and can avoid surgical treatment in some patients [23, 24]
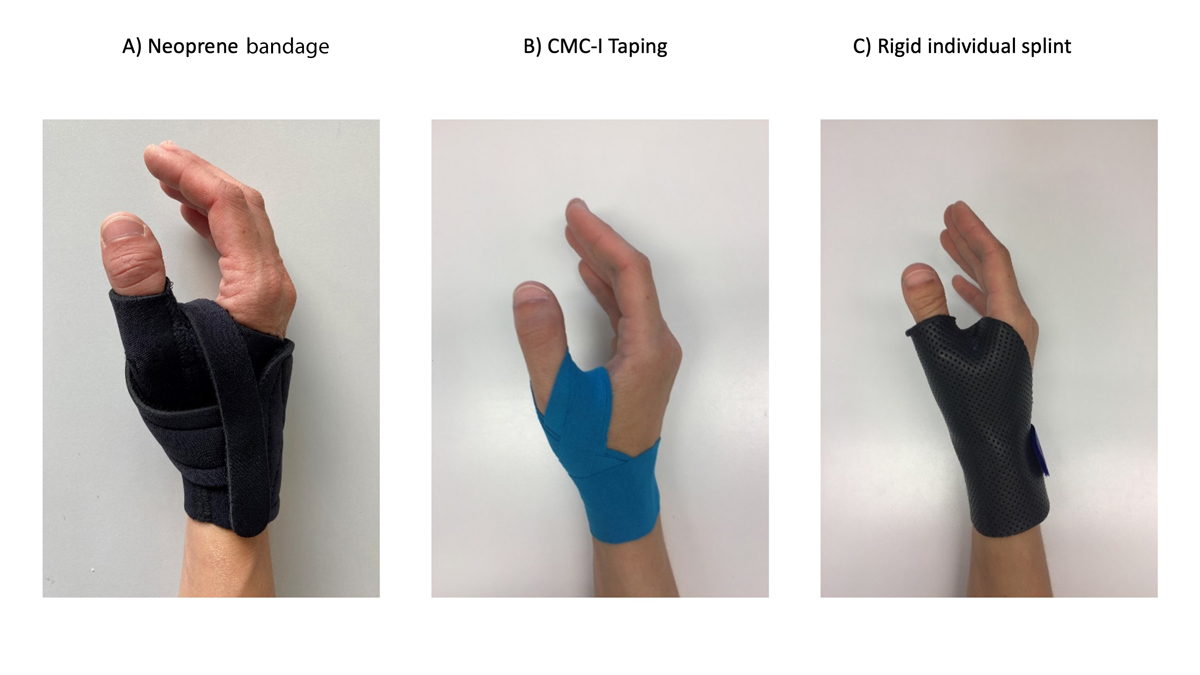
In our experience, neoprene bandages provide a high level of comfort for the patients with low risk of developing pressure points, at low cost. Additionally, they serve as an insulation layer, which may help to reduce cold-related worsening of symptoms (fig. 3a). For some patients, taping may present a good alternative (fig. 3b) [25]. For those more comfortable with a rigid support, a thermomoulded splint can be an option (fig. 3c).
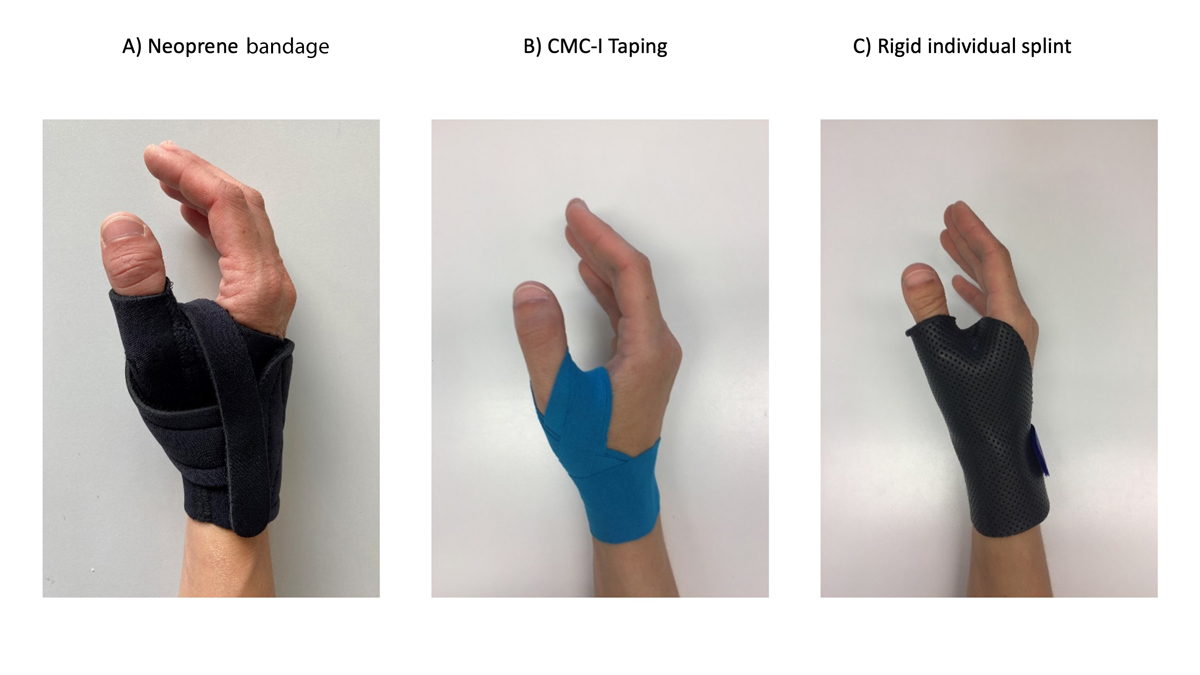
Figure 3 Different splints of the TMC joint. The right splint has to be chosen according to the patient’s needs and demands. Neoprene bandages (a) provide a high level of comfort and serve as insulation layer. Taping (b) presents a good alternative, especially for those needing to wear gloves at work (e.g., healthcare professionals). Rigid individual splints (c) provide the highest level of stability.
Physical therapy
Physical therapy by specialised hand therapists leads to a significant improvement in pain and hand function [26]. Specific hand exercises help to increase grip strength and function, reduce pain and improve the range of movement of the thumb [27]. Some investigators focus primarily on increasing the range of movement and strengthening intrinsic and extrinsic muscles by providing a set of exercises that are based on biomechanical findings in cadaver studies [28]. Others prefer the so-called dynamic stability modelled approach, including a variety of hand exercises that focus on restoration of the thumb web space, re-education of thumb muscles, joint mobilisation and muscle strengthening, which has been able to show significant reduction in pain and disability [29].
We therefore recommend initiating physical therapy, together with splinting, as one of the first steps in treating TMO [30].
Step 2: Pharmacological therapy
The American College of Rheumatology in 2012 and the European League against Rheumatism recommended the use of one or more of the following drugs for patients suffering from hand osteoarthritis [31, 32]:
- Topical capsaicin
- Topical nonsteroidal anti-inflammatory drugs (NSAIDs)
- Oral NSAIDs, including cyclo-oxygenase-2 (COX2)-selective inhibitors
- Oral chondroitin sulphate
In patients older than 75 years, topical use of NSAIDs is preferred, as side effects might outweigh the benefits of systemic application, especially when used over a longer period of time [31–33]. There is no evidence on superiority of one specific anti-inflammatory treatment over another in TMO [31, 32]. In addition, topical capsaicin has been described as an option to reduce tenderness and pain [34, 35].
Oral chondroitin sulphate has shown effectiveness in relieving symptoms of hand osteoarthritis [36]. As side effects are rare and benign, we recommend its use.
Paracetamol is regularly prescribed for patients suffering from hand osteoarthritis with contraindications for NSAID use [31]. However, in three small trials, paracetamol showed no superiority over placebo or an active comparator [31, 37–39].
Therefore, as an add-on therapy to step 1, we recommend analgesics for short-term use, if applied orally. If all conservative treatments fail, treatment can be escalated to more invasive approaches.
Step 3: Infiltration therapy
Corticosteroid injections into the TMC joint can provide short-term benefits, with pain relief and improved function [40]. Unfortunately, the effect usually does not last longer than 1–3 months [40–42]. Nevertheless, in early stages of TMO or when inflammation is predominant corticosteroids infiltration, in combination with splinting, can provide long-term pain relief [43]. It remains unclear whether the volume injected into the joint or specific anti-inflammatory effects are responsible for pain reduction, as some studies have revealed that saline injections can provide similar results [9, 42].
Hyaluronic acid or dextrose injections present alternatives for injection therapy [44] and autologous fat transfer (stem cells) was suggested as an interesting alternative [45]. Nevertheless, only steroid injections are reimbursed by insurance companies in Switzerland. Complications and morbidity of injections are generally low. In a recent systematic review and meta-analysis, no adverse effects, such as intra-articular infections, were found in the studies included [44]. On the other hand, the evidence for long-term benefits was considered low, so that injections remain a topic of discussion [44].
If pain relief is provided effectively by the first steroid injection, we recommend up to three injections with a delay of 3 months before escalating to a surgical intervention.
Step 4: Surgical interventions
Several surgical interventions exist for the treatment of TMO, but none has been shown to be ultimately superior [46]. We will shortly describe the different options and their indications hereafter.
Trapeziectomy with or without ligament reconstruction and interposition
Resection arthroplasty consists of surgical removal of the trapezium bone and can be combined with ligament reconstruction and interposition (LRTI).
The latter adds suspension with a tendon strip in order to support the first metacarpal bone, as well as filling the trapezial space with the partially resected local tendon (fig. 4) [47]. Both interventions show equal long-term outcomes, nevertheless simple trapeziectomy is a shorter procedure with slightly lower complication rates [48–51]. Nevertheless, most hand surgeons prefer LRTI to simple trapeziectomy [52] and it thus represents the most common surgical therapy for patients suffering from advanced stages of TMO [6]. A possible explanation could be that the ligament reconstruction allows initial suspension and early functional rehabilitation. Ligament reconstruction and interposition using artificial material or allografts have fallen out of favour due to significantly higher complication rates [53].
Shortcomings of both techniques are the risk of subsidence of the first ray and decreased strength and mobility [54]. Although studies show no correlation between success of LRTI and radiologic subsidence [55–57], a conflict between the scaphoid and the base of the metacarpal I can be a reason for persistence or recurrent pain. Especially in advanced TMO, when the scaphotrapeziotrapezoidal (STT) joint is involved, partial trapezial excision has been shown to exacerbate pre-existing positional abnormalities and degenerative changes of the carpus [52, 58]. Other options should be considered in these situations.
Joint replacement surgery
Alternatives consist of a wide variety of interpositional prosthetic implants, whose use has been increasing in the last decades [59]. In the early days, loosening presented the main complication of the different subtypes, with rates ranging from 3% up to 53% [60–62]. Most prosthetic implants changed continuously over time, so that long-term outcomes mainly exist for models not being used anymore because of high complication rates. On the other hand, some studies report better postoperative pinch strength, greater reduction in metacarpophalangeal (MCP) joint hyperextension and faster recovery for patients treated with a prosthesis [63–65]. Non-cemented prostheses provide better results in mid-term follow-up [66, 67], high rates of patient satisfaction and 71–92% survival rates in a 10-year follow-up [68, 69]. There is a lack of prospective studies directly comparing trapeziectomy with the different prostheses [59], but at present overall prosthetic implants seem to have a higher complication rate and inferior long-term outcomes compared with resection arthroplasty [69, 70]. There are several other treatment options, but for an overview we focus on the procedures and techniques used in the department of hand surgery at Inselspital (Bern, Switzerland). Thus, one model representative of a total joint replacement prosthesis (Touch®), one surface replacement implant (Pyrocardan®) and the surgical technique of arthrodesis are described below.
Total joint replacement prosthesis
The Touch® prosthesis (KeriMedical, Geneva, Switzerland) has been introduced onto the market as a dual mobility trapeziometarcarpal prosthesis. A first case series of 132 patients showed a reduction of luxations and a longer lifespan compared with older prosthesis [71]. Because of faster rehabilitation and preservation of length in the first ray, this possibility can be considered especially for younger patients and if fine motor skills are needed. However, as long-term data for this prosthesis are not yet available, the pros and cons should be discussed in detail with the patient. At this point, there is a need for high-quality randomised studies to investigate whether it is able to deliver superior long-term results [72].
Spacer
Pyrocarbon has a module of elasticity similar to that of cortical bone and is therefore well suited for interposition arthroplasties [73]. There are several implant models for different joints. The Pyrocardan® spacer is a hyperbolic paraboloid disk, which is inserted into the joint after partial resection of the first metacarpal and the trapezium bone (fig. 5). Five-year survival rates of 90% were reported [74]. In several studies, the Pyrocardan® spacer had similar outcomes to conventional arthroplasties, but shorter postoperative rehabilitation until relief of symptoms [75, 76]. Revision rates in several studies vary from 3.2% after 60 months of follow up to 25% after 26 months [75, 77].
The main benefit of using an interposition arthroplasty is the maintenance of length of the first ray. Furthermore, it can easily be revised by a trapeziectomy with or without LRTI in the case of failure [78, 79]. Pyrocardan® implants can also be used as a double arthroplasty in the TMC and STT joints in patients with stage IV osteoarthritis, or as an interposition spacer after failed trapeziectomy with subsidence [80]. As for the other prosthetic implants, no prospective long-term data proving its superiority to simple trapeziectomy are available and thus the potential advantages have to be outweighed with the complication rate and higher cost.
Arthrodesis
Lastly, arthrodesis may be a primary or a salvage option for TMO [81]. Arthrodesis as a treatment option for TMO is reserved for a limited subgroup of patients, as it fixes the position of the thumb in physiological antepulsion. However, the length of the first ray is better preserved with more force due to the proximal stability on the cost of motion. Arthrodesis has been shown to have relatively high rates of non-union, especially with earlier bone fixation techniques and it may lead to further progression of STT arthrosis [82–84]. In one study, an increased grip strength following arthrodesis as compared with trapeziectomy with LRTI has been described [50]. In our opinion, arthrodesis is therefore only indicated in exceptional cases such as young manual workers or complex revision cases.
Overview
In our ageing society, osteoarthrosis of the trapeziometacarpal joint represents a common disease of growing importance. The challenge to enable good access to optimised treatment options requires a stepwise approach. The growing number of patients suffering from TMO demands standardised treatment schemes applicable not only by hand surgeons.
Following clinical examination and conventional x-rays, to ensure the right diagnosis, we therefore recommend the subsequent stepwise approach for all caregivers involved in the patient’s care:
Step 1: Multimodal conservative treatment, including education, physical therapy and splinting. Specific hand therapy may apply physical anti-inflammatory and analgesic treatments, as well as instruct correct use of the weakened thumb.
Step 2: Pharmacological therapy, which involves chondroitin sulphate, topical capsaicin, short-term treatment with oral NSAIDs. For all pharmacological treatments, the individual patient’s risk factors need to be respected to ensure the right risk-benefit-ratio. In addition, oral chondroitin sulphate has been investigated and might present an alternative in the future.
Step 3: Infiltration therapy of the TMC joint, using steroids, hyaluronic acid, dextrose or saline showed contradictory results in the latest studies. They might offer a treatment option, as the rate of adverse effects is very low. Also, infiltration therapy showed a potential to postpone surgery. We recommend only cortisone infiltration, as it is the only product accepted by insurance companies.
Step 4: Surgical interventions are indicated, if all conservative treatment options fail and symptoms lead to unacceptably diminished function for the patient.
Many different surgical options exist. Currently, simple trapeziectomy or trapeziectomy with LRTI present comparable options with no significant differences in long-term results. Newer therapies, such as total joint or surface replacement using implants were able to show faster rehabilitation time, but often less convincing long-term results. For many newer types of prosthesis, long-term follow-up data are still lacking. Therefore, they should only be discussed with caution in young patients with high demands. In the case of an unfavourable outcome, secondary trapeziectomy presents a surgical option.
Steps 1–3 can easily be taken by general practitioners, rheumatologists, orthopaedic surgeons and other colleagues caring for TMO patients and do not require immediate consultation of a hand surgeon. These steps have been shown to avoid or postpone more invasive treatments, while reducing the patient’s symptoms.
If these measures fail over a period of at least 3 months, we recommend discussing referral to a hand surgeon to evaluate the patient’s needs and will for surgery.
This review of current state-of-the-art therapies aims to emphasise that coordinated and combined use of different treatment options has a higher chance to lead to long-term patient satisfaction and might postpone or prevent surgery.
References
1
Armstrong
AL
,
Hunter
JB
,
Davis
TR
. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg [Br]. 1994;19(3):340–1. doi:.https://doi.org/10.1016/0266-7681(94)90085-X
2
Swigart
CR
,
Eaton
RG
,
Glickel
SZ
,
Johnson
C
. Splinting in the treatment of arthritis of the first carpometacarpal joint. J Hand Surg Am. 1999;24(1):86–91. doi:.https://doi.org/10.1053/jhsu.1999.jhsu24a0086
3National Institute for Health and Clinical Excellence. Guidance. Osteoarthritis: Care and Management in Adults. London: NICE; 2014.
4
Botha-Scheepers
S
,
Riyazi
N
,
Watt
I
,
Rosendaal
FR
,
Slagboom
E
,
Bellamy
N
, et al.
Progression of hand osteoarthritis over 2 years: a clinical and radiological follow-up study. Ann Rheum Dis. 2009;68(8):1260–4. doi:.https://doi.org/10.1136/ard.2008.087981
5
Dahaghin
S
,
Bierma-Zeinstra
SM
,
Ginai
AZ
,
Pols
HA
,
Hazes
JM
,
Koes
BW
. Prevalence and pattern of radiographic hand osteoarthritis and association with pain and disability (the Rotterdam study). Ann Rheum Dis. 2005;64(5):682–7. doi:.https://doi.org/10.1136/ard.2004.023564
6
Wolf
JM
,
Delaronde
S
. Current trends in nonoperative and operative treatment of trapeziometacarpal osteoarthritis: a survey of US hand surgeons. J Hand Surg Am. 2012;37(1):77–82. doi:.https://doi.org/10.1016/j.jhsa.2011.10.010
7
Wilkens
SC
,
Meghpara
MM
,
Ring
D
,
Coert
JH
,
Jupiter
JB
,
Chen
NC
. Trapeziometacarpal Arthrosis. JBJS Rev. 2019;7(1):e8. doi:.https://doi.org/10.2106/JBJS.RVW.18.00020
8
McQuillan
TJ
,
Kenney
D
,
Crisco
JJ
,
Weiss
AP
,
Ladd
AL
. Weaker Functional Pinch Strength Is Associated With Early Thumb Carpometacarpal Osteoarthritis. Clin Orthop Relat Res. 2016;474(2):557–61. doi:.https://doi.org/10.1007/s11999-015-4599-9
9
Hamasaki
T
,
Laprise
S
,
Harris
PG
,
Bureau
NJ
,
Gaudreault
N
,
Ziegler
D
, et al.
Efficacy of non-surgical interventions for trapeziometacarpal (thumb base) osteoarthritis: A systematic review. Arthritis Care Res (Hoboken). 2020;72(12):1719–35. doi:.https://doi.org/10.1002/acr.24084
10
Ladd
AL
,
Weiss
AP
,
Crisco
JJ
,
Hagert
E
,
Wolf
JM
,
Glickel
SZ
, et al.
The thumb carpometacarpal joint: anatomy, hormones, and biomechanics. Instr Course Lect. 2013;62:165–79.
11
Berger
AJ
,
Meals
RA
. Management of osteoarthrosis of the thumb joints. J Hand Surg Am. 2015;40(4):843–50. doi:.https://doi.org/10.1016/j.jhsa.2014.11.026
12
Jensen
JC
,
Sherson
D
. Work-related bilateral osteoarthritis of the first carpometacarpal joints. Occup Med (Lond). 2007;57(6):456–60. doi:.https://doi.org/10.1093/occmed/kqm029
13
Wolf
JM
,
Schreier
S
,
Tomsick
S
,
Williams
A
,
Petersen
B
. Radiographic laxity of the trapeziometacarpal joint is correlated with generalized joint hypermobility. J Hand Surg Am. 2011;36(7):1165–9. doi:.https://doi.org/10.1016/j.jhsa.2011.03.017
14
Jónsson
H
,
Valtýsdóttir
ST
,
Kjartansson
O
,
Brekkan
A
. Hypermobility associated with osteoarthritis of the thumb base: a clinical and radiological subset of hand osteoarthritis. Ann Rheum Dis. 1996;55(8):540–3. doi:.https://doi.org/10.1136/ard.55.8.540
15
Hamasaki
T
,
Lalonde
L
,
Harris
P
,
Bureau
NJ
,
Gaudreault
N
,
Ziegler
D
, et al.
Efficacy of treatments and pain management for trapeziometacarpal (thumb base) osteoarthritis: protocol for a systematic review. BMJ Open. 2015;5(10):e008904. doi:.https://doi.org/10.1136/bmjopen-2015-008904
16
Eaton
RG
,
Glickel
SZ
. Trapeziometacarpal osteoarthritis. Staging as a rationale for treatment. Hand Clin. 1987;3(4):455–71.
17
Kennedy
CD
,
Manske
MC
,
Huang
JI
. Classifications in Brief: The Eaton-Littler Classification of Thumb Carpometacarpal Joint Arthrosis. Clin Orthop Relat Res. 2016;474(12):2729–33. doi:.https://doi.org/10.1007/s11999-016-4864-6
18
Cernohorsky
P
,
Strackee
SD
,
Streekstra
GJ
,
van den Wijngaard
JP
,
Spaan
JAE
,
Siebes
M
, et al.
Computed Tomography-Mediated Registration of Trapeziometacarpal Articular Cartilage Using Intraarticular Optical Coherence Tomography and Cryomicrotome Imaging: A Cadaver Study. Cartilage. 2019:1947603519860247. doi:.https://doi.org/10.1177/1947603519860247
19
Hayashi
D
,
Roemer
FW
,
Guermazi
A
. Imaging of osteoarthritis-recent research developments and future perspective. Br J Radiol. 2018;91(1085):20170349. doi:.https://doi.org/10.1259/bjr.20170349
20
van Rijn
SF
,
de Vries
MR
,
Kraan
GA
. The use of single photon emission computed tomography/computed tomography to differentiate between pain arising from trapeziometacarpal joint and scaphotrapeziotrapezoid joint osteoarthritis. J Hand Surg Eur Vol. 2016;41(7):776–7. doi:.https://doi.org/10.1177/1753193415606070
21
Strobel
K
,
van der Bruggen
W
,
Hug
U
,
Gnanasegaran
G
,
Kampen
WU
,
Kuwert
T
, et al.
SPECT/CT in Postoperative Hand and Wrist Pain. Semin Nucl Med. 2018;48(5):396–409. doi:.https://doi.org/10.1053/j.semnuclmed.2018.05.001
22
Badia
A
. Trapeziometacarpal arthroscopy: a classification and treatment algorithm. Hand Clin. 2006;22(2):153–63. doi:.https://doi.org/10.1016/j.hcl.2006.02.006
23
Buhler
M
,
Chapple
CM
,
Stebbings
S
,
Sangelaji
B
,
Baxter
GD
. Effectiveness of splinting for pain and function in people with thumb carpometacarpal osteoarthritis: a systematic review with meta-analysis. Osteoarthritis Cartilage. 2019;27(4):547–59. doi:.https://doi.org/10.1016/j.joca.2018.09.012
24
Valdes
K
,
Marik
T
. A systematic review of conservative interventions for osteoarthritis of the hand. J Hand Ther. 2010;23(4):334–50, quiz 351. doi:.https://doi.org/10.1016/j.jht.2010.05.001
25
Villafañe
JH
,
Langford
D
,
Alguacil-Diego
IM
,
Fernández-Carnero
J
. Management of trapeziometacarpal osteoarthritis pain and dysfunction using mobilization with movement technique in combination with kinesiology tape: a case report. J Chiropr Med. 2013;12(2):79–86. doi:.https://doi.org/10.1016/j.jcm.2013.06.001
26
Ahern
M
,
Skyllas
J
,
Wajon
A
,
Hush
J
. The effectiveness of physical therapies for patients with base of thumb osteoarthritis: Systematic review and meta-analysis. Musculoskelet Sci Pract. 2018;35:46–54. doi:.https://doi.org/10.1016/j.msksp.2018.02.005
27
Spaans
AJ
,
van Minnen
LP
,
Kon
M
,
Schuurman
AH
,
Schreuders
AR
,
Vermeulen
GM
. Conservative treatment of thumb base osteoarthritis: a systematic review. J Hand Surg Am. 2015;40(1):16–21.e6. doi:.https://doi.org/10.1016/j.jhsa.2014.08.047
28
Valdes
K
,
von der Heyde
R
. An exercise program for carpometacarpal osteoarthritis based on biomechanical principles. J Hand Ther. 2012;25(3):251–62, quiz 263. doi:.https://doi.org/10.1016/j.jht.2012.03.008
29
O’Brien
VH
,
Giveans
MR
. Effects of a dynamic stability approach in conservative intervention of the carpometacarpal joint of the thumb: a retrospective study. J Hand Ther. 2013;26(1):44–51, quiz 52. doi:.https://doi.org/10.1016/j.jht.2012.10.005
30
Østerås
N
,
Kjeken
I
,
Smedslund
G
,
Moe
RH
,
Slatkowsky-Christensen
B
,
Uhlig
T
, et al.
Exercise for Hand Osteoarthritis: A Cochrane Systematic Review. J Rheumatol. 2017;44(12):1850–8. doi:.https://doi.org/10.3899/jrheum.170424
31
Kloppenburg
M
,
Kroon
FP
,
Blanco
FJ
,
Doherty
M
,
Dziedzic
KS
,
Greibrokk
E
, et al.
2018 update of the EULAR recommendations for the management of hand osteoarthritis. Ann Rheum Dis. 2019;78(1):16–24. doi:.https://doi.org/10.1136/annrheumdis-2018-213826
32
Hochberg
MC
,
Altman
RD
,
April
KT
,
Benkhalti
M
,
Guyatt
G
,
McGowan
J
, et al.; American College of Rheumatology. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res (Hoboken). 2012;64(4):465–74. doi:.https://doi.org/10.1002/acr.21596
33
Pelletier
JP
,
Martel-Pelletier
J
,
Rannou
F
,
Cooper
C
. Efficacy and safety of oral NSAIDs and analgesics in the management of osteoarthritis: Evidence from real-life setting trials and surveys. Semin Arthritis Rheum. 2016;45(4, Suppl):S22–7. doi:.https://doi.org/10.1016/j.semarthrit.2015.11.009
34
McCarthy
GM
,
McCarty
DJ
. Effect of topical capsaicin in the therapy of painful osteoarthritis of the hands. J Rheumatol. 1992;19(4):604–7.
35
Laslett
LL
,
Jones
G
. Capsaicin for osteoarthritis pain. Prog Drug Res. 2014;68:277–91.
36
Gabay
C
,
Medinger-Sadowski
C
,
Gascon
D
,
Kolo
F
,
Finckh
A
. Symptomatic effects of chondroitin 4 and chondroitin 6 sulfate on hand osteoarthritis: a randomized, double-blind, placebo-controlled clinical trial at a single center. Arthritis Rheum. 2011;63(11):3383–91. doi:.https://doi.org/10.1002/art.30574
37
Reginster
JY
,
Neuprez
A
,
Lecart
MP
,
Sarlet
N
,
Bruyere
O
. Role of glucosamine in the treatment for osteoarthritis. Rheumatol Int. 2012;32(10):2959–67. doi:.https://doi.org/10.1007/s00296-012-2416-2
38
Rovetta
GMP
. Dexketoprofen-trometamol in patients with osteoarthritis of the hands. Minerva Ortop Traumatol. 2001;52(1):27–30.
39
McKendry
RTC
,
Weisman
M
. Hydroxychloroquine (HCQ) versus acetaminophen (ACM) versus placebo (PL) in the treatment of nodal osteoarthritis (NOA) of the hands. J Rheumatol. 2001;28:1421.
40
Fowler
A
,
Swindells
MG
,
Burke
FD
. Intra-articular corticosteroid injections to manage trapeziometacarpal osteoarthritis-a systematic review. Hand (N Y). 2015;10(4):583–92. doi:.https://doi.org/10.1007/s11552-015-9778-3
41
Swindells
MG
,
Logan
AJ
,
Armstrong
DJ
,
Chan
P
,
Burke
FD
,
Lindau
TR
. The benefit of radiologically-guided steroid injections for trapeziometacarpal osteoarthritis. Ann R Coll Surg Engl. 2010;92(8):680–4. doi:.https://doi.org/10.1308/003588410X12699663905078
42
Rocchi
L
,
Merolli
A
,
Giordani
L
,
Albensi
C
,
Foti
C
. Trapeziometacarpal joint osteoarthritis: a prospective trial on two widespread conservative therapies. Muscles Ligaments Tendons J. 2018;7(4):603–10. doi:.https://doi.org/10.32098/mltj.04.2017.16
43
Day
CS
,
Gelberman
R
,
Patel
AA
,
Vogt
MT
,
Ditsios
K
,
Boyer
MI
. Basal joint osteoarthritis of the thumb: a prospective trial of steroid injection and splinting. J Hand Surg Am. 2004;29(2):247–51. doi:.https://doi.org/10.1016/j.jhsa.2003.12.002
44
Riley
N
,
Vella-Baldacchino
M
,
Thurley
N
,
Hopewell
S
,
Carr
AJ
,
Dean
BJF
. Injection therapy for base of thumb osteoarthritis: a systematic review and meta-analysis. BMJ Open. 2019;9(9):e027507. doi:.https://doi.org/10.1136/bmjopen-2018-027507
45
Herold
C
,
Rennekampff
HO
,
Groddeck
R
,
Allert
S
. Autologous Fat Transfer for Thumb Carpometacarpal Joint Osteoarthritis: A Prospective Study. Plast Reconstr Surg. 2017;140(2):327–35. doi:.https://doi.org/10.1097/PRS.0000000000003510
46
Baker
RHJ
,
Al-Shukri
J
,
Davis
TRC
. Evidence-Based Medicine: Thumb Basal Joint Arthritis. Plast Reconstr Surg. 2017;139(1):256e–66e. doi:.https://doi.org/10.1097/PRS.0000000000002858
47
Klionsky
DJ
,
Abdelmohsen
K
,
Abe
A
,
Abedin
MJ
,
Abeliovich
H
,
Acevedo Arozena
A
, et al.
Guidelines for the use and interpretation of assays for monitoring autophagy (3rd edition). Autophagy. 2016;12(1):1–222. doi:.https://doi.org/10.1080/15548627.2015.1100356
48
Zafonte
B
,
Szabo
RM
. Evidence-based medicine in hand surgery: clinical applications and future direction. Hand Clin. 2014;30(3):269–83, v. doi:.https://doi.org/10.1016/j.hcl.2014.04.005
49
Vermeulen
GM
,
Slijper
H
,
Feitz
R
,
Hovius
SE
,
Moojen
TM
,
Selles
RW
. Surgical management of primary thumb carpometacarpal osteoarthritis: a systematic review. J Hand Surg Am. 2011;36(1):157–69. doi:.https://doi.org/10.1016/j.jhsa.2010.10.028
50
Raven
EE
,
Kerkhoffs
GM
,
Rutten
S
,
Marsman
AJ
,
Marti
RK
,
Albers
GH
. Long term results of surgical intervention for osteoarthritis of the trapeziometacarpal joint : comparison of resection arthroplasty, trapeziectomy with tendon interposition and trapezio-metacarpal arthrodesis. Int Orthop. 2007;31(4):547–54. doi:.https://doi.org/10.1007/s00264-006-0217-5
51
Huang
K
,
Hollevoet
N
,
Giddins
G
. Thumb carpometacarpal joint total arthroplasty: a systematic review. J Hand Surg Eur Vol. 2015;40(4):338–50. doi:.https://doi.org/10.1177/1753193414563243
52
Yuan
BJ
,
Moran
SL
,
Tay
SC
,
Berger
RA
. Trapeziectomy and carpal collapse. J Hand Surg Am. 2009;34(2):219–27. doi:.https://doi.org/10.1016/j.jhsa.2008.11.007
53
Marks
M
,
Hensler
S
,
Wehrli
M
,
Scheibler
AG
,
Schindele
S
,
Herren
DB
. Trapeziectomy With Suspension-Interposition Arthroplasty for Thumb Carpometacarpal Osteoarthritis: A Randomized Controlled Trial Comparing the Use of Allograft Versus Flexor Carpi Radialis Tendon. J Hand Surg Am. 2017;42(12):978–86. doi:.https://doi.org/10.1016/j.jhsa.2017.07.023
54
Wajon
A
,
Vinycomb
T
,
Carr
E
,
Edmunds
I
,
Ada
L
. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2015;(2):CD004631.
55
Yang
Y
,
Tien
HY
,
Kumar
KK
,
Chen
S
,
Li
Z
,
Tian
W
, et al.
Ligament reconstruction with tendon interposition arthroplasty for first carpometacarpal joint osteoarthritis. Chin Med J (Engl). 2014;127(22):3921–5.
56
Yang
SS
,
Weiland
AJ
. First metacarpal subsidence during pinch after ligament reconstruction and tendon interposition basal joint arthroplasty of the thumb. J Hand Surg Am. 1998;23(5):879–83. doi:.https://doi.org/10.1016/S0363-5023(98)80167-6
57
Gangopadhyay
S
,
McKenna
H
,
Burke
FD
,
Davis
TR
. Five- to 18-year follow-up for treatment of trapeziometacarpal osteoarthritis: a prospective comparison of excision, tendon interposition, and ligament reconstruction and tendon interposition. J Hand Surg Am. 2012;37(3):411–7. doi:.https://doi.org/10.1016/j.jhsa.2011.11.027
58
Tay
SC
,
Moran
SL
,
Shin
AY
,
Linscheid
RL
. The clinical implications of scaphotrapezium-trapezoidal arthritis with associated carpal instability. J Hand Surg Am. 2007;32(1):47–54. doi:.https://doi.org/10.1016/j.jhsa.2006.10.021
59Ceruso M, Munz G, Carulli C, Virgili G, Viviani A, Hollevoet N, et al. Thumb TMC Joint Osteo-Arthritis. In: Giddins G, Leblebicioğlu G (eds). Evidence Based Data In Hand Surgery And Therapy. St Gallen: FESSH; 2017. pp 368–428
60
Wachtl
SW
,
Guggenheim
PR
,
Sennwald
GR
. Cemented and non-cemented replacements of the trapeziometacarpal joint. J Bone Joint Surg Br. 1998;80-B(1):121–5. doi:.https://doi.org/10.1302/0301-620X.80B1.0800121
61
van Cappelle
HG
,
Elzenga
P
,
van Horn
JR
. Long-term results and loosening analysis of de la Caffinière replacements of the trapeziometacarpal joint. J Hand Surg Am. 1999;24(3):476–82. doi:.https://doi.org/10.1053/jhsu.1999.0476
62
Giddins
G
. Thumb arthroplasties. J Hand Surg Eur Vol. 2012;37(7):603–4. doi:.https://doi.org/10.1177/1753193412455988
63
Degeorge
B
,
Dagneaux
L
,
Andrin
J
,
Lazerges
C
,
Coulet
B
,
Chammas
M
. Do trapeziometacarpal prosthesis provide better metacarpophalangeal stability than trapeziectomy and ligamentoplasty?
Orthop Traumatol Surg Res. 2018;104(7):1095–100. doi:.https://doi.org/10.1016/j.otsr.2018.07.008
64
Jager
T
,
Barbary
S
,
Dap
F
,
Dautel
G
. Analyse de la douleur postopératoire et des résultats fonctionnels précoces dans le traitement de la rhizarthrose. Étude prospective comparative de 74 patientes trapézectomie-interposition vs prothèse MAIA® [Evaluation of postoperative pain and early functional results in the treatment of carpometacarpal joint arthritis. Comparative prospective study of trapeziectomy vs. MAIA(®) prosthesis in 74 female patients]. Chir Main. 2013;32(2):55–62. Article in French. doi:.https://doi.org/10.1016/j.main.2013.02.004
65
Jurča
J
,
Němejc
M
,
Havlas
V
. [Surgical Treatment for Advanced Rhizarthrosis. Comparison of Results of the Burton-Pellegrini Technique and Trapeziometacarpal Joint Arthroplasty]. Acta Chir Orthop Traumatol Cech. 2016;83(1):27–31. Article in Czech.
66
Vandenberghe
L
,
Degreef
I
,
Didden
K
,
Fiews
S
,
De Smet
L
. Long term outcome of trapeziectomy with ligament reconstruction/tendon interposition versus thumb basal joint prosthesis. J Hand Surg Eur Vol. 2013;38(8):839–43. doi:.https://doi.org/10.1177/1753193412469010
67
Cebrian-Gomez
R
,
Lizaur-Utrilla
A
,
Sebastia-Forcada
E
,
Lopez-Prats
FA
. Outcomes of cementless joint prosthesis versus tendon interposition for trapeziometacarpal osteoarthritis: a prospective study. J Hand Surg Eur Vol. 2019;44(2):151–8. doi:.https://doi.org/10.1177/1753193418787151
68
Tchurukdichian
A
,
Guillier
D
,
Moris
V
,
See
LA
,
Macheboeuf
Y
. Results of 110 IVORY® prostheses for trapeziometacarpal osteoarthritis with a minimum follow-up of 10 years. J Hand Surg Eur Vol. 2020;45(5):458–64. doi:.https://doi.org/10.1177/1753193419899843
69
Froschauer
SM
,
Holzbauer
M
,
Hager
D
,
Schnelzer
R
,
Kwasny
O
,
Duscher
D
. Elektra prosthesis versus resection-suspension arthroplasty for thumb carpometacarpal osteoarthritis: a long-term cohort study. J Hand Surg Eur Vol. 2020;45(5):452–7. doi:.https://doi.org/10.1177/1753193419873230
70
Froschauer
SM
,
Holzbauer
M
,
Schnelzer
RF
,
Behawy
M
,
Kwasny
O
,
Aitzetmüller
MM
, et al.
Total arthroplasty with Ivory® prosthesis versus resection-suspension arthroplasty: a retrospective cohort study on 82 carpometacarpal-I osteoarthritis patients over 4 years. Eur J Med Res. 2020;25(1):13. doi:.https://doi.org/10.1186/s40001-020-00411-8
71
Lussiez
B
,
Ledoux
P
,
Falaise
C
. Prothèse trapèze-métacarpienne à double mobilité: revue d’une série de 132 cas à plus de 1 an de recul [Dual-mobility trapezio-metacarpal prosthesis: Report of 132 first cases with a minimum follow-up of 1 year]. Revue de Chirurgie Orthopédique et Traumatologique.
2017;103(7):S61. Article in French. doi: https://doi.org/10.1016/j.rcot.2017.09.092
72
Remy
S
,
Detrembleur
C
,
Libouton
X
,
Bonnelance
M
,
Barbier
O
. Trapeziometacarpal prosthesis: an updated systematic review. Hand Surg Rehabil. 2020;39(6):492–501. doi:.https://doi.org/10.1016/j.hansur.2020.08.005
73
Russo
S
,
Bernasconi
A
,
Busco
G
,
Sadile
F
. Treatment of the trapeziometacarpal osteoarthritis by arthroplasty with a pyrocarbon implant. Int Orthop. 2016;40(7):1465–71. doi:.https://doi.org/10.1007/s00264-015-3016-z
74
Barrera-Ochoa
S
,
Vidal-Tarrason
N
,
Correa-Vázquez
E
,
Reverte-Vinaixa
MM
,
Font-Segura
J
,
Mir-Bullo
X
. Pyrocarbon interposition (PyroDisk) implant for trapeziometacarpal osteoarthritis: minimum 5-year follow-up. J Hand Surg Am. 2014;39(11):2150–60. doi:.https://doi.org/10.1016/j.jhsa.2014.07.011
75
Erne
HC
,
Schmauß
D
,
Cerny
M
,
Schmauss
V
,
Ehrl
D
,
Löw
S
, et al.
Resektionsarthroplastik nach Lundborg vs. Pyrocarbon-Spacer (Pyrocardan®) bei fortgeschrittener Rhizarthrose – Eine Zwei-Center-Studie [Lundborg’s resection arthroplasty vs. Pyrocarbon spacer (Pyrocardan®) for the treatment of trapeziometacarpal joint osteoarthritis: a two-centre study]. Handchir Mikrochir Plast Chir. 2017;49(3):175–80. Article in German. dio:.https://doi.org/10.1055/s-0043-115220
76
Oh
WT
,
Chun
YM
,
Koh
IH
,
Shin
JK
,
Choi
YR
,
Kang
HJ
. Tendon versus Pyrocarbon Interpositional Arthroplasty in the Treatment of Trapeziometacarpal Osteoarthritis. BioMed Res Int. 2019;2019:7961507. doi:.https://doi.org/10.1155/2019/7961507
77
Gerace
E
,
Royaux
D
,
Gaisne
E
,
Ardouin
L
,
Bellemère
P
. Pyrocardan® implant arthroplasty for trapeziometacarpal osteoarthritis with a minimum follow-up of 5 years. Hand Surg Rehabil. 2020;39(6):528–38. doi:.https://doi.org/10.1016/j.hansur.2020.09.003
78
Odella
S
,
Querenghi
AM
,
Sartore
R
,
DE Felice
A
,
Dacatra
U
. Trapeziometacarpal osteoarthritis: pyrocarbon interposition implants. Joints. 2015;2(4):154–8.
79
Lauwers
TM
,
Brouwers
K
,
Staal
H
,
Hoekstra
LT
,
van der Hulst
RR
. Early outcomes of Pyrocardan® implants for trapeziometacarpal osteoarthritis. Hand Surg Rehabil. 2016;35(6):407–12. doi:.https://doi.org/10.1016/j.hansur.2016.09.004
80
Gauthier
E
,
Truffandier
MV
,
Gaisne
E
,
Bellemère
P
. Treatment of scaphotrapeziotrapezoid osteoarthritis with the Pyrocardan® implant: Results with a minimum follow-up of 2 years. Hand Surg Rehabil. 2017;36(2):113–21. doi:.https://doi.org/10.1016/j.hansur.2017.01.003
81
De Smet
L
,
Van Meir
N
,
Verhoeven
N
,
Degreef
I
. Is there still a place for arthrodesis in the surgical treatment of basal joint osteoarthritis of the thumb?
Acta Orthop Belg. 2010;76(6):719–24.
82
Rizzo
M
,
Moran
SL
,
Shin
AY
. Long-term outcomes of trapeziometacarpal arthrodesis in the management of trapeziometacarpal arthritis. J Hand Surg Am. 2009;34(1):20–6. doi:.https://doi.org/10.1016/j.jhsa.2008.09.022
83
Hartigan
BJ
,
Stern
PJ
,
Kiefhaber
TR
. Thumb carpometacarpal osteoarthritis: arthrodesis compared with ligament reconstruction and tendon interposition. J Bone Joint Surg Am. 2001;83(10):1470–8. doi:.https://doi.org/10.2106/00004623-200110000-00002
84
Taylor
EJ
,
Desari
K
,
D’Arcy
JC
,
Bonnici
AV
. A comparison of fusion, trapeziectomy and silastic replacement for the treatment of osteoarthritis of the trapeziometacarpal joint. J Hand Surg [Br]. 2005;30(1):45–9. doi:.https://doi.org/10.1016/J.JHSB.2004.08.006